Abstract
Objective
Ischemic heart disease is the leading cause of death in India. Many of these deaths are due to acute coronary syndromes (ACS), which require prompt symptom recognition, care-seeking behavior, and transport to a treatment facility in the critical pre-hospital period. In India, little is known about pre-hospital management of individuals with ACS. We aim to understand the facilitators, barriers, and context of optimal pre-hospital ACS care to provide opportunities to reduce pre-hospital delays and improve acute cardiovascular care.
Methods and results
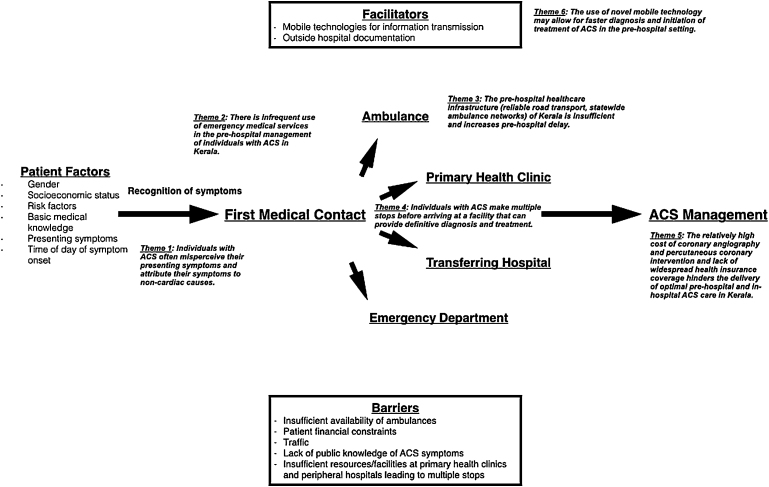
We conducted a qualitative study using in-depth interviews and focus group discussions with 27 ACS providers in Kerala, India to understand facilitators, barriers, and context to pre-hospital ACS care. Six themes emerged from these interviews and discussions: (1) individuals with ACS misperceive their symptoms as non-cardiac in origin; (2) emergency medical services are infrequently used; (3) insufficient pre-hospital healthcare infrastructure contributes to pre-hospital delay; (4) multiple stops are made before arriving at a facility that can provide definitive diagnosis and treatment; (5) relatively high costs of treatment and lack of widespread health insurance coverage limits care delivery; and (6) novel mobile technologies may allow for faster diagnosis and initiation of treatment in the pre-hospital setting.
Conclusions
Individualized patient-based factors (general knowledge of ACS symptoms, socioeconomic position) and broader systems-based factors (ambulance networks, coordination of transport) affect pre-hospital ACS care in Kerala. Improving public awareness of ACS symptoms, increasing appropriate use of emergency medical services, and building a infrastructure for rapid and coordinated transport may improve pre-hospital ACS care.
Keywords: Acute coronary syndromes, Pre-hospital care, Qualitative methods, Healthcare infrastructure
1. Introduction
1.1. Background
Ischemic heart disease is the leading cause of death in India.1 Deaths due to ischemic heart disease are frequently caused by acute coronary syndromes (ACS), which occur suddenly and outside of the hospital setting. In high-income countries, short-term case fatality rates for ACS, including acute myocardial infarction, have fallen dramatically from approximately 25% in the early 1980s to as low as 4% in the current era, due at least in part to a combination of medical therapy, reperfusion, and better overall intensive care, including availability of defibrillation.2, 3, 4, 5 More recent initiatives like the American Heart Association's Mission: Lifeline have sought to reduce morbidity and mortality from ACS in the United States by targeting the pre-hospital delivery of ACS care and improving healthcare system readiness and response to acute myocardial infarction.6 In India, despite the magnitude and well-recognized need for emergency medical care for patients with ACS, few data are available on the pre-hospital structure and delivery of ACS care.
1.2. Importance
The World Health Organization describes health systems in a framework that includes six “building blocks”: service delivery, health workforce, information, medicines, financing, and governance.7 For the optimal delivery of pre-hospital ACS care in India, each “block” in this model may be considered as a target for development. Inaccessibility to medical evaluation, insufficient numbers of trained pre-hospital ACS providers, lack of public knowledge of ACS symptoms, and relatively high costs of procedures for ACS treatment may contribute to suboptimal pre-hospital care in this population. In fact, limited pre-hospital data from a 2008 Indian ACS registry has shown that Indian patients with ACS delay an average of six hours from symptom onset to medical presentation and rarely use emergency medical transport services.8 Describing the pre-hospital experience of an ACS patient from a healthcare provider's perspective, particularly addressing the facilitators, barriers, and context of optimal pre-hospital care, may provide valuable insights into factors that contribute to excessive delay and targets for intervention. Furthermore, understanding ACS providers’ interactions with the healthcare system may provide opportunities to improve early detection and treatment in the critical pre-hospital time period.
1.3. Goals
To address these gaps in knowledge, we interviewed a variety of ACS providers and asked them to describe their experiences in caring for ACS patients. We sought to identify facilitators and barriers to the delivery of optimal pre-hospital care and engaging the healthcare system.
