Summary
Although technically challenging even for the experienced surgeon, simultaneous open reduction and internal fixation (ORIF) of acetabular fracture and total hip replacement (THR) have some potential advantages over the more traditional treatment options in specific patient subgroups; theoretically allowing immediate weight bearing and faster rehabilitation, reducing the cost of inpatient stay, and reducing the risks of early and late local complications associated with standard treatment for this type of injury. We review the evolution of the indications and techniques, outline the surgical challenges, and discuss implant options and outcomes for this treatment paradigm.
Keywords: acetabular fractures, hip arthroplasty, fragility fracture, osteoporosis, trauma
Introduction
The treatment of choice for displaced acetabular fractures in younger patients involves open reduction and internal fixation, as joint restoration helps to reduce the risk of post-traumatic arthritis. Despite the complications involved [degenerative changes, avascular necrosis (AVN), heterotopic ossification (HO), failure of fixation necessitating THR)] (1–4), anatomical restoration offers the optimal choice for most displaced fractures.
The incidence of acetabular fractures in patients over the age of 60 has increased markedly in the last quarter of a century (5), and the rate of increase is rising faster than for any other subgroup of acetabular fractures (6). In the elderly low energy injuries predominate, making injury profiles different from younger patients with acetabular fractures, both for the mechanism of injury and other associated injuries. Falls from standing height accounted for 50% of acetabular fractures in patients over 60 years old, while 82% of fractures in younger patients was as a result of high energy mechanisms of injury (5). The rate of other associated injury is much less for the elderly group (less than 30%) than for younger patients due to the decreased rate of RTAs (7). Although these elderly patients frequently have poor bone quality, multiple medical co-morbidities and an increased peri-operative risk profile- all of which may reduce the expectation of a favourable outcome- with prompt diagnosis, careful monitoring of the physiological parameters of injury, optimisation of pre-operative status, involvement of experienced teams, and a highly specific patient-tailored management programme (8–11), successful outcomes can be achieved. Associated injuries, previous medical history of cardio-respiratory, neurological or cognitive issues, ambulatory status, functional demands, and a previous history of arthritic hip pain must be elicited and documented. Osteoporosis and fragility fracture treatment should be undertaken as for any fragility fracture of the elderly.
Simultaneous acetabular fixation and total hip arthroplasty - evolution of the concept
Non-operative treatment of acetabular fractures is really only a treatment option for minimally displaced fractures, or for those unable to successfully tolerate the surgical intervention (12). These are the very patients who are most likely to benefit from early mobilisation and weight-bearing (13). ORIF remains the treatment of choice for displaced acetabular fractures (13), however failure rates for acetabular fracture ORIF are high; in the general population a 10% failure rate has been reported (14). In a more elderly cohort, a failure rate – requiring re-intervention with a THR – has been reported in over 30% of patients (15).
Indications, limitations, technical challenges
First advanced by Westerborn in 1954 as a treatment modality for central dislocations (16), both the nomenclature and indications have evolved with time. The procedure has been known as, among other names, simultaneous ORIF and THR, combined internal fixation with acute THR, the combined hip procedure, and acute THR for acetabular fractures. The Authors have, for brevity, coined the term ‘Fix and Replace’. Indications for this treatment option are based around a number of factors, including:
Patient factors: age, osteoporosis, obesity, low functional demand, pre-existing ipsilateral osteoarthritis of the affected hip, or previous arthroplasty to the contralateral hip
Fracture pattern factors: severe posterior wall comminution, articular cartilage damage to femoral head, marginal impaction of the acetabulum, ipsilateral displaced femoral head or neck fractures, anterior head dislocation
External factors: prolonged hip dislocation (which has a high association with AVN, and sciatic nerve palsy), and delay to reconstruction (which is associated with higher rates of AVN, HO, infection) (15, 17–22).
