Abstract
Background
Persons with low health literacy have difficulty dealing with the health care system and understanding health-related information. Studies from multiple countries have shown that low health literacy negatively affects health, health-related and illness-related behavior, and the utilization of health care resources. The data available till now on health literacy in Germany have been sparse. The goal of this study is to acquire representative data on the health literacy of the German population.
Methods
In a cross-sectional study, we collected data from a representative group of 2000 persons over age 15 in Germany by means of computer-assisted personal interviews (CAPI) that were based on the long version of the questionnaire used in the European Health Literacy Survey (HLS-EU-Q47). Sociodemographic data were also collected.
Results
The respondents were a representative sample of the German population. 54.3% of them were found to have limited health literacy. Multiple logistic regression revealed associations of limited health literacy with advanced age (odds ratio [OR] 1.83, 95% confidence interval [CI] [1.36; 2.48]), an immigrant background (OR 1.87 [1.27; 2.75]), low self-assessed social status (OR 5.25 [3.57; 7.72]), and low functional literacy (OR 1.94 [1.49; 2.52]).
Conclusion
The low health literacy of many Germans can impair communication between doctors and patients and exacerbate existing problems in health policy. In the future, greater effort will have to be made to foster health literacy, make health-related information for patients easier to understand, and intensify research in the field of health literacy.
Many people have difficulty identifying the date on an appointment slip or filtering out the parts of a general disease information sheet that are relevant to their individual case. These were among the findings of a study of adults in the USA (1). They also find it hard to understand what physicians say to them and therefore cannot take advantage of their doctor’s verbal communications to help cope with their disease (2). They lack the health literacy to understand, assess, and exploit health-related information.
A low level of health literacy has negative consequences for health and for uptake of health system services. Studies in the USA show that low health literacy goes hand in hand with higher risk of hospitalization, greater likelihood of readmission within 30 days of hospital discharge, and more frequent resource to medical emergency services (3). Poor self-assessed health status and difficulties in communication with physicians are also associated with limited health literacy (4– 6).
The existing evidence on health literacy derives mostly from studies carried out in nations other than Germany: little research has been carried out in this country. Only one federal state of Germany (North Rhine–Westphalia) participated in the European Health Literacy Study (HLS-EU). Although a few research projects were initiated thereafter (7– 10), there has still been no comprehensive and representative survey of the health literacy in the German population. To fill this gap, we designed and executed the German Health Literacy Survey (HLS-GER) as the first study to acquire representative data on the health literacy of the population of Germany together with associated sociodemographic factors.
Methods
Our study adopts the concepts and methods of the HLS-EU and is based on the same definition of health literacy: “Health literacy is linked to literacy and entails people’s knowledge, motivation and competences to access, understand, appraise, and apply health information in order to make judgments and take decisions in everyday life concerning healthcare, disease prevention and health promotion to maintain or improve quality of life during the life course” (11, 12).
Measurement of health literacy
Health literacy was assessed using the German translation of the long version of the HLS-EU questionnaire (HLS-EU-Q47) (12). The 47 items, formulated as direct questions, are aimed at identifying self-assessed difficulty in dealing with selected health-related demands (etable 1). Each question has the same possible answers. For calculation of a health literacy index, numerical values were assigned to the responses:
eTable 1. Percentage responses to the HLS-EU-Q47*1 for the total sample of HLS-GER*2.
|
Very difficult |
Fairly difficult |
Fairly easy |
Very easy |
Don’t know |
||
| Item | How easy/difficult is it to… | % | % | % | % | % |
| 1 | find information about symptoms of illnesses that concern you? | 0.8 | 18.2 | 58.2 | 21.5 | 1.4 |
| 2 | find information on treatments of illnesses that concern you? | 2.1 | 25.0 | 50.6 | 19.3 | 3.0 |
| 3 | find out what to do in case of a medical emergency? | 1.5 | 16.7 | 47.3 | 33.1 | 1.3 |
| 4 | find out where to get professional help when you are ill? | 1.1 | 12.7 | 50.0 | 35.4 | 0.7 |
