Abstract
Background
Laboratory-based studies on neuromuscular control after concussion and epidemiological studies suggest that concussion may increase the risk of subsequent musculoskeletal injury.
Objective
The purpose of this study was to determine if athletes have an increased risk of lower extremity musculoskeletal injury after return-to-play from a concussion.
Methods
Injury data were collected from 2006–2013 for men’s football and women’s basketball, soccer, and lacrosse at a NCAA Division I university. Ninety cases in 73 athletes (52 Male, 21 Female) of in-season concussion with return-to-play at least 30 days prior to the end of the season were identified. A period of up to 90 days of in-season competition following return-to-play was reviewed for time-loss injury. The same period was studied in up to two control athletes who were without a concussion within the prior year and were matched on sport, starting status, and position.
Results
Lower extremity musculoskeletal injuries occurred at a higher rate in the concussed athletes (45/90 or 50%) compared to the non-concussed athletes (30/148 or 20%) (p < 0.01). The odds of sustaining a musculoskeletal injury were 3.39 times higher in the concussed athletes (95% CI = 1.90, 6.05; p < 0.01). Overall, the number of days lost due to injury was similar between concussed and non-concussed athletes (Median = 9 vs 15, p = 0.41).
Conclusions
The results of this study demonstrate a relationship between concussion and an increased risk of lower extremity musculoskeletal injury after return to play, and may have implications for current medical practice standards regarding the evaluation and management of concussion injuries.
Introduction
Sports and recreation-related concussion is a common injury with an estimated incidence of 1.6 to 3.6 million annually in the United States [1, 2]. Concussions are known to result in transient decrements of neurocognitive function; however, previous studies have demonstrated that alterations may exist across multiple domains of function, including neuromuscular control. For example, there is a growing body of evidence that post-concussion neuromuscular control impairments are present during simple gait-related tasks such as obstacle navigation, obstacle clearance, gait initiation, and gait termination [3–9]. These neuromuscular control impairments extend well beyond symptomatic recovery and fulfillment of return to play criteria [6, 10]. Given the limited challenge posed by these gait tasks, neuromuscular control impairments are likely to be accentuated during high-demand athletic tasks.
Poor neuromuscular control has been demonstrated to be a risk factor for musculoskeletal injury. For example, abnormal movement patterns in the lower extremity and trunk have been shown to be different between high and low risk groups for anterior cruciate ligament injury; in particular, excessive frontal plane motion at the knee and poor trunk control have been found to be predictive of injury [11, 12]. As neuromuscular performance impairments have been demonstrated in concussed athletes even after the point of return to play, there may be an undefined ”window of susceptibility” during which the risk of experiencing serious musculoskeletal injuries is increased.
The potential for such an increased risk of musculoskeletal injury after concussion has been observed in recently published studies in professional athletes. Nordstrom et. al. examined an injury registry comprised of 46 elite male professional soccer clubs from the 2001/02 to 2011/12 seasons [13]. Sixty-six cases of concussion were examined and were found to have a hazard ratio of 1.70 for sustaining an acute-onset musculoskeletal injury in the year after concussion compared to the year prior to concussion. The hazard ratios for acute-onset injury in comparison to non-concussed players ranged from 1.76 to 3.69 depending on the duration of time from the concussion injury. Cross et. al. noted similar findings among professional rugby players, with the incidence of any injury for players who returned to play in the same season following a diagnosed concussion being 60% higher compared to non-concussed players [14]. Finally, Pietrosimone et. al. employed a survey of 2429 retired professional football players and demonstrated an association of multiple injury types in players who also reported a history of concussion [15]. The number of injuries experienced was also found to increase with increasing number of concussions.
Similar findings have been noted in collegiate populations. Lynall et. al. examined the risk of injury of concussed collegiate athletes in comparison to their risk of injury over the prior year and to that of matched non-concussed control athletes [16]. They reported that concussed athletes were 1.97 times more likely to have experienced an acute lower extremity musculoskeletal injury in the 365 days post-concussion than prior to concussion, and 1.64 times more likely to have such an injury in comparison to the matched controls. Brooks et. al. also examined the risk of musculoskeletal injury in concussed collegiate athletes compared to non-concussed controls, finding that the odds of concussed players experiencing an injury to be 2.48 times that of the control athletes over a 90 day follow up window [17].