Sierra et al. describe their indications for THR with these factors in mind, and include physiologically older patients with significant posterior wall involvement, and or significant impaction of the femoral head articular surface (23). Chana-Rodriguez et al. also add these factors into their indications, using the description of patients who fall into the ‘recognised subset’ of patients for whom ‘combined internal fixation with THA may be a more appropriate treatment option’ (22). In the review article by Herscovici et al., inclusion criteria for the ‘Combined Hip Procedure’ (defined as ORIF and THR performed during the same anaesthetic) includes elderly patients with significant ipsilateral OA of the hip, osteoporosis producing poor stock, or those presenting with associated femoral head fractures (24). Guerado et al. elegantly describe their treatment algorithm for acetabular fractures in the elderly (8), dividing patients into three groups – those with good general health, those who are senile, and those with poor general health. Those considered suitable for acute THR include patients with non-easily reducible fracture within the good general health group, and those suitable for ORIF & acute THR include all patients in the senile group, and some of those in the poor general health group. De Bellis et al. conclude that ‘physicians’ practice and expertise are the most useful tools in clinical practice’ (25).
Surgical options: approaches, techniques
Careful planning of surgical approach is essential. Fractures of the anterior wall may require ORIF through an anterior approach, either using the ilioinguinal (II) approach or through the modified Stoppa approach. Herscovici et al. describe their operative management as stabilization of the fracture using standard ORIF techniques, approached via either the KL (n=19) or II (n=3) approach, with patients having II approach being repositioned and re-draped to allow placement of a THA through a posterior or posterolateral approach. The II approach was selected when posterior approach alone was deemed pre-operatively insufficient to provide stability of the columns or of the acetabular component (24). Recently the modified Stoppa approach has become popular, with a traditional Pfannensteil incision coupled with the lateral window of the ilioinguinal approach. This approach, described by Hirvensalo (26) and later Cole (27), is a modification of the intrapelvic approach described by Stoppa et al. (28), and avoids the dissection of the middle window of the ilioinguinal approach, sparing dissection of the femoral neurovascular bundle. Visualization through this approach is adequate for access for most of the inner true bony pelvis (29–31). The lateral window – common to both approaches –is relatively uncomplicated and gives excellent access across the pelvic brim and SI joint. Plating is often required for infrapectineal buttressing of the quadrilateral plate, though loss of reduction over time is common. Where the anterior approach can be avoided, good results can be achieved through the KL approach combining use of morcellised graft impacted onto the denuded face of the anterior wall – using the technique common in revision hip arthroplasty –followed by either a cemented or uncemented cup.
Osteosynthesis for fractures involving the posterior column is crucial to achieve a degree of joint stability. The KL approach is suitable for managing access to isolated fractures of the posterior column, and the associated type transverse with posterior wall components. Osteosynthesis with neutralisation and buttressing plates is essential before proceeding to the arthroplasty section of the case. Regardless of approach, as has been demonstrated in multiple series, instability of the bone fragments/columns integrity can threaten implant fixation, hence primary stability of fixation is of paramount importance (8, 32).
Treatment options for Fix and Replace
Implant choices and combinations must be planned carefully, tailored to the specific patient and their respective fracture pattern, be ordered in when necessary, and be compatible where modularity is available. Reconstructive options have been described from simple to highly complex, using the full panoply of implants (and adjuncts such as graft) for both the acetabular and proximal femoral components respectively. Prosthesis alone were used in one study (33), prostheses with anti-protrusio cages and bone grafting for others (22, 34), some studies report on cable fixation for fracture fixation (35–37), another describes standard ORIF without cable fixation (24), while a variety of options were described over a twenty year period by Sarker et al. (38) ranging from standard plate fixation to reinforcement with anti-prostrusio cage devices.
Treatment of these fractures with THR is challenging due to the need to ensure primary stability of the acetabular component, which is threatened by unstable bony fragments/columns. Strong osteosynthesis is vital, and even if initial fixation is obtained, hip arthroplasty components may subside as a result of subsequent instability at the fracture site (24, 35, 39). Percutaneous reduction and fixation has been advocated using large cannulated 6.5 mm or 7.3 mm screws (40, 41). This technique requires considerable expertise, but in the elderly may have a role to allow sufficient stability to allow early mobilisation (7).