| 5 | understand what your doctor says to you? | 0.5 | 9.1 | 58.0 | 32.2 | 0.3 |
| 6 | understand the leaflets that come with your medicine? | 6.9 | 30.1 | 40.8 | 21.6 | 0.7 |
| 7 | understand what to do in a medical emergency? | 1.6 | 20.3 | 49.6 | 27.1 | 1.5 |
| 8 | understand your doctor’s or pharmacist’s instruction on how to take a prescribed medicine? | 0.7 | 8.4 | 52.9 | 37.7 | 0.3 |
| 9 | judge how information from your doctor applies to you? | 0.7 | 13.5 | 61.6 | 22.2 | 2.0 |
| 10 | judge the advantages and disadvantages of different treatment options? | 4.0 | 39.4 | 39.4 | 14.7 | 2.5 |
| 11 | judge when you may need to get a second opinion from another doctor? | 5.7 | 35.7 | 41.2 | 15.0 | 2.4 |
| 12 | judge if the information about illness in the media is reliable? | 9.3 | 38.5 | 37.5 | 11.7 | 3.0 |
| 13 | use information the doctor gives you to make decisions about your illness? | 0.7 | 21.6 | 56.9 | 18.6 | 2.2 |
| 14 | follow the instructions on medication? | 0.6 | 8.1 | 50.5 | 40.7 | 0.1 |
| 15 | call an ambulance in an emergency? | 0.4 | 5.0 | 35.1 | 58.8 | 0.7 |
| 16 | follow instructions from your doctor or pharmacist? | 0.3 | 6.7 | 47.9 | 44.7 | 0.4 |
| 17 | find information about how to manage unhealthy behaviour such as smoking, low physical activity and drinking too much? | 1.4 | 14.8 | 53.9 | 25.6 | 4.4 |
| 18 | find information on how to manage mental health problems like stress or depression? | 7.8 | 34.1 | 37.5 | 12.4 | 8.3 |
| 19 | find information about vaccinations and health screenings that you should have? | 1.4 | 16.8 | 54.9 | 24.8 | 2.2 |
| 20 | find information on how to prevent or manage conditions like being overweight, high blood pressure or high cholesterol? | 2.3 | 15.3 | 58.1 | 22.6 | 1.7 |
| 21 | understand health warnings about behaviour such as smoking, low physical activity and drinking too much? | 0.3 | 7.6 | 53.4 | 38.0 | 0.8 |
| 22 | understand why you need vaccinations? | 1.8 | 16.0 | 49.1 | 32.2 | 0.9 |
| 23 | understand why you need health screenings? | 1.2 | 11.7 | 52.9 | 33.6 | 0.7 |
| 24 | judge how reliable health warnings are, such as smoking, low physical activity and drinking too much? | 1.0 | 12.9 | 52.9 | 31.1 | 2.1 |
| 25 | judge when you need to go to a doctor for a check-up? | 1.2 | 13.8 | 50.9 | 33.4 | 0.8 |
| 26 | judge which vaccinations you may need? | 3.3 | 27.6 | 47.4 | 20.4 | 1.2 |
| 27 | judge which health screenings you may have? | 2.0 | 20.9 | 51.1 | 24.8 | 1.3 |
| 28 | judge if the information on health risks in the media is reliable? | 8.2 | 36.1 | 40.2 | 12.7 | 2.7 |
| 29 | decide if you should have a flu vaccination? | 3.5 | 21.1 | 43.9 | 29.9 | 1.6 |
| 30 | decide how you can protect yourself from illness based on advice from family and friends? | 3.0 | 22.9 | 46.0 | 25.8 | 2.3 |
| 31 | decide how you can protect yourself from illness based on information in the media? | 5.1 | 29.5 | 47.6 | 14.8 | 2.9 |
| 32 | find information on healthy activities such as exercise,healthy food and nutrition? | 1.2 | 13.1 | 55.5 | 29.0 | 1.2 |
| 33 | find out about activities that are good for your mental well-being? | 2.7 | 20.8 | 51.4 | 22.4 | 2.7 |
| 34 | find information on how your neighbourhood could be more health-friendly? | 9.0 | 34.1 | 38.9 | 12.9 | 5.1 |
| 35 | find out about political changes that may affect health? | 12.8 | 42.0 | 30.5 | 10.3 | 4.4 |
| 36 | find out about efforts to promote your health at work, at school or in the ‧community? | 8.1 | 30.9 | 40.0 | 13.9 | 7.1 |
| 37 | understand advice on health from family members or friends? | 0.7 | 11.1 | 53.1 | 33.8 | 1.2 |
| 38 | understand information on food packaging? | 11.0 | 33.6 | 38.7 | 15.3 | 1.4 |
| 39 | understand information in the media on how to get healthier? | 4.1 | 23.2 | 54.6 | 15.9 | 2.2 |
| 40 | understand information on how to keep your mind healthy? | 6.4 | 29.9 | 46.3 | 12.8 | 4.5 |
| 41 | judge where your life affects your health and wellbeing? | 5.7 | 24.2 | 47.9 | 19.7 | 2.5 |
| 42 | judge how your housing conditions help you to stay healthy? | 5.4 | 24.4 | 47.8 | 20.1 | 2.3 |
| 43 | judge which everyday behaviour is related to your health? | 1.4 | 13.4 | 57.1 | 27.7 | 0.5 |
| 44 | make decisions to improve your health? | 1.0 | 20.2 | 52.9 | 25.2 | 0.7 |
| 45 | join a sports club or exercise class if you want to? | 4.0 | 13.2 | 36.5 | 44.0 | 2.4 |
| 46 | influence your living conditions that affect your health and wellbeing? | 2.1 | 20.0 | 50.2 | 27.1 | 0.6 |
| 47 | take part in activities that improve health and wellbeing? | 6.7 | 32.7 | 40.7 | 16.1 | 3.8 |
| Average percentages for all 47 questions | 3.5 | 21.2 | 48.1 | 25.2 | 3.5 |
*1 The European Health Literacy Survey Questionnaire
*2 The German Health Literacy Survey; n = 2000
4 = very easy
3 = fairly easy
2 = fairly difficult
1 = very difficult.
The higher the score (range 0–50; eBox), the greater the health literacy.
eBOX. Calculation of the Health Literacy Index.
