Abstract
Objective
To analyze the effects of a decision aid on improving patients’ and family members’ information giving and question asking during consultations for prostate cancer treatment decision-making.
Methods
This study is a secondary analysis of archived audio-recorded real-time consultation visits with participants from a randomized clinical trial. Participants were randomly assigned into three groups: TD—intervention targeted patient-only; TS—intervention targeted patients and family members; and control—a handout on staying healthy during treatment. We conducted content analysis using a researcher-developed communication coding system. Using SAS 9.3, we conducted Chi-square/Fisher’s exact test to examine whether information giving and question asking among patients and family members varied by groups when discussing different content/topics.
Results
Compared with those in the TS and control groups, significantly higher percentages of participants in the TD group demonstrated information giving in discussing topics about diagnosis, treatment options, risks and benefits, and preferences; and engaged in question asking when discussing diagnosis, watchful waiting/active surveillance, risks and benefits, and preferences for treatment impacts.
Conclusion
Information support and communication skills training for patients were effective in improving communication during treatment decision-making consultations.
Practice implications
Providing information about prostate cancer and communication skills training empower patients and their family members.
Keywords: Localized prostate cancer, Decision-making, Patient-provider communication, Decision aid, Uncertainty, Intervention
1. Introduction
Prostate cancer is the most frequently diagnosed non-skin cancer for men in the U.S., with 181,000 new cases diagnosed in 2016 [1]; approximately 90% have localized or regional disease Although several treatment options are available, no one is clearly superior in terms of mortality benefits and risks treatment complications and side-effects [3]. Given the about the optimal treatment strategy for localized cancer, the decision on whether and how to treat cancer is considered preference sensitive because and providers need to balance the significant impact treatment on patients’ quality and length of life [4]. Intentional cooperative communication between patients, their family and providers, thus, is critical in sharing knowledge, values, and preferences [5]. This communication can also help patients and their family members obtain balanced and comprehensive information; understand potential treatment options and their impacts; reflect on their values and preferences; and ultimately, enhance shared decision-making [6–8]. While patient-provider communication is critical during treatment decision-making, family members, especially their spouses, often attend consultation visits and are involved in discussing treatment options with both the patient and the providers [9,10] and directly assist in information giving and question asking during consultations [11]. Research has found that the presence of family members enhances patients’ communication behaviors such as asking questions [12,13] and active involvement in decision-making [13].
To help patients with localized prostate cancer make an informed treatment decision, intervention strategies in current decision aids include communication skills training or role modeling to improve communication between patients, their family members, and providers for clinical encounters [14–16]; providing information using multimedia [14,15,17–24]; facilitating value clarification and reducing decision conflicts [14,18,19,22,24]; and providing consultation plans and preparation materials [19,23–25]. Although improving communication skills for patients and their family members is one of the integral strategies in decision aid interventions for localized prostate cancer treatment choices, a recent systematic review and meta-analysis [5] found that patient-provider communication was evaluated only in one clinical trial using a Likert-type scale after consultation visits [16]. Patients’ and their family members’ communication behaviors during treatment decision-making consultation visits have not been evaluated as an outcome in decision aid research in the context of prostate cancer.
Research-to-date has analyzed real time recordings of medical encounters about physicians’ communication behaviors and the clinical visit structure within the context of treatment decision-making for prostate cancer [26,27] or used self-reported data collected from patients after treatment decisions were made [16,28–31]. Effective and competent physician-directed communication constitutes only one of the core communication dimensions in cancer care [32]; patients and their family members also participate in the consultation and play a role in communication that is equally important to that of the providers. Patients’ responses to providers’ statements may significantly influence the content and structure of medical encounters as well as providers beliefs and behaviors [33]. Medical encounters such as treatment consultation visits are considered deliberation processes where patients and their family members become aware of choices and options, and have the time and support to consider what matters most to them; in other words a patient-centered approach to decision-making [7]. Therefore, it is important to examine patients’ and their family members’ communication behaviors (e.g., providing information, asking questions) when discussing specific topics related to treatment decision-making. Yet, commonly used patient self-reported retrospective data increase the risk for flawed recall [34] and social desirability bias [35]. Furthermore provider reported patient data do not reflect patient communication and participation in decision-making [30,36]. No decision aid studies to-date have assessed the real-time communication behaviors of patients with localized prostate cancer and their family members using audiotaped or videotaped data during treatment decision-making consultation visits.
To address these gaps, the purpose of this study was to analyze the effects of a decision aid on improving patients’ and their family members’ participation in communication focused on treatment decision-making for localized prostate cancer using real-time audio-recordings of consultation visits. Given the small proportion of family members actively involved in these consultations, we focused on the “joint” patient-family member communication with providers in each encounter (rather than the roles of individual participants in the consultations) and quantitatively examined the dynamic process information giving and question asking that occur during the verbal information exchange between providers, patients, and their family member(s) [6,37]. We hypothesized that higher percentages of patients and family members in the intervention groups would demonstrate more information giving and question asking behaviors than those in the control group.
