Abstract
Introduction
Chinese Americans have low colorectal cancer (CRC) screening rates. Evidence-based interventions to increase CRC screening in this population are lacking. This study aims to compare the efficacy of two interventions in increasing CRC screening among Chinese Americans.
Design
Cluster randomized comparative trial.
Setting/participants
From 2010 to 2014, a community–academic team conducted this study in San Francisco, CA with Chinese Americans aged 50–75 years who spoke English, Cantonese, or Mandarin.
Intervention
Lay health worker (LHW) intervention plus in-language brochure (LHW+Print) versus brochure (Print). LHWs in the LHW+Print arm were trained to teach participants about CRC in two small group sessions and two telephone calls.
Main outcome measures
Change in self-reports of ever having had CRC screening and being up to date for CRC screening from baseline to 6-months post-intervention. Statistical analysis was performed from 2014 to 2015.
Results
This study recruited 58 LHWs, who in turn recruited 725 participants. The average age of the participants was 62.2 years, with 81.1% women and 99.4% foreign born. Knowledge increase was significant (p<0.002) for nine measures in the LHW+Print group and six in the Print group. Both groups had increases in having ever been screened for CRC (LHW+Print, 73.9% to 88.3%, p<0.0001; Print, 72.3% to 79.5%, p=0.0003) and being up to date for CRC screening (LHW+Print, 60.0% to 78.1%, p<0.0001; Print, 58.1% to 64.1%, p=0.0003). In multivariable analyses, the intervention OR for LHW+Print versus Print was 1.94 (95% CI=1.34, 2.79) for ever screening and 2.02 (95% CI=1.40, 2.90) for being up to date.
Conclusions
Both in-language print materials and LHW outreach plus print materials increased CRC screening among Chinese Americans. The combination of LHW+Print was more effective than Print alone. These findings can guide clinicians and policymakers in choosing appropriate interventions to increase CRC screening among Chinese American immigrants.
Trial registration
ClinicalTrials.gov registry number NCT00947206.
INTRODUCTION
Chinese Americans constitute the largest group of Asian Americans, the fastest growing U.S. racial population.1 Approximately 70% of the 3.6 million Chinese Americans are immigrants with 46% being limited English proficient (LEP).2 With an incidence rate similar to non-Hispanic whites, colorectal cancer (CRC) is the second most common cancer among Chinese Americans.3 Asian American immigrants have a higher risk of CRC compared with those in Asia.4 Although 5-year survival rates are >90% if diagnosed at a local stage,5 only 40% of CRC cases among Chinese Americans are diagnosed early.3
Screening for CRC reduces mortality6–8 and is cost effective, making its underutilization an important priority.9 The U.S. Preventive Services Task Force recommends screening with fecal occult blood test (FOBT) annually, sigmoidoscopy every 5 years, or colonoscopy every 10 years for average-risk individuals aged 50–75 years.10 Compared with non-Hispanic whites, Chinese Americans were less likely to have ever been screened11 or be up to date.12 There have been few RCTs of interventions to increase CRC screening among Asian Americans and no comparative effectiveness trials for Chinese Americans.13–19
Cancer screening interventions targeting Asian Americans need to address language and cultural beliefs.20 Lay health workers (LHWs), or community health workers, have been employed worldwide to promote healthy behaviors.21,22 Their efficacy in promoting cervical and breast cancer screening23,24 among Asian Americans25 suggests that LHWs might be efficacious for CRC screening. This research team did find LHW efficacy in promoting CRC screening in a study with Vietnamese Americans who were never screened17 and a pilot study with never-screened Chinese Americans.26 The present article reports results from an RCT comparing the efficacy of LHW plus print materials to print materials alone in promoting CRC screening among Chinese Americans who were either never screened or not up to date for CRC screening.
METHODS
Study Design
A cluster RCT (ClinicalTrials.gov #NCT00947206) design with a 1:1 allocation ratio was employed to test the efficacy of two LHW outreach sessions and two follow-up telephone calls combined with a brochure (LHW+Print) compared with a brochure alone (Print). Using a community-based participatory research approach, researchers at the University of California, San Francisco and San Francisco State University collaborated with the NICOS Chinese Health Coalition, a community-based organization. All three organizations participated in developing, implementing, and analyzing the pilot study26; obtaining grant funding; conducting the RCT (2010–2014); and analyzing and interpreting the results (2014–2015). The University of California, San Francisco and San Francisco State University IRBs approved all protocols and instruments.
Eligibility criteria for LHWs were: age ≥35 years; self-identifying as Chinese/Chinese Americans; speaking English, Cantonese, or Mandarin; and residing in San Francisco with intention to stay for 1 year. Recruitment involved press releases to Chinese-language newspapers, radio, and TV and distribution of fliers to community organizations. Ninety-five applicants were screened by telephone and in-person interview and 58 were selected (median age, 50 years; 79% female). Each LHW received a stipend of $1,000 for 45–50 hours of training, participant recruitment, and intervention delivery over 12 months. Given the skills development required for this work and the high cost of living in San Francisco, the compensation rate of approximately $20 per hour after accounting for expenses such as telephone and transportation was reasonable for each LHW’s research assistance work.
