Abstract
Background and Aims
Endoscopist fatigue may impact colonoscopy quality, but prior studies conflict, and minimal data exist from community-based practices where most colonoscopies are performed.
Methods
Within a large, community-based integrated healthcare system, we evaluated the associations among 4 measures of endoscopist fatigue and colonoscopic adenoma detection during the years 2010 to 2013. Fatigue measures included afternoon versus morning colonoscopy and the number of GI procedures performed before a given colonoscopy, including consideration of prior procedure complexity. Analyses were adjusted for potential confounders using multivariate logistic regression.
Results
We identified 126 gastroenterologists who performed 259,064 total GI procedures (median: 6/day, range: 1–24), including 76,445 screening and surveillance colonoscopies. Compared with morning examinations, colonoscopies in the afternoon were not associated with lower adenoma detection for screening examinations, surveillance examinations, or their combination (odds ratio (OR) for combination 0.99; 95% confidence interval (CI), 0.96–1.03). The number of procedures performed before a given colonoscopy, with or without consideration of prior procedure complexity, was also not inversely associated with adenoma detection (OR for adenoma detection for colonoscopies in the fourth quartile of fatigue based on the number of prior procedures performed versus colonoscopies performed as the first procedure of the day 0.99; 95% CI, 0.94–1.04).
Conclusions
In a large community-based setting, adenoma detection for screening and surveillance colonoscopies was not associated with either time of day or the number of prior procedures performed by the endoscopist, within the range of procedure volumes evaluated. The lack of association persisted after accounting for prior procedure complexity.
INTRODUCTION
Colorectal adenocarcinoma is the second leading cause of cancer death in the United States.1 Colonoscopy is a diagnostic and therapeutic modality capable of detecting and removing adenomas (the precursor lesion), thereby preventing progression to adenocarcinoma. However, the practice of colonoscopy is operator-dependent and repetitive activity may render endoscopists susceptible to mental and perceptual errors due to fatigue.
Recent reports have examined the relationships between measures of endoscopist fatigue and indicators of colonoscopic quality such as adenoma detection rate, the percentage of screening colonoscopies detecting at least one adenoma.2 A physician’s adenoma detection rate is a benchmark of colonoscopic quality; it is associated with patients’ subsequent risk of mortality from colorectal cancer,3 and recommended detection rates were recently increased to 20% or more for women and 30% or more for men.4 However, most prior studies of endoscopist fatigue and colonoscopy quality were conducted in tertiary referral centers, included small numbers of colonoscopies, and had relatively few endoscopists. Only 2 prior studies were conducted in community-based settings where most colonoscopies are performed; 1 was in the United Kingdom5 and the other included just 3 endoscopists.6 No study has examined the relationship between fatigue and colonoscopy quality in a large community-based endoscopy setting within the United States, and no study has used highly standardized measures to account for the complexity of prior procedures, such as relative value units (RVUs), to better estimate the combination of both procedure volume and complexity as a surrogate measure of endoscopist fatigue.7
The aim of this study was to evaluate whether in a large community-based integrated healthcare delivery system in the United States, estimates of endoscopist fatigue at the time of a screening or surveillance colonoscopy were associated with the frequency with which an adenoma was detected during the examination. We evaluated 4 different measures of endoscopist fatigue, including time of day of the colonoscopy, total number of GI procedures before the colonoscopy, and 2 separate measures which incorporated both the total number of prior GI procedures and the prior procedure complexity.
METHODS
Study setting and oversight
This retrospective cross-sectional study was performed within Kaiser Permanente Northern California (KPNC), an integrated health care delivery system. KPNC serves approximately 3.8 million health plan members in urban, suburban, and semi-rural regions throughout Northern California. The KPNC membership is diverse and similar in socioeconomic characteristics to the region’s census demographics, including the proportion with commercial insurance and those with government-sponsored insurance due to older age or disability (Medicare), or low income (Medicaid).8
The study was approved by the KPNC institutional review board, which waived the requirement for informed consent. The listed authors had sole responsibility for the study design, data collection, decision to submit the manuscript for publication and drafting of the manuscript. This study was conducted within the National Cancer Institute-funded Population-based Research Optimizing Screening through Personalized Regimens (PROSPR) consortium (U54 CA163262). The PROSPR consortium conducts multisite, coordinated, transdisciplinary research to evaluate and improve cancer-screening processes.
Study design, eligibility criteria, and data sources
We evaluated whether multiple measures of endoscopist fatigue at the time of screening and surveillance colonoscopy examinations were associated with adenoma detection during the colonoscopy examinations. Endoscopists performed procedures at ambulatory or in-patient endoscopy centers. Colonoscopies were performed according to routine practice using high-definition scopes (almost all centers use Olympus equipment) with images displayed on high-definition video monitors. Optical enhancement tools, such as narrow-band imaging or chromoendoscopy, were used at the discretion of performing providers, and were available for most settings, although these are not routinely used during screening examinations for polyp detection. All identified polyps were retrieved per standard practice and sent for pathologic assessment. Documentation, orders, and patient instructions were completed in an EPIC-based electronic medical record. Although GI procedures vary in length, current scheduling includes approximately 6 patients per 4-hour block, with each patient scheduled for an esophagogastroduodenoscopy, colonoscopy, or both. Typically, the gastroenterologists’ days are divided between clinical/office and procedure-related work, although some days include both morning and afternoon procedure blocks. Patients were provided with a split-dose colonoscopy bowel preparation (e.g., MoviPrep, Salix Pharmaceuticals, Inc) and advised to follow the manufacturer’s split-dose regimen: dose 1 the evening before the colonoscopy (10 to 12 hours before dose 2) and dose 2 the next morning, on the day of the colonoscopy (starting at least 3½ hours before the colonoscopy).
