The authors present a framework for conceptualizing interventions for children with differences in sensory processingand integration that incorporates multiple evidence-based approaches.
Abstract
Pediatric occupational therapy practitioners frequently provide interventions for children with differences in sensory processing and integration. Confusion exists regarding how best to intervene with these children and about how to describe and document methods. Some practitioners hold the misconception that Ayres Sensory Integration intervention is the only approach that can and should be used with this population. The issue is that occupational therapy practitioners must treat the whole client in varied environments; to do so effectively, multiple approaches to intervention often are required. This article presents a framework for conceptualizing interventions for children with differences in sensory processing and integration that incorporates multiple evidence-based approaches. To best meet the needs of the children and families seeking occupational therapy services, interventions must be focused on participation and should be multifaceted.
Differences in sensory processing and integration are prevalent in many of the children seen by pediatric occupational therapy practitioners and can be grouped broadly into two constructs: (1) differences in sensory responsivity, potentially leading to poor modulation of sensory information from the environment, and (2) differences in sensory discrimination and perception, potentially leading to deficits in postural stability, visual–motor control, and motor planning (Lane & Bundy, in press). Importantly, differences in sensory processing and integration have been shown to affect participation in meaningful childhood tasks including play with friends, performance at school, and engagement in family activities (Armstrong, Redman-Bentley, & Wardell, 2013; Cosbey, Johnston, & Dunn, 2010; Cosbey, Johnston, Dunn, & Bauman, 2012; Davis et al., 2013; Little, Ausderau, Sideris, & Baranek, 2015; Reynolds, Bendixen, Lawrence, & Lane, 2011; Shochat, Tzischinsky, & Engel-Yeger, 2009). Occupational therapists are recognized as the experts in assessment and intervention for children who have differences in sensory processing and integration. This recognition is in large part because of the efforts of A. Jean Ayres (1972), whose academic and clinical work led to the development of sensory integration theory, assessment tools to measure differences in sensory processing and integration in children, and the clearly defined intervention technique of sensory integration.
Sensory integration (SI) is a theory that attempts to link observable behaviors with underlying neurological functions and is used clinically to help explain behavior, plan interventions, and predict change. A primary assertion of SI theory is that learning is dependent on the ability to take in and process sensation from movement and the environment and use it to plan and organize behavior (Bundy & Murray, 2002). Interventions based on SI theory use enhanced sensory experiences as part of meaningful activity to improve the central nervous system’s ability to process sensation, thereby enhancing learning and behavior. Outcomes of SI intervention, therefore, are assumed to be the result of the brain’s ability to change, biochemically and structurally, in response to experiences in the environment (Reynolds, Lane, & Richards, 2010)
Historically, there has been some confusion about what is and is not SI treatment. Between 2007 and 2010, in an attempt to clarify and preserve SI as envisioned by Ayres, the term Ayres Sensory Integration® (ASI) was trademarked, and several publications documented the key features that must be present (Parham et al., 2007, 2011; Smith-Roley, Mailloux, Kuhaneck, & Glennon, 2007). Delineating what ASI is (and is not) has been essential in both clinical practice and research. From a clinical standpoint, clinicians who claim to be doing SI intervention but who are not adhering to the fidelity of Ayres’s model have been forced to reexamine their own clinical practice. From a research standpoint, critical reviews that claim that SI intervention is not effective, but that fail to exclude articles not meeting fidelity criteria, can be called into question. Overall, the movement to clarify and delineate ASI has been a positive and necessary step in this field of practice.
Unfortunately, a byproduct of this work appears to be additional confusion about what should and should not be included in occupational therapy interventions that aim to improve function and participation in children with differences in sensory processing and integration. More specifically, there appears to be a misconception both within and outside of the field that ASI is the only approach that can and should be used with this population. The issue is that as occupational therapy practitioners, we focus on treating the whole client, which includes the child as well as the family and support networks. In addition, practitioners deal with not only the complexity of a child’s underlying neurological or physical differences but also the impact of these differences on various areas of function across multiple environments. The purpose of this article is to present a framework for conceptualizing the various interventions that can support the functional and participation needs of children with differences in sensory processing and integration. This framework incorporates multiple evidence-based approaches available to pediatric occupational therapy practitioners and focuses on the overarching goal of increased function and participation.
Multifaceted Approach to Pediatric Intervention
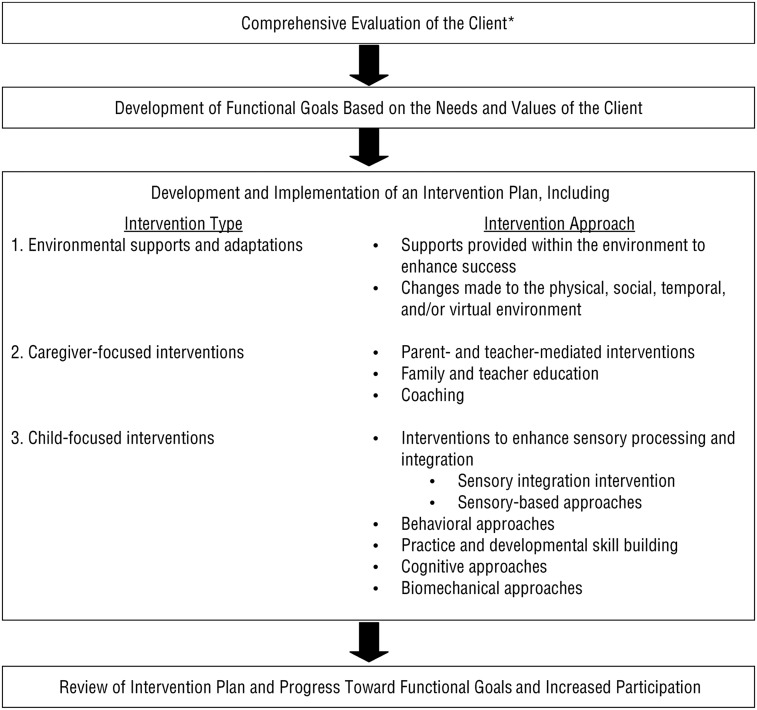
As part of the occupational therapy process, practitioners conduct a comprehensive evaluation, develop functional goals based on the needs and values of the client, and implement an intervention plan that aims to help enhance the function and participation of the client (American Occupational Therapy Association [AOTA], 2014). A systematic review of the literature (Bodison et al., in press) suggests that pediatric occupational therapy practitioners use three broad types of intervention when working with children who have differences in sensory processing and integration: (1) environmental supports and adaptations; (2) caregiver-focused interventions, including parent- and teacher-mediated interventions; and (3) child-focused, therapist-led interventions related primarily to skill building or eliciting neurological change.Within these three broad intervention types, various evidence-based approaches can be used as part of the intervention plan.
