Abstract
Traumatic brain injury (TBI), which is seen more in young adults, affects both patients and their families. The need for palliative care in TBI and the limits of the care requirement are not clear. The aim of this study was to investigate the length of stay in the palliative care center (PCC), Turkey, the status of patients at discharge, and the need for palliative care in patients with TBI. The medical records of 49 patients with TBI receiving palliative care in PCC during 2013–2016 were retrospectively collected, including age and gender of patients, the length of stay in PCC, the cause of TBI, diagnosis, Glasgow Coma Scale score, Glasgow Outcome Scale score, Karnofsky Performance Status score, mobilization status, nutrition route (oral, percutaneous endoscopic gastrostomy), pressure ulcers, and discharge status. These patients were aged 45.4 ± 20.2 years. The median length of stay in the PCC was 34.0 days. These included TBI patients had a Glasgow Coma Scale score ≤ 8, were not mobilized, received tracheostomy and percutaneous endoscopic gastrostomy nutrition, and had pressure ulcers. No difference was found between those who were discharged to their home or other places (rehabilitation centre, intensive care unit and death) in respect of mobilization, percutaneous endoscopic gastrostomy, tracheostomy and pressure ulcers. TBI patients who were followed up in PCC were determined to be relatively young patients (45.4 ± 20.2 years) with mobilization and nutrition problems and pressure ulcer formation. As TBI patients have complex health conditions that require palliative care from the time of admittance to intensive care unit, provision of palliative care services should be integrated with clinical applications.
Keywords: nerve regeneration, trauma, palliative care, brain injury, retrospective study, neural regeneration
Introduction
Traumatic injuries have high morbidity and mortality rates and they can also cause disability (Garcia-Altes et al., 2012). Although traumatic brain injury (TBI) is seen more in young adults in economically developed countries, it may also be a cause of disability or death in children (Hukkelhoven et al., 2003; Jagnoor and Cameron, 2014; Godbolt et al., 2015). TBI is one of the most significant causes of long-term disability throughout the world, primarily in industrialized, developed countries, and it is not only a medical problem but also a public health problem. However, its global incidence remains unknown (Narayan et al., 2002; Corrigan et al., 2010; Humphreys et al., 2013). Surviving TBI patients experience a significant degree of cognitive and physical problems which disturb the establishment of direct communication (Nichol et al., 2011). For those who survive, TBI gives rise to various social and community negative effects (Selassie et al., 2008). The high costs incurred by TBI during the critical period and following acute care can have devastating results for the patient and their family (Hall et al., 2015). Together with the high costs of care, there is also a severe economic burden of TBI due to the loss of productivity (Narayan et al., 2002; Corrigan et al., 2010; Garcia-Altes et al., 2012). For all these reasons, TBI is a significant health and socio-economic problem throughout the world in general.
Patients admitted to the neurological and neurosurgical intensive care unit (ICU) are at a high risk of mortality and because of severe physical and cognitive problems, they are unable to participate in the decision-making of their own treatment (Creutzfeldt et al., 2015). The increasing severity of illness in surviving TBI patients increases the need for institutional care or care in rehabilitation centers (McGarry et al., 2002). TBI does not just affect the individual who has suffered the trauma, but also deeply affects the caregivers and the community as a whole (Nichol et al., 2011). Although patients and their families have a high requirement for palliative care (PC), there is insufficient knowledge on the best means of administering this care, the frequency and manner (Creutzfeldt et al., 2015).
The World Health Organization defines PC as an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual (World Health Organization (WHO), 2015). ICU services administered to TBI patients are oriented towards prolonging life span, whereas PC attempts to improve the quality of life. In this context, even if it seems contrary to the definition of PC, it is thought that PC could be administered to trauma patients (Mosenthal and Murphy, 2003). Despite some significant differences, as the need for PC is the same, the provision of PC has started to be extended from malignant diseases to non-malignant diseases (Chahine et al., 2008). PC, as a human right, must be accessible, fair and inclusive for all (Brennan, 2007). However, the training and experience of trauma surgeons and other specialists are poor in palliative procedures that require skills such as communication and pain and symptom management (Mosenthal and Murphy, 2003). Thus, for patients with severe stroke, PC needs have been identified and addressed (Holloway et al., 2014). In Turkey, as throughout the world, research into PC and TBI patients is limited, and there are extremely few studies regarding neurological and neurosurgical patients and PC (Creutzfeldt et al., 2015).
The evaluation of PC as a human right renders PC both as a privilege and separated from other healthcare services. There is a very limited amount of data, even almost negligible, regarding PC needs in patients with head trauma. Thus, how PC can be integrated into the care process in the treatment of TBI has become a very important topic. The aim of this study was to investigate PC requirement, hospitalization period, and discharge status of TBI patients in the palliative care center (PCC), Turkey. This retrospective study is important as the first study in this field in Turkey.