However, there are limitations to this data. In particular, some of the above studies [13–15] lack controls for relative amounts of participation; hence, it is possible that the relationship between concussion and musculoskeletal injury may have been a function of higher rates of exposure (e.g. starters versus reserve players). In addition to recall bias associated with retrospective survey data, the temporal relationship between the injuries is not known in the study by Pietrosimone et. al. [15]; that is, the concussions experienced may or may not have been prior to the reported musculoskeletal injuries. Finally, with the exception of the study by Pietrosimone et. al., the number of athletes studied has been relatively limited; while Lynall et. al. used a mixed-sex cohort, there have been no sex-specific comparisons of injury rates after concussion.
In summary, there is evidence from both laboratory-based studies on neuromuscular control after concussion and epidemiological studies to suggest that concussion may increase the risk of subsequent musculoskeletal injury. An increased risk of musculoskeletal injury following concussion may necessitate changes in clinical management and rehabilitation of concussion injuries; thus accurate knowledge of the parameters of this potential relationship is required. The purpose of this study was to determine the risk of experiencing a time-loss lower extremity musculoskeletal injury after return to play from concussion in collegiate athletes (“time-loss” defined as being withheld from competition for at least one day). We hypothesized that athletes who had experienced a concussion would be at higher odds for injury during an in-season period of up to 90 days after return to play compared to non-concussed athletes matched on sport, starting status, and position. Furthermore, we hypothesized that the severity of injuries experienced would be greater in the athletes who had experienced a concussion (“severity” defined as number of time-loss days).
Methods
This research project was approved by the Institutional Review Board at the University of Florida.
Study design
This investigation was designed as an observational historical cohort study. Exposed athletes were those with an in-season concussion as diagnosed by the university primary care sports medicine certified physician assigned to each athlete’s sport team. Non-exposed athletes were those without a concussion. Exposed and non-exposed athletes were matched by sport, starting status (starter, reserve), and main position played. Players were determined to be starters if they started in 50% or greater available matches during the season studied, and were classified as reserves if they started in less than 50% available matches. The goal ratio of non-exposed to exposed players was 2 to 1. In the event that more than two non-exposed athletes were qualified to be matched to a given exposed athlete, the two non-exposed athletes used for analysis were selected from the pool of available non-exposed athletes using a random sequence generator. A given non-exposed athlete was only matched to one exposed athlete at any given time during the study.
Exclusion criteria
Athletes were excluded if 1) there was a history of concussion within the prior six months (either group), 2) the concussion occurred outside the competitive season (e.g. off-season or spring football), 3) the player had time loss within 30 days of return to play due to issues unrelated to a musculoskeletal injury (e.g. suspension), or 4) the duration of the remaining competitive season at the time of return to play from a concussion was less than 30 days.
Outcomes
The main outcome of interest was the first time-loss lower extremity musculoskeletal injury (yes, no) in athletes exposed to concussion and the matched non-exposed athletes within up to 90 days of in-season return to play after the concussion. Time-loss was defined as being withheld from competition for at least one day. Each exposed athlete and their respective matched non-exposed athlete(s) were followed for the outcome of interest along the same exact time line starting at day one of the exposed athlete’s full return to play after concussion and ending after 90 days. Any injuries which occurred after the first musculoskeletal injury during the 90 day follow-up period were not included in the analysis. A musculoskeletal injury was defined was a strain, sprain, dislocation, or rupture but did not include overuse injuries, fractures, or contusions. A secondary outcome of interest was severity, defined as the number of days the player was withheld from competition due to lower extremity musculoskeletal injury.
Data collection
Training room-base injury surveillance data (SIMS, Iowa City, IA) from an elite Division I collegiate athletics program (The University of Florida Athletic Association) was queried for cases of concussion from the 2006/07 to 2012/13 seasons for men’s football and women’s basketball, soccer, and lacrosse. For each study subject, the following data were collected: player identification number, status (exposed, non-exposed to concussion), gender (male, female), age (years), sport (football, basketball, soccer, lacrosse), main position played (see Table 1), starting status (starter, reserve), lower extremity musculoskeletal injury (yes, no) and time lost from any lower extremity musculoskeletal injury (days).