Although child-focused interventions are the most dominant and varied in clinical occupational therapy practice, all three intervention types should be considered in the intervention plan. An overview of each intervention type, along with associated intervention approaches, is provided in the sections that follow. Because a full systematic review was beyond the scope of this article, the literature featured in each section was purposefully sampled based on relevance to key theoretical principles, target population served (preferably children with differences in sensory processing and integration), and strength of available evidence. Figure 1 outlines the proposed multifaceted conceptual framework within the context of the broader occupational therapy process.
Figure 1.
Framework for conceptualizing intervention approaches that can support the functional goals of children with differences in sensory processing and integration as part of the occupational therapy process.
*Note. Client refers to the child with differences in sensory processing and integration and the people involved in the care of the child such as parents, teachers, and other professionals.
Environmental Supports and Adaptations
As part of their client evaluation, occupational therapists consider the impact of the environment on a child’s occupational performance (AOTA, 2014). In the current conceptualization, the term environment includes both the physical environment, such as the home and the classroom, and the cultural, social, temporal, and virtual environments (AOTA, 2014). For example, some sensory aspects of the physical environment can diminish a child’s ability to learn and participate in important daily activities (Barrett, Zhang, Moffat, & Kobbacy, 2013; Reynolds et al., 2011; Schaaf, Toth-Cohen, Johnson, Outten, & Benevides, 2011). Classroom environments can be stimulating (Choi & McPherson, 2005; Crandell & Smaldino, 2000; Shield & Dockrell, 2003), and visual and auditory stimuli in particular may distract students from learning activities (Fisher, Godwin, & Seltman, 2014; Godwin & Fisher, 2011; Klatte, Bergström, & Lachmann, 2013). Children’s attention and readiness for participation may also be influenced by sensory aspects of home and classroom routines.
In client-centered practice, the child is included in the process of deciding which environments to assess whenever possible. Using skill with activity analysis and observation in natural environments, in conjunction with the specific assessment results for the client, practitioners make recommendations for accommodations or modifications that match the child’s needs with provision of appropriate supports and removal of barriers that hinder functioning. Appropriate modifications to the environment are believed to support participation and typically include ways to reduce or enhance sensory stimulation from the environment to promote regulation and attention or to improve behavior. Environmental interventions to enhance sensory stimulation include altered seating (e.g., ball chairs, air cushions, rocker chairs), compression clothing, fidget toys, and weighted tools. Environmental interventions to reduce sensory stimuli include the use of headphones, visors, sunglasses, study carrels, light covers, and special surfaces for soundproofing.
There is preliminary evidence that guides best practice when implementing environmental modifications such as the use of alternative seating (Bagatell, Mirigliani, Patterson, Reyes, & Test, 2010; Case-Smith, Weaver, & Fristad, 2015; Fedewa & Erwin, 2011; Pfeiffer, Henry, Miller, & Witherell, 2008; Schilling & Schwartz, 2004; Schilling, Washington, Billingsley, & Deitz, 2003; Umeda & Deitz, 2011), modifications to the dental environment (Cermak et al., 2015), and changes to sounds and lighting in the classroom (Kinnealey et al., 2012; Reynolds, Kuhaneck, & Pfeiffer, 2016). Other approaches, such as the use of weighted vests, have limited to no evidence to support their continued use (Case-Smith et al., 2015; Watling & Hauer, 2015). Therefore, before including environmental adaptations as part of the intervention plan, it is important to consider the evidence available for the specific type of intervention because research findings are mixed and environmental interventions vary greatly.
Caregiver-Focused Interventions
When considering the impact of a child’s sensory experiences on family occupations and school participation, the concept of caregiver-focused interventions is integral to pediatric occupational therapy practice (AOTA, 2014; Bagby, Dickie, & Baranek, 2012; Case-Smith, 2013). As part of a multifaceted approach to pediatric intervention, the occupational therapy practitioner may work to develop the parent or teacher’s ability to facilitate learning opportunities for the child, scaffold the child’s participation in meaningful tasks, and skillfully respond to the child’s sensory needs.
Coaching and caregiver-mediated intervention approaches are increasingly being used as part of the therapeutic process, particularly in young children with autism spectrum disorder (ASD; Oono, Honey, & McConachie, 2013). Recent studies suggest that these approaches have a positive impact on a variety of outcomes such as play and social skills (Wilkes-Gillan, Bundy, Cordier, & Lincoln, 2016), social–emotional development (Case-Smith, 2013), as well as joint attention and social communication (Dawson et al., 2010; Kasari, Gulsrud, Wong, Kwon, & Locke, 2010). Outcomes such as reduced parental stress, increased maternal competency, improved family relationships, and enhanced parenting efficacy have also been noted with these types of intervention approaches (Bendixen et al., 2011; Graham, Rodger, & Ziviani, 2013; Kingsley & Mailloux, 2013), thus illustrating the importance of supporting the family system within which the child functions as a key component of client-centered occupational therapy.
A small number of studies have specifically included children with differences in sensory processing and integration as their target population or included related sensory processing outcomes when using a caregiver-focused intervention. For example, Baranek and colleagues (2015) implemented a 6- to 9-mo parent-mediated intervention aimed at improving developmental outcomes in a community sample of young children at risk for ASD. Parent–child interactions and adaptive behaviors improved, as did sensory responsiveness. In addition, using a contextual intervention with children with ASD and identified sensory challenges, Dunn, Cox, Foster, Mische-Lawson, and Tanquary (2012) found significant improvements in children’s daily participation and increased parent competency after 10 reflective coaching sessions.
Because of the effectiveness of coaching and parent-mediated interventions, occupational therapy practitioners should consider implementing these types of caregiver-focused interventions as part of a multifaceted intervention plan when working with children who have differences in sensory processing and integration. These intervention approaches may be initiated with a variety of functional outcomes and are closely aligned with traditional occupational therapy practices. In addition, these interventions often build on family strengths, occur in natural contexts, and are embedded in daily occupations, all of which further support goal acquisition.
Child-Focused Interventions
Intervention for children with differences in sensory processing and integration may include approaches explicitly designed to enhance sensory processing and integration as well as approaches targeting other behaviors and skills that that are affected by sensory processing difficulties, such as dressing, play, or self-regulation. Five approaches that may be used with this population of children are featured here.
Interventions to Enhance Sensory Processing and Integration.
Two types of child-focused, therapist-led interventions relate primarily to enhancing sensory processing abilities or eliciting neurological change: (1) therapist-led interventions grounded in the theory, assessment, and intervention strategies outlined by ASI and (2) therapist-led sensory-based approaches that are often protocol driven.
Therapist-led interventions grounded in ASI and that account for each child’s preferences and intrinsic motivation are clearly defined, and recent research has used an intervention manual and fidelity measure to assess adherence to the manualized intervention (Parham et al., 2011). A growing body of well-designed research studies has investigated the efficacy of these interventions. Thus far, positive outcomes of ASI have been identified in the areas of self-care, play, and participation in family routines (Pfeiffer, Koenig, Kinnealey, Sheppard, & Henderson, 2011; Schaaf, Benevides, Kelly, & Mailloux-Maggio, 2012; Schaaf et al., 2014; Watling & Hauer, 2015). These findings suggest that therapist-led interventions grounded in ASI may be a key component of a multifaceted intervention plan that focuses on outcomes related to function and participation.