The underlying conceptual model of health literacy and the item matrix derived from it permit calculation of various subindexes of health literacy. These subindexes represent specific dimensions or summarized dimensions and comprise a combination of many subitems with which the respective dimensions are operationalized. For this analysis we used the comprehensive Health Literacy Index, which contains all 47 items on health literacy and covers all aspects of health literacy. To simplify calculations, comparisons, and the analysis of various analyses, however, the indexes are assigned a common metric (between 0 and 50). The transformation was calculated using the following equation (13):
Index = (X – 1) × 50/3
X = mean, calculated from all (validly answered) items summarized by the index
1 = smallest valid value that an item can have
50 = chosen maximum for the new index metric
3 = range of item values (1– 4)
Reliability was checked using Cronbach’s a-coefficient (0,93). An international team of experts confirmed the validity of the instrument in the European Health Literacy Survey (HLS-EU) by systematic process design of item development and selection (12, 14).
Data acquisition procedure
The Working Group of German Market and Social Research Agencies (Arbeitskreis Deutscher Markt- und Sozialforschungsinstitute e. V.; ADM) represents the interests of the commercial research agencies in Germany. The ADM selection procedure begins with random selection of 258 sampling locations over the whole of Germany. The interviewer follows a predetermined procedure to choose the survey households in a given location. In each of the 3082 chosen households, the target person was determined according to the date of birth code (adjusted gross sample). Each household was contacted up to 4 times for the purpose of an interview. The contact attempts were made on various days of the week, including at least one Saturday, and at different times of day. According to the study protocol of the German Health Literacy Survey (HLS-GER), a total of 507 selected persons were not reached despite multiple attempts. A further 526 persons declined to participate in the survey. The reasons for refusal are not recorded. For another 32 target persons there were other reasons. Finally, 17 interviews were conducted incorrectly. Altogether, there were 1082 systematic drop-outs.
After calculation of the health literacy index, and again in analogy with the HLS-EU, three threshold values were defined, dividing the health literacy score into four levels. The guiding criterion for the threshold values was the risk of a person being confronted with demands they found subjectively challenging (14). Participants with a score below 25 points fell into the category “inadequate”. The second threshold value, set at 33 points, divided the categories “problematic” and “sufficient”. A score of >42 to 50 points showed “excellent” health literacy. For the purpose of further analysis, health literacy was dichotomized (“limited”: inadequate and problematic; “not limited”: sufficient and excellent). “Limited” health literacy was interpreted as the primary measure.
Sociodemographic determinants
Age, education level, health insurance status, social status, immigration background, and functional literacy were selected as sociodemographic determinants for HLS-GER, because international studies have indicated that these characteristics are associated with health literacy (14– 16).
The education level was determined with the aid of the International Standard Classification of Education 1997 (ISCED-97). The interviewer asked about the highest educational qualification acquired and assigned the response to one of the seven ISCED categories. For purposes of analysis these seven categories were organized into three groups with low, intermediate, and high levels of education. The low educational level group comprised ISCED categories 0–2, including, for example, persons who had never attended school, those with no general school qualification, those with no vocational qualification, and those who completed Hauptschule or Realschule (the lower two of the three tiers of secondary school in Germany) without obtaining a vocational qualification or receiving any vocational training. The intermediate educational level group covered ISCED categories 3 and 4 and included, for instance, persons with university entrance qualifications without a vocational qualification or a completed apprenticeship. The high educational level group combined ISCED categories 5 and 6 and included, for example, persons with university education, a higher vocational school qualification, qualification as a master craftsman or technician, or a doctorate (17).
Health insurance was categorized as private or statutory. For assessment of social status, each participant was asked to estimate his or her position in society on a 10-point scale. Responses of 1–4 were classified as low, 5–7 as intermediate, and >7 as high social status.
Participants who were born outside Germany or whose parents were born outside Germany were classified as having an immigration background. Objective functional literacy was assessed using the Newest Vital Sign instrument (NVS) (18), which measures the ability to read and understand the information on an ice-cream container. The test comprises six questions. Scores of 0–3 were defined as limited functional literacy, 4–6 as high functional literacy.
Data acquisition
The investigation was designed as a cross-sectional survey of the German-speaking residential population of Germany over 15 years old living in private households by means of computer-assisted personal interviews (CAPI). The field study took place in July and August 2014.
The participants were recruited with the aid of the selection procedure of the Working Group of German Market and Social Research Agencies (Arbeitskreis Deutscher Markt- und Sozialforschungsinstitute e. V.; ADM) (ebox).
Statistical analyses
The software SPSS 23.0 was used for all analyses. With regard to age, sex, and federal state of residence, the sample differs in part from the general population, as assessed in the 2012 microcensus. The proportion of persons with a low level of education is slightly higher in the HLS-GER sample than in the general population, while the proportions with high educational level and with private health insurance are slightly lower. The HLS-GER data were accordingly weighted for age, sex, and federal state by means of the iterative proportional fitting procedure to achieve comparability with the official statistics, and can thus be regarded as representative. The data reported are percentage rates of individual response items from the HLS-EU-Q47 and prevalences of limited health literacy with 95% confidence intervals (CI) according to age group, sex, social status, functional literacy, health insurance status, educational level, and immigration background. Possible differences between groups were verified using chi-square tests. Furthermore, odds ratios (OR) and the corresponding CI and p-values are given, as calculated by means of multiple logistic regression. The dichotomized health literacy level served as dependent variable. The independent variables were the sociodemographic determinants listed above. The logistic regression included all relevant variables, controlling for possible differences in the other model variables.
