Abstract
Depression is one of the most prevalent mental health challenges in low- and middle-income countries. However, the mechanisms of parental depression on children’s development are understudied in these countries. This study examined the prevalence of parental depression, contextual predictors of parental depression, and the associations between parental depression, parenting and children’s development in one of the Sub-Saharan African countries-Uganda. Three hundred and three Ugandan parents of young children were recruited and interviewed. Results indicated that about 28 % of parents were depressed. Contextual factors such as low educational attainment, food insecurity, low social support, and high number of children were associated with parental depression. Structural equation modeling also indicated that Ugandan parents’ depression was associated with less optimal parenting, and higher problem behavior, lower social competence, and poorer physical health and school functioning in children. Results provide several cross cultural consistency evidence in associations among parental depression, parenting, and child development.
Keywords: Parental depression, Parenting, Child mental health, Uganda, Sub-Saharan Africa, Low- and middle-income country
Introduction
Adult depression, including major depression and post-partum depression, is a major public health challenge throughout the world [1]. Studies show that the prevalence of depression (i.e., maternal depression) varies by country, with prevalence of 10–15 % in high-income countries (HICs) [2] and 15–57 % in low- and middle-income countries (LMICs) [3–5]. Depression can lead to a host of negative consequences, resulting in a huge burden in population health [6]. Adult depression also has a significant negative impact on the child population, as many adults struggling with depression are parents and caretakers. It is well-documented that parental depression has a detrimental impact on parenting, family functioning, parent–child relationships, and children’s physical, social and behavioral health, and cognitive functioning [3, 7–9]. However, while such epidemiological and developmental research is well-known in HICs, studies on the impact of parental depression are limited in parents and children in Sub-Saharan African (SSA) countries, such as Uganda, where the effects of poverty and limited resources are rampant and likely to exacerbate parental depression and its negative correlates. To effectively address the child physical and mental health burden in African countries, a better understanding of the etiology and influence of contextual factors is needed to inform the development of culturally sensitive interventions and services.
Global research on the prevalence of parental depression and the association with child health and development has primarily focused on mothers [10]. In addition, most maternal depression research has focused on the postnatal period during the first 2 years after child’s birth, and less has focused on the broader early childhood period. Although studies conducted in HICs have documented that maternal depressive symptoms decreased 1 month after childbirth to a very similar level assessed at subsequent time periods (i.e., 6, 24, 36 months after childbirth) [7], information on the patterns of maternal and paternal depression in the post-infancy period is lacking in SSA countries. Given the high rates of poverty, food insecurity, domestic violence, and health problems in SSA countries, it is possible that the etiology of parental depression varies by country and region, and deserves nuanced study.
Several risk factors have been identified for parental depression, and risk factors findings were generally consistent across LMICs and HICs [3, 5, 11–13]. For example, a review of 24 international studies, including those conducted in the country of focus in this study, Uganda, identified that poverty, economic stress, low social support, domestic violence, low parental education, poor parental health, poor child health, child gender (e.g., female child in a culture where there is a strong preference for male children), and large number of young children at home are risk factors for parental depression [3]. A separate review of 47 studies on LMIC replicated most of these findings and identified additional risk factors for parental depression, such as young parental age, history of mental health problems, single marital status, child birth complications, and poor child health [5]. Overall, these studies were primarily based on mothers and families with preschool age children.
In investigating the impact of parental depression on children, numerous review studies based on HICs and LMICs have documented the direct association between parental depression and a range of adverse child behavioral, emotional, cognitive, and physical health outcomes [3, 14–16]. In a more comprehensive approach of investigating mechanisms, empirical evidence has supported that mothers who are depressed are more likely to show decreased sensitivity with children, lower responsiveness, more intrusive and controlling parenting, poorer monitoring of child health needs, and experience poorer quality of parent–child interactions and lowered parental self-efficacy [4, 7, 17–20]. Subsequently, these negative parenting outcomes were related to poorer child emotion regulation abilities, adaptive skills, and increased mental health problems [7, 18, 21]. These findings suggest a mediation mechanism that parental depression impacts child outcomes through its negative influence on parenting. Although some of these studies were conducted in SSA countries, most research in this region focuses on the impact of maternal depression on child physical growth, such as stature or weight [16], but few studies in SSA have focused on children’s mental health or school functioning outcomes, mechanism testing, or in samples that include school-age children.
Building on the vast literature on adult depression, the current study investigates prevalence of parental depression (considering both male and female caregivers) and the links between parental depression, parenting and school-age child outcomes in Ugandan families. This study was guided by the Family Stress Model [21–24], which posits that the stress of poverty and environmental-related pressure influences parents’ level of emotional distress (e.g., depression), which negatively impacts parenting, and in turn, adversely impacts child outcomes. Three related research questions were tested: (1) What are the patterns of parental depression in Ugandan families? (2) What are the family demographic predictors (i.e., marital status, religion, parental age, child gender, child age) for parental depression? We examined these factors because they have not yet been systematically studied in Ugandan caregivers. (3) Is parental depression related to parenting and child outcomes (i.e., child physical, mental health, and school functioning), and whether the link between parental depression and child outcomes is mediated through parenting? We hypothesized that parental depression would be highly prevalent in Uganda, given its rates of widespread poverty and related stress. Social-demographic factors (e.g., food insecurity, social support, parental health) would predict parental depression. Furthermore, relative to non-depressed parents, parents with depression would use more negative parenting, characterized by using more harsh discipline, having more conflicted parent–child relationships, and being less involved in children’s education, which would be further related to their children’s suboptimal health status and school functioning.