Subjects and Methods
Ethics statement
The study was approved by Ankara Numune Training and Research Hospital Ethics Committee (approval No. 11.11.2015/E-15-654).
Patients
The hospital records of TBI patients admitted to the PCC of Ankara Ulus State Hospital, Turkey during 2013–2016 were retrospectively collected (Figure 1).
Figure 1.
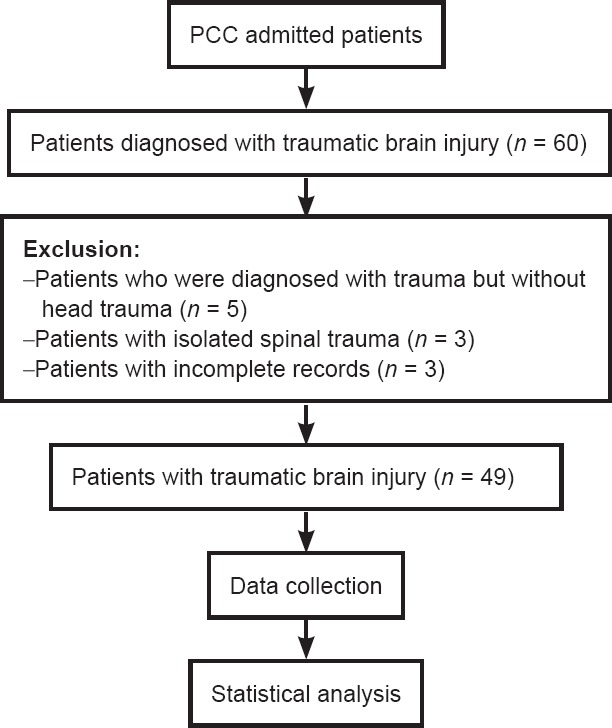
Study flowchart.
PCC: Palliative care center.
Measurements
Medical records comprise the information including the age and gender of patients, the length of stay (LOS) in PCC, the cause of TBI, diagnosis, Glasgow Coma Scale (GCS) score, Glasgow Outcome Scale (GOS) score, Karnofsky Performance Status (KPS) score, mobilization status, nutrition routes (oral, percutaneous endoscopic gastrostomy (PEG)), tracheostomy), pressure ulcers (PU) and discharge status (home, rehabilitation centre, intensive care unit, death).
Following TBI, in addition to the use of scales evaluating disability and functionality, GOS is generally used for evaluation of quality of life (Nichol et al., 2011). The KPS is a scale consisting of 11 grades progressing from 0 to 100 points with increments of 10 points according to the performance status, where 0 points = death and 100 points = normal status with no complications or findings of disease (Buccheri et al., 1996). The KPS measures the health status in three areas of activity, work and ability for self-care and can be used by any healthcare personnel as a rapid assessment of general function and status (Abernethy et al., 2005). In this study, analysis was made by grouping GCS, GOS and KPS. Patients were divided into three groups as severe GCS (GCS score: 3–8), moderate GCS (GCS score: 9–12) and mild GCS (GCS score: 13–15) (Jagnoor and Cameron, 2014); poor GOS (death and vegetative state), moderate GOS (severe disability) and good GOS (moderate disability and full recovery); severe KPS (KPS score: 0–30), moderate KPS (KPS score: 40–60), and mild KPS (KPS score: 70–100).
In addition, the patients were also grouped according to gender, mobilization status, oral nutrition, PEG, tracheostomy, the presence of PU, and discharge status. All the groups formed were compared in respect of age, LOS in PCC, GCS, GOS and KPS scores.
Statistical analysis
The calculations and statistical analyses of the study data were made using Windows-based Microsoft® Office Excel 2003 SP 3 (Excel© 1985–2003 Microsoft Corporation) and IBM SPSS Statistics 23.0 (IBM Corp., Armonk, NY, USA). The conformity to normal distribution of continuous variables (age, LOS in PCC) was examined graphically and with the Shapiro-Wilk test. The variable of age conformed to normal distribution and all the other continuous variables were skewed. In descriptive statistics, age was expressed as the mean ± standard deviation (SD) and all skewed data were expressed as median and interquartile range [IQR]. Categorical data were stated as number (n) and percentage (%). The Kruskal-Wallis test was applied for comparison of continuous variables among groups. Post-hoc pairwise comparisons were made with the Bonferroni corrected Mann-Whitney U test. The chi-square test was used for comparison of differences between categorical variables. To define the risk increase in 2 × 2 tables, odds ratio and 95% confidence interval values were calculated. A value of P < 0.05 was accepted as statistically significant.
