Abstract
Human papillomavirus (HPV) vaccination is routinely recommended for U.S. adolescents ages 11 to 12 years, yet vaccine coverage remains low. Text message HPV immunization reminders to parents have been effective with increasing uptake, but text messages directly to adolescents in order to increase HPV vaccination uptake are unknown. The purpose of this study was to examine the acceptability of text messages about HPV vaccination and message preferences among adolescents. Middle school students (n = 43) assisted in designing text messages to promote HPV vaccine among their peers. Through seven focus groups and two in-class surveys, we assessed students’ knowledge of HPV vaccine, use of texting, and preferences for text messages and sources. The average age of participants was 13 years, and all were White (17 males, 26 females) in this rural setting. More than 70% used text messaging with a cell phone. The text message with the best composite score (M = 2.33, SD = 0.72) for likeability, trustworthiness, and motivation to seek more information was a gain frame emphasizing reduction in HPV infection if vaccinated against HPV. Text messages with lower scores emphasized threats of disease if not vaccinated. Participants (68%) preferred doctors as their information source. Text messaging to adolescents may be a strategy to improve HPV knowledge and vaccination.
Keywords: text messaging, adolescents, HPV vaccination
INTRODUCTION
Human papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the United States (Centers for Disease Control and Prevention, 2012), yet HPV vaccination coverage is far below the national objective set at 80% by Healthy People 2020 (Centers for Disease Control and Prevention, 2013). HPV causes genital warts and is associated with cervical, vaginal, vulvar, anal, penile, and throat cancers (Centers for Disease Control and Prevention, 2013; Markowitz et al., 2013; National Cancer Institute, 2012). HPV vaccination is routinely recommended for adolescents ages 11 to 12 years in an effort to vaccinate teens prior to their sexual debut (Centers for Disease Control and Prevention, 2011). At the end of 2012, completion of the three-dose HPV vaccine series among females and males ages 13 to 17 in the United States was only 33.4% and 6.8%, respectively (Centers for Disease Control and Prevention, 2013).
Diverse communication strategies to inform parents and adolescents about HPV vaccination are needed in order to motivate them to complete the vaccination series (Centers for Disease Control and Prevention, 2013; Sherris et al., 2006; Task Force on Community Preventive Services, 2011). Reminders by telephone are a well-established best practice to encourage immunization (Jacobsen Vann & Szilagyi, 2005; Szilagyi et al., 2013).Though sparse evidence exists to date, texting is one promising communication innovation to inform and remind audiences because of its potential for broad and individualized reach (Buhi et al., 2012; Glasgow, Vogt, & Boles, 1999; Gurol-Urganci, de Jongh, Vodopivec-Jamsek, Atun, & Car, 2013; Kharbanda et al., 2011; Kharbanda, Stockwell, Fox, & Rickert, 2009; Ralph, Berglas, Schwartz, & Brindis, 2011).
Texting adolescents directly about HPV vaccination is a possible strategy to increase HPV vaccination. The vast majority of American teens (78% of those ages 12–17) have cell phones, and the majority of these teens text every day, more frequently than other forms of daily communication, including phone calls, face-to-face socializing, and social media use (Lenhart, 2012). The acceptability and effectiveness of text messages sent to adolescents have been tested with other health issues, including sexual health and knowledge of STIs (Gold et al., 2011; Perry et al., 2012). Development of vaccination messages with input from middle school adolescents has been demonstrated in one study as promoting flu vaccine (Painter et al., 2010). Adolescents are learning to be their own health care navigators and can be informed partners in the decision to pursue HPV vaccination (McRee, Reiter, Gottlieb, & Brewer, 2011). Parents are usually responsible for consenting to their minor children’s vaccinations, but some states, including North Carolina, also have “minors’ consent laws” allowing children younger than 18 to consent for themselves for certain services such as prevention and treatment of STIs (English et al., 2008; Guttmacher Institute, 2013).
This exploratory study examined young adolescents’ knowledge of HPV infection and vaccination, preferences for text messages, and sources of information about HPV vaccination. The study incorporated an innovative research to practice linkage between (a) communication, medical, and public health researchers; and (b) practitioners in school-based health clinics. Findings will inform similar efforts to communicate with adolescents and their parents about health topics.
METHOD
Participants
Two middle schools in a rural western North Carolina county helped the study team recruit 43 students from four seventh-grade social studies classes to give input on designing text messages in order to raise awareness of HPV vaccination among their age-group. Children at these schools tend to be poorer, more likely to be uninsured, less likely to have access to adolescent health care providers, and more likely to have unemployed parents, compared to the average child in North Carolina (Kids Count Data Center, 2012). The county is predominantly White. Both schools have school-based clinics that students can access during the day and that could be sites for HPV vaccination in a future intervention. Participants whose parents consented to the study represented 63% of the 68 students enrolled in the four classes. We sent consent forms home with the students the day before the focus groups and asked students to sign assent forms at the beginning of the group discussion. Focus group leaders were a White female and Black male, both in their early 30s and part of the ongoing research team.