Results
Health literacy of the German population
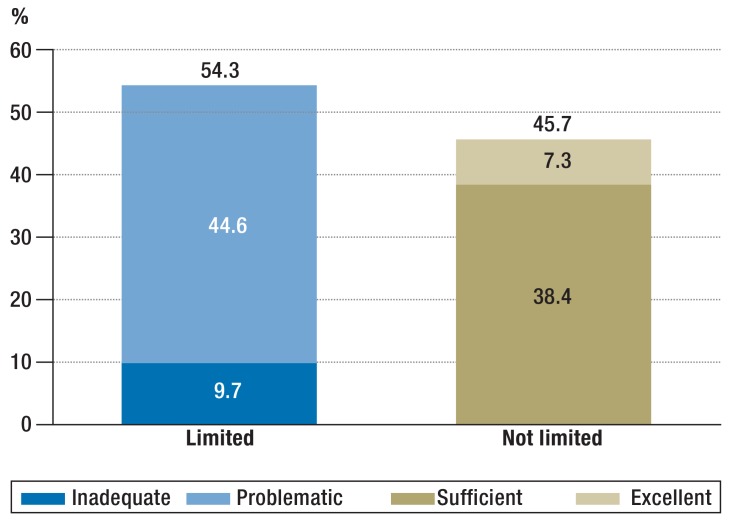
This survey of 2000 persons representative for the population of Germany found that 7.3% (response rate 65%; Table 1) had excellent health literacy and 38.4% showed sufficient health literacy. The remaining 54.3% of the interviewees had limited health literacy, including 9.7% whose health literacy was inadequate. This last group had considerable difficulty in accessing, understanding, appraising, and applying health-related information and believe the demands placed on them by the health system are too complex (figure 1).
Table 1. Characteristics of the German Health Literacy Survey sample*1.
| Variable |
Unweighted sample (%) |
Case number (n) |
Weighted sample (%)*2 |
Case number (n)*2 |
| Sex | ||||
| Male | 46.9 | 938 | 48.9 | 977 |
| Female | 53.1 | 1062 | 51.1 | 1022 |
| Age (years) | ||||
| 15–29 | 16.6 | 332 | 19.7 | 394 |
| 30–45 | 25.2 | 504 | 24.9 | 499 |
| 46–64 | 35.4 | 707 | 31.6 | 631 |
| 65 and over | 22.9 | 457 | 23.8 | 476 |
| Education level | ||||
| Low | 33.6 | 672 | 33.6 | 669 |
| Intermediate | 48.7 | 973 | 48.9 | 972 |
| High | 17.3 | 347 | 17.5 | 349 |
| No data | 0.4 | 8 | – | – |
| Health insurance | ||||
| Statutory | 93.2 | 1853 | 93.1 | 1851 |
| Private | 6.8 | 136 | 6.9 | 137 |
| No data | 0.5 | 11 | – | – |
| Migration background | ||||
| No | 92.4 | 1844 | 92.1 | 1836 |
| Yes | 7.6 | 151 | 7.9 | 158 |
| No data | 0.3 | 5 | – | – |
| Functional literacy skills | ||||
| Low | 19.9 | 398 | 19.6 | 392 |
| Adequate | 80.1 | 1602 | 80.4 | 1608 |
| Social status | ||||
| Low | 14.6 | 285 | 12.9 | 252 |
| Intermediate | 68.4 | 1334 | 68.6 | 1337 |
| High | 17.0 | 332 | 18.5 | 360 |
| No data | 2.5 | 49 | – | – |
| Health literacy | ||||
| Inadequate | 10.5 | 210 | 9.7 | 188 |
| Problematic | 43.2 | 863 | 44.6 | 869 |
| Sufficient | 36.6 | 731 | 38.4 | 747 |
| Excellent | 7.3 | 146 | 7.3 | 142 |
| No data | 2.5 | 50 | – | – |
n = 2000
*1 HLS-GER
*2 Data weighted according to age, sex, and federal state in the 2012 microcensus, not including participants with missing data
Figure 1.
Health literacy levels in %
Examination of individual items shows variation in the stated difficulty of the demands in the different areas covered. Particular problems were reported with tasks that require advanced cognitive skills, such as evaluation of health-related information. Thus, 41.4% of those interviewed found it somewhat difficult or very difficult to judge when a second opinion has to be obtained from a physician. For 43.4% it was somewhat or very difficult to judge the advantages and disadvantages of various treatment options (items 10 and 11 in eTable 1).