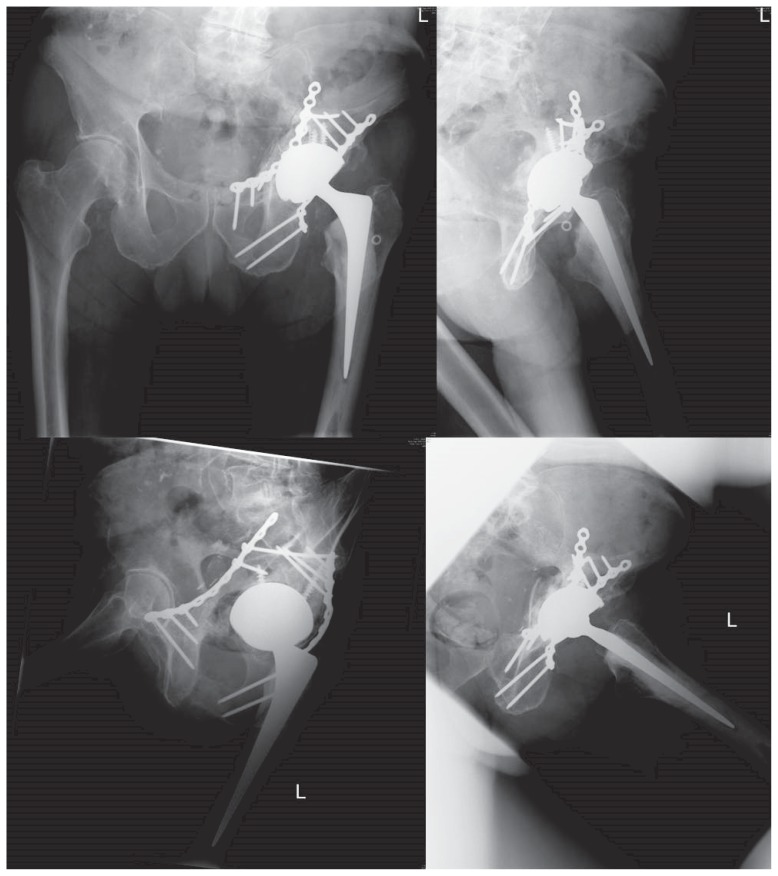
The Authors’ preference is, where possible, for stable osteosynthesis using a single KL approach. If the anterior column is unstable, the anterior column is plated using a modified Stoppa approach. For the posterior elements, a standard KL approach is used, with a trochanteric osteotomy used only when necessary for proximal access. Once a stable construct has been achieved with standard plate fixation, the acetabular defect is addressed. If graft is required, the patients’ femoral head, supplemented with allograft femoral head, is then bone mill morcellised and impacted. A revision-type cup can then be implanted. A highly porous metal cup with multiple screw options is preferred. These screws are placed in both columns and the use of a cemented polyethylene liner, to accommodate a 28 mm or ideally a 32 mm metal head, effectively creates an intra-acetabular locking plate (Figures 1 and 2). A dual mobility metal-backed shell can also be cemented into this porous cup, depending on clinical need. For the stem, a cemented highly polished double-tapered primary hip prosthesis is favoured. Routine cell salvage, use of tranexamic acid and consideration of an IVC filter preoperatively is employed. Full weight bearing with crutches is commenced the day following surgery unless otherwise contraindicated.
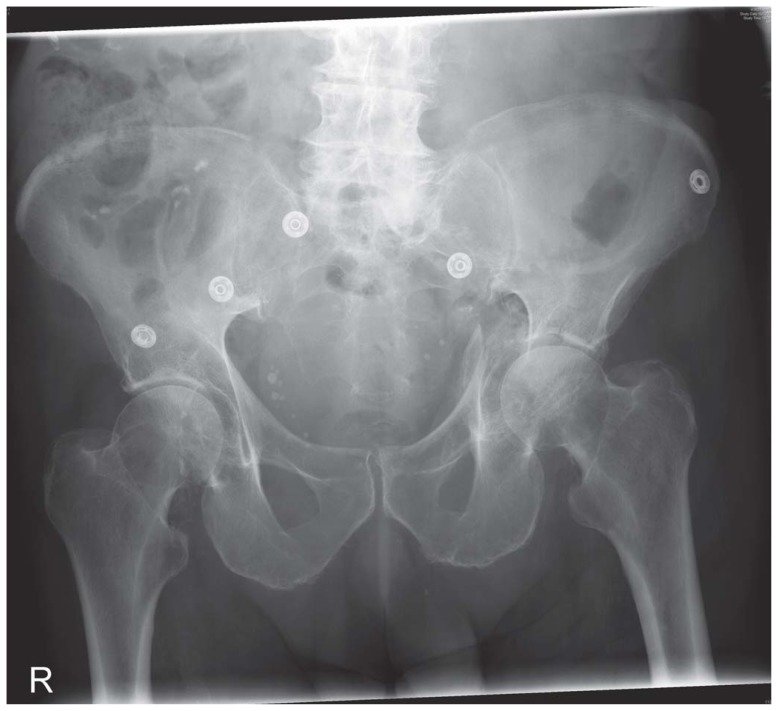
Figure 1.