2. Methods
2.1. Study design and sample
We conducted a qualitative study of pre-hospital ACS providers and administrators (cardiologists, emergency room physicians, emergency room nurses, coronary care unit nurses, cardiac catheterization laboratory technicians, ambulance paramedics, a hospital administrator, and a state government health policy official) who were associated with the Acute Coronary Syndromes: Quality Improvement in Kerala (ACS QUIK) study, a cluster-randomized, stepped-wedge clinical trial investigating the implementation of a quality improvement toolkit on major adverse cardiovascular events in 63 hospitals throughout the South-Indian state of Kerala (ClinicalTrials.gov Identifier: NCT02256657). We chose a qualitative approach because we were interested in capturing critical aspects of a complicated process that is difficult to measure quantitatively and where little is known in the Indian context: namely, the individualized regional systems of the delivery of pre-hospital ACS care. Such methods are increasingly recognized as providing unique and valuable contributions to cardiovascular disease outcomes and health services research.9, 10 We used a grounded theory approach to guide our study, deriving explanations or theories inductively from the data we acquired.11
We selected an initial sample of participants who were uniquely able to provide insights of central importance to the study's purpose (purposive sampling frame) and who varied widely in the scope of their interactions with patients (maximum variability sampling). We then used a snowballing sampling technique12 based on these initial interviews and focus group discussions (FGDs). We contacted eligible participants either by a phone call or by an introductory letter sent via email explaining the purpose of the study and inviting their participation. We conducted in-depth interviews and FGDs in-person from October 2014 to March 2015. The final sample size was determined by the criterion of theoretical saturation, or the point at which no novel concepts emerged from successive interviews.13 Collective saturation was achieved on completion of 20 interviews and FGDs.
2.2. Data collection and measures
In-depth interviews and FGDs elicited individual provider perceptions and experiences through open, nondirective questions in a semi-structured format. The interviews began with a broad grand tour question14: “Tell me about your typical experience or interaction with an acute coronary syndrome patient prior to hospitalization.” We used standard, open-ended probes to encourage providers to increase the breadth or depth of responses and clarify their statements. Consistent with the grounded theory approach, data collection and analysis were iterative in nature, and our interview guide evolved as more interviews were conducted and analysis was done to ensure that emerging themes were explored in subsequent interviews.11, 15
Two members of the research team conducted all the interviews and FGDs in-person, except one interview, which was conducted via telephone. Interviews and FGDs ranged from nine minutes to one hour and six minutes in length, with a median length of 24 min (IQR: 24–30 min). All interviews and FGDs were conducted in English, audiotaped on two separate devices, and transcribed by one author (AP). To further describe the sample, we collected demographic data on each participant and the hospital where they worked. The study was approved by the Institutional Review Board at Northwestern University in Chicago, USA and the Ethics Committee of the Centre for Chronic Disease Control in Gurgaon, India, which is the national coordinating center of the ACS QUIK study. Interviewees and discussants provided written or verbal informed consent for their participation in the study.
2.3. Data analysis
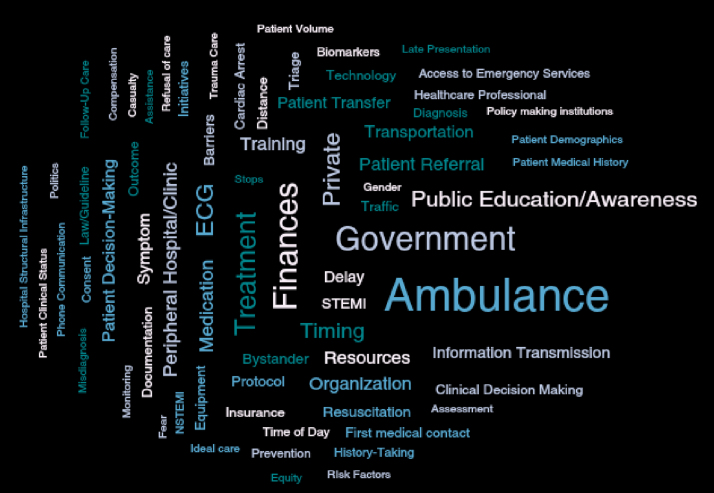
We analyzed data from the transcribed interviews by classifying quotes from participants with specific codes (labels assigning meaning to excerpted segments of text) developed iteratively. We created an initial code structure after the first several transcripts were reviewed, and as additional transcripts were added, we compared excerpts from new transcripts with previously coded sections to ensure consistent assignment of codes to similar data. We defined the properties and dimensions of each code as the code was created. We continued the process by refining and grouping codes into subcategories based on similarities with other codes, until no new concepts emerged in subsequent transcripts. One author (AP) coded all 19 transcripts independently, and individual codes were discussed among members of the research team. The process generated a set of 15 codes with 58 sub-codes that captured major concepts in the acquired data. Using the coded data, two authors developed the initial theoretical framework, which was updated with input from the study team to describe the key themes related to pre-hospital ACS care in Kerala as well as facilitators, barriers, and context for optimal pre-hospital ACS care. We used Dedoose v5.3.12 software (Manhattan Beach, USA) for data organization, analysis, and retrieval.