Methods
Participants
Study participants included 303 Ugandan parents whose children attended primary schools. Study participants were recruited from two studies, including 149 families from a cross-sectional child development study that aimed to understand the influence of family stress on child development in a community sample, and 154 families from a school-based mental health intervention trial that aimed to improve teachers’ utilization of evidence-based behavioral management strategies in classrooms to promote child mental health [25]. For the intervention sample, teachers were the target of intervention, and only baseline data were utilized. In both studies, children were not the subject of the studies. Parents in both studies were defined as biological birth parents/primary caregivers (mothers or fathers) or non-birth adult primary caregivers who lived with target children and played a major caregiver role. Non-birth adult primary caregivers (i.e., grandparents, relatives) were recruited if the biological parents were not actively in the children’s lives (due to parental health, death, or different living arrangement). Because of our early childhood focus, parents of children enrolled in Nursery to Primary 3 were eligible for the study. Table 1 presents the demographic information on the study sample. About half of the families (48 %) reported having food insecurity (defined below). Most parents were female (82 %). Parents’ mean age was 35.92 years (SD = 9.80 years, range 18–79 years). About one-third of parents (32 %) were single, 65 % parents were mothers (11 % fathers and 24 % grandparents or relatives), and 48 % had educational attainment of primary school or less and 44 % had secondary or higher education. Study children were an average of 6.51 years old (SD = 1.08 years, range 4–9 years), 49 % were boys, and all were enrolled in Nursery to Primary 3 in Kampala, the capital city of Uganda.
Table 1.
Family demographic, parenting, and child functioning by depression status
| Demographic characteristics | Total Mean (SD) or (%) |
Depressed Mean (SD) or (%) |
Non-Depressed Mean (SD) or (%) |
OR (95 % CI) | p |
|---|---|---|---|---|---|
| Caregiver gender | |||||
| Male (ref) | 18.1 % | 9.3 % | 90.7 % | 4.52 (1.73, 11.79) | .001 |
| Female | 81.9 % | 31.6 % | 68.4 % | ||
| Caregiver types | |||||
| Birth primary caregiver (ref) | 76.5 % | 29.9 % | 70.1 % | .683 (.37, 1.28) | .146 |
| Non-birth primary caregivers | 23.5 % | 22.5 % | 77.5 % | ||
| Education status | |||||
| Primary or less | 47.7 % | 41.0 % | 59.0 % | 3.15 (1.81, 5.48) | <.001 |
| Non-standard | 8.3 % | 8.0 % | 92.0 % | 0.40 (.09, 1.79) | |
| Secondary or higher (ref) | 44.1 % | 18.0 % | 82.0 % | ||
| Marital status | |||||
| Single (ref) | 32.2 % | 33.3 % | 66.7 % | 0.69 (.41, 1.18) | .227 |
| Married or live with partner | 67.8 % | 25.7 % | 74.3 % | ||
| Employed | |||||
| Yes | 68.8 % | 24.1 % | 75.9 % | 0.63 (.37, 1.07) | .087 |
| No (ref) | 31.2 % | 33.7 % | 66.3 % | ||
| Food security (ref) | 51.5 % | 7.7 % | 49.7 % | <.001 | |
| Insecurity | 48.5 % | 49.7 % | 50.3 % | 11.84 (6.05, 23.18) | |
| Religion | |||||
| Muslim (ref) | 22.6 % | 22.1 % | 77.9 % | 1.12 (.53, 2.39) | .351 |
| Christian | 28.9 % | 24.1 % | 75.9 % | 1.84 (.92, 3.67) | |
| Catholic | 37.9 % | 34.2 % | 65.8 % | 1.45 (.55, 3.79) | |
| Other | 10.6 % | 29.0 % | 71.0 % | ||
| Number of household members | 6.41 (2.57) | 6.64 (2.61) | 6.32 (2.55) | – | .331 |
| Number of children < 18 years old | 3.79 (1.82) | 4.33 (2.11) | 3.58 (1.66) | – | .004 |
| Parental age | 35.92 (9.80) | 35.87 (9.92) | 35.94 (9.78) | – | .955 |
| Parental health | 2.58 (0.92) | 2.03 (0.91) | 2.79 (0.84) | – | <.001 |
| Social support | 4.00 (0.80) | 3.77 (0.90) | 4.09 (0.74) | – | .002 |
| Child gender | |||||
| Boy | 49.3 % | 27.1 % | 72.9 % | 1.07 (.64, 1.78) | .805 |
| Girl (ref) | 50.7 % | 28.4 % | 71.6 % | ||
| Child age | 6.51 (1.08) | 6.86 (1.16) | 6.38 (1.02) | – | <.001 |
| Parenting | |||||
| Belief about corporal punishment | 2.50 (1.05) | 2.80 (1.09) | 2.39 (1.02) | – | .002 |
| Harsh-inconsistent parenting | 1.80 (0.43) | 1.88 (0.46) | 1.77 (0.43) | – | .046 |
| Parent involvement in education | 4.09 (1.38) | 3.98 (1.62) | 4.12 (1.28) | – | .427 |
| Conflicted parent–child relationship | 2.36 (0.58) | 2.67 (0.57) | 2.24 (0.54) | – | <.001 |
| Child health and development | |||||
| Child health | 5.34 (1.24) | 4.48 (1.37) | 5.67 (1.01) | – | <.001 |
| Social competence | 2.38 (0.69) | 2.37 (0.69) | 2.39 (0.69) | – | .853 |
| Poor school functioning | 1.02 (1.33) | 1.34 (1.44) | 0.90 (1.26) | – | .010 |
| Total behavioral problems | 14.28 (5.35) | 16.54 (4.98) | 13.40 (5.24) | – | <.001 |
| Abnormal level of problem | |||||
| Yes | 33.3 % | 40.6 % | 59.4 % | 2.45 (1.46, 4.12) | .001 |
| No (ref) | 66.7 % | 21.8 % | 78.2 % | ||
Percentages (%) showed in the 1st column are demographic characteristics for the entire sample. Percentages showed in the 2nd and 3rd columns are % depressed and % non-depressed in each subgroup (e.g., male, female). OR (=Odds ratio) and p values are a result of the unadjusted association between categorical demographic predictors and depression (1 = yes, 0 = no). (ref) = reference group. N = 303 for the total sample, and N = 85 and 218 for depressed and non-depressed sample
Procedure
Participants were recruited between October 2013 and March 2014 from diverse communities located across 16 neighborhoods. Primary schools and communities were identified through a regional school list and non-governmental organization (NGO) network. About 15–25 families from each community/school were randomly selected and recruited through introduction of teachers or community guides (who work for NGOs or schools and know families in the designated community). Eligible primary care-givers/parents who agree to participate were provided with oral or written informed consent. For parents who were literate, a written consent was given, and a sign consent form was documented. For parents who were illiterate, an oral consent was given, and a literate witness (e.g., research staff, community guide) signed the consent form on behalf of the participant, which was then documented. After consent, parents were scheduled for an interview at home or in their child’s school. All data collection was conducted in a one-on-one interview format by a trained bachelor or master-level social science researcher. Consents and interviews were conducted in English (the official language in Ugandan schools) or Luganda (the primary local language) based on parents’ preference. The majority of the consents/interviews (>60 %) were conducted in Luganda, and the rest were conducted in English. Based on the parents’ preference, either the English or Luganda version of assessment package was used. Children did not participate in the evaluation. The study procedures and method of consent were approved by the Internal Review Boards of Makerere University College of Health Sciences (IRB Number: SBS132).
