Abstract
We report a case of severe Plasmodium knowlesi and dengue coinfection in a previously healthy 59-year-old Malay man who presented with worsening shortness of breath, high-grade fever with chills and rigors, dry cough, myalgia, arthralgia, chest discomfort and poor appetite of 1 week duration. There was a history mosquito fogging around his neighbourhood in his hometown. Further history revealed that he went to a forest in Jeli (northern part of Kelantan) 3 weeks prior to the event. Initially he was treated as severe dengue with plasma leakage complicated with type 1 respiratory failure as evidenced by positive serum NS1-antigen and thrombocytopenia. Blood for malarial parasite (BFMP) was sent for test as there was suspicion of malaria due to persistent thrombocytopenia despite recovering from dengue infection and the presence of a risk factor. The test revealed high count of malaria parasite. Confirmatory PCR identified the parasite to be Plasmodium knowlesi. Intravenous artesunate was administered to the patient immediately after acquiring the BFMP result. Severe malaria was complicated with acute kidney injury and septicaemic shock. Fortunately the patient made full recovery and was discharged from the ward after 2 weeks of hospitalisation.
Background
Plasmodium knowlesi is the fifth malaria parasite recognised that infects humans. It is associated with severe clinical manifestation and death. Dengue fever is a mosquito-borne viral infection which may progress to severe dengue with multiorgan failure and dengue shock syndrome. Plasmodium knowlesi and dengue coinfection is rare, presumably due to different habitats of related vectors, Anopheles and Aedes mosquitos, respectively. To the best of our knowledge this is not yet reported in the literature.
Case presentation
We report a case of severe Plasmodium knowlesi with dengue coinfection in a previously healthy 59-year-old Malay man who presented to Hospital Universiti Sains Malaysia on day 8 of illness. His presenting symptoms were worsening shortness of breath, chest discomfort and dry cough of 1 week duration. He also reported of prodromal symptoms with high-grade fever, chills and rigors, poor appetite, myalgia, arthralgia and malaise of almost a week. He was given antibiotics by a local clinician, however, his symptoms persisted. There was no history of diarrhoea, vomiting or any mucosal bleeding. There was a recent mosquito fogging activity in the neighbourhood in his hometown. Clinical examination on admission revealed a normal built, however, breathless (respiratory rate 40 breaths per minute) and dehydrated man. He was conscious and orientated. He was feverish (40°C). Oxygen saturation under room air was 94%. Heart rate was 96 beats per minute. Blood pressure was stable (130/80 mm Hg). There was no viral exanthem or petechiae seen. There were bibasal fine crackles on chest auscultations. Of note, there was no hepatosplenomegaly.
Investigations
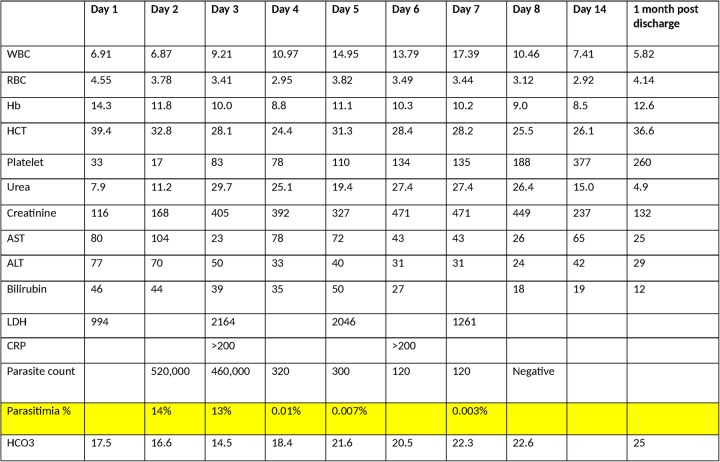
Blood investigations showed thrombocytopenia (33×109/L) with normal white cell count and haemoglobin level. Haematocrit was 39.6%. There was raised bilirubin level, predominantly unconjugated bilirubin with raised transaminases. Serum NS1 antigen was positive on day 5 of illness. Arterial blood gas showed compensated severe metabolic acidosis with type 1 respiratory failure. Creatine kinase level was normal (177 U/L). Plasma lactate dehydrogenase was markedly raised (995 IU/L). There was an atypical lymphocyte seen on the full blood picture together with left shift which was suggestive of viral infection. Chest radiograph showed evidence of pulmonary congestion. The platelet count remained low although dengue infection was in the recovery phase. Blood for malarial parasite (BFMP) was sent in view of the former and also history of going to a forest. It revealed high level of plasmodium parasite count (520 000 uL/blood). Confirmatory PCR sample was also sent which later identified the parasite to P. knowlesi.