Therapist-led sensory-based approaches include programs that address single sensory systems, such as sound-based programs (e.g., Therapeutic Listening, Vital Links, Madison, WI), and that incorporate SI theory constructs with other types of intervention practices, for example, Interactive Metronome (IM; Sunrise, FL), Astronaut Training (Vital Links), and the Alert Program (Williams & Shellenberger, 1996). These approaches are less clearly defined than therapist-led ASI interventions, both in practice and in the literature (Polatajko & Cantin, 2010). In addition, evidence is limited on the efficacy of these approaches; the few studies available have methodological challenges such as small sample sizes, lack of control groups, and poorly defined interventions. Future research related to these interventions should focus on clearly defining the constructs under study, the intended population, and the specific targeted outcomes.
Behavioral Approaches.
Behavioral approaches are primarily concerned with modifying observable behaviors that can be recorded and measured (Skinner, 1938; Watson, 1913). Children with differences in sensory processing and integration may exhibit aggressive, avoidance, or seeking behaviors as a result of sensory modulation problems; have difficulty learning new skills or expanding play schemas because they struggle with praxis; or may choose not to engage in tasks that are perceived to be too difficult secondary to postural or motor challenges. Behavioral approaches may be beneficial for some children with difficulties in sensory processing and integration to target specific, discrete behaviors that may need to be developed (e.g., the ability to complete a dressing sequence), elicited (e.g., engagement in a difficult yet achievable motor action), or reduced (e.g., aggression toward a teacher) to facilitate optimal participation.
Common behavioral intervention strategies include introducing or removing environmental cues that trigger a behavior, teaching an alternative behavior when a specific cue is present, and prompting a response that is not independently exhibited (Watling, 2015). Reward and reinforcement can be provided to enhance learning of desired skills and may be based on the child’s specific sensory preferences.
Incorporating an extensive range of approaches that are based on behavior theory, positive behavioral support (PBS) is a widely implemented intervention aimed at proactively enhancing competency in the school, home, and community (Dunlap et al., 2010). PBS uses techniques such as environmental or curricular redesign to address goodness of fit between the context and client (Albin, Lucyshyn, Horner, & Flannery, 1996). PBS has been shown to produce improved academic performance, improved quality of life, and reduced negative behavior (Dunlap et al., 2010). Although the research has not specifically examined use of PBS for children with differences in sensory processing and integration, favorable outcomes have been found for children with developmental disabilities (Carr et al., 1999; Feldman, Condillac, Tough, Hunt, & Griffiths, 2002), emotional and behavioral disorders (Chitiyo, Makweche-Chitiyo, Park, Ametepee, & Chitiyo, 2010), and autism (Horner, Carr, Strain, Todd, & Reed, 2002)—conditions that are often accompanied by poor sensory processing and integration.
By providing positive behavioral supports for children with differences in sensory processing and integration, occupational therapy practitioners may evaluate how sensory experiences serve as antecedents for undesirable behaviors and identify positive sensory experiences to use as rewards for reinforcing desirable behaviors. Creating environments that are consistent and predictable with regard to physical and social features can also help to decrease the processing load, lead to reduced vigilance and anxiety, and allow the child to focus attention on a functional task rather than constantly evaluate the environment for sensory threats. As part of a multifaceted intervention plan, behavioral approaches can be used in concert with other approaches to enhance learning and support engagement in daily or therapeutic activities.
Practice and Developmental Skill Building.
The concept of practice is a major tenet of motor learning theory, and the effects of practice on functional task performance have been well studied in the literature (Zwicker & Harris, 2009). The type and amount of practice given to typical children during their daily routine are simply not enough for children with differences in sensory processing and integration to learn or master the functional skills necessary for participation in school, home, or community activities. However, research suggests that interventions that strategically manipulate the timing and organization of skilled motor practice (e.g., distributed practice schedules) can lead to learning-dependent changes in the primary motor cortex and to measurable outcomes in motor skill performance (Kwon, Kwon, & Lee, 2015; Rroji, van Kuyck, Nuttin, & Wenderoth, 2015; Willingham, 1998). Interestingly, similar changes in both brain structure and motor function have been noted with mental practice or visual–motor imagery (Avanzino et al., 2015). Improvements in daily living skills, safety, and social skills after practice in virtual contexts (i.e., virtual reality) have also been documented (den Brok & Sterkenburg, 2015). Although much of motor learning and practice-based research has been done with adults, a growing body of literature supports its use in pediatric populations (for a review, see Zwicker & Harris, 2009).
Feedback is an important concept associated with practice and motor learning. Extrinsic (or augmented) feedback refers to feedback that is added to what is typically received by a person while performing a task (Schmidt & Lee, 2005). In adults, frequent extrinsic feedback is thought to reduce reliance on intrinsic feedback and decrease the overall information-processing demands during practice trials. Subsequently, motor learning research suggests that faded and reduced extrinsic feedback is preferable in adults to engage active problem-solving mechanisms and improve skill retention over time (Anderson, Magill, Sekiya, & Ryan, 2005; Winstein & Schmidt, 1990). However, research suggests that typical children use feedback in a manner different from adults and may require longer periods of practice with more frequent feedback to retain new motor skills (Goh, Kantak, & Sullivan, 2012; Sullivan, Kantak, & Burtner, 2008). This requirement may be particularly true for children with differences in sensory processing and integration who cannot always rely on accurate intrinsic feedback from their body. Interestingly, research also shows that nongeneric feedback (e.g., “Those last kicks were very good”) is preferable to generic feedback (e.g., “You are a great soccer player”) when children are learning new motor tasks (Chiviacowsky & Drews, 2014).
Developmental theories also emphasize practice and skill acquisition as a basis for functional performance and participation; however, a greater emphasis is placed on ascertaining a child’s current developmental level as a basis for determining which skills or patterns should be attained, and in what sequence, during the intervention process (Kramer & Hinojosa, 2010). Working with a child to first practice cutting straight lines before learning to cut curves or turn corners is an example of how occupational therapy practitioners often consider normal developmental trajectories in the context of skill building.
Handwriting is one area of participation that is often difficult for children with differences in sensory processing and integration. Although handwriting difficulties may stem from underlying difficulties in sensory discrimination or praxis, interventions that use sensory-based approaches without handwriting practice have generally been shown to be ineffective (Hoy, Egan, & Feder, 2011). Therefore, for these children with handwriting difficulties, a multifaceted intervention plan should include the use of therapeutic handwriting practice, particularly when a child cannot participate in expected school-based tasks. Keys to successful practice for these children is for practitioners to assess the appropriate developmental skill level of the child to set up the just-right challenge and to provide augmented feedback of both task performance and task results (Zwicker & Harris, 2009).
Cognitive Approaches.