2. Methods
2.1. Study design
This study is a secondary analysis of archived audio-recorded real-time consultation visits with participants from a randomized clinical trial (RCT) that tested the effects of a decision aid intervention in the southeast of USA [16]. Built upon the Uncertainty in Illness Theory [38], the Decision-Making Uncertainty Management Intervention (DMUMI) aimed to improve informed treatment decision-making for patients with localized prostate cancer by empowering patients and their family members through communication skills training and information support [16]. In the RCT patients were randomly assigned to the treatment direct (TD, DMUMI targeted the patient-only), treatment supplemented (TS, DMUMI targeted the patient and his family member), or control (usual care plus a handout on staying healthy during treatment) groups [16].
The purpose of the consultation visits was for men and their family members to discuss treatment options and seek support for treatment decision-making after receiving their biopsy results and diagnosis. Physicians agreed to place a sign in their clinics announcing that consultation sessions would be randomly taped in order to verify the length of their interviews. Non-study patients that were newly diagnosed but refused to participate in the RCT or did not meet study criteria were approached and consented for the recording of random interviews; and their interview tapes were erased after their sessions. Consented physicians were blinded to the randomization and patient participation in the DMUMI by taping an equal number of non-study patients. Details describing the study sample and recruitment procedures were reported previously [16]. Approval was obtained from the Institutional Review Boards at all study sites.
2.2. Participants
In the RCT, patients were eligible if they (1) were newly diagnosed with localized prostate cancer (stages T1a, T1b, T1c, T2a or T2b); (2) were identified at least 10 days before the treatment consultation appointment; (3) had no major cognitive impairment; (4) had no prior cancer history; (5) could read and speak English; and (6) had a family member who was identified as providing primary support to the patient (PSP) and was willing to participate in the study. The study and recruitment process have been described previously [16]. All intervention and control groups contained both African-American and Caucasian men with prostate cancer. Among 410 men contacted, 343 were eligible, and 256 agreed to participate [16]. This study included 156 patients and their family members who provided demographic data and agreed to be recorded during their consultation visits (N = 54 in TD; N = 56 in TS; and N = 46 in Control).
2.3. The DMUMI intervention
As previously reported [16], patients in the TD and TS arms received a DVD, a booklet, and four phone calls. The only difference between the TD and TS groups was that patients’ PSPs in the TS group also received the same phone calls, separately, from the same nurse [16]. The professionally produced DVD, entitled “Talking to your doctor about prostate cancer,” was designed to demonstrate how to engage in effective communication using information giving, seeking, verifying, and clarifying skills. Actors portrayed Caucasian and African-American men as prostate cancer patients in scenarios in which patients talked with their doctors about treatment options by providing information and asking questions. The booklet, “Treatment Choices for Early Stage Prostate Cancer: Patients’ Questions–Doctors’ Answers,” provided patient-focused, evidence-based guidelines to treatment issues for early stage prostate cancer. Participants could use the tear-out sheet in the back of the booklet to identify their personal concerns, specific questions about treatment options for their physicians, and record answers to their questions.
Four nurse-delivered intervention calls over 7–10 days began immediately after participants received the DVD and booklet. These calls focused on participants’ questions about the content in the booklet and review of a handout on “The Competent Patient”. The nurses also helped participants to identify and formulate specific questions based on their concerns as well as review and practice using role-play the communication skills on the DVD and the strategies for using them.
2.4. Analytical approach
2.4.1. Patient characteristics measures
Patient characteristics information (i.e., age, education, and race) and prostate cancer information (i.e., Gleason score and prostate-specific antigen, PSA) were collected using questionnaires prior to the randomization and treatment consultation visits.
2.4.2. Communication coding
To identify and analyze information giving and question asking behaviors when discussing prostate cancer treatment-related content/topics, we first used a communication coding system [39] developed previously by the research team based on the National Comprehensive Cancer Network (NCCN) treatment guideline for localized prostate cancer [40], theories on shared decision-making [7,41], and previous research on patient-provider communication [42,43] and medical consultation [37]. The measures included codes for communicators, communication behaviors, and content/topics of the consultation visits. The communicators included patients, their family members (including PSPs), and physician(s) at the consultations. The communication behaviors included information giving (any direct statement on a topic initiated by either a patient, a family member, or a physician about facts and evidence, personal thoughts and experiences) and question asking (any verbal attempt to seek, clarify, or verify information with a traditional interrogative form that included who, what, when, why, or how, or a subject-verb inversion (e.g., “Can I …”)). Information giving, clarifying, seeking, and verifying were the communication skills that DMUMI aimed to enhance. Communication content/topics included prostate cancer treatment-related topics in 4 domains: (a) delivering diagnosis (diagnosis, current prostate cancer-related symptoms, and patient health status/comorbid conditions related to decision-making); (b) treatment options of watchful waiting/active surveillance, surgery, and radiotherapy; (c) risks and benefits related to urinary and sexual side-effects, treatment procedures, complications, cancer progression and recurrence; and (d) patient/family member treatment preferences related to cancer control; treatment cost and health insurance coverage; patient life arrangement/employment; treatment impact on urinary and sexual functions; and more time to obtain additional input from others. These content/topics, critical for informed decision-making, have been promoted in the DMUMI. Use of different communication behaviors to cover these content/topics ensures that patients are supported to explore their preferences while being informed about treatment options and related risks, benefits, and impacts.
