Abstract
Stercoral perforation is a rare cause of bowel perforation. It is caused by faecal impaction, which generates pressure against the colon wall, leading to ischaemic necrosis and subsequent perforation. Since diagnosis is often delayed, stercoral perforation is usually mistreated as constipation or faecal impaction, leading to high mortality. This report presents a case of stercoral perforation in a woman aged 34 years who was promptly diagnosed and successfully treated.
Background
Stercoral perforation is a rare cause of bowel perforation. Most cases of colonic perforation are attributed to diverticulitis, malignancy, trauma, inflammatory bowel disease, ischaemia, infection and iatrogenic conditions.1 2 Stercoral perforation occurs in the context of chronic constipation, typically in elderly or bedridden patients. Overtime, faecal impaction develops into a large faecoloma. As the faecoloma exerts pressure against the colonic wall, it impairs regional transmural perfusion. If the intraluminal pressure exceeds 35 cm H2O for several hours, ischaemic necrosis develops, leading to bowel wall necrosis and, ultimately, to perforation.3–6 The sigmoid colon and rectum, and particularly the rectosigmoid junction, are the most susceptible parts of the colon for several reasons, including the decreasing water content of the stool, their relatively narrow diameter and the poor blood supply to these regions from inefficient or absent anastomosis between the branches of the inferior mesenteric and superior rectal arteries, often referred to as Sudeck's point.3–6 While it is difficult to recognise stercoral colitis on physical examination, it is crucial to diagnose and treat this condition as soon as possible, as the mortality rate of stercoral perforation is high.5
Case presentation
A woman aged 34 years with a medical history of hypertension and end-stage renal disease on haemodialysis presented with pain and purulent drainage at the site of the patient's dialysis catheter. The patient received a kidney transplant in 2004. The allograft subsequently failed and she was placed on haemodialysis 3 weeks prior to this incident. At the time of admission, the patient was taking ciclosporin, prednisone and mycophenolate mofetil, as well as clonidine for hypertension. She reported constipation, having not had a bowel movement for 3 weeks. The dialysis catheter was removed, a temporary Quinton catheter was placed and the patient was started on broad-spectrum antibiotics. The patient began to experience abdominal pain after admission. The abdomen was soft and not tender on examination. Abdominal radiograph revealed a large stool burden. The patient was given bisacodyl, polyethylene glycol, docusate sodium and enemas with no response. The pain persisted into the next day, she reported extreme sharp pain in the lower abdomen. Her blood pressure was 152/93 mm Hg, pulse was 104 and temperature was 102.5°F. The patient's abdomen was tender to palpation, especially the left lower quadrant, and there was no rebound tenderness. The white cell count was 11 600/mm3. Our leading diagnosis at this stage was acute diverticulitis. Ischaemic colitis and pelvic inflammatory disease were considered less likely causes for this presentation.
Investigations
Abdominal CT revealed pneumoperitoneum, along with focal wall thickening of the proximal sigmoid colon and moderate adjacent free fluid extending into the pelvis (figures 1 and 2).
Figure 1.
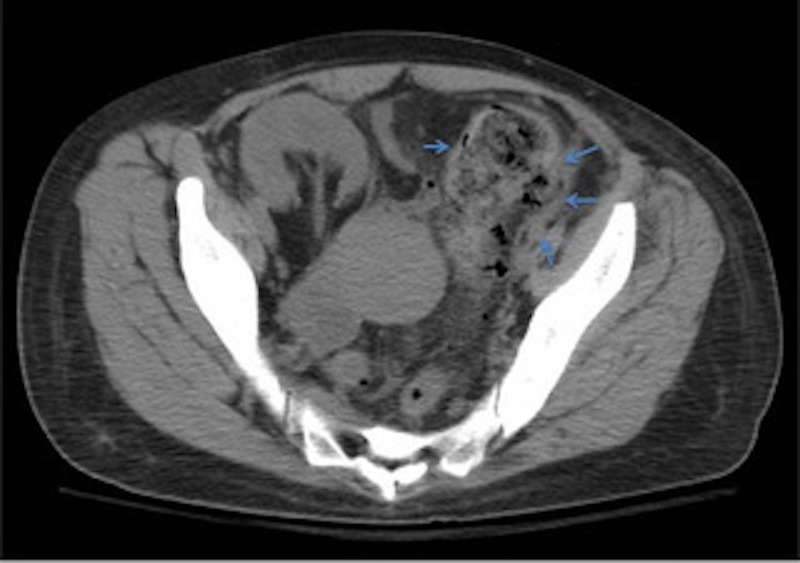
Wall thickening and fluid adjacent to the sigmoid colon ‘ arrows’.
