Abstract
Background
Monitoring trends in cardiovascular events can provide key insights into the effectiveness of prevention efforts. Leveraging data from electronic health records provides a unique opportunity to examine contemporary, community-based trends in acute myocardial infarction hospitalizations.
Methods
We examined trends in hospitalized acute myocardial infarction incidence among adults aged ≥25 years in 13 U.S. health plans in the Cardiovascular Research Network. The first hospitalization per member for acute myocardial infarction overall and for ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction was identified by ICD-9 primary discharge codes in each calendar year from 2000 through 2008. Age- and sex-adjusted incidence was calculated per 100,000 person-years using direct adjustment with 2000 U.S. census data.
Results
Between 2000 and 2008, we identified 125,435 acute myocardial infarction hospitalizations. Age- and sex-adjusted incidence rates (per 100,000 person-years) of acute myocardial infarction declined an average 3.8%/year from 230.5 in 2000 to 168.6 in 2008. Incidence of ST-segment elevation myocardial infarction declined 8.7%/year from 104.3 in 2000 to 51.7 in 2008 while incidence of non-ST-segment elevation myocardial infarction increased from 126.1 to 129.4 between 2000 and 2004 and then declined thereafter to 116.8 in 2008. Age- and sex-specific incidence rates generally reflected similar patterns, with relatively larger declines in ST-segment elevation myocardial infarction rates in women compared with men. As compared to 2000, the age-adjusted incidence of ST-segment elevation myocardial infarction in 2008 was 48% lower among men and 61% lower among women.
Conclusions and Relevance
Among a large, diverse, multicenter community-based insured population, there were significant declines in incidence of hospitalized acute myocardial infarction and the more serious ST-segment elevation myocardial infarctions between 2000 and 2008. Declines in ST-segment elevation myocardial infarctions were most pronounced among women. While ecologic in nature, these secular declines likely reflect, at least in part, results of improvement in primary prevention efforts.
Keywords: Cardiovascular disease, acute myocardial infarction, epidemiology, sex differences, trends
Although death rates from coronary heart disease have declined in recent decades, coronary heart disease is still the leading cause of death and is an important cause of morbidity in the U.S. (1). Despite the enormous burden of coronary heart disease in the U.S., the changing epidemiology of coronary heart disease is poorly understood in the absence of an integrated, comprehensive, national surveillance system for coronary heart disease, which currently does not exist (2). Recent studies measuring acute myocardial infarction in the U.S. have focused on individual communities or select populations that generally have not included younger age groups or broad socioeconomic, geographic and racial/ethnic diversity (3–6). As such, the usefulness of existing estimates of acute myocardial infarction incidence, and temporal trends, are limited in scope.
A number of prevention efforts have been implemented over recent decades including lower target levels for low density lipoprotein cholesterol and blood pressure, use of cardioprotective medications, and anti-tobacco campaigns resulting in improved control of cardiovascular disease risk factors (7–11). Together with improvements in care for patients hospitalized with acute myocardial infarction, these efforts have led to a sustained decline in mortality attributed to coronary heart disease (12–14). However, the increasing prevalence of obesity (15,16) and diabetes (17–19) during recent decades could have opposite effects on changing trends in the burden of coronary heart disease (20,21). Without comprehensive surveillance, it is difficult to determine the overall effect of these opposing forces on the burden of coronary heart disease. Such data are important to understand which preventive measures have been successful over time and more importantly, such data reveal areas that merit further investigation in order to reduce the morbidity and mortality attributable to coronary heart disease.
We examined trends (years 2000–2008) in the annual incidence of hospitalized acute myocardial infarction among 11 million adults aged ≥25 years from 13 health care delivery systems.
METHODS
Data Source
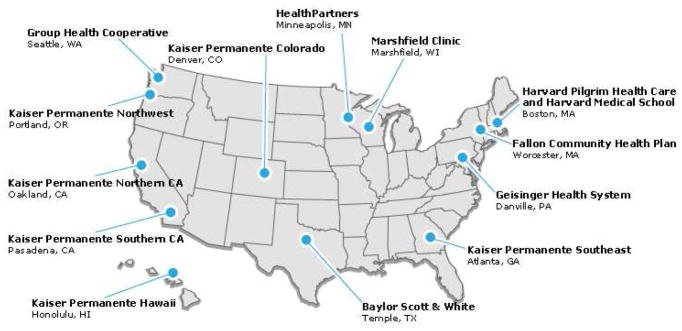
This study included data from the Cardiovascular Research Network (CVRN) Cardiovascular Disease Surveillance Study, a study that compiled a broad range of clinical and demographic electronic health record data for individuals receiving care through health care delivery systems participating in the CVRN (www.cvrn.org) who were hospitalized for acute myocardial infarction, stroke, or heart failure between 2000–2008 (Figure 1). Briefly, the CVRN was funded by the National Heart, Lung, and Blood Institute to leverage expertise, populations, and data sources from geographically and ethnically diverse health care delivery systems that participate in the Health Care Systems Research Network (www.hcsrn.org) (22). The research centers embedded within these systems compile their administrative, claims, and electronic health record data into standardized repositories. Data from 13 health care delivery systems were available and included in this analysis.
Figure 1.