Endoscopic procedures were identified from electronic medical records based on Current Procedural Terminology codes9 and International Classification of Diseases, 9th Revision procedure codes. We identified all colonoscopies performed at KPNC facilities between January 1, 2011 and December 31, 2013, among health plan members ≥50 years of age. For each colonoscopy performed, all the other GI procedures performed by the gastroenterologist that same day were identified, including colonoscopies, esophagogastroduodenoscopies, endoscopic retrograde cholangiopancreatographies, push or balloon-assisted enteroscopies, endoscopic ultrasound examinations, luminal stent placements, flexible sigmoidoscopies, paracenteses, and liver biopsies. This yielded an analytic sample of 76,445 screening and surveillance colonoscopies (46,297 screening and 30,148 surveillance) performed at 21 KPNC facilities by 126 gastroenterologists, and a total of 259,064 GI procedures performed by these gastroenterologists on the days of the colonoscopy examinations.
Colonoscopy examination indication (ie, diagnostic, surveillance, or screening) was assigned using a validated algorithm from electronic consultation reports, clinical diagnoses, laboratory results, and prior pathology data.10 Colonoscopies were considered diagnostic if any sources noted a possible diagnostic indication in the previous 6 months, a positive fecal blood stool test within the previous year, or an inflammatory bowel disease diagnosis within the previous 10 years. In the absence of a diagnostic indication, a surveillance indication was assigned if the patient had a history of colorectal adenomas or polyps, a colonoscopy <10 years before, or a sigmoidoscopy <5 years beforehand. A screening indication was assigned in the absence of indications for a surveillance or diagnostic examination. Family history of colorectal cancer did not affect the assigning of examination indication.
Systematized Nomenclature of Medicine codes from electronic pathology databases were used for histological confirmation of colorectal adenomas; prior validation studies have demonstrated that these codes within KPNC are >95% accurate in their histologic diagnoses compared with manual review of pathology reports (unpublished data).
Data on patient sex, age, race/ethnicity, body mass index, and family history of colorectal cancer, as well as provider codes and procedure start times were extracted from electronic medical records. A small proportion of GI procedures with unknown start times were assigned randomly imputed start times; this included 8,014 total procedures (3.1% of total) and 3,792 colonoscopies (5.0% of total).
Measures of endoscopist fatigue
The exposure of interest, endoscopist fatigue at the time of a given colonoscopy, was estimated using 4 different measures. First, endoscopist fatigue was estimated as a function of the colonoscopy start time (afternoon [≥1:00 pm] vs morning <1:00 pm).
Endoscopist fatigue was also estimated using 3 methods based on the total number of GI procedures performed by the physician before the colonoscopy of interest that same day, including 2 methods that incorporated the complexity of the prior procedures:
The raw fatigue score was calculated as the sum of the raw weights for the GI procedures performed by the physician before the given colonoscopy. Each procedure was assigned a weight of 1 (Table 1) without accounting for prior procedure complexity.
The consensus fatigue score was calculated as the sum of the consensus weights for the GI procedures performed by the physician before the given colonoscopy. Consensus weights reflect procedure complexity based on published studies,11 and ranged from 0.5 to 1.5 (Table 1).
The RVU fatigue score was calculated as the sum of the RVU weights for the GI procedures performed by the physician before the given colonoscopy. RVUs reflect the level of time, skill, training, and intensity needed to perform a procedure (eg, a procedure with a higher RVU typically takes more time, intensity, training, or skill) and use the Centers for Medicare and Medicaid Services’ RVU reimbursement formula for physician services.12 The highest RVU for each individual procedure was used and weights ranged from 1.24 to 20.39 (Table 1).
Table 1.
Raw, consensus, and RVU weights for GI procedures.
| GI procedure | Raw weights | Consensus weights* | RVU weights† |
|---|---|---|---|
| Colonoscopy | 1 | 1.0 | 2.82 – 5.86 |
| Esophagogastroduodenoscopy | 1 | 0.5 | 1.90 – 5.50 |
| Enteroscopy (push or single balloon) | 1 | 1.5 | 2.59 – 7.46 |
| Endoscopic ultrasound | 1 | 1.5 | 3.98 – 7.30 |
| Endoscopic retrograde cholangiopancreatography | 1 | 1.5 | 2.24 – 20.39 |
| Flexible sigmoidoscopy | 1 | 0.5 | 0.80 – 4.05 |
| Luminal stent (small bowel or colon) | 1 | 1.5 | 2.94 – 6.54 |
| Abdominal paracentesis | 1 | 1.0 | 1.24 |
| Liver biopsy | 1 | 0.5 | 1.90 |
RVU, relative value units.
Adapted from Lurix et al. Gastrointest Endosc. 2012;75(4):827–834.
For each GI procedure, reported Current Procedural Terminology codes were extracted from the medical record and corresponding RVU weights specified by the Centers of Medicare and Medicaid Services were recorded; the highest RVU among procedure codes recorded for each individual procedure was used.
Individual patients could have multiple GI procedure types in a single day (eg, esophagogastroduodenoscopy and colonoscopy). If multiple codes were recorded for a single procedure type (eg, for colonoscopy and colonoscopy with biopsy), we assumed a single procedure of that type was performed on that patient and used the code with the highest associated RVU weight.
A sample endoscopy schedule with corresponding fatigue scoring is shown in Table 2. In this example, the endoscopist (provider 1) performed a total of 7 GI procedures, including an esophagogastroduodenoscopy at 7:34 am, a colonoscopy at 9:20 am, and a second colonoscopy at 10.05 am. Focusing on the 10:05 am colonoscopy as an example, the procedure start time is ‘morning’ and the corresponding values for the raw, consensus, and RVU fatigue scores are 2, 1.5, and 8.25, respectively.
Table 2.