Using Atlas Ti 6© (Scientific Software Development GmbH, Berlin), five trained coders conducted a content analysis by independently coding whether the communication behaviors related to each content/topic category were present or absent in different communicators (i.e., coded as “Yes” and “No”, respectively). The communication behaviors of patients and their family members were combined in each domain to capture the communication characteristics during the consultation visits. This decision was made due to the concerns that the study would not yield statistical results in most of the communication content/topics for family members. Family members of approximately 100 patients were not present at the consultation visits or did not engage in any verbal communication, resulting in extremely low sample sizes (such as zeros in all groups) in most of the communication content/topic areas in each study group. In addition, the communication behaviors among patients whose family members were not present at the consultations and those accompanied by family members with or without verbal communication may be different, which also resulted in sample sizes that were too small to generate any statistical results. In order to assess the effects of the DMUMI program, we thus decided to examine the communication characteristics of each encounter rather than to focus on individual participant’s roles and contributions in these consultations.
In addition, although more than one provider was involved during some consultation visits, consultations occurred separately with each provider. In order to capture all communication behaviors used by patients and their family members, we coded their communication behaviors as if they were interacting with one provider during one single interview. The decision to combine providers’ communication behaviors across interviews during the same consultation encounter was based on the consideration that patients and family members might use different communication behaviors when discussing the same content/topic (as listed above) with different providers to help understand their treatment options and make informed decisions.
The initial codebook was tested in the control group and later refined by all members of the coding team. A random sample of 25% of the transcripts (N = 40) was used to evaluate the inter-rater coding reliability. Each of these transcripts was independently coded by at least two coders; the percent agreement among coders was above 80%, indicating satisfactory inter-rater reliability [44,45]. During the study period, the research team had constant discussions weekly or biweekly about coding and related issues to reach consensus among coders.
2.5. Data analysis
Data analyses were conducted using SAS 9.3 (Cary, NC). Univariate analysis was conducted to describe the counts of communication behaviors within content/topic categories for patients and their family members. Chi-square test and Fisher’s exact test were used to examine whether patients’ and family members’ communication behaviors when discussing different contents varied by being in different groups (TD, TS, and control). We used two-tailed tests and a p-value of 0.05 as a threshold to evaluate the null hypothesis.
3. Results
3.1. Participant characteristics
Table 1 presents the demographic information of patients and their PSPs. Thirty percent of patients and twenty-four percent of family members were African-Americans. On average, patients were about 62 years of age and had 15 years of education; their family members were about 58 years of age and had 15 years of education. Close to 82% of the providers at the consultation visits were urologic surgeons; attending physicians presented at all visits whereas residents and fellows presented at 7.7% of the visits. Family members provided information at approximately 48%, 59%, and 49% of the visits in the TD, TS, and control groups, respectively. Significantly higher percentages of family members in the control group asked questions than those in the other two groups (p<0.01).
Table 1.
Participant Characteristics.
| Patient | Total N = 156 | TD (N = 54) | TS (N = 56) | Control (N = 46) | |
|---|---|---|---|---|---|
| Variables | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ANOVA |
| Age | 61.99 (7.24) | 62.98 (7.32) | 62.36 (7.47) | 60.43 (6.75) | – |
| Education | 15.15 (3.55) | 14.48 (3.78) | 15.38 (3.23) | 15.62 (3.39) | – |
|
| |||||
| N (%) | N(%) | N (%) | N(%) | Ch-sq | |
|
| |||||
| Race: Caucasian | 110 (70) | 40 (74) | 37 (66) | 33 (70) | – |
| African American | 47 (30) | 14 (26) | 19 (34) | 14 (30) | |
| Physician specialties at the visit | |||||
| Urologic Surgeon | 129 (82.7) | 46 (85.2) | 44 (78.6) | 39 (84.8) | |
| Radiation Oncologist | 12 (7.7) | 4 (7.4) | 5 (8.9) | 3 (6.5) | |
| Medical oncologist | 17 (10.9) | 4 (7.4) | 8 (14.3) | 5 (10.9) | |
| Physician rank | |||||
| Resident/fellow | 12 (7.7) | 2 (3.7) | 5 (8.9) | 5 10.9) | |
| Attending | 156 (100) | 54 (100) | 56 (100) | 46 (100) | |
| Family member(s) provided information | 82 (52) | 26 (48) | 33 (59) | 23 (49) | 1.57 |
| Family member(s) asked question(s) | 74 (47) | 18 (33) | 28 (50) | 28 (60) | 7.23** |
|
| |||||
| Primary family member to support the patient | Total N = 135 | TD (N = 43) | TS (N = 56) | Control (N = 36) | |
| Variables | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ANOVA |
|
| |||||
| Age | 58.04 (9.04) | 59.44 (8.93) | 57.18 (8.62) | 57.69 (9.04) | – |
| Education | 14.87 (2.54) | 14.60 (2.97) | 15.21 (2.40) | 14.63 (2.60) | – |
| N (%) | N(%) | N (%) | N(%) | – | |
| Race | |||||
| Caucasian | 102 (75.6) | 33 (71.9) | 37 (66.1) | 31 (86.1) | |
| African American | 33 (24.4) | 9 (28.1) | 19 (33.9) | 5 (13.9) | |
Note: TD—intervention targeted patient-only; TS—intervention targeted patients and family members.