Results
Patients and PC requirement
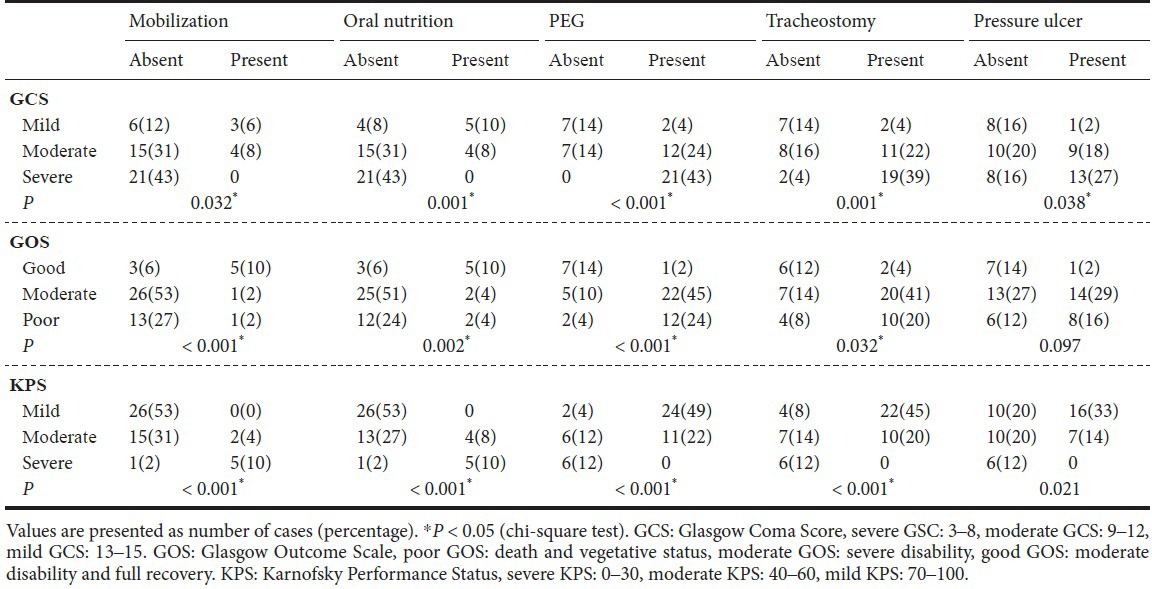
After excluding 11 patients including 3 diagnosed with trauma but no head trauma, 5 with isolated spinal trauma and 3 with incomplete records, 49 patients were included in this study. The clinical characteristics of patients diagnosed with head trauma and subjected to PC from admission to discharge are shown in Table 1. The 49 patients included in this study comprised 35 (71.4%) males and 14 (28.6%) females, with a mean age of 45.4 ± 20.2 years (range, 15–89 years). The median LOS in PCC was 34.0 days (IQR = 91.0), ranging from 3–293 days. The median GCS value was 10.0 (IQR = 4.0), ranging from 4–15. Patients in the severe GCS group were those who had the characteristics of inability to mobilize, nutrition route (oral or PEG), tracheostomy and PU (Table 2). There was significant difference in the median GCS value between groups according to the KPS score (P < 0.001). Patients with severe KPS had a significantly lower median GCS than patients with moderate and mild KPS (P < 0.001) (Table 2).
Table 1.
Clinical characteristics of TBI patients subjected to palliative care
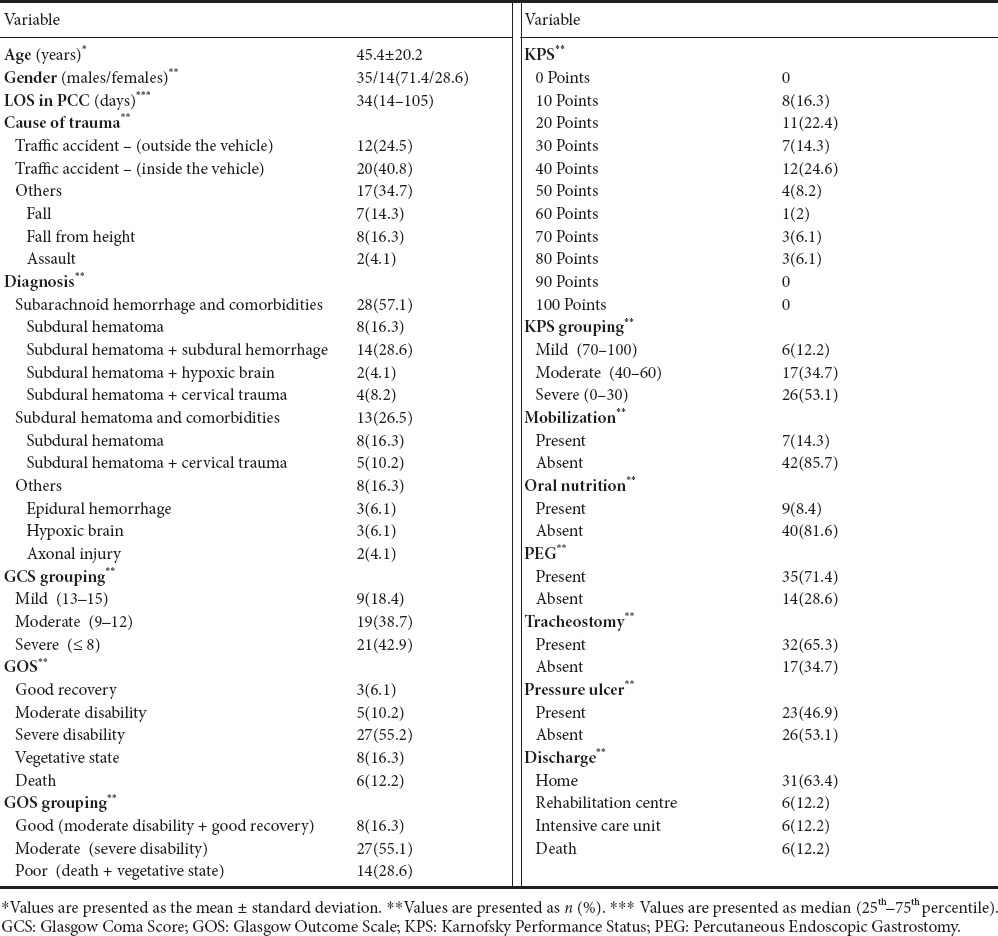
Table 2.
