Abstract
The diagnosis of idiopathic dilatation of pulmonary artery is challenging because its clinical recognition is difficult and various other causes of dilated pulmonary artery need to be excluded. The clinical findings mimic various common cardiac disorders and both invasive and non-invasive investigations should be done to arrive at the diagnosis. It is a known clinical entity but etiology and pathophysiology are largely unknown. The current echocardiographic and catheterization based diagnostic criteria, may not be satisfied completely in a particular patient and need to be revisited in view of newer imaging modalities. There is paucity of information about the natural history of the disease with attendant lack of clarity in treatment guidelines. Certain cases may progress to huge dilatation and consequent serious implications. It is a rare disease and is the diagnosis of exclusion.
Keywords: Pulmonary artery, Idiopathic dilatation, Aneurysm
1. Introduction
Idiopathic dilatation of the pulmonary artery (IDPA) was first reported by Wessler and Jaches.1 The clinical relevance and challenges in the diagnosis of idiopathic dilatation of pulmonary artery lie in exclusion of various other causes of dilated pulmonary artery. Clinical diagnosis is challenging because the symptoms are highly variable and clinical findings may mimic common cardiac disorders like mild pulmonary stenosis, atrial septal defect and pulmonary artery hypertension. The purpose of this article is to emphasize on varied clinical presentations, the need for an inclusive and comprehensive evaluation of patients, given the fact that clinical and investigative findings may be not coherent and to discuss the treatment options in light of natural history of the disease.
2. Incidence
Idiopathic dilatation of pulmonary artery is an uncommon anomaly occurring in 0.6% (in isolation) of patients with congenital heart disease.2 In a series of autopsy cases of 109,571 cases Deterling and Clagett reported an incidence of 0.0073%.3 The exact incidence is underreported because of very benign nature of disease in most of the cases. In the past the diagnosis was based on cardiac catheterization/angiocardiogram or autopsy, but with the advancement in echocardiography, cardiac computed tomography or cardiac magnetic resonance (CMR), more number of cases are being reported.
3. Etiopathology
Not much is known about the etiology of idiopathic dilatation of pulmonary artery. Most of the cases have been reported in adults, but there is description of this disease in children which supports the theory of congenital origin.4 Preponderance toward any sex is not described. The main pulmonary artery and the origin of the right and left main pulmonary arteries are mainly affected. Assman5 postulated theory of an unequal division of truncus arteriosus communis as the possible mechanism which was supported by Kourilsky et al.,6 Laubry et al.7 and Gold8 while Greene et al.,9 did not agree with this theory. Laubry and Gold suggested the association of hypoplastic aorta with dilated pulmonary artery – grosse pulmonaire – petite aorte. According to Kaplan10 this anomaly was due to maldevelopment of entire pulmonary tree. Carlotti et al.11 demonstrated that there was no parallelism between the dilatation of pulmonary artery in and the pressure or cardiac output in contrast to earlier theories relating dilatation of pulmonary artery, cardiac output and pulmonary blood flow in cases of IDPA. Congenital weakness in the wall of the pulmonary artery is the most accepted theory keeping in with the concept of medial deficiency and aneurysm formation.12, 13 Deb et al. also suggested cystic medial degeneration of arterial wall as an etiological factor in idiopathic dilatation of pulmonary artery.14 An association between cystic medial degeneration and increased hemodynamic forces leading to aneurysm formation is postulated, even in the absence of a bona fide connective tissue disorder.13 Pulmonary artery aneurysms have been associated with structural cardiac anomalies, structural vascular anomalies, vasculities and infection. Idiopathic term should be applied when all these have been excluded conclusively.
4. Pathophysiology
The disease process usually involves the central pulmonary artery, however it may extend to any of the main branches. A few studies with histological evaluation reported evidence of cystic medial deficiency in such cases. With the constant blood flow across the heart and great vessels, pressure varies directly with resistance to flow (resistance = pressure/flow). As the dilatation becomes more, the resistance to blood flow in dilated pulmonary artery is decreased and as well proportional drop in pressure, which accounts for the pressure gradient as the driving force between right ventricle and the pulmonary artery during cardiac systole without right ventricular hypertension. At the same time, progressive and hugely dilated pulmonary artery results in reverse systolic flow due to increased capacitance. This reverse systolic flow persists in early diastole.