Sociodemographic factors and health literacy
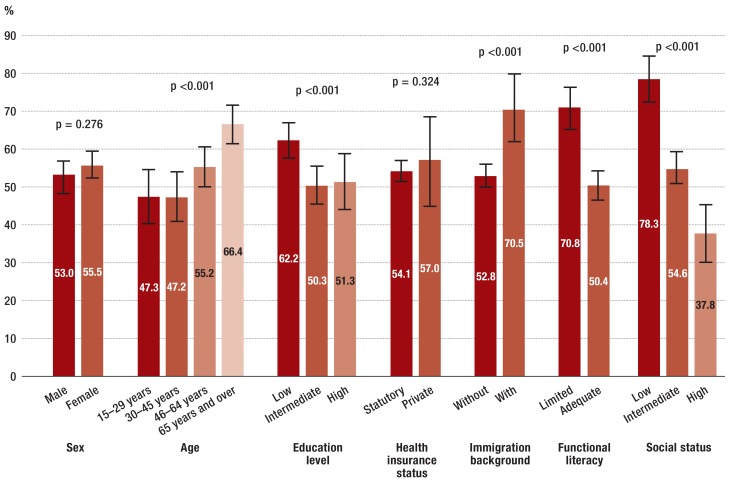
In the sample as a whole, the sociodemographic factors age, education level, immigration background, social status, and functional literacy skills were associated with health literacy (Figure 2, eTable 2, eTable 3).
Figure 2.
Prevalence of limited health literacy
The bars show 95% confidence intervals; p-values from chi-square tests
eTable 2. Health literacy scores in the total sample and in the various subgroups.
| n | Mean |
Standard deviation |
Minimum | Maximum | |
| Sex | |||||
| Male | 949 | 32.89 | 6.18 | 1.06 | 50.00 |
| Female | 997 | 32.67 | 6.18 | 12.06 | 49.65 |
| Age (years) | |||||
| 15–29 | 376 | 33.77 | 6.25 | 12.06 | 49.65 |
| 30–45 | 490 | 33.99 | 5.95 | 14.18 | 50.00 |
| 46–64 | 619 | 32.75 | 6.07 | 12.06 | 49.29 |
| 65 and over | 462 | 30.75 | 6.02 | 1.06 | 48.89 |
| Education level | |||||
| Low | 648 | 31.29 | 6.68 | 1.06 | 49.65 |
| Intermediate | 950 | 33.62 | 5.66 | 12.06 | 48.58 |
| High | 339 | 33.32 | 6.04 | 15.96 | 50.00 |
| Health insurance status | |||||
| Statutory | 1810 | 32.79 | 6.18 | 1.06 | 50.00 |
| Private | 127 | 32.62 | 6.02 | 14.81 | 48.58 |
| Immigration background | |||||
| No | 1788 | 32.97 | 6.06 | 12.06 | 50.00 |
| Yes | 154 | 30.76 | 7.18 | 1.06 | 47.87 |
| Functional literacy skills | |||||
| Low | 371 | 30.25 | 6.22 | 1.06 | 49.65 |
| Adequate | 1575 | 33.38 | 6.02 | 12.06 | 50.00 |
| Social status | |||||
| Low | 247 | 29.48 | 5.58 | 12.06 | 46.81 |
| Intermediate | 1303 | 32.74 | 6.00 | 12.06 | 49.65 |
| High | 357 | 35.07 | 5.61 | 19.50 | 48.89 |
| Total | 1946 | 32.79 | 6.18 | 1.06 | 50.00 |
eTable 3. Proportions of persons with limited health literacy in the various subgroups.
| n | Proportion (%) | 95% CI | p-value* | |
| Sex | ||||
| Male | 503 | 53.0 | [48.6; 57.4] | 0.276 |
| Female | 553 | 55.5 | [51.4; 59.6] | |
| Age (years) | ||||
| 15–29 | 178 | 47.3 | [40.0; 54.6] | <0.001 |
| 30–45 | 231 | 47.2 | [40.8; 53.6] | |
| 46–64 | 341 | 55.2 | [49.9; 60.5] | |
| 65 and over | 307 | 66.4 | [61.1; 71.7] | |
| Education level | ||||
| Low | 403 | 62.2 | [57.5; 66.9] | <0.001 |
| Intermediate | 477 | 50.3 | [45.8; 54.8] | |
| High | 174 | 51.3 | [43.9; 58.7] | |
| Health insurance status | ||||
| Statutory | 979 | 54.1 | [51.0; 57.2] | 0.324 |
| Private | 72 | 57.0 | [45.6; 68.4] | |
| Immigration background | ||||
| No | 944 | 52.8 | [49.6; 56.0] | <0.001 |
| Yes | 109 | 70.5 | [61.9; 79.1] | |
| Functional literacy skills | ||||
| Low | 263 | 70.8 | [65.3; 76.3] | <0.001 |
| Adequate | 793 | 50.4 | [46.9; 53.9] | |
| Social status | ||||
| Low | 193 | 78.3 | [72.5; 84.1] | <0.001 |
| Intermediate | 711 | 54.6 | [50.9; 58.3] | |
| High | 135 | 37.8 | [29.6; 46.0] | |
* p-values from chi-square tests
95% CI, 95% confidence interval
The link between health literacy and social status, functional literacy, immigration background, and age persisted after adjusting for other variables (table 2). Persons aged 65 years or more had a 1.83 times higher rate of limited health literacy than younger participants (95% CI [1.36; 2.48]). Furthermore, participants with low functional literacy skills were almost twice as likely to have limited health literacy as those with adequate functional literacy skills, independent of their formal educational level and all other variables in the model (OR 1.94 [1.49; 2.52]). In those with an immigration background, the rate of limited health literacy was 1.87-fold, regardless of their functional literacy skills in German [1.27; 2.75]. The prevalence of limited health literacy was particularly high in interviewees with low self-assessed social status (OR 5.25 [3.57; 7.72]) (table 2).
Table 2. Limited health literacy in various subgroups*1.
| OR*2 | 95% CI | p-value | |
| Sex | |||
| Male | 0.95 | [0.78; 1.15] | 0.575 |
| Female | Ref. | ||
| Age (years) | |||
| 15–29 | Ref. | ||
| 30–45 | 1.07 | [0.80; 1.43] | 0.651 |
| 46–64 | 1.31 | [0.99; 1.74] | 0.056 |
| 65 and over | 1.83 | [1.36; 2.48] | <0.001 |
| Education level | |||
| Low | 1.32 | [0.99; 1.77] | 0.059 |
| Intermediate | 0.92 | [0.71; 1.21] | 0.557 |
| High | Ref. | ||
| Immigration background | |||
| No | Ref. | ||
| Yes | 1.87 | [1.27; 2.75] | 0.002 |
| Health insurance status | |||
| Statutory | 0.73 | [0.49; 1.09] | 0.122 |
| Private | Ref. | ||
| Functional literacy skills | |||
| Low | 1.94 | [1.49; 2.52] | <0.001 |
| Adequate | Ref. | ||
| Social status | |||
| Low | 5.25 | [3.57; 7.72] | <0.001 |
| Intermediate | 1.89 | [1.47; 2.43] | <0.001 |
| High | Ref. | ||
Bold type shows significant differences
n = 1898; CI, confidence interval; OR, odds ratio; Ref., reference value
*1 Results of multiple logistic regression
*2 OR adjusted for all other variables in model; OR >1 indicates increased ?chance of l imited health literacy
Discussion
This representative population study provides a well-substantiated data set that for the first time permits conclusions regarding the health literacy of the German population and the associated sociodemographic factors. Over half of the population encounters difficulties in dealing with health-related information and possesses limited health literacy. The prevalence of limited health literacy is higher than expected and exceeds the prevalence in some other European countries. In the Netherlands, only around a third of the population has less than sufficient health literacy. In Ireland too, the rate of limited health literacy is lower than in Germany (40% versus 54.3%). The findings tend to confirm the results of previous surveys in Germany, although the latter used the short version of the survey instrument, HLS-EU-Q16 (7, 8) (table 3) and data were acquired using standardized questionnaires filled out by the participants themselves or by means of telephone interviews. In our survey we used CAPI to ensure we reached participants with low functional literacy skills. The differences can partly be explained by the fact that HLS-EU included only European Union (EU) citizens (14), while HLS-GER also included other nationalities.
Table 3. Health literacy in the populations of various countries: selected studies.
| Year | Country | Study | Study population | Prevalence of limited health literacy |
| 1993 | USA | National Adult Literacy Survey (NALS) (19) |
ca. 13 600 participants, age ≥ 16 years |
|
| 2003 | USA | National Adult Assessment of Adult Literacy (NAAL) (1) |
ca. 19.000 participants, age ≥ 16 years |
|
| 2011 | Bulgaria, Germany (NRW), Greece, Ireland, Netherlands, Austria, Poland, Spain |
European Health Literacy Survey (HLS-EU) (14) |
ca. 1000 participants per country, age ≥ 15 years; overall ca. 8000 participants |
|
| 2012 | Austria | Austrian Adolescent Health Literacy Study in framework of HBSC Study (12) |
571 adolescents resident in Austria, age 15 years |
|
| 2013 | Germany | German Health Update (GEDA), RKI (8) |
4952 participants, age ≥ 18 years; representative for the residential population in private households |
|
| 2013 | Germany | Survey of insurees by Scientific Institute of AOK (WIdO) (7) |
2010 participants from the population of persons with statutory health insurance, age ≥ 18 years |
|
| 2015 | Switzerland | Survey of Health Literacy 2015 (20) |
1105 participants, age ≥ 15 years |
|
AOK, Allgemeine Ortskrankenkasse (a large German statutory health insurance provider); HBSC, Health Behaviour in School-aged Children;
NRW, North Rhine–Westphalia; RKI, Robert Koch Institute
Stratification by sociodemographic characteristics shows that advanced age (OR 1.83), immigration background (OR 1.87), low social status (OR 5.25), and low functional literacy (OR 1.94) are associated with limited health literacy. This association was also demonstrated in other European studies, though sometimes with varying magnitude (8, 21, 22).
Particularly noteworthy is the association between advanced age and limited health literacy, because the proportion of the population made up by the elderly will continue to increase (23). Elderly people already constitute the majority of patients in many areas of medical care and are more often confronted with health impairments and chronic disease than other segments of the population (24). Therefore, they are highly dependent on health literacy. However, the complexity and frequency of health-related demands, coupled with the lack of transparency of the health service system, often present them with particularly severe challenges in this regard. At the same time, a cohort effect could be present, so further studies—above all, longitudinal investigations—of health literacy in the elderly are necessary. The same is true for the chronically ill and for intensive users of the healthcare system—they too must be more closely examined in future studies.
The findings also demonstrate that functional literacy is indispensable for successful handling of health-related information; these skills are associated with health literacy in the multiple logistic model. Although the prevalence of limited health literacy is greater in persons with a low educational level than in those with a high educational level, the formal educational status has no effect after adjustment for functional literacy. Our results are therefore in accordance with studies in other countries (15, 16). For routine daily practice, this means that physicians must interact more intensively with patients who have lower levels of education and literacy. In particular, they must adapt their verbal and written communications to meet the needs of this segment of their clientele.
Persons with an immigration background often have low health literacy. Language barriers are not the only reason: differences remain after adjustment for functional literacy skills in German. The possible reasons include differences between Germany and the country of origin in healthcare delivery or in the cultural concept of health and illness (25). Culture-sensitive behavior, information, and communication play an important part in physicians’ interactions with this group of patients.
Social status is of high importance. The close association between health literacy and social status may well be explained by the fact that both concepts were assessed subjectively. An important part is played by self-efficacy. It can be assumed that interviewees with high self-efficacy also have better health literacy. The role of self-efficacy should be examined more closely in future studies on health literacy.
Methodological strengths and limitations
Our data on health literacy are derived from the interviewees’ own assessment of their difficulties in handling health-related information. This has the advantage that abilities can be depicted comprehensively. In contrast with objective instruments for measuring competence and skills, a broad spectrum of health literacy components are described. The questions were posed projectively, so the participants could also estimate the problems they would have with demands that had not yet been placed on them. However, this may lead to the difficulty of some tasks being rated differently by different groups of people, based on personal experience. For this reason, we included an objective test of health-related functional literacy skills. It should be noted that educational level was defined by means of the ISCED classification of highest qualification achieved. Young interviewees may not have completed their education, resulting in assignment to a lower educational level. As further limitations, the health literacy level may be influenced by the quality of health-related information, and the fact that the survey was cross-sectional means that no causal conclusions can be drawn.
Because Germany has no publicly available register of all private households, the sample was drawn from ADM data. The multistage ADM procedure produced a representative sample.
Conclusions
A large part of the population of Germany has problems dealing with health-related information. Systematic promotion of health literacy is therefore an important task. The bundle of measures that need to be introduced ranges from ways of talking to patients, e.g, the teach-back method, through provision of readily comprehensible information specifically designed for various target groups, more intensive use of images and text in information materials, and well-prepared information on the internet to easily understandable product information sheets, food packaging, and forms.
Existing initiatives for improvement of health-related information, e.g., guidelines on evidence-based health-related information, also need to take more account of the findings from studies on health literacy.
At the same time, more importance has to be attached to promotion of health literacy by physicians on a day-to-day basis. Verbal and written communication with patients needs to be improved. As a precondition, the communicative and educative competence of health professionals has to be reinforced. The health service system must be made more informative and easier to understand. German research into health literacy is still in its infancy and must be intensified.
Individual measures will not be enough. We believe that Germany has to follow the example set by other countries and introduce a national action plan.
Key Messages.
Research on health literacy in Germany is in its infancy. Studies have been initiated, but no representative information on health literacy in the German population is yet available. The German Health Literacy Survey (HLS-EU) is the first to provide such data.
The results show that 54.3% of a random sample of the German population have limited health literacy, i.e., experience difficulties in dealing with health-related information and finding their way around the health service system.
Social status, functional literacy, immigration background, and age are associated with health literacy.
Priority must be given to development of a national action plan to improve health literacy in the German population, assure quality, and increase the intelligibility of health-related information.
Acknowledgments
Acknowledgments
Jürgen Pelikan, Florian Röthlin, and Kristin Ganahl of the Ludwig Boltzmann Institute for Health Promotion Research (LBIHPR), Vienna provided assistance in data analysis.
Funding
The HLS-GER study is supported by the German Federal Ministry of Justice and Consumer Protection (BMJV).
Translated from the original German by David Roseveare
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: results from the 2003 national assessment of adult literacy National Center for Education Statistics 2006. nces.ed.gov/pubs2006/2006483.pdf (last accessed on 21 September 2016) [Google Scholar]
- 2.Nielsen-Bohlman L, Kindig DA, Panzer AM, editors. National Academies Press. Washington: 2004. Health literacy: a prescription to end confusion. [PubMed] [Google Scholar]
- 3.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 4.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 5.DeWalt DA, Berkman ND, Sheridan S, Lohr K, Pignone M. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morrow D, Clark D, Tu W, et al. Correlates of health literacy in patients with chronic heart failure. Gerontologist. 2014-2006;46:669–676. doi: 10.1093/geront/46.5.669. [DOI] [PubMed] [Google Scholar]
- 7.Zok K. Unterschiede bei der Gesundheitskompetenz: Ergebnisse einer bundesweiten Repräsentativ-Umfrage unter gesetzlich Versicherten WIdO monitor. www.wido.de/fileadmin/wido/downloads/pdf_wido_monitor/wido_mon_ ausg_2_ 2014_0714.pdf (last accessed on 21 September 2016) [Google Scholar]
- 8.Jordan S, Hoebel J. [Health literacy of adults in Germany: Findings from the German Health Update (GEDA) study] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2015;58:942–950. doi: 10.1007/s00103-015-2200-z. [DOI] [PubMed] [Google Scholar]
- 9.Quenzel G, Schaeffer D, Messer M, Vogt D. [Health literacy among less well-educated young people: influencing factors and consequences] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2015;58:951–957. doi: 10.1007/s00103-015-2201-y. [DOI] [PubMed] [Google Scholar]
- 10.Zamora P, Pinheiro P, Okan O, et al. „Health Literacy“ im Kindes- und Jugendalter Struktur und Gegenstand eines neuen interdisziplinären Forschungsverbunds (HLCA-Forschungsverbund) Prävention und Gesundheitsförderung. 2015;10:167–172. [Google Scholar]
- 11.Sorensen K, van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12 doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Röthlin F, Pelikan J, Ganahl K. Die Gesundheitskompetenz von 15-jährigen Jugendlichen in Österreich: Abschlussbericht der österreichischen Gesundheitskompetenz Jugendstudie im Auftrag des Hauptverbands der österreichischen Sozialversicherungsträger (HVSV) Ludwig Boltzmann Gesellschaf. lbihpr.lbg.ac.at.w8.netz-werk.com/sites/files/lbihpr/attachments/ hljugend_bericht.pdf (last accessed on 21 September 2016) [Google Scholar]
- 13.Sorensen K, van den Broucke S, Pelikan JM, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q) BMC Public Health. 2013;13 doi: 10.1186/1471-2458-13-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.HLS-EU Consortium. Comparative report of health literacy in eight EU member states: the European Health Literacy Survey HLS-EU Second revised and extended version, lbihpr.lbg.ac.at.w8.netz-werk.com/sites/files/lbihpr/attachments/ neu_rev_hls-eu_report_2015_05_13_lit.pdf (last accessed on 21 September 2016) [Google Scholar]
- 15.Protheroe J, Whittle R, Bartlam B, Estacio EV, Clark L, Kurth J. Health literacy, associated lifestyle and demographic factors in adult population of an English city: a cross-sectional survey. Health Expect. 2016 doi: 10.1111/hex.12440. DOI: 10.1111/hex.12440 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith SG, Curtis LM, O’Conor R, Federman AD, Wolf MS. ABCs or 123s? The independent contributions of literacy and numeracy skills on health task performance among older adults. Patient Educ Couns. 2015;98:991–997. doi: 10.1016/j.pec.2015.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schneider SL, Kogan I, editors. The international standard classification of education 1997: challenges in the application to national data and the implementation in cross-national surveys. Mannheim: MZES 2008. www.mzes.uni-mannheim.de/publications/misc/isced_97/schn08b_the_international_standard_classification_of_educa.pdf (last accessed on 21 September 2016) [Google Scholar]
- 18.Weiss BD, Mays MZ, Merriam Castro K, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirsch IS, Jungeblut A, Jenkins L, Kolstad A. U.S. Department of Education. Washington: 2002. Adult literacy in America A first look at the findings of the national adult literacy survey. [Google Scholar]
- 20.Bieri U, Kocher J, Gauch C, et al. Bundesamt für Gesundheit, Abteilung Gesundheitsstrategien. Bern: 2016. Bevölkerungsbefragung „Erhebung Gesundheitskompetenz 2015“ Schlussbericht. Studie im Auftrag des Bundesamts für Gesundheit BAG, Abteilung Gesundheitsstrategien. [Google Scholar]
- 21.Sørensen K, Pelikan JM, Röthlin F, et al. Health literacy in Europe: comparative results of the European Health Literacy Survey (HLS-EU) Eur J Public Health. 2015;6:1053–1058. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van der Heide I, Rademakers J, Schipper M, Droomers M, Sorensen K, Uiters E. Health literacy of Dutch adults: a cross sectional survey. BMC Public Health. 2013;13 doi: 10.1186/1471-2458-13-179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Statistisches Bundesamt. Bevölkerung Deutschlands bis 2060. 12. koordinierte Bevölkerungsvorausberechnung. Begleitheft zur Pressekonferenz am 18. November 2009. www.destatis.de/DE/Publikationen/Thematisch/Bevoelkerung/Vorausberechnung Bevoelkerung/BevoelkerungDeutschland2060Presse5124204099004. pdf%3F__blob%3DpublicationFile (last accessed on 21 September 2016) 2012 [Google Scholar]
- 24.Robert Koch-Institut. edoc.rki.de/documents/rki_fv/remDCCtjOJxI/PDF/21TgKGZEOWNCY.pdf (last accessed on 21 September 2016) Berlin: Daten und Fakten: Ergebnisse der Studie „Gesundheit in Deutschland aktuell 2010“: Beiträge zur Gesundheitsberichterstattung des Bundes. Robert Koch-Institut. [Google Scholar]
- 25.Spallek J, Razum O. Erklärungsmodelle für die gesundheitliche Situation von Migrantinnen und Migranten Health Inequalities. Determinanten und Mechanismen gesundheitlicher Ungleichheit. In: Bauer U, Bittlingmayer U, Richter M, editors. VS Verlag für Sozialwissenschaften. 1. Wiesbaden: 2008. pp. 271–290. [Google Scholar]