Summary
Bisphosphonates have been commonly used in the treatment of osteoporosis, demonstrating its efficacy in fracture risk reduction. However, even if are generally safe and well tolerated, concerns have emerged about atypical fractures related to its prolonged use. Although atypical femoral fracture are more common, case reports demonstrated that even other skeletal areas can be involved by unusual pattern of fracture.
We report a atypical acetabular periprosthetic fracture in a 83-year-old female patient after prolonged alendronate treatment for osteoporosis and isolated acetabular revision surgery. The patient underwent to clinical, bioumoral and radiological evaluation and all the history cases were fully reported.
We believe this periprosthetic fracture, according to the available data, may have similar underlying pathology to atypical femoral fractures. Awareness of symptoms, in addition to a regular radiographic survey may facilitate early diagnosis and possible prevention of spontaneous periprosthetic fractures, in patients receiving bisphosphonate therapy beyond 5 years. The treatment of this atypical periprosthetic fracture should include both surgical than pharmacological therapy to obtained bone healing.
Keywords: periprosthetic fracture, acetabular fracture, atypical fracture, bisphosphonates, alendronic acid, acetabular revision, total hip arthroplasty
Introduction
Bisphosphonates (BPs) are widely used anti-resorptive drugs, which have been proven to reduce the risk of osteoporotic fractures, and to better instead patients quality of life. Additionally alendronate and risendronate significantly inhibit the decrease of periprosthetic bone mineral density (BMD) and bone resorption in the proximal femur after cementless total hip arthroplasty (THA) and enhance the long-term stability of the prosthesis.
Even though bisphosphonates prolonged therapy is generally safe and effective, it carries the potential risk of oversuppressing bone turnover that can potentially compromise some of the biomechanical properties of bone and has been reported to relate with so-called “atypical fractures” (AFs), which typically involve the femur. First, in 2005 Odvina et al. (1) demonstrated unusual nonspinal fractures as a result of minor or none trauma that commonly involved alendronate treated patients.
In particular they described femoral, ischiatic, pubic and sacral fractures and presented iliac bone histomorphometric findings in all cases. Cells were barely observed in the bone surface, and osteoid volume and bone formation rate were severely suppressed. In addition, the resorbing surface of the bone was also intensively inhibited in most cases. As noted above, they defined the condition in which both bone formation and resorption are extremely hampered as severely suppressed bone turnover (SSBT). In clinical settings, this condition indicates that atypical and non-traumatic fracture has occurred in cortical bone-rich areas, such as the pubis, ischium, or femoral diaphysis.
Lenart et al. (2) described as “atypical” fractures that involved the strongest part of the femur, the subtrochanteric and diaphyseal region, and then the American Society for Bone and Mineral Research Task force (3) identified major and minor features that define distinctly “typical” osteoporotic femoral fractures from “atypical” fractures.
A recent review demonstrated that the incidence of atypical femoral fractures (AFFs) is 0.6%, according to data from the most recent literature, referred to all femoral fractures, including both medial fractures, lateral and diaphyseal fractures (4).
Moreover, in the literature are reported atypical fractures that occur to other skeletal districts in addition to femur (1) and several case reports in the literature related periprosthetic femoral fractures to the same or similar pathology as that of an atypical femoral fracture (5, 6).
In this report, the Authors describe an atypical acetabular periprosthetic fracture in a female patient after prolonged alendronate and isolated acetabular revision surgery, that to our knowledge is the first case in the literature.
Case report
A 83-year-old woman presented to our Department in December 2013, with a sudden right groin pain and a limp.
She had the history of right hip fracture treated with cementless THA in 1999. After surgery the patient received vitamin D orally, 10,000 IU, and 70 mg alendronate orally every week since 2002, when she was 71 years old, for secondary prevention of fragility fractures.
In 2010, the patient showed limitations in gait and daily living activities without trauma. Routine blood investigations showed normal ESV and PCR serum levels. Vitamin D levels were found to be <24 ng/dl (range 30 – 74 ng/dl), alkaline phosphatase 74 U/L, serum calcium 8.9 mg/dl (8,5 – 10 mg/dl), and serum levels of parathormone being 47,40 pg/ml (15 – 68 pg/ml). Lumbar BMD measured by DEXA scan was found to be − 2,9 SD T-Score. Radiographs showed images suggestive for polyethylene wear and mild acetabular osteolysis (Figure 1a).