3.2. Patients’ and family members’ communication behaviors
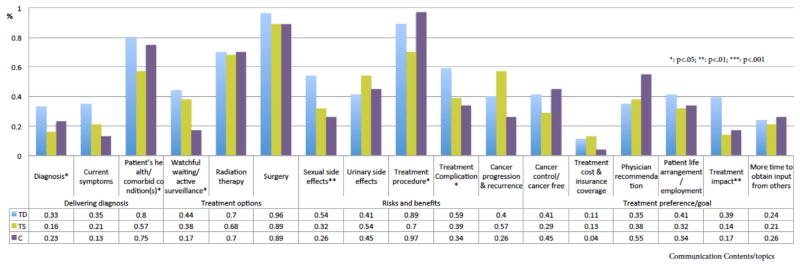
Results of differences in information giving behaviors across groups are displayed in Fig. 1. Examples of quotes related to each communication content/topic are in Table 2. The results showed a consistently higher percentage of patients and family members demonstrating information giving behaviors in the TD group than those in the TS and control groups when discussing topics across all communication content domains. Specifically, significantly higher percentages of patients and family members in the TD group than those in TS and control groups provided information about their prostate cancer diagnosis (p <0.001), prostate cancer-related current symptoms (p <0.01), and their health status and comorbid conditions (p <0.05). Compared with the TS and control groups, a significantly higher percentage of participants in the TD group provided their thoughts about watchful waiting/active surveillance (p <0.05). When discussing treatment-related risks and benefits, higher percentages of participants in the TD group than those in the TS and control groups provided information on topics about sexual (p <0.05) and urinary side-effects (p <0.01), treatment procedures (p <0.001), cancer progression (p <0.001), and treatment complications (p <0.01). Finally, among all communication topics about patient treatment preference, a significantly higher percentage of participants in the TD and control groups than those in the TS group provided information when discussing their preferences related to the impact of different types of treatment (p <0.01).
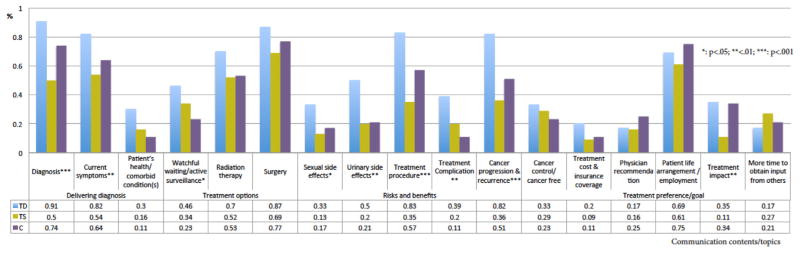
Results about question asking behaviors across groups are displayed in Fig. 2. Examples of quotes related to each communication content/topic are in Table 3. In the delivering diagnosis domain, a higher percentage of participants in the TD group engaged in question asking behaviors when discussing prostate cancer diagnosis (p <0.05) and patient’s health status and comorbid conditions (p <0.05) compared with those in the TS and control groups. Among all treatment options discussed, higher percentages of participants in the TD and TS groups than those in the control group asked questions related to watchful waiting/active surveillance. In the treatment risks and benefits domain, higher percentages of participants in the TD group asked questions about sexual side effects (p <0.01) and treatment complications (p<0.05), whereas a higher percentage of participants in the control group asked questions about treatment procedures (p <0.05). Finally, a higher percentage of participants in the TD group than those in the other two groups asked questions about preferences related to treatment impacts (p <0.01).
Fig. 1.
Comparison of patient and family companion information giving behaviors among groups.
Note: TD—intervention targeted patient-only; TS—intervention targeted patients and family members; C—Control group.
Table 2.
Patient and family information giving communication behaviors during consultation visits.
| Domains | Contents/Topics | Example of Quotes |
|---|---|---|
| Delivering diagnosis | Current symptoms related to prostate cancer |
|
| Diagnosis |
|
|
| Patient’s health status/comorbid condition(s) |
|
|
| Treatment options | Watchful waiting/active surveillance | na |
| Radiation therapy |
|
|
| Surgery |
|
|
| Risks and benefits | Urinary side effects |
|
| Sexual side effects |
|
|
| Treatment procedure |
|
|
| Treatment Complications |
|
|
| Cancer progression and recurrence |
|
|
| Treatment preference | Cancer control/cancer free result |
|
| Treatment cost and insurance coverage |
|
|
| Provider recommendation |
|
|
| Patient life arrangement/employment |
|
|
| Treatment impact |
|
|
| More time to obtain input from others |
|
Fig. 2.
Comparison of patient and family companion question asking behaviors among groups.
Note: TD—intervention targeted patient-only; TS—intervention targeted patients and family members; C—Control group.
Table 3.
