Abstract
Objective
The prevalence of symptomatic knee osteoarthritis (OA) has been increasing over the past several decades in the United States concurrent with an aging population and the growing obesity epidemic. We quantify the impact of these factors on the number of persons with symptomatic knee OA in the first decades of 21st century.
Methods
We calculated prevalence of clinically diagnosed symptomatic knee OA from the National Health Interview Survey 2007–08 and derived the proportion with advanced disease (Kellgren-Lawrence grades 3–4) using the Osteoarthritis Policy Model, a validated simulation model of knee OA. Incorporating contemporary obesity rates and population estimates, we calculated the number of persons living with symptomatic knee OA.
Results
We estimate that about fourteen million persons had symptomatic knee OA, with advanced OA comprising over half of those cases. This includes over three million African American, Hispanic, and other racial/ethnic minorities. Adults under 45 years of age represented nearly two million cases of symptomatic knee OA and individuals between 45 and 65 years of age six million more.
Conclusion
Over half of all persons with symptomatic knee OA are younger than 65 years of age. As many of these younger persons will live for three decades or more, there is substantially more time for greater disability to occur and policymakers should anticipate healthcare utilization for knee OA to increase further in upcoming decades. These data emphasize the need for the deployment of innovative prevention and treatment strategies for knee OA, especially among younger persons.
INTRODUCTION
The knees are among the joints most commonly affected by osteoarthritis (OA), and persons with knee OA commonly experience pain, aching, stiffness, and associated functional loss. Risk factors for the developing knee OA are multifactorial and include genetics, female sex, obesity, and knee injury.1 Given that current conservative treatment options have limited long-term efficacy, knee OA presents challenges to treatment.2,3 People with advanced knee OA are thus at risk for undergoing total knee replacement (TKR), which, while effective, is an expensive procedure.4,5
There is sparse literature on the number of persons with symptomatic knee OA in the US.6 The National Arthritis Data Workgroup and the Global Burden of Disease Study both relied extensively on data from the Framingham Osteoarthritis Study (1983–85).7,8 The Framingham Osteoarthritis Study, like the most recent iteration of the National Health and Nutrition Examination Survey (NHANES) that evaluated radiographic knee OA, restricted radiographic imaging to persons above 60 years of age.9,10 While OA was historically considered a condition of older persons, today it is commonly recognized to affect younger adults as well,11 and the fastest growth in TKR rates has been among persons younger than 60 years.12 Additionally, since the 1980s the prevalence of some major modifiable risk factors for knee OA development (obesity, knee injury) have increased substantially.13-17 Knowing the number of persons with symptomatic knee OA and the demographics of those at risk for TKR will allow for better planning and optimization of healthcare delivery.
Our objective was to provide a contemporary estimate of the number of persons with symptomatic, clinically diagnosed knee OA in the United States in the first decades of the 21st century using population-based data. We evaluated the combined effect of increasing prevalence of knee OA by age with the current population distributions, and used mathematical modeling techniques to determine the number of individuals who have advanced knee OA.
METHODS
Analytic Overview
We used data from the National Health Interview Survey (NHIS) 2007–08, a cross-sectional household survey conducted by the Centers for Disease Control and Prevention that is representative of the US civilian non-institutionalized population, to calculate the proportion of adults with symptomatic knee OA, which was defined as having recent knee symptoms as well as a previous diagnosis of arthritis (and no other rheumatologic condition) by a health professional. Using the Osteoarthritis Policy (OAPol) Model and published data on the progression of knee OA, we then estimated the proportion of individuals with advanced symptomatic disease in strata defined by combinations of age, sex, race/ethnicity, and obesity.
To calculate the number of individuals in the US with symptomatic knee OA or advanced symptomatic knee OA, we multiplied the prevalence proportions by population estimates from the US Census Bureau. We assumed that variance in racial/ethnic symptomatic knee OA prevalence was primarily due to differences in obesity rates. The data on obesity were derived from the National Health and Nutrition Examination Survey (NHANES). Our calculations used two reference points: 2007–08 (to match the years used from NHIS) and 2011–12 (most recent available).
Prevalence of Symptomatic Knee Osteoarthritis
We used the results from a previously reported method for determining the prevalence of symptomatic knee OA.18 We first identified all persons at least 25 years of age in the 2007–08 waves of NHIS19 who reported having felt “any symptoms of pain, aching, or stiffness in or around” either knee joint within the previous month and who also reported having been previously told by a health professional that they had “some form of arthritis, rheumatoid arthritis, gout, lupus or fibromyalgia.” Those who reported having been diagnosed with RA, gout, lupus, or fibromyalgia were excluded from potentially having symptomatic knee OA, which may lead to our results being more conservative. We used the years 2007 and 2008 as they were the only two recent sequential years in which NHIS interviewees were also asked with which of those five conditions they had been diagnosed.