All LHWs first received a 4-hour training session about the project goals, their roles, how to recruit and retain participants, and concepts such as randomization. After they had recruited participants as described below, LHWs randomized to the LHW+Print arm received 12 more hours of training about CRC over 2 days. The training centered around a flipchart, which was made out of hard cardboard, with the side facing participants containing culturally appropriate graphics with simple text, and the other side facing the LHW with talking points. To train LHWs, bilingual trainers used the flipchart sections to model small group teaching. After each section, LHWs practiced delivering that section using the flipchart to one another in a small group. A trainer observed and gave feedback on each LHW’s delivery style and content of the presentation. Thus, each LHW received CRC information three times. They learned how to use an FOBT kit via a video and props and were given one to try at home. The LHWs visited an endoscopy suite where a gastroenterologist showed equipment and described CRC screening procedures. LHWs were also trained on how to conduct telephone calls using a one-page guide to assess participants’ “stage of change”27,28 for screening, address barriers, and provide motivation. Approximately 1 month after the LHWs started intervention delivery, a 90-minute booster training was conducted to discuss problems, brainstorm solutions, maintain camaraderie, and reinforce knowledge.
Participants’ eligibility criteria were: age 50–75 years; self-identifying as Chinese/Chinese American; speaking English, Cantonese, or Mandarin; residing in San Francisco with intention to stay for 6 months; no personal history of CRC; and no other participants in the same household. Participants were eligible regardless of their prior CRC screening status (i.e., both never screened or ever screened were eligible) because this enabled participants with different screening experiences to influence screening behaviors of others in their group. LHWs recruited participants from their social network through telephone calls and face-to-face encounters using sample scripts that included a description of the study as learning how best to teach Chinese Americans about topics such as CRC prevention and nutrition and physical activity. LHWs were encouraged to recruit equal numbers of participants who had and had never been screened to test the effect of the interventions on first screening and being up to date. The NICOS coordinator reviewed each LHW’s list of potentially eligible participants to ensure that sufficient eligibility information had been collected. Participants received $20 after completing the pre-intervention survey and $30 after the post-intervention survey 6 months later, reasonable compensation for the amount of time spent on the surveys (approximately 20–30 minutes each).
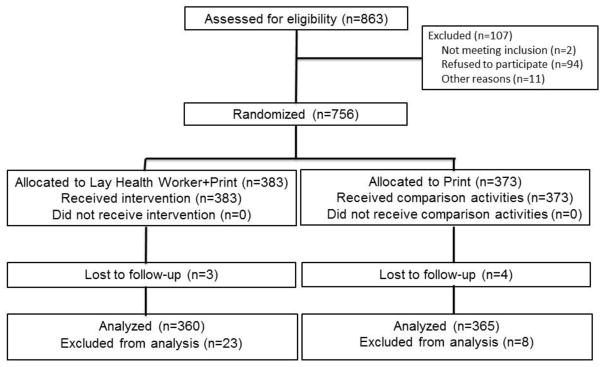
The LHWs and participants were recruited in four waves (time periods) between August 2010 and September 2013. Each LHW participated in only one wave. Within each wave, LHWs were stratified by sex and then randomly assigned to the study arms. The biostatistician used SAS, version 9.3 to randomize the LHWs 1:1 to the LHW+Print or Print group in blocks of variable size. Participants were cluster randomized along with their LHW. Research staff and LHWs learned study arm assignments only after the LHW completed participant recruitment. LHWs submitted 863 participants for eligibility verification (Figure 1). Among 861 eligible participants, 94 (10.9%) refused. On average, each LHW recruited 12 (SD=1.9; range, 4–15) participants, for a total of 756, all of whom received the assigned intervention. Only seven (0.9%) were lost to post-intervention assessment but were included in intention-to-treat analyses. Another 31 were excluded from analyses because their age as reported in the pre-intervention survey (after enrollment and randomization) did not meet eligibility.
Figure 1.
CONSORT diagram.
The interventions were developed based on prior experience with LHW interventions17,23,24,26 and integrating principles from the Transtheoretic Model.27,28 The materials included a training manual in Chinese and English, a bilingual brochure and flipchart, a telephone call guide, and a one-page guide showing where to obtain free or low-cost CRC screening and how to get there. All materials were written at a fifth grade reading level. A community advisory board reviewed the materials for cultural and linguistic appropriateness. The materials were finalized after input from focus groups of community members.
For the two LHW sessions, participants met in small groups at the home of the LHW or a participant or NICOS’ office. At the first session, the LHW delivered information from the flipchart as described earlier. The flipchart contained information about CRC prevalence, causes and prevention, including screening methods. It emphasized the importance of screening for Chinese Americans and ways to address barriers to screening. The LHW also handed out the CRC brochure, which discussed CRC prevalence among Chinese Americans and how to prevent CRC, with emphasis on screening tests, particularly the FOBT/fecal immunochemical test. The LHW answered questions whenever possible. About 3–4 weeks later, the LHW called each participant to assess their “stage of change,”27,28 address barriers, and remind about the next session. The LHW conducted the second session approximately 2 months after the first to review information, identify barriers to screening, and provide motivation and encouragement (from both the LHW and other participants) to get screening. About 3–4 weeks later, the LHW made the second follow-up telephone call, addressing similar issues. The two sessions and two calls were completed within approximately 4 months.
The LHWs received training on recruitment and retention. For attention control and to meet the community-based participatory research principle that control groups should benefit, their participants received: two in-language lectures on nutrition and physical activity delivered by a health educator at a community site, two LHW telephone calls after each lecture to ask participants about their impressions and recall of the lecture materials and to remind them about activities, and the same CRC brochure at the second lecture. After completion of participants’ post-intervention surveys, the Print group LHWs received a condensed version of the CRC training and were encouraged to deliver the information to their participants.