Procedures
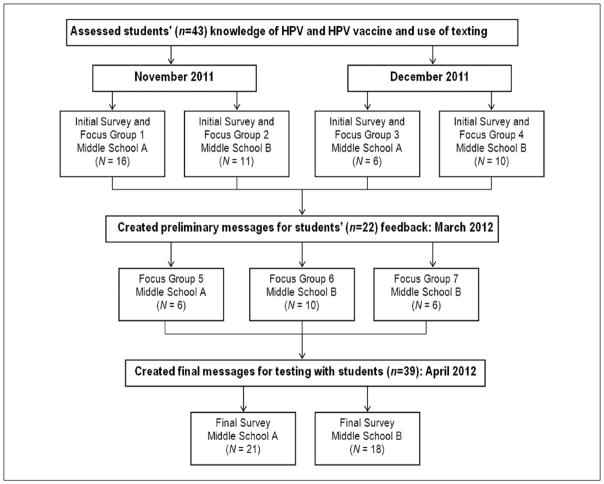
We conducted the research in three phases from November 2011 to April 2012 with the initial 43 students (Figure 1). First, we assessed students’ knowledge of HPV and HPV vaccine and their use of texting through four focus groups and in-class surveys. Second, we created preliminary text messages based on responses from the first round of focus groups and solicited further feedback in a second round of three groups with 22 of the original participants who were able to attend that day. Third, we created final text messages for testing with 39 of the initial 43 students with in-class paper surveys. Additionally, we conducted key informant interviews (not reported here) with three school administrators, a teacher, and four parents to ask about the feasibility of text messaging students about HPV vaccine. The study was approved by the university’s institutional review board.
FIGURE 1. Flowchart of Methods for Soliciting Input on HPV Vaccine Messages From Middle School Students.
NOTE: HPV = human papillomavirus.
Instruments
Theoretical Concepts
We used theoretical concepts from mass communication research (Hornik, 2002; Noar, 2006), the health belief model (Becker, 1974; Janz, Champion, & Strecher, 2002; Rosenstock, Strecher, & Becker, 1988), and message design studies (Dillard & Nabi, 2006; Rothman, Bartels, Wlaschin, & Salovey, 2006). Based on models used in mass communication, we assessed middle school students’ preferences for a cell phone as a channel for a message about HPV vaccination from a trusted source (doctor, school nurse, friend). From the health belief model, we drew questions about the students’ perceptions of their susceptibility to HPV infection and disease; severity of HPV-related disease, benefits from getting the HPV vaccine; possible barriers, such as access; and self-efficacy to talk with others about vaccination. We used message design concepts of gain framing (Rothman et al., 2006; highlighting positive outcomes of behavior compliance) and emotional relevance (Dillard & Nabi, 2006) to increase the possibility that the persuasive messages would encourage HPV vaccination (Noar, 2006).
Surveys
We administered an initial paper survey at the beginning of the first focus group to ascertain students’ demographics, cell phone ownership and text message usage, sexual activity and knowledge, perceptions and experience with HPV and HPV vaccine, and attitude toward getting HPV vaccine at the school-based clinic. Survey questions were based on (a) Guidelines for Adolescent Preventive Services (Elster & Kuznets, 1994) and (b) published surveys on HPV knowledge (Brewer et al., 2011; Hughes et al., 2009). We administered a second paper survey with similar questions at the final session to assess whether students, as a result of focus group discussions, retained knowledge about HPV vaccine and expressed any differences in attitude or behavior since the initial survey and to solicit feedback on final text messages. The surveys were pretested with a convenience sample of 15 seventh-grade students.
For testing with the students, we crafted sample text messages based on students’ focus group responses to draw attention to their susceptibility to HPV and the benefits of HPV vaccine. We divided the sample text messages into three parts: (a) message greeting, (b) body of message, and (c) action statement, and asked students about each part. The greetings varied by tone (friendly, serious, neutral), and the messages varied by both tone (nondirective/soft vs. directive/hard) and frame (loss/ gain/social norm). Students rated each sample message for likeability, trustworthiness, and whether the message made them want more information about HPV and HPV vaccine. They rated message greetings and action statements by best or worst and indicated whether they preferred messages spelled out or in shorthand (i.e., text language, such as LOL, OMG, U).
Focus Groups
The seven focus groups ranged from 6 to 16 participants and ran from 40 to 50 minutes. They were audiotaped and transcribed. Discussion guides for the four groups in Round 1 posed questions about HPV and HPV vaccine knowledge and attitudes and use and perceptions of cell phones and texting. Discussion guides for the three focus groups in Round 2 devoted time for thoughts on potential text messages promoting HPV vaccination to young audiences. One purpose of the study was to deconstruct a text message about HPV vaccination and to design messages that could be tested in parts. We created final test messages from feedback given in both rounds of focus groups.