We then conducted a logistic regression analysis, controlling for covariates age, age2, age3, age4 (to account for potential non-linear associations of age; age cut in 10-year intervals beginning at age 25 and ending at 75+), and sex-stratified BMI (with BMI dichotomized at 30), to derive OA prevalences in strata defined by sex, BMI and age, as well as associated 95% confidence intervals (CI). We multiplied our derived stratified prevalences by positive predictive values of self-diagnosis of knee OA, as self-reported data often overstates the prevalence of diagnosed rheumatologic conditions.20,21 These positive predictive values were derived from studies that have examined the relationship among community diagnosis of knee OA and either the American College of Rheumatology classification criteria for knee OA or radiographic imaging among persons with regular knee pain; they ranged from 66% for younger adults to 81% for older adults.18
Prevalence of Advanced Symptomatic Knee Osteoarthritis
We derived the distribution of disease severity in each cohort using the OAPol Model, a validated, state transition, Monte Carlo computer simulation model that can be used to simulate the natural history of a cohort of individuals with user-defined characteristics that include age, sex, race/ethnicity, BMI, and knee OA severity (on the Kellgren-Lawrence [KL] grading scale). Details of the model structure and key data elements are published elsewhere.18,22 Simulated individuals in the cohort undergo annual transitions in their health states, whereupon they might develop knee OA, progress in knee OA severity, gain or lose weight, develop comorbidities, or die, all with varying probabilities depending on their demographic and clinical characteristics.
Progression in KL grade was based on published, calibrated rates specific to a simulated individual's sex, current KL grade, and obesity status.22,23 We determined the distribution of KL grade within each age-sex-obesity bracket, and persons progressing to either KL 3 or KL 4 were classified as having advanced symptomatic knee OA (‘advanced’ is defined only by level of structural damage, not pain or functional limitation). Incidence rates, progression rates, and prevalence are presented in Table 1.
Table 1.
Radiographic development, progression, and calculated prevalence estimates of symptomatic knee OA
| Obesity | Sex | Age | Annual Incidence | Annual Progression | Prevalence Estimate (95% CI) | |||
|---|---|---|---|---|---|---|---|---|
| KL 2 | KL 2 to KL 3 | KL 3 to KL 4 | KL 2 | KL 3 | KL 4 | |||
| Non-Obese | Female | 25-34 | 0.1% | 4% | 2% | 1% (1%–1%) | 0% (0%–0%) | 0% (0%–0%) |
| 35-44 | 0.2% | 2% (1%–2%) | 1% (0%–1%) | 0% (0%–0%) | ||||
| 45-54 | 0.3% | 3% (3%–3%) | 1% (1%–1%) | 0% (0%–0%) | ||||
| 55-64 | 0.5% | 5% (4%–5%) | 2% (2%–3%) | 1% (0%–1%) | ||||
| 65-74 | 0.3% | 6% (6%–7%) | 4% (4%–4%) | 1% (1%–1%) | ||||
| 75+ | 0.2% | 6% (5%–6%) | 6% (5%–7%) | 2% (2%–3%) | ||||
| Male | 25-34 | 0.1% | 6% | 1% | 1% (0%–1%) | 0% (0%–0%) | 0% (0%–0%) | |
| 35-44 | 0.1% | 1% (1%–1%) | 1% (1%–1%) | 0% (0%–0%) | ||||
| 45-54 | 0.2% | 2% (2%–2%) | 1% (1%–1%) | 0% (0%–0%) | ||||
| 55-64 | 0.4% | 4% (3%–4%) | 3% (2%–3%) | 0% (0%–0%) | ||||
| 65-74 | 0.2% | 4% (4%–5%) | 4% (4%–5%) | 1% (1%–1%) | ||||
| 75+ | 0.2% | 4% (4%–4%) | 6% (6%–7%) | 2% (2%–2%) | ||||
| Obese | Female | 25-34 | 0.4% | 9% | 4% | 2% (1%–2%) | 0% (0%–0%) | 0% (0%–0%) |
| 35-44 | 0.4% | 3% (3%–4%) | 2% (2%–2%) | 1% (0%–1%) | ||||
| 45-54 | 0.6% | 5% (4%–5%) | 4% (4%–5%) | 2% (2%–2%) | ||||
| 55-64 | 1.2% | 7% (7%–8%) | 7% (6%–8%) | 4% (4%–4%) | ||||