5. Clinical picture
Absence or mildness of symptoms was the most significant finding in all previous studies. Patients may present with exertional dyspnea, palpitation, fatigue and chest pain. Symptoms usually appear with onset of complications like compression of nearby structures, dissection, thrombosis or rupture. Zhao et al. reported 21 cases of IDPA. Majority of patients were asymptomatic (66.67%) and all patients had normal respiratory and cardiovascular function. It was misdiagnosed (clinically) as pulmonary stenosis (42.86%), secundum atrial septal defect (38.50%) and pulmonary artery hypertension (28.57%).15 Around 10% patients had a duration of illness lasting for more than 20 years. IDPA has been ascribed to as one of the rare cause of angina pectoris which can be missed at times.16 The idiopathic dilatation of the pulmonary artery may be extensive (aneurysm) and patients have more symptoms, especially breathlessness. Taussig17 described a case of severe form of idiopathic dilatation of the pulmonary artery where postural changes in hugely dilated pulmonary artery constricted the trachea and its main branches causing attacks of cyanosis with severe dyspnea. Dilated pulmonary arteries (from any cause) can lead to compression of left main coronary artery18 and even sudden cardiac death has been described in cases of IDPA.19
Clinical examination is not conclusive because IDPA can mimic findings of common cardiac disorders. The second heart sound may be normal or accentuated but splitting is usually fixed. In cases of hugely dilated pulmonary artery/aneurysm the second heart sound may be soft. The pulsations of dilated arteries may be felt in second space on the lateral sternal border. A pulmonic ejection systolic murmur is usually present. The systolic murmur in cases of idiopathic dilatation of pulmonary artery does not show typical transmittance to subclavicular or interscapular area as compared to pulmonary stenosis with dilatation pulmonary artery. The systolic murmur was thought to be originating from dilatation of pulmonary ostium and greater stress in a dilated pulmonary artery.8, 20 Kaplan et al.10 emphasized that the only constant feature of murmur is its inconstancy. Sometimes a diastolic murmur can also be present.7 The systolic ejection click may be present as in other conditions with dilatation of great vessels. The typical phonocardiographic findings were described by Karnegis et al.,21 Pulmonary insufficiency of varying severity is observed in majority of cases although consistently not present in all of the patients.
6. Investigations
6.1. ECG
It is usually normal but deviation of the cardiac axis toward the right or bundle branch blocks can be present.
6.2. Chest X-ray
In idiopathic dilatation of pulmonary artery, lung parenchyma and its vascularity are normal with normal cardiothoracic ratio and dilated pulmonary artery. The characteristic picture of pulmonary stenosis e.g. enlarged main pulmonary artery with diminished vascularity is absent in this condition (Fig. 1).22 The hyperemic lungs fields with hilar dance, common in large left to right shunts, are also absent. It is interesting that the pattern of dilatation is the same as in uncomplicated pulmonary stenosis (localization is restricted to the trunk or occasionally to one of the main branches of the pulmonary artery, but no dilatation of the peripheral branches is present).
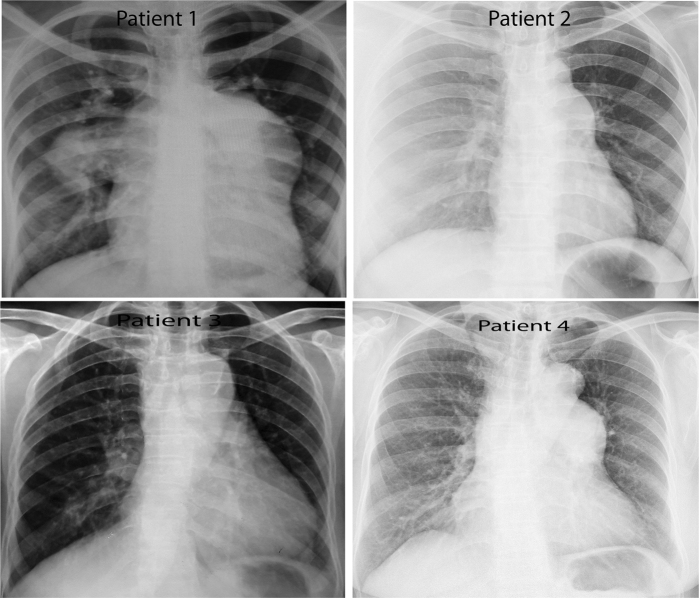
Fig. 1.