Data Analyses
Surveys
Quantitative analysis conducted in SPSS 17.0 included examination of descriptive statistics and basic comparisons between initial and final surveys. Stratified analyses (e.g., by gender) were limited by insufficient sample size. We computed composite scores as an average of liking, wanting more information, and trust scores for each message.
Focus Groups
Using a constant comparative method, two authors independently coded categories from the first transcript of each of the two rounds of focus groups. A third coder, who was a graduate student but not an author, paired with one of the authors on subsequent coding. After discussing and coming to consensus, coders reached reliability on 22 variables (based on our theoretical constructs; e.g., preferences for channel and messages, perceived susceptibility to HPV infection) from the first round of focus groups, with agreement at 99% and Cohen’s κ from .79 to 1.0 (average of .94). We followed a similar process for Round 2 of the focus groups and reached reliability on 24 variables with 99.7% agreement and Cohen’s κ from .72 to 1.0 (average of .91).
RESULTS
Student Surveys
Participants
The average age of the 17 boys and 26 girls was 13, and all were White, reflecting the racial composition of the county. More than 70% of the students said they had their own cell phone and used text messaging. Fewer than 5% indicated that they had ever received text messages about health topics before. More than 60% of the students reported that their parents had talked with them about sex. Only one student indicated that he or she had engaged in sexual intercourse. The majority (more than 92%) responded that they were not thinking about having sex anytime soon.
Knowledge About HPV and HPV Vaccine
Following discussions in focus groups, the students’ awareness and knowledge of HPV and HPV vaccine increased from the initial to the final survey (Table 1). On the initial survey, the most common sources for hearing about HPV vaccine were a teacher or other adult at school (48.7%), doctor or nurse (46.2%), an ad by a drug company on the television or radio (38.5%), and friends or other kids at school (30.8%). In the second survey, most students wanted to receive more information about HPV from their doctor (72%) or mother (54%). Other common sources were teacher or other adult at school (46.2%), text message (28.2%), other family members (25.6%), or various Internet sources (25.6%).
TABLE 1.
Descriptive Statistics of Middle School Students Responding to Initial (N = 43) and Final (N = 39) Questionnaires About HPV and HPV Vaccine
| Question | Initial Survey, N (%) | Final Survey, N (%) |
|---|---|---|
| Have you ever heard of HPV before today? | ||
| Yes | 3 (7.0) | 34 (87.2) |
| No | 35 (81.4) | 3 (7.7) |
| Don’t know | 5 (11.6) | 2 (5.1) |
| Do you think people can get HPV from having sex? | ||
| Yes | 7 (16.3) | 34 (87.2) |
| No | 0 (0.0) | 0 (0.0) |
| Don’t know | 36 (83.7) | 5 (12.8) |
| Do you think a person can have HPV and not know he or she has it? | ||
| Yes | 20 (46.5) | 30 (76.9) |
| No | 0 (0.0) | 0 (0.0) |
| Don’t know | 23 (53.5) | 9 (23.1) |
| Do you think a lot of people get HPV? | ||
| Yes | 5 (11.6) | 22 (56.4) |
| No | 1 (2.3) | 1 (2.6) |
| Don’t know | 37 (86.0) | 16 (41.0) |
| Do you think HPV can cause cancer in females? | ||
| Yes | 2 (4.7) | 20 (51.3) |
| No | 0 (0.0) | 1 (2.6) |
| Don’t know | 41 (95.3) | 18 (46.2) |
| Do you think HPV can cause cancer in males? | ||
| Yes | 1 (2.3) | 15 (38.5) |
| No | 1 (2.3) | 5 (12.8) |
| Don’t know | 41 (95.3) | 19 (48.7) |
| Do you think HPV can cause genital warts? | ||
| Yes | 4 (9.3) | 26 (66.7) |
| No | 0 (0.0) | 2 (5.1) |
| Don’t know | 39 (90.7) | 11 (28.2) |
| Do you think a person can avoid getting HPV by using a condom when he or she has sex? | ||
| Yes | 4 (9.3) | 21 (53.8) |
| No | 1 (2.3) | 5 (12.8) |
| Don’t know | 38 (88.4) | 13 (33.3) |
| Have you ever heard of the HPV vaccine before today?a | ||
| Yes | 4 (9.8) | 34 (87.2) |
| No | 29 (70.7) | 1 (2.6) |
| Not sure | 8 (19.5) | 4 (10.3) |
| Before today, did you know that the HPV vaccine can be given to boys?a | ||
| Yes | 2 (4.9) | 28 (73.7) |
| No | 27 (65.9) | 7 (18.4) |
| Not sure | 12 (29.3) | 3 (7.9) |
| Have you had any shots of the HPV vaccine?a | ||
| Yes, one shot | 0 (0.0) | 2 (5.1) |
| Yes, two shots | 1 (2.6) | 0 (0.0) |
| Yes, all three | 0 (0.0) | 2 (5.1) |
| Yes, not sure how many shots | 1 (2.6) | 0 (0.0) |
| No | 21 (55.3) | 26 (66.7) |
| Don’t know | 15 (39.5) | 9 (23.1) |
| Without the shots, what do you think is the chance that you will get HPV someday?a | ||
| No chance | 14 (40.0) | 4 (10.3) |
| Low chance | 14 (40.0) | 20 (51.3) |
| High chance | 7 (20.0) | 15 (38.5) |
| If I got the HPV shots, I would think it was ok to have sex without a condom.a | ||
| Agree | 0 (0.0) | 3 (7.7) |
| Disagree | 34 (100.0) | 36 (92.3) |
| If you decided to get the HPV shots, how comfortable would you be getting the shots at school in your school- based health center?a | ||
| Comfortable | 5 (14.3) | 8 (20.5) |
| Not comfortable | 18 (51.4) | 14 (35.9) |
| Not sure | 12 (34.3) | 17 (43.6) |
NOTE: HPV = human papillomavirus.