3. Results
3.1. Participant characteristics
Our sample included 27 pre-hospital ACS providers (Table 1). The majority of the providers were male (59%) and worked for a private hospital (70%). Six themes, derived from our theoretical framework (Fig. 1), characterized the experiences and insights of these providers related to pre-hospital ACS care (Fig. 2).
Table 1.
Participant characteristics.
| Participants | N = 27 (%) |
|---|---|
| Type of acute coronary syndrome provider | |
| Cardiologist | 7 (26) |
| Emergency room physician | 1 (4) |
| Nurse | 10 (37) |
| Catheterization laboratory technician | 2 (7) |
| Ambulance paramedic | 5 (19) |
| Hospital administrator | 1 (4) |
| Government official | 1 (4) |
| Male | 16 (59) |
| Employed by private hospital | 19 (70) |
Fig. 1.
Theoretical framework used to elucidate major themes from in-depth interviews and focus group discussions.
Fig. 2.
Code Cloud showing all included codes, with size of word corresponding to frequency with which code was used in the transcribed text.
3.2. Study themes
Theme 1
Individuals with ACS often misperceive their presenting symptoms and attribute their symptoms to non-cardiac causes.
All participants in our sample reported that there was a common lack of awareness among the general public about the severity and urgency of ACS symptoms. Many nurses and paramedics said that patients confused their symptoms with indigestion or related gastrointestinal problems.
“Some people think it's a gastric problem. That's why two, three days they are waiting for that. Then only, if the symptoms worsen, they will come to the hospital.” (Emergency Department Nurse, government hospital)
Cardiologists agreed that patients misinterpreted their symptoms and delayed evaluation until the symptoms became unbearable, leading to significant pre-hospital delay.
“Because many times… they think that it may be gas or it may be something else. Or it may be… till the time they develop a major, unbearable problem, like breathlessness or something happens that alerts everybody. And so, very often, there's a delay in the first stage.” (Cardiologist, private hospital)
Theme 2
There is infrequent use of emergency medical services in the pre-hospital management of individuals with ACS in Kerala.
Participants in this sample universally described infrequent use of emergency medical services in the pre-hospital setting for patients with ACS. Reasons given include: lack of knowledge from the patient's perspective that chest pain or other symptoms suggestive of ACS are appropriate reasons to request emergency medical services, the lack of availability of emergency medical services in particular areas throughout the state, among others. Participants reported that the government-funded ambulance system, reached by dialing the number 1-0-8, was more often used to seek medical attention for victims of road accidents. One participant said:
“If [it is] an accident, people will call 1-0-8. This chest pain, like that, they never call. Maybe they will come through bus or taxi or auto rickshaw.” (Emergency Department and Coronary Care Unit Nurse, government hospital)
Another participant reported:
“… people doesn’t (sic) know. Public people… maybe they are less educat[ed]… That's the problem… Otherwise the [motor vehicle] accident means, there will be bleeding, [the] patient is fainting [and] unconscious. People will [be] frighten[ed] and they will call the ambulance.” (Emergency Department Nurse, government hospital)
Of the private ambulance paramedics interviewed, all agreed that their primary role was to transfer patients from peripheral clinics or small hospitals without the ability to treat ACS patients to larger hospitals where thrombolysis, cardiac catheterization laboratories, or both were available. The private paramedics all said that they had minimal to no experience in responding to emergency requests from patient's homes.
Theme 3
The pre-hospital healthcare infrastructure (reliable road transport, statewide ambulance network) of Kerala is insufficient and increases pre-hospital delay.
Interviews with emergency department nurses and ambulance paramedics revealed that the government-funded ambulance system was functional in two of 14 administrative districts in the state of Kerala (Thiruvananthapuram and Alappuzha). In districts where the system was operating, there were too few ambulances to meet the needs of the population, resulting in patients opting for private modes of transportation because they proved faster. One emergency department nurse said:
“The 1-0-8 is not available every time. It's rare. Only one or two ambulances in one district or one panchayat or local area. That maybe already busy… Taxi [is] faster… Almost, I think, almost 75-80% [of] people will come [by] taxi or auto rickshaw… Ambulance, every time they are busy.” (Emergency Department Nurse, government hospital)
An emergency department nurse from a district where the 1-0-8 systems is operational said:
“And another thing is that only two ambulances are available in each center. If I am calling and the ambulance is engaged with another case, they won’t come. They can’t come.” (Emergency Department Nurse, private hospital)
Theme 4
Individuals with ACS make multiple stops before arriving at a facility that can provide definitive diagnosis and treatment.
Many interviewed participants agreed that patients with ACS in Kerala made multiple stops before arriving at a facility where definitive diagnostic and treatment measures could be provided due to lack of a coordinated system to transfer patients. They described that most patients arrived at a facility capable of thrombolysis or primary percutaneous coronary intervention only after first visiting a personal physician, a primary health center, a peripheral hospital, or some combination thereof.