Gastroenterology provider schedule examples and calculation of raw, consensus, and RVU fatigue scores.
| Provider | Date | Time | Procedure | Raw weights | Raw fatigue score | Consensus weights | Consensus fatigue score | RVU weights | RVU fatigue score |
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Provider 1 | 3/7/2012 | 07:34 | EGD | 1 | 0 | 0.5 | 0 | 2.39 | 0 |
| Provider 1 | 3/7/2012 | 09:20 | COLO | 1 | 1 | 1.0 | 0.5 | 5.86 | 2.39 |
| Provider 1 | 3/7/2012 | 10:05 | COLO | 1 | 2 | 1.0 | 1.5 | 5.86 | 8.25 |
| Provider 1 | 3/7/2012 | 10:31 | COLO | 1 | 3 | 1.0 | 2.5 | 5.86 | 14.11 |
| Provider 1 | 3/7/2012 | 11:02 | COLO | 1 | 4 | 1.0 | 3.5 | 3.69 | 19.97 |
| Provider 1 | 3/7/2012 | 12:29 | ERCP | 1 | 5 | 1.5 | 4.5 | 8.89 | 23.66 |
| Provider 1 | 3/7/2012 | 13:31 | EGD | 1 | 6 | 0.5 | 6.0 | 3.38 | 32.55 |
|
|
|
|
|||||||
| Provider 2 | 3/7/2012 | 09:12 | COLO | 1 | 0 | 1.0 | 0 | 5.30 | 0 |
| Provider 2 | 3/7/2012 | 09:46 | COLO | 1 | 1 | 1.0 | 1.0 | 3.69 | 5.30 |
| Provider 2 | 3/7/2012 | 10:34 | COLO | 1 | 2 | 1.0 | 2.0 | 3.69 | 8.99 |
| Provider 2 | 3/7/2012 | 11:51 | EGD | 1 | 3 | 0.5 | 3.0 | 2.39 | 12.68 |
| Provider 2 | 3/7/2012 | 11:51 | COLO | 1 | 4 | 1.0 | 3.5 | 5.68 | 15.07 |
| Provider 2 | 3/7/2012 | 12:51 | EGD | 1 | 5 | 0.5 | 4.5 | 2.87 | 20.75 |
| Provider 2 | 3/7/2012 | 12:51 | COLO | 1 | 6 | 1.0 | 5.0 | 3.69 | 23.62 |
| Provider 2 | 3/7/2012 | 13:11 | FLEX | 1 | 7 | 0.5 | 6.0 | 0.96 | 27.31 |
|
|
|
|
|||||||
COLO, colonoscopy; EGD, esophagogastroduodenoscopy; ERCP, endoscopic retrograde cholangiopancreatography; FLEX, flexible sigmoidoscopy; RVU, relative value units.
Raw fatigue score is the sum of the raw weights for the GI procedures performed by the physician before the given colonoscopy; consensus fatigue score is the sum of the consensus weights for the GI procedures performed by the physician before the given colonoscopy; and RVU fatigue score is the sum of the RVU weights for the GI procedures performed by the physician before the given colonoscopy.
Statistical Analyses
Summary statistics were generated to describe the characteristics of the patient population and the adenoma detection rates for the physicians who performed the GI procedures, overall and by patient sex.
The study outcome was colonoscopic adenoma detection, defined as the detection of at least one adenoma per colonoscopy performed. Outcomes were determined for screening and surveillance colonoscopies combined and separately. Diagnostic colonoscopies were excluded from the outcome analyses.
The primary predictors (exposures) were the 4 measures of endoscopist fatigue based on colonoscopy start time (afternoon vs morning), and the number (or number and complexity) of GI procedures performed before the colonoscopy (ie, raw, consensus, and RVU fatigue scores).
The associations between the measures of endoscopist fatigue and risk of adenoma detection were evaluated using multilevel logistic regression models and expressed as adjusted odds ratios (ORs) with 95% confidence intervals (CI). Models were adjusted for patient sex, age (50–54, 55–59, 60–64, 65–69, 70–74, 75–84, and ≥85 years), race/ethnicity (non-Hispanic white, Hispanic, African American, Asian/Pacific Islander, other, and unknown), body mass index (<25, 25–29.9, and ≥30 kg/m2), family history of colorectal cancer, and colonoscopy indication (screening vs surveillance), with clustering on gastroenterologist. This method accounts for the within-endoscopist correlation of patient outcomes. Results are presented for screening and surveillance examinations combined and separately.
For the fatigue measure based on colonoscopy start time, the reference group was all colonoscopies with morning start times (ie, morning screening and surveillance examinations combined and separate), and we hypothesized that colonoscopies performed in the afternoon would be less likely to detect an adenoma than those performed in the morning.
For the 3 fatigue measures based on the number of GI procedures performed by the physician before the given colonoscopy, all the GI procedures performed in a day by a given gastroenterologist were ordered from first to last and then assigned a raw, consensus, and RVU fatigue score. This was done for each physician for each day in which colonoscopies were performed. The screening and surveillance colonoscopy procedures and their associated fatigue scores comprised the analytic data set. Colonoscopies performed as the first GI procedure of the day were assigned a fatigue score of 0 (no fatigue) and these examinations (screening and surveillance examinations combined and separate) served as the reference group. The remaining colonoscopies were divided into approximate quartiles based on their fatigue scores. When the raw fatigue score is used as an example (Table 3), quartile 1 included screening and surveillance colonoscopies with raw fatigue scores of 1 and 2, quartile 2 was comprised of examinations with a score of 3, quartile 3 included examinations with scores of 4 and 5, and quartile 4 included colonoscopies with scores that ranged from 6 to 19. We hypothesized that colonoscopies performed in quartiles 1, 2, 3, or 4 (presumably with higher levels of fatigue) would be less likely to detect an adenoma than colonoscopies performed as the first GI procedure of the day (presumably with the lowest level of fatigue). To examine the linear association between endoscopist fatigue and adenoma detection we performed separate analyses in which fatigues scores were included in the logistic regression models as continuous variables.
Table 3.