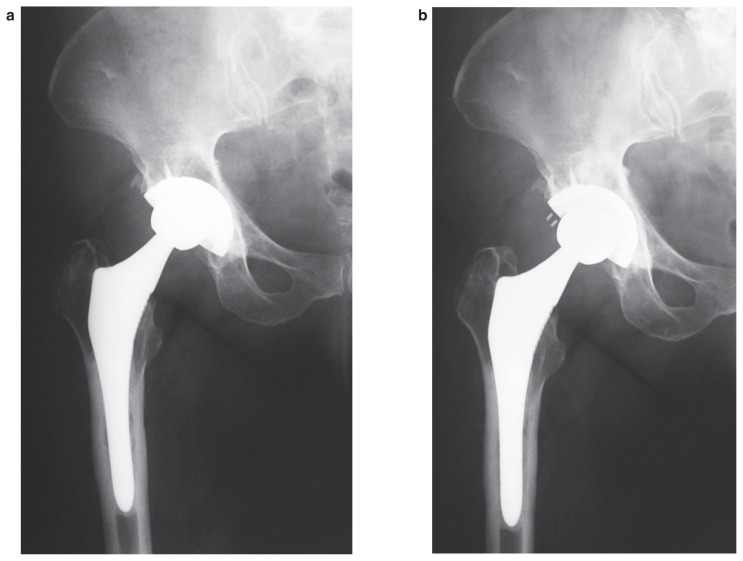
Figure 1 a, b.
a) AP view X-ray demonstrate polyethylene wear and mild acetabular osteolysis; b) Post op AP view after polyethylene exchange and Mg-hydroxyapatite filling of osteolysis area.
Therefore, since there were not any sign of acetabular cup loosening, she underwent isolated acetabular revision surgery with polyethylene exchange alone and hydroxyapatite grafting of the bony defect (Figure 1b). The patient received postoperative oral calcium (600 mg/day), vitamin D (400 IU/day) and alendronate (70 mg/week) therapy.
Then, in May 2013, following a long day of walking the patient referred spontaneous right groin pain and limp. Radiographs and pelvic computerized tomography demonstrated an incomplete transverse acetabular fracture and superomedial ilium osteolysis without migration of the acetabular component (Figure 2a).
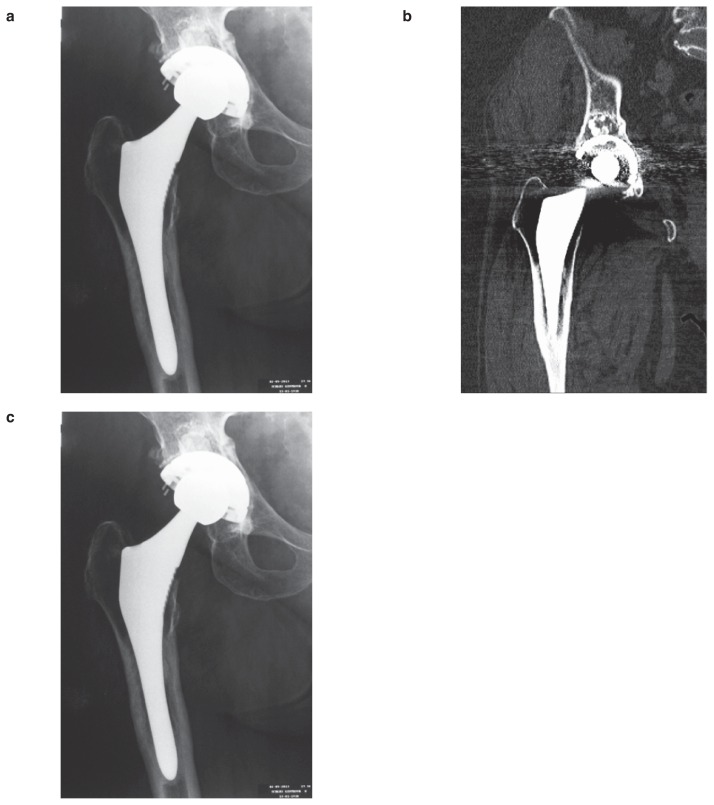
Figure 2 a–c.
a) May 2013, AP view X-ray showed an incomplete periprostethic acetabular fracture with no migration of the acetabular cup; b) December 2013, AP view X-ray revealed complete fracture periprostethic acetabular and medial migration of the acetabular cup; c) Pelvic CT scan confirmed medial migration of the cup with lamina quadrilateral fracture.