Patient and family question asking communication behaviors during consultation visits.
| Domains | Contents/Topics | Example of Quotes |
|---|---|---|
| Delivering diagnosis | Current symptoms related to prostate cancer Diagnosis |
|
| Patient’s health status/comorbid condition(s) |
|
|
| Treatment options | Watchful waiting/active surveillance |
|
| Radiation therapy |
|
|
| Surgery |
|
|
| Risks and benefits | Sexual side effects |
|
| Urinary side effects |
|
|
| Treatment procedure |
|
|
| Treatment Complications |
|
|
| Cancer progression and recurrence |
|
|
| Treatment preference | Cancer control/cancer free result |
|
| Treatment cost and insurance coverage |
|
|
| Physician recommendation |
|
|
| Patient life arrangement/employment |
|
|
| Treatment impact |
|
|
| More time to obtain input from others |
|
4. Discussion and conclusion
4.1. Discussion
To our knowledge, this is the first study that has used direct observation (i.e., real-time audio recordings of consultation visits) to examine the effects of a decision aid on improving patients’ and their family members’ communication behaviors during consultation visits for prostate cancer treatment decision-making. Overall, our results indicated that higher percentages of patients and their family members in the TD group than those in the TS and control groups demonstrated information giving and question asking behaviors when discussing different content/topics related to treatment decision-making for prostate cancer. These results, partially confirmed our hypotheses, showed that the multi-component decision aid DMUMI targeting patient-only effectively enhanced patients’ and their family members’ information giving and questions asking behaviors when discussing different content/topics related to prostate cancer treatment decision-making during consultation visits. The DMUMI decision aid included a culturally sensitive DVD video demonstrating skills of information giving, seeking, verifying and clarifying for effective communication with providers; the information booklet about treatment options for early stage prostate cancer; and the nurses’ phone calls to educate and help patients practice communication skills [16]. These information and skills training not only informed patients about what to expect during prostate cancer treatment and consultation visits, but also empowered them to engage in interactions with physicians during consultation visits. Our findings among patients with newly diagnosed localized prostate cancer corroborated the findings of recent intervention research using video-clips among primary health-care patients [46] as well as the findings of a previous systematic review that reported patient-directed communication interventions (such as model communication behaviors, help practice question-asking skills) significantly increased question asking behaviors among patients with different illnesses [47].
It was somewhat surprising that lower percentages of participants in the TS group demonstrated information giving and question asking behaviors when discussing content/topics related to diagnosis, treatment procedures, and preferences of treatment impacts than those in the TD group. It is likely that prior to their consultation visits, patients and their family members, when both were involved in the DMUMI, received more information from the multi-component intervention about prostate cancer that was pertinent to the patient’s condition. They may also have discussed the related issues with the intervention nurse and between themselves, especially the psychosocial issues related to prostate cancer. These information and discussions ahead of the consultation visit, in turn, may have resulted in a reduction in their subsequent requests for additional information from physicians than what had been provided during consultation. A recent meta-analysis found that family presence helped patient information giving and question asking during medical visits. However, physicians engaged in more biomedical information giving and less social conversation, and patients provided less psychosocial information [11]. Prostate cancer and its treatment can impact both patients’ physical and psychosocial well-being; patients depend on their family, especially their partners, for social and emotional support. Compared with the intervention targetting patient-only (TD), involving both patients and family members in the intervention (TS) may have equipped them with skills needed to discuss more freely private and sensitive issues related to prostate cancer and its treatment, and thus, reduced their needs for more information exchange with their providers at consultation visits.
It was interesting that, compared with those in the TD and TS groups, a significantly higher percentage of patients and family members in the control group asked questions about treatment procedures and physician recommendations for treatment. In the original RCT, patients in the control group received information about how to stay healthy during treatment for prostate cancer, which may have increased patients’ and family members’ concerns about the treatment procedures and thus may have led them to ask more related questions for physicians to clarify. Lacking sufficient information about prostate cancer and its treatments (such as options, risks and benefits) and communication skills training may also have led these patients and their family members to ask for providers’ recommendations.
Finally, our findings indicated that, compared with those in the TD group, significantly higher percentages of family members in the TS and control groups asked questions during the consultation visits, despite the fact that patients and family members in the TS and control groups engaged in singnificantly less information giving and question asking than those in the TD group. In a recent study using KINcode to analyze communication behaviors in cancer consultations, researchers found that family members interrupted or answered for the patients; prompted patient questions; summarized or repeated information for the patient; and made optimistic/positive statements [48]. Our future research needs to examine whether the patients and their family members in the DMUMI study engaged in similar patterns of communication, which may have contributed to our findings.