Posterior anterior chest radiograph of four patients: Patient (1) – bulging of left pulmonary mediastinal margin with prominent right pulmonary artery. Patient (2) – bulge at second curve of left cardiac border. Patient (3) – prominent pulmonary bay. Patient (4) – bulge at second curve of left cardiac border.
6.3. Echocardiography
Although idiopathic dilatation of pulmonary artery is mainly the diagnosis of exclusion, authors have given criteria for diagnosing idiopathic dilatation of pulmonary artery. In 1949, Greene9 proposed the criteria for diagnosis of idiopathic dilatation of pulmonary artery (Table 1, Fig. 2). Desmukh23 proposed fifth criteria of normal pressure in the right ventricle and pulmonary artery.
Table 1.
Diagnostic criteria for idiopathic dilatation of pulmonary artery.
| Author | Diagnostic criteria |
|---|---|
| Greene et al. (1949) | (1) Simple dilatation of the pulmonary trunk with or without involvement of the rest of arterial tree |
| (2) Absence of abnormal intracardiac or extracardiac shunts | |
| (3) Absence of chronic cardiac or pulmonary disease | |
| (4) Absence of arterial diseases such as syphilis, arteriosclerosis or arteritis | |
| Deshmukh et al. (1960) | (1) Simple dilatation of the pulmonary trunk with or without involvement of the rest of arterial tree |
| (2) Absence of abnormal intracardiac or extracardiac shunts | |
| (3) Absence of chronic cardiac or pulmonary disease | |
| (4) Absence of arterial diseases such as syphilis, arteriosclerosis or arteritis | |
| (5) Normal pressure in the right ventricle and pulmonary artery | |
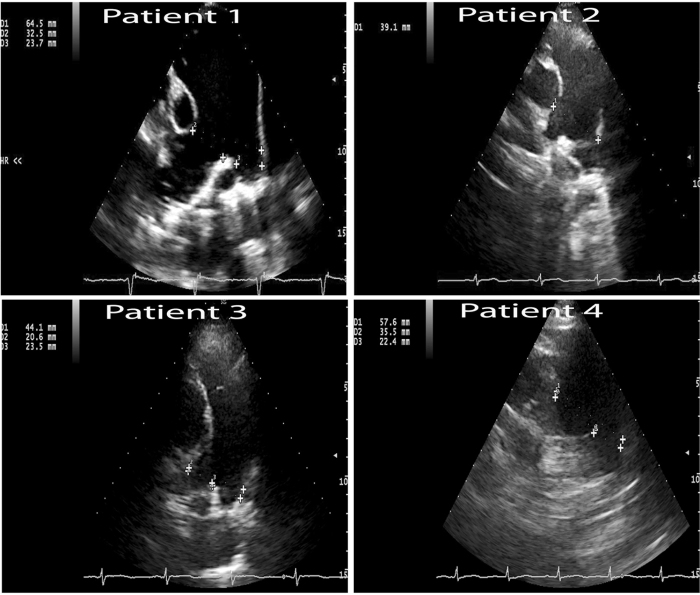
Fig. 2.
Parasternal short axis showing dilated main pulmonary artery. MPA measures at its bifurcation: patient (1) – 64.5 mm, patient (2) – 39.1 mm, patient (3) – 44.1 mm and patient (4) – 57.6 mm.
The other echocardiographic based diagnostic criteria were described by Boutin et al.24 in 1994. It was based on study of 30 patients in which 17 had characteristic radiological findings and 13 others had clinical signs of idiopathic dilatation of the pulmonary artery, compared with a group of 20 normal control subjects. Comparison with the control group showed significant differences (p < 0.05) in 4 parameters:
-
1)
The diameter of the pulmonary artery at the bifurcation/m2 body surface area (2.8 ± 0.4 cm versus 2.4 ± 0.4 cm)
-
2)
The diameter of the aorta 2 cm beyond the aortic valve/m2 of body surface area (1.7 ± 0.3 cm versus 2.1 ± 0.7 cm)
-
3)
The ratio of pulmonary artery/aortic diameters at the valve rings (1.4 ± 0.2 versus 1.1 ± 0.02)
-
4)
The ratio of the aorta 2 cm beyond the valve/aortic ring (1.02 ± 0.07 versus 1.09 ± 0.09).