Participating health care delivery systems in the Cardiovascular Research Network
Identification and Characterization of Acute Myocardial Infarction
We identified hospitalizations occurring between 1996–2008 with a primary discharge diagnosis of acute myocardial infarction based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes 410.x0 or 410.x1 from hospital-discharge records and billing claims for all members aged ≥25 years. We defined incident acute myocardial infarction events as the first hospitalization that occurred between 2000–2008 with no prior hospitalization for acute myocardial infarction during all available years of look-back. Hospitalizations for acute myocardial infarction were categorized as either ST-segment elevation myocardial infarction using ICD-9-CM codes 410.0 to 410.6 and 410.8 or non-ST-segment elevation myocardial infarction using ICD-9-CM codes 410.7 and 410.9. We assigned ICD-9-CM code 410.9 as non-ST-segment elevation myocardial infarction based on previous research (13). Individuals experiencing an incident ST-segment elevation myocardial infarction and an incident non-ST-segment elevation myocardial infarction were included separately in corresponding analyses, but only first-ever events were considered in overall acute myocardial infarction incidence. Readmissions within 7 days of a hospital discharge where the principal discharge diagnosis code of both admissions was 410.x were considered to be the same clinical event.
To determine the accuracy and consistency of diagnostic coding over time, we conducted detailed manual chart reviews consisting of 35 randomly selected acute myocardial infarction hospitalizations (15 presumed ST-segment elevation myocardial infarction, 15 presumed non-ST-segment elevation myocardial infarction, and 5 indeterminate based on discharge diagnostic codes) at each of the study sites at 3 time points 2000–2002, 2003–2006, and 2007–2009. Experienced chart abstractors used a standardized form to obtain ischemic symptoms, history of myocardial infarction, serial measures of cardiac biomarkers, and all electrocardiograms during the index hospitalization. We abstracted available cardiac biomarkers from 72 hours prior to hospital admission until discharge or death. Abstracted information was independently reviewed and adjudicated by 2 physicians using criteria from the Atherosclerosis Risk in Communities (ARIC) study that were modified by using clinical readings of the 12-lead electrocardiograms (23). Using the diagnosis assigned by the adjudication process as the gold standard, the positive predictive value was 91.2% for acute myocardial infarction, 67.8% for ST-segment elevation myocardial infarction, and 70.7% for non-ST-segment elevation myocardial infarction, with consistency across years.
Patient Characteristics
Patient demographic characteristics, relevant medical history, and clinical data were obtained from health care delivery system databases. Using previously validated approaches (24–27), we extracted information on history of cardiovascular disease and chronic lung disease, prior percutaneous coronary intervention or coronary artery bypass graft, and cardiovascular disease risk factors occurring 4 years before cohort entry. Prescription medications known to lower cardiovascular disease risk or reduce the severity of the type of clinical presentation of coronary heart disease were extracted from outpatient pharmacy records or claims data for the 30 days before the acute myocardial infarction hospitalization. Length of the hospital stay and death within 30 days of the acute myocardial infarction hospitalization were also collected.
Statistical Analysis
Patient characteristics were calculated as mean and standard deviation for continuous variables and frequency for categorical variables by year. Differences across time in continuous variables were tested using linear regression, and Cochrane-Armitage tests were used to assess trends across time in categorical variables. Incidence rates per 100,000 person-years were calculated for each year, overall and stratified by sex. Denominators were derived from health care delivery system membership composition for each year and site. Rates were directly standardized to the age and sex distribution of the 2000 U.S. census population. Standard errors and 95% confidence intervals (CIs) were estimated using the Poisson distribution. To evaluate temporal trends, we estimated average annual percent change (AAPC) and 95% CIs using log-linear Poisson models. We compared trends between men and women by including an interaction term between year and sex in the regression models. Death within 30 days was calculated using the total number of hospitalized acute myocardial infarctions as the denominator and the number of deaths as the numerator.
Seven of the 13 participating sites provided incidence data for all years of the study. Analyses were conducted including available years of data from the 13 sites and repeated including only data from the 7 sites with complete data. Results were similar, so only the overall incidence rates by study year are presented separately for both 13 sites and 7 sites; all other results are presented for only the 7 sites. These 7 sites represent 75% of the total person-time and 80% of the incident acute myocardial infarction cases from the 13 sites. Analyses were conducted using SAS software version 9.2 (SAS Institute., Cary, NC). This study was approved by the institutional review board at each participating institution.
RESULTS
Surveillance Population
A total of 125,435 patients representing 61,892,452 person-years of observation from 13 CVRN sites were hospitalized with incident acute myocardial infarction between 2000–2008 (100,599 patients and 46,630,193 person-years at the 7 sites with data for all years). Across the 13 CVRN sites, 47,400 patients (38%) presented with ST-segment elevation myocardial infarction and 78,035 (62%) with non-ST-segment elevation myocardial infarction; 64% of all acute myocardial infarction events occurred in men and 34% in members aged ≥75 years. The proportion of incident acute myocardial infarctions that were classified as ST-segment elevation myocardial infarctions decreased from 46% in 2000 to 31% in 2008.
Compared with patients hospitalized for incident acute myocardial infarction in 2000, patients hospitalized in 2008 were less likely to be white or black and more likely to have comorbid conditions (Table 1). The mean hospital stay decreased from 4.2 days in 2000 to 3.8 days in 2008. The use of cardioprotective medications (except platelet inhibitors) within 30 days before the hospitalization for acute myocardial infarction all markedly increased over time (Figure 2). Use of these cardiac medications was more prevalent among incident non-ST-segment elevation myocardial infarction cases compared with ST-segment elevation myocardial infarction cases.
Table 1.
