Abstract
Background:
Increasing evidence highlights the association of occupational exposure and cutaneous malignant melanoma (CMM). We estimated the burden of CMM and total skin cancer burden in Britain due to occupational solar radiation exposure.
Methods:
Attributable fractions (AF) and numbers were estimated for CMM mortality and incidence using risk estimates from the published literature and national data sources for proportions exposed. We extended existing methods to account for the exposed population age structure.
Results:
The estimated total AF for CMM is 2.0% (95% CI: 1.4–2.7%), giving 48 (95% CI: 33–64) deaths in (2012) and 241 (95% CI: 168–325) registrations (in 2011) attributable to occupational exposure to solar radiation. Higher exposure and larger numbers exposed led to much higher numbers for men than women. Industries of concern are construction, agriculture, public administration and defence, and land transport.
Conclusions:
These results emphasise the urgent need to develop appropriate strategies to reduce this burden.
Keywords: occupation, cancer, skin, melanoma
Burden of disease estimation is increasingly being used to identify risk factors contributing to important morbidity burdens and to help prioritise risk reduction approaches. Previously published estimates of the burden of occupational cancer for over 20 cancer sites (Rushton et al, 2012) include non-melanoma skin (NMSC) cancer from occupational exposure to solar radiation (Young et al, 2012).
Evidence for a causal role of occupational sunlight exposure in development of cutaneous malignant melanoma (CMM) is equivocal. The meta-analysis by Caini et al (2009) shows that high naevi counts are associated with CMM on body sites not usually exposed to sun and that skin/hair colour and sunburns are highly associated with all types of CMM. Intermittent, relatively high exposure has been highlighted (Elwood and Jopson, 1997; Gandini et al, 2005). An increased risk for CMM has been found for outdoor work or farming in some studies; Odds Ratio (OR) 2.7 (95% CI: 1.2, 5.8; Settimi et al, 1999); OR 1.31 (95% CI: 1.14, 1.52) (Freedman et al, 1997) but a negative association in others; OR 0.78 (95% CI: 0.61, 0.99; Walter et al, 1999). It has been suggested that recreational sun exposure increases risk of trunk and limb CMM, whereas occupational sun exposure tends to increase risk of head and neck melanoma especially at low latitudes (Whiteman et al, 2006; Chang et al, 2009). Whiteman et al found raised risk for head and neck melanoma associated with high occupational sun exposure (OR: 3.25; 95% CI: 1.3, 8.0) compared with patients with trunk melanoma and in particular for lentigo maligna melanoma.
However, an Australian study found no increased risk for CMM and occupational sun exposure (defined as weekday exposure) overall or at different sites with an inverse association for head and neck CMM (Vuong et al, 2014).
A large multicentre European study comparing outdoor and indoor workers found highest risks for outdoor work for basal cell and squamous cell carcinomas (statistically significantly increased for farmers/construction workers and for other outdoor work) but non-significantly raised risks for melanoma (Trakatelli et al, 2016). However, duration of work >5 years gave odds ratios of 3.02 (95% CI: 1.88–4.86) for melanoma in situ and 1.97 (95% CI: 1.43–2.71) for invasive melanoma.
Although the evidence for CMM is not entirely convincing, it is suggestive of a potential causal relationship and that a contribution from occupational exposure is plausible. Hence we estimated the CMM burden assuming causality and also provide a summary of the total skin cancer burden in Britain due to occupational solar radiation exposure.
Materials and methods
Burden of cancer was estimated using the attributable fraction (AF) that is, the proportion of cases that would not have occurred in the absence of exposure; this was then used to estimate the attributable numbers (Hutchings and Rushton, 2012). The AF requires an estimate of the risk of disease, (e.g., a relative risk (RR)), which we obtained from published literature, and the proportion of the population exposed (p(E)). To account for cancer latency a Risk Exposure Period (REP), that is, the exposure period relevant to a cancer appearing in a specific target year, was defined as 10–50 years for CMM.
The p(E) was derived from the national data sources, accounting for employment turnover and life expectancy, and adjusted for employment trends. We here extend our methods to estimate CMM AF by age group to account for variation in cancer rates by age, assuming the exposed population and national working population have the same age structure and that workers enter the workforce between ages 15–45 and retire at 65.