| 65-74 | 0.6% | 7% (6%–8%) | 10% (9%–11%) | 8% (7%–9%) | ||||
| 75+ | 0.5% | 5% (4%–6%) | 11% (10%–12%) | 14% (12%–16%) | ||||
| Male | 25-34 | 0.3% | 12% | 3% | 1% (1%–1%) | 0% (0%–0%) | 0% (0%–0%) | |
| 35-44 | 0.3% | 2% (2%–2%) | 2% (2%–2%) | 0% (0%–0%) | ||||
| 45-54 | 0.5% | 3% (2%–3%) | 4% (3%–4%) | 1% (1%–1%) | ||||
| 55-64 | 0.8% | 4% (4%–5%) | 6% (6%–7%) | 2% (2%–3%) | ||||
| 65-74 | 0.5% | 4% (4%–4%) | 9% (8%–10%) | 5% (4%–5%) | ||||
| 75+ | 0.4% | 3% (3%–3%) | 11% (10%–12%) | 8% (7%–9%) | ||||
Number with Symptomatic and Advanced Symptomatic Knee Osteoarthritis
To quantify how many people in the US are living with symptomatic and advanced symptomatic knee OA, we first obtained intercensal population projections from the US Census Bureau,24 stratified by age, sex, and race/ethnicity, and estimated the proportion of individuals in each stratum who were obese using NHANES.25 We used BMI from NHANES rather than NHIS because weight and height are measured by trained staff members in NHANES and self-reported in NHIS. We assumed that any differences in prevalence by race/ethnicity could be attributed solely to differences in age-sex stratified obesity rates for each racial/ethnic group (Hispanic, non-Hispanic black, non-Hispanic white, and non-Hispanic other race). By matching these stratified obesity data with their respective population size projections, we were able to estimate the number of persons in each age-sex-obesity category among the US adult population ≥25 years of age. We then multiplied these population values with the prevalences of symptomatic and advanced symptomatic knee OA to obtain the number of persons with symptomatic and advanced symptomatic knee OA, and also calculated associated 95% CIs using the lower and upper bounds of the 95% CI for the prevalence values.
Reference Time Points
We conducted our analysis using two reference time points. The first was 2007–08, reflecting the years for which the data from NHIS for the present analysis were available. To match these years, we therefore used the 2007–08 wave of NHANES and the average of population estimates from July 1, 2007 and July 1, 2008. The second time point incorporated the most recently available population-based obesity data as of the date of analysis, from NHANES 2011–12, along with the corresponding population estimates (the average of July 1, 2011 and July 1, 2012). In the later years, we assumed that the prevalence of knee OA within each age-sex-obesity stratum was the same as it had been in 2007–08.
The 2007–08 wave of NHANES grouped all persons who were not white, black or Hispanic into an “other” racial/ethnic group. We similarly combined non-Hispanic American Indians and Alaskan Natives and non-Hispanic Asian Americans and Pacific Islanders from other data sources into one race/ethnicity category (“non-Hispanic other race”) to allow comparison across multiple years.
Software
The OAPol Model is implemented in C# 2.0 (Microsoft, Redmond, WA). Statistical analyses were conducted in SAS 9.2 (SAS Institute, Cary, NC).
RESULTS
Overall Number and Trends over Time
We estimated that in the United States in 2007–08, 13.7 million (13.7M, 6.9% of the total US population at least 25 years of age [199M]; 95% CI 12.4M–15.3M) have symptomatic knee OA, with 7.7M (3.9%; 95% CI 7.0M–8.6M) having advanced (KL 3-4) symptomatic knee OA. In 2011–12, we estimated that the number with symptomatic knee OA increased to 15.1M (7.3% of 208M; 95% CI 13.6M–16.8M) and the number with advanced symptomatic knee OA to 8.6M (4.2%; 95% CI 7.8M–9.6M) (Table 2).
Table 2.