The pre-intervention survey was self-administered in written Chinese or English immediately before the first session or lecture. About 6 months later, the post-intervention surveys were administered individually in large group gatherings at a community site. The surveys were developed in English, translated to Chinese, and cognitively tested to ensure cultural appropriateness and readability.
Measures
The pre-intervention survey contained questions about age, sex, birthplace, educational attainment, spoken English proficiency, health insurance status, years in the U.S., marital status, self-rated health, employment status, height, weight, comorbidities, household size, annual household income, and visits with a healthcare provider in the last 12 months. Both surveys assessed knowledge about CRC (having heard of CRC or polyps), screening (ever heard of FOBT, sigmoidoscopy, or colonoscopy), initiation (age 50 years) and frequency (FOBT every year, sigmoidoscopy every 5 years, colonoscopy every 10 years), and intention to obtain screening. The behavior outcomes were self-reports of ever having had FOBT, sigmoidoscopy, or colonoscopy (and, if so, when), with the primary outcomes of ever having had any CRC screening and being up to date for CRC screening.
A sample size of 290 participants in each study arm was required to detect the difference between an increase of 0.25 in the intervention group and 0.10 in the control group in the proportion ever screened for CRC with 80% power at the 0.05 level (two-sided), assuming 12 participants per LHW, an intra-cluster correlation of 0.05, and 5% loss to follow-up, based on previous experience. The sample size was adjusted to account for possible attrition of LHWs and higher than expected baseline screening rates.
Statistical Analysis
The statistical analysis was performed from 2014 to 2015. Means and SDs were computed for numeric frequencies and percentages for categorical variables. The study arms were compared with respect to sociodemographic characteristics (Table 1) and pre–post changes in knowledge, screening behavior, and screening intention (Table 2), using generalized estimating equations to account for clustering of participants by LHW. Multivariable logistic regressions were used to estimate ORs and 95% CIs for intervention effects on behavior (ever receiving and being up to date for CRC screening) (Table 3), using generalized estimating equations to account for within-LHW clustering. As covariates, study wave was included to adjust for any potential impact related to time of study enrollment and sociodemographic characteristics, self-reported health status, and healthcare access variables that were found associated with CRC screening status in previous research. Analyses were conducted on an intention-to-treat basis, with pre-intervention values carried forward for dropouts. Data were analyzed using SAS, version 9.3, and statistical significance was assessed at the 0.05 level (two-sided).
Table 1.
Sociodemographics and Health Characteristics of Participants by Study Arm at Enrollment, N=725
| Characteristics | Total | Lay health worker + print n=360 | Print n=365 | p-valuea |
|---|---|---|---|---|
| Age, mean (years) + SD | 62.2 + 6.9 | 62.8 + 6.8 | 61.6 + 7.0 | 0.11 |
| Female, % | 81.1 | 83.1 | 79.2 | 0.30 |
| Married, % | 73.9 | 70.8 | 77.0 | 0.12 |
| Spoken English proficiency, % | 0.58 | |||
| Fluent like a native speaker | 1.8 | 2.2 | 1.4 | |
| Well | 2.5 | 2.2 | 2.8 | |
| So-so | 28.5 | 27.5 | 29.5 | |
| Poor | 38.9 | 36.9 | 40.8 | |
| Not at all | 28.4 | 31.1 | 25.6 | |
| Education, % | 0.70 | |||
| <high school diploma | 70.5 | 71.4 | 69.7 | |
| >high school diploma | 29.5 | 28.6 | 30.3 | |
| Employment, % | 0.10 | |||
| Employed | 27.2 | 22.5 | 31.8 | |
| Retired | 34.1 | 38.3 | 29.9 | |
| Other b | 38.8 | 39.2 | 38.4 | |
| Household income, % | 0.44 | |||
| Less than $5,000 | 13.2 | 12.1 | 14.3 | |
| $5,000 to <$10,000 | 18.7 | 17.7 | 19.7 | |
| $10,000 to <$20,000 | 27.3 | 28.4 | 26.3 | |
| $20,000 to <$30,000 | 9.7 | 8.4 | 11.0 | |
| $30,000 to <$40,000 | 6.0 | 5.1 | 6.9 | |
| $40,000 to <$50,000 | 2.8 | 2.5 | 3.0 | |
| $50,000 or more | 3.9 | 3.1 | 4.7 | |
| Don’t know | 18.5 | 22.8 | 14.3 | |
| Health status, % | 0.89 | |||
| Excellent | 1.8 | 1.4 | 2.2 | |
| Very good | 5.7 | 6.1 | 5.2 | |
| Good | 27.6 | 27.2 | 27.9 | |
| Fair | 57.5 | 58.9 | 56.2 | |
| Poor | 7.4 | 6.4 | 8.5 | |
| Has health insurance | 91.9 | 92.5 | 91.5 | 0.617 |
| Has regular place for health care | 89.6 | 89.4 | 89.9 | 0.86 |
| Has a primary care doctor | 88.6 | 88.6 | 88.7 | 0.97 |
| Saw a medical provider in last 12 months | 80.3 | 80.8 | 79.7 | 0.70 |
p-values accounted for lay health worker cluster.
“Other” employment category includes unemployed, homemaker, students, and otherwise unspecified.
Table 2.