“From onset of symptoms, an average of six hours passed. That's what we have seen. And, uh, nowadays I think it is coming down little bit. But the thing is they go to multiple centers. So many of the doctors are private doctors, they don’t know how to coordinate, they don’t know how to coordinate, so patients themselves, they go to their own private clinic where, we, in Kerala we have an advantage of having many private small, small clinics who have electrocardiogram facilities. So they go there, take an ECG, and from there they go to the nearest hospital which may be a primary healthcare center or a community healthcare or a nursing home kind of situation where the doctor looks at the ECG, makes a diagnosis. Some of them may not make a diagnosis. And then, as time elapses, [the] patient becomes sicker and then they go to another major hospital, [and] from there they refer. So, average is three to four stops. At least 2.5 stops I would say before they reach the CCU.” (Cardiologist, government hospital)
Theme 5
The relatively high cost of coronary angiography and percutaneous coronary intervention and lack of widespread health insurance coverage limits the delivery of optimal pre-hospital and early hospital ACS care in Kerala.
When asked to describe the barriers to optimal ACS care in Kerala, all providers mentioned the patient's financial status as a major factor. Given the predominantly private nature of the Indian healthcare system, the majority of patients seek care from private healthcare sources, if they can afford to do so.16 For those patients who cannot afford private care, our interviewees frequently discussed their struggles to provide the best care possible under the financial circumstances. When a poor ACS patient arrived at a private hospital, multiple providers described the process of stabilizing the patient acutely before eventual transfer to a government hospital for definitive treatment.
“Private hospitals won’t accept government insurance mostly. Most of them won’t accept government insurances. That's another thing. Financial constraints are crucial for treating that rural people… [If a patient cannot afford] then definitely they’ll refer, they’ll be referred to the government hospital, and they will do. But mostly they will postpone the case. They try medicines.” (Emergency Department Nurse, private hospital)
“If [the patient cannot pay], we even provide emergency management for the patient. If they wish to go to some other hospital, then we provide all the emergency care as possible, as much as, you know, possible to the patient and then patient be referred to the [government] medical college…Yeah, stabilize and then shift the patient with the ambulance…Usually if they can’t [pay], then, you know, that's the only thing that we can do from here.” (Emergency Department Nurse, private hospital)
This predicament can place ambulance drivers and paramedics in a particularly difficult situation because they may be forced to bear the responsibility of deciding where to take a patient for care based on their rapid assessment of a patient's ability to pay. A miscalculation on their part can result in them being reprimanded, as one describes:
“I will, uh, at that time I [took the patient to a private hospital] with the permission of the bystander. I shift the patient to private hospital. When the patient is discharged, the bystander claimed that, “We are unable to pay that much money.” So, what they do? At that time, the control room [gave] a message to me, identify the patient… ask the patient… about the financial problems, financial needs. Then only shift the patient. Otherwise we have to answer to their questions.” (Ambulance Paramedic, 1-0-8 government ambulance system)
The responsibility of determining what emergency treatment modalities a patient can afford (thrombolysis vs. primary percutaneous intervention) falls on the spectrum of providers ranging from ambulance paramedics to cardiologists. For example, nurses often address the details of costs for treatment options in the acute setting of the patient's presentation. One nurse describes:
“About treatment we will talk, that primary we can do…angioplasty. For that it will be nearly one lakh [rupees] (about $1,700) so they can’t pay that much money. So they will take the option of lysing… Lysis, that medicine for that [is] Rs. 4,500 (about $75)… The treatment cost, the travelling and all. If they are poor, means they won’t get more treatment, they won’t take. They will hesitate…” (Coronary Care Unit Nurse, private hospital)
When we discussed ACS patients’ finances with cardiologists, most said they took a direct approach in advising patients and their families about the most appropriate way to proceed with treatment. One cardiologist says:
“…as a doctor, when I see a patient, I help them to take the decision. Because, see, what I do is I decide this patient's best thing is this treatment and also find out what is their financial background, and if the financial background is good, I tell them, this (primary percutaneous coronary intervention) is the correct treatment.” (Cardiologist, private hospital)
Theme 6
The use of novel mobile technology may allow for faster diagnosis and initiation of treatment of ACS in the pre-hospital setting.
In our interviews and FGDs, one of the most useful facilitators of pre-hospital care described across providers was the use of mobile technologies (smartphones and social networking applications, such as What's App) to enable swift transmission of information, such as electrocardiograms performed in the field or at a peripheral hospital prior to transfer. Here, multiple cardiologists describe the way in which these mobile technologies have affected their care for ACS patients:
“…we do get transmissions of ECG… What we do now is that, you know, you use the iPhone and then, you know, you transfer the images.” (Cardiologist, private hospital)
“…now with the What's App going on, that's a huge change, everybody now gets ten ECGs in your What's App…” (Cardiologist, private hospital)
Some participants believed that more widespread use of such mobile technologies could allow remotely located clinics and hospitals to expedite transfer of ACS patients to better-equipped facilities.