Characteristics of Hospitalized Patients with Incident Acute Myocardial Infarction from 7 Health Care Delivery Systems in the Cardiovascular Research Network, 2000–2008
| Characteristic | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | P for trend |
|---|---|---|---|---|---|---|---|---|---|---|
| No. of patients | 11,216 | 11,507 | 11,794 | 11,650 | 11,537 | 11,326 | 10,957 | 10,500 | 10,112 | |
| Denominator | 4,810,385 | 4,984,293 | 5,146,621 | 5,163,675 | 5,133,630 | 5,228,768 | 5,332,072 | 5,397,580 | 5,433,169 | |
| Mean (SD) age, years | 67.8 (13.2) | 68.2 (13.3) | 68.0 (13.5) | 68.3 (13.6) | 68.3 (13.6) | 68.1 (13.7) | 67.9 (13.9) | 68.0 (13.7) | 68.0 (13.8) | 0.21 |
| Age group, % | ||||||||||
| 25–54 | 19.2 | 18.1 | 19.0 | 18.7 | 18.4 | 18.8 | 19.5 | 19.1 | 19.4 | 0.11 |
| 55–74 | 47.6 | 46.9 | 46.4 | 46.2 | 46.2 | 46.9 | 46.5 | 46.6 | 46.4 | 0.29 |
| ≥75 | 33.2 | 35.0 | 34.6 | 35.1 | 35.3 | 34.3 | 34.0 | 34.3 | 34.0 | 0.83 |
| Men, % | 64.0 | 63.4 | 63.9 | 63.2 | 63.2 | 63.4 | 63.8 | 63.8 | 64.4 | 0.50 |
| Race/Ethnicity, % | ||||||||||
| Asian/Pacific Islander | 5.9 | 6.3 | 6.1 | 7.0 | 8.0 | 7.3 | 8.2 | 9.1 | 9.3 | <0.0001 |
| Black/African American | 8.0 | 7.7 | 7.5 | 7.6 | 7.7 | 7.7 | 7.3 | 7.4 | 7.0 | 0.009 |
| Hispanic | 10.9 | 11.2 | 11.4 | 11.6 | 11.7 | 12.6 | 13.0 | 12.4 | 13.2 | <0.0001 |
| White | 65.6 | 64.5 | 64.0 | 62.9 | 61.4 | 60.6 | 59.1 | 58.2 | 58.4 | <0.0001 |
| Other/Unknown | 9.6 | 10.3 | 11.1 | 10.9 | 11.2 | 12.0 | 12.4 | 12.9 | 12.1 | <0.0001 |
| Mean (SD) LOS, days | 4.2 (6.3) | 4.6 (25.9) | 4.5 (13.0) | 4.1 (6.5) | 4.2 (10.7) | 4.1 (12.8) | 3.8 (7.1) | 3.8 (6.1) | 3.8 (4.7) | <0.0001 |
| Comorbid Conditions, % | ||||||||||
| Hypertension | 27.0 | 40.0 | 44.4 | 48.0 | 52.7 | 55.2 | 57.0 | 57.7 | 61.3 | <0.0001 |
| Diabetes mellitus | 24.8 | 27.7 | 27.9 | 28.6 | 29.5 | 29.0 | 29.2 | 29.7 | 29.7 | <0.0001 |
| Dyslipidemia | 27.0 | 31.2 | 34.8 | 41.6 | 46.8 | 49.6 | 52.3 | 55.6 | 57.6 | <0.0001 |
| Other Medical History, % | ||||||||||
| Angina | 5.8 | 6.2 | 6.7 | 6.3 | 6.6 | 6.5 | 5.8 | 5.3 | 4.8 | <0.0001 |
| PCI/CABG | 2.8 | 2.9 | 2.8 | 2.8 | 3.0 | 2.8 | 3.3 | 2.8 | 2.6 | 0.85 |
| Heart failure | 6.6 | 7.7 | 8.2 | 9.2 | 9.9 | 9.7 | 9.7 | 9.3 | 10.5 | <0.0001 |
| Stroke or TIA | 1.3 | 1.2 | 1.3 | 1.2 | 1.2 | 1.2 | 1.3 | 1.2 | 1.3 | 0.82 |
| PAD | 1.5 | 1.6 | 1.9 | 2.0 | 1.8 | 2.4 | 3.2 | 3.9 | 4.0 | <0.0001 |
| Chronic lung disease | 10.8 | 11.8 | 12.2 | 13.1 | 13.7 | 14.8 | 15.6 | 16.9 | 19.1 | <0.0001 |
SD = standard deviation; LOS = length of hospital stay; PCI = percutaneous coronary intervention; CABG = coronary artery bypass surgery; TIA=transient ischemic attack; PAD=peripheral arterial disease
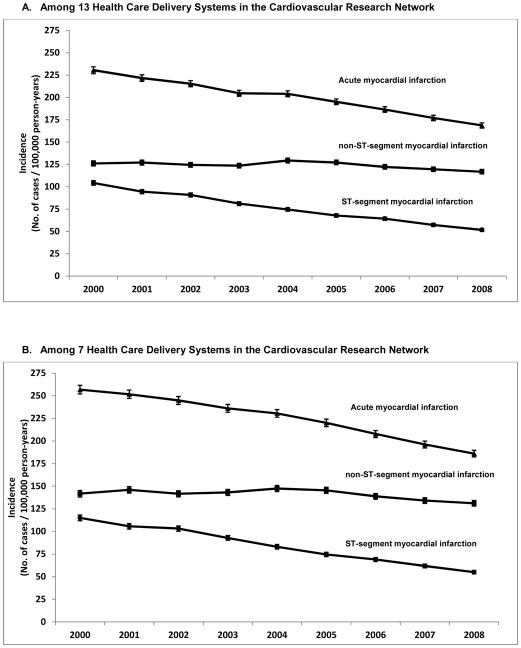
Figure 2.