3Some respondents in the initial survey did not answer this question.
Most students could not answer any of the knowledge questions correctly in the initial survey, but most correctly answered all but one of the eight knowledge questions in the final survey. The answer where almost half of the students (48.7%) indicated “don’t know” in the final survey was to the following knowledge question: “Do you think HPV can cause cancer in males?”
HPV Vaccine Perceptions and Experience
In both surveys, most of the students indicated they had not received any shots of the HPV vaccine. When asked what they believed was their chance of getting HPV someday if they did not get the vaccine, 20% in the initial survey and 38.5% in the final survey selected “high chance.”
Focus Groups
We identified four main themes through coding and analysis of the focus group transcripts: (a) misconceptions about HPV and HPV vaccine, (b) acceptability in using a cell phone for texting, (c) preferred language in text messages about HPV and HPV vaccine, and (d) preferred sources of text messages about HPV and HPV vaccine (Table 2).
TABLE 2.
Summary of Themes in Focus Groups With Middle School Students (N = 43)
| Themes | Specific Patterns Within Theme | Sample Quotes From Students |
|---|---|---|
| 1. Misconceptions about HPV and HPV vaccine |
|
“I think I’ve heard it before too but I don’t remember where or anything about it.” “I just heard the commercials.” “Is there a guarantee that it will cause cancer if you have the disease?” “Is there a medicine I can take to get it to go away?” “Can it be like passed down from your parents?” “Do you have to get it like every year or no?” “Why do they recommend it for 11- and 12-year-olds?” “I’m scared of needles.” “Well if you get [the vaccine] then it like makes it easier. It like gets rid of that nasty stuff that happens.” “Because what if you do get [the vaccine] and then you get cancer [anyway].” |
| 2. Comfort in using a cell phone for texting |
|
“I’m too lazy to talk to people.” “Well, you can say anything that you feel like, but if, like, you type it out and don’t feel like you want to say that . . . you can just delete it and then you can say something else.” “I would rather sign up for it than I would just get it randomly because then you’d be like, delete.” |
| 3. Preferred language to use (or not use) in text messages about HPV vaccination |
|
“A doctor wouldn’t say ‘LOL.’” “You should probably think about getting this” was a suggested message to use |
| 4. Preferred sources of text messages about HPV vaccination |
|
“Maybe like a specialist, someone that has studied the HPV for a long time and know what it is.” |
NOTE: HPV = human papillomavirus.
Misconceptions About HPV and the HPV Vaccine
Students were generally unaware of their susceptibility to HPV, confused about how the virus was contracted and its severity. One student thought it could be contracted through basic skin-to-skin contact, for example, from wrestling. Students also did not know about the HPV vaccine, although some said it sounded vaguely familiar and thought they may have heard about it from television commercials. They were surprised that the vaccine was available for boys and not just for girls and expressed both positive responses, such as “It’s good for you” and “It will make you live,” and less positive responses, such as concern with side effects and anxiety about needles.
Comfort in Using a Cell Phone for Texting
Students who had a cell phone said they liked having it because they often preferred the privacy of texting to calling. Most students had not used text messaging to receive information about health topics. Some said they would not mind being able to text with their doctor or receive information from him or her by text. They did not want to receive unsolicited text messages and said that if they did not know the number where the message was coming from, they would delete it.
Preferred Language to Use (or not Use) in Text Messages About HPV and HPV Vaccine
Some students said they wanted to see shortened and misspelled words common to text message lingo, such as “U” for “you.” Others preferred words to be spelled out and grammatically correct, as they would expect in a text message about something as “serious” as HPV. “A doctor wouldn’t say ‘LOL’ [laugh out loud],” explained one student. Some preferred “shots” instead of “vaccine” and “disease” instead of “infection” to describe HPV.