Initially the patient underwent conservative treatment with rest and partial weight-bearing. Vitamin D levels were found to be lower <15 ng/dl, serum calcium 6.9 mg/dl and PTH levels increased to 72 pg/dl. Thus, alendronate treatment have been ceased, and she received oral calcium (600 mg/day), vitamin D (1000 IU/day) and strontium ranelate (2 g/day). After two weeks she dropped strontium ranelate, due to side effects to the drug, such as rash and itch.
In December 2013 lumbar BMD measured by DEXA dropped to a − 3.5 SD T-Score and the patient still complained pain and severe limp. Even more radiograph and pelvic computerized tomography demonstrated a complete transverse acetabular fracture with medial migration of acetabular cup (Figure 2 b, c). This required acetabular revision surgery with a reconstruction cage and cemented polyethilene socket, while femoral stem appeared well-fixed (Figure 3a). Bone defect was filled with RegenOss® grafting (FinCeramica Faenza S.p.A., Faenza, Italy), a collagen-hydroxyapatite composite patch. The patient received oral calcium (600 mg/day) and vitamin D (1000 IU/day) and she achieved the normalization of vitamin D (26 ng/dl) and PTH (54,40 pg/ml) serum levels.
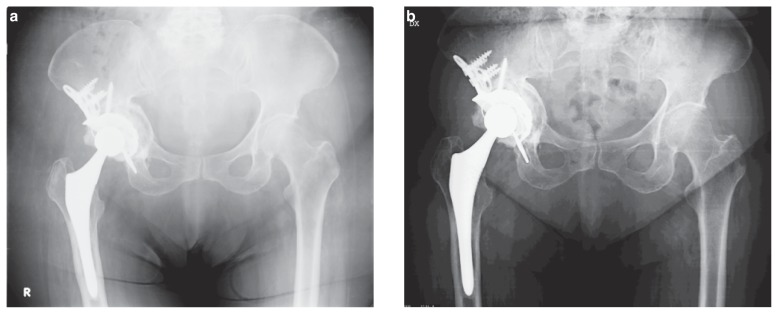
Figure 3 a, b.
a) January 2014, post-operative AP pelvis X-ray showed acetabular revision with reconstruction cage and RegenOss? grafting of medial wall; b) 12 months follow up X-ray showed the cage well fixed and the healing of acetabular fracture with bone stock restoration.
Two years after surgery, Harris Hip Score was 78 points and the patient was ambulating with limp but without pain. Radiographs showed acetabular bone reconstruction with valid fixation of the cage (Figure 3b).
Discussion
Periprosthetic acetabular fractures are rare complications of total hip arthroplasty and according to recent reviews, except for iatrogenic intraoperative fractures that represent 0.4%, the most common causes are trauma, aseptic loosening and periprosthetic osteolysis (7).
However, we speculated that the periprosthetic acetabular fracture reported in this paper was due to long-term alendronate therapy for the reasons explained below.
Clinical case presentation was comparable to AFFs features described by ASBMR Task Force. In fact the patient first showed to our attention with prodromal symptoms such as dull pain in the groin followed by severe groin pain and limp without history of recent trauma or minor trauma.
These symptoms can be related to acetabulum osteolysis due to polywear as primary cause of fracture and pain, although the isolated polyethylene exchange seemed to stop the extension of osteolysis, as confirmed by computerized tomography imaging. Thus, we performed hydroxyapatite (HA) grafting through the retroacetabular defect in order to increase the overall quality of the bone with infilling and remodeling, and halt the progression of osteolysis.
According to the literature isolated polyethylene exchange is considered appropriate especially in well-fixed acetabular cups. Restrepo et al. (8) found a similar acetabular failure rate after revision THA for isolated polyethylene exchange compared to complete acetabular revision for polyethylene wear in cementless cups and they advocated revision of malpositioned cups and in case of mechanical failure only.