Distribution of colonoscopy procedures by fatigue score method.
| Procedures | Fatigue score range | ||
|---|---|---|---|
| n | (%) | ||
| Raw fatigue score | |||
| First of day* | 12,733 | (16.7) | 0 |
| Quartile 1 | 22,998 | (30.1) | 1 – 2 |
| Quartile 2 | 10,240 | (13.4) | 3 – 3 |
| Quartile 3 | 15,074 | (19.7) | 4 – 5 |
| Quartile 4 | 15,400 | (20.1) | 6 – 19 |
| Consensus fatigue score | |||
| First of day* | 12,733 | (16.7) | 0 |
| Quartile 1 | 16,622 | (21.7) | 0.5 – 1.5 |
| Quartile 2 | 18,958 | (24.8) | 2.0 – 3.0 |
| Quartile 3 | 12,334 | (16.1) | 3.5 – 4.5 |
| Quartile 4 | 15,798 | (20.7) | 5.0 – 14.0 |
| RVU fatigue score | |||
| First of day* | 12,733 | (16.7) | 0 |
| Quartile 1 | 14,980 | (19.6) | 0.8 – 7.3 |
| Quartile 2 | 16,405 | (21.5) | 7.3 – 12.7 |
| Quartile 3 | 16,041 | (21.0) | 12.7 – 20.8 |
| Quartile 4 | 16,286 | (21.3) | 20.9 – 67.4 |
The colonoscopy that was the first endoscopy procedure of the day.
SD, standard deviation; n, number; RVU, relative value units.
Raw fatigue score is the sum of the raw weights for the GI procedures performed by the physician before the given colonoscopy; consensus fatigue score is the sum of the consensus weights for the GI procedures performed by the physician before the given colonoscopy; and RVU fatigue score is the sum of the RVU weights for the GI procedures performed by the physician before the given colonoscopy.
Sensitivity analyses were performed excluding 5 medical centers in which patients were formally admitted for same-day procedures, as these centers included most of the small proportion of patients with imputed procedure start times; excluding lower-volume procedure days, defined as days in which individual physicians performed only 1, <4, and <6 total GI procedures that day; and modeling without clustering on endoscopist.
In post-hoc analyses, we examined whether colonoscopy examinations with the highest fatigue scores were less likely to detect adenomas than examinations with the lowest fatigue scores. We divided the 15,400 examinations with 4th quartile raw fatigue scores into 4 approximate sub-quartiles and compared the 2,590 examinations from the sub-quartile with the highest fatigue scores (10–19) with the 12,733 examination that had a raw fatigue score of 0. We used a similar approach for the consensus and RVU fatigue scores. We also evaluated whether endoscopist age modified the relationship between endoscopist fatigue estimates and the likelihood of adenoma detection by including an interaction term for endoscopist age in the adjusted analyses.
All analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC) and STATA version 10.1 (StataCorp, College Station, Tex).
RESULTS
Characteristics of the Patients and Endoscopists
A total of 76,445 colonoscopies were performed, comprised of 46,297 screening and 30,148 surveillance examinations. The characteristics of the patients who received colonoscopy are summarized in Table 4. Women had a higher proportion of screening examinations (54.9%), whereas men had a higher proportion of surveillance examinations (57.2%). Overall, patients were predominately white (64.3%), the mean age was 62.5 years, and more than half were either overweight (25.3%) or obese (31.6%).
Table 4.
Characteristics of patients who had screening or surveillance colonoscopy examinations.
| Screening exams n (%) | Surveillance exams n (%) | All exams n (%) | |
|---|---|---|---|
| Total | 46,297 (60.1) | 30,148 (39.9) | 76,445 (100.0) |
| Male | |||
| Female | 25,420 (54.9) | 12,898 (42.8) | 38,318 (50.1) |
| Male | 20,877 (45.1) | 17,250 (57.2) | 38,127 (49.9) |
| Race/ethnicity | |||
| Non-Hispanic White | 29,121 (62.9) | 20,043 (66.5) | 49,164 (64.3) |
| Hispanic | 4,419 (9.5) | 2,688 (8.9) | 7,107 (9.3) |
| African American | 3,008 (6.5) | 1,711 (5.7) | 4,719 (6.2) |
| Asian/Pacific Islander | 7,191 (15.5) | 4,030 (13.4) | 11,221 (14.7) |
| Other | 1,775 (3.8) | 1,436 (4.8) | 3,211 (4.2) |
| Unknown | 783 (1.7) | 240 (0.8) | 1,023 (1.3) |
| Age | |||
| 50–54 | 12,445 (26.9) | 2,689 (8.9) | 15,134 (19.8) |
| 55–59 | 9,421 (20.4) | 5,099 (16.9) | 14,520 (19.0) |
| 60–64 | 9,362 (20.2) | 6,161 (20.4) | 15,523 (20.3) |
| 65–69 | 8,997 (19.4) | 6,732 (22.3) | 15,729 (20.6) |
| 70–74 | 3,955 (8.5) | 4,898 (16.3) | 8,853 (11.6) |
| 75–84 | 1,986 (4.3) | 4,341 (14.4) | 6,327 (8.3) |
| 85+ | 131 (0.3) | 228 (0.8) | 359 (0.5) |
| Mean (SD) | 60.6 (7.7) | 65.5 (8.1) | 62.5 (8.2) |
| Family history of CRC | |||
| Yes | 9,167 (19.8) | 6,134 (20.4) | 15,301 (20.0) |
| Body mass index (kg/m2) | |||
| <25 | 9,524 (20.6) | 5,911 (19.6) | 15,435 (20.2) |
| 25–29.9 (overweight) | 11,116 (24.0) | 8,207 (27.2) | 19,323 (25.3) |
| ≥ 30 (obese) | 13,380 (28.9) | 10,810 (35.9) | 24,190 (31.6) |
| Unknown | 12,277 (26.5) | 5,220 (17.3) | 17,497 (22.9) |
| Colonoscopy start time | |||
| Morning | 28,134 (60.8) | 19,301 (64.0) | 47,435 (62.1) |
| Afternoon | 15,471 (33.4) | 9,747 (32.3) | 25,218 (33.0) |
| Imputed time | 2,692 (5.8) | 1,100 (3.7) | 3,792 (5.0) |
| Year of colonoscopy | |||
| 2011 | 15,253 (33.0) | 8,689 (28.8) | 23,942 (31.3) |
| 2012 | 15,288 (33.0) | 10,256 (34.0) | 25,544 (33.4) |
| 2013 | 15,756 (34.0) | 11,203 (37.2) | 26,959 (35.3) |
CRC, colorectal cancer; n, number; SD, standard deviation.