The CARcinogen EXposure (CAREX) database, which gives numbers exposed to certain occupational carcinogens in 1991 by standard industry sector, was used to estimate the numbers exposed occupationally to solar radiation (Pannett et al, 1998). The data from CAREX are not differentiated by sex; the 1991 Census data by industry were used to estimate the relative proportions of men and women exposed within the CAREX industry sectors. Industry sectors were allocated as one of (i) farmers (agriculture, forestry, hunting, logging) (ii) other outdoor workers (e.g., construction, defence) (iii) mixed indoor and outdoor exposure (e.g., transport, recreational services) or having low exposure (e.g., retail, real estate).
Since Britain has relatively low sunlight exposure generally, we used risk estimates for residential areas of low sunlight, (adjusted for age, sex, race, socioeconomic status) from a 24 state US mortality database (Freedman et al, 1997). Sunlight exposure was assessed by state of residence (low, moderate, high sun exposure) and usual occupation recorded on the death certificate (classified as indoor work, combined indoor and outdoor work, outdoor work by non-farmers and farming). The RRs were 11.31, 95% CI: 1.14–1.52) for farmers, 1.22, (95% CI: 0.99–1.50) for outdoor non-farmer occupational exposure, and set to 1 for mixed indoor and outdoor occupations as the risk estimate was <1; indoor work (low exposure) was set to 1.
AFs were then estimated separately by age group and applied to age specific British data available at the time of the study for CMM deaths (2012) and cancer registrations (2011), and summed to obtain occupation attributable numbers.
We also estimated disability-adjusted life-years (DALY), the sum of years of life lost (YLL; estimated from cancer deaths and life expectancy) and years lived with disability (YLD). Years lived with disabilities are estimated using cancer numbers, average survival and an evaluation of health related quality of life using disability weights developed for the Netherlands (Murray and Lopez, 1996).
Results
The estimated total AF for CMM is 2.0% (95% CI: 1.4–2.7%), giving 48 (95% CI: 33–64) deaths in (2012) and 241 (95% CI: 168–325) registrations (in 2011) attributable to occupational exposure to solar radiation (Table 1). Higher results for men reflect both higher exposure and larger numbers exposed to solar radiation. Average years of life lost through early death is ∼17 years, and estimated DALYs due to occupationally related CMM are 1038 (95% CI: 700–1394) per year.
Table 1. Results for cutaneous malignant melanoma and exposure to occupational solar radiation.
| Men | Women | Total | |
|---|---|---|---|
| Numbers ever exposed over the risk exposure period | 3 112 940 | 1 709 973 | 4 822 913 |
| Proportion of the population exposed | 15.0% | 7.7% | 11.2% |
| Number (95% CI) | Number (95% CI) | Number (95% CI) | |
| Attributable fraction | 3.2% (2.2%, 4.3%) | 0.9% (0.7%, 1.3%) | 2.0 (1.4%, 2.7%) |
| Attributable deaths (2012) | 39 (27, 52) | 8 (6, 12) | 48 (33, 64) |
| Attributable registrations (2011) | 184 (127, 248) | 57 (41, 77) | 241 (168, 325) |
| Years of life lost | 660 (441, 863) | 160 (116, 216) | 820 (557, 1079) |
| Disability-adjusted life-years | 826 (546, 1100) | 212 (154, 295) | 1038 (700, 1394) |
The main industries of concern are construction (21 deaths, 101 registrations), agriculture (11 deaths, 55 registrations), public administration and defence (5 deaths, 26 registrations), and land transport (4 deaths, 21 registrations).
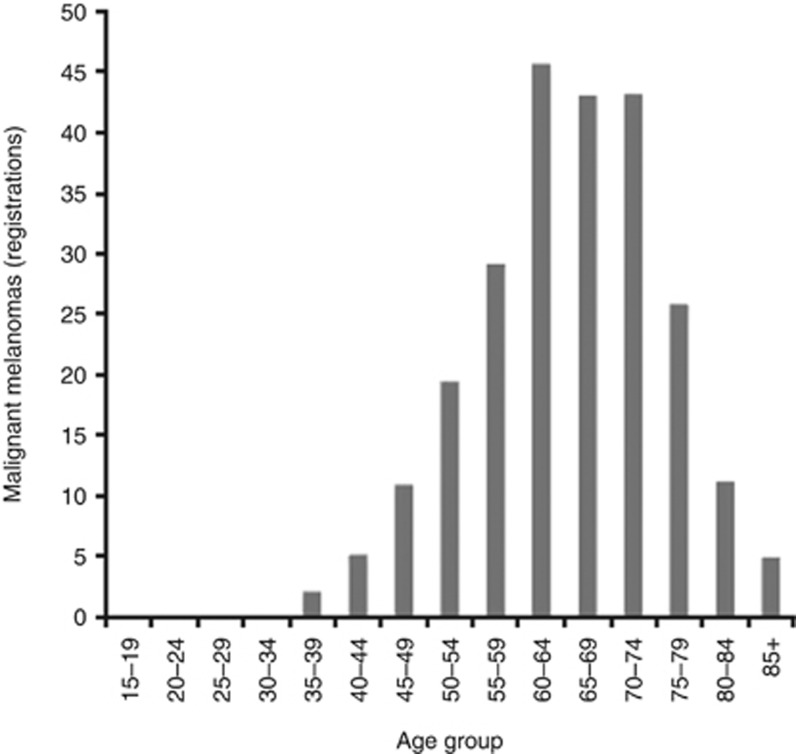
Figure 1 shows the distribution of CMM registrations by age. Over 50% (128) occur after retirement (65+).