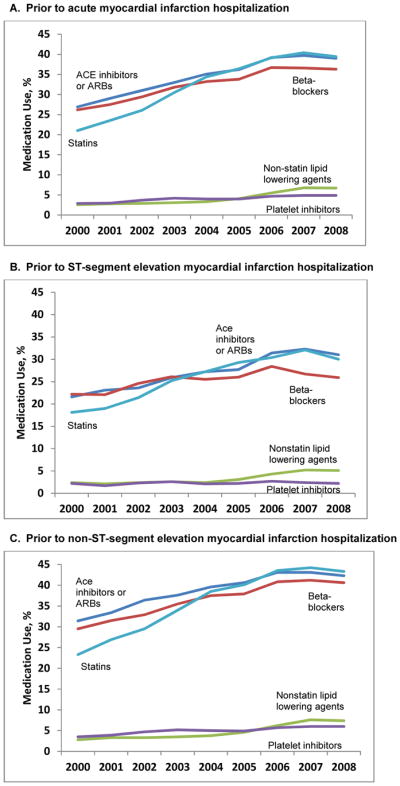
Use of outpatient medications prior to index hospitalization with acute myocardial infarction from 7 health care delivery systems in the Cardiovascular Research Network, 2000–2008
The use of medications in patients presenting with any acute myocardial infarction in Panel A, ST-segment elevation myocardial infarction in Panel B, and non-ST-segment elevation myocardial infarction in Panel C. ACE = angiotensin-converting enzyme, and ARB = angiotensin II-receptor blocker
Incidence Rates of Acute Myocardial Infarction
Age- and sex-adjusted incidence rates of acute myocardial infarction per 100,000 person-years among the 13 health care delivery systems decreased from 230.5 cases (95% CI, 226.6 to 234.3) in 2000 to 168.6 (95% CI, 165.6 to 171.5) in 2008, a 26.9% decline (Figure 3a). The AAPC of hospitalized incident acute myocardial infarction was −3.8% (95% CI, −4.0 to −3.6; P<0.001 for linear trend). Incidence of ST-segment elevation myocardial infarction decreased 50.4%, from 104.3 cases (95% CI, 101.8 to 106.9) in 2000 to 51.7 cases (95% CI, 50.1 to 53.4) in 2008 (AAPC, −8.7%; 95% CI, −9.0 to −8.3; P<0.001 for linear trend). In contrast, incidence of non-ST-segment elevation myocardial infarction increased from 126.1 cases (95% CI, 123.3 to 129.0) in 2000 to 129.4 (95% CI, 126.8 to 132.1) in 2004 before decreasing thereafter to 116.8 cases (95% CI, 114.4 to 119.3) in 2008 (AAPC, −0.9%; 95% CI −1.2 to −0.6; P<0.001 for linear trend) for a decrease of 7.4% over the 9 year period. Similar patterns were found for acute myocardial infarction and ST-segment elevation myocardial infarction when restricting analyses to the 7 sites that had data for all years with a 27.5% decrease in acute myocardial infarction, a 52.2% decrease in ST-segment elevation myocardial infarction, and a 7.5% decrease in incidence of non-ST-segment elevation myocardial infarction over the 9-year period (Figure 3b).
Figure 3.
Age- and sex-adjusted incidence of acute myocardial infarction among health care delivery systems of the Cardiovascular Research Network, 2000–2008
Panel A includes data from 13 health care delivery systems and Panel B includes data from a subset of 7 health care delivery systems with data for all years of the study (p-value for trend <0.001 for all)
 bars represent 95% confidence intervals.
bars represent 95% confidence intervals.
Statistically significant declines in incidence of hospitalized acute myocardial infarction and ST-segment elevation myocardial infarction were observed among all age groups, but the younger age group (25–54 years) had the smallest declines relative to the older age groups (Table 2). Statistically significant declines in incidence of non-ST-segment elevation myocardial infarction were only observed among those aged ≥55 years. Incidence of non-ST-segment elevation myocardial infarction increased among those aged 25–54 years.
Table 2.
Age-Specific Incidence per 100,000 person-years (95% CI) of Hospitalized Acute Myocardial Infarction from 7 Health Care Delivery Systems of the Cardiovascular Research Network, 2000–2008
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | AAPC (95% CI) |
|
|---|---|---|---|---|---|---|---|---|---|---|
| AMI | ||||||||||
| 25–54 | 65.7 (63.0–68.5) | 61.7 (59.1–64.4) | 64.9 (62.3–67.6) | 64.0 (61.3–66.7) | 63.8 (61.1–66.6) | 63.1 (60.5–65.8) | 62.5 (59.9–65.2) | 58.3 (55.8–60.9) | 56.9 (54.4–59.4) | −1.4 (−1.9, −0.8) |
| 55–74 | 445.7 (433.9–457.8) | 430.6 (419.3–442.3) | 411.1 (400.4–422.2) | 389.9 (379.7–400.5) | 377.8 (367.8–388.1) | 363.5 (353.8–373.4) | 338.4 (329.2–347.8) | 318.1 (309.3–327.1) | 299.3 (290.9–308.0) | −4.9 (−5.3, −4.6) |
| 75+ | 1132.0 (1096.2–1169.0) | 1153.1 (1118.1–1189.3) | 1108.2 (1074.7–1142.7) | 1077.8 (1045.3–1111.4) | 1053.3 (1021.4–1086.1) | 976.8 (946.6–1008.0) | 916.2 (887.3–946.1) | 877.5 (849.3–906.6) | 827.7 (800.5–855.8) | −4.2 (−4.6, −3.8) |
| STEMI | ||||||||||