The 126 gastroenterologists in the study performed 259,064 GI procedures on the days in which screening or surveillance colonoscopies were performed. Individually, physicians performed a median of 3,113 GI procedures during the study period for the calculation of fatigue scores; these included a median of 588 screening and surveillance colonoscopies per physician (interquartile range: 398–778 examinations). A median of 6 GI procedures and 3 colonoscopies were performed per physician per day, with a maximum of 14 colonoscopies and 24 total GI procedures per physician per day. Mean physician adenoma detection rates were 28.9% for screening colonoscopy examinations (34.8% for men and 24.0% for women), and 45.4% for surveillance examinations (51.1% for men and 37.8% for women).
Association of endoscopist fatigue and colonoscopic adenoma detection
There were no differences in adenoma detection for afternoon compared with morning colonoscopies overall (OR 0.99; 95% CI, 0.96–1.03) or by examination indication (screening examination OR 0.97; 95% CI, 0.93–1.02; surveillance examination OR 1.02; 95% CI, 0.97–1.08) (Table 5).
Table 5.
Association between measures of endoscopist fatigue and colonoscopic adenoma detection.
| Fatigue measures | Screening exams n=46,297 OR (95% CI) |
Surveillance exams n=30,148 OR (95% CI) |
All exams* n=76,445 OR (95% CI) |
|---|---|---|---|
| Start time: | |||
| Morning Exam | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Afternoon Exam | 0.97 (0.93 – 1.02) | 1.02 (0.97 – 1.08) | 0.99 (0.96 – 1.03) |
| Raw fatigue score | |||
| First of the day† | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Quartile 1 | 1.09 (1.02 – 1.16) | 0.97 (0.90 – 1.04) | 1.03 (0.99 – 1.09) |
| Quartile 2 | 1.10 (1.02 – 1.19) | 1.05 (0.96 – 1.14) | 1.08 (1.02 – 1.14) |
| Quartile 3 | 1.06 (0.99 – 1.14) | 1.05 (0.97 – 1.14) | 1.05 (1.00 – 1.11) |
| Quartile 4 | 0.99 (0.92 – 1.06) | 1.00 (0.92 – 1.08) | 0.99 (0.94 – 1.04) |
| Consensus fatigue score | |||
| First of the day† | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Quartile 1 | 1.08 (1.00 – 1.15) | 0.98 (0.91 – 1.06) | 1.03 (0.98 – 1.09) |
| Quartile 2 | 1.12 (1.05 – 1.20) | 1.01 (0.94 – 1.09) | 1.07 (1.02 – 1.12) |
| Quartile 3 | 1.04 (0.97 – 1.12) | 1.03 (0.95 – 1.12) | 1.04 (0.98 – 1.10) |
| Quartile 4 | 0.99 (0.93 – 1.07) | 1.02 (0.94 – 1.10) | 1.00 (0.95 – 1.05) |
| RVU fatigue score | |||
| First of the day† | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| Quartile 1 | 1.10 (1.03 – 1.18) | 0.99 (0.91 – 1.07) | 1.05 (1.00 – 1.11) |
| Quartile 2 | 1.09 (1.02 – 1.17) | 0.99 (0.92 – 1.07) | 1.04 (0.99 – 1.10) |
| Quartile 3 | 1.06 (0.99 – 1.14) | 1.02 (0.94 – 1.10) | 1.04 (0.99 – 1.09) |
| Quartile 4 | 1.00 (0.93 – 1.07) | 1.04 (0.96 – 1.13) | 1.01 (0.96 – 1.06) |
Screening and surveillance examinations combined.
The colonoscopy that was the first GI procedure of the day.
OR, odds ratio; n, number; CI, confidence interval; RVU, relative value units.
Raw fatigue score is the sum of the raw weights for the GI procedures performed by the physician before the given colonoscopy; consensus fatigue score is the sum of the consensus weights for the GI procedures performed by the physician before the given colonoscopy; and RVU fatigue score is the sum of the RVU weights for the GI procedures performed by the physician before the given colonoscopy.
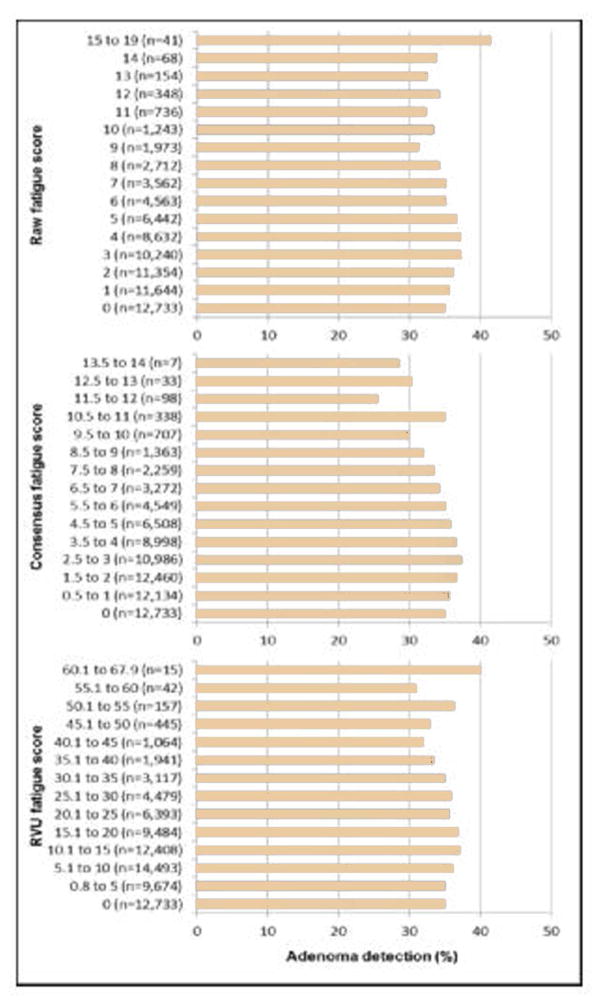
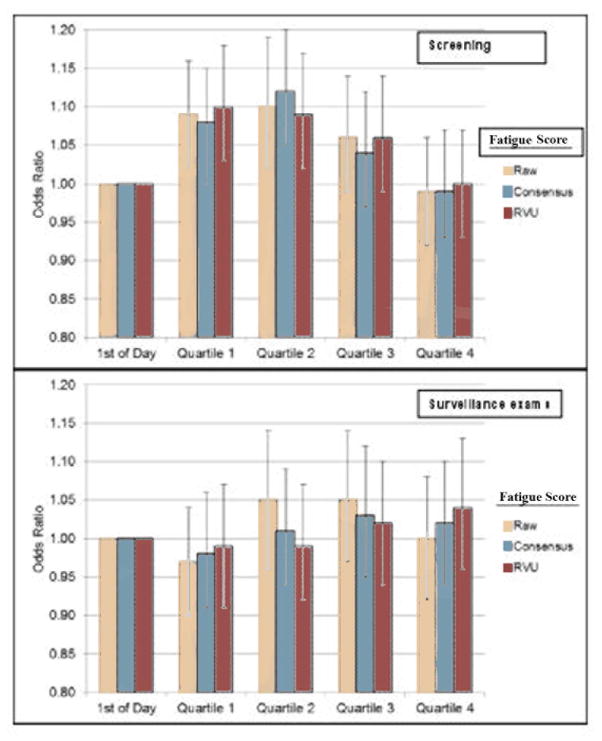
The frequency of adenoma detection for screening and surveillance colonoscopies combined across the range of endoscopist fatigue scores is shown in Figure 1 with no obvious patterns noticeable, even within the highest fatigue scores clustered within the fourth quartile. Using multivariate logistic regression analyses, we found no inverse relationship between the raw, consensus, and RVU fatigue scores and the frequency of colonoscopic adenoma detection. For example, for all colonoscopies combined, compared with the frequency of adenoma detection for colonoscopies that were performed as the first endoscopic procedure of the day, the adjusted