Some children with differences in sensory processing and integration do not receive accurate information from their bodies during task performance (e.g., poor tactile, proprioceptive, or vestibular discrimination) and secondarily cannot effectively draw on past experiences when refining or developing new motor plans. For these children, cognitive approaches may be used in conjunction with interventions to enhance sensory processing and integration as a way to enhance motor skills and motor planning needed for successful participation in daily living activities.
Specific cognitive approaches that may be useful for children with differences in sensory processing and integration include problem-solving interventions such as the Cognitive Orientation to daily Occupational Performance (CO–OP; Polatajko & Mandich, 2004) and neuromotor task training (NTT; Niemeijer, Smits‐Engelsman, & Schoemaker, 2007). Several studies support the use of CO–OP and NTT for children who have difficulties with motor coordination, including children with developmental coordination disorder (DCD) and ASD (Hyland & Polatajko, 2012; Rodger & Brandenburg, 2009; Rodger, Pham, & Mitchell, 2009; Smits-Engelsman et al., 2013).
CO–OP uses a four-phase process in which the occupational therapy practitioner works with the child to (1) identify goals for participation, (2) develop a plan, (3) execute the plan, and (4) evaluate the success of the plan (Missiuna, Mandich, Polatajko, & Malloy-Miller, 2001). During this process, the practitioner serves as the child’s coach or guide; however, recent evidence suggests that children’s ability to self-monitor may improve over time and carry over to other functional tasks (Jokić, Polatajko, & Whitebread, 2013). Similarly, NTT aims to develop a child’s metacognitive skills as a way to improve motor performance. In NTT, practitioners guide children through different phases of motor learning by manipulating task and environmental demands and using techniques such as guided discovery (Schoemaker & Smits-Engelsman, 2005).
Note that these types of top-down, task-based approaches are not intended to address the child’s underlying issues in sensory processing and integration but may be used to help children with motor planning or coordination difficulties learn strategies to enhance performance of specific functional skills. Practitioners considering using CO–OP or NTT as part of a multifaceted intervention plan should consider whether the child has the intellectual, speech, language, and self-regulatory abilities to benefit from such problem-solving approaches.
Other cognitive approaches that may be helpful for children with sensory processing and integration differences include the use of low- and high-tech cognitive aids for prompting during functional tasks. Use of videos (e.g., video modeling) and pictures on handheld devices, in particular, have been shown to improve performance of daily living skills and vocational tasks (den Brok & Sterkenburg, 2015). Importantly, although problem-solving approaches such as CO–OP require intact cognitive abilities, preliminary evidence suggests that video modeling may be effective for children with intellectual disabilities (Walton & Ingersoll, 2013).
Biomechanical Approaches.
Children with differences in sensory processing and integration may present with low muscle tone, poor alignment, or inadequate postural strength and stability to effectively or efficiently participate in functional self-care or play tasks. Biomechanical approaches, therefore, may be incorporated as part of a multifaceted intervention plan to position the child during functional tasks or enhance client factors such as muscle strength, position sense, and endurance. For example, two case studies have demonstrated the benefits of a supervised strength-training intervention for children with DCD (Kaufman & Schilling, 2007; Menz, Hatten, & Grant-Beuttler, 2013). In both studies, strength training involved a high number of repetitions with low resistance, with a focus on proper positioning and technique during the exercises. Although both cases demonstrated only minimal improvement in standardized scores on the Bruininks–Oseretsky Test of Motor Proficiency (Bruininks & Bruininks, 2005), functional gains were noted in playground skills (e.g., monkey bars, climbing on jungle gym), and increased confidence and participation were reported for motor tasks. Other therapeutic or recreational activities that may promote participation through improvement in muscle strength and endurance for children with sensory processing and integration differences include (but are not limited to) martial arts (Fong, Chung, Chow, Ma, & Tsang, 2013), horseback riding (Ajzenman, Standeven, & Shurtleff, 2013), and aquatic programs (Hillier, McIntyre, & Plummer, 2010).
Directions for Action
Occupational therapy practitioners can provide a broad and diverse range of evidence-based services to children with differences in sensory processing and integration to enhance function and participation. This message needs to be communicated clearly to those outside of the profession who may view pediatric occupational therapy an ASI-only endeavor or who may not recommend occupational therapy in settings where the delivery of ASI is not possible (e.g., in regular education classrooms). In addition, within the profession, dialogue should be undertaken on how to best address the needs of children with differences in sensory processing and integration across multiple contexts. Specifically, this dialogue should include how outpatient and school-based practitioners can collaborate to develop an optimal plan of care through the implementation of varied approaches that successfully address contextually based activity requirements.
Trained and experienced pediatric practitioners are equipped with the clinical reasoning skills to address treatment goals from multiple angles. Through the work of many, pediatric occupational therapy also has several researched-based intervention approaches that can be used in concert, based on the needs of the client, to promote optimal function and participation. As the profession moves forward, it is important that practitioners are explicit about what intervention approaches they use and why, state the evidence to support them, and document their contribution to enhancing children’s function and participation.
Looking ahead, it may be helpful to develop tools to help clinicians choose which intervention types and approaches may best suit specific client needs and goals. For example, a clinical decision-making tree could be developed to systematically analyze a variety of client factors (e.g., presence of symptoms, areas of strength, other services currently being received), in combination with the strength of current evidence, to decide which approaches or combination of approaches should be prioritized in the intervention plan. Similarly, specific intervention approaches may be more useful for children who present with specific categories or subtypes of sensory processing differences or with certain associated conditions such as ASD or attention deficit hyperactivity disorder. Systematic methods for decision analysis may be used by occupational therapy practitioners to make treatment decisions with their individual clients, by researchers to manualize occupational therapy interventions, and by health administrators to economically appraise health care programs.
Conclusion
In summary, to meet the complex needs of children and their families, occupational therapy interventions must be participation focused and multifaceted. The list of intervention types and approaches outlined in the framework presented (Figure 1) is intended to be a starting point for a discussion among a community of practitioners, researchers, and scholars who have knowledge and experience to share. Clearly, each client is unique; therefore, the design of an intervention plan will be established with the full consideration of the client’s values, needs, and goals. Moreover, the selection of interventions to use when working with children who have differences in sensory processing and integration should evolve over time based on changes in the evidence and on critical appraisal from the profession.
Acknowledgments
We acknowledge the American Occupation Therapy Association (AOTA), which has continued to provide a location for our annual Pediatric Research Interest Group meeting during the AOTA Annual Conference. In addition, we acknowledge the following funding sources for support: National Institutes of Health/National Center for Research Resources/National Center for Advancing Translational Sciences Grant KL2TR000131 and the University of Southern California Division of Occupational Science and Occupational Therapy (Stephanie C. Bodison) and Quinnipiac University School of Health Sciences (Tara J. Glennon).
Contributor Information
Stacey Reynolds, Stacey Reynolds, PhD, OTR/L, is Associate Professor, Department of Occupational Therapy, Virginia Commonwealth University, Richmond; reynoldsse3@vcu.edu.