AP pelvis of a 73-year-old man (fall from standing height, symptomatic left osteoarthritis before fall), presenting with a left acetabular fracture. He had plating of his anterior column via a modified Stoppa, then posterior plating, before acute THR using a highly porous metal cup with screws through both columns, into which a cemented DM cup was inserted, and a cemented femoral stem with a 32 mm head. The patient mobilised fully weight bearing the following day, and was discharged on post op Day 7.
Figure 2.
Interval radiographic views at 6 months post surgery.
Outcomes
In a systematic review comparing studies on the outcome of patients (mean age of 71.8 years, range 55 to 96 years) managed with simultaneus ORIF and THR and studies with patients undergoing ORIF, alone operative times were longer, and blood loss was greater for the former group, but no difference was noted in mortality between the groups (42). In De Bellis et al. systematic review (25), outcomes, complications and failure rates for acute THR were analysed in studies meeting their pre-defined criteria, noting that in studies looking at Harris Hip Scores (HHS) outcomes were good (Mears, Tidemark, Herscovici reporting HHS of 89, 85 and 74 respectively) (24, 34, 35). Heterotopic ossification (HO) was a problem in 6 studies, with a range of HO between 10–40%. Dislocation, a significant problem for THR surgery, is particularly relevant for the patients with cognitive impairment or neurological impairment. Sarkar et al. recommend THR for patients suffering neurological impairment or psychiatric conditions due to poor compliance with postoperative instructions (38). Although the highest dislocation rate was reported by Herscovici et al. at 14% (24), Sarkar et al. report the highest rate of radiographic loosening (21%) (38). A growing body of evidence indicates that Dual Mobility cups reduce dislocation rates in primary and revision total hip arthroplasty and, when used with prudence, in selected tumour cases (43). Sierra et al. note that these components are gaining popularity in Europe and consider them an option in high risk cases (23). In a study comparing the results of primary THR (mean age 78 years) to delayed THR (average age 53 years) for ace-tabular fracture, Sermon et al. noted – although not statistically significant – a reduced revision rate (8% compared to 22%) and reduced HO (28% compared to 41%) for those treated with acute THR, but noted better HHS scores for the delayed THR group (33).
Late complications are frequent in this patient cohort. Younger patients experience reduced levels of activity and a reduced quality of life following acetabular fractures (14), while the elderly experience more significant morbidity from both fracture and treatment (44, 45). For patients treated non-operatively, post-traumatic arthritis, non-union, protrusio and HO formation are common. For those treated with ORIF, the standard post operative complications in elderly patients are de rigueur, in addition to the late local complications, including HO, sciatic nerve palsy, prominence of metalwork or failure of fixation and infection. Risk factors for surgical site infection include high BMI, presence of Morel-Lavallée lesions and stay in the intensive care (46). Given the paucity of studies comparing directly the outcomes between acute THR for acetabular fractures and those treated with ORIF in the elderly cohort, further randomised control trials are needed to determine optimal therapy in this extremely challenging cohort of patients, in addition to delineating the effects of comorbidities, associated injuries and the timing of surgery in specific patient groups (8).
Conclusion
Although ORIF is widely considered to be the standard of care for younger and middle aged patients with acetabular fractures, in elderly patients with concomitant chronic disease acute THR may be a more suitable option. Specific factors relating to the patient (osteoporosis, obesity, low functional demand, pre-existing ipsilateral OA of the affected hip), the fracture pattern (posterior wall comminution, articular cartilage damage to the femoral head, marginal impaction of the acetabulum, ipsilateral displaced femoral head or neck fractures, anterior head dislocation) or external factors (prolonged dislocation, delay to fixation) are all relative indications.