The limitations of this study warrant further research. This study examined the effects of the overall DMUMI on information giving and question asking behaviors during consultations for prostate cancer treatment. Future research is needed to determine the effects of different intervention components (e.g., the DVD, nurse phone calls, and the booklet) and different dosages of the intervention (e.g., 4 versus fewer nurse calls) so as to provide clinicians the evidence to enhance oncologic care that requires the least resources. Next, we focused on verbal communication but did not examine the nonverbal behaviors or the affective component although they are all critical aspects of communication. Additionally, we analyzed the audio recordings of one consultation visit of each patient although patients with prostate cancer may have had more than one clinical visit or contact that was not face-to-face and may have discussions with others and/or used other decision support [7]. In addition, the data available from the RCT only allowed us to quantitatively examine the effects of DMUMI on the “joint” communication behaviors of patients and family members because a limited number of family members presented at the consultations and/or actively participated in the communication. Future research, however, is needed to explore the roles and contributions of the individual participants in these encounters. Research is also needed to examine the family dynamics; their impact on the communication among patients, family members, and providers; and the benefits, challenges, and strategies to facilitate family involvement to enhance healthcare outcomes. Finally, this study focused on the communication behaviors of patients and family members, which may have simplified the interpersonal process in which providers played an extremely important role in eliciting patient and family concerns [49]. Future research is needed to explore the complexity of the communication interactions during treatment consultation visits.
4.2. Conclusion
The DMUMI program that provided information support and communication skills training to patients with newly diagnosed localized prostate cancer was effective in improving information giving and question asking behaviors in patients and their family members when they jointly discussed about cancer diagnosis, treatment options, risks and benefits, and treatment preferences during treatment decision-making consultation visits. The same decision aid intervention targeting both patients and their family members may decrease their needs for extensive information exchange during consultations.
4.3. Practice implications
In addition to providing treatment-related information for localized prostate cancer, it is important to provide communication skills training to patients and their family members to empower their interaction with healthcare providers.
Acknowledgments
The authors thank Drs. Merle Mishel and Barbara Germino for sharing the dataset and the research participants participating in the Uncertainty Management study (5R01NR08144, PI: Mishel) for their contributions.
Footnotes
Conflict of interest disclosures
None.
Support/financial disclosures
The work of Dr. Song is sponsored by the Clinical and Translational Sciences Award (CTSA), University of North Carolina-Chapel Hill (grant number: KL2TR001109 and UL1TR001111, PI: Runge, and then Buse and Carey) and the UNC Lineberger Comprehensive Cancer Center University Cancer Research Fund (PI: Song).
References
- 1.American Cancer Society. Cancer Facts & Figs 2016 Figs 2016. Atlanta: 2016. [Google Scholar]
- 2.Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, et al. Cancer treatment and survivorship statistics. CA Cancer J Clin. 2012;62:220–241. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 3.National Cancer Institute. Prostate Cancer Treatment-for Health Professionals (PDQ®)-General Information for Prostate Cancer. National Cancer Institute; Bethesda, MD: 2015. [Google Scholar]
- 4.Stacey D, Légaré F, Col Nananda F, Bennett Carol L, Barry Michael J, Eden Karen B, et al. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2014. Decision aids for people facing health treatment or screening decisions. [DOI] [PubMed] [Google Scholar]
- 5.Violette PD, Agoritsas T, Alexander P, Riikonen J, Santti H, Agarwal A, et al. Decision aids for localized prostate cancer treatment choice: systematic review and meta-analysis. CA: Cancer J Clin. 2015;65:239–251. doi: 10.3322/caac.21272. [DOI] [PubMed] [Google Scholar]
- 6.Albrecht TL, Eggly SS, Gleason ME, Harper FW, Foster TS, Peterson AM, et al. Influence of clinical communication on patients’ decision making on participation in clinical trials. J Clin Oncol. 2008;26:2666–2673. doi: 10.1200/JCO.2007.14.8114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elwyn G, Frosch D, Thomson R, Joseph-Williams N, Lloyd A, Kinnersley P, et al. Shared decision making: a model for clinical practice. J Gen Internal Med. 2012;27:1361–1367. doi: 10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clayton MF, Latimer S, Dunn TW, Haas L. Assessing patient-centered communication in a family practice setting: how do we measure it, and whose opinion matters. Patient Edu Couns. 2011;84:294–302. doi: 10.1016/j.pec.2011.05.027. [DOI] [PubMed] [Google Scholar]