Evaluation of clinical characteristics and concomitant problems according to GCS, GOS and KPS grouping of the patients
LOS
No significant difference was determined in the age, LOS in PCC and median GCS of the patients under different conditions (P > 0.05). There were no significant differences in age (P = 0.423) and LOS in PCC (P = 0.046) between KPS groups (Table 3).
Table 3.
The effects of clinical characteristics and concomitant problems of the patients according to age distribution, LOS in PCC and GCS
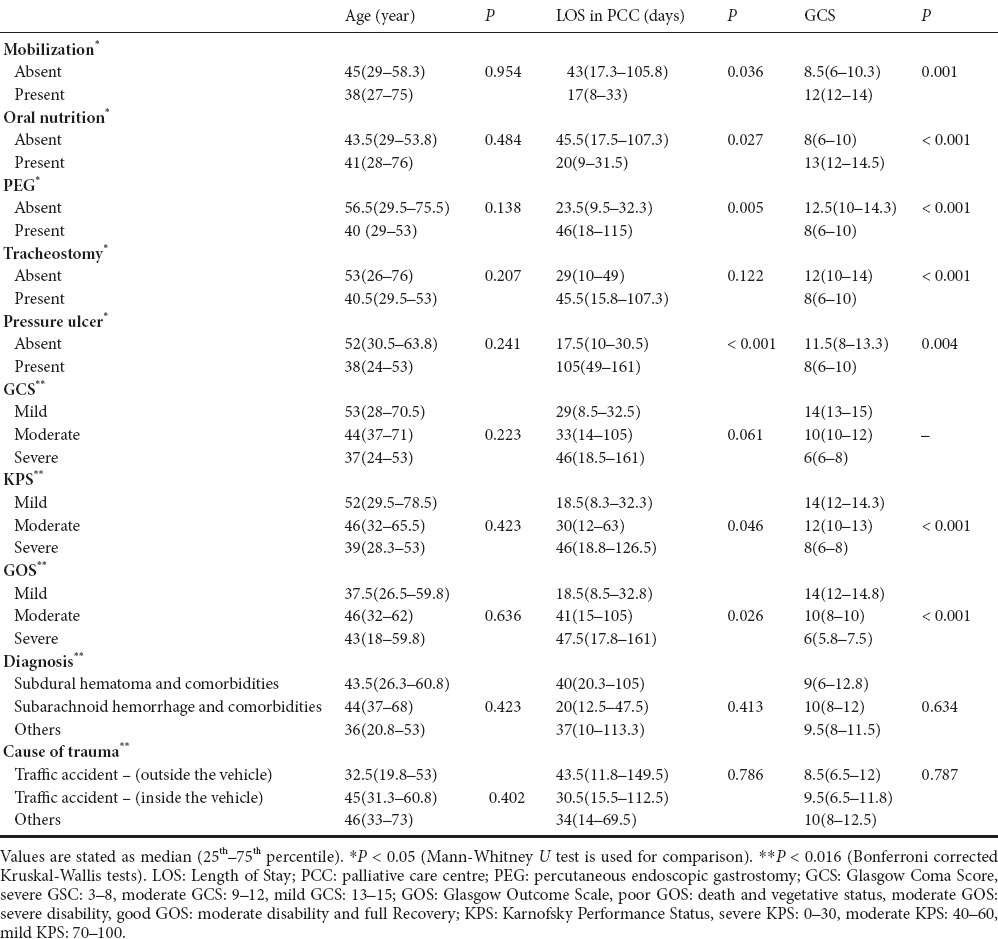
Patients subjected to PEG and patients with PU had a significantly greater median LOS in PCC than those not subjected to PEG and those without PU separately (P < 0.001) (Table 3). There were no significant differences in age and LOS in PCC between poor GOS, moderate GOS and good GOS groups (P > 0.05) (Table 3). Patients with good GOS had a significantly greater median GCS than in patients with moderate and poor GOS, and patients with moderate GOS had a significantly greater GCS than in patients with poor GOS (P ≤ 0.001) (Table 3).