Long-term alendronate therapy is strongly associated with atypical fracture, both in femur and other skeletal areas, and the current consensus is that AFs are stress or insufficiency fractures that develop over time. Although periprosthetic fractures are excluded by the traditional definition of AFFs, there may be a periprosthetic fracture that has the same or similar pathology as an AFF. In 2012, Cross et al. (5) reported a periprosthetic femoral fracture around a cemented THA stem in an 81-year-old woman who had a more than 12-year history of alendronate use, and recently Niikura et al. (6) a periprosthetic femoral fracture a little below the tip of a cementless stem in a 69-year-old Japanese woman who received alendronate for more than 7-years.
Tantavisut et al. (9) recently reported an acetabular periprosthetic fracture as consequence from prolonged usage of zoledronic acid in bone metastasis prevention. Authors believed that the acetabulum failed due to the chronic stress from repetitive workload in daily activities and atypical fracture in subtrochanteric area did not occur in this case, because the application of femoral stem bypassed the subtrochanteric area. We strongly agree with their speculation.
Even the discontinuation of the treatment did not result in an immediate reduction of atypical fracture risk, because bisphosphonates are incorporated into the bone and continue to exert an anti-resorptive effect for a variable period of time. As regards alendronate the average terminal half-life of is 10.5 years. It stands to reason that if rare undesirable medical occurrences are related to bisphosphonate use, then the risk should diminish over time as the bisphosphonate is eliminated from the bone. Studies suggest that for many women, discontinuation of alendronate for up to 5 years does not appear to significantly increase osteoporotic fracture risk (10), so, the concept of a drug holiday (11) has emerged, whereby the risk of adverse effects might be decreased while the patient still benefits from anti-fracture efficacy. However, apart from the Swedish study suggesting that the risk of atypical femoral fractures decreases following discontinuation of oral bisphosphonate (12) there are no data to answer this question.
Moreover, prolonged treatment is associated with higher risk of delay in fracture healing or nonunion (1, 13), and this would explain why even if bisphosphonate therapy have been ceased immediately after incomplete fracture detection, conservative treatment has been ineffective.
The final bone healing of the periprosthetic acetabular fracture reported, in our opinion, was achieved through stability of the reconstruction cage after revision surgery and the discontinuation of anti-resorptive treatment, even though the “therapeutical tail”, in association with calcium and vitamin D supplements. Studies demonstrated that increasing 25-hydroxyvitamin D levels to optimal (>30 ng/dL) and calcium levels to normal with normalization of parathyroid hormone levels enhances AFs healing (14).
In order to promoting AFs healing, case reports and case series showed beneficial effects of anabolic drugs alone (13, 15) (teriparatide and strontium ranelate) or in association with bisphosphonates used in early postoperative period (16–18). In contrast, variable response to teriparatide was reflected in reports of medical treatment of AFFs presented at the ASBMR Annual Meeting in 2012 (19).
In the absence of a randomized, placebo-controlled trial, no definite conclusion can be reached regarding the efficacy of TPTD treatment of patients with AFs. From the low-quality evidence available, the last recommendations of ASBMR task force for medical management remain reasonable: discontinuation of BPs, adequate calcium and vitamin D, and consideration of TPTD for those who appear not to heal on conservative therapy (3).
Even though periprosthetic fractures are not included in the current definition of AFs, available data indicate that there may be similar underlying pathology. Therefore, treatment includes both surgical than pharmacological therapy (20). In unstable acetabular components, with uncontained cavitary defect and severe bone loss revision surgery is mandatory, but there might be likely an important role of anabolic drugs in promoting fracture healing.