Acute THR is a technically demanding intervention, not without significant risks to the patient. Challenges include longer anaesthetic times, higher blood transfusion rates, and technical difficulties (24). The risks of surgery of this magnitude are certainly front-loaded to the patient, but must be seen in the context of the risks to the patient from other forms of treatment – for ORIF the risk of failure is relatively high, frequently necessitating further surgery at a future date. For non-operative treatment, historically the more likely option, the inevitable decubitus-related risks for this patient cohort are well documented. Acute simultaneous ORIF and THR theoretically allows immediate weight bearing and faster rehabilitation, reduces the cost of inpatient stay, and reduces the risks of early and late local complications associated with standard treatment for this type of injury. Although the evidence base is to date limited, ‘fix and replace’ is emerging as a treatment paradigm in specific patient groups.
References
- 1.Routt ML, Jr, Swiontkowski MF. Operative treatment of complex ace-tabular fractures. Combined anterior and posterior exposures during the same procedure. J Bone Joint Surg Am. 1990 Jul;72(6):897–904. [PubMed] [Google Scholar]
- 2.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996 Nov;78(11):1632–45. [PubMed] [Google Scholar]
- 3.Wright R, Barrett K, Christie MJ, Johnson KD. Acetabular fractures: long-term follow-up of open reduction and internal fixation. J Orthop Trauma. 1994 Oct;8(5):397–403. doi: 10.1097/00005131-199410000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Kreder HJ, Rozen N, Borkhoff CM, Laflamme YG, McKee MD, Schemitsch EH, Stephen DJ. Determinants of functional outcome after simple and complex acetabular fractures involving the posterior wall. J Bone Joint Surg Br. 2006 Jun;88(6):776–82. doi: 10.1302/0301-620X.88B6.17342. [DOI] [PubMed] [Google Scholar]
- 5.Ferguson TA, Patel R, Bhandari M, Matta JM. Fractures of the acetabulum in patients aged 60 years and older: an epidemiological and radiological study. J Bone Joint Surg Br. 2010 Feb;92(2):250–7. doi: 10.1302/0301-620X.92B2.22488. [DOI] [PubMed] [Google Scholar]
- 6.Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999 Mar-Apr;7(2):128–41. doi: 10.5435/00124635-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Butterwick D, Papp S, Gofton W, Liew A, Beaulé PE. Acetabular Fractures in the Elderly: Evaluation and Management. J Bone Joint Surg Am. 2015 May 6;97(9):758–768. doi: 10.2106/JBJS.N.01037. [DOI] [PubMed] [Google Scholar]
- 8.Guerado E, Cano JR, Cruz E. Fractures of the acetabulum in elderly patients: an update. Injury. 2012 Dec;43(Suppl 2):S33–41. doi: 10.1016/S0020-1383(13)70177-3. [DOI] [PubMed] [Google Scholar]
- 9.Guerado E, Cano JR, Cruz E. Surgical technique: Intraacetabular osteosynthesis with arthroplasty for acetabular fracture in the octogenarian. Injury. 2012;43:509–12. doi: 10.1016/j.injury.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 10.Pagenkopf E, Grose A, Partal G, Helfet DL. Acetabular fractures in the elderly: treatment recommendations. HSS J. 2006;2:161–71. doi: 10.1007/s11420-006-9010-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vallier HA, Cureton BA, Ekstein C, Oldenburg FP, Wilber JH. Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. J Trauma. 2010;69:677–84. doi: 10.1097/TA.0b013e3181e50914. [DOI] [PubMed] [Google Scholar]