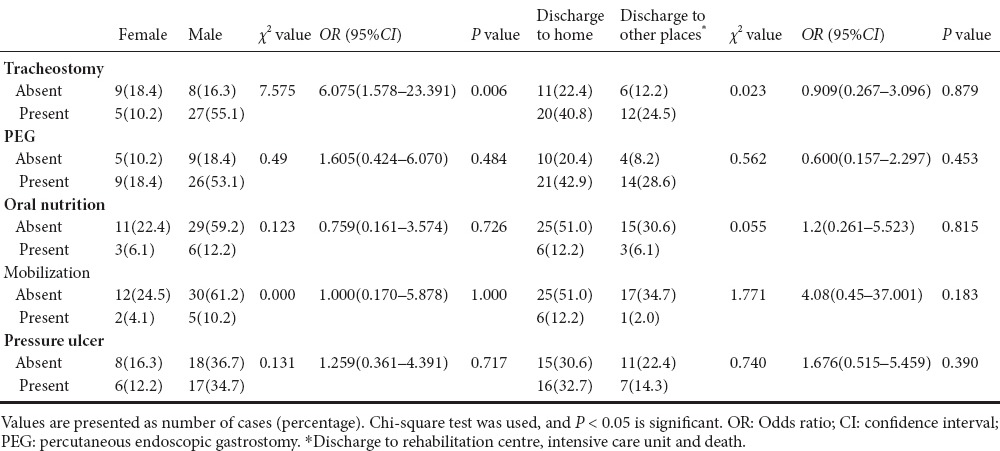
Discharge status
There were no differences in LOS in PCC and median GCS between different discharge statuses (P > 0.05). The mean age was lower in males than in females, and in patients discharged to home than in patients discharged to others (Supplementary Table 1 (838.7KB, tif) ). Tracheostomy was performed at a significantly higher rate in males than in females (χ2 = 7.575; P = 0.006) and male gender had a much greater risk of tracheostomy (OR = 6.08, 95%CI: 1.58–23.39). There were no differences in mobilization, oral nutrition, PEG and PU between males and females (P > 0.05; Table 4). No significant differences in mobilization, oral nutrition, PEG and PU were observed between patients discharged to their home and those discharged to other places (P > 0.05; Table 4). The causes of trauma, diagnosis, GOS grouping were similar between males and females (P > 0.05; Supplementary Table 2 (1.5MB, tif) ). There were no significant differences in cause of head trauma, diagnosis, GOS grouping between severe, moderate and mild KPS groups (Supplementary Table 3 (966.2KB, tif) ).
Table 4.
Comparison of clinical characteristics and concomitant problems according to gender and discharge status
Comparisons of age, LOS in PCC and GCS according to gender and discharge status
Comparison of GOS grouping, diagnosis and causes of trauma according to gender and discharge status
Comparison of clinical characteristics according to KPS grouping
In this study, 49 patients who stayed in PCC were included in this study, and 10 of them died and 4 were transferred to ICU during the 3-year study period, with a mortality rate of 20.4%. Of the surviving 39 patients, 36 (73%) patients (28 with sequelae and 8 in a vegetative state) were dependent on or needed care, and only 3 were discharged with no sequelae. The high rate of 73% of dependent patients in need of care was thought to be due to terminal-stage patients having been transferred from the ICUs of other hospitals for palliative care.
Discussion
TBI is one of the leading causes of morbidity and disability worldwide with a greater economic burden in low and middle income countries, and very little is known about the outcomes after treatment (Hukkelhoven et al., 2003; De Silva et al., 2009; Corrigan et al., 2010). Although the treatment outcome of surviving TBI patients is associated with many factors, the costs of the condition to the individuals and community are involved in the macro-level outcomes reflecting quality of life and a return to independent living (Narayan et al., 2002; Selassie et al., 2008; Nichol et al., 2011; Hall et al., 2015). TBI in some form develops in approximately 2.5 million individuals per year in Europe, 1 million of these are admitted to hospital and of these 75,000 die (Maas et al., 2015). In the USA, it has been reported that 1.1 million individuals per year are treated in emergency departments with a diagnosis of non-fatal TBI, 235,000 are admitted to hospital, approximately 50,000 die and 124,000 (43.1%) are discharged from hospital. Long-term disabilities develop because of TBI and these disabilities form the most significant obstacle to the continuation of life (Corrigan et al., 2010; Jagnoor and Cameron, 2014). Following TBI, there is a need for every kind of care and support which will improve quality of life and the economic situation for those who survive and their families, possibly throughout the life (Nichol et al., 2011; Jagnoor and Cameron, 2014).