“If I have some doubts with the ECG, sometimes we get a What's App ECG also. Through What's App other doctors from other hospitals they send up this…” (Cardiologist, private hospital)
“What's App can used as a medium for transacting vital information in time… Yeah, I feel that the modern technology's benefits should be for everybody. So I feel that everybody should assimilate. I am going as a consultant to the local hospital, nearby, 25 km. I have asked, I have shown these methods, urged them to form a What's App group. They are all slightly reluctant on the techni[cal] side, so it has not started.” (Cardiologist, private hospital)
4. Discussion
We identified recurrent themes that characterized the insights and experiences of the pre-hospital ACS providers whom we interviewed. Common barriers and relevant context to optimal pre-hospital ACS care that participants reported include: lack of recognition among the public of ACS symptoms that warrant emergency care, infrequent use of emergency medical services by the public, an insufficient system to transport ACS patients, and the high cost of ACS treatment, namely cardiac catheterization and primary percutaneous coronary intervention. A common facilitator to optimal pre-hospital care that participants reported was the use of a mobile social networking technology to share patient information quickly, so as to expedite diagnosis and management of ACS.
The reported infrequent use of emergency medical services in Kerala (Theme 2) is likely multifactorial with possible contributors including the public's lack of knowledge of the appropriate use of emergency medical services, lack of availability of a free government ambulance (1-0-8) service in many of the state's districts, too few ambulances in those states that do have a 1-0-8 service, which leads to longer wait times than might be experienced when compared with private transportation,17 lack of a coordinated system to transfer ACS patients for definitive therapy, and expensive private ambulance/hospital services (Themes 1, 3, 4, 5).
Many of our interviewees and discussants reported that patients in Kerala were likely to misinterpret their symptoms as non-cardiac in origin, thinking that the cause of their discomfort was indigestion. However, previous observational data has demonstrated that, compared to other ethnicities in the Asia-Pacific region and compared to Caucasians, Indians more often have typical chest pain when experiencing ACS.18 This disconnect may point to a need for greater education among the general Keralan and Indian public regarding the nature of ACS symptoms and, if those symptoms are present, the promptness with which evaluation should be sought. Examples of such public education efforts have been shown to be effective in the United States and Europe. For example, a 2001 collaborative effort by the American Heart Association and Minnesota cardiologists to educate area citizens about the signs and symptoms of acute myocardial infarction through a one-month education program consisting of presentations, news releases, print advertisements, and public service announcements showed an increase in emergency room visits for acute myocardial infarction when compared to baseline values from a year prior to beginning the educational program (18% vs. 12%, p < 0.05) and an increase in the number of patients transported by ambulance to the hospital for acute chest pain (47% vs. 27%, p < 0.05).19 In Switzerland, after a nationwide educational campaign between 2005 and 2008, median pre-hospital delay was reduced from 197 min during the pre-intervention period to 180 min during the post-intervention period (reduction 10% (95% confidence interval (CI) 6–14%), p < 0.001), in STEMI (reduction 10% (95% CI 5–14%), p < 0.001) and NSTEMI patients (reduction 11% (95% CI 4–17%), p = 0.001).20 In India, lack of recognition of ACS symptoms and use of emergency medical transport services leads to significant pre-hospital delay. Data from the CREATE registry of over 20,000 ACS patients estimate the average time from symptom onset to hospital arrival to be approximately 360 min (p < 0.001) with less than 6% of patients arriving by ambulance.8 To provide more optimal pre-hospital ACS care, increasingly widespread educational efforts to improve public awareness and link knowledge to action may help shorten the critical time period from symptom onset to first medical contact.21
In addition to a lack of public education, a disorganized network of ambulances and roads was frequently cited as a barrier to optimal pre-hospital ACS care. When ambulances are used, paramedics reported that single-lane roads and congested traffic prevent their ability to quickly navigate to the nearest medical center. Though gridlock traffic conditions can be present during peak hours, several recent examples of the speedy transfer of donor hearts for transplantation,22, 23 have encouraged many cities to develop systems that allow for similar quick delivery of care. The use of so-called “Green Corridors”, or the clearing of vehicular traffic to allow the passage of emergency medical convoys, has since been implemented in a few major Indian cities.24 Given that the frequency of ACS is far greater than that of cardiac transplant, it may be difficult to implement “Green Corridors” for ACS, but educating the public about giving priority to ambulances on the road may be a good starting point to speed up patient transportation. By emphasizing the delivery of expeditious care in these time-critical situations, local road and health authorities can play a major role in improving how pre-hospital care is delivered for all patients with emergency medical conditions, including those with ACS.