Colorectal Cancer Knowledge, Behavior, and Intention from Pre- and Post-Intervention by Study Arm (N=725)
| Variable | Lay health worker + print | Pre-post differences between arms p-valuea |
|||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Pre-intervention % | Post-intervention % | p- valuea | Pre-intervention % | Post-intervention % | p- valuea | ||
| Knowledge | |||||||
| Ever heard of colorectal cancer | 54.2 | 86.7 | <0.0001 | 51.2 | 69.3 | <0.0001 | 0.001 |
| Ever heard of colorectal polyp | 56.9 | 88.8 | <0.0001 | 55.3 | 75.6 | <0.0001 | 0.0004 |
| Ever heard of FOBT | 59.2 | 84.7 | <0.0001 | 62.2 | 68.2 | 0.048 | <0.0001 |
| Ever heard of sigmoidoscopy or colonoscopy | 68.6 | 92.8 | <0.0001 | 67.1 | 78.4 | <0.0001 | <0.001 |
| Heard of any CRC screening test | 79.7 | 96.9 | <0.0001 | 79.7 | 88.2 | <0.0001 | 0.0004 |
| Screening starts at age 50 | 40.0 | 58.6 | <0.0001 | 48.5 | 50.1 | 0.622 | 0.0004 |
| FOBT should be done every year | 38.6 | 67.2 | <0.0001 | 32.9 | 43.3 | 0.001 | 0.001 |
| Sigmoidoscopy should be done every 5 years | 25.3 | 55.0 | <0.0001 | 27.4 | 31.0 | 0.141 | <0.0001 |
| Colonoscopy should be done every 10 years | 7.0 | 40.0 | <0.0001 | 7.7 | 25.2 | <0.0001 | 0.046 |
| Behavior | |||||||
| Ever had FOBT | 68.6 | 82.5 | <0.0001 | 65.8 | 70.7 | 0.032 | 0.003 |
| Ever had sigmoidoscopy or colonoscopy | 40.6 | 47.2 | <0.0001 | 37.5 | 43.0 | 0.0003 | 0.625 |
| Ever had any CRC screening | 73.9 | 88.3 | <0.0001 | 72.3 | 79.5 | 0.0003 | 0.0003 |
| Up-to-date for CRC screening | 60.0 | 78.1 | <0.0001 | 58.1 | 64.1 | 0.0003 | 0.0004 |
| Intention to get screening (all participants) | |||||||
| Plan to get FOBT in next 6 months | 33.9 | 51.7 | <0.0001 | 32.0 | 34.8 | 0.392 | 0.003 |
| Plan to get sigmoid/colonoscopy in next 6 months | 14.4 | 19.7 | 0.010 | 14.8 | 14.5 | 0.896 | 0.096 |
| Plan on any CRC screening in next 6 months | 38.3 | 55.6 | <0.0001 | 36.7 | 40.0 | 0.369 | 0.004 |
| Intention to get screening (not up-to- date participants) | |||||||
| Plan to get FOBT in next 6 months | 22.9 | 41.7 | 0.015 | 23.5 | 29.4 | 0.977 | 0.061 |
| Plan to get sigmoid/colonoscopy in next 6 months | 11.1 | 17.4 | 0.072 | 15.7 | 13.1 | 0.208 | 0.028 |
| Plan on any CRC screening in next 6 months | 25.0 | 45.1 | 0.019 | 28.8 | 34.6 | 0.776 | 0.036 |
Note: Boldface indicates statistical significance (p<0.05).
Adjusted for lay health worker clusters
FOBT, fecal occult blood test; CRC, colorectal cancer
Table 3.
Multivariable Models for Intervention Effects and Other Significant Factors of Colorectal Cancer Screeninga (N=725)
| Variable | Ever had colorectal cancer screening | Up-to-date for colorectal cancer screening |
|---|---|---|
|
| ||
| AOR (95% CI) | ||
| Intervention effect for lay health worker+print vs. print | 1.94 (1.34, 2.79) | 2.02 (1.40, 2.90) |
| Post- versus pre-intervention effect for lay health worker+print | 3.01(2.31, 3.91) | 2.69 (1.95, 3.72) |
| Post- versus pre-intervention effect for print | 1.56(1.19, 2.03) | 1.34 (1.11, 1.60) |
| Residence in U.S. >10 years (ref <10 years) | 1.65 (1.11, 2.46) | 1.37 (0.94, 2.00) |
| Fair/poor general health (ref. excellent/very good/good health) | 1.52 (1.07, 2.15) | 1.29 (0.97, 1.73) |
| Have a regular place for healthcare (ref. none) | 1.81 (1.01, 3.25) | 1.81 (0.99, 3.29) |
| Have a primary care doctor (ref. none) | 2.64 (1.42, 4.92) | 2.66 (1.47, 4.83) |
| Have health insurance (ref. none or don’t know) | 2.51 (1.34, 4.68) | 2.60 (1.37, 4.94) |
Models are intention-to-treat and adjusted for lay health worker cluster, wave of recruitment, participant age, sex, education, income, marital status, English fluency, and employment.
RESULTS
Table 1 shows the pre-intervention sociodemographic and health characteristics of the 725 participants. The average age was 62.2 (SD 6.9) years, with 81.1% women and 73.9% married. Almost all (99.4%) were foreign born. The average length of U.S. residency was 17.2 (SD 12.3) years, and 95.8% spoke English less than well. Most (70.5%) had not completed high school, and 59.2% had annual household incomes <$20,000. Most had health insurance (91.9%), a regular place for healthcare (89.6%), a primary care doctor (88.6%), and a doctor visit the last 12 months (80.3%). Only 6.1% reported a family history of CRC. There were no statistically significant differences between the LHW+Print and Print participants.