| 25–54 | 36.6 (34.6–38.7) | 33.6 (31.7–35.60 | 33.9 (32.0–35.9) | 32.1 (30.3–34.1) | 30.9 (29.1–32.9) | 28.3 (26.5–30.1) | 27.0 (25.3–28.8) | 24.2 (22.6–25.9) | 23.1 (21.6–24.8) | −5.6 (−6.4, −4.8) |
| 55–74 | 211.8 (203.7– 220.2) | 190.7 (183.2–198.50 | 186.7 (179.5–194.10 | 164.0 (157.4–170.9) | 145.2 (139.0–151.6) | 134.6 (128.8–140.7) | 121.5 (116.1–127.2) | 108.9 (103.9–114.3) | 96.1 (91.4–101.1) | −9.8 (−10.3, −9.2) |
| 75+ | 402.0 (380.9–424.3) | 383.7 (363.7–404.8) | 363.0 (344.0–383.0) | 327.0 (309.3–345.7) | 279.9 (263.7–297.1) | 231.6 (217.2–247.1) | 218.7 (204.8–233.5) | 196.6 (183.5–210.6) | 163.0 (151.2–175.8) | −11.4 (−12.2, −10.6) |
| NSTEMI | ||||||||||
| 25–54 | 29.1 (27.3–31.0) | 28.1 (26.4–30.0) | 31.0 (29.2–32.9) | 31.8 (30.0–33.8) | 32.9 (31.0–34.9) | 34.9 (32.9–36.9) | 35.6 (33.6–37.6) | 34.0 (32.2–36.0) | 33.8 (31.9–35.8) | 2.5 (1.7, 3.3) |
| 55–74 | 233.9 (225.4–242.7) | 239.9 (231.5–248.6) | 224.5 (216.6–232.7) | 225.9 (218.1–234.0) | 232.6 (224.8–240.7) | 228.9 (221.2–236.8) | 216.9 (209.5–224.4) | 209.1 (202.0–216.5) | 203.2 (196.3–210.4) | −1.7 (−2.2, −1.3) |
| 75+ | 730.0 (701.4–759.9) | 769.4 (740.9–799.1) | 745.2 (717.8–773.6) | 750.9 (723.8–778.9) | 773.4 (746.1–801.6) | 745.2 (718.8–772.5) | 697.6 (672.4–723.7) | 680.9 (656.1–706.6) | 664.7 (640.3–689,8) | −1.5 (−2.0, −1.0) |
AAPC=average annual percent change; p-for trend <0.0001 for all
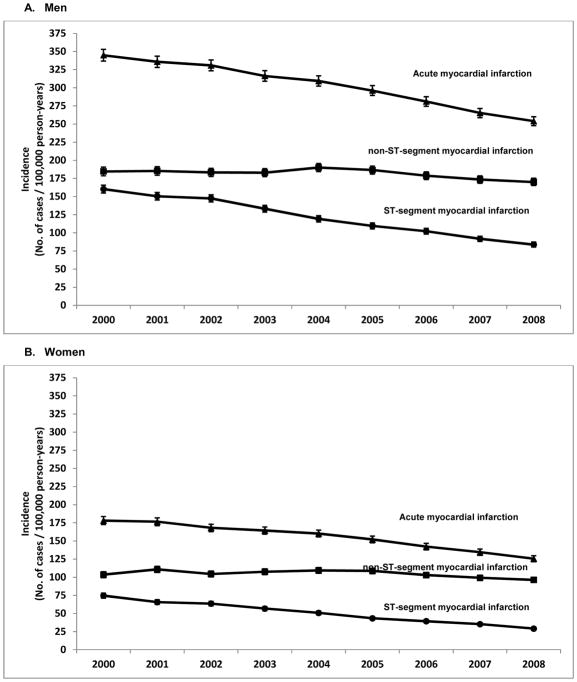
Incidence of hospitalized acute myocardial infarction was higher in men than women in each study year (Figure 4). For men, age-adjusted incidence of hospitalized acute myocardial infarction (per 100,000 person-years) was 26.4% lower in 2008 (254.0 cases; 95% CI, 247.8 to 260.1) than in 2000 (344.9 cases; 95% CI, 336.9 to 352.9), an AAPC of −3.6% (95% CI, −3.9 to −3.3; P<0.001 for linear trend), while the age-adjusted incidence of hospitalized acute myocardial infarction among women was 29.5% lower in 2008 (125.5 cases; 95% CI, 121.4 to 129.6) than in 2000 (178.1 cases; 95% CI, 172.6 to 183.6), an AAPC of −4.2% (95% CI, −4.6 to −3.8; P<0.001 for linear trend) [p for interaction=0.21]. Among both men and women, incidence of non-ST-segment elevation myocardial infarction increased from 2000–2004 and declined slightly thereafter for an overall relative decrease of 7.9% in men and 7.0% in women over the 9 year period. In contrast to acute myocardial infarction and non-ST-segment elevation myocardial infarction, women experienced statistically significantly greater declines in incidence of ST-segment elevation myocardial infarction over the study period compared with men. Incidence of ST-segment elevation myocardial infarction decreased 47.7% among men from 160.3 cases (95% CI, 154.9 to 165.7) in 2000 to 83.8 cases (95% CI, 80.3 to 87.4) in 2008 (AAPC, −8.0%; 95% CI, −8.4 to −7.5; P<0.001 for linear trend) versus a decline of 60.9% among women (P for interaction <0.001), from 74.6 cases (95% CI, 71.0 to 78.1) in 2000 to 29.2 cases (95% CI, 27.2 to 31.2) in 2008 (AAPC, −11.0%; 95% CI, −11.7 to −10.3; P<0.001 for linear trend).
Figure 4.
Age-adjusted incidence of acute myocardial infarction by sex among 7 health care delivery systems of the Cardiovascular Research Network, 2000–2008 (p-value for trend <0.001 for all)
Incidence among men in Panel A and women in Panel B.
 bars represent 95% confidence intervals.
bars represent 95% confidence intervals.
Thirty-Day Case-Fatality Rates
Short-term death rates also declined during the study period. Age- and sex-adjusted 30-day mortality after acute myocardial infarction decreased 38.5% from 5.7% (95% CI, 4.4 to 6.9) in 2000 to 3.5% (95% CI, 2.9 to 4.1) in 2008 (P<0.001 for trend) [data not shown]. This decrease was primarily driven by the case fatality rate for non-ST-segment elevation myocardial infarction, which decreased 48.0% from 5.4% (95% CI, 3.7 to 7.1) in 2000 to 2.8% (95% CI, 2.1 to 3.5) in 2008 (P<0.001 for trend) while the case-fatality rate for ST-segment elevation myocardial infarction decreased 16.3% from 6.0% (95% CI, 4.2 to 7.9) in 2000 to 5.1% (95% CI, 3.9 to 6.3) in 2008 (P<0.001 for trend).