The lack of a coordinated system to transfer patients to centers where they can receive definitive treatment further complicates the pre-hospital care of ACS patients in Kerala. The formation of novel partnerships in other parts of India between the public and private sector to address this problem might serve as an example that can be applied to other localities. For instance, a pilot project in the South-Indian state of Tamil Nadu that employed the use of a hub-and-spoke model for pre-hospital STEMI diagnosis and triage demonstrated a mean time from symptom onset to hospital arrival of 170 min with 77% of patients arriving by ambulance (transport time: 5–99 min; mean: 44 min), a major improvement from the data reported in CREATE.8, 25 This model employs the use of a handheld mobile device that allows paramedics in the field to record a 12-lead electrocardiogram and instantly transmit it to an on-call cardiologist for decision-making, thus reducing unnecessary stops at hospitals that cannot provide definitive treatment. In areas where ambulance services are not available, the recording of an electrocardiogram by a more quickly available general practitioner has also been shown to be a cost-effective strategy to reduce disability and mortality from ACS.26
The most prohibitive barrier of all, in our interviews, was the socioeconomic position of the patient and his/her ability to pay for transport costs, diagnostic tests (including electrocardiograms and laboratory tests for cardiac biomarkers), and treatment (fibrinolytics and/or cardiac catheterization with primary percutaneous coronary intervention) related to his/her ACS care. The way a patient might finance an ACS admission was a major factor in clinical decision making among the spectrum of ACS providers ranging from ambulance paramedics to cardiologists. Given the predominantly private nature of the Indian healthcare system and lack of widespread health insurance coverage,16, 27 out-of-pocket expenses for ACS care are relatively high when compared to individual monthly incomes.28 Covering such costs can lead to significant financial distress for individuals and families. In a 2011 cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries including Argentina, China, Tanzania, and Kerala, India, catastrophic health spending (annual out-of-pocket health expenditures ≥40% of total, non-food household expenditures) and distress financing (financial activities, such as borrowing money from relatives/friends, taking loans from banks/other lenders, or selling assets that were directly related to the patient's most recent hospitalization) were highest in Kerala, India with rates of 92% and 64% respectively.28 Since 2008, government-sponsored insurance programs have been created to help address this problem for those who live below the poverty line,27 but the lack of widespread availability of such schemes to the growing Indian middle-class may make optimal ACS care out-of-reach for much of the population.29 Additionally, the nature of varying insurance schemes in Kerala and the coverage they provide may not be widely known to healthcare providers. For example, though one of our participants reported that private hospitals would not accept government insurance schemes, others reported a more complex system where individuals with incomes below the poverty line could apply for financial aid through a state-specific, lottery-funded government insurance scheme to raise funds for any acute ailment.30 The complex nature of the delivery of and reimbursement for healthcare services in Kerala and a lack of general knowledge by providers of the coverage these schemes cover would suggest that the development of a simpler and more integrated system may help streamline care.
The major facilitator of pre-hospital ACS care cited by our interviewees and discussants was the use of mobile technology in the form of social networking applications that allowed the quick transmission of patient information (such as electrocardiograms) for more efficient diagnosis and triage. Success of such technology has been demonstrated elsewhere in the literature. In 2006, data from the Timely Intervention in Myocardial Emergency – NorthEast Experience (TIME-NE) showed that the intervention of performing a wireless pre-hospital electrocardiographic transmission in STEMI patients was associated with a lowering in the median door-to-reperfusion time from 101 min in the pre-intervention group to 50 min in the intervention group (p < 0.001).31 Similarly, in the ST-Segment Analysis Using Wireless Technology in Acute Myocardial Infarction (STAT-MI) trial, simultaneous transmission of a pre-hospital 12-lead electrocardiogram from emergency medical services personnel in the field to the emergency department and offsite cardiologists using Bluetooth devices, receiving/transmitting stations, dedicated e-mail servers, and smartphones was associated with an improvement in door-to-intervention time from 146 min prior to pre-hospital electrocardiogram transmission to 80 min with use of the network (p < 0.01).32 In both studies, pre-hospital electrocardiograms were transmitted via secure hospital intranet, networks, and servers. Caution must be exercised when using applications such as What's App, iMessage, or other applications due to lower levels of encryption. While the use of social networking applications allows the quick transfer of valuable data, the security of the process by which the data are submitted must also be considered to ensure that patient privacy is maintained. Though such social networking applications have been reported as useful thus far, providers must know these technologies will not be a panacea, and that other data storage and transmission infrastructure, like an electronic medical record, may be necessary.
4.1. Comparison with mission: lifeline
In the United States, the American Heart Association has taken an active role in trying to improve pre-hospital systems of care for ACS patients. In a 2012 report from its Mission: Lifeline initiative, which aims to improve the quality of care and outcomes for patients with STEMI and to improve healthcare system readiness and response to STEMI, predominant system characteristics that were identified in STEMI systems of care included: patient acceptance at percutaneous coronary intervention hospital regardless of bed availability (N = 346, 97%); single phone call activation of catheterization laboratory (N = 335, 92%); data registry participation (N = 311, 84%); and pre-hospital activation of the laboratory through emergency department notification without cardiology notification (N = 297, 78%).6 Based on our interviews, these commonly occurring procedures are not the norm in Kerala. The financial status of patients weighs heavily on their ability to be admitted to hospitals in the private sector, cardiac catheterization laboratory activation is performed via multiple individual phone calls to on-call personnel, and until recent years, few hospitals have participated in data registries.33 Increasing participation in both registries, such as the Kerala ACS Registry of 25,748 patients, and clinical trials, such as the ongoing Acute Coronary Syndromes Quality Improvement in Kerala (ACS QUIK) clinical trial is promising for future cardiovascular quality improvement.33 In ACS QUIK, the use of audit and feedback reports to assess performance measures, standardized admission/discharge checklists, patient education materials, and code blue/rapid response team protocols aims to target quality improvement for in-hospital ACS care. Data collection in ACS QUIK also includes pre-hospital metrics including mode of transportation to the hospital, times of symptom onset, first medical contact, initiation of treatment, presence of pre-hospital electrocardiogram, etc. Our hope is that a combination of the qualitative data presented here and the quantitative data being collected for ACS QUIK will serve as a starting point for the development of targeted interventions to optimize pre-hospital ACS care in the future.