Table 2 shows the intention-to-treat changes in knowledge, behavior, and intention from baseline to post-intervention by group assignment. About half of each group had heard of CRC and polyps at baseline. At post-intervention, the LHW+Print group had an increase in awareness of CRC (54.2% to 86.7%) and polyps (56.9% to 88.8%) (p<0.0001); the Print group had increases as well (51.2% to 69.3% and 55.3% to 75.6%, respectively) (p<0.0001). Similarly, the LHW+Print group had increases in having heard of FOBT (59.2% to 84.7%), sigmoidoscopy or colonoscopy (68.6% to 92.8%), and any CRC screening test (79.7% to 96.9%) (all p<0.0001), as did the Print group (62.2% to 68.2%, p=0.048; 67.1% to 78.4%, p<0.0001; and 79.7% to 88.2%, p<0.0001, respectively). Knowledge that CRC screening should start at age 50 years increased significantly in the LHW+Print group (40.0% to 58.6%, p<0.0001) but not the Print group (48.5% to 50.1%, p=0.622). Knowledge of screening frequency increased in the LHW+Print group for FOBT (38.6% to 67.2%), sigmoidoscopy (25.3% to 55.0%), and colonoscopy (7.0% to 40.0%) (all p<0.0001). The Print group had increases in knowledge of frequency for FOBT (32.9% to 43.3%, p=0.001) and colonoscopy (7.7% to 25.2%, p<0.0001). Pre- to post-intervention increases were significantly greater in the LHW+Print group than in the Print group for all nine knowledge measures.
The LHW+Print group reported increases in ever having had FOBT (68.6% to 82.5%), sigmoidoscopy or colonoscopy (40.6% to 47.2%), or any CRC screening (73.9% to 88.3%) (all p<0.0001). The Print group reported smaller but still significant increases in ever having had FOBT (65.8% to 70.7%, p=0.032), sigmoidoscopy or colonoscopy (37.5% to 43.0%, p=0.0003), or any CRC screening (72.3% to 79.5%, p=0.0003). Increases in FOBT receipt (p=0.003) and any CRC screening (p=0.0003) were significantly greater in the LHW+Print arm than the Print arm. Being up to date for CRC screening also increased significantly in the LHW+Print group (60.0% to 78.1%, p<0.0001), less so in the Print comparison group (58.1% to 64.1%, p=0.0003), with the difference between changes being significant (p=0.0004). The intra-cluster correlation for ever screening was 0.025 and for being up to date with screening was 0.035.
In the LHW+Print arm, intention to get any CRC screening increased significantly among all participants (38.3% to 55.6%, p<0.0001) and among those who were not up to date (25.0% to 45.1%, p=0.019). Screening intention did not change significantly in the Print alone arm.
Table 3 shows multivariable analyses based on intention to treat and adjusted for LHW cluster. For the outcome of reporting ever having had CRC screening, the LHW+Print intervention group had a post- versus pre-intervention AOR of 3.01 (95% CI=2.31, 3.91) whereas the Print comparison group had an OR of 1.56 (95% CI=1.19, 2.03). The intervention effect for LHW+Print group versus Print group had an OR of 1.94 (95% CI=1.34, 2.79).
For the outcome of reporting being up to date for CRC screening at post- versus pre-intervention, the LHW+Print group had an OR of 2.69 (95% CI=1.95, 3.72) whereas the Print group had an OR of 1.34 (95% CI=1.11, 1.60). The intervention effect for LHW+Print group versus Print group had an OR of 2.02 (95% CI=1.40, 2.90).
Other factors associated with higher odds of ever having received CRC screening included: having lived in the U.S. for at least 10 years (OR=1.65, 95% CI=1.11, 2.46), having fair or poor general health (OR=1.52, 95% CI=1.07, 2.15), and having a regular place for health care (OR=1.81, 95% CI=1.01, 3.25). Having a primary care doctor was associated with both ever having received CRC screening (OR=2.64, 95% CI=1.42, 4.92) and being up to date (OR=2.66, 95% CI=1.47, 4.83). Having health insurance was also associated with ever screening (OR=2.51, 95% CI=1.34, 4.68) and being up to date (OR=2.60, 95% CI=1.37, 4.94).
DISCUSSION
To this team’s knowledge, this is the first community-based RCT of CRC screening promotion among Chinese Americans and one of the first comparative effectiveness studies of CRC screening promotion among Asian Americans.15–17 It is also the first RCT for CRC screening promotion among Asian Americans that included those who had had CRC screening but were not up to date, important as the benefits of screening depend on getting rescreened regularly. Both the LHW+Print and Print groups had significant increases in first CRC screening and being up to date, with LHW+Print being superior to Print only, with intervention effects ORs being 1.94 for ever screening and 2.02 for being up to date (Table 3).
At pre-intervention, knowledge about CRC and its screening was low, which underscores the need for outreach. The Print group had small increases in knowledge. Because this study did not include a “no intervention” group, these changes could be due to the in-language brochure, repeated surveys, secular trends, or a combination of these factors. The LHW+Print group had moderate to large increases in knowledge, likely reflecting the impact of the number of times CRC information was delivered, its oral delivery by the LHW, and the relationships between the participants and LHWs.