- 12.Tornetta P., 3rd Displaced acetabular fractures: indications for operative and nonoperative management. J Am Acad Orthop Surg. 2001 Jan-Feb;9(1):18–28. doi: 10.5435/00124635-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Kumar A, Shah NA, Kershaw SA, Clayson AD. Operative management of acetabular fractures. A review of 73 fractures. Injury. 2005 May;36(5):605–12. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 14.Giannoudis PV, Nikolaou VS, Kheir E, Mehta S, Stengel D, Roberts CS. Factors determining quality of life and level of sporting activity after internal fixation of an isolated acetabular fracture. J Bone Joint Surg Br. 2009 Oct;91(10):1354–9. doi: 10.1302/0301-620X.91B10.22572. [DOI] [PubMed] [Google Scholar]
- 15.Carroll EA, Huber FG, Goldman AT, Virkus WW, Pagenkopf E, Lorich DG, Helfet DL. Treatment of acetabular fractures in an older population. J Orthop Trauma. 2010 Oct;24(10):637–44. doi: 10.1097/BOT.0b013e3181ceb685. [DOI] [PubMed] [Google Scholar]
- 16.Westerborn A. Central dislocation of the femoral head treated with mold arthroplasty. J Bone Joint Surg Am. 1954 Apr;36(A:2):307–14. [PubMed] [Google Scholar]
- 17.Matta JM, Anderson LM, Epstein HC, Hendricks P. Fractures of the acetabulum. A retrospective analysis. Clin Orthop Relat Res. 1986 Apr;(205):230–40. [PubMed] [Google Scholar]
- 18.Rommens PM, Giménez MV, Hessmann M. Posterior wall fractures of the acetabulum: characteristics, management, prognosis. Acta Chir Belg. 2001 Nov-Dec;101(6):287–93. [PubMed] [Google Scholar]
- 19.Moed BR, WillsonCarr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002 May;84-A(5):752–8. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Mears DC, Velyvis JH, Chang CP. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003 Feb;(407):173–86. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]
- 21.Tannast M, Najibi S, Matta JM. Two to twenty-year survivorship of the hip in 810 patients with operatively treated acetabular fractures. J Bone Joint Surg Am. 2012 Sep 5;94(17):1559–67. doi: 10.2106/JBJS.K.00444. [DOI] [PubMed] [Google Scholar]
- 22.Chana-Rodríguez F, Villanueva-Martínez M, Rojo-Manaute J, Sanz-Ruíz P, Vaquero-Martín J. Cup-cage construct for acute fractures of the acetabulum, re-defining indications. Injury. 2012 Dec;43(Suppl 2):S28–32. doi: 10.1016/S0020-1383(13)70176-1. [DOI] [PubMed] [Google Scholar]
- 23.Sierra RJ, Mabry TM, Sems SA, Berry DJ. Acetabular fractures: the role of total hip replacement. Bone Joint J. 2013 Nov;95-B(11 Suppl A):11–6. doi: 10.1302/0301-620X.95B11.32897. [DOI] [PubMed] [Google Scholar]
- 24.Herscovici D, Jr, Lindvall E, Bolhofner B, Scaduto JM. The combined hip procedure: open reduction internal fixation combined with total hip arthroplasty for the management of acetabular fractures in the elderly. J Orthop Trauma. 2010 May;24(5):291–6. doi: 10.1097/BOT.0b013e3181b1d22a. [DOI] [PubMed] [Google Scholar]
- 25.De Bellis UG, Legnani C, Calori GM. Acute total hip replacement for acetabular fractures: a systematic review of the literature. Injury. 2014 Feb;45(2):356–61. doi: 10.1016/j.injury.2013.09.018. [DOI] [PubMed] [Google Scholar]
- 26.Hirvensalo E, Lindahl J, Bostman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993;297:28–32. [PubMed] [Google Scholar]
- 27.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123. [PubMed] [Google Scholar]
- 28.Stoppa RE, Rives JL, Warlaumont CR, et al. The use of Dacron in the repair of hernias of the groin. Surg Clin North Am. 1984;64:269–285. doi: 10.1016/s0039-6109(16)43284-6. [DOI] [PubMed] [Google Scholar]
- 29.Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified rives-stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010 May;24(5):263–70. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 30.Archdeacon MT, Kazemi N, Guy P, Sagi HC. The modified Stoppa approach for acetabular fracture. J Am Acad Orthop Surg. 2011 Mar;19(3):170–5. doi: 10.5435/00124635-201103000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Bible JE, Choxi AA, Kadakia RJ, Evans JM, Mir HR. Quantification of bony pelvic exposure through the modified Stoppa approach. J Orthop Trauma. 2014 Jun;28(6):320–3. doi: 10.1097/BOT.0000000000000032. [DOI] [PubMed] [Google Scholar]