Number of individuals (in thousands) with symptomatic and advanced symptomatic knee OA in the US
| Age | Race / Ethnicity | Sex | 2007–08 | 2011–12 | ||||
|---|---|---|---|---|---|---|---|---|
| Population | Symptomatic Knee OA | Advanced Symptomatic Knee OA | Population | Symptomatic Knee OA | Advanced Symptomatic Knee OA | |||
|
25-44
|
Hispanic | Female | 7,190 | 140 (2%) | 40 (1%) | 7,790 | 190 (2%) | 60 (1%) |
|
45-64
|
3,930 | 300 (8%) | 140 (4%) | 4,750 | 490 (10%) | 260 (5%) | ||
| 65+ | 1,440 | 210 (15%) | 130 (9%) | 1,760 | 330 (19%) | 220 (13%) | ||
|
25-44
|
Male | 7,810 | 110 (1%) | 30 (0%) | 8,450 | 150 (2%) | 60 (1%) | |
|
45-64
|
3,790 | 230 (6%) | 120 (3%) | 4,650 | 300 (6%) | 160 (4%) | ||
| 65+ | 1,060 | 120 (11%) | 80 (7%) | 1,310 | 180 (14%) | 130 (10%) | ||
|
25-44
|
Non-Hispanic Black | Female | 5,620 | 150 (3%) | 50 (1%) | 5,690 | 170 (3%) | 60 (1%) |
|
45-64
|
4,730 | 480 (10%) | 250 (5%) | 5,240 | 560 (11%) | 300 (6%) | ||
| 65+ | 1,980 | 380 (19%) | 260 (13%) | 2,210 | 440 (20%) | 300 (14%) | ||
|
25-44
|
Male | 5,030 | 90 (2%) | 40 (1%) | 5,160 | 90 (2%) | 40 (1%) | |
|
45-64
|
4,060 | 270 (7%) | 150 (4%) | 4,520 | 310 (7%) | 170 (4%) | ||
| 65+ | 1,270 | 180 (14%) | 130 (10%) | 1,450 | 190 (13%) | 140 (9%) | ||
|
25-44
|
Non-Hispanic Other Race | Female | 3,040 | 70 (2%) | 20 (1%) | 3,320 | 60 (2%) | 20 (1%) |
|
45-64
|
2,200 | 220 (10%) | 110 (5%) | 2,550 | 190 (7%) | 80 (3%) | ||
| 65+ | 850 | 150 (18%) | 100 (12%) | 1,060 | 170 (16%) | 110 (10%) | ||
|
25-44
|
Male | 2,770 | 50 (2%) | 20 (1%) | 3,000 | 50 (2%) | 20 (1%) | |
|
45-64
|
1,900 | 130 (7%) | 70 (4%) | 2,200 | 130 (6%) | 60 (3%) | ||
| 65+ | 650 | 80 (13%) | 60 (9%) | 820 | 100 (13%) | 70 (8%) | ||
|
25-44
|
Non-Hispanic White | Female | 25,310 | 610 (2%) | 200 (1%) | 24,590 | 550 (2%) | 170 (1%) |
|
45-64
|
29,080 | 2,580 (9%) | 1,260 (4%) | 29,970 | 2,720 (9%) | 1,330 (4%) | ||
| 65+ | 17,770 | 3,020 (17%) | 1,950 (11%) | 18,930 | 3,380 (18%) | 2,220 (12%) | ||