Measures
For parental depression, child behavioral outcomes and demographic/family functioning measures (available in English and Luganda), all have been validated with Ugandan population [26–28]. For parenting measures, we selected measures that have been used with diverse cultural groups from parenting literature [29–32]. The Luganda version of parenting assessments were translated based on the recommended method suggested in the literature (i.e., applying translation and back-translation, and using a team review approach to resolve any discrepancies between the versions and to determine whether the translated material is appropriate and meaningful for English and Luganda speakers) [33, 34]. We carefully examined the psychometric properties of each scale to ensure its reliability and validity in the present study sample, as describe below.
Parental Depression
The Patient Health Questionnaire (PHQ-9; 10 items; α = .83 using our Ugandan sample) [35, 36], a brief depression screening measure, was used for this study. PHQ-9 has been widely used in many countries and validated with Ugandan adults [26]. Parents rated 9 symptom items over the last 2 weeks on a 4-point scale (0 = not at all; 3 = nearly every day; sample item: “little interest or pleasure in doing things” “thoughts that you would be better off dead or of hurting yourself in some way”). The scale also includes an overall functioning rating that evaluates the level of functional impairment (0 = not at all difficult to function, 3 = extremely difficult to function). A total score was created for nine symptom items. PHQ-9 has been validated previously based on Ugandan samples [26, 27], using the Mini-International Neuropsychiatric Interview (MINI; a widely used short structured diagnostic interview for DSM-IV and ICD-10 psychiatric disorders) [37]. The clinical cut-off score of 10 has been suggested for the Ugandan population (with sensitivity of 0.91 and specificity 0.81). Individuals with a score of 10 or above would suggest a high likelihood of having a depressive disorder [26]. The 10 cut-off is compatible to the developers’ version, which defines 1–4: minimal depression, 5–9: mild depression, 10–14: moderate depression, 15–19: moderately severe depression, and 20–27: severe depression. For the purpose of this study, we defined a score of 10 or above as “depressed” and a score below 10 (1–9) as “non-depressed.” The dichotomized scale (or dummy variable) was used for analyses.
Parenting
Four measures were used to assess four areas of parenting. Constructs that had been identified as significant predictors for child development in the literature were targeted. The Parent–Child Relationship Scale [38] (12 items) measures Conflicted Parent–Child Relationship (e.g., child and I always seem to be struggling with each other) on a 5-point scale (1 = definitely does not apply; 5 = definitely applies). The Parenting Practices Interview (PPI) [39] assessed Harsh and Inconsistent Discipline (11 items; e.g., “how often do you slap or hit your child when he/she misbehaves,” “how often does your child manage to get around the rules you set”) on a 4-point scale (0 = never, 3 = Often). Both Parent–Child Relationship and Harsh and Inconsistent Discipline scales have been used with diverse ethnic populations in studies conducted in HICs, and showed adequate reliability in this Ugandan study sample (α = .72 and .66, respectively). Parent Involvement in Education was assessed using 2 items. Parents were asked to rate how often they help their child with school-type activities (e.g., reading or discussing a story together, working on a project together) on a 7-point scale (1 = never, 4 = a few times per month, 7 = everyday). They were also asked to rate the number of total hours they help their child with any education related activities (e.g., spend time talking about school activities, doing homework, reading together) in the last two school days (1 ≤ 0.5 h, 4 = 1.5–2 h, 7 = 3 or more hours). The two items were correlated (r = .23, p < .001); therefore, we combined the items into one scale. To consider information bias (e.g., potential under-report of harsh discipline use by parents), we also included the Attitude About Corporal Punishment scale (3 items; α = .78), which is a measure we developed for this study. This measure assesses parents’ attitude toward corporal punishment (e.g., in order to bring up a child properly, you need to physically punish your child) on a 5-point scale (1 = strongly disagree, 5 = strongly agree). This attitude scale considers a proxy measure for parental use of corporal punishment (r = .14, p < .05).