Patients in PCC stay in single rooms together with either a family member who undertakes the care or a person providing professional care. An anesthesia and re-animation specialist is responsible for the service provided to patients in PCC 24 hours a day and 7 days a week. Specialists from brain surgery, general surgery, internal cardiology, chest diseases, infectious diseases, plastic and reconstructive surgery, physical therapy and rehabilitation work as consulting doctors. Dieticians and physiotherapists also have a function in PCC. In addition to the medical treatment, psychological support is provided for the patient and their family by psychologists and psychological care specialists.
Continuation of life with severe and moderate sequelae is a difficult situation to be accepted by both the patient and their family. In the early stages after TBI, the patient and their family together require physical, psychosocial, and emotional support. Creutzfeldt et al. (2015) reported that 62% of patients admitted to neuro-ICU were defined as in need of PC by ICU clinicians. In recent years, PC has been accepted as a part of comprehensive care for the increasing number of critical patients, irrespective of diagnosis and prognosis, and has been extremely effective for developing strategies (Aslakson et al., 2014). While KPS is often used as a prognostic tool in PC, GOS and GCS are used as prognostic tools in ICU. In the current study, patients with good GOS were observed to have significantly high median GCS and patients in the severe KPS group had significantly low median GCS. Twenty-one patients were determined with GCS ≤ 8, as the prognosis was expected to be poor in the majority, and the necessity to implement PC from the time of admittance to ICU was shown.
PEG has become a routine procedure for patients with prolonged lack of consciousness after TBI. In this study, only 9 patients could be fed orally and PEG was applied to 35 (71.4%). The ability for oral feeding of patients in PC or nutritional support with PEG, NG or TPN provides significant positive support especially for the patient's family. In 32 patients, early tracheostomy was applied because of a prolonged requirement for mechanical ventilation in ICU, but as mechanical ventilation could not be applied to these patients in PC, oxygen support was provided at intervals from the tracheostomy cannula. The 32 (65.3%) patients subjected to tracheostomy had similar KPS, GOS and GCS values. Cases with tracheostomy performed in the early stage of severe isolated head injury had a decreased LOS in ICU and fewer total days of ventilation (Siddiqui et al., 2015). Impaired nutrition has been reported to affect the formation of PU and has a negative effect on prognosis by increasing mortality (Montalcini et al., 2015). Sufficient albumin has a direct effect on neurological injures and improves vital and functional outcomes together with reduced oxygenation in secondary brain damage (Bernard et al., 2008; Baltazar et al., 2015). A low GCS score was seen in the severe KPS group and in patients with poor GOS who were not mobilized, had a tracheostomy, had PEG applied, were not fed orally, and had PU.
In patients with PEG who were not fed orally and not mobilized, the LOS in PCC was significantly high. Among patients included in this study, 42 (85.7%) patients were bedridden and 23 (46.9%) patients developed PU, indicating that other patients without PU who were not mobilized have the risk of developing PU over time. The patients with a TBI and those who have to live together with the patients were considered in this study. Patient's conditions including tracheostomy, PEG, inability to take oral nutrition, development of PU, and inability to be mobile make lives of the patients and their caregivers extremely difficult. At the same time, their quality of life is directly affected. For example, taking prophylactic precautions to prevent PU formation will make a positive contribution to the quality of life of the patient and their family. It would be possible to educate the patient and their family in preventative measures. PCCs are centers where communication is prioritized and the patient and their family can learn how they can live with the situation they find themselves in (Owens et al., 2005).
Healthcare professionals can facilitate PC services to TBI patients with PC rules and applications (Frontera et al., 2015). Those working in ICU in particular know how communication should be established when sharing information with terminal-stage patients and their family and as a result the communication is more supportive and empathic (Curtis et al., 2001; Simmons et al., 2008). Simmons et al. (2008) applied PC to patients with intracerebral hemorrhage and reported that those administering PC should help the family at the stage of decision-making for surgery to withdraw technological support and other invasive interventions such as artificial feeding which affects the prognosis. If the family members make a decision not to apply treatment or to close down a life support unit, the clinician will work easily (Owens et al., 2005). In Turkey, the non-application of treatment or terminating treatment or ‘do not resuscitate’ – DNR orders, are not legal and are not applied. In brain-dead patients, the decision to close down the life support unit is controversial except for organ transplantation and again is not applied. Therefore, in practice, in communication with the families of TBI patients, the subjects of DNR, terminating or not applying treatment are not discussed and treatment of the patient is continued. Throughout the hospitalization period, support was provided by psychologists and emotional care specialists for the patient and their family to make them to accept the prognosis and the state of dependency.
In conclusion, there is a very limited amount of data, even almost negligible, related to the PC needs of TBI patients. This retrospective study has shown that TBI patients have complex health conditions entailing high treatment costs and they are dependent on family care after discharge. To improve the quality of life of TBI patients, it is important to determine the PC requirements and to integrate PC with other services according to the principles of PC. Criteria must be defined to be able to implement more effective and better quality PC for these patients. There is a need for further studies on this subject.