Van Buchem et al.25 reported that the normal diameter of pulmonary artery ranged from 22 to 33 mm. These three sets diagnostic criteria may not be satisfied together in a particular patient owing to different parameters used by different authors. Asayama et al.26 described fine systolic fluttering of pulmonary valve in IDPA. Echocardiography is also useful in assessing parameters which help in making treatment decisions such as right ventricular function, pulmonary regurgitation and hemodynamic parameters in excluding other causes of dilated pulmonary artery.
6.4. Cardiac computed tomography (CT)
Cardiac computed tomography is very helpful in assessing the size of pulmonary artery and excluding other causes of dilated pulmonary artery. Owing to its high spatial resolution, contrast enhanced computed tomography is considered to be the primary technique for diagnosing pulmonary artery dilation as it offers a unique opportunity to evaluate the presence, size, shape, exact location of the aneurysm, and concomitant cardiovascular abnormalities (Fig. 3). The upper limit of the normal diameter of the main pulmonary artery on computed tomography is 29 mm and of the right interlobar artery is 17 mm.27 CT angiography is excellent modality because it readily identifies mural thrombus, dissection or any other abnormalities. Multiplanar reconstruction can help plan surgical intervention. There are no specific criteria on CT imaging developed for diagnosing IDPA.
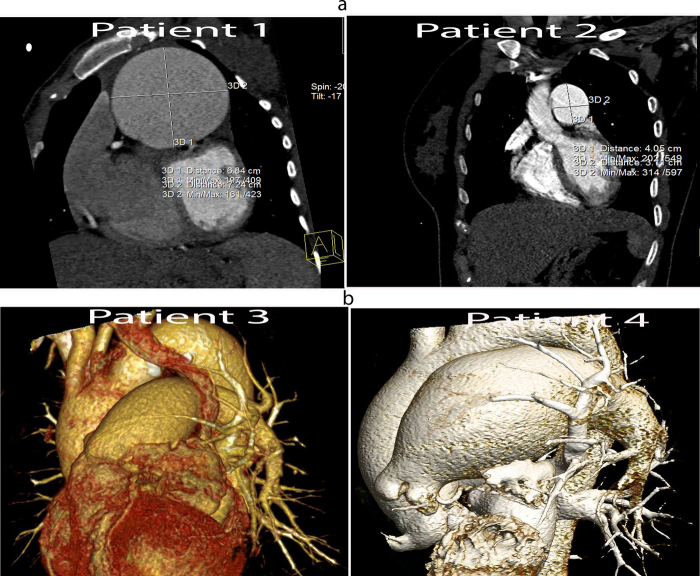
Fig. 3.
(a) CT angiography with 128 slices CT scan. Reconstructed short axis view at the level of main pulmonary artery shows dilated main pulmonary artery. Diameter of MPA of patient (1) is 7.2 cm × 6.8 cm and patient (2) is 4 cm × 3.1 cm. (b) Volume rendered images showing dilated pulmonary trunk. Diameter of MPA of patient (3) is 3.63 cm × 3.75 cm and patient (4) is 4.76 cm × 4.88 cm.
6.5. Cardiac magnetic resonance imaging (CMR)
Magnetic resonance imaging is very useful non-invasive imaging modality, especially in the detection of possible intimal flap. It may show the arterial wall thickening in connective tissue diseases and also provide information regarding hemodynamics in cases of post-stenotic dilatation due to disease involving the pulmonary valve. Cardiac MRI has been shown to detect milder forms of pulmonary stenosis which is largely undetectable by other means.28 Ugolini et al. described four cases where CMR played a major role in diagnosis and ascribed that CMR is accurate, reproducible measure of artery structure and a must for diagnosis and follow up.29 CMR is a useful non-invasive modality with advantages of measuring the precise diameters, evaluation of the right ventricular outflow tract, quantification of pressure gradient of pulmonary artery stenosis without need of contrast agents or radiation exposure. CMR is a excellent tool to rule out other causes of dilated pulmonary artery.