Child Functioning
Four scales were used to assess child health and development. The Strengths and Difficulties Questionnaire (20 items) [40, 41], is a brief screening measure for child mental health problems including ratings of emotional symptoms, conduct problems, hyperactivity, and peer problems (e.g., “Often fights with other children or bullies them,” “Often unhappy, down-hearted or tearful”). The measure has been widely used for research purposes in the United States and other high and LMICs [42–46]. The parent version was used in this study. Parents responded in terms of how true each behavior was for their child on a 3-point scale (0 = not true, 2 = certainly true). A total difficulty sum score, ranging from 0–40, was created. A score of 0–13 is considered normal, a score of 14–16 is considered borderline, and a score of 17–40 is considered abnormal. In this Ugandan sample, internal consistency is adequate (α = .63), and about 33 % of children were rated to have abnormal levels of problem behaviors (relative to 6–7 % for the US 4–10 year olds using the same measure) [47]. The Social Competence Scale (12 items; e.g., “shares things with others,” “copes well with failure”; α = .80 for Ugandan sample) [48, 49], evaluates children’s positive social behaviors, including emotion regulation, prosocial behaviors, and communication skills. Parents were asked to rate how well the statements describe their child on a 5-point scale (0 = not at all to 4 = very well). Child Health was measured with two global items. Parents were asked to rate their overall perception of their child’s health on a 4-point scale (1 = poor health; 4 = very good or excellent health) and their perception about their child’s tendency to get physical illness on a 3-point scale (1 = certainly true, 3 = not true). Both items are statistically significantly related (r = .52; α = .68); therefore, we created a sum score. A higher score indicates good health. The Child School Functioning scale (3 items; α = .52), developed for this study, measures children’s difficulty in school (i.e., lacks motivation/enjoyment in going to school, complains about school, and has trouble with school grades). Parents were asked to rate these behaviors on a 3-point scale (1 = not true, 3 = certainly true), and a sum score was then created; a higher score indicates poor school functioning.
Additional test–retest reliability (for a subsample of 42 families) and concurrent validity (assessed with correlations) among key study constructs were examined. Test-test reliability (assessed 6 month apart using Pearson correlations) show adequate reliability for the parenting measures (rs for 4 measures ranged from .36 to .59) and child functioning measures (rs for 4 measures ranged from .36 to .50) Inter-correlations within domains (i.e., parenting, child outcomes) and across domains were also correlated in expected directions (see Table 2), suggesting support of concurrent and construct validity of study measures for use in Uganda. For example, harsh/inconsistent parenting, value of corporal punishment, and conflicted parent–child relationship were related to poor child physical health, school functioning and higher problem behavior. Better child health was related to fewer problem behaviors and higher social competence. Higher parental attitude about corporal punishment and harsh/inconsistent discipline were associated with higher conflicted parent–child relationship.
Table 2.
Correlations among study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Depression | – | |||||||
| Parenting | ||||||||
| 2. Corporal punishment | .18** | – | ||||||
| 3. Harsh/Inconsistent | .12* | .14* | – | |||||
| 4. Conflicted P–C relationship | .34*** | .30*** | .16** | – | ||||
| 5. P-Involvement in education | −0.05 | .00 | 0.03 | −0.05 | – | |||
| Child outcomes | ||||||||
| 6. Child physical health | −0.44*** | −0.24*** | −0.11* | −0.27*** | .15** | – | ||
| 7. Social competence | −0.01 | −0.06 | −0.02 | −0.07 | 0.01 | 0.23*** | – | |
| 8. Problem behavior | .26*** | .27*** | .28*** | .36*** | −0.07 | −0.30*** | −0.24*** | – |
| 9. Poor school functioning | .15* | .15** | .13* | .22*** | −0.01 | −0.11* | −0.12* | 0.31*** |
P–C = Parent Child. Corporal punishment = attitude about corporal punishment.
p < .05.
p < .01.
p < .001
Demographics
To consider demographic predictors of parental depression and potential confounders, parent education, employment status, household size, religion, food insecurity, parental health, and social support were included. Categories for parental education, employment status, and religion (including the reference categories) are specified in Table 1. Religious groups were considered because of the diverse religious background in Uganda, and their potential impact on psychological well-being in both adults and children. Food insecurity (3 items; α = .85 for the study sample) was assessed using the Household Hunger Scale [50], which evaluates family food resources and hunger status over the past 4 weeks on a yes/no dichotomized scale (e.g., no food to eat because of lack of resources to purchase food; any household member going to sleep at night hungry, any household member going a whole day and night without eating anything at all because there was not enough food in the home). If any food resource or hunger issue was reported (or the sum score equal or above 1), the family would be grouped into the food insecure group. Parental health was assessed based on parent perception of overall health and quality of life (2 items; α = .84 for the study sample) on a 5-point scale (1 = poor, 5 = excellent). Social Support (4 items; α = .85 for the study sample) was evaluated using the Multidimensional Scale of Perceived Social Support [51, 52]. The scale evaluates perceived support for comfort, sharing emotion, and needing help on a 5-point scale (1 = strongly disagree, 5 = strongly agree).
Analyses
To study prevalence of parental depression, a series of descriptive analyses were conducted. We evaluated prevalence of depression by parents’ gender and family contexts (i.e., marital status, religion, parental age, child gender, child age). For child age, we examined prevalence by 4 age groups (for age 5, 6, 7, and 8 groups, excluding age 4 and 9 groups because of samples smaller than 10 in these two age groups). To study predictors of parental depression, we used multiple logistic regression analysis and examined a set of potential socio-demographic predictors. To study the associations between parental depression and parenting and child functioning, we applied structural equation modeling (SEM), allowing for (a) meditational links from parental depression status to parenting to child functioning, (b) variables within each domain (i.e., parenting, child functioning) to be correlated; and (c) adjusting for potential confounders (i.e., parent gender, education and health, food insecurity status, number of children in the family, child age). The SEM model was tested using MPLUS 6 [53] and maximum likelihood estimation method (ML). To judge the closeness of fit of the hypothesized association model, three indices were used as recommended by Muthén & Muthén [53]: Chi square (χ2 > .05 or χ2/df ratio < 3.0), root mean square error of approximation (RMSEA <.08), and comparative fit index (CFI > .95).