At 6-month post-intervention, the LHW+Print group reported moderate increases of 14.4% for ever screening and 18.1% for being up to date, and the Print group reported modest but statistically significant increases of 7.2% and 6.0%, respectively. The LHW+Print effect was smaller than that of a more intensive clinic-based intervention that included a bilingual professional health educator, videos, pamphlets, and direct offering of FOBT to Chinese American patients.13 However, the LHW+Print effect is comparable to other clinic-based interventions to increase CRC screening among disadvantaged populations, such as the direct offering of FOBT kits to patients getting influenza vaccines in clinics with diverse patient populations (13% became up to date)18 and to low-income Chinese American patients attending a Chinese-focused health center (14% became up to date),19 as well as a study of direct offering of FOBT kits combined with brochure (8.7% became up to date) or telephone counseling (17.9% became up to date) to Vietnamese American patients in a safety net system.15 The current LHW+Print intervention effect is slightly smaller than that in a community-based study among Filipino Americans of a lecture delivered by a health educator combined with direct offering of FOBT kits (30% became up to date) or no FOBT kit (25% became up to date),16 but similar to the effect of a media campaign among Vietnamese Americans.29 In the only other trial of LHW outreach for CRC screening promotion in Asian Americans, this team found an intervention effect of 56% on reports of ever receiving CRC screening among Vietnamese Americans.17 The difference in intervention effect sizes of that study and this present study of Chinese Americans may be due to variations in how Chinese and Vietnamese Americans respond to LHW education or to the Vietnamese study only including participants who reported never having been screened. In support of the latter explanation, this team’s pilot study of LHW outreach among Chinese Americans who reported never having been screened also found an intervention effect of 56%.26
The LHW+Print intervention was significantly more effective than Print alone, with intervention effect ORs of 1.94 for ever screening and 2.02 for being up to date. These findings indicate that, although a bilingual brochure can increase CRC screening among Chinese American immigrants who are LEP, a more intensive intervention involving LHWs can lead to larger increases. An increase in screening intention from the LHW+Print intervention was also observed, both among all participants and among those who were not up to date; no change in screening intention was observed in those who received the Print only intervention. Though this finding may be due to survey social desirability bias, it may also indicate that brochures are not as effective as the more intensive and personal LHW intervention in persuading those who remain unscreened after learning about CRC.
In the multivariable analyses, the association between length of U.S. residence and CRC screening reinforces the need to target recent immigrants. The association of CRC screening with healthcare access (factors such as having health insurance, a regular place of care, and a primary care doctor) has been found repeatedly in studies of cancer screening among Asian Americans11,24,29,30 and emphasizes the continued need for policy changes to increase health insurance coverage and, once low-income immigrants have health insurance, to connect them to regular primary care.
Limitations
This study’s main limitation is that the outcomes of CRC screening are based on self-report, though validation studies have shown that self-reports of CRC screening are both sensitive and specific.31–33 The Chinese Americans in the study sample were primarily immigrants who had limited educational attainment, LEP, and low income; thus, the findings of the efficacy of both LHW outreach and an in-language brochure, as well as the superiority of LHW+Print over Print alone, may not be generalizable to other populations. The LHWs and participants were predominantly women, similar to LHW studies in other populations, possibly because minority women may be more willing than men to participate in health outreach and research. This may limit the generalizability of these findings to men; however, a Vietnamese American study, which had equal number of male and female LHWs and participants, found no gender difference in intervention efficacy.17 The study sample does have high rates of healthcare access, owing to changes in the healthcare delivery system in San Francisco that antedated the Affordable Care Act.
One strength of this study is the high participation (89.1%) and retention (99.1%) rates in a population often thought to be difficult to recruit for research. The high rate of LEP immigrants in this study is comparable to other studies of LHW outreach with Asian Americans. This shows the value of the social network approach utilized in LHW outreach for recruiting and retaining hard-to-reach participants. Owing to the RCT design, the issue of recruitment or selection bias from social network recruitment is not a threat to the study’s internal validity. However, it does limit the generalizability of this study’s findings to the general population or the overall population of Chinese Americans, although the screening rates in this study sample are comparable to those found in population-based studies of Asian Americans.34 Indeed, the characteristics of this study population, research participation rates, and RCT design indicate that the findings from this study have strong internal and external validity.
CONCLUSIONS
This study shows that in-language and targeted educational print materials may be effective in promoting CRC screening among Chinese American immigrants, and that the addition of LHW outreach further increases screening rates. More research should be done to understand how LHWs achieve their effectiveness and whether such programs are cost effective. Nonetheless, the findings from this RCT of two different interventions may be helpful to community organizations, clinical providers, and policymakers in deciding what interventions to use to promote CRC screening in immigrant communities. Those working with Chinese Americans in low-resource settings can download the bilingual brochure and flip chart for their patients, which are available at www.asianarch.org. LHWs can play an effective role in promoting CRC screening in Chinese Americans and other underserved populations, as demonstrated by this and other studies. Other benefits of LHW outreach extend beyond screening outcomes, including increasing the outreach capacity of underserved communities with limited access to bilingual professional health educators and clinicians.35 Sustainability of LHW interventions requires building the capacity of community-based organizations to train and manage LHWs. This could be accomplished through the Clinical and Translational Sciences Institutes, which can support local community–academic partnerships, and through the Clinical and Translational Sciences Institutes’ funder, the National Center for Advancing Translational Sciences, which can create an online infrastructure to train community-based organizations on how to conduct successful interventions. Of course, reimbursement is also needed to sustain LHW interventions, which is now possible with payment for community health workers from the Center for Medicare and Medicaid Services.