Tara J. Glennon, Tara J. Glennon, EdD, OTR/L, FAOTA, is Professor of Occupational Therapy, Quinnipiac University, Hamden, CT
Karla Ausderau, Karla Ausderau, PhD, OTR/L, is Assistant Professor, Department of Kinesiology, Occupational Therapy Program, University of Wisconsin, Madison.
Roxanna M. Bendixen, Roxanna M. Bendixen, PhD, OTR/L, is Assistant Professor, Department of Occupational Therapy, University of Pittsburgh, Pittsburgh, PA
Heather Miller Kuhaneck, Heather Miller Kuhaneck, PhD, OTR/L, FAOTA, is Associate Professor of Occupational Therapy, Sacred Heart University, Fairfield, CT.
Beth Pfeiffer, Beth Pfeiffer, PhD, OTR/L, BCP, is Associate Professor, Department of Rehabilitation Sciences, Temple University, Philadelphia, PA.
Renee Watling, Renee Watling, PhD, OTR/L, FAOTA, is Visiting Assistant Professor, University of Puget Sound, Tacoma, WA.
Kimberly Wilkinson, Kimberly Wilkinson, PhD, OTR/L, is Assistant Professor of Occupational Therapy, Ithaca College, Ithaca, NY.
Stefanie C. Bodison, Stefanie C. Bodison, OTD, OTR/L, is Assistant Professor, Division of Occupational Science and Occupational Therapy, University of Southern California, Los Angeles
References
- Ajzenman H. F., Standeven J. W., & Shurtleff T. L. (2013). Effect of hippotherapy on motor control, adaptive behaviors, and participation in children with autism spectrum disorder: A pilot study. American Journal of Occupational Therapy, 67, 653–663. https://doi.org/10.5014/ajot.2013.008383 [DOI] [PubMed] [Google Scholar]
- Albin R. W., Lucyshyn L. M., Horner R. H., & Flannery K. B. (1996). Contextual fit for behavior support plans: A model for a goodness-of-fit. In Koegel L. K., Koegel R. L., & Dunlap G. (Eds.), Positive behavior support: Including people with difficult behavior in the community (pp. 81–89). Baltimore: Brookes. [Google Scholar]
- American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and Process (3rd ed.). American Journal of Occupational Therapy, 68(Suppl. 1), S1–S48. https://doi.org/10.5014/ajot.2014.682006 [PubMed] [Google Scholar]
- Anderson D. I., Magill R. A., Sekiya H., & Ryan G. (2005). Support for an explanation of the guidance effect in motor skill learning. Journal of Motor Behavior, 37, 231–238. https://doi.org/10.3200/JMBR.37.3.231-238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong D. C., Redman-Bentley D., & Wardell M. (2013). Differences in function among children with sensory processing disorders, physical disabilities, and typical development. Pediatric Physical Therapy, 25, 315–321. https://doi.org/10.1097/PEP.0b013e3182980cd4 [DOI] [PubMed] [Google Scholar]
- Avanzino L., Gueugneau N., Bisio A., Ruggeri P., Papaxanthis C., & Bove M. (2015). Motor cortical plasticity induced by motor learning through mental practice. Frontiers in Behavioral Neuroscience, 9, 105 https://doi.org/10.3389/fnbeh.2015.00105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayres A. J. (1972). Sensory integration and learning disorders. Los Angeles: Western Psychological Services. [Google Scholar]
- Bagatell N., Mirigliani G., Patterson C., Reyes Y., & Test L. (2010). Effectiveness of therapy ball chairs on classroom participation in children with autism spectrum disorders. American Journal of Occupational Therapy, 64, 895–903. https://doi.org/10.5014/ajot.2010.09149 [DOI] [PubMed] [Google Scholar]
- Bagby M. S., Dickie V. A., & Baranek G. T. (2012). How sensory experiences of children with and without autism affect family occupations. American Journal of Occupational Therapy, 66, 78–86. https://doi.org/10.5014/ajot.2012.000604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baranek G. T., Watson L. R., Turner-Brown L., Field S. H., Crais E. R., Wakeford L., . . . Reznick J. S. (2015). Preliminary efficacy of adapted responsive teaching for infants at risk of autism spectrum disorder in a community sample. Autism Research and Treatment, 2015, 386951 https://doi.org/10.1155/2015/386951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett P., Zhang Y., Moffat J., & Kobbacy K. (2013). A holistic, multi-level analysis identifying the impact of classroom design on pupils’ learning. Building and Environment, 59, 678–689. https://doi.org/10.1016/j.buildenv.2012.09.016 [Google Scholar]
- Bendixen R. M., Elder J. H., Donaldson S., Kairalla J. A., Valcante G., & Ferdig R. E. (2011). Effects of a father-based in-home intervention on perceived stress and family dynamics in parents of children with autism. American Journal of Occupational Therapy, 65, 679–687. https://doi.org/10.5014/ajot.2011.001271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodison S. C., Glennon T. J., Reynolds S., Kuhaneck H. M., Watling R., Pfeiffer B., & Wilkinson K. (in press). Evaluating the effectiveness of occupational therapy interventions used in clinical settings to improve sensory processing and integration in children with developmental and behavioral disorders: A systematic review. American Journal of Occupational Therapy. [Google Scholar]
- Bruininks R., & Bruininks B. (2005). Bruininks–Oseretsky Test of Motor Proficiency (2nd ed.). Minneapolis: NCS Pearson. [Google Scholar]
- Bundy A. C., & Murray E. A. (2002). Sensory integration: A. Jean Ayres’ theory revisited. In Bundy A. C., Lane S. J., & Murray E. A. (Eds.), Sensory integration theory and practice (2nd ed., pp. 3–29). Philadelphia: F. A. Davis. [Google Scholar]
- Carr E. G., Horner R. H., Turnbull A. P., Marquis J., Magito-McLaughlin D., McAtee M. L., . . . Dooblah A. (1999). Positive behavior support for people with developmental disabilities: A research synthesis. Washington, DC: American Association on Mental Retardation. [Google Scholar]
- Case-Smith J. (2013). Systematic review of interventions to promote social–emotional development in young children with or at risk for disability. American Journal of Occupational Therapy, 67, 395–404. https://doi.org/10.5014/ajot.2013.004713 [DOI] [PubMed] [Google Scholar]
- Case-Smith J., Weaver L. L., & Fristad M. A. (2015). A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism, 19, 133–148. https://doi.org/10.1177/1362361313517762 [DOI] [PubMed] [Google Scholar]
- Cermak S. A., Duker L. I. S., Williams M. E., Lane C. J., Dawson M. E., Borreson A. E., & Polido J. C. (2015). Feasibility of a sensory-adapted dental environment for children with autism. American Journal of Occupational Therapy, 69, 6903220020 https://doi.org/10.5014/ajot.2015.013714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chitiyo M., Makweche-Chitiyo P., Park M., Ametepee L. K., & Chitiyo J. (2010). Examining the effect of positive behavior support on academic achievement of students with disabilities. Journal of Research in Special Educational Needs, 11, 171–177. https://doi.org/10.1111/j.1471-3802.2010.01156.x [Google Scholar]