Students puzzled over how to explain that the virus is “sexually transmitted” in a text message and laughed when the words “sexual,” “vagina,” and “penis” were spoken. They used terms such as “doing the nasty,” “baby making,” and “doing the dirty” to talk about sexual intercourse. Most students, however, did not recommend using colloquial terms in text messages about HPV because they thought such terms might minimize the seriousness of the issue.
In the second round of focus groups, students responded to sample text messages created from feedback in the previous focus groups. Many participants liked starting the text messages with a warning such as “You need to know this” or “This is important.” Some students disagreed and said warning messages like these may scare them or make them nervous. Others liked a more conversational tone, such as “Hey! What’s up?” or “Hey girl!” However, students said the conversational tone would not work if the text message was coming from an unknown source. They suggested a series of messages. “I would say who I was in the very first text message,” suggested one student. “And then second: ‘You need to know this;’ ‘This is important.’ And then talk about the virus.” In all groups, students preferred that any of the text messages not be directive, and they did not want to be told that they “had to get the shot.” For some, knowing that the vaccine had already been given to many other boys and girls was a motivator to get the vaccine themselves.
Preferred Sources of Text Messages About HPV and HPV Vaccine
Students stressed the importance of receiving messages from credible sources, including doctors and HPV experts.
Final Message Testing
In the final survey, 39 students (26 females, 13 males) supported the idea of receiving text messages about HPV and HPV vaccine and preferred messages that allowed them to make their own decision about whether to get vaccinated (Table 3).
TABLE 3.
Preferences of Individual Portions of Proposed Text Messages About HPV and HPV Vaccine (N = 39)
| Message Greeting | Tone | Best, N (%) | Worst, N (%) | ||
|---|---|---|---|---|---|
| “Hey! What’s up?” | Friendly | 16 (44.4) | 9 (24.3) | ||
| “You need to know this.” | Serious | 16 (44.4) | 13 (35.1) | ||
| “Hi there.” | Neutral | 4 (11.1) | 15 (40.5) | ||
|
| |||||
| Body of Message | Tone/Frame | Likea, M (SD) | Want More Infoa, M (SD) | Trusta,M (SD) | Compositeb, M (SD) |
|
| |||||
| “HPV is a sexually transmitted infection. But there is a vaccine you can get to prevent it!” | Gain frame | 2.31 (0.80) | 2.36 (0.78) | 2.33 (0.77) | 2.33 (0.72) |
| “If you get the HPV vaccine, it will help keep you healthy.” | Gain frame | 2.21 (0.80) | 2.26 (0.72) | 2.10 (0.75) | 2.19 (0.67) |
| “Did you know that HPV vaccine can keep you from getting HPV one day?” | Nondirective/ soft tone | 2.10 (0.60) | 1.97 (0.58) | 2.18 (0.64) | 2.09 (0.47) |
| “Many boys and girls have already gotten the HPV vaccine.” | Social norm frame | 1.92 (0.77) | 2.05 (0.83) | 1.97 (0.74) | 1.98 (0.73) |
| “HPV is a sexually transmitted infection. You need to get the HPV vaccine or you might get it.” | Directive/loss frame | 1.82 (0.76) | 2.03 (0.81) | 2.03 (0.74) | 1.96 (0.68) |
| “If you do not get the HPV vaccine before you are sexually active, it may be too late.” | Loss frame | 1.74 (0.72) | 1.95 (0.72) | 1.97 (0.63) | 1.89 (0.62) |
| “You need to get the HPV vaccine to keep from getting HPV one day.” | Directive/hard tone | 1.74 (0.64) | 1.79 (0.70) | 1.97 (0.58) | 1.84 (0.55) |
|
| |||||
| Action Statement | Best, N (%) | Worst, N (%) | |||
|
| |||||
| “Go to the doctor to get the vaccine.” | 2 (5.4) | 27 (73.0) | |||
| “Talk to your doctor about the vaccine.” | 18 (48.6) | 5 (13.5) | |||
| “Talk to your parents about getting the vaccine.” | 17 (45.9) | 5 (13.5) | |||
|
| |||||
| Text Message Suggestions for Practitioners Based on Participant Preferences | |||||
|
| |||||
| “Hey! HPV is the most common sexually transmitted infection, but there is a vaccine you can get to prevent it! Talk to your doctor about getting the vaccine today.” | |||||
| “You need to know this: If you get the HPV vaccine, it will help keep you healthy. Talk to your parents about getting the vaccine today.” | |||||
| “Hey! Did you know that the HPV vaccine can keep you from getting HPV one day? Talk to your doctors about getting the vaccine today.” | |||||
Liking, wanting more information, and trustworthiness were measured on a 3-point scale, where 1 = not at all, 2 = a little, 3 = a lot.
The composite score is an average of the like, wanting more info, and trust scores for each respective message.