Figure 1.
Attributable registrations (2011) for cutaneous malignant melanoma and exposure to occupational solar radiation by age group.
Discussion
Assuming a causal link, we estimate that 2% of all CMM in Britain can be attributed to occupational exposure to solar radiation, giving ∼1 death and 5 new cancers per week. The construction industry has the largest burden (44% of the deaths and 42% of the registrations), followed by agriculture, public administration/defence, and land transport. These results add to the concern arising from our previous estimate for NMSC of the adverse health effects of occupational solar radiation (AF=2.4%, 12 attributable deaths and 1541 attributable registrations; Young et al, 2012). Our estimation by age has highlighted the issue of many similar long latency occupational cancers occurring many years after leaving work.
Under or over estimation of the burden may have resulted from methodological assumptions and uncertainties in the data, including choice of risk estimates, inaccurate estimates of proportions exposed and latency.
Risk estimates for CMM varied between studies. Different study designs, definitions of personal characteristics and exposure assessment and inconsistent adjustment for non-occupational exposure and other risk factors could have contributed to this (Hutchings and Rushton, 2012). Many were hospital case-control studies increasing the likelihood of accurate CMM diagnosis but raising the possibility of selection bias (e.g., Trakatelli et al, 2016). Recall bias could have occurred in self-reporting of sun exposure, particularly in more recent studies as awareness of the hazards of sun exposure became more common. Hospital patient controls with other dermatological conditions or non-melanoma malignancies in some studies may have been more aware about the effects of sun exposure; use of case friends, family or neighbours may give controls with similar occupations and lifestyles (e.g., Vuong et al, 2014). Adjustment for hair and/or skin colour, ethnicity and freckling was usual, with some studies also adjusting for tendency to burn, socio-economic status, sun screen use and recreational sun exposure.
For CMM, there was no good quality British study of workplace exposure to solar radiation. The Freedman study chosen may not have completely reflected exposure experienced in Britain; the use of death certificate information for residence and occupation might reflect more recent rather than lifetime exposure.
Industry sectors were allocated as outdoor, mixed indoor/outdoor and mainly indoor for solar radiation because of the lack of data on proportions exposed at different levels of exposure. Implicit assumptions were made regarding the similarity of durations and intensities of exposure between the population in the chosen study and British exposed workforce.
Summary
Assuming a causal relationship for all skin cancers and occupational sun exposure this study quantifies the total burden specifically for Britain and highlights several industry sectors, particularly construction. This highlights the need to develop appropriate strategies to reduce this burden. The Institution of Occupational Safety and Health (IOSH) have used these results as a basis for their successful ‘No Time to Lose Campaign', including specific factsheets, posters, toolbox talks, films, case studies targeting occupational solar radiation (IOSH 2016).
Acknowledgments
The funding for the original British Occupational Cancer Burden Study was obtained from the Health and Safety Executive. The funding for this work was obtained from the Institution of Occupational Safety and Health.
Footnotes
The authors declare no conflict of interest.