DISCUSSION
Our study demonstrated remarkable reductions in incidence of hospitalized acute myocardial infarction from 2000–2008 among U.S. adults aged ≥25 years. This overall decline was driven by major reductions in incidence of hospitalized ST-segment elevation myocardial infarction, which declined by more than 50% over this period. In contrast, hospitalized non-ST-segment elevation myocardial infarction incidence increased until 2004 and declined only slightly thereafter. The declines in hospitalized acute myocardial infarction were found in all age groups and among both men and women. However, women experienced a significantly greater decline in incidence of ST-segment elevation myocardial infarctions compared with men. The 30-day mortality after acute myocardial infarction also decreased significantly while the use of medications with preventive and cardioprotective effects increased substantially.
Despite the lack of a national surveillance system to monitor trends in coronary heart disease, recent population-based studies in modestly-sized cohorts such as the Framingham Heart Study, Olmsted County (Minnesota), ARIC study, Worcester Heart Attack Study, Minnesota Heart Survey, and the Corpus Christi Heart project have examined trends in incidence of acute myocardial infarction (3–5,12,28,29). Some regional estimates from later periods of the 20th century indicated stable incidence of hospitalized acute myocardial infarction (30,31). More recently, however, incidence of hospitalized acute myocardial infarction is declining, perhaps at an accelerated rate. In our 9-year period of observation, incidence of hospitalized acute myocardial infarction declined by 27%. By comparison, acute myocardial infarction incidence declined by a similar 25% in the Worcester Heart Attack Study, but that decline occurred over 30 years from 1975–2005 (3). In Olmsted County, Minnesota, a 20% decline in age- and sex-adjusted incidence of hospitalized acute myocardial infarction identified by creatine kinase/creatine kinase-MB biomarkers was observed over a 20-year period from 1987–2006 (5). These previous studies have been limited with regards to age, racial/ethnic composition, and national breadth. Furthermore, few studies have characterized trends in incidence of ST-segment elevation myocardial infarctions and non-ST-segment elevation myocardial infarctions separately, as in the current study.
Understanding the specific reasons for the observed declines in incidence of hospitalized episodes of acute myocardial infarction requires additional study. We speculate that the widespread improvements in awareness, treatment, and control of cardiovascular disease risk factors that have occurred over recent decades have likely started to yield considerable influence on the declining incidence of hospitalized acute myocardial infarction, particularly incidence of hospitalized ST-segment elevation myocardial infarction (20). We documented a substantial increase in use of outpatient cardioprotective medications from 2000–2008. Although comorbid conditions increased over the study period, the increase is possibly due to better coding practices or increased screening over time. However, an increase in the prevalence of obesity, diabetes, and hypertension, may have led to the small decline in hospitalized acute myocardial infarction and ST-segment elevation myocardial infarction incidence and increase in hospitalized non-ST-segment elevation myocardial infarction incidence among those aged 25–54 years. It is also possible that the modest decline in incidence of hospitalized non-ST-segment elevation myocardial infarction that we observed may reflect the increasing sensitivity of cardiac biomarkers more recently, resulting in the detection of smaller, previously unrecognized infarctions (32). The observed increase in non-ST-segment elevation myocardial infarction incidence from 2000–2004, which mirrors the widespread increase in troponin testing, supports this hypothesis.
Similar to the results of other studies (5,33,34), incidence of hospitalized acute myocardial infarction was higher for men compared to women during each year of our study. However, in our study, women experienced significantly greater declines in incidence of ST-segment elevation myocardial infarction when compared to men. Few studies have examined long-term sex specific trends by type of acute myocardial infarction. The ARIC study reported a 5.4% and 4.4% decline/year in ST-segment elevation myocardial infarction incidence for men and women, respectively, between 1987–2008 (12). However, the declines were much larger in the period 1997–2008. For men, ST-segment elevation myocardial infarction incidence declined an average of 8.4%/year between 1997–2008 versus 3.0%/year between 1987–1996. For women, ST-segment elevation myocardial infarction incidence declined 6.9%/year between 1997–2008 versus 2.2%/year between 1987–1996 (12). The greater declines we observed in women could be due to better awareness of coronary heart disease among women during recent years due to national public education campaigns introduced in the early 2000s geared towards women or improved screening for and treatment of cardiovascular disease risk factors in women (35–37). Future studies that explore reasons underlying these sex-related differences in temporal trends of acute myocardial infarction are warranted.
The decline in short-term death rates we observed could be the result of a shift from in-hospital to out-of-hospital deaths due to decreased length of hospitalization and improvements in care. This effect may be blunted by our use of the 30-day mortality metric. However, our results support and extend results from previous studies and with reports of the overall decline of age-adjusted coronary heart disease mortality in the U.S. (4,5,12,28,29,38). Furthermore, in a population-based study in New England, declining length of stay between 1995–2005 was not associated with an increased risk of death in the 30 and 90 days following acute myocardial infarction discharge (39).
Our study has several limitations. We did not examine out-of-hospital acute myocardial infarction and relied upon the accuracy and validity of electronic health record and administrative claims data. While our validation study showed that the positive predictive values of codes for ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction were not perfect, the accuracy of the codes did not differ significantly over time. We were unable to assess the effect of changes in diagnostic sensitivity with the introduction of troponins, the most sensitive biomarker of acute myocardial necrosis, because laboratory data were not available at many of the sites. However, troponin assays were already being used in the vast majority of facilities by 2000 (12). Any bias would have likely resulted in an overestimation of incidence of acute myocardial infarction in the latter study years and, therefore, incidence rates of hospitalized acute myocardial infarction over time might have actually declined more than what we observed. Finally, our results may not be fully generalizable to patients in less integrated settings or to uninsured populations.