Message Greeting
Students were split on whether they wanted to receive text messages about HPV and HPV vaccine with greetings spelled out (e.g., “you”; 54.3%) or in shorthand (e.g., “U”; 45.7%). They were also split on preference for type of greeting, such that 44.4% chose a friendly “Hey! What’s up?” whereas 44.4% chose a more serious “You need to know this.” A neutral “Hi there” emerged as the least favorite, with 11.1% choosing it.
Body of Message
The text message that received the best composite score (M = 2.33, SD = 0.72) for likeability, trustworthiness, and making the students want more information was “HPV is a sexually transmitted infection. But there is a vaccine you can get to prevent it!” This is a gain frame message stating that the chance of getting HPV infection would be reduced if the student was vaccinated against HPV.
The text message with the second best composite score (M = 2.19, SD = 0.67) for likeability, trustworthiness, and making the students want more information was “If you get the HPV vaccine, it will help keep you healthy.” This is also a gain frame message indicating that vaccination will result in better health. Loss frame messages with threats about not getting vaccinated were scored lower overall. A nondirective message asking a question “Did you know that HPV vaccine can keep you from getting HPV one day?” scored higher (M = 2.09, SD = .47) than a directive message “You need to get the HPV vaccine to keep from getting HPV one day” (M = 1.84, SD = 0.55). The social norm frame, “Many boys and girls have already gotten the HPV vaccine,” ranked in the middle (M = 1.98, SD = 0.73).
Message Closing
For the closing text, students were divided between “Talk to your doctor about the vaccine” and “Talk to your parents about getting the vaccine,” both action steps seen as acceptable in the initial focus groups. The majority of students (73%) disliked the more directive “Go to the doctor to get the vaccine.” For their preferred sources of text messages, the majority (68.4%) indicated their doctor, followed by someone slightly older who knows a lot about HPV (36.8%), and a major health organization (31.6%). They were least interested in hearing from the school nurse (13.2%) and someone their age who knows a lot about HPV (13.2%).
DISCUSSION
This study explored sending text messages about HPV and HPV vaccine directly to young adolescents and was based on theoretical concepts from mass communication, health behavior, and message design. We enlisted middle school students to partner with us to design persuasive messages for their peers to raise awareness about, seek more information about, and ultimately seek HPV vaccination (mass communication). Findings suggest that providing messages through texting on cell phones could be a strategic way to promote HPV vaccine to young adolescents (mass communication), the population for whom the HPV vaccine will be most effective (Markowitz et al., 2013).
The students in our study were mostly sexually naive but curious and took the prospect of risk of STIs and negative consequences seriously (health behavior). Students retained knowledge about HPV and HPV vaccine over the three educational sessions, as indicated by the surveys (health behavior). They said they would respond most to messages from a doctor or other respected health professionals, as opposed to peers (mass communication). They tended to prefer a positive gain frame rather than a threatening loss frame (message design).
The findings complement research on both texting as a channel to promote health messages and gain or loss framing of messages to adolescents (Gold et al., 2011; Hwang, Cho, Sands, & Jeong, 2012; Latimer et al., 2012; Perry et al., 2012). Gain versus loss framing of health messages is the topic of much research, including decisions about HPV vaccination (Nan, 2012a, 2012b). These studies have generally found that loss-framed messages are more effective in promoting vaccination behaviors of adults and that gain-framed messages are effective with people who are more future oriented (Rothman et al., 2006). However, effectiveness of gain or loss framing may be situational and somewhat undetermined (Akl et al., 2011). Even though framing HPV vaccine messages with young adolescents has not been researched previously, framing messages about other health behaviors with adolescents has been studied (e.g., sun safety and smoking), and both gain and loss frames have been effective (Hwang et al., 2012; Latimer et al., 2012).
Limitations
Our study findings are limited in that we explored text messaging with students in the middle schools in one rural county. As our sample of students was from the same geographic area, socioeconomic setting, and racial group, generalization to other schools, age-groups, or racial groups is limited. However, we also believe that this study is an important addition to the literature as much of the research on texting health messages has engaged minority participants in urban areas. Most important, we did not proceed to the next steps of assessing whether text messaging was either acceptable or feasible in the community.
Despite these limitations, this study has important implications. The students’ insights on HPV vaccination and the use of text messaging can be used to enhance communication between parents and children and between health care providers and adolescents. We would suggest that future school-based projects use similar procedures with parental consent and child assent plus voluntary provision of cell phone numbers for adolescents to participate. Communication between parents/students and school personnel about health issues or events could be enhanced with the use of widely available mobile phones.
Future research is needed to develop a protocol for texting about HPV vaccination, and a plan for implementing and evaluating the effect of such communication via a mobile device. Additional research is also needed on testing adolescents’ preferences for gain- or loss-framed messages, sources of those messages, and possible differences by age, gender, or race/ethnicity.
CONCLUSIONS
The disappointing uptake of an important vaccine to reduce transmission of HPV means that it is strategic to explore all possible ways of increasing HPV vaccination. The use of cell phones and text messaging to educate adolescents about and promote HPV vaccination might be one way.