4.2. Strengths and limitations
Our study has several strengths. Our use of qualitative methodology has allowed us to capture a variety of perspectives surrounding a complex problem that would not have been possible with a purely quantitative approach. The rich, first-hand data provided by our participants provide novel insights into the facilitators, barriers, and context of optimal pre-hospital ACS care. Our research strategy took care to ensure data reliability through the consistent use of a pre-prepared interview guide, audiotaping interviews on two separate devices, independent transcript preparation, standardized coding and analysis using qualitative software, and maintenance of study materials, including consent forms, to achieve auditability.15
Our study also has several limitations. First, our participants were chosen from sites participating in an ongoing clinical trial and may not be representative of all clinical centers throughout Kerala, thus introducing the possibility of selection bias and not being representative of India as a whole. However, we used a purposive sampling frame with maximum variability sampling to include the widest range of perspectives possible. Second, interviews and FGDs we held were solely with ACS providers. However, the participation of other stakeholders in this process, such as ACS patients and the management of ambulance companies might have added valuable insights and is an area of future research within our group. Third, all interviews were conducted in English. Though all participants had some working knowledge of the English language and most were entirely fluent in English, language barriers may have led to difficulty in communicating in English, which was their second or third language. Fourth, recall bias may have affected participants’ responses of their experiences in caring for ACS patients. Fifth, the differences between Kerala's relatively more developed health system and education levels compared to the rest of India limit the generalizability of our results. Finally, the qualitative nature of our work does not allow us to report useful quantitative data, such as breakdown of treatment modalities used, outcomes, and door-to-balloon times, which are important metrics in ACS care. However, future work from our group will aim to collect and report this data as part of ACS QUIK.
5. Conclusions
Because cardiovascular disease is the leading cause of death in India, generating hypotheses about the facilitators, barriers, and context for optimal pre-hospital ACS care is essential for the development of targeted interventions to reduce pre-hospital delay. Results from our study provide novel insights about gaps in pre-hospital systems of care that must be addressed to improve care delivery. Identifying opportunities to improve public awareness of ACS symptoms and appropriate use of emergency medical services, and creating simplified, coordinated systems to streamline ACS care are important targets for healthcare providers, researchers, and policymakers to improve outcomes for ACS patients in Kerala and India.
Conflicts of interest
The authors have none to declare.
Acknowledgements
This work was supported by the National Institutes of Health/National Heart, Lung, and Blood Institute through the Fogarty International Clinical Research Scholars and Fellows Program at Vanderbilt University (R24 TW007988) and the American Recovery and Reinvestment Act.
References
- 1.Lozano R., Naghavi M., Foreman K. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gillum R.F. Trends in acute myocardial infarction and coronary heart disease death in the United States. J Am Coll Cardiol. 1994;23:1273–1277. doi: 10.1016/0735-1097(94)90367-0. [DOI] [PubMed] [Google Scholar]
- 3.Krumholz H.M., Normand S.-L.T., Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130:966–975. doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flynn A., Moscucci M., Share D. Trends in door-to-balloon time and mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Intern Med. 2010;170:1842–1849. doi: 10.1001/archinternmed.2010.381. [DOI] [PubMed] [Google Scholar]
- 5.de Vreede J.J., Gorgels A.P., Verstraaten G.M. Did prognosis after acute myocardial infarction change during the past 30 years? A meta-analysis. J Am Coll Cardiol. 1991;18:698–706. doi: 10.1016/0735-1097(91)90792-8. [DOI] [PubMed] [Google Scholar]
- 6.Jollis J.G., Granger C.B., Henry T.D. Systems of care for ST-segment-elevation myocardial infarction: a report From the American Heart Association's Mission: Lifeline. Circ Cardiovasc Qual Outcomes. 2012;5:423–428. doi: 10.1161/CIRCOUTCOMES.111.964668. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Health Services Development. Available from: http://www.wpro.who.int/health_services/health_systems_framework/en/HO Accessed 04.05.15.
- 8.Xavier D., Pais P., Devereaux P.J. CREATE registry investigators. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 9.Curry L.A., Nembhard I.M., Bradley E.H. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119:1442–1450. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 10.Krumholz H.M., Bradley E.H., Curry L.A. Promoting publication of rigorous qualitative research. Circ Cardiovasc Qual Outcomes. 2013;6:133–134. doi: 10.1161/CIRCOUTCOMES.113.000186. [DOI] [PubMed] [Google Scholar]
- 11.Glaser B.G., Strauss A.L. Aldine Publishing Company; Chicago, IL: 1967. The Discovery of Grounded Theory; Strategies for Qualitative Research. [Google Scholar]
- 12.Biernacki P, Waldorf D. Snowball Sampling. Available from: http://ftp.columbia.edu/itc/hs/pubhealth/p8462/misc/biernacki_lect4.pdf Accessed 29.04.15.