There are several strengths of the current study. First, this study was significantly larger than many other existing surveillance efforts. Second, we included community-based populations throughout the U.S. with broad diversity in terms of age, sex, race/ethnicity, and geography. Finally, few previous studies have characterized relatively contemporary trends in incidence of hospitalized ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction from a broad multisite perspective.
In summary, our study indicates that the community-based incidence of hospitalized acute myocardial infarction declined between 2000–2008, with dramatic reductions in incidence of the more severe ST-segment elevation myocardial infarctions, with relatively greater improvements observed in women. The secular trends documented in this study are suggestive of improvements in primary prevention efforts. Despite these advances, the increasing prevalence of obesity, diabetes, and hypertension could reverse these encouraging trends in acute myocardial infarction incidence. Therefore, continued population-based surveillance efforts are warranted to monitor recent trends in cardiovascular disease so that appropriate public health strategies can be implemented to prevent a reversal of the gains that have been achieved from primary and secondary prevention efforts during recent decades.
Clinical Significance.
Incidence of hospitalized AMI declined from 2000–2008 among US adults ≥25 years.
The decline in incidence of STEMIs was more pronounced in women than men.
Incidence of hospitalized NSTEMIs did not decline among younger individuals.
Acknowledgments
The writing group for this manuscript wishes to acknowledge the contributions of the following research, administrative, and programming staff at the participating institutions:
Kaiser Permanente Northern California: Noelle Blick, MPH for project management, Michael Emery, MS for programming and statistical support, and the following physicians for medical record adjudication: Philip Chase, MD, Arthur Klatsky, MD, and Arthur Levine, MD.
Kaiser Permanente Southern California: Sole Cardoso for administrative assistance with manuscript preparation, Teresa N. Harrison SM, for project management, Claire Mesirov, MPH and Denison S. Ryan, MPH for medical record abstraction, and Tony Yiu, MS for programming support.
Henry Ford Hospital: Dayna Johnson, MPH, MSW, MS for project management and Carrie Fedorick, RHIT and Cathy McKeon, BA, RHIT for medical record abstraction.
Kaiser Permanente Northwest: Amanda Petrik, MS for programming support.
Meyers Primary Care Institute and Fallon Community Health Plan: Jackie Fuller, MPH for programming support.
Harvard Pilgrim HealthCare Institute: Kelly Horan, MPH for project management, Inna Dashevsky, MS for programming support, and Tracy Lieu, MD, MPH for scientific and methodological support.
Kaiser Permanente Colorado: David Brand, MSPH for project management, Karen Glenn, BS for programming support, and Marilyn Pearson, Kate Burniece and Elizabeth Nash for medical record abstraction.
Scott & White Healthcare: Debbie Godwin, BS and Bhushan Mahajan, MS for programming support and Cindy Hobizal and Shari Wilkerson for medical record abstraction.
Kaiser Permanente Hawaii: Kathleen Bow, RN, BSN, CS for medical record abstraction and Caryn E.S. Oshiro, PhD, MS for administrative support and medical record abstraction.
Geisinger Health System: James Pitcavage, MSPH for project management and Matt Krutsick for programming support.
Marshfield Clinic Research Foundation: Aaron Miller, PhD for programming support and Robert Greenlee, PhD for scientific and methodological support.
Funding/Support: This work was supported through research grants from the National Heart, Lung, and Blood Institute of the National Institutes of Health (RC2 HL101666 and U19 HL091179) and the American Recovery and Reinvestment Act of 2009 (ARRA).
Footnotes
All authors had access to the data and a role in writing the manuscript.
Role of the Funder/Sponsor: The National Institutes of Health had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review or approval of the manuscript; and decision to submit the manuscript for publication. The contents of the manuscript are solely the responsibility of the authors and do not necessarily represent the official views of Kaiser Permanente or the National Institutes of Health.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2015 doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.Sidney S, Rosamond WD, Howard VJ, Luepker RV National Forum for Heart Disease Stroke Prevention. The “heart disease and stroke statistics--2013 update” and the need for a national cardiovascular surveillance system. Circulation. 2013;127(1):21–23. doi: 10.1161/CIRCULATIONAHA.112.155911. [DOI] [PubMed] [Google Scholar]
- 3.Floyd KC, Yarzebski J, Spencer FA, et al. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2(2):88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Parikh NI, Gona P, Larson MG, et al. Long-term trends in myocardial infarction incidence and case fatality in the National Heart, Lung, and Blood Institute’s Framingham Heart study. Circulation. 2009;119(9):1203–1210. doi: 10.1161/CIRCULATIONAHA.108.825364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roger VL, Weston SA, Gerber Y, et al. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121(7):863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang OJ, Wang Y, Chen J, Krumholz HM. Recent trends in hospitalization for acute myocardial infarction. Am J Cardiol. 2012;109(11):1589–1593. doi: 10.1016/j.amjcard.2012.01.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52(5):818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 8.Gregg EW, Cheng YJ, Cadwell BL, et al. Secular trends in cardiovascular disease risk factors according to body mass index in US adults. JAMA. 2005;293(15):1868–1874. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 9.Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42(9):1208–1215. doi: 10.1345/aph.1L181. [DOI] [PubMed] [Google Scholar]