Investigations table is as shown in the figure 1.
Figure 1.
Serial blood investigations. ALT, alanine transaminase; AST, aspartate aminotransferase; CRP, C reactive protein; Hb, haemoglobin; HCT, haematocrit; LDH, RBC, red blood cell; WCC, white cell count.
Differential diagnosis
Dengue fever with secondary bacterial infection
Yellow fever
Leptospirosis
Treatment
He was treated as severe dengue fever with plasma leakage complicated with type 1 respiratory failure. On day 2 of admission, BFMP was positive for malaria parasite. The patient was started on intravenous artesunate for severe malaria infection. Malaria was then complicated with acute kidney injury requiring four sessions of haemodialysis. He was put on non-invasive ventilation on admission and weaned off to room air on day 11 of admission. Intravenous norepinephrine infusion was given for 3 days due to septicaemic shock.
Outcome and follow-up
After 16 days of stay in ward, the patient made full recovery and was discharged. Plasmodium parasite count was undetectable after completing 1 week of intravenous artesunate. His blood counts, renal and liver functions had normalised during follow-up 1 month after discharge.
Discussion
P. knowlesi is the fifth malaria parasite recognised to infect humans, apart from Plasmodium vivax, ovale, malariae and falciparum.1 It is morphologically similar to Plasmodium malariae on blood film thus requires confirmatory PCR for identification.2 3 Clinical presentation ranges from uncomplicated, non-specific febrile illness in majority of patients to complicated and fatal illness in a small proportion of patients.4 The risk of fatalities is a consequence of a very high level of parasiteamia as P.knowlesi only needs 24 hours to complete its erythrocytic cycle. The most common complication is acute respiratory distress.4 Thrombocytopenia is very common4 despite the different speculated mechanisms, thus mimicking viral illnesses. The treatment for uncomplicated Plasmodium knowlesi infection includes oral chloroquine or other artermisinin derivatives for 3 days.5 Criteria for severe knowlesi malaria is rather similar to those seen in falciparum malaria except for the following 2: Hyperparasitaemia >100 000 µL; jaundice and parasite density >20 000 µL.5 Intravenous or intramuscular artesunate is given for at least 24 hours and then substituted to oral therapy once the patient able to swallow. The duration of oral treatment is 3 days.6 Previous small studies have shown the efficacy of parenteral artesunate in treating severe knowlesi malaria, likely attributed to its fast parasite clearance properties.7 A study by Fatih et al8 has shown that Plasmodium knowlesi is highly sensitive to artemisinins compared to chloroquine and mefloquine. An randomised controlled trial carried out by Dr Matthew J Grigg and his team, published in February 2016, has shown that artesunate-mefloquine was better compared to chloroquine monotherapy in uncomplicated Plasmodium knowlesi infection.9 Thus, based on current evidence, parenteral artesunate is the preferred choice in severe knowlesi malaria while artemisinin combination therapy is preferred for non-severe knowlesi malaria.
Despite being a common infection in tropical countries, coexistence malaria and dengue infection in a patient is rare. Even after extensive literature search we have not found a single case of coexistence malaria and dengue infection reported. Possible explanations for the least likelihood of coinfection include difference in habitats of the vectors, immunity from infection in endemic areas and very low chance of concurrent infection given the prevalence of dengue and malaria in certain areas.10 It is undeniable that both Chikungunya11 and Zika virus12 infections has been reported in Malaysia. The last outbreak of Chikungunya in Kelantan was in 2009. Nevertheless, both infections are rarely fatal and thus were not screened in our case.13–15
Our case report is the first to report a severe Plasmodium knowlesi infection with dengue coinfection. The likely reason for such coinfection in this patient was because of the patient is living in the dengue endemic area. At same time, he went to malaria endemic area without any prophylaxis. Previous reported cases by Azira et al16 were mild cases without multiorgan failure and were treated with oral antimalarial. Thus this case report should raise the awareness among medical personnel of possible malaria infection in dengue fever, particular those with atypical presentation and coming from endemic areas of both diseases.