Acknowledgments
This study was supported by the National Cancer Institute (NCI) Grant R01CA138778. The NCI Center to Reduce Cancer Health Disparities through Grant 1U54153499 and the Asian American Research Center on Health provided additional support. The content is solely the responsibility of the authors and does not reflect NCI’s official views. We thank the staff of the NICOS Chinese Health Coalition (Michael Liao, Corina Liew, Christina Nip, and Ying Wang) and the Vietnamese Community Health Promotion Project (Hy Lam, Ching Wong) for developing the materials and carrying out data collection, and the San Francisco Asian American Network for Cancer Awareness, Research, and Training (including its Chairs, Drs. Edward Chow and Angela Sun) for providing community oversight and input into intervention development intervention and interpretation of the results. We also thank the community’s unsung heroes, the Lay Health Workers, for their collaborative partnership, dedication, and commitment to enhancing the community’s health and wellness.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Hoeffel EM, Rastogi S, Kim MO, Shahid HT. The Asian Population: 2010. Washington, DC: U.S. Census Bureau; 2012. [Google Scholar]
- 2.U.S. Census Bureau. [Accessed November 15, 2015];2011–2013 American Community Survey 3-Year Estimates. 2014 http://factfinder.census.gov/bkmk/table/1.0/en/ACS/13_3YR/S0201/0100000US/popgroup~016.
- 3.Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;19(3):227–256. doi: 10.1007/s10552-007-9088-3. http://dx.doi.org/10.1007/s10552-007-9088-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Le Marchand L, Wilkens LR, Kolonel LN, Hankin JH, Lyu LC. Associations of sedentary lifestyle, obesity, smoking, alcohol use, and diabetes with the risk of colorectal cancer. Cancer Res. 1997;57(21):4787–4794. [PubMed] [Google Scholar]
- 5.Vernon SW. Participation in colorectal cancer screening: a review. J Natl Cancer Inst. 1997;89(19):1406–1422. doi: 10.1093/jnci/89.19.1406. http://dx.doi.org/10.1093/jnci/89.19.1406. [DOI] [PubMed] [Google Scholar]
- 6.Selby JV, Friedman GD, Quesenberry CP, Jr, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326(10):653–657. doi: 10.1056/NEJM199203053261001. http://dx.doi.org/10.1056/NEJM199203053261001. [DOI] [PubMed] [Google Scholar]
- 7.Mandel JS, Bond JH, Church TR, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328(19):1365–1371. doi: 10.1056/NEJM199305133281901. http://dx.doi.org/10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 8.Hardcastle JD, Chamberlain JO, Robinson MH, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348(9040):1472–1477. doi: 10.1016/S0140-6736(96)03386-7. http://dx.doi.org/10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 9.Maciosek MV, Coffield AB, Edwards NM, Flottemesch TJ, Goodman MJ, Solberg LI. Priorities among effective clinical preventive services: results of a systematic review and analysis. Am J Prev Med. 2006;31(1):52–61. doi: 10.1016/j.amepre.2006.03.012. http://dx.doi.org/10.1016/j.amepre.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Screening for colorectal cancer: U. S. Preventive services task force recommendation. Ann Intern Med. 2008;149(9):I44. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 11.Wong ST, Gildengorin G, Nguyen T, Mock J. Disparities in colorectal cancer screening rates among Asian Americans and non-Latino whites. Cancer. 2005;104(12 Suppl):2940–2947. doi: 10.1002/cncr.21521. http://dx.doi.org/10.1002/cncr.21521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Homayoon B, Shahidi NC, Cheung WY. Impact of asian ethnicity on colorectal cancer screening: a population-based analysis. Am J Clin Oncol. 2013;36(2):167–173. doi: 10.1097/COC.0b013e3182439068. http://dx.doi.org/10.1097/COC.0b013e3182439068. [DOI] [PubMed] [Google Scholar]
- 13.Tu SP, Taylor V, Yasui Y, et al. Promoting culturally appropriate colorectal cancer screening through a health educator: a randomized controlled trial. Cancer. 2006;107(5):959–966. doi: 10.1002/cncr.22091. http://dx.doi.org/10.1002/cncr.22091. [DOI] [PubMed] [Google Scholar]
- 14.Inadomi JM, Vijan S, Janz NK, et al. Adherence to colorectal cancer screening: a randomized clinical trial of competing strategies. Arch Intern Med. 2012;172(7):575–582. doi: 10.1001/archinternmed.2012.332. http://dx.doi.org/10.1001/archinternmed.2012.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh JM, Salazar R, Nguyen TT, et al. Healthy colon, healthy life: a novel colorectal cancer screening intervention. Am J Prev Med. 2010;39(1):1–14. doi: 10.1016/j.amepre.2010.02.020. http://dx.doi.org/10.1016/j.amepre.2010.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maxwell AE, Bastani R, Danao LL, Antonio C, Garcia GM, Crespi CM. Results of a community-based randomized trial to increase colorectal cancer screening among Filipino Americans. Am J Public Health. 2010;100(11):2228–2234. doi: 10.2105/AJPH.2009.176230. http://dx.doi.org/10.2105/AJPH.2009.176230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen BH, Stewart SL, Nguyen TT, Bui-Tong N, McPhee SJ. Effectiveness of Lay Health Worker Outreach in Reducing Disparities in Colorectal Cancer Screening in Vietnamese Americans. Am J Public Health. 