Results
Prevalence of Parental Depression and Predictors
The overall estimated prevalence of parental depression (based on the clinical cut-off of 10 identified in Ugandan adults) was 28 % in this sample. Among the depressed group of parents, 65 % (or 18 % of the study population) reported high levels of functioning impairment (very difficult or extremely difficult to function). The prevalence of parental depression was higher among families who reported food insecurity compared to those without food insecurity (50 vs. 8 %, OR = 11.84, p <.001); among female parents compared to male parents (32 vs. 9 %, OR = 4.52, p = .001); and among less educated parents compared to those higher educated parents (41 % for primary or less education vs. 18 % for secondary or higher education, OR = 3.15, p < .001) (also see Table 1). In understanding whether the likelihood of parental depression varies by child age, we found an increased likelihood of parental depression by child age (26 %, 17 %, 30 %, 44 % among families with age 5, 6, 7, and 8 years old children, respectively, p <.002).
To consider demographic predictors for parental depression, we carried out multiple logistic regression analyses by including a set of demographic predictors that were shown to be different between depressed and non-depressed groups in Table 1 (7 predictors were included). We found after adjusting for other demographic factors, 6 of the 7 demographic predictors (caregiver gender, education, food insecurity, number of children, parental health, and child age) were significant predictors for parental depression, except for social support.
Parental Depression and Associations with Parenting and Child Functioning
We compared parenting and child functioning differences between depressed and non-depressed parents. Mean differences, without adjusting for demographic factors, are shown in the bottom of Table 1. Unadjusted correlations between parental depression and parenting and child outcomes are shown in Table 2 (1st column). As hypothesized, we found that depressed parents were more likely to believe in the use of corporal punishment as an effective parenting strategy, more likely to use harsh/inconsistent parenting, and reported more conflicted parent–child relationships than non-depressed parents. Similarly, children of depressed parents showed poorer physical health, more school problems, and more behavioral problems than children of non-depressed parents.
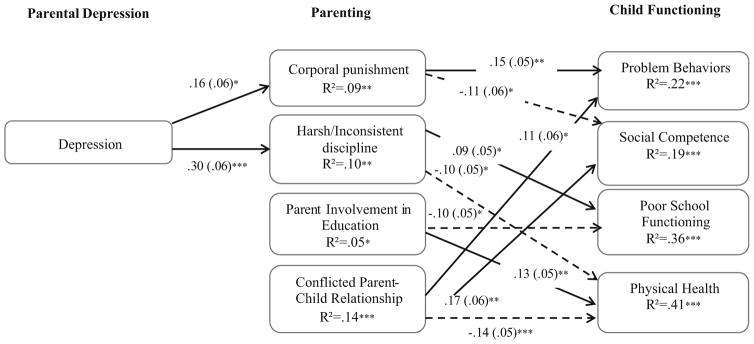
To test mediation mechanisms (examining whether the influence of parental depression on child health/development is through parenting mediators), we conducted SEM (see Fig. 1). To consider potential confounders, we carried out adjusted SEM that controlled for six demographic covariates (caregiver gender, education and health, family food insecurity, number of children in the family and child age). SEM results showed support of our conceptual model. The overall χ2 statistics showed a reasonable fit of the model, χ2 (4) = 10.31, p = .04 (χ2/df ratio = 2.6), RMSEA = .07 (95 % CI .02, .13) and CFI = .99. Figure 1 presents the standardized path coefficients for the significant paths and the R2 values for each endogenous variable (parenting, and child functioning). We found that after adjusting for demographic confounders, parental depression was associated with attitudes about corporal punishment and use of harsh and inconsistent discipline; and that harsh and inconsistent parenting practices were associated with higher levels of child problem behaviors, lower social competence, and poor school functioning and physical health. Parental depression and four parenting constructs considered in this study explain 19–42 % of variance of child outcomes. Although the SEM did not show direct association between parental depression and parental involvement or parent–child relationship, both parenting measures were related to child functioning in expected ways, with one exception. We found that high parental involvement was associated with better child school functioning and physical health, and a conflicted parent–child relationship was associated with high child problem behaviors and poorer physical health. Unexpectedly, having a conflicted parent–child relationship was associated with higher child social competence in the adjusted SEM model. In the non-adjusted analysis (Table 2), this association was not significant.
Fig. 1.
Structural equation modeling for association among parental depression, parenting, and child functioning
Discussion
This study extends the parental depression literature in low-income and high-risk populations. It is unique in that it investigated patterns of depression in both male and female caregivers, in parents of school-age children, and in diverse community samples. This study also investigated associations of parental depression, parenting and child functioning in a SSA country (Uganda) with consideration of the overwhelming economic hardship and food insecurity in the country. Similar to the prevalence observed in the general Uganda population (9–24 %) [54, 55], we found approximately 30 % of Ugandan parents reported to have depression (with symptom scores above 10 clinical cut-off) and 20 % had functioning impaired depression. We also found differential prevalence by certain characteristics. Female caregivers, less educated parents, the presence of food insecurity, and having older children put parents at greater risk for struggling with depression. Similar to other studies of risk factors for depression in LMICs [3], parental education, health status, and economic hardship (as measured by food insecurity) were associated with levels of depression in expected ways. Findings of high depression prevalence and risk factors suggest that demographic determinants for adult depression maybe consistent across cultures or country’s economic context. Our findings also suggest that Ugandan families are in great need of a range of cost-effective family interventions to promote health family functioning and child development, and that these family interventions need to be extended beyond infancy to reach families of school-age children.