Learning points.
Coinfection of malaria and dengue infection is rare.
Plasmodium knowlesi can mimic clinical features of dengue infection.
There should be suspicion of coinfection of malaria infection in dengue fever if patient comes from endemic areas or presence of recent exposure.
Prompt recognition of malaria infection and initiation of antimalarial drugs is a must to prevent complications and mortality.
Plasmodium knowlesi has similar criteria for severe infection seen in malaria falciparum except two parameters.
Footnotes
Contributors: MJCR prepared the manuscript. AMB managed the patient. WSWG and NM edited and approved the final draft of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.White NJ. Plasmodium knowlesi: the Fifth Human Malaria Parasite. Clin Infect Dis 2008;46:172–3. 10.1086/524889 [DOI] [PubMed] [Google Scholar]
- 2.Cox-Singh J, Davis TME, Lee KS et al. . Plasmodium knowlesi malaria in humans is widely distributed and potentially life threatening. Clin Infect Dis 2008;46:165–71. 10.1086/524888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilairatana P, Krudsood S, Tangpukdee N. Management of Plasmodium knowlesi malaria without PCR confirmation. Southeast Asian J Trop Med Public Health 2010;41:19–21. [PubMed] [Google Scholar]
- 4.Daneshvar C, Davis TME, Cox-Singh J et al. . Clinical and laboratory features of human Plasmodium knowlesi infection. Clin Infect Dis 2009;49:852–60. 10.1086/605439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guidelines for the treatment of malaria. WHO, 2015. [Google Scholar]
- 6.Management of dengue infection in adults, 3rd edn Ministry of Health Malaysia, 2015. [Google Scholar]
- 7.Visser BJ, Wieten RW, Kroon D et al. . Efficacy and safety of artemisinin combination therapy (ACT) for non-falciparum malaria: a systematic review. Malar J 2014;13:463 10.1186/1475-2875-13-463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fatih FA, Staines HM, Siner A et al. . Susceptibility of human Plasmodium knowlesi infections to anti-malarials. Malar J 2013;12:425 10.1186/1475-2875-12-425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grigg MJ, William T, Menon J et al. . Artesunate–mefloquine versus chloroquine for treatment of uncomplicated Plasmodium knowlesi malaria in Malaysia (ACT KNOW): an open-label, randomised controlled trial. Lancet Infect Dis 2016;16:180–8. 10.1016/S1473-3099(15)00415-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiwanitkit V. Concurrent malaria and dengue infection: a brief summary and comment. Asian Pac J Trop Biomed 2011;1:326–7. 10.1016/S2221-1691(11)60053-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diop D, Meseznikov G, Sanicas M. Chikungunya outbreaks from 2000 to 2015: a review. MOJ Public Health 2015;2:00043 10.15406/mojph.2015.02.00043 [DOI] [Google Scholar]
- 12.Sam JI, Chan YF, Vythilingam I et al. . Zika virus and its potential re-emergence in Malaysia. Med J Malaysia 2016;71:68–70. [PubMed] [Google Scholar]
- 13. http://www.who.int/denguecontrol/arbo-viral/other_arboviral_chikungunya/en/
- 14. http://www.who.int/mediacentre/factsheets/zika/en/
- 15.Swaminathan S, Schlaberg R, Lewis J et al. . Fatal Zika virus infection with secondary nonsexual transmission. N Engl J Med 2016;375:1907–9. 10.1056/NEJMc1610613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azira NMS, Zairi NZ, Amry AR et al. . Case series of naturally acquired Plasmodium knowlesi infection in a tertiary teaching hospital. Trop Biomed 2012;29:398–404. [PubMed] [Google Scholar]