Findings from this study in the context of previous work on vaccination promotion among adults may provide useful strategies to create sound protocols for promotion of HPV vaccine among adolescents. Ongoing research on the use of mobile technology is needed as these devices continue to evolve and shape health communication. We hope our findings will promote more research that values input from adolescents and capitalizes on their comfort with texting as a primary form of communication.
Acknowledgments
This research is supported by Health-e-NC, an initiative of the University Cancer Research Fund at the University of North Carolina at Chapel Hill. The authors thank Travis Battle and Chassidy Hanley for assistance on the project and Jane Brown and Sandra Diehl for article review. Dr. Coyne-Beasley receives research funding from Merck & Co; none of these funds were used in the conduction or completion of the research contained in this article.
References
- Akl EA, Oxman AD, Herrin J, Vist GE, Terrenato I, Sperati F, … Schünemann H. Framing of health information messages. Cochrane Database of Systematic Reviews. 2011;(12) doi: 10.1002/14651858.CD006777.pub2. [DOI] [PubMed] [Google Scholar]
- Becker MH. Health Education Monographs. Vol. 2. San Francisco, CA: Society for Public Health Education; 1974. The health belief model and personal health behavior; pp. 324–508. [Google Scholar]
- Brewer NT, Gottlieb S, Reiter PLR, McRee AL, Liddon N, Markowitz LM, Smith JS. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sexually Transmitted Diseases. 2011;38:197–204. doi: 10.1097/OLQ.0b013e3181f12dbf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhi ER, Trudnak TE, Martinasek MP, Oberne AB, Fuhrmann HJ, McDermott RJ. Mobile phone-based behavioural interventions for health: A systematic review. Health Education Journal. 2012 doi: 10.1177/0017896912452071. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. Recommendations on the use of quadrivalent human papilloma-virus vaccine in males—Advisory Committee on Immunization Practices. Morbidity and Mortality Weekly Report. 2011;60:1705–1708. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HPV infection fact sheet. 2012 Retrieved from http://www.cdc.gov/std/HPV/STDFact-HPV.htm#common.
- Centers for Disease Control and Prevention. National and state vaccination coverage among adolescents aged 13–17 years—United States, 2012. Morbidity and Mortality Weekly Report. 2013;62:685–693. [PMC free article] [PubMed] [Google Scholar]
- Dillard JP, Nabi RL. The persuasive influence of emotion in cancer prevention and detection messages. Journal of Communication. 2006;56(Suppl 1):S123–S139. doi: 10.1111/j.1460-2466.2006.00286.x. [DOI] [Google Scholar]
- Elster AB, Kuznets N, editors. AMA guidelines for Adolescent Preventive Services (GAPS): Recommendations and rationale. Baltimore, MD: Williams & Wilkins; 1994. [Google Scholar]
- English A, Shaw FE, McCauley MM, Fishbein DB for the Working Group on Legislation V & Health A. Legal basis of consent for health care and vaccination for adolescents. Pediatrics. 2008;121(Suppl 1):S85–S87. doi: 10.1542/peds.2007-1115J. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold J, Lim MSC, Hocking JS, Keogh LA, Spelman T, Hellard ME. Determining the impact of text messaging for sexual health promotion to young people. Sexually Transmitted Diseases. 2011;38:247–252. doi: 10.1097/OLQ.Ob013e3I8lf68d7b. [DOI] [PubMed] [Google Scholar]
- Gurol-Urganci I, de Jongh T, Vodopivec-Jamsek V, Atun R, Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database of Systematic Reviews. 2013;(12) doi: 10.1002/14651858.CD007458.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmacher Institute. State policies in brief: An overview of minors’ consent law. 2013 Jun; Retrieved from http://www.guttmacher.org/statecenter/spibs/spib_OMCL.pdf.
- Hornik RC. Exposure: Theory and evidence about all the ways it matters. Social Marketing Quarterly. 2002;8:31–37. [Google Scholar]
- Hughes J, Cates J, Liddon N, Smith J, Gottlieb S, Brewer N. Disparities in how parents are learning about the HPV vaccine. Cancer Epidemiology, Biomarkers & Prevention. 2009;18:363–372. doi: 10.1158/1055-9965.EPI-08-0418. [DOI] [PubMed] [Google Scholar]
- Hwang Y, Cho H, Sands L, Jeong SH. Effects of gain- and loss-framed messages on the sun safety behavior of adolescents: The moderating role of risk perceptions. Journal of Health Psychology. 2012;17:929–940. doi: 10.1177/1359105311428536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen Vann JC, Szilagyi P. Patient reminder and recall systems to improve immunization rates. Cochrane Database of Systematic Reviews. 2005 Jul;(3):CD003941. doi: 10.1002/14651858.CD003941.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janz NL, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research, and practice. 3. San Francisco, CA: Jossey-Bass; 2002. pp. 45–66. [Google Scholar]
- Kharbanda EO, Stockwell MS, Fox HW, Andres R, Lara M, Rickert VI. Text message reminders to promote human papillomavirus vaccination. Vaccine. 2011;29:2537–2541. doi: 10.1016/j.vaccine.2011.01.065. [DOI] [PubMed] [Google Scholar]
- Kharbanda EO, Stockwell MS, Fox HW, Rickert VI. Text4Health: A qualitative evaluation of parental readiness for text message immunization reminders. American Journal of Public Health. 2009;99:2176–2178. doi: 10.2105/AJPH.2009.161364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kids Count Data Center. Statistical profile. 2012 Retrieved from http://datacenter.kidscount.org/data/bystate/Rankings.aspx?state=NC&ind=2271.