ORs (95% CIs) for detecting an adenoma for colonoscopies that were in the fourth quartile were 0.99 (95% CI, 0.94–1.04) for the raw fatigue score (number of prior procedures), 1.00 (95% CI, 0.95–1.05) for the consensus fatigue score (number and complexity of prior procedures), and 1.01 (95% CI, 0.96–1.06) for the RVU fatigue score (number and complexity of prior procedures) (Table 5). Findings were similar when surveillance colonoscopies were examined separately. However, compared with screening colonoscopies that were performed as the first endoscopic procedure of the day, there was a small increase in adenoma detection for screening colonoscopies in quartiles 1 and 2 (raw fatigue score: OR 1.09; 95% CI, 1.02–1.16 and OR 1.10; 95% CI, 1.02–1.19, respectively), whereas adenoma detection for screening colonoscopies in quartile 4 returned to the baseline detection level (OR 0.99; 95% CI, 0.92–1.06) (Table 5 and Figure 2). This same pattern was observed for consensus and RVU fatigue scores which incorporated the number and complexity of prior procedures.
Figure 1. The frequency of colonoscopic adenoma detection by endoscopist fatigue score.
Raw fatigue score is the sum of the raw weights for the GI procedures performed by the physician before the given colonoscopy; consensus fatigue score is the sum of the consensus weights for the GI procedures performed by the physician before the given colonoscopy; and RVU fatigue score is the sum of the RVU weights for the GI procedures performed by the physician before the given colonoscopy.
Figure 2. Association between endoscopist fatigue scores (raw, consensus, and RVU fatigue scores) and colonoscopic adenoma detection (screening and surveillance colonoscopy examinations).
1st of Day is the reference and refers to the colonoscopies that were the first GI procedures of the day. Error bars represent 95% confidence intervals. RVU, relative value units.
Raw fatigue score is the sum of the raw weights for the GI procedures performed by the physician before the given colonoscopy; consensus fatigue score is the sum of the consensus weights for the GI procedures performed by the physician before the given colonoscopy; and RVU fatigue score is the sum of the RVU weights for the GI procedures performed by the physician before the given colonoscopy.
Sensitivity analyses demonstrated similar patterns to those described above, although smaller sample sizes produced wider confidence intervals. These analyses included the exclusion of 5 medical centers in which patients were admitted for same-day procedures, which excluded the majority of the small number of GI procedures that required imputed start times (Supplementary Table 1) and the exclusion of endoscopist-days in which <6 endoscopy procedures were performed (Supplementary Table 2). When fatigue scores were modeled as continuous variables, endoscopist fatigue was not related to adenoma detection for either screening examinations, surveillance examinations, or screening and surveillance examinations combined (data not shown).
In post-hoc analyses, compared with examinations with a raw fatigue score of 0 (34.9% adenoma detection rate), the adjusted OR for adenoma detection for examinations with raw fatigue scores of 10 to 19 (33.2% adenoma detection rate) was 0.98 (95% CI, 0.89–1.08). The adjusted ORs were similarly not statistically significant for the consensus and RVU fatigue score measures (OR 0.94; 95% CI, 0.87–1.02 for both measures). We also found that endoscopist age did not modify the relationship between endoscopist fatigue estimates and the likelihood of adenoma detection (interaction p>0.35).
DISCUSSION
In a large community-based integrated health care delivery setting, we found that colonoscopies performed in the afternoon were not less likely to detect adenomas than examinations in the morning and that endoscopist fatigue based on the number of prior GI procedures performed, with or without consideration of procedure complexity, were not inversely associated with colonoscopic adenoma detection within the range of procedure volumes evaluated.