6.6. Cardiac catheterization
Heart catheterization is deemed essential for establishing the diagnosis, while it helps to rule out other causes of dilated pulmonary artery conclusively but more so it establishes the normal pressures in heart chambers quintessential for diagnosis. In idiopathic dilatation of pulmonary artery the systolic pressure in right ventricle and pulmonary artery are equal, the pressure in right ventricle is not increased and normal oxygen saturations in various parts of right heart and vessels. Angiocardiogram confirms the absence of shunts and shows dilated pulmonary artery. If the right ventricle pressure exceeds pulmonary artery even though it is in the normal range it is nonetheless possible that slight pulmonary stenosis is present.
It is essential to note that in a study by Van Buchem et al.,25 in patients with pulmonary valve stenosis, poststenotic dilatation was observed when the pressure gradient was more than 25 mmHg. While patients with IDPA showed remarkably dilated pulmonary arteries in the absence of pressure gradients (≤5 mmHg). In 1987, Futagami et al.,30 reported 59 cases of idiopathic dilatation of the pulmonary artery. Niida et al.,28 analyzed the pressure data of 39 of these patients. A pressure gradient of ≤5 mmHg, considered as no or trivial pressure gradient was observed in 64% of the 39 patients, but 36% of patients showed mild pressure gradients (6–22 mmHg) between the right ventricle and the pulmonary artery. These data suggest that a mild pressure gradient might often be seen in patients with idiopathic pulmonary aneurysms. In such cases it is necessary to image pulmonary valves and demonstrate morphological normalcy. In online supplementary table, we present four of our cases which highlight the variability in clinical presentation and diagnostic tests in cases of IDPA.
7. Prognosis and natural history
Prognostic evaluation of idiopathic dilatation of pulmonary artery is limited by the number of clinically studied cases and lack of adequate follow up but it is believed to be a benign anomaly. Most of the reported cases have survived into sixth or seventh decade. The increase in size of the main pulmonary artery can be progressive. The appearance of exertional dyspnea and a restrictive impairment of ventilatory capacity may be due to left ventricular strain and space-occupying compressive effect of the expanding pulmonary arteries. Periodical follow up is advisable to check for formation of aneurysm or regurgitation. Fang and Tsai suggested that prognosis of IDPA is better than other causes of pulmonary artery dilatation.31 Ring et al.,32 stressed upon the fact that a long period of observation should be considered to be a further criterion for diagnosis, as in some patients who appear to have this condition, an underlying pathology will become apparent.
8. Treatment
No definite guidelines exist for treatment recommendations in IDPA. Although surgical repair is recommended if isolated aneurysm of pulmonary artery is large (>6 cm) or they are symptomatic because risk of rupture or dissection is high.14, 33 The criteria for intervention are based on limited data on natural history.34 Various techniques of repair have been described, including aneurysm plication (aneurysmorrhaphy or arterioplasty), pericardial patch reconstruction, and interposition grafting with allografts or synthetic textile grafts.
9. Conclusion
Clinical presentation of IDPA is very variable and the manifestation range from being incidentally detected to florid and at times catastrophic scenarios. Whenever a patient presents with no or minimal symptoms with systolic or diastolic or both murmurs at the base of the heart with evidence of dilated pulmonary artery, idiopathic dilatation of the pulmonary artery should be considered in the differential diagnosis. Benign nature with nonprogressive character of the disease favors the diagnosis. It is a rare disease and is the diagnoses of exclusion. Majority cases will have no or minimal gradient (0–5 mmHg) between right ventricle and pulmonary artery but presence of mild gradient (6–22 mmHg) does not rule out IDPA (all secondary causes must be ruled out and pulmonary valve morphological normalcy should be established). Pulmonary valve disease must be excluded in such cases using appropriate imaging modality (e.g. CMR). Any rapid progression of symptoms with apparent idiopathic dilatation of pulmonary artery may have an arteritis or connective tissue disorder. Rarely it may give rise to huge aneurysm or progressive pulmonary regurgitation which may cause symptoms. So even asymptomatic cases need to be followed up. It is very interesting to note that a particular patient may not satisfy all of the three sets of current diagnostic criteria and diagnosis should be based on both invasive and non-invasive investigations including the clinical perspective.