- 9.Zeliadt SB, Penson DF, Moinpour CM, Blough DK, Fedorenko CR, Hall IJ, et al. Provider and partner interactions in the treatment decision-making process for newly diagnosed localized prostate cancer. BJU Int. 2011;108(6):851–856. doi: 10.1111/j.1464-410X.2010.09945.x. [DOI] [PubMed] [Google Scholar]
- 10.Symes Y, Song L, Heineman RG, Barbosa BD, Tatum K, Greene G, et al. Involvement in decision making and satisfaction with treatment among partners of patients with newly diagnosed localized prostate cancer. Oncol Nurs Forum. 2015;42:672–679. doi: 10.1188/15.ONF.672-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wolff JL, Roter DL. Family presence in routine medical visits: a meta-analytical review. Soc Sci Med. 2011;72:823–831. doi: 10.1016/j.socscimed.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eggly S, Harper FW, Penner LA, Gleason MJ, Foster T, Albrecht TL. Variation in question asking during cancer clinical interactions: a potential source of disparities in access to information. Patient Educ Couns. 2011;82:63–68. doi: 10.1016/j.pec.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clayman ML, Roter D, Wissow LS, Bandeen-Roche K. Autonomy-related behaviors of patient companions and their effect on decision-making activity in geriatric primary care visits. Soc Sci Med (1982) 2005;60:1583–1591. doi: 10.1016/j.socscimed.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 14.Marcus AC, Diefenbach MA, Stanton AL, Miller SM, Fleisher L, Raich PC, et al. Cancer patient and survivor research from the cancer information service research consortium: a preview of three large randomized trials and initial lessons learned. J Health Commun. 2013;18:543–562. doi: 10.1080/10810730.2012.743629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hack TF, Pickles T, Bultz BD, Ruether JD, Degner LF. Impact of providing audiotapes of primary treatment consultations to men with prostate cancer: a multi-site, randomized, controlled trial. Psychooncology. 2007;16:543–552. doi: 10.1002/pon.1094. [DOI] [PubMed] [Google Scholar]
- 16.Mishel MH, Germino BB, Lin L, Pruthi RS, Wallen EM, Crandell J, et al. Managing uncertainty about treatment decision making in early stage prostate cancer: a randomized clinical trial. Patient Educ Couns. 2009;77:349–359. doi: 10.1016/j.pec.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 17.Davison BJ, Goldenberg SL, Wiens KP, Gleave ME. Comparing a generic and individualized information decision support intervention for men newly diagnosed with localized prostate cancer. Cancer Nurs. 2007;30:E7–E15. doi: 10.1097/01.NCC.0000290819.22195.d6. [DOI] [PubMed] [Google Scholar]
- 18.Taylor KL, Davis KM, Lamond T, Williams RM, Schwartz MD, Lawrence W, et al. Use and evaluation of a CD-ROM-based decision aid for prostate cancer treatment decisions. Behav Med (Washington, DC) 2010;36:130–140. doi: 10.1080/08964289.2010.525263. [DOI] [PubMed] [Google Scholar]
- 19.Berry DL, Halpenny B, Hong F, Wolpin S, Lober WB, Russell KJ, et al. The personal patient profile-prostate decision support for men with localized prostate cancer: a multi-center randomized trial. Urol Oncol: Semin Original Invest. 2013;31:1012–1021. doi: 10.1016/j.urolonc.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diefenbach MA, Mohamed NE, Butz BP, Bar-Chama N, Stock R, Cesaretti J, et al. Acceptability and preliminary feasibility of an internet/CD-ROM-based education and decision program for early-stage prostate cancer patients: randomized pilot study. J Med Internet Res. 2012;14:e6. doi: 10.2196/jmir.1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van Tol-Geerdink JJ, Willem Leer J, Weijerman PC, van Oort IM, Vergunst H, van Lin EN, et al. Choice between prostatectomy and radiotherapy when men are eligible for both: a randomized controlled trial of usual care vs decision aid. BJU Int. 2013;111:564–573. doi: 10.1111/j.1464-410X.2012.11402.x. [DOI] [PubMed] [Google Scholar]
- 22.Feldman-Stewart D, Tong C, Siemens R, Alibhai S, Pickles T, Robinson J, et al. The impact of explicit values clarification exercises in a patient decision aid emerges after the decision is actually made: evidence from a randomized controlled trial. Med Decis Making. 2012;32:616–626. doi: 10.1177/0272989X11434601. [DOI] [PubMed] [Google Scholar]
- 23.Hacking B, Wallace L, Scott S, Kosmala-Anderson J, Belkora J, McNeill A. Testing the feasibility, acceptability and effectiveness of a ‘decision navigation’ intervention for early stage prostate cancer patients in Scotland-a randomised controlled trial. Psychooncology. 2013;22:1017–1024. doi: 10.1002/pon.3093. [DOI] [PubMed] [Google Scholar]
- 24.Chabrera C, Zabalegui A, Bonet M, Caro M, Areal J, Gonzalez JR, et al. A decision aid to support informed choices for patients recently diagnosed with prostate cancer: a randomized controlled trial. Cancer Nurs. 2015;38:E42–50. doi: 10.1097/NCC.0000000000000170. [DOI] [PubMed] [Google Scholar]
- 25.Davison BJ, Degner LF. Empowerment of men newly diagnosed with prostate cancer. Cancer Nurs. 1997;20:187–196. doi: 10.1097/00002820-199706000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Henry SG, Czarnecki D, Kahn VC, Chou WY, Fagerlin A, Ubel PA, et al. Patient-physician communication about early stage prostate cancer: analysis of overall visit structure. Health Expect. 2015;18:1757–1768. doi: 10.1111/hex.12168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holmes-Rovner M, Montgomery JS, Rovner DR, Scherer LD, Whitfield J, Kahn VC, et al. Informed decision making: assessment of the quality of physician communication about prostate cancer diagnosis and treatment. Med Decis Making. 2015;35:999–1009. doi: 10.1177/0272989X15597226. [DOI] [PubMed] [Google Scholar]