Prior studies differ regarding whether measures of colonoscopist fatigue are associated with lower frequency of adenoma detection. Two studies in 2009 reported that, in comparison to colonoscopies performed earlier in the day, later examinations detected fewer polyps and adenomas; respectively, these studies reported morning colonoscopies had a 27% higher polyp yield than afternoon colonoscopies (p<0.001), and morning versus afternoon adenoma detection rates of 29.3% versus 25.3% (p=0.008).13,14 Conversely, 3 other studies reported no significant time-of-day effect for procedures performed in half-day or 3-hour blocks, compared with full-day blocks.6,15,16 A study in 2011 found that increasing procedure queue position (similar to the current study’s raw fatigue score) was associated with decreased polyp detection; specifically, each increase in queue position by one was associated with a 5.4% decrease in polyp detection.17 Three other studies,5,18,19 found lower adenoma detection with increasing operator fatigue measured by various means, including use of a questionnaire to designate endoscopists as fatigued versus not-fatigued and which reported detection rates of 25.0% versus 42.6% (p=0.008), respectively.18 In contrast, 4 studies evaluated hours elapsed in the day, morning versus afternoon procedure time, and/or queue position and found no or minimal differences in adenoma detection.11,20–22
Almost all of the studies cited above were conducted at academic institutions with relatively small numbers of endoscopists and colonoscopy examinations; only 2 were in community-based settings,5,6 and the only community-based study in the United States included just 3 endoscopists.6 Our study is the largest to date to investigate the relationship between endoscopist fatigue and colonoscopy quality, and it focuses on a community-based population of both patients and physicians. This distinction is important as community-based settings are where most gastroenterologists practice and where colonoscopies are performed in the United States. In contrast, academic hospital settings often include trainees or part-time clinicians. In addition, average endoscopist adenoma detection rates in our study were consistent with colonoscopic quality benchmarks, including ≥30% for men and ≥20% for women.4,23 We also evaluated 4 different measures of endoscopist fatigue, including highly standardized RVUs, which quantify the complexity of different GI procedures. The study’s performance in a health care system which used split-dose evening/morning bowel preparations is another strength. Split-dose bowel preparations may decrease confounding of the endoscopist versus time-of-day relationship by differences in bowel preparation over the day, given that split-dose preparations provide more consistent results over the day. Finally, potential study biases were investigated through sensitivity analyses. In particular, excluding the small proportion of procedures with imputed start times and excluding lower volume days did not substantively change our findings.
It is likely that at some level, GI procedure volume before a colonoscopy will adversely impact the time needed for adenoma detection; the moderate median number of GI procedures performed per day in this population largely represented days that physicians divided between clinical/office and procedure-related work. Conceivably, the impact of fatigue on colonoscopy quality might be diluted by lower volume endoscopists or by lower volume days. Although excluding endoscopist-days with 1, <4, and <6 total GI procedures did not change the pattern of our findings, this study could not evaluate the effect of consistently larger daily volumes (i.e., frequent days with procedures in both the morning and afternoon) or of consistently larger volumes in a single session (eg, in either the morning or afternoon). Another potential limitation of our study is the lack of detailed cecal intubation and bowel preparation data for each colonoscopy. However, reported physician adenoma detection rates in our setting suggest high-quality colonoscopy performance,3 with prior large-scale chart reviews in our population demonstrating cecal intubation rates of 97.7% and adequate-to-excellent bowel preparations in 92.0% of examinations.10 Although some reports suggest that colonoscopies performed later in the day may have lower-quality bowel preparations which could reduce adenoma detection,24–26 we did not observe a decline in adenoma detection with later procedure start times or a higher number of procedures performed before a given colonoscopy; thus, it is unlikely that adjustment for bowel preparation quality would have substantively altered our results. Finally, another possible limitation is an inability to account for other non-endoscopic activities which may contribute to physician fatigue, such as outpatient and inpatient clinical duties. This limitation is inherent to virtually all studies of colonoscopic operator fatigue, apart from those using direct measurements;18 however, the reported lack of an association with time of day would argue against this being a substantial factor in the current study.
An unexpected finding of our study was the small increase in adenoma detection for screening colonoscopies after the first screening colonoscopy procedure of the day, followed by a return to baseline detection levels for subsequent screening examinations. This is the first study, to our knowledge, to report this possible “warming-up” effect. With its repetitive nature and reliance on stereotypical and rehearsed movements, colonoscopy may be an activity in which peak performance is reached after one or a few initial endoscopy procedures are completed and the operator’s movements are comfortably set. As seen in athletes, this effect may be more psychological than physical/fatigue-oriented in nature, although some improvement in physical performance has been documented with short periods of stretching/warming-up.27,28 The fact that increased adenoma detection was found only for screening colonoscopy examinations raises the question of whether endoscopists were systematically more vigilant during screening procedures, although the higher observed adenoma detection rates for surveillance examinations suggest otherwise. Finally, the observed increase in adenoma detection was small (a relative increase of 8% to 12%), and thus the clinical relevance of this possible “warming-up” effect is unclear.
In conclusion, we found no difference in adenoma detection for afternoon versus morning colonoscopies in this large community-based practice setting. Also, multiple measures of endoscopist fatigue based on the number or number and complexity of prior procedures performed were not inversely associated with colonoscopic adenoma detection, within the range of GI procedure volumes evaluated.
Supplementary Material
Text Abbreviations
- CI
confidence interval
- KPNC
Kaiser Permanente Northern California
- n
number
- OR
odds ratio
- PROSPR
Population-based Research Optimizing Screening through Personalized Regimens
- RVU
Relative Value Unit
Footnotes
Disclosures: No conflicts of interest exist for any of the authors.