Figure 2.
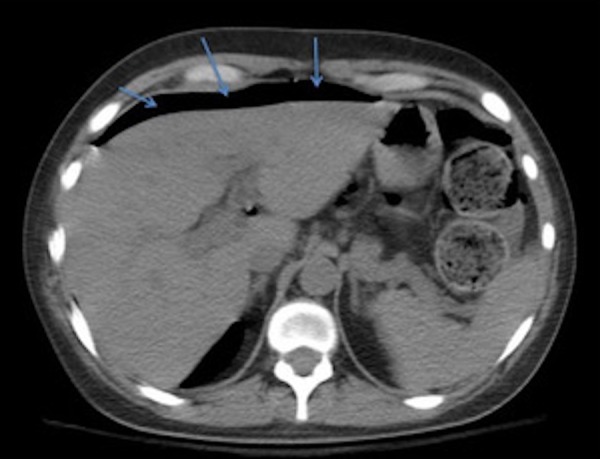
Free intraperitoneal air ‘ arrows’.
Treatment
An emergent exploratory laparotomy revealed a perforation in the medial wall of the sigmoid colon at the rectosigmoid junction. There was impacted stool ranging from the midtransverse colon to the rectum, as well as murky, purulent fluid throughout the abdomen. The sigmoid colon was resected with end colostomy and stool lavage was performed until the colon was clear. Additionally, the appendix was removed due to the presence of fecoliths and ischaemic change.
The fascia was closed and a wound vacuum-assisted closure (VAC) was placed. The peritoneal fluid cultures found extended-spectrum producing β lactamase, Escherichia coli and Enterococcus. The patient received intravenous meropenem and metronidazole.
The pathology revealed a single perforation of the sigmoid colon. There were areas of focal mucosal ulceration with acute inflammatory cells and acute serositis in the resected sigmoid colon.
Outcome and follow-up
The remainder of the hospital stay was complicated by a deep vein thrombosis in the right brachial vein associated with the peripherally inserted central cannula (PICC line). It was treated with intravenous heparin infusion and warfarin. The wound VAC was removed after 3 days. The patient was discharged after a total of 15 days of hospital stay. She was readmitted 9 days later for constipation. Her constipation eventually resolved with golytely use, and she was discharged the following day. She was last seen in the renal clinic 1 month ago. Her constipation has improved with the use of multiple laxatives. Immunosuppressant drugs were discontinued.
Discussion
Stercoral perforation is a very serious consequence of untreated constipation. The estimated incidence of colon perforation secondary to stercoral perforation is 3.2%.7 The overall mortality of stercoral perforation is estimated to be 34%.3 The average age of patients with stercoral colitis is 62 years (range 4–106 years).3 Stercoral perforation often presents with non-specific symptoms, making it difficult to differentiate it from constipation. A study of 13 patients with stercoral perforation revealed that all patients in the study presented with constipation, and most had abdominal pain or distention.5 Leucocytosis with left shift was present in 11 patients and septic shock was diagnosed in 5 patients.5 Another study of 10 patients with stercoral perforation reported fever in 2 patients, peritoneal signs in 2 patients and leucocytosis in 7 patients.8 Elderly people, nursing home residents, bedridden individuals and patients with hypothyroidism, scleroderma or diabetic enteropathy are at higher risk for stercoral perforation, as faecal impaction is more prevalent in these groups.3 4 6 Opiates, tricyclic antidepressants, non-steroidal anti-inflammatory drugs (NSAIDs), verapamil and immunosuppressive agents used after renal transplantation can cause constipation.3 4 6 Additionally, NSAIDs reduce the production of protective prostaglandins.3 4 6 Chronic renal failure causes disturbances in fluid volume and electrolyte activity that predispose these patients to impaction. The effects of uraemia and underlying diseases such as diabetes mellitus on the autonomic nervous system also predispose patients to constipation and impaction.9 There were 21 cases of colon perforation among 1611 patients who had kidney transplants who were followed over 31 years. The majority of these cases were secondary to diverticulitis, with roughly half being fatal.10 Abdominal radiography has not been shown to be a sensitive method for diagnosing stercoral perforation.5 8 However, abdominal radiography can demonstrate large stool burden and may show evidence of bowel obstruction or free intraperitoneal air. An abdominal CT scan is the best option for diagnosis. In one study, the most sensitive CT findings in decreasing order were pericolonic stranding (80%), perfusion defects (70%), dense mucosa (62%), thickening of the colon wall (60%), abnormal gas (50%) and pericolonic abscess (20%).8 In this case, free intraperitoneal air was identified in CT imaging but was not seen in the plain radiography on two consecutive days. Emergent surgery with resection of the affected segment of the colon, end colostomy and Hartmann's closure of the rectum should not be delayed.3 4 The remaining colon should be inspected for hard faecal masses or stercoral ulcers, as well as the possibility of a second perforation.4 Other interventions, such as exteriorisation of the perforation without resection or repairing the perforation with a proximal colostomy, have a high mortality rate.4 Intravenous antibiotics and fluid resuscitation are a standard part of treatment management. Stercoral perforation is a rare but lethal complication of constipation and faecal impaction. Early diagnosis of faecal impaction and aggressive treatment by manual disimpaction and enemas may prevent this complication.5 11 Maintenance laxative therapy is recommended to prevent further episodes of impaction.5 11 It is recommended to maintain a high index of suspicion for stercoral perforation in patients with a history of chronic constipation who present with acute abdominal pain. A chronically constipated patient with increasing abdominal pain, without clinical peritonitis may either be developing or already have subclinical stercoral perforation.3 An early abdominal CT scan can diagnose this condition and prevent possible death.