- 32.Wang ZM, Sun HZ, Wang AM, DU QY, Wu SY, Zhao YF, Tang Y. Primary total hip arthroplasty for acetabular fracture. Chin J Traumatol. 2006 Dec;9(6):341–4. [PubMed] [Google Scholar]
- 33.Sermon A, Broos P, Vanderschot P. Total hip replacement for acetabular fractures. Results in 121 patients operated between 1983 and 2003. Injury. 2008 Aug;39(8):914–21. doi: 10.1016/j.injury.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 34.Tidermark J, Blomfeldt R, Ponzer S, Söderqvist A, Törnkvist H. Primary total hip arthroplasty with a Burch-Schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma. 2003 Mar;17(3):193–7. doi: 10.1097/00005131-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Mears DC, Velyvis JH. Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve-year results. J Bone Joint Surg Am. 2002 Jan;84-A(1):1–9. doi: 10.2106/00004623-200201000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Borens O, Wettstein M, Garofalo R, Blanc CH, Kombot C, Leyvraz PF, Mouhsine E. Treatment of acetabular fractures in the elderly with primary total hip arthroplasty and modified cerclage. Early results. Unfallchirurg. 2004 Nov;107(11):1050–6. doi: 10.1007/s00113-004-0827-6. [DOI] [PubMed] [Google Scholar]
- 37.Mouhsine E, Garofalo R, Borens O, Fischer JF, Crevoisier X, Pelet S, Blanc CH, Leyvraz PF. Acute total hip arthroplasty for acetabular fractures in the elderly: 11 patients followed for 2 years. Acta Orthop Scand. 2002 Dec;73(6):615–8. doi: 10.1080/000164702321039552. [DOI] [PubMed] [Google Scholar]
- 38.Sarkar MR, Wachter N, Kinzl L, Bischoff M. Acute total hip replacement for displaced acetabular fractures in older patients. Eur J Trauma. 2004;30:296–304. [Google Scholar]
- 39.Simko P, Braunsteiner T, Vajcziková S. Early primary total hip arthroplasty for acetabular fractures in elderly patients. Acta Chir Orthop Traumatol Cech. 2006 Aug;73(4):275–82. [PubMed] [Google Scholar]
- 40.Starr AJ, Reinert CM, Jones AL. Percutaneous fixation of the columns of the acetabulum: a new technique. J Orthop Trauma. 1998 Jan;12(1):51–8. doi: 10.1097/00005131-199801000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Gary JL, Lefaivre KA, Gerold F, Hay MT, Reinert CM, Starr AJ. Survivorship of the native hip joint after percutaneous repair of acetabular fractures in the elderly. Injury. 2011 Oct;42(10):1144–51. doi: 10.1016/j.injury.2010.08.035. [DOI] [PubMed] [Google Scholar]
- 42.Daurka JS, Pastides PS, Lewis A, Rickman M, Bircher MD. Acetabular fractures in patients aged > 55 years: a systematic review of the literature. Bone Joint J. 2014 Feb;96-B(2):157–63. doi: 10.1302/0301-620X.96B2.32979. [DOI] [PubMed] [Google Scholar]
- 43.Grazioli A, Ek ET, Rüdiger HA. Biomechanical concept and clinical outcome of dual mobility cups. Int Orthop. 2012;36(12):2411–8. doi: 10.1007/s00264-012-1678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bhaskar D, Parker MJ. Haematological indices as surrogate markers of factors affecting mortality after hip fracture. Injury. 2011 Feb;42(2):178–82. doi: 10.1016/j.injury.2010.07.501. [DOI] [PubMed] [Google Scholar]
- 45.Gabbe BJ, de Steiger R, Esser M, Bucknill A, Russ MK, Cameron PA. Predictors of mortality following severe pelvic ring fracture: results of a population-based study. Injury. 2011 Oct;42(10):985–91. doi: 10.1016/j.injury.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 46.Suzuki T, Morgan SJ, Smith WR, Stahel PF, Gillani SA, Hak DJ. Postoperative surgical site infection following acetabular fracture fixation. Injury. 2010 Apr;41(4):396–9. doi: 10.1016/j.injury.2009.11.005. [DOI] [PubMed] [Google Scholar]