This study is one of few studies to examine the mediation mechanisms of parental depression on multiple domains of parenting and child outcomes and with school-age children in SSA countries. This is an important contribution because school-age children’s health and development research in SSA countries is scarce. Consistent with the Family Stress Model and findings reported in HICs, poverty related stress in Ugandan families was associated with increased risk of parental depression. Depressive symptoms were associated with negative parenting (including belief in the use of corporal punishment and practice of more harsh/inconsistent parenting), and these negative parenting practices/beliefs were associated with poor child physical, mental health and school functioning. Findings suggest cross-cultural and international consistency particularly regarding developmental mechanisms for optimal child health and development, and suggest that existing evidence-based family interventions used in HICs targeting similar parenting and child outcomes [32, 56] may be applicable in Uganda and other LMICs.
In the SEM mechanism testing, some unexpected findings emerged. We found that parental depression was not significantly associated with a conflicted parent–child relationship. Two reasons may explain this. It is possible that the structure of the living contexts and child care arrangements in Uganda are very different from developing countries. In our Ugandan sample, the family size tends to be big (i.e., average family size was six, average number of children in households was four) relative to what is normative in American samples (family size of 4, average 2 children). Additionally, other adult caregivers (i.e., relatives, spouse, or grandparent) or older children in the house may also share caregiving role. When the primary caregiver is depressed, it is likely that the child avoids interacting with the depressed caregiver and seeks for comfort from other secondary caregivers. Therefore, impacts of caregiver depression on parent–child relationship might be minimized or not be observed. Another possible reason for the unexpected direction of the finding is related to neighborhood context. In our sample, about half of our families (48 %) experienced the impact of low financial resources (suffered from food insecurity), and they were more likely to live in a single-room, crowded, and ill-equipped homes with no electricity or common living room spaces, and home are built quite close to one another. In such living conditions, children may be more likely spend more time outside of the house interacting with neighbors and extended family members living close by, and they tend to be cared by neighbors when parents are not available. Therefore, children of depressed parents might not be as negatively impacted by their parents’ sadness, detachment or emotional distance due to the depression. Another unexpected finding was a positive link between the conflicted parent–child relationship and child social competence. This reverse association may further support the hypothesis that living environments emphasizing collective impact and community more than individual needs may contribute to confounding effects that we have not included in the study. It is also possible that children with depressed parents benefit by learning nuances of interpersonal relationships and communication that actually expanded their abilities to relate to and socialize well with their peers. An adaptive copying strategy such as this would be more likely to be common in community societies like Uganda. Our unexpected findings highlights that mechanisms for parental depression and social competence in LMIC context are complex and require more systematic research.
This study has some limitations. First, it is based on a cross-sectional study design, and we therefore cannot exclude the potential for reverse causality. In addition, the measures were based solely on parental self-report, and parent self-report on only global items of child health. Estimation bias due to a single information source cannot be excluded, and caution for the interpretation of the results is warranted. It is possible that depressed parents may overstate their children’s problem behaviors or other aspects of behaviors [57, 58] as they are more likely to have a negative attribution bias, impacting their perceptions of their environment. However, studies have argued that although depressed parents may have more negative attributions about their children’s behaviors, to some extent, their report accurately reflects children’s function rather than a biased observation [7]. Evidence from cross-informant examinations suggests that evaluation from depressed parents can be still highly correlated with other informant’s observations [59]. Future studies should utilize data collected from multiple sources, including biological and/or objective parenting and child functioning measures, to fully understand the influence of depression on parenting and child functioning. Furthermore, the subsamples of families (e.g., small sample of depressed parents and for mothers/fathers/non-birth caregivers, representing n = 198, 34, 71) were not large enough to test mechanisms separately by subgroups, or for including many predictors simultaneously. Future studies should apply larger samples to explore the impact of parental depression on child physical and mental health for different subpopulations, examine similar relations in rural samples, and use a longitudinal design.
Summary
A body of research from HICs has documented the impact of parental depression on children, the mechanisms of parental depression on parenting and children’s health and development are understudied in LMICs. This study adds to the extant literature on families in LMIC and the Family Stress Model, providing evidence for some generalizability of this model in the international context. Specifically, this study identifies multiple stressors (e.g., parents with low educational attainment, in poor physical health, and families with food insecurity) and risk factors (e.g., harsh/inconsistent parenting, conflicted parent–child relationship) are related to lower levels of child health and development. This study also found some inconsistent findings. We found that not all negative parenting correlates (i.e., conflicted parent–child relationships) will result in similarly negative outcomes for children, as research evidence from developed countries generally supports. Our findings suggest more careful consideration of living contexts and influence of the dynamics of relationships in cultures that emphasize co-parenting and strong community relationships. Our findings have implications for prevention and the development and adaption of existing evidence-based programs for Ugandan children and families. Future research may focus on how to adapt existing evidence-based interventions to fit local community contexts and service settings.
Acknowledgments
Funding provided by National Institutes of Mental Health (1R21MH097115-01A1). We wish to acknowledge the generous participation of the schools, community leaders and parents; data collection assistance from Joy Gumikiriza, Diana Kalema, and Annet Kembabazi; and technical support from ChildFund Uganda and Child Protection in Crisis Network for Research, Learning and Action.