- Chiviacowsky S., & Drews R. (2014). Effects of generic versus non-generic feedback on motor learning in children. PLoS One, 9, e88989 https://doi.org/10.1371/journal.pone.0088989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi C. Y., & McPherson B. (2005). Noise levels in Hong Kong primary schools: Implications for classroom listening. International Journal of Disability Development and Education, 52, 345–360. https://doi.org/10.1080/10349120500348714 [Google Scholar]
- Cosbey J., Johnston S. S., & Dunn M. L. (2010). Sensory processing disorders and social participation. American Journal of Occupational Therapy, 64, 462–473. https://doi.org/10.5014/ajot.2010.09076 [DOI] [PubMed] [Google Scholar]
- Cosbey J., Johnston S. S., Dunn M. L., & Bauman M. (2012). Playground behaviors of children with and without sensory processing disorders. OTJR: Occupation, Participation and Health, 32, 39–47. [Google Scholar]
- Crandell C., & Smaldino J. (2000). Classroom acoustics for children with normal hearing and with hearing impairment. Language, Speech, and Hearing Services in Schools, 31, 362–370. https://doi.org/10.1044/0161-1461.3104.362 [DOI] [PubMed] [Google Scholar]
- Davis A. M., Bruce A. S., Khasawneh R., Schulz T., Fox C., & Dunn W. (2013). Sensory processing issues in young children presenting to an outpatient feeding clinic. Journal of Pediatric Gastroenterology and Nutrition, 56, 156–160. https://doi.org/10.1097/MPG.0b013e3182736e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G., Rogers S., Munson J., Smith M., Winter J., Greenson J., . . . Varley J. (2010). Randomized, controlled trial of an intervention for toddlers with autism: The Early Start Denver Model. Pediatrics, 125, e17–e23. https://doi.org/10.1542/peds.2009-0958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Brok W. L., & Sterkenburg P. S. (2015). Self-controlled technologies to support skill attainment in persons with an autism spectrum disorder and/or an intellectual disability: A systematic literature review. Disability and Rehabilitation, 10, 1–10. https://doi.org/10.3109/17483107.2014.921248 [DOI] [PubMed] [Google Scholar]
- Dunlap G., Carr E. G., Horner R. H., Koegel R. L., Sailor W., Clarke S., . . . Fox L. (2010). A descriptive, multiyear examination of positive behavior support. Behavioral Disorders, 35, 259–279. [Google Scholar]
- Dunn W., Cox J., Foster L., Mische-Lawson L., & Tanquary J. (2012). Impact of a contextual intervention on child participation and parent competence among children with autism spectrum disorders: A pretest–posttest repeated-measures design. American Journal of Occupational Therapy, 66, 520–528. https://doi.org/10.5014/ajot.2012.004119 [DOI] [PubMed] [Google Scholar]
- Fedewa A. L., & Erwin H. E. (2011). Stability balls and students with attention and hyperactivity concerns: Implications for on-task and in-seat behavior. American Journal of Occupational Therapy, 65, 393–399. https://doi.org/10.5014/ajot.2011.000554 [DOI] [PubMed] [Google Scholar]
- Feldman M. A., Condillac R. A., Tough S., Hunt S., & Griffiths D. (2002). Effectiveness of community positive behavioral intervention for persons with developmental disabilities and severe behavior disorders. Behavior Therapy, 33, 377–398. https://doi.org/10.1016/S0005-7894(02)80034-X [Google Scholar]
- Fisher A. V., Godwin K. E., & Seltman H. (2014). Visual environment, attention allocation, and learning in young children: When too much of a good thing may be bad. Psychological Science, 25, 1362–1370. https://doi.org/10.1177/0956797614533801 [DOI] [PubMed] [Google Scholar]
- Fong S. S. M., Chung J. W. Y., Chow L. P. Y., Ma A. W. W., & Tsang W. W. N. (2013). Differential effect of Taekwondo training on knee muscle strength and reactive and static balance control in children with developmental coordination disorder: A randomized controlled trial. Research in Developmental Disabilities, 34, 1446–1455. https://doi.org/10.1016/j.ridd.2013.01.025 [DOI] [PubMed] [Google Scholar]
- Godwin K. E., & Fisher A. V. (2011). Allocation of attention in classroom environments: Consequences for learning. In Carlson L. A., Hölscher C., Shipley T. G. (Eds.), Proceedings of the 33rd Annual Conference of the Cognitive Science Society (pp. 2806–2811). Austin, TX: Cognitive Science Society. [Google Scholar]
- Goh H. T., Kantak S. S., & Sullivan K. J. (2012). Movement pattern and parameter learning in children: Effects of feedback frequency. Research Quarterly for Exercise and Sport, 83, 346–352. [DOI] [PubMed] [Google Scholar]
- Graham F., Rodger S., & Ziviani J. (2013). Effectiveness of occupational performance coaching in improving children’s and mothers’ performance and mothers’ self-competence. American Journal of Occupational Therapy, 67, 10–18. https://doi.org/10.5014/ajot.2013.004648 [DOI] [PubMed] [Google Scholar]
- Hillier S., McIntyre A., & Plummer L. (2010). Aquatic physical therapy for children with developmental coordination disorder: A pilot randomized controlled trial. Physical and Occupational Therapy in Pediatrics, 30, 111–124. https://doi.org/10.3109/01942630903543575 [DOI] [PubMed] [Google Scholar]
- Horner R. H., Carr E. G., Strain P. S., Todd A. W., & Reed H. K. (2002). Problem behavior interventions for young children with autism: A research synthesis. Journal of Autism and Developmental Disorders, 32, 423–446. https://doi.org/10.1023/A:1020593922901 [DOI] [PubMed] [Google Scholar]
- Hoy M. M., Egan M. Y., & Feder K. P. (2011). A systematic review of interventions to improve handwriting. Canadian Journal of Occupational Therapy, 78, 13–25. https://doi.org/10.2182/cjot.2011.78.1.3 [DOI] [PubMed] [Google Scholar]
- Hyland M., & Polatajko H. J. (2012). Enabling children with developmental coordination disorder to self-regulate through the use of dynamic performance analysis: Evidence from the CO–OP approach. Human Movement Science, 31, 987–998. https://doi.org/10.1016/j.humov.2011.09.003 [DOI] [PubMed] [Google Scholar]
- Jokić C. S., Polatajko H., & Whitebread D. (2013). Self-regulation as a mediator in motor learning: The effect of the cognitive orientation to occupational performance approach on children with DCD. Adapted Physical Activity Quarterly, 30, 103–126. [DOI] [PubMed] [Google Scholar]