Conflicts of interest
The authors have none to declare.
Footnotes
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.ihj.2016.07.009.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.Wessler H., Jaches L. The Southworth Company; Troy, NJ/New York: 1923. Clinical Roentgenology of Disease of the Chest; p. 26. [Google Scholar]
- 2.Abbott M.E. 1936. Atlas of Congenital Cardiac Disease. [Google Scholar]
- 3.Deterling R.A., Clagett O.T. Aneurysm of the pulmonary artery: review of the literature and report of a case. Am Heart J. 1947;34:471–499. doi: 10.1016/0002-8703(47)90527-9. [DOI] [PubMed] [Google Scholar]
- 4.Balboni F.A., Lopresti J. Congenital idiopathic dilatation of the pulmonary artery in children. A report of seven cases. Heart Cent Bull (Roslyn) 1961;17:1–21. [PubMed] [Google Scholar]
- 5.Assman H. 4th ed. F.C.W. Vogel; Leipzig: 1929. Roentgendiagnostik der inneren Erkrankungen. [Google Scholar]
- 6.Kourilsky R., Guede M., Regaud J. Les dilatations congenitales de l’artere pulmonaire. Bull Mem Soc Med Hop Paris. 1940;56:772. [Google Scholar]
- 7.Laubry C., Routier D., Heim de Balsac R. Grosse pulmonaire. Petite aorte. affection congenitale. Bull Mem Soc Med Hop Paris. 1940;56:847. [Google Scholar]
- 8.Gold M. Congenital dilatation of the pulmonary arterial tree. Arch Int Med. 1946;78:197. doi: 10.1001/archinte.1946.00220020075005. [DOI] [PubMed] [Google Scholar]
- 9.Greene D.G., Baldwin E.F., Baldwin J.S., Himmmelstein A., Rob C.E., Cournand A. Pure congenital pulmonary stenosis and idiopathic congenital dilatation of the pulmonary artery. Am J Med. 1949;6:24. doi: 10.1016/0002-9343(49)90004-2. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan B.M., Schlichter J.G., Graham G., Miller G. Idiopathic congenital dilatation of the pulmonary artery. J Lab Clin Med. 1953;41:697. [PubMed] [Google Scholar]
- 11.Carlotti J., Sicot J.R., Joly F. Etudes de la dynamique des grosses arteres pulmonaires. Arch Mal Coeur Vaiss. 1950;43:705. [PubMed] [Google Scholar]
- 12.Balboni F.A., Lopresti J. Congenital idiopathic dilatation of the pulmonary artery in children. A report of seven cases. Bull St Francis Hosp Sanat. 1961;17:1. [PubMed] [Google Scholar]
- 13.Dreyfus P., Morin B. La dilatation isolee del’artere pulmonaire. Coeur Med Intern. 1963;2:145. [Google Scholar]
- 14.Deb S.J., Zehr K.J., Shields R.C. Idiopathic pulmonary artery aneurysm. Ann Thorac Surg. 2005;80(4):1500–1502. doi: 10.1016/j.athoracsur.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Zhao Y.J., Cheng X.S. An analysis of 21 cases of idiopathic dilatation of the pulmonary artery. Zhonghua Nei Ke Za Zhi. 1992;31(January (1)):24–25. 60. [PubMed] [Google Scholar]
- 16.Mallesh K.N., Srinivas B.C., Manjunath C.N. Idiopathic dilatation of pulmonary artery with effort angina. IOSR J Dent Med Sci. 2013;5(March–April (5)):32–33. [Google Scholar]
- 17.Taussig H.B. 1947. Congenital Malformations of Heart; p. 377. [PubMed] [Google Scholar]
- 18.Choi Y.-J., Kim U., Lee J.S. A case of extrinsic compression of the left main coronary artery secondary to pulmonary artery dilatation. J Korean Med Sci. 2013;28(October (10)):1543–1548. doi: 10.3346/jkms.2013.28.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Andrews R., Colloby P., Hubner P.J. Pulmonary artery dissection in a patient with idiopathic dilatation of the pulmonary artery: a rare cause of sudden cardiac death. Br Heart J. 1993;69(March (3)):268–269. doi: 10.1136/hrt.69.3.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chisholm D.R. Trigonoidation of the semilunar valves and its relationship to certain basal systolic murmurs. Am Heart J. 1937;13:362. [Google Scholar]