References
- 1.WHO. Closing the gap in a generation: health equity through action on the social determinants of health. Report from the commission on social determinants of health. 2008 doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 2.Wittkowski A, Gardner PL, Bunton P, Edge D. Culturally determined risk factors for postnatal depression in Sub-Saharan Africa: a mixed method systematic review. J Affect Disord. 2014;163:115–124. doi: 10.1016/j.jad.2013.12.028. [DOI] [PubMed] [Google Scholar]
- 3.Wachs TD, Black MM, Engle PL. Maternal depression: a global threat to children’s health, development, and behavior and to human rights. Child Dev Perspect. 2009;3:51–59. [Google Scholar]
- 4.Cooper PJ, et al. Post-partum depression and the mother-infant relationship in a South African peri-urban settlement. Br J Psychiatry. 1999;175:554–558. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- 5.Fisher J, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90:139–149G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weissman MM, et al. Offspring of depressed parents: 30 years later. Am J Psychiatry. 2016 doi: 10.1176/appi.ajp.2016.15101327. [DOI] [PubMed] [Google Scholar]
- 7.Lee L-C, Huang KY, Halpern CT, Newschaffer CJ. The impact of maternal depression on developmental psychopathology during early childhood. Nova Science Publishers; Hauppauge: 2007. [Google Scholar]
- 8.Minkovitz CS, et al. Maternal depressive symptoms and children’s receipt of health care in the first 3 years of life. Pediatrics. 2005;115:306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- 9.NICHD Early Child Care Research Network. Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Dev Psychol. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- 10.Ramchandani PG, et al. Depression in men in the postnatal period and later child psychopathology: a population cohort study. J Am Acad Child Adolesc Psychiatry. 2008;47:390–398. doi: 10.1097/CHI.0b013e31816429c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ross LE, McQueen K, Vigod S, Diennis CL. Risk for postpartum depression associated with assisted reproductive technologies and multiple births: a systematic review. Hum Reprod Update. 2011;17:96–106. doi: 10.1093/humupd/dmq025. [DOI] [PubMed] [Google Scholar]
- 12.Schmied V, et al. Maternal mental health in Australia and New Zealand: a review of longitudinal studies. Women Birth. 2013;26:167–178. doi: 10.1016/j.wombi.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 13.Gulamani SS, Premji SS, Kanji Z, Azam SI. A review of postpartum depression, preterm birth, and culture. J Perinat Neonatal Nurs. 2013;27:52–59. doi: 10.1097/JPN.0b013e31827fcf24. [DOI] [PubMed] [Google Scholar]
- 14.National Research Council and Institute of Medicine Group. Depression in parents, parenting, and children: Opportunities to improve identification, treatment, and prevention. In: England MJ, Sim LJ, editors. Committee on depression, parenting practices, and the healthy development of children. The Natinonal Academies Press; Washington: 2009. [PubMed] [Google Scholar]
- 15.Goodman SH, et al. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 16.Surkan PJ, Kennedy CE, Hurley KM, Black MM. Maternal depression and early childhood growth in developing countries: systematic review and meta-analysis. Bull World Health Organ. 2011;89:608–615. doi: 10.2471/BLT.11.088187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: a meta-analytic review. Clin Psychol Rev. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 18.Rahman A, Harrington R, Bunn J. Can maternal depression increase infant risk of illness and growth impairment in developing countries? Child Care Health Dev. 2002;28:51–56. doi: 10.1046/j.1365-2214.2002.00239.x. [DOI] [PubMed] [Google Scholar]
- 19.Caughy MO, Huang KY, Lima J. Patterns of conflict interaction in mother-toddler dyads: differences between depressed and non-depresed mothers. J Child Fam Stud. 2009;18:10–20. doi: 10.1007/s10826-008-9201-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leiferman J. The effect of maternal depressive symptomatology on maternal behaviors associated with child health. Health Educ Behav. 2002;29:596–607. doi: 10.1177/109019802237027. [DOI] [PubMed] [Google Scholar]
- 21.Conger RD, Conger KJ, Martin MJ. Socioeconomic status, family processes, and individual development. J Marriage Fam. 2010;72:685–704. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Conger RD, et al. Economic pressure in African American families: a replication and extension of the family stress model. Dev Psychol. 2002;38:179–193. [PubMed] [Google Scholar]
- 23.McLoyd VC. The impact of economic hardship on Black families and children: psychological distress, parenting, and socioemotional development. Child Dev. 1990;61:311–346. doi: 10.1111/j.1467-8624.1990.tb02781.x. [DOI] [PubMed] [Google Scholar]
- 24.McLoyd VC, Vonnie C. Socioeconomic disadvantage and child development. Am Psychol. 1998;53:185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- 25.Huang KY, et al. Implementing an early childhood school-based mental health promotion intervention in low-resource Ugandan schools: study protocol for a cluster randomized controlled trial. Trials. 2014;15:471. doi: 10.1186/1745-6215-15-471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Akena D, Joska J, Obuku EA, Stein DJ. Sensitivity and specificity of clinician administered screening instruments in detecting depression among HIV-positive individuals in Uganda. AIDS Care. 2013;25:1245. doi: 10.1080/09540121.2013.764385. [DOI] [PubMed] [Google Scholar]
- 27.Akena D, et al. The assocaition between depressioni, qulaity of life, and the health care expenditure of patients with diabetes melitus in Uganda. J Affect Disord. 2015;174:7–12. doi: 10.1016/j.jad.2014.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nakigudde J, Bauta B, Wolf S, Huang K-Y. Screening child social emotional and behavioral functioning in low-income country contexts. J J Psych Behav Sci. 2016 In Press. [PMC free article] [PubMed] [Google Scholar]