- 13.Morse J.M. The significance of saturation. Qual Health Res. 1995;5:147–149. [Google Scholar]
- 14.Crabtree B.F., Miller W.L. 2nd ed. Sage Publications; Thousand Oaks, CA: 1999. Doing Qualitative Research. [Google Scholar]
- 15.Lichtman J.H., Leifheit-Limson E.C., Watanabe E. Symptom recognition and healthcare experiences of young women with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2015;8:S31–S38. doi: 10.1161/CIRCOUTCOMES.114.001612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar C, Prakash R. Public-Private Dichotomy in Utilization of Health Care Services in India. Available from: http://www.consiliencejournal.org/index.php/consilience/article/viewFile/76/55 Accessed 29.04.15.
- 17.CAG report pulls up Health Department. Available from: http://www.thehindu.com/todays-paper/tp-national/tp-kerala/cag-report-pulls-up-health-department/article7026348.ece Accessed 29.04.15.
- 18.Greenslade J.H., Cullen L., Parsonage W. Examining the signs and symptoms experienced by individuals with suspected acute coronary syndrome in the Asia-Pacific region: a prospective observational study. Ann Emerg Med. 2012;60 doi: 10.1016/j.annemergmed.2012.05.008. 777–785.e3. [DOI] [PubMed] [Google Scholar]
- 19.Wright R.S., Kopecky S.L., Timm M. Impact of community-based education on health care evaluation in patients with acute chest pain syndromes: the Wabasha Heart Attack Team (WHAT) project. Fam Pract. 2001;18:537–539. doi: 10.1093/fampra/18.5.537. [DOI] [PubMed] [Google Scholar]
- 20.Naegeli B., Radovanovic D., Rickli H. Impact of a nationwide public campaign on delays and outcome in Swiss patients with acute coronary syndrome. Eur J Cardiovasc Prev Rehab. 2011;18(2):297–304. doi: 10.1177/1741826710389386. [DOI] [PubMed] [Google Scholar]
- 21.Prabhakaran D., Jeemon P., Mohanan P.P. Management of acute coronary syndromes in secondary care settings in Kerala: impact of a quality improvement programme. Natl Med J India. 2008;21:107–111. [PubMed] [Google Scholar]
- 22.Hemlatha K, Sunitha Rao R. Bangalore, Chennai join forces for inter-state heart transplant – The Times of India. Available from: http://timesofindia.indiatimes.com/city/chennai/Bangalore-Chennai-join-forces-for-inter-state-heart-transplant/articleshow/41648762.cms Accessed 29.04.15.
- 23.Upreti M. Gurgaon, Delhi Police make green corridor to transfer heart for a teen, cover 32 kms in 29 minutes. Available from: http://ibnlive.in.com/news/gurgaon-delhi-police-make-green-corridor-to-transfer-heart-for-a-teen-cover-32-kms-in-29-minutes/521479-3-244.html Accessed 29.04.15.
- 24.Desouza PR. India's heart is in the right place. Available from: http://www.thehindu.com/opinion/lead/indias-heart-is-in-the-right-place/article7000184.ece Accessed 29.04.15.
- 25.Alexander T., Mullasari A.S., Narula J. Developing a STEMI system of care for low- and middle-income countries: the STEMI-India model. Global Heart. 2014;9:419–423. doi: 10.1016/j.gheart.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Schulman-Marcus J., Prabhakaran D., Gaziano T.A. Pre-hospital ECG for acute coronary syndrome in urban India: a cost-effectiveness analysis. BMC Cardiovasc Disord. 2010;10:13. doi: 10.1186/1471-2261-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Virk A.K., Atun R. Towards universal health coverage in India: a historical examination of the genesis of Rashtriya Swasthya Bima Yojana – The health insurance scheme for low-income groups. Public Health. 2015 doi: 10.1016/j.puhe.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Huffman M.D., Rao K.D., Pichon-Riviere A. A cross-sectional study of the microeconomic impact of cardiovascular disease hospitalization in four low- and middle-income countries. PLoS ONE. 2011;6:e20821. doi: 10.1371/journal.pone.0020821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kharas H. 2011. The Emerging Middle Class in Developing Countries.http://siteresources.worldbank.org/EXTABCDE/Resources/7455676-1292528456380/7626791-1303141641402/7878676-1306699356046/Parallel-Sesssion-6-Homi-Kharas.pdf Available from: Accessed 29.04.15. [Google Scholar]
- 30.Government of Kerala, The Official Web Portal. Available from: http://www.kerala.gov.in/index.php?option=com_content&view=article&id=4494&Itemid=3307 Accessed 04.05.15.
- 31.Adams G.L., Campbell P.T., Adams J.M. Effectiveness of prehospital wireless transmission of electrocardiograms to a cardiologist via hand-held device for patients with acute myocardial infarction (from the Timely Intervention in Myocardial Emergency, NorthEast Experience [TIME-NE]) Am J Cardiol. 2006;98:1160–1164. doi: 10.1016/j.amjcard.2006.05.042. [DOI] [PubMed] [Google Scholar]
- 32.Dhruva V.N., Abdelhadi S.I., Anis A. ST-segment analysis using wireless technology in acute myocardial infarction (STAT-MI) trial. J Am Coll Cardiol. 2007;50:509–513. doi: 10.1016/j.jacc.2007.04.049. [DOI] [PubMed] [Google Scholar]
- 33.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]