- Kasari C., Gulsrud A. C., Wong C., Kwon S., & Locke J. (2010). Randomized controlled caregiver mediated joint engagement intervention for toddlers with autism. Journal of Autism and Developmental Disorders, 40, 1045–1056. https://doi.org/10.1007/s10803-010-0955-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman L. B., & Schilling D. L. (2007). Implementation of a strength training program for a 5-year-old child with poor body awareness and developmental coordination disorder. Physical Therapy, 87, 455–467. https://doi.org/10.2522/ptj.20060170 [DOI] [PubMed] [Google Scholar]
- Kingsley K., & Mailloux Z. (2013). Evidence for the effectiveness of different service delivery models in early intervention services. American Journal of Occupational Therapy, 67, 431–436. https://doi.org/10.5014/ajot.2013.006171 [DOI] [PubMed] [Google Scholar]
- Kinnealey M., Pfeiffer B., Miller J., Roan C., Shoener R., & Ellner M. L. (2012). Effect of classroom modification on attention and engagement of students with autism or dyspraxia. American Journal of Occupational Therapy, 66, 511–519. https://doi.org/10.5014/ajot.2012.004010 [DOI] [PubMed] [Google Scholar]
- Klatte M., Bergström K., & Lachmann T. (2013). Does noise affect learning? A short review on noise effects on cognitive performance in children. Frontiers in Psychology, 4, 578 https://doi.org/10.3389/fpsyg.2013.00578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer P., & Hinojosa J. (2010). Developmental perspective: Fundamentals of Developmental Theory. In Kramer P. & Hinojosa J. (Eds.), Frames of reference for pediatric occupational therapy (3rd ed., pp. 23–29). Baltimore: Lippincott Williams & Wilkins. [Google Scholar]
- Kwon Y. H., Kwon J. W., & Lee M. H. (2015). Effectiveness of motor sequential learning according to practice schedules in healthy adults: Distributed practice versus massed practice. Journal of Physical Therapy Science, 27, 769–772. https://doi.org/10.1589/jpts.27.769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane S. J., & Bundy A. (in press). Theoretical constructs of sensory integration: A. Jean Ayres’ theory revisited. In Lane S. J., Bundy A. C., Mulligan S., & Reynolds (Eds.), Sensory integration theory and practice (3rd ed.). Philadelphia: F. A. Davis. [Google Scholar]
- Little L. M., Ausderau K., Sideris J., & Baranek G. T. (2015). Activity participation and sensory features among children with autism spectrum disorders. Journal of Autism and Developmental Disorders, 45, 2981–2990. https://doi.org/10.1007/s10803-015-2460-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menz S. M., Hatten K., & Grant-Beuttler M. (2013). Strength training for a child with suspected developmental coordination disorder. Pediatric Physical Therapy, 25, 214–223. https://doi.org/10.1097/PEP.0b013e31828a2042 [DOI] [PubMed] [Google Scholar]
- Missiuna C., Mandich A. D., Polatajko H. J., & Malloy-Miller T. (2001). Cognitive Orientation to daily Occupational Performance (CO–OP): Part I—Theoretical foundations. Physical and Occupational Therapy in Pediatrics, 20, 69–81. https://doi.org/10.1080/J006v20n02_05 [PubMed] [Google Scholar]
- Niemeijer A. S., Smits‐Engelsman B. C., & Schoemaker M. M. (2007). Neuromotor task training for children with developmental coordination disorder: A controlled trial. Developmental Medicine and Child Neurology, 4, 406–411. https://doi.org/10.1111/j.1469-8749.2007.00406.x [DOI] [PubMed] [Google Scholar]
- Oono I. P., Honey E. J., & McConachie H. (2013). Parent-mediated early intervention for young children with autism spectrum disorders (ASD). Evidence-Based Child Health: A Cochrane Review Journal, 8, CD009774 https://doi.org/10.1002/ebch.1952 [DOI] [PubMed] [Google Scholar]
- Parham L. D., Cohn E. S., Spitzer S., Koomar J. A., Miller L. J., Burke J. P., . . . Summers C. A. (2007). Fidelity in sensory integration intervention research. American Journal of Occupational Therapy, 61, 216–227. https://doi.org/10.5014/ajot.61.2.216 [DOI] [PubMed] [Google Scholar]
- Parham L. D., Roley S. S., May-Benson T. A., Koomar J., Brett-Green B., Burke J. P., . . . Schaaf R. C. (2011). Development of a fidelity measure for research on the effectiveness of the Ayres Sensory Integration intervention. American Journal of Occupational Therapy, 65, 133–142. https://doi.org/10.5014/ajot.2011.000745 [DOI] [PubMed] [Google Scholar]
- Pfeiffer B., Henry A., Miller S., & Witherell S. (2008). Effectiveness of Disc ‘O’ Sit cushions on attention to task in second-grade students with attention difficulties. American Journal of Occupational Therapy, 62, 274–281. https://doi.org/10.5014/ajot.62.3.274 [DOI] [PubMed] [Google Scholar]
- Pfeiffer B. A., Koenig K., Kinnealey M., Sheppard M., & Henderson L. (2011). Effectiveness of sensory integration interventions in children with autism spectrum disorders: A pilot study. American Journal of Occupational Therapy, 65, 76–85. https://doi.org/10.5014/ajot.2011.09205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polatajko H. J., & Cantin N. (2010). Exploring the effectiveness of occupational therapy interventions, other than the sensory integration approach, with children and adolescents experiencing difficulty processing and integrating sensory information. American Journal of Occupational Therapy, 64, 415–429. https://doi.org/10.5014/ajot.2010.09072 [DOI] [PubMed] [Google Scholar]
- Polatajko H. J., & Mandich A. (2004). Enabling occupation in children: The Cognitive Orientation to daily Occupational Performance (CO–OP) approach. Ottawa, ON: CAOT Publications. [Google Scholar]
- Reynolds S., Bendixen R. M., Lawrence T., & Lane S. J. (2011). A pilot study examining activity participation, sensory responsiveness, and competence in children with high functioning autism spectrum disorder. Journal of Autism and Developmental Disorders, 41, 1496–1506. https://doi.org/10.1007/s10803-010-1173-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds S., Kuhaneck H. M., & Pfeiffer B. (2016). Systematic review of the effectiveness of frequency modulation devices in improving academic outcomes in children with auditory processing difficulties. American Journal of Occupational Therapy, 70, 7001220030 https://doi.org/10.5014/ajot.2016.016832 [DOI] [PubMed] [Google Scholar]
- Reynolds S., Lane S. J., & Richards L. (2010). Using animal models of enriched environments to inform research on sensory integration intervention for the rehabilitation of neurodevelopmental disorders. Journal of Neurodevelopmental Disorders, 2, 120–132. https://doi.org/10.1007/s11689-010-9053-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodger S., & Brandenburg J. (2009). Cognitive Orientation to (daily) Occupational Performance (CO–OP) with children with Asperger’s syndrome who have motor-based occupational performance goals. Australian Occupational Therapy Journal, 56, 41–50. https://doi.org/10.1111/j.1440-1630.2008.00739.x [DOI] [PubMed] [Google Scholar]