References
- 1.Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90(3):1294–1301. doi: 10.1210/jc.2004-0952. [DOI] [PubMed] [Google Scholar]
- 2.Lenart BA, Lorich DG, Lane JM. Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med. 2008;358(12):1304–1306. 20. doi: 10.1056/NEJMc0707493. [DOI] [PubMed] [Google Scholar]
- 3.Shane E, et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014 Jan;29(1):1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 4.Bottai V, Giannotti S, Dell’osso G, De Paola G, Menconi A, Falossi F, Raffaetà G, Guido G. Atypical femoral fractures: retrospective radiological study of 319 femoral fractures and presentation of clinical cases. Osteoporos Int. 2013;25:993–997. doi: 10.1007/s00198-013-2546-8. [DOI] [PubMed] [Google Scholar]
- 5.Cross MB, Nam D, van der Meulen MC, Bostrom MP. A rare case of a bisphosphonate-induced peri-prosthetic femoral fracture. J Bone Joint Surg Br. 2012;94:994–7. doi: 10.1302/0301-620X.94B7.28778. [DOI] [PubMed] [Google Scholar]
- 6.Niikura, et al. Rare non-traumatic periprosthetic femoral fracture with features of an atypical femoral fracture: a case report. Journal of Medical Case Reports. 2015;9:103. doi: 10.1186/s13256-015-0590-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benazzo F, Formagnana M, Bargagliotti M, Perticarini L. Periprosthetic acetabular fractures. International Orthopaedics (SICOT) 2015;39:1959–1963. doi: 10.1007/s00264-015-2971-8. [DOI] [PubMed] [Google Scholar]
- 8.Restrepo C, Ghanem E, Houssock C, Austin M, Parvizi J, Hozack WJ. Isolated Polyethylene Exchange versus Acetabular Revision for Polyethylene Wear. Clin Orthop Relat Res. 2009;467:194–198. doi: 10.1007/s11999-008-0533-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tantavisut S, Tanavalee A, Thanakit V, Ngarmukos S, Wilairatana V, Wangroongsub Y. Spontaneous Acetabular Periprosthetic Fracture in a Patient Continuously Having Zoledronic. Acid Clinics in Orthopedic Surgery. 2014;6:358–360. doi: 10.4055/cios.2014.6.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Black DM, et al. Effects of continuing or stopping alendronate after 5 years of treatment: the fracture intervention trial long-term extension (FLEX): a randomized trial. Jama. 2006;296(24):2927–2938. doi: 10.1001/jama.296.24.2927. [DOI] [PubMed] [Google Scholar]
- 11.Bonnick SL. Going on a drug holiday? J Clin Densitom. 2011;14:377–383. doi: 10.1016/j.jocd.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Schilcher J, Koeppen V, Aspenberg P. Risk of Atypical Femoral Fracture during and after Bisphosphonate Use. N Engl J Med. 2014;371:974–976. doi: 10.1056/NEJMc1403799. [DOI] [PubMed] [Google Scholar]
- 13.Carvalho NNC, Voss LA, et al. Atypical femoral fractures during prolongued use of bisphosphonates: short-term responses to strontium ranelate and teriparatide. J Clin Metab. 2011 Sep;96(9):2675–80. doi: 10.1210/jc.2011-0593. [DOI] [PubMed] [Google Scholar]
- 14.Eschle D, Aeschlimann AG. Is supplementation of vitamin d beneficial for fracture healing? A short review of the literature. Geriatr Orthop Surg Rehabil. 2011 May;2(3):90–3. doi: 10.1177/2151458511408568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Im G, Lee S. Effect of Teriparatide on Healing of Atypical Femoral Fractures: A Systemic Review. J Bone Metab. 2015 Nov;22(4):183–9. doi: 10.11005/jbm.2015.22.4.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Capone A, Orgiano F, Pianu F, Planta M. Orthopaedic surgeons’ strategies in pharmacological treatment of fragility fractures. Clin Cases Miner Bone Metab. 2014 May;11(2):105–9. [PMC free article] [PubMed] [Google Scholar]
- 17.Brandi ML. Healing of the bone with anti-fracture drugs. Expert Opin Pharmacother. 2013 Aug;14(11):1441–7. doi: 10.1517/14656566.2013.801959. [DOI] [PubMed] [Google Scholar]
- 18.Hegde V, Jo JE, Andreopoulou P, Lane JM. Effect of osteoporosis medications on fracture healing. Osteoporos Int. 2015 Sep 29; doi: 10.1007/s00198-015-3331-7. [DOI] [PubMed] [Google Scholar]
- 19.Cheung AM, Bleakney R, Kahn A, et al. Effect of teriparatide on fracture healing in patients with non-displaced incomplete atypical femur fractures. J Bone Miner Res. 2012;27(Suppl 1) [Google Scholar]
- 20.Marongiu G, Mastio M, Capone A. Current options to surgical treatment in osteoporotic fractures. Aging Clin Exp Res. 2013 Oct;25(Suppl 1):S15–7. doi: 10.1007/s40520-013-0081-2. [DOI] [PubMed] [Google Scholar]