Author Contributions: AL, CDJ, ARM, and DAC participated in study concept and design, obtaining of funding, study supervision, acquisition and interpretation of data, statistical analysis, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. WKZ participated in acquisition and interpretation of data and critical revision of the manuscript for important intellectual content. TRL, CAD, AGZ and VPQ participated in critical revision of the manuscript for important intellectual content.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008;134:1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 2.Williams JE, Holub JL, Faigel DO. Polypectomy rate is a valid quality measure for colonoscopy: results from a national endoscopy database. Gastrointestinal Endoscopy. 2012;75:576–82. doi: 10.1016/j.gie.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. The New England journal of medicine. 2014;370:1298–306. doi: 10.1056/NEJMoa1309086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointestinal Endoscopy. 2015;81:31–53. doi: 10.1016/j.gie.2014.07.058. [DOI] [PubMed] [Google Scholar]
- 5.Lee TJ, Rees CJ, Blanks RG, et al. Colonoscopic factors associated with adenoma detection in a national colorectal cancer screening program. Endoscopy. 2014;46:203–11. doi: 10.1055/s-0033-1358831. [DOI] [PubMed] [Google Scholar]
- 6.Freedman JS, Harari DY, Bamji ND, et al. The detection of premalignant colon polyps during colonoscopy is stable throughout the workday. Gastrointestinal Endoscopy. 2011;73:1197–206. doi: 10.1016/j.gie.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 7.Spiegel BM. Does time of day affect polyp detection rates from colonoscopy? Gastrointestinal Endoscopy. 2011;73:476–9. doi: 10.1016/j.gie.2010.09.026. [DOI] [PubMed] [Google Scholar]
- 8.Gordon NP. How Does the Adult Kaiser Permanente Membership in Northern California Compare with the Larger Community? Oakland, CA: Kaiser Permanente Division of Research; 2006. [Google Scholar]
- 9.CPT 2011 Professional Edition. American Medical Association Press; 2010. [Google Scholar]
- 10.Lee JK, Jensen CD, Lee A, et al. Development and validation of an algorithm for classifying colonoscopy indication. Gastrointestinal Endoscopy. 2015;81:575–82. e4. doi: 10.1016/j.gie.2014.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lurix E, Hernandez AV, Thoma M, Castro F. Adenoma detection rate is not influenced by full-day blocks, time, or modified queue position. Gastrointestinal Endoscopy. 2012;75:827–34. doi: 10.1016/j.gie.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 12. [Accessed October 9, 2015];Physician Fee Schedule Relative Value Items Files. at https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files-Items/RVU13AR.html.
- 13.Chan MY, Cohen H, Spiegel BM. Fewer polyps detected by colonoscopy as the day progresses at a Veteran’s Administration teaching hospital. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2009;7:1217–23. doi: 10.1016/j.cgh.2009.07.013. quiz 143. [DOI] [PubMed] [Google Scholar]
- 14.Sanaka MR, Deepinder F, Thota PN, Lopez R, Burke CA. Adenomas are detected more often in morning than in afternoon colonoscopy. The American journal of gastroenterology. 2009;104:1659–64. doi: 10.1038/ajg.2009.249. quiz 65. [DOI] [PubMed] [Google Scholar]
- 15.Gurudu SR, Ratuapli SK, Leighton JA, Heigh RI, Crowell MD. Adenoma detection rate is not influenced by the timing of colonoscopy when performed in half-day blocks. The American journal of gastroenterology. 2011;106:1466–71. doi: 10.1038/ajg.2011.125. [DOI] [PubMed] [Google Scholar]
- 16.Munson GW, Harewood GC, Francis DL. Time of day variation in polyp detection rate for colonoscopies performed on a 3-hour shift schedule. Gastrointestinal Endoscopy. 2011;73:467–75. doi: 10.1016/j.gie.2010.07.025. [DOI] [PubMed] [Google Scholar]
- 17.Lee A, Iskander JM, Gupta N, et al. Queue position in the endoscopic schedule impacts effectiveness of colonoscopy. The American journal of gastroenterology. 2011;106:1457–65. doi: 10.1038/ajg.2011.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee CK, Cha JM, Kim WJ. Endoscopist Fatigue May Contribute to a Decline in the Effectiveness of Screening Colonoscopy. Journal of clinical gastroenterology. 2015;49:e51–6. doi: 10.1097/MCG.0000000000000175. [DOI] [PubMed] [Google Scholar]
- 19.Paeck KH, Heo WJ, Park DI, et al. Colonoscopy scheduling influences adenoma and polyp detection rates. Hepato-gastroenterology. 2013;60:1647–52. [PubMed] [Google Scholar]
- 20.Leffler DA, Kheraj R, Bhansali A, et al. Adenoma detection rates vary minimally with time of day and case rank: a prospective study of 2139 first screening colonoscopies. Gastrointestinal Endoscopy. 2012;75:554–60. doi: 10.1016/j.gie.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 21.Borda F, Borda A, Jimenez FJ, Fernandez-Urien I, Vila JJ, Zozaya JM. Does endoscopist fatigue play a role in incomplete colonoscopies and detection of polypoid lesions? Gastroenterol Hepatol. 2014;37:9–16. doi: 10.1016/j.gastrohep.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Thurtle D, Pullinger M, Tsigarides J, McIntosh I, Steytler C, Beales I. Colonoscopic polyp detection rate is stable throughout the workday including evening colonoscopy sessions. F1000Res. 2014;3:107. doi: 10.12688/f1000research.4045.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rex DK, Petrini JL, Baron TH, et al. Quality indicators for colonoscopy. The American journal of gastroenterology. 2006;101:873–85. doi: 10.1111/j.1572-0241.2006.00673.x. [DOI] [PubMed] [Google Scholar]
- 24.Gurudu SR, Ratuapli S, Heigh R, DiBaise J, Leighton J, Crowell M. Quality of bowel cleansing for afternoon colonoscopy is influenced by time of administration. The American journal of gastroenterology. 2010;105:2318–22. doi: 10.1038/ajg.2010.235. [DOI] [PubMed] [Google Scholar]
- 25.Eun CS, Han DS, Hyun YS, et al. The timing of bowel preparation is more important than the timing of colonoscopy in determining the quality of bowel cleansing. Digestive diseases and sciences. 2011;56:539–44. doi: 10.1007/s10620-010-1457-1. [DOI] [PubMed] [Google Scholar]
- 26.Siddiqui AA, Yang K, Spechler SJ, et al. Duration of the interval between the completion of bowel preparation and the start of colonoscopy predicts bowel-preparation quality. Gastrointestinal Endoscopy. 2009;69:700–6. doi: 10.1016/j.gie.2008.09.047. [DOI] [PubMed] [Google Scholar]
- 27.Hale CJ, Karpovich PV. Effect of warming-up upon physical performance. J Am Med Assoc. 1956;162:1117–9. doi: 10.1001/jama.1956.02970290013005. [DOI] [PubMed] [Google Scholar]
- 28.Behm DG, Chaouachi A. A review of the acute effects of static and dynamic stretching on performance. Eur J Appl Physiol. 2011;111:2633–51. doi: 10.1007/s00421-011-1879-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.