- 21.Karnegis J.N., Wang Y. The phonocardiogram in idiopathic dilatation of the pulmonary artery. Am J Cardiol. 1964;14(July):75–78. doi: 10.1016/0002-9149(64)90109-2. [DOI] [PubMed] [Google Scholar]
- 22.Turano L., Gambaccini P. Anatomical and roentgenological aspects of the solitary s.c. idiopathic dilatation of the pulmonary artery (with some remarks regarding its pathogenesis) Sci Med Ital. 1958;6(January–March (3)):435–462. [PubMed] [Google Scholar]
- 23.Deshmukh M., Guvenc S., Bentivoglio L., Goldberg H. Idiopathic dilatation of the pulmonary artery. Circulation. 1960;21:710–716. doi: 10.1161/01.cir.21.5.710. [DOI] [PubMed] [Google Scholar]
- 24.Boutin C., Davignon A., Fournier A., Houyel L., Van Doesburg N. Dilatation idiopathique de l’arterie pulmonaire: aspects echocardiographiques. Arch Mal Coeur Vaiss. 1994;87:663–666. [PubMed] [Google Scholar]
- 25.Van Buchem F.S.P., Nieveen J., Marring W., Van Der Slikke L.B. Idiopathic dilatation of the pulmonary artery. Dis Chest. 1955;28:326. doi: 10.1378/chest.28.3.326. [DOI] [PubMed] [Google Scholar]
- 26.Asayama J., Matsuura T., Endo N. Echocardiographic findings of idiopathic dilatation of the pulmonary artery. Chest. 1977;71(May (5)):671–673. doi: 10.1378/chest.71.5.671. [DOI] [PubMed] [Google Scholar]
- 27.Nguyen E.T., Silva C.I., Seely J.M., Chong S., Lee K.S., Müller N.L. Pulmonary artery aneurysms and pseudoaneurysms in adults: findings at CT and radiography. Am J Roentgenol. 2007;188:W126–W134. doi: 10.2214/AJR.05.1652. [DOI] [PubMed] [Google Scholar]
- 28.Niida T., Kitai T., Isoda K., Adachi T., Ohsuzu F. A case of idiopathic dilatation of the pulmonaryartery with mild subvalvular pulmonary stenosis. J Cardiol Cases. 2011;3:e53–e56. doi: 10.1016/j.jccase.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ugolini P., Mousseaux E., Sadou Y. Idiopathic dilatation of the pulmonary artery: report of four cases. Magn Reson Imaging. 1999;17(July (6)):933–937. doi: 10.1016/s0730-725x(99)00013-2. [DOI] [PubMed] [Google Scholar]
- 30.Futagami Y., Yada T., Konishi T. Idiopathic dilatation of the pulmonary artery: a case report and review of 59 cases in Japan. Mieigaku. 1987;31:425–432. [Google Scholar]
- 31.Fang C.C., Tsai C.C. Idiopathic pulmonary artery aneurysm. J Formos Med Assoc. 1996;95(November (11)):873–876. [PubMed] [Google Scholar]
- 32.Ring N.J., Marshall A.J. Idiopathic dilatation of the pulmonary artery. Br J Radiol. 2002;75(June (894)):532–535. doi: 10.1259/bjr.75.894.750532. [DOI] [PubMed] [Google Scholar]
- 33.Theodoropoulos, P., Ziganshin B.A., Tranquilli M., Elefteriades J.A. Pulmonary artery aneurysms: four case reports and literature review. Int J Angiol. 2013;22(September (3)):143–148. doi: 10.1055/s-0033-1347907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vural A.H., Türk T., Ata Y., Göncü T., Ozyazicioglu A. Idiopathic asymptomatic main pulmonary artery aneurysm: surgery or conservative management? A case report. Heart Surg Forum. 2007;10(4):E273–E275. doi: 10.1532/HSF98.20061199. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.