Footnotes
Declaration of patient consent: The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Conflicts of interest: None declared.
Supplementary information: Supplementary data associated with this article can be found, in the online version, by visiting www.nrronline.org.
Plagiarism check: This paper was screened twice using CrossCheck to verify originality before publication.
Peer review: This paper was double-blinded and stringently reviewed by international expert reviewers.
Copyedited by Li CH, Song LP, Zhao M
References
- Abernethy AP, Shelby-James T, Fazekas BS, Woods D, Currow DC. The Australia-modified Karnofsky Performance Status (AKPS) scale: a revised scale for contemporary palliative care clinical practice (ISRCTN81117481) BMC Palliat Care. 2005;4:7. doi: 10.1186/1472-684X-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aslakson RA, Curtis JR, Nelson JE. The changing role of palliative care in the ICU. Crit Care Med. 2014;42:2418–2428. doi: 10.1097/CCM.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltazar GA, Pate AJ, Panigrahi B, Sharp A, Smith M, Chendrasekhar A. Higher haemoglobin levels and dedicated trauma admission are associated with survival after severe traumatic brain injury. Brain Inj. 2015;29:607–611. doi: 10.3109/02699052.2015.1004558. [DOI] [PubMed] [Google Scholar]
- Bernard F, Al-Tamimi YZ, Chatfield D, Lynch AG, Matta BF, Menon DK. Serum albumin level as a predictor of outcome in traumatic brain injury: potential for treatment. J Trauma. 2008;64:872–875. doi: 10.1097/TA.0b013e31803428cc. [DOI] [PubMed] [Google Scholar]
- Brennan F. Palliative care as an international human right. J Pain Symptom Manage. 2007;33:494–499. doi: 10.1016/j.jpainsymman.2007.02.022. [DOI] [PubMed] [Google Scholar]
- Buccheri G, Ferrigno D, Tamburini M. Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer. 1996;32A:1135–1141. doi: 10.1016/0959-8049(95)00664-8. [DOI] [PubMed] [Google Scholar]
- Chahine LM, Malik B, Davis M. Palliative care needs of patients with neurologic or neurosurgical conditions. Eur J Neurol. 2008;15:1265–1272. doi: 10.1111/j.1468-1331.2008.02319.x. [DOI] [PubMed] [Google Scholar]
- Corrigan JD, Selassie AW, Orman JA. The epidemiology of traumatic brain injury. J Head Trauma Rehabil. 2010;25:72–80. doi: 10.1097/HTR.0b013e3181ccc8b4. [DOI] [PubMed] [Google Scholar]
- Creutzfeldt CJ, Engelberg RA, Healey L, Cheever CS, Becker KJ, Holloway RG, Curtis JR. Palliative Care Needs in the Neuro-ICU. Crit Care Med. 2015;43:1677–1684. doi: 10.1097/CCM.0000000000001018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis JR, Patrick DL, Shannon SE, Treece PD, Engelberg RA, Rubenfeld GD. The family conference as a focus to improve communication about end-of-life care in the intensive care unit: opportunities for improvement. Crit Care Med. 2001;29(2 Suppl):26–33. doi: 10.1097/00003246-200102001-00006. [DOI] [PubMed] [Google Scholar]
- De Silva MJ, Roberts I, Perel P, Edwards P, Kenward MG, Fernandes J, Shakur H, Patel V. CRASH Trial Collaborators. Patient outcome after traumatic brain injury in high-, middle- and low-income countries: analysis of data on 8927 patients in 46 countries. Int J Epidemiol. 2009;38:452–458. doi: 10.1093/ije/dyn189. [DOI] [PubMed] [Google Scholar]
- Frontera JA, Curtis JR, Nelson JE, Campbell M, Gabriel M, Mosenthal AC, Mulkerin C, Puntillo KA, Ray DE, Bassett R, Boss RD, Lustbader DR, Brasel KJ, Weiss SP, Weissman DE. Improving Palliative Care in the ICU Project Advisory Board (2015) Integrating palliative care into the care of neurocritically ill patients: a report from the improving palliative care in the ICU Project Advisory Board and the Center to Advance Palliative Care. Crit Care Med. 43:1964–1977. doi: 10.1097/CCM.0000000000001131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Altes A, Perez K, Novoa A, Suelves JM, Bernabeu M, Vidal J, Arrufat V, Santamariña-Rubio E, Ferrando J, Cogollos M, Cantera CM, Luque JC. Spinal cord injury and traumatic brain injury: a cost-of-illness study. Neuroepidemiology. 2012;39:103–108. doi: 10.1159/000338297. [DOI] [PubMed] [Google Scholar]
- Godbolt AK, Stenberg M, Jakobsson J, Sorjonen K, Krakau K, Stålnacke BM, Nygren DeBoussard C. Subacute complications during recovery from severe traumatic brain injury: frequency and associations with outcome. BMJ Open. 2015;5:e007208. doi: 10.1136/bmjopen-2014-007208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall R, Turgeon AF. Palliative care in the neurologic ICU-are we there yet? Crit Care Med. 2015;43:2033–2034. doi: 10.1097/CCM.0000000000001176. [DOI] [PubMed] [Google Scholar]