- 29.Brotman LM, et al. Promoting effective parenting practices and preventing conduct problems among ethnic minority families from low-income, urban communities. Child Dev. 2011;82:258–276. doi: 10.1111/j.1467-8624.2010.01554.x. [DOI] [PubMed] [Google Scholar]
- 30.Dawson-McClure S, et al. A population-level approach to promoting healthy child development and school success in low-income, urban neighborhoods: impact on parenting and child conduct problems. Prev Sci. 2015;16:279–290. doi: 10.1007/s11121-014-0473-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang K-Y, Calzada E, Cheng S, Barajas RG, Brotman LM. Cultural adaptation, parenting and child mental health among English speaking Asian American immigrant families. Child Psychiatry Hum Dev. 2016 doi: 10.1007/s10578-016-0683-y. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang K-Y, et al. Applying public health frameworks to advance the promotion of mental health among Asian American children. Asian Am J Psychol. 2014;5:145–152. doi: 10.1037/a0036185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alegria M, et al. Cultural relevance and equivalence in the NLAAS instrument: integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. Int J Methods Psychiatr Res. 2004;13:270–288. doi: 10.1002/mpr.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knight GP, Roosa MW, Umana-Taylor AJ. Studying ethnic minority and economically disadvantaged populations: methodological challenges and best practices. American Psychological Association; Washington: 2009. [Google Scholar]
- 35.Kroenke K, Spitzer R, Williams JB. The PHQ-9 validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pfizer I. PHQ-9 (Patient Health Questionnaire) Pfizer; 1999. [Google Scholar]
- 37.Sheehan DV, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interveiw for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 38.Pianta RC. Child-parent relationship scale. University of Virginia; Charlottesville: 1992. [Google Scholar]
- 39.Webster-Stratton C. Preventing conduct problems in Head Start children: strengthening parenting competencies. J Consult Clin Psychol. 1998;66:715–730. doi: 10.1037//0022-006x.66.5.715. [DOI] [PubMed] [Google Scholar]
- 40.Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 41.Goodman A, Goodman R. Strengths and Difficulties Questionnaire as a dimensional measure of child mental health. J Am Acad Child Adolesc Psychiatry. 2009;48:400–403. doi: 10.1097/CHI.0b013e3181985068. [DOI] [PubMed] [Google Scholar]
- 42.Youthinmind. Strengths and Difficulties Questionnaire. 2012. [Google Scholar]
- 43.Woerner W, et al. The strengths and difficulties questionnaire overseas: evaluations and applications of the SDQ beyond Europe. Eur Child Adolesc Psychiatry. 2004;13:47–54. doi: 10.1007/s00787-004-2008-0. [DOI] [PubMed] [Google Scholar]
- 44.Mullick MSI, Goodman R. Questionnaire screening for mental health problems in Bangladeshi children: a preliminary study. Soc Psychiatry Psychiatr Epidemiol. 2001;36:94–99. doi: 10.1007/s001270050295. [DOI] [PubMed] [Google Scholar]
- 45.Samad L, Hollis C, Prince M, Goodman R. Child and adolescent psychopathology in a developing country: testing the validity of the Strengths and Difficulties Questionnaire. Int J Methods Psychiatr Res. 2005;13:158–166. doi: 10.1002/mpr.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kashala E, Elgen I, Sommerfelt K, Tylleskar T. Teacher ratings of mental health among school children in Kinshasa, Democratic Republic of Congo. Eur Child Adolesc Psychiatry. 2005;14:208–215. doi: 10.1007/s00787-005-0446-y. [DOI] [PubMed] [Google Scholar]
- 47.Goodman A. SDQ- Normative data. Youthinmind; 2013. [Google Scholar]
- 48.Corrigan A. Social Competence Scale—Parent Version, Grade 1/Year 2 (Fast Track Project technical report) The Fast Track Project Web site. 2002 http://www.fasttrackproject.org/
- 49.Gouley KK, Brotman LM, Huang K-Y, Shrout P. Construct validation of the social competence scale in preschool-age children. Soc Dev. 2007;17:380–398. [Google Scholar]
- 50.Ballard T, Coates J, WSwindale A, Deitchler M. USAID, editor. FANTA III Food and Nutrition Technical Assistance. USAID & Fhi360; Washington DC: 2011. Household Hunger scale: indicator definition and measurement guide. [Google Scholar]
- 51.Zimet GD, Powell SS, Farley GK. Psychometric characteristics of the multidimesnional scale of perceived social support. J Pers Assess. 1990;53:610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 52.Nakigudde J, Musisi S, Ehnvall A, Airaksinen E, Agren H. Adaptation of the multidimensional scale of perceived social support in a Ugandan setting. Afr Health Sci. 2009;9:35–41. [PMC free article] [PubMed] [Google Scholar]
- 53.Muthén LK, Muthén BO. Mplus user’s guide. 6. Muthen & Muthen; Los Angeles, CA: 2010. [Google Scholar]
- 54.Bolton P, Wilk CM, Ndogoni L. Assessment of depression prevalence in rural Uganda using symptom and function criteria. Soc Psychiatry Psychiatr Epidemiol. 2004;39:442–447. doi: 10.1007/s00127-004-0763-3. [DOI] [PubMed] [Google Scholar]
- 55.Ovuga E, Boardman J, Wasserman D. The prevalence of depression in two districts of Uganda. Soc Psychiatry Psychiatr Epidemiol. 2005;40:439–445. doi: 10.1007/s00127-005-0915-0. [DOI] [PubMed] [Google Scholar]
- 56.UNODC. Compilation of Evidence-Based Family Skills Training Programmes. United Nations Publication; 2013. [Google Scholar]
- 57.Chilcoat HD, Breslau N. Does psychiatric history bias mothers’ reports? An application of a new analytic approach. J Am Acad Child Adolesc Psychiatry. 1997;36:971–979. doi: 10.1097/00004583-199707000-00020. [DOI] [PubMed] [Google Scholar]
- 58.Najman JM, et al. Mothers’ mental illness and child behavior problems: cause-effect association or observation bias? J Am Acad Child Adolesc Psychiatry. 2000;39:592–602. doi: 10.1097/00004583-200005000-00013. [DOI] [PubMed] [Google Scholar]
- 59.Lee L-C, Newschaffer CJ, Halpem CT, Hertz-Picciotto I. Effect of maternal depressive symptoms on their ratings of toddlers’ behavior problems. Society for Epidemiologic Research; Toronto, Canada: 2005. [Google Scholar]