Learning points.
Stercoral perforation is a rare but lethal complication of constipation and faecal impaction.
Maintain a high index of suspicion for stercoral perforation in patients with a history of chronic constipation who present with acute abdominal pain.
A chronically constipated patient with increasing abdominal pain without clinical peritonitis may either be developing stercoral perforation or already have it subclinically.
A plain abdominal radiography may not diagnose stercoral perforation, but early abdominal CT scans can diagnose this condition and prevent possible death.
Footnotes
Contributors: MM wrote the manuscript, reviewed the literature and he also participated in managing the case as the patient was assigned to him during his internal medicine rotation. HA managed the case during the admission, participated in writing the manuscript and reviewed the literature.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Langell JT, Mulvihill SJ. Gastrointestinal perforation and the acute abdomen. Med Clin North Am 2008;92:599–625. 10.1016/j.mcna.2007.12.004 [DOI] [PubMed] [Google Scholar]
- 2.Nam JK, Kim BS, Kim KS et al. Clinical analysis of stercoral perforation of the colon. Korean J Gastroenterol 2010;55:46–51. 10.4166/kjg.2010.55.1.46 [DOI] [PubMed] [Google Scholar]
- 3.Chakravartty S, Chang A, Nunoo-Mensah J. A systematic review of stercoral perforation. Colorectal Dis 2013;15:930–5. 10.1111/codi.12123 [DOI] [PubMed] [Google Scholar]
- 4.Haddad R, Bursle G, Piper B. Stercoral perforation of the sigmoid colon. ANZ J Surg 2005;75:244–6. 10.1111/j.1445-2197.2005.03337.x [DOI] [PubMed] [Google Scholar]
- 5.Saksonov M, Bachar GN, Morgenstern S et al. Stercoral colitis: a lethal disease-computed tomographic findings and clinical characteristic. J Comput Assist Tomogr 2014;38:721–6. 10.1097/RCT.0000000000000117 [DOI] [PubMed] [Google Scholar]
- 6.Beharrysingh R, McDaniel JL, Abdel Hak A et al. Break in the wall: stercoral colitis. Am J Med 2016;129:479–80. 10.1016/j.amjmed.2016.01.005 [DOI] [PubMed] [Google Scholar]
- 7.Maurer CA, Renzulli P, Mazzucchelli L et al. Use of accurate diagnostic criteria may increase incidence of stercoral perforation of the colon. Dis Colon Rectum 2000;43:991–8. 10.1007/BF02237366 [DOI] [PubMed] [Google Scholar]
- 8.Wu CH, Wang LJ, Wong YC et al. Necrotic stercoral colitis: importance of computed tomography findings. World J Gastroenterol 2011;17:379–84. 10.3748/wjg.v17.i3.379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wrenn K. Fecal impaction. N Engl J Med 1989;321:658–62. 10.1056/NEJM198909073211007 [DOI] [PubMed] [Google Scholar]
- 10.Catena F, Ansaloni L, Gazzotti F et al. Gastrointestinal perforations following kidney transplantation. Transplant Proc 2008;40:1895–6. 10.1016/j.transproceed.2008.06.007 [DOI] [PubMed] [Google Scholar]
- 11.Wald A. Management and prevention of fecal impaction. Curr Gastroenterol Rep 2008;10:499–501. 10.1007/s11894-008-0091-y [DOI] [PubMed] [Google Scholar]