- Latimer AE, Krishnan-Sarin S, Cavallo DA, Duhig A, Salovey P, … Malley SA. Targeted smoking cessation messages for adolescents. Journal of Adolescent Health. 2012;50:47–53. doi: 10.1016/j.jadohealth.2011.04.013. [DOI] [PubMed] [Google Scholar]
- Lenhart A. Teens, Smartphones & Texting. 2012 Retrieved from Pew Research Internet Project website: http://pewrsr.ch/1m8gDqR.
- Markowitz LE, Hariri S, Lin C, Dunne EF, Steinau M, McQuillan G, Unger ER. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. Journal of Infectious Diseases. 2013 doi: 10.1093/infdis/jit192. Retrieved from http://www.oxfordjournals.org/our_journals/jid/prpaper.pdf. [DOI] [PubMed]
- McRee AL, Reiter PL, Gottlieb SL, Brewer NT. Mother–Daughter communication about HPV vaccine. Journal of Adolescent Health. 2011;48:314–317. doi: 10.1016/j.jadohealth.2010.07.006. http://dx.doi.org/10.1016/j.jadohealth.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nan X. Communicating to young adults about HPV vaccination: Consideration of message framing, motivation, and gender. Health Communication. 2012a;27(1):10–18. doi: 10.1080/10410236.2011.567447. [DOI] [PubMed] [Google Scholar]
- Nan X. Relative persuasiveness of gain-versus loss-framed human papillomavirus vaccination messages for the present- and future-minded. Human Communication Research. 2012b;38:72–94. doi: 10.1111/j.1468-2958.2011.01419.x. [DOI] [Google Scholar]
- National Cancer Institute. Fact sheet–HPV and cancer. 2012 Retrieved from http://www.cancer.gov/cancertopics/factsheet/Risk/HPV.
- Noar SM. A 10-year retrospective of research in health mass media campaigns: Where do we go from here? Journal of Health Communication. 2006;11(1):21–42. doi: 10.1080/10810730500461059. [DOI] [PubMed] [Google Scholar]
- Painter JE, Sales JM, Pazol K, Grimes T, Wingood GM, DiClemente RJ. Development, theoretical framework, and lessons learned from implementation of a school-based influenza vaccination intervention. Health Promotion Practice. 2010;11(3 Suppl):42S–52S. doi: 10.1177/1524839909360171. [DOI] [PubMed] [Google Scholar]
- Perry RCW, Kayekjian KC, Braun RA, Cantu M, Sheoran B, Chung PJ. Adolescents’ perspectives on the use of a text messaging service for preventive sexual health promotion. Journal of Adolescent Health. 2012;51:220–225. doi: 10.1016/j.jadohealth.2011.11.012. [DOI] [PubMed] [Google Scholar]
- Ralph L, Berglas N, Schwartz S, Brindis C. Finding teens in their space: Using social networking sites to connect youth to sexual health services. Sexuality Research and Social Policy. 2011;8:38–49. doi: 10.1007/s13178-011-0043-4. [DOI] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education Quarterly. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Rothman AJ, Bartels RD, Wlaschin J, Salovey P. The strategic use of gain- and loss-framed messages to promote healthy behavior: How theory can inform practice. Journal of Communication. 2006;56(s1):S202–S220. doi: 10.1111/j.1460-2466.2006.00290.x. [DOI] [Google Scholar]
- Sherris J, Friedman A, Wittet S, Davies P, Steben M, Saraiya M. Chapter 25: Education, training, and communication for HPV vaccines. Vaccine. 2006;24(Suppl 3):S210–S218. doi: 10.1016/j.vaccine.2006.05.124. [DOI] [PubMed] [Google Scholar]
- Szilagyi PG, Albertin C, Humiston SG, Rand CM, Schaffer S, Brill H, … Stokley S. A randomized trial of the effect of centralized reminder/recall on immunizations and preventive care visits for adolescents. Academic Pediatrics. 2013;13:204–213. doi: 10.1016/j.acap.2013.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Task Force on Community Preventive Services. Vaccinations to prevent diseases: Universally recommended vaccinations. 2011 Retrieved from http://www.thecommunityguide.org/vaccines/universally/index.html.