- 28.Song L, Bensen JT, Zimmer C, Sleath B, Blackard B, Fontham E, et al. Patient-health care provider communication among patients with newly diagnosed prostate cancer: findings from a population-based survey. Patient Educ Couns. 2013;91:79–84. doi: 10.1016/j.pec.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Song L, Hamilton JB, Moore AD. Patient-healthcare provider communication: perspectives of African American cancer patients. Health Psychol. 2012;31:539–547. doi: 10.1037/a0025334. [DOI] [PubMed] [Google Scholar]
- 30.Mazor KM, Street RL, Jr, Sue VM, Williams AE, Rabin BA, Arora NK. Assessing patients’ experiences with communication across the cancer care continuum. Patient Educ Couns. 2016;99(8):1343–1348. doi: 10.1016/j.pec.2016.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cegala DJ, Bahnson RR, Clinton SK, David P, Gong MC, Monk JP, III, et al. Information seeking and satisfaction with physician-patient communication among prostate cancer survivors. Health Commun. 2008;23:62–69. doi: 10.1080/10410230701806982. [DOI] [PubMed] [Google Scholar]
- 32.Ishikawa H, Hashimoto H, Kiuchi T. The evolving concept of patient-centeredness in patient-physician communication research. Soc Sci Med (1982) 2013;96:147–153. doi: 10.1016/j.socscimed.2013.07.026. [DOI] [PubMed] [Google Scholar]
- 33.Street RL, Jr, Millay B. Analyzing patient participation in medical encounters. Health Commun. 2001;13:61–73. doi: 10.1207/S15327027HC1301_06. [DOI] [PubMed] [Google Scholar]
- 34.Litwin MS, McGuigan KA. Accuracy of recall in health-related quality-of-life assessment among men treated for prostate cancer. J Clin Oncol. 1999;17:2882–2888. doi: 10.1200/JCO.1999.17.9.2882. [DOI] [PubMed] [Google Scholar]
- 35.Holtgraves T. Social desirability and self-reports: testing models of socially desirable responding. Pers Soc Psychol Bull. 2004;30:161–172. doi: 10.1177/0146167203259930. [DOI] [PubMed] [Google Scholar]
- 36.Clayton MF, Dudley WN, Musters A. Communication with breast cancer survivors. Health Commun. 2008;23:207–221. doi: 10.1080/10410230701808376. [DOI] [PubMed] [Google Scholar]
- 37.Pendleton D, Schofield T, Tate P, Havelock P. The New Consultation: Developing Doctor-patient Communication. Oxford University Press; 2003. [Google Scholar]
- 38.Mishel MH, Padilla G, Grant M, Sorenson DS. Uncertainty in illness theory: a replication of the mediating effects of mastery and coping. Nurs Res. 1991;40:236–240. [PubMed] [Google Scholar]
- 39.Song L, Toles MP, Bai J, Nielsen ME, Bailey DE, Sleath B, et al. Patient participation in communication about treatment decision-making for localized prostate cancer during consultation visits. Health. 2015;7:1419–1429. doi: 10.4236/health.2015.711156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guideline): Prostate Cancer. National Comprehensive Cancer Network; 2014. http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. [Google Scholar]
- 41.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. J Am Med Assoc. 1992;267:2221–2226. [PubMed] [Google Scholar]
- 42.McNeilis KS. Analyzing communication competence in medical consultations. Health Commun. 2001;13:5–18. doi: 10.1207/S15327027HC1301_02. [DOI] [PubMed] [Google Scholar]
- 43.Griffin SJ, Kinmonth AL, Veltman MW, Gillard S, Grant J, Stewart M. Effect on health-related outcomes of interventions to alter the interaction between patients and practitioners: a systematic review of trials. Ann Fam Med. 2004;2:595–608. doi: 10.1370/afm.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Polit DE, Beck CT. Nursing Research: Principles and Methods. 7. Lippincott Williams & Wilkins; Philadelphia, PA: 2004. [Google Scholar]
- 45.Krippendorff K. Agreement information in the reliability of coding. Commun Methods Measures. 2011;5:93–112. [Google Scholar]
- 46.Shepherd HL, Barratt A, Jones A, Bateson D, Carey K, Trevena LJ, et al. Can consumers learn to ask three questions to improve shared decision making? A feasibility study of the ASK (AskShareKnow) patient-clinician communication model intervention in a primary health-care setting. Health Expect. 2015;19(5):1160–1168. doi: 10.1111/hex.12409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harrington J, Noble LM, Newman SP. Improving patients’ communication with doctors: a systematic review of intervention studies. Patient Educ Couns. 2004;52:7–16. doi: 10.1016/s0738-3991(03)00017-x. [DOI] [PubMed] [Google Scholar]
- 48.Laidsaar-Powell R, Butow P, Bu S, Dear R, Fisher A, Coll J, et al. Exploring the communication of oncologists, patients and family members in cancer consultations: development and application of a coding system capturing family-relevant behaviours (KINcode) Psychooncology. 2016;25:787–794. doi: 10.1002/pon.4003. [DOI] [PubMed] [Google Scholar]
- 49.Clayton MF, Reblin M, Carlisle M, Ellington L. Communication behaviors and patient and caregiver emotional concerns: a description of home hospice communication. Oncol Nurs Forum. 2014;41:311–321. doi: 10.1188/14.ONF.311-321. [DOI] [PubMed] [Google Scholar]