References
- Cain S, Gandini S, Sera F, Raimondi S, Fargnoli MC, Boniol M, Armstrong BK (2009) Meta-analysis of risk factors for cutaneous melanoma according to anatomical site and clinic-pathological variant. Eur J Cancer 45: 3054–3063. [DOI] [PubMed] [Google Scholar]
- Chang Y, Barrett JH, Bishop DT, Armstrong BK, Bataille V, Bergman W, Berwick M, Bracci PM, Elwood JM, Ernstoff MS, Gallagher RP, Green AC, Gruis NA, Holly EA, Ingvar C, Kanetsky PA, Karagas MR, Lee TK, Le Marchand L, Mackie RM, Olsson H, Østerlind A, Rebbeck TR, Sasieni P, Siskind V, Swerdlow AJ, Titus-Ernstoff L, Zens MS, Newton-Bishop JA (2009) Sun exposure and melanoma risk at different latitudes: a pooled analysis of 5700 cases and 7216 controls. Int J Epidem 38(3): 814–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwood JM, Jopson J (1997) Melanoma and sun exposure: an overview of published studies. Int J Epidem 73: 198–203. [DOI] [PubMed] [Google Scholar]
- Freedman DM, Zahm SH, Dosemeci M (1997) Residential and occupational exposure to sunlight and mortality from non-Hodgkin's lymphoma: composite (threefold) case-control study. BMJ 314(7092): 1451–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gandini S, Sera F, Cattaruzza MS, Pasquini P, Picconi O, Boyle P, Melchi CF (2005) Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer 41(1): 45–60. [DOI] [PubMed] [Google Scholar]
- Hutchings S, Rushton L (2012) The burden of occupational cancer in Britain: statistical methodology. Br J Cancer 107: S8–S17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOSH (2016) Institution for Occupational Safety and Health No Time to Lose Campaign http://www.notimetolose.org.uk/ (Accessed on August 2016).
- Murray CJL, Lopez AD (1996) The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. In: Global Burden of Disease and Injury Series, vol. 1. Harvard Sch. Public Health/WHO/World Bank, Cambridge, MA, USA, pp 990.
- Pannett B, Kauppinen T, Toikkanen J, Pedersen J, Young R, Kogevinas M (1998) Occupational exposure to carcinogens in Great Britain in 1990–1993: preliminary results. In: CAREX: International Information System on Occupational Exposure to Carcinogens. Finnish Institute of Occupational Health, Helsinki, Finland, Available at http://www.ttl.fi/en/chemical_safety/carex/Pages/default.aspx (Accessed on August 2016).
- Rushton L, Hutchings SJ, Fortunato L, Young C, Evans GS, Brown T, Bevan R, Slack R, Holmes P, Bagga S, Cherrie J, Van Tongeren M (2012) The Burden of Occupational Cancer in Britain. Introduction. Br J Cancer 107: S3–S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushton L, Hutchings S, Fortunato L, Young C, Evans G, Brown T, Bevan R, Slack R, Holmes P, Bagga S, Cherrie J, Van Tongeren M (2012) Occupational cancer burden in Great Britain. Br J Cancer 107: S3–S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Settimi L, Comba P, Carrier P, Boffetta P, Magnani C, Terracinin B, Andrion A, Bosia S, Ciapini C, De Santis M, Desideri E, Fedi A, Luccoli L, Maiozzi P, Masina A, Perazzo PL, Axelson O (1999) Cancer risk among female agricultural workers: a multi-center case-control study. Am J Ind Med 36(1): 135–141. [DOI] [PubMed] [Google Scholar]
- Trakatelli M, Barkitzi K, Apap C, Majewski S De Vries E, the EPIDERM group (2016) Skin cancer risk in outdoor workers: a European multicenter case-control study. J Eur Acad Dermatol Venereol 30(Suppl. 3): 5–11. [DOI] [PubMed] [Google Scholar]
- Vuong K, McGeechan K, Armstring BK AMFS investigators, GEM investigators,Cust AE (2014) Occupational sun exposure and risk of melanoma according t anatomical site. Int J Cancer 134: 2735–2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter SD, King WD, Marrett LD (1999) Association of cutaneous malignant melanoma with intermittent exposure to ultraviolet radiation: results of a case-control study in Ontario, Canada. Int J Epidemiol 28(3): 418–427. [DOI] [PubMed] [Google Scholar]
- Whiteman DC, Stickely M, Watt P, Hughes MC, Davis MB, Green AC (2006) Anatomic site, sun exposure and risk of cutaneous melanoma. J Clin Oncol 24(19): 3172–3177. [DOI] [PubMed] [Google Scholar]
- Young C, Rushton L with the British Occupational Cancer Study Group (2012) The burden of occupational cancer in Britain. skin cancer. Br J Cancer 107: S71–S75. [DOI] [PMC free article] [PubMed] [Google Scholar]