- 10.Pierce JP, Fiore MC, Novotny TE, Hatziandreu EJ, Davis RM. Trends in cigarette smoking in the United States. Projections to the year 2000. JAMA. 1989;261(1):61–65. [PubMed] [Google Scholar]
- 11.Ford ES, Ajani UA, Croft JB, et al. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356(23):2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 12.Rosamond WD, Chambless LE, Heiss G, et al. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125(15):1848–1857. doi: 10.1161/CIRCULATIONAHA.111.047480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 14.Young F, Capewell S, Ford ES, Critchley JA. Coronary mortality declines in the U.S. between 1980 and 2000 quantifying the contributions from primary and secondary prevention. Am J Prev Med. 2010;39(3):228–234. doi: 10.1016/j.amepre.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 16.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 17.Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29(6):1263–1268. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 18.Fox CS, Pencina MJ, Meigs JB, Vasan RS, Levitzky YS, D’Agostino RB., Sr Trends in the incidence of type 2 diabetes mellitus from the 1970s to the 1990s: the Framingham Heart Study. Circulation. 2006;113(25):2914–2918. doi: 10.1161/CIRCULATIONAHA.106.613828. [DOI] [PubMed] [Google Scholar]
- 19.Geiss LS, Pan L, Cadwell B, Gregg EW, Benjamin SM, Engelgau MM. Changes in incidence of diabetes in U.S. adults, 1997–2003. Am J Prev Med. 2006;30(5):371–377. doi: 10.1016/j.amepre.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 20.Huffman MD, Capewell S, Ning H, Shay CM, Ford ES, Lloyd-Jones DM. Cardiovascular health behavior and health factor changes (1988–2008) and projections to 2020: results from the National Health and Nutrition Examination Surveys. Circulation. 2012;125(21):2595–2602. doi: 10.1161/CIRCULATIONAHA.111.070722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooper R, Cutler J, svigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation. 2000;102(25):3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 22.Go AS, Magid DJ, Wells B, et al. The Cardiovascular Research Network: a new paradigm for cardiovascular quality and outcomes research. Circ Cardiovasc Qual Outcomes. 2008;1(2):138–147. doi: 10.1161/CIRCOUTCOMES.108.801654. [DOI] [PubMed] [Google Scholar]
- 23.White AD, Folsom AR, Chambless LE, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49(2):223–233. doi: 10.1016/0895-4356(95)00041-0. [DOI] [PubMed] [Google Scholar]
- 24.Fireman BH, Fehrenbacher L, Gruskin EP, Ray GT. Cost of care for patients in cancer clinical trials. J Natl Cancer Inst. 2000;92(2):136–142. doi: 10.1093/jnci/92.2.136. [DOI] [PubMed] [Google Scholar]
- 25.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 26.Go AS, Lee WY, Yang J, Lo JC, Gurwitz JH. Statin therapy and risks for death and hospitalization in chronic heart failure. JAMA. 2006;296(17):2105–2111. doi: 10.1001/jama.296.17.2105. [DOI] [PubMed] [Google Scholar]
- 27.Selby JV, Ray GT, Zhang D, Colby CJ. Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care. 1997;20(9):1396–1402. doi: 10.2337/diacare.20.9.1396. [DOI] [PubMed] [Google Scholar]
- 28.Goff DC, Nichaman MZ, Chan W, Ramsey DJ, Labarthe DR, Ortiz C. Greater incidence of hospitalized myocardial infarction among Mexican Americans than non-Hispanic whites. The Corpus Christi Heart Project, 1988–1992. Circulation. 1997;95(6):1433–1440. doi: 10.1161/01.cir.95.6.1433. [DOI] [PubMed] [Google Scholar]
- 29.McGovern PG, Pankow JS, Shahar E, et al. Recent trends in acute coronary heart disease--mortality, morbidity, medical care, and risk factors. The Minnesota Heart Survey Investigators. N Engl J Med. 1996;334(14):884–890. doi: 10.1056/NEJM199604043341403. [DOI] [PubMed] [Google Scholar]
- 30.Greenlee RT, Naleway AL, Vidaillet H. Incidence of myocardial infarction in a general population: the Marshfield Epidemiologic Study Area. WMJ. 2002;101(7):46–52. [PubMed] [Google Scholar]
- 31.Roger VL, Jacobsen SJ, Weston SA, et al. Trends in the incidence and survival of patients with hospitalized myocardial infarction, Olmsted County, Minnesota, 1979 to 1994. Ann Intern Med. 2002;136(5):341–348. doi: 10.7326/0003-4819-136-5-200203050-00005. [DOI] [PubMed] [Google Scholar]
- 32.McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124(1):40–47. doi: 10.1016/j.amjmed.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Med. 2010;123(3):259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 34.Towfighi A, Markovic D, Ovbiagele B. National gender-specific trends in myocardial infarction hospitalization rates among patients aged 35 to 64 years. Am J Cardiol. 2011;108(8):1102–1107. doi: 10.1016/j.amjcard.2011.05.046. [DOI] [PubMed] [Google Scholar]
- 35.Mosca L, Ferris A, Fabunmi R, Robertson RM American Heart A. Tracking women’s awareness of heart disease: an American Heart Association national study. Circulation. 2004;109(5):573–579. doi: 10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]
- 36.Mosca L, Linfante AH, Benjamin EJ, et al. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111(4):499–510. doi: 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- 37.Mosca L, Mochari H, Christian A, et al. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113(4):525–534. doi: 10.1161/CIRCULATIONAHA.105.588103. [DOI] [PubMed] [Google Scholar]
- 38.Fox CS, Evans JC, Larson MG, Kannel WB, Levy D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: the Framingham Heart Study. Circulation. 2004;110(5):522–527. doi: 10.1161/01.CIR.0000136993.34344.41. [DOI] [PubMed] [Google Scholar]
- 39.Saczynski JS1, Lessard D, Spencer FA, Gurwitz JH, Gore JM, Yarzebski J, Goldberg RJ. Declining length of stay for patients hospitalized with AMI: impact on mortality and readmissions. Am J Med. 2010;123(11):1007–15. doi: 10.1016/j.amjmed.2010.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]