2015;105(10):2083–2089. doi: 10.2105/AJPH.2015.302713. http://dx.doi.org/10.2105/AJPH.2015.302713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Potter MB, Walsh JM, Yu TM, Gildengorin G, Green LW, McPhee SJ. The effectiveness of the FLU-FOBT program in primary care a randomized trial. Am J Prev Med. 2011;41(1):9–16. doi: 10.1016/j.amepre.2011.03.011. http://dx.doi.org/10.1016/j.amepre.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 19.Potter MB, Yu TM, Gildengorin G, et al. Adaptation of the FLU-FOBT Program for a primary care clinic serving a low-income Chinese American community: new evidence of effectiveness. J Health Care Poor Underserved. 2011;22(1):284–295. doi: 10.1353/hpu.2011.0030. [DOI] [PubMed] [Google Scholar]
- 20.Tu SP, Yip MP, Chun A, Choe J, Bastani R, Taylor V. Development of intervention materials for individuals with limited English proficiency: lessons learned from “Colorectal Cancer Screening in Chinese Americans”. Med Care. 2008;46(9 Suppl 1):S51–61. doi: 10.1097/MLR.0b013e31817f0cde. http://dx.doi.org/10.1097/MLR.0b013e31817f0cde. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO. Community health workers: working document for the WHO study group. Geneva, Switzerland: WHO; 1987. [Google Scholar]
- 22.Swider SM. Outcome effectiveness of community health workers: an integrative literature review. Public Health Nurs. 2002;19(1):11–20. doi: 10.1046/j.1525-1446.2002.19003.x. http://dx.doi.org/10.1046/j.1525-1446.2002.19003.x. [DOI] [PubMed] [Google Scholar]
- 23.Mock J, McPhee SJ, Nguyen T, et al. Effective lay health worker outreach and media-based education for promoting cervical cancer screening among Vietnamese American women. Am J Public Health. 2007;97(9):1693–1700. doi: 10.2105/AJPH.2006.086470. http://dx.doi.org/10.2105/AJPH.2006.086470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nguyen TT, Le G, Nguyen T, et al. Breast cancer screening among Vietnamese Americans: a randomized controlled trial of lay health worker outreach. Am J Prev Med. 2009;37(4):306–313. doi: 10.1016/j.amepre.2009.06.009. http://dx.doi.org/10.1016/j.amepre.2009.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Engelstad LP, Stewart S, Otero-Sabogal R, Leung MS, Davis PI, Pasick RJ. The effectiveness of a community outreach intervention to improve follow-up among underserved women at highest risk for cervical cancer. Prev Med. 2005;41(3–4):741–748. doi: 10.1016/j.ypmed.2005.06.003. http://dx.doi.org/10.1016/j.ypmed.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen TT, Love MB, Liang C, et al. A pilot study of lay health worker outreach and colorectal cancer screening among Chinese Americans. J Cancer Educ. 2010;25(3):405–412. doi: 10.1007/s13187-010-0064-3. http://dx.doi.org/10.1007/s13187-010-0064-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prochaska JO. A theorectical model of behavior change: learning from mistakes with majority populations. NIH; 1992. [Google Scholar]
- 28.Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. http://dx.doi.org/10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 29.Nguyen BH, McPhee SJ, Stewart SL, Doan HT. Effectiveness of a controlled trial to promote colorectal cancer screening in Vietnamese Americans. Am J Public Health. 2010;100(5):870–876. doi: 10.2105/AJPH.2009.166231. http://dx.doi.org/10.2105/AJPH.2009.166231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nguyen TT, McPhee SJ, Gildengorin G, et al. Papanicolaou testing among Vietnamese Americans: results of a multifaceted intervention. Am J Prev Med. 2006;31(1):1–9. doi: 10.1016/j.amepre.2006.03.005. http://dx.doi.org/10.1016/j.amepre.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 31.Baier M, Calonge N, Cutter G, et al. Validity of self-reported colorectal cancer screening behavior. Cancer Epidemiol Biomarkers Prev. 2000;9(2):229–232. [PubMed] [Google Scholar]
- 32.Khoja S, McGregor SE, Hilsden RJ. Validation of self-reported history of colorectal cancer screening. Can Fam Physician. 2007;53(7):1192–1197. [PMC free article] [PubMed] [Google Scholar]
- 33.Jones RM, Mongin SJ, Lazovich D, Church TR, Yeazel MW. Validity of four self-reported colorectal cancer screening modalities in a general population: differences over time and by intervention assignment. Cancer Epidemiol Biomarkers Prev. 2008;17(4):777–784. doi: 10.1158/1055-9965.EPI-07-0441. http://dx.doi.org/10.1158/1055-9965.EPI-07-0441. [DOI] [PubMed] [Google Scholar]
- 34.Liss DT, Baker DW. Understanding current racial/ethnic disparities in colorectal cancer screening in the United States: the contribution of socioeconomic status and access to care. Am J Prev Med. 2014;46(3):228–236. doi: 10.1016/j.amepre.2013.10.023. http://dx.doi.org/10.1016/j.amepre.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 35.Nguyen TT, McPhee SJ, Bui-Tong N, et al. Community-based participatory research increases cervical cancer screening among Vietnamese-Americans. J Health Care Poor Underserved. 2006;17(2 Suppl):31–54. doi: 10.1353/hpu.2006.0091. http://dx.doi.org/10.1353/hpu.2006.0078. [DOI] [PubMed] [Google Scholar]