- Rodger S., Pham C., & Mitchell S. (2009). Cognitive strategy use by children with Asperger’s syndrome during intervention for motor-based goals. Australian Occupational Therapy Journal, 56, 103–111. https://doi.org/10.1111/j.1440-1630.2007.00719.x [DOI] [PubMed] [Google Scholar]
- Rroji O., van Kuyck K., Nuttin B., & Wenderoth N. (2015). Anodal tDCS over the primary motor cortex facilitates long-term memory formation reflecting use-dependent plasticity. PLoS One, 10, e0127270 https://doi.org/10.1371/journal.pone.0127270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaaf R. C., Benevides T. W., Kelly D., & Mailloux-Maggio Z. (2012). Occupational therapy and sensory integration for children with autism: A feasibility, safety, acceptability and fidelity study. Autism, 16, 321–327. https://doi.org/10.1177/1362361311435157 [DOI] [PubMed] [Google Scholar]
- Schaaf R. C., Benevides T., Mailloux Z., Faller P., Hunt J., van Hooydonk E., . . . Kelly D. (2014). An intervention for sensory difficulties in children with autism: A randomized trial. Journal of Autism and Developmental Disorders, 44, 1493–1506. https://doi.org/10.1007/s10803-014-2111-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaaf R. C., Toth-Cohen S., Johnson S. L., Outten G., & Benevides T. W. (2011). The everyday routines of families of children with autism: Examining the impact of sensory processing difficulties on the family. Autism, 15, 373–389. https://doi.org/10.1177/1362361310386505 [DOI] [PubMed] [Google Scholar]
- Schilling D. L., & Schwartz I. S. (2004). Alternative seating for young children with autism spectrum disorder: Effects on classroom behavior. Journal of Autism and Developmental Disorders, 34, 423–432. https://doi.org/10.1023/B:JADD.0000037418.48587.f4 [DOI] [PubMed] [Google Scholar]
- Schilling D. L., Washington K., Billingsley F. F., & Deitz J. (2003). Classroom seating for children with attention deficit hyperactivity disorder: Therapy balls versus chairs. American Journal of Occupational Therapy, 57, 534–541. https://doi.org/10.5014/ajot.57.5.534 [DOI] [PubMed] [Google Scholar]
- Schmidt R. A., & Lee T. D. (2005). Motor learning and control (4th ed.). Champaign, IL: Human Kinetics. [Google Scholar]
- Schoemaker M. M., & Smits-Engelsman B. C. M. (2005). Neuromotor task training: A new approach to treat children with DCD. In Sugden D. A. & Chambers M. (Eds.), Children with developmental coordination disorder (pp. 212–227). London: Whurr. [Google Scholar]
- Shield B., & Dockrell J. (2003). The effects of noise on children at school: A review. Journal of Building Acoustics, 10, 97–106. https://doi.org/10.1260/135101003768965960 [Google Scholar]
- Shochat T., Tzischinsky O., & Engel-Yeger B. (2009). Sensory hypersensitivity as a contributing factor in the relation between sleep and behavioral disorders in normal schoolchildren. Behavioral Sleep Medicine, 7, 53–62. https://doi.org/10.1080/15402000802577777 [DOI] [PubMed] [Google Scholar]
- Skinner B. F. (1938). The behavior of organisms: An experimental analysis. New York: Appleton-Century. [Google Scholar]
- Smith-Roley S., Mailloux Z., Kuhaneck H. M., & Glennon T. J. (2007). Understanding Ayres Sensory Integration. OT Practice, 12, CE1–CE8. [Google Scholar]
- Smits-Engelsman B. C. M., Blank R., van der Kaay A. C., Mosterd-van der Meijs R., Vlugt-van den Brand E., Polatajko H. J., & Wilson P. H. (2013). Efficacy of interventions to improve motor performance in children with developmental coordination disorder: A combined systematic review and meta-analysis. Developmental Medicine and Child Neurology, 55, 229–237. https://doi.org/10.1111/dmcn.12008 [DOI] [PubMed] [Google Scholar]
- Sullivan K. J., Kantak S. S., & Burtner P. A. (2008). Motor learning in children: Feedback effects on skill acquisition. Physical Therapy, 88, 720–732. https://doi.org/10.2522/ptj.20070196 [DOI] [PubMed] [Google Scholar]
- Umeda C., & Deitz J. (2011). Effects of therapy cushions on classroom behaviors of children with autism spectrum disorder. American Journal of Occupational Therapy, 65, 152–159. https://doi.org/10.5014/ajot.2011.000760 [DOI] [PubMed] [Google Scholar]
- Walton K. M., & Ingersoll B. R. (2013). Improving social skills in adolescents and adults with autism and severe to profound intellectual disability: A review of the literature. Journal of Autism and Developmental Disorders, 43, 594–615. https://doi.org/10.1007/s10803-012-1601-1 [DOI] [PubMed] [Google Scholar]
- Watling R. (2015). Interventions and strategies for challenging behaviors. In Case-Smith J. & O’Brien J. (Eds.), Occupational therapy for children and adolescents (7th ed., pp. 374–388). St. Louis: Mosby. [Google Scholar]
- Watling R., & Hauer S. (2015). Effectiveness of Ayres Sensory Integration® and sensory-based interventions for people with autism spectrum disorder: A systematic review. American Journal of Occupational Therapy, 69, 6905180030. [DOI] [PubMed] [Google Scholar]
- Watson J. B. (1913). Psychology as the behaviorist views it. Psychological Review, 20, 158–178. https://doi.org/10.1037/h0074428 [Google Scholar]
- Wilkes-Gillan S., Bundy A., Cordier R., & Lincoln M. (2016). Child outcomes of a pilot parent-delivered intervention for improving the social play skills of children with ADHD and their playmates. Developmental Neurorehabilitation, 119, 238–245. 10.3109/17518423.2014.948639 [DOI] [PubMed] [Google Scholar]
- Williams M. S., & Shellenberger S. (1996). How does your engine run? A leader’s guide to the Alert Program for self-regulation. Albuquerque, NM: Therapy Works. [Google Scholar]
- Willingham D. B. (1998). A neuropsychological theory of motor skill learning. Psychological Review, 105, 558–584. https://doi.org/10.1037/0033-295X.105.3.558 [DOI] [PubMed] [Google Scholar]
- Winstein C. J., & Schmidt R. A. (1990). Reduced frequency of knowledge of results enhances motor skill learning. Journal of Experimental Psychology: Learning, Memory, and Cognition, 16, 677–691. https://doi.org/10.1037/0278-7393.16.4.677 [Google Scholar]
- Zwicker J. G., & Harris S. R. (2009). A reflection on motor learning theory in pediatric occupational therapy practice. Canadian Journal of Occupational Therapy, 76, 29–37. https://doi.org/10.1177/000841740907600108 [DOI] [PubMed] [Google Scholar]