TABLE 1.
Cases by Position
| Sport | Position | Exposed Cases (N = 90) |
Non-Exposed Cases (N = 148) |
|---|---|---|---|
| Football | |||
|
| |||
| Defensive Back | 8 | 14 | |
| Defensive Line | 10 | 18 | |
| Linebacker | 12 | 19 | |
| Offensive Line | 9 | 16 | |
| Running Back | 10 | 14 | |
| Wide Receiver | 17 | 25 | |
| Lacrosse | |||
|
| |||
| Attack | 1 | 1 | |
| Defender | 6 | 10 | |
| Midfielder | 2 | 4 | |
| Soccer | |||
|
| |||
| Attack | 1 | 1 | |
| Defender | 6 | 10 | |
| Midfielder | 5 | 10 | |
| Basketball | |||
|
| |||
| Guard | 1 | 2 | |
| Forward | 3 | 4 | |
Data analyses
The incidence of sustaining a lower extremity musculoskeletal injury was compared between athletes exposed or non-exposed to concussion by using a chi-square test. Univariate conditional logistic regression analysis was used to estimate the odds of sustaining a lower extremity musculoskeletal injury in athletes with a recent concussion compared to athletes without concussion. In addition, the odds of lower extremity musculoskeletal injury were compared between athletes exposed or non-exposed to concussion on the basis of sex (male, female) and starting status (starter, reserve). Survival curves for time (days) to lower extremity musculoskeletal injury during competition in athletes affected and non-affected with concussion were estimated by using the Kaplan-Meier test. Median time to injury (days) during competition and median time to lost due to lower extremity musculoskeletal injury (days) were compared between groups using the Wilcoxon signed-rank test.
Results
The study sample included 52 male and 21 female athletes with a total of 90 qualifying exposures (Table 1). Two matching non-exposed athletes (82M, 34F) were available for 58 cases, while only one matching non-exposed athlete (24M, 8F) was available for 32 cases. Thirty-nine of the exposed athletes were classified as starters (23M, 16F), while the remaining 51 cases were classified as reserves (42M, 9F). Athletes were followed for an average of 80 days (Range = 35 – 90, SD = 15) due to 38 of the exposed athletes being returned to play less than a full 90 days due to the end of the season. The average period for return to play after concussion was 9 days (SD = 7).
The incidence of sustaining the outcome of interest (first time-loss lower extremity musculoskeletal injury) during the follow-up period was significantly higher in exposed athletes (45/90 or 50%), compared to non-exposed athletes (30/148 or 20%) (p < 0.01). A list of injuries observed in the athletes can be found in Table 2. Using univariate conditional logistic regression analysis, the odds of sustaining a lower extremity musculoskeletal injury was 3.39 times higher in exposed athletes compared to non-exposed (OR = 3.39; 95% CI = 1.90, 6.05; p < 0.01). Median time lost after a lower extremity musculoskeletal injury was not significantly different between exposed athletes (9 days; range 1 – 261), compared to non-exposed athletes (15 days; range 3 – 213) (p = 0.41).
TABLE 2.
Number of Athlete Injuries
| Anatomic Location | Injury Type | Concussed (N=45) |
Non-concussed (N = 30) |
|---|---|---|---|
| Hip | |||
|
| |||
| Flexor Strain | 2 | 1 | |
| Adductor Strain | 3 | 0 | |
| Thigh | |||
|
| |||
| Hamstring Strain | 6 | 6 | |
| Quadriceps Strain | 2 | 2 | |
| Knee | |||
|
| |||
| ACL Rupture | 3 | 2 | |
| MCL Sprain | 4 | 3 | |
| Meniscus Injury | 1 | 2 | |
| Popliteus Strain | 1 | 0 | |
| Leg | |||
|
| |||
| Peroneal Strain | 1 | 0 | |
| Ankle | |||
|
| |||
| Ankle Sprain | 18 | 13 | |
| Foot | |||
|
| |||
| Midfoot Sprain | 3 | 0 | |
| Toe Sprain | 1 | 1 | |
Secondary analyses were also performed by sex and starting status. Among male athletes, the odds of sustaining a lower extremity musculoskeletal injury was 3.72 times higher in athletes with concussion, (OR = 3.72; 95% CI = 1.84, 7.54; p < 0.01) whereas in female athletes, the odds of sustaining a lower extremity musculoskeletal injury was 2.75 times higher in athletes with concussion (OR = 2.75; 95% CI = 0.98, 7.69; p = 0.05). With respect to starting status, the odds of sustaining a lower extremity musculoskeletal injury was 2.84 times higher in athletes with concussion (95% CI = 1.20, 6.71; p < 0.01), whereas among reserves, the odds of sustaining a lower extremity musculoskeletal injury was 3.90 times higher in athletes with concussion (OR = 3.90; 95% CI = 1.78, 8.54; p < 0.01).
Discussion
We hypothesized that athletes who had been exposed to a concussion would be at higher odds for sustaining an in-season time-loss lower extremity musculoskeletal injury after return to play compared to matched non-exposed athletes. The study results indicated statistically significant odds of 3.39 for sustaining a lower extremity musculoskeletal injury in the concussed athletes, thus confirming the hypothesis. The main strength of this investigation is that it was designed as a historical cohort study, where exposed and non-exposed athletes to concussion were matched by sport, position played, and starting status and followed in a prospective fashion. These results support previous studies which demonstrated an increased risk of musculoskeletal injury in players with a history of concussion [13–17]; however, as previously noted, three of these studies are limited in part by lacking controls for participation rates [13–15] and lacking a definitive temporal relationship between concussion and injury [15]. Hence, the results of this study add particular strength to the current literature as our study design controlled for both participation (in terms of starting status and position played) and established a clear temporal relationship between concussion and any subsequent lower extremity musculoskeletal injury. The studies by Lynall et. al. and Brooks et. al. also had similar features with respect to participation, with the latter being very similar in terms of design, follow-up, and statistical analysis. The odds ratio of 3.39 for the current study is high in comparison to Brooks et. al. (OR = 2.48). This could be due to differences in reporting injuries among players, institutional differences accounting for or defining time-loss, and/or difference in style of play or coaching (e.g. more/less contact practices and hitting drills).
We also hypothesized that the severity of injuries experienced would be greater in the athletes who had experienced a concussion. As the median number of days lost in training after sustaining a lower extremity musculoskeletal injury was not significantly different between the two groups, this hypothesis was rejected. The study size potentially limited our ability to test this hypothesis as the incidence of particularly severe injuries such as ACL ruptures was limited. Study designs featuring much larger sample sizes are needed to provide sufficient power to compare groups based on particular injury types and severities.
Although the number of females was limited relative to the males, this study is the first to our knowledge to report increased odds for sustaining an in-season time-loss lower extremity musculoskeletal injury after return to play from concussion specifically for female athletes. Previous studies have either been limited to male athletes [13, 15] or have used a mixed-sex cohort without reporting sex-specific risk [16]. Our results demonstrated an odds ratio for a lower extremity musculoskeletal injury of 2.75 for exposed female athletes compared to matched non-exposed female athletes, which was lower than the 3.72 odds ratio demonstrated by male athletes; however, the number of female athletes in this study was relatively limited and the study design was not adequate to make direct sex-based comparisons. We speculate that differences in the magnitude of the odds ratios between the sexes may be a function of sport played (football for males vs soccer, lacrosse, and basketball for females). Further research is needed to better characterize any differences in lower extremity musculoskeletal injury risk after concussion based on athlete sex. Care should be taken to make sex-based comparisons within sports using similar styles of play (e.g. soccer) as opposed to those using dissimilar styles of play (e.g. lacrosse).
The finding of an increased risk of musculoskeletal injuries after concussion may be due to persistent subclinical effects of concussion. Neuromuscular control may be directly impaired secondary to reduced excitability of the motor cortex. Prior studies on concussed athletes have noted reduced maximal voluntary muscle activation, motor evoked potential amplitude, and intra-cortical facilitation, as well as increased intracortical inhibition and motor evoked potential latencies [18–20]. Such alterations have been noted to potential persist well past the point of symptomatic resolution [21–23]. Maintaining optimal force-generating capacity throughout athletic activity is likely to be beneficial in reducing injury risk and improving functional performance. Altered motor cortex excitability has been observed in populations with a history of ACL injury, chronic ankle instability, and low back pain, and may be correlated with neuromuscular control and subject functionality [24–27]. In light of this evidence, it is possible that the elevated risk for lower extremity musculoskeletal injury observed in the concussed athletes may be mediated through changes in motor cortex function.
This increased risk may also be caused by persistent alterations in neurocognition. Athletes with low neurocognitive performance may not able to interpret environmental cues or anticipate the actions of opponents. This may inhibit their ability to create appropriate neuromuscular responses to perform an athletic maneuver in a safe manner, successfully dodge an opponent, or brace for a collision, thus leading to an elevated risk of injury [28]. Indeed, athletes who have experienced ACL injuries have previously been found to demonstrate significantly worse performance across all testing domains on a pre-season computer-based neurocognitive testing program compared to non-injured matched control athletes [29]. Poor reaction time on a pre-season computer-based neurocognitive test has also been demonstrated to be predictive of lower extremity strains and sprains in college football players [30].
A similar relationship may be playing a role in the relationship between concussion and subsequent musculoskeletal injury risk. Studies have indicated that there may be neurocognitive deficits from concussion that persist past the point of return to play [31, 32] that current clinical neurocognitive assessments may not be able to detect under current standard testing protocols [33, 34]. Similarly, there is a growing body of evidence that persistent neuromuscular performance impairments are present in concussed athletes during relatively simple gait tasks; furthermore, these impairments are more prominent when a concomitant dual-attention cognitive task is employed [3–9]. Although the criteria for return to play for athletes in this study and at many institutions include a return to baseline neurocognitive and balance measures, it is possible that subtle neurocognitive and neuromuscular impairments were present at the time of return to play. These neurocognitive and neuromuscular deficits are likely subtle and not easily detected with current assessment strategies, yet they may have a significant clinical impact on subsequent injury risk as such deficits are likely to be magnified with more challenging athletic tasks [28]. Hence, these deficits may create a “window of susceptibility” to musculoskeletal injury following return to play after concussion.
The duration of this “window of susceptibility” to musculoskeletal injury is not well understood. It is interesting to note that the rate of injuries sustained after concussion as viewed by the approximate slope of the line in the survival plot (Figure 1) remained relatively constant through the 90 day follow-up period. This implies that the magnitude of risk for a musculoskeletal injury was similarly constant throughout this period, and suggests that the increased risk for injury may extend well beyond the 90 day follow-up period used in this study. This is in contrast to Cross et. al. who noted significantly shorter time to injury following return to play in concussed athletes (mean 53 days) compared to non-concussed athletes (mean 114 days) with a resulting curvilinear survival analysis plot [14]. On the other hand, Nordstrom et.al. noted a time-dependent elevation in risk of injury out to twelve months after a concussion, whereas Lynall et. al. detected a difference in injury risk between concussed and non-concussed athletes over 365 days but not over 90 or 180 days [13, 16]. This underscores the need to gain a better understanding of the duration of this elevated risk of injury and factors which may modify the magnitude of this effect.
FIGURE 1.
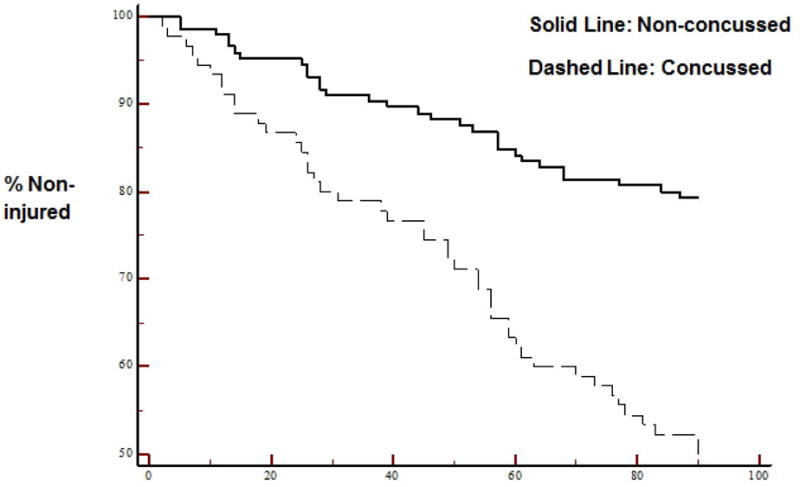
Distribution of Injuries Over Time
The results of the current study may have implications for current practice standards regarding the evaluation and management of concussion. The presence of this “window of susceptibility” to musculoskeletal injury following concussion implies that current return to play guidelines may not be sufficient as currently designed to protect athletes from potential significant post-concussion sequelae. Musculoskeletal injury risk may need to be an item of consideration in the development of future guidelines. Current clinical tools may also be insensitive at detecting meaningful post-concussion deficits, or provide insufficient coverage of possible domains of effect (such as neuromuscular function). Continued development of clinical tests, potentially including novel testing paradigms incorporating measures of neuromuscular control, may be required to adequately assess athletes for suitability for return to play. Finally, post-concussion rehabilitation strategies may also need to be altered to account for this relationship. This may include incorporating aspects of neuromuscular-based injury prevention strategies that have been used with evidence of success for reducing the risk of injuries such ankle sprains and ACL ruptures [35–37].
Limitations
The current study is not without its limitations. The data was collected at a single institution, which may limit the overall generalizability of the results. The study utilized historical data in a prospective design with a relatively small sample size. As such, comparisons of subsequent injury risk based on injury type or comparisons by sport or position were not feasible. The study also used a relatively short duration of observation after concussion injury, which limits our understanding of the possible duration of this increased risk of injury. Similarly, it is possible that this window of susceptibility has a very long duration, and as such our exclusion criteria of concussion within the prior six months may not be of sufficient duration. The duration of observation after return to play was not completely uniform across all athletes, with some cases censored short of the full 90 days due to the end of the season studied; however, this would likely reduce the magnitude of the difference in injury risk between the groups.
Any effects of a history of prior lower extremity injury were not included in the current analysis. This decision was made due to multiple factors. One, we had a lack of reliable information on pre-collegiate injury history. There was also a lack of consensus on what would qualify as a meaningful prior injury history both in terms of the injury experienced and the historical timeframe for inclusion given our limited sample size and the breath of reported injuries. In light of these issues, prior injury history was not included in the analysis; however, we attempted to control for this factor in part by limiting our analysis to the first musculoskeletal injury experienced during the 90 day follow-up period. it is possible that our findings are somewhat amplified relative to these studies due to this missing factor, and future studies utilizing large sample sizes should certainly take this possible confounding factor into account.
Although the data was from a single institution with a single training protocol for injury documentation, it is possible that there were differences in injury documentation and reporting among the training room staff using the medical record system. There is a risk that athletes were misclassified as being exposed or non-exposed to concussion; however, due to the fact that all concussions were diagnosed by a sports medicine fellowship-trained physician, we feel it is unlikely that exposed athletes were misclassified. On the other hand, in light of the well-documented under-reporting of concussion symptoms among athletes we feel it is likely that some non-exposed athletes were potentially misclassified; the effect would likely result in a underestimation of the odds of experiencing a lower extremity musculoskeletal injury after concussion.
Conclusions
Athletes who have experienced a concussion are at an elevated risk for lower extremity musculoskeletal injury within the first 90 days after return to play. Future research is warranted to determine the duration of this risk; factors such as age, sport, or gender which may modify this risk; and methods by which this risk may be mitigated.
Key Points.
Athletes who experience a concussion may be at elevate risk for experiencing a lower extremity musculoskeletal injury after return to play.
This risk of lower extremity musculoskeletal injury may be elevated in both male and female athletes.
The duration of this elevated risk for lower extremity musculoskeletal injury is currently unknown and may extend beyond the end of the season during which the concussion occurred.
Acknowledgments
This study was supported in part by the National Institutes of Health grant #5K12HD001097-17.
Footnotes
Ethical Approval
This study was approved by the University of Florida Institutional Review Board. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest Statement
Daniel Herman, Debi Jones, Ashley Harrison, Michael Moser, Susan Tillman, Kevin Farmer, Anthony Pass, Jay Clugston, Jorge Hernandez, and Terese Chmielewski declare that they have no conflict of interest.
References
- 1.Daneshvar DH, et al. The epidemiology of sport-related concussion. Clin Sports Med. 2011;30(1):1–17, vii. doi: 10.1016/j.csm.2010.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–8. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Buckley TA, et al. Altered gait termination strategies following a concussion. Gait Posture. 2013;38(3):549–51. doi: 10.1016/j.gaitpost.2013.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chiu SL, Osternig L, Chou LS. Concussion induces gait inter-joint coordination variability under conditions of divided attention and obstacle crossing. Gait Posture. 2013 doi: 10.1016/j.gaitpost.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 5.Fait P, et al. Alterations to locomotor navigation in a complex environment at 7 and 30 days following a concussion in an elite athlete. Brain Inj. 2009;23(4):362–9. doi: 10.1080/02699050902788485. [DOI] [PubMed] [Google Scholar]
- 6.Fait P, et al. Altered integrated locomotor and cognitive function in elite athletes 30 days postconcussion: a preliminary study. J Head Trauma Rehabil. 2013;28(4):293–301. doi: 10.1097/HTR.0b013e3182407ace. [DOI] [PubMed] [Google Scholar]
- 7.Catena RD, van Donkelaar P, Chou LS. Cognitive task effects on gait stability following concussion. Exp Brain Res. 2007;176(1):23–31. doi: 10.1007/s00221-006-0596-2. [DOI] [PubMed] [Google Scholar]
- 8.Catena RD, van Donkelaar P, Chou LS. Altered balance control following concussion is better detected with an attention test during gait. Gait Posture. 2007;25(3):406–11. doi: 10.1016/j.gaitpost.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 9.Catena RD, van Donkelaar P, Chou LS. Different gait tasks distinguish immediate vs. long-term effects of concussion on balance control. J Neuroeng Rehabil. 2009;6:25. doi: 10.1186/1743-0003-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Martini DN, et al. The chronic effects of concussion on gait. Arch Phys Med Rehabil. 2011;92(4):585–9. doi: 10.1016/j.apmr.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 11.Hewett TE, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 12.Zazulak BT, et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123–30. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 13.Nordstrom A, Nordstrom P, Ekstrand J. Sports-related concussion increases the risk of subsequent injury by about 50% in elite male football players. Br J Sports Med. 2014;48(19):1447–50. doi: 10.1136/bjsports-2013-093406. [DOI] [PubMed] [Google Scholar]
- 14.Cross M, et al. Professional Rugby Union players have a 60% greater risk of time loss injury after concussion: a 2-season prospective study of clinical outcomes. Br J Sports Med. 2015 doi: 10.1136/bjsports-2015-094982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pietrosimone B, et al. Concussion Frequency Associates with Musculoskeletal Injury in Retired NFL Players. Med Sci Sports Exerc. 2015 doi: 10.1249/MSS.0000000000000684. [DOI] [PubMed] [Google Scholar]
- 16.Lynall RC, et al. Acute Lower Extremity Injury Rates Increase following Concussion in College Athletes. Med Sci Sports Exerc. 2015 doi: 10.1249/MSS.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 17.Brooks MA, et al. Concussion Increases Odds of Sustaining a Lower Extremity Musculoskeletal Injury After Return to Play Among Collegiate Athletes. Am J Sports Med. 2016;44(3):742–7. doi: 10.1177/0363546515622387. [DOI] [PubMed] [Google Scholar]
- 18.De Beaumont L, et al. Persistent motor system abnormalities in formerly concussed athletes. J Athl Train. 2011;46(3):234–40. doi: 10.4085/1062-6050-46.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Livingston SC, et al. A preliminary investigation of motor evoked potential abnormalities following sport-related concussion. Brain Inj. 2010;24(6):904–13. doi: 10.3109/02699051003789245. [DOI] [PubMed] [Google Scholar]
- 20.Powers KC, Cinelli ME, Kalmar JM. Cortical hypoexcitability persists beyond the symptomatic phase of a concussion. Brain Inj. 2014;28(4):465–71. doi: 10.3109/02699052.2014.888759. [DOI] [PubMed] [Google Scholar]
- 21.De Beaumont L, et al. Brain function decline in healthy retired athletes who sustained their last sports concussion in early adulthood. Brain. 2009;132(Pt 3):695–708. doi: 10.1093/brain/awn347. [DOI] [PubMed] [Google Scholar]
- 22.Pearce AJ, et al. The long-term effects of sports concussion on retired Australian football players: a study using transcranial magnetic stimulation. J Neurotrauma. 2014;31(13):1139–45. doi: 10.1089/neu.2013.3219. [DOI] [PubMed] [Google Scholar]
- 23.Tallus J, et al. Long-lasting TMS motor threshold elevation in mild traumatic brain injury. Acta Neurol Scand. 2012;126(3):178–82. doi: 10.1111/j.1600-0404.2011.01623.x. [DOI] [PubMed] [Google Scholar]
- 24.Kuenze CM, et al. Persistent neuromuscular and corticomotor quadriceps asymmetry after anterior cruciate ligament reconstruction. J Athl Train. 2015;50(3):303–12. doi: 10.4085/1062-6050-49.5.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pietrosimone BG, Gribble PA. Chronic ankle instability and corticomotor excitability of the fibularis longus muscle. J Athl Train. 2012;47(6):621–6. doi: 10.4085/1062-6050-47.6.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pietrosimone BG, et al. Quadriceps strength and corticospinal excitability as predictors of disability after anterior cruciate ligament reconstruction. J Sport Rehabil. 2013;22(1):1–6. doi: 10.1123/jsr.22.1.1. [DOI] [PubMed] [Google Scholar]
- 27.Tsao H, Galea MP, Hodges PW. Reorganization of the motor cortex is associated with postural control deficits in recurrent low back pain. Brain. 2008;131(Pt 8):2161–71. doi: 10.1093/brain/awn154. [DOI] [PubMed] [Google Scholar]
- 28.Herman DC, et al. Effect of neurocognition and concussion on musculoskeletal injury risk. Current Sports Medicine Reports. 2015;14(3):194–9. doi: 10.1249/JSR.0000000000000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Swanik CB, et al. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. Am J Sports Med. 2007;35(6):943–8. doi: 10.1177/0363546507299532. [DOI] [PubMed] [Google Scholar]
- 30.Wilkerson G. Neurocognitive reaction time predicts lower extremity sprains and strains. International Journal of Athletic Therapy & Training. 2012;17(6):4–9. [Google Scholar]
- 31.Moore RD, Hillman CH, Broglio SP. The persistent influence of concussive injuries on cognitive control and neuroelectric function. J Athl Train. 2014;49(1):24–35. doi: 10.4085/1062-6050-49.1.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moore RD, et al. The persistent influence of pediatric concussion on attention and cognitive control during flanker performance. Biol Psychol. 2015;109:93–102. doi: 10.1016/j.biopsycho.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 33.McGrath N, et al. Post-exertion neurocognitive test failure among student-athletes following concussion. Brain Inj. 2013;27(1):103–13. doi: 10.3109/02699052.2012.729282. [DOI] [PubMed] [Google Scholar]
- 34.Tsushima WT, et al. Effects of Two Concussions on the Neuropsychological Functioning and Symptom Reporting of High School Athletes. Appl Neuropsychol Child. 2014:1–5. doi: 10.1080/21622965.2014.902762. [DOI] [PubMed] [Google Scholar]
- 35.Dai B, et al. Prevention of ACL injury, part II: effects of ACL injury prevention programs on neuromuscular risk factors and injury rate. Res Sports Med. 2012;20(3–4):198–222. doi: 10.1080/15438627.2012.680987. [DOI] [PubMed] [Google Scholar]
- 36.Sadoghi P, von Keudell A, Vavken P. Effectiveness of anterior cruciate ligament injury prevention training programs. J Bone Joint Surg Am. 2012;94(9):769–76. doi: 10.2106/JBJS.K.00467. [DOI] [PubMed] [Google Scholar]
- 37.Verhagen EA, Bay K. Optimising ankle sprain prevention: a critical review and practical appraisal of the literature. Br J Sports Med. 2010;44(15):1082–8. doi: 10.1136/bjsm.2010.076406. [DOI] [PubMed] [Google Scholar]