- Holloway RG, Arnold RM, Creutzfeldt CJ, Lewis EF, Lutz BJ, McCann RM, Rabinstein AA, Saposnik G, Sheth KN, Zahuranec DB, Zipfel GJ, Zorowitz RD. American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, and Council on Clinical Cardiology: Palliative and end-of-life care in stroke: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:1887–1916. doi: 10.1161/STR.0000000000000015. [DOI] [PubMed] [Google Scholar]
- Hukkelhoven CW, Steyerberg EW, Rampen AJ, Farace E, Habbema JD, Marshall LF, Murray GD, Maas AI. Patient age and outcome following severe traumatic brain injury: an analysis of 5600 patients. J Neurosurg. 2003;99:666–673. doi: 10.3171/jns.2003.99.4.0666. [DOI] [PubMed] [Google Scholar]
- Humphreys I, Wood RL, Phillips CJ, Macey S. The costs of traumatic brain injury: a literature review. Clinicoecon Outcomes Res. 2013;5:281–287. doi: 10.2147/CEOR.S44625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagnoor J, Cameron ID. Traumatic brain injury--support for injured people and their carers. Aust Fam Physician. 2014;43:758–763. [PubMed] [Google Scholar]
- Lynch T, Connor S, Clark D. Mapping levels of palliative care development: a global update. J Pain Symptom Manage. 2013;45:1094–1106. doi: 10.1016/j.jpainsymman.2012.05.011. [DOI] [PubMed] [Google Scholar]
- Maas A, Menon DK, Steyerberg EW, Citerio G, Lecky F, Manley GT, Hill S, Legrand V, Sorgner A. CENTER-TBI Participants and Investigators. Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI): A prospective longitudinal observational study. Neurosurgery. 2015;76:67–80. doi: 10.1227/NEU.0000000000000575. [DOI] [PubMed] [Google Scholar]
- McGarry LJ, Thompson D, Millham FH, Cowell L, Snyder PJ, Lenderking WR, Weinstein MC. Outcomes and costs of acute treatment of traumatic brain injury. J Trauma. 2002;53:1152–1159. doi: 10.1097/00005373-200212000-00020. [DOI] [PubMed] [Google Scholar]
- Montalcini T, Moraca M, Ferro Y, Romeo S, Serra S, Raso MG, Rossi F, Sannita WG, Dolce G, Pujia A. Nutritional parameters predicting pressure ulcers and short-term mortality in patients with minimal conscious state as a result of traumatic and non-traumatic acquired brain injury. J Transl Med. 2015;13:305. doi: 10.1186/s12967-015-0660-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosenthal AC, Murphy PA. Trauma care and palliative care: time to integrate the two. J Am Coll Surg. 2003;197:509–516. doi: 10.1016/S1072-7515(03)00651-3. [DOI] [PubMed] [Google Scholar]
- Narayan RK, Michel ME, Ansell B, Baethmann A, Biegon A, Bracken MB, Bullock MR. Clinical trials in head injury. J Neurotrauma. 2002;19:503–557. doi: 10.1089/089771502753754037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichol AD, Higgins AM, Gabbe BJ, Murray LJ, Cooper DJ, Cameron PA. Measuring functional and quality of life outcomes following major head injury: common scales and checklists. Injury. 2011;42:281–287. doi: 10.1016/j.injury.2010.11.047. [DOI] [PubMed] [Google Scholar]
- Owens D, Flom J. Integrating palliative and neurological critical care. AACN Clin Issues. 2005;6:542–550. doi: 10.1097/00044067-200510000-00010. [DOI] [PubMed] [Google Scholar]
- Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, Steiner C. Incidence of long-term disability following traumatic brain injury hospitalization, United States. J Head Trauma Rehabil. 2008;23:123–131. doi: 10.1097/01.HTR.0000314531.30401.39. [DOI] [PubMed] [Google Scholar]
- Siddiqui UT, Tahir MZ, Shamim MS, Enam SA. Clinical outcome and cost effectiveness of early tracheostomy in isolated severe head injury patients. Surg Neurol Int. 2015;6:65. doi: 10.4103/2152-7806.155757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons BB, Parks SM. Intracerebral hemorrhage for the palliative care provider: what you need to know. J Palliat Med. 2008;11:1336–1339. doi: 10.1089/jpm.2008.0169. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2015) WHO Definition of Palliative Care. [Accessed.22.06.2016]. Available at: http://www.who.int/cancer/palliative/definition/en/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Comparisons of age, LOS in PCC and GCS according to gender and discharge status
Comparison of GOS grouping, diagnosis and causes of trauma according to gender and discharge status
Comparison of clinical characteristics according to KPS grouping