|
25-44
|
Male | 25,520 | 450 (2%) | 170 (1%) | 24,940 | 420 (2%) | 160 (1%) | |
|
45-64
|
28,260 | 1,880 (7%) | 1,030 (4%) | 29,110 | 2,050 (7%) | 1,150 (4%) | ||
| 65+ | 13,450 | 1,840 (14%) | 1,300 (10%) | 14,890 | 1,960 (13%) | 1,360 (9%) | ||
| Total | 198,600 | 13,750 (6.9%) | 7,720 (3.9%) | 207,710 | 15,170 (7.3%) | 8,650 (4.2%) | ||
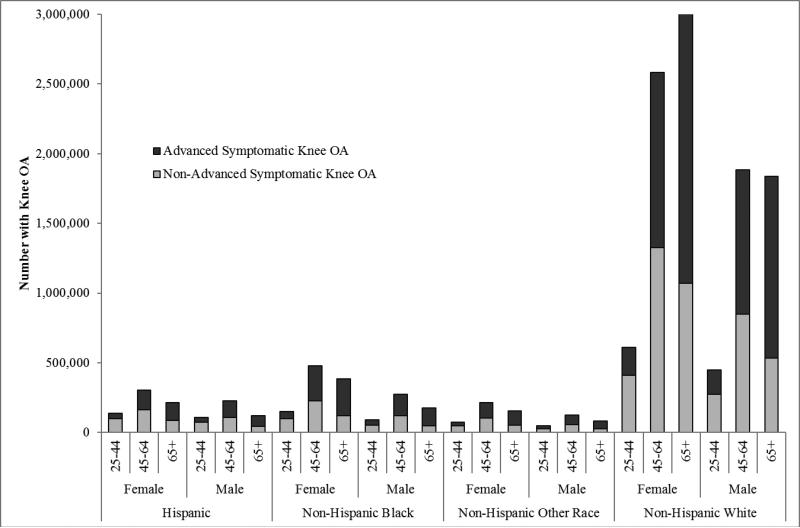
Race/Ethnicity
Partly due to the risk of competing mortality,22 racial/ethnic minorities were more likely to be younger and therefore were less likely than non-Hispanic whites to have symptomatic knee OA. As depicted in Figures 1 and 2, over 10.4M non-Hispanic whites (7.5% of non-Hispanic whites at least 25 years of age [139M]), 1.6M non-Hispanic blacks (6.9% of 23M), 1.1M Hispanics (4.4% of 25M), and 0.7M other non-Hispanics (6.2% of 11M) had symptomatic knee OA in 2007–08. The prevalence of advanced disease was 57% among both non-Hispanic Whites and non-Hispanic blacks with symptomatic knee OA, 48% among Hispanics, and 55% among other non-Hispanic persons with symptomatic knee OA.
Figure 1.
Number of persons with knee OA in the United States, by age, sex, and race/ethnicity, in 2007–08
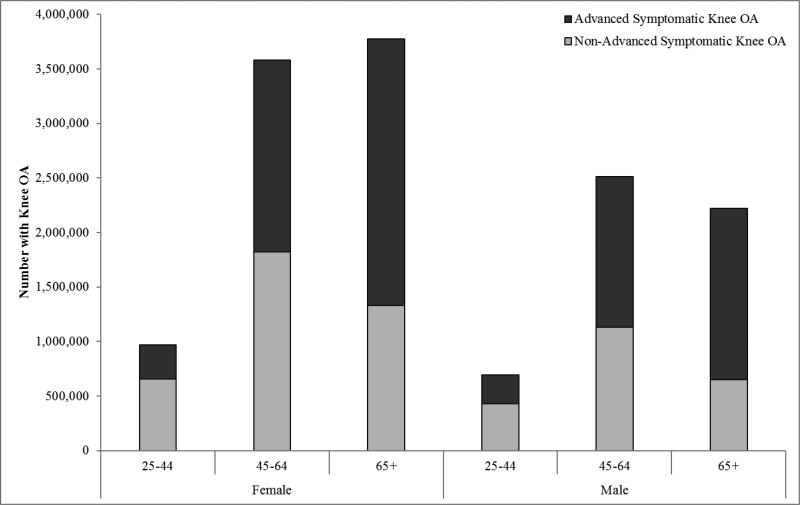
Figure 2.
Number of persons with knee OA in the United States, by age and sex, in 2007–08
Our analyses produced similar results using 2011–12 population parameters, except for Hispanics (primarily the result of a near-doubling in the obesity rate observed among Hispanics in NHANES 2011–12 as compared to NHANES 2007–08). Over 11.0M non-Hispanic whites (7.8% of 142M), 1.7M non-Hispanic blacks (7.2% of 24M), 1.6M Hispanics (5.7% of 29M), and 0.7M other non-Hispanics (5.4% of 13M) had symptomatic knee OA in 2011–12. The prevalence of advanced disease was 58% among non-Hispanic whites, 57% among non-Hispanic blacks, 55% among Hispanics, and 51% among other non-Hispanic persons with symptomatic knee OA.
Age and Sex
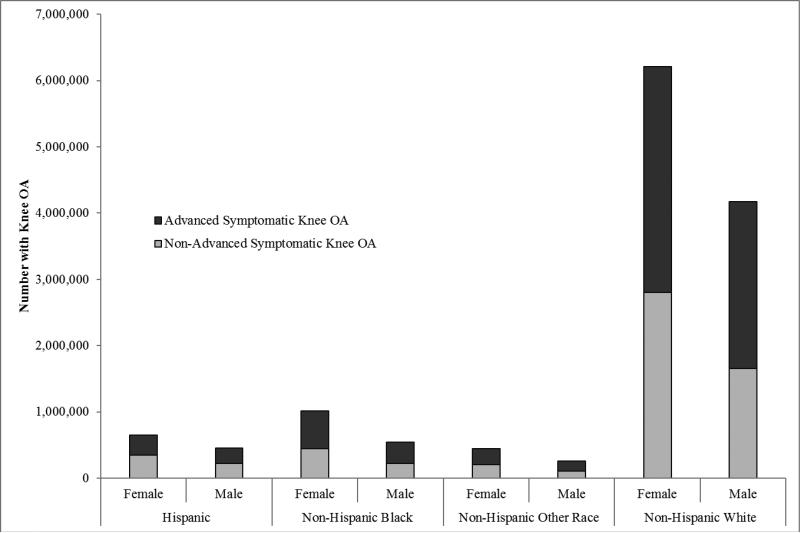
The prevalence of symptomatic knee OA increases with every decade of life, with the annual incidence of knee OA being highest between 55 and 64 years of age (Table 1). Because there are nearly twice as many persons in the US between the ages of 45 and 64 years than there are persons older than 65 years of age, even though prevalence is higher among the latter group, the overall number of persons with symptomatic knee OA was nearly identical among both groups (Figure 3).
Figure 3.
Number of persons with knee OA in the United States, by race/ethnicity and sex, in 2007–08
Among those 45–64 years old, there were 6.1M (7.8% of 78M) persons with symptomatic knee OA in 2007–08; 3.6M were female, and 2.5M were male. This increased to 6.6M (8.0% of 83M) in 2011–12. Among adults older than 65 years, there were 6.0M (15.6% of 38M) persons with symptomatic knee OA in 2007–08; 3.8M were female, and 2.2M were male. This increased to 6.8M (16.0% of 42M) in 2011–12. The proportion of persons with advanced disease was greater among the older group (67%) than the younger group (51%).
Additionally, we estimated that among adults under 45 years of age, 1.7M (2.0% of 82M) had symptomatic knee OA in 2007–08, with that figure remaining stable at 1.7M (2.1% of 83M) in 2011–12. About a third of younger persons have advanced symptomatic knee OA.
DISCUSSION
Using a nationally representative cross-sectional survey, we estimated that symptomatic knee OA affected about 14 million individuals among US adults aged 25 years and older in 2007–08, including 8.3 million females and 5.4 million males. Although more prevalent among older persons, one in eight persons with symptomatic knee OA is under 45 years old and nearly half are between 45–64 years of age. Symptomatic knee OA is prevalent among non-Hispanic whites (10.4 million persons) but also is a substantial public health concern among racial/ethnic minorities (3.4 million persons), especially among non-Hispanic blacks and Hispanics. Over the four years following our primary analysis years, we observed a net increase of 1.4 million with symptomatic knee OA and 0.9 million persons with advanced symptomatic knee OA as a result of population aging in all demographic strata and changes in obesity rates. The net increase may potentially have been twice as much if we had accounted for increased knee OA prevalence at the same rate as between 2000 and 2008.8
While there have been previous estimates of the number of persons with arthritis and related rheumatic conditions in the US (22% of the adult population in 2007–09, or 50 million persons total),26 to the best of our knowledge none have provided detailed age- and sex-stratified estimates of the number of persons affected by symptomatic knee OA among all racial/ethnic groups. Our overall estimate of the number of persons affected by symptomatic knee OA (13.7 million) is substantially larger than the National Arthritis Data Workgroup's 2005 estimate (9.3 million).8 We observe this large difference despite the fact that we conservatively adjusted our prevalence estimates in recognition of the fact that self-reported nature of NHIS that may lead persons to over-report a clinical diagnosis of arthritis.20,21 We believe that the differences primarily arise because of an increase in obesity rates as well as younger clinical diagnosis of knee OA in the previous several decades. In support of the estimates derived in the current report, a recent Medical Expenditure Panel Survey-based analysis by Cisternas et al. calculated that symptomatic OA of all joints affected 31 million Americans in 2008–11.27 Comparing results presented in this report with those of Cisternas et al. implies that slightly under half of all persons with symptomatic OA have symptomatic OA of the knee, consistent with data from the Johnston County Osteoarthritis Project that indicate that over two-fifths of all cases of radiographic OA involve the knee joint.28
We also estimated the proportion of persons with symptomatic knee OA that have advanced courses of knee joint damage (KL grades 3 or 4). The prevalence of KL 4 is lower than KL 3 because by the time that someone has advanced to KL 4, they are likely to be substantially older than someone with KL 3 OA and will accordingly have an elevated competing risk of mortality. While radiographically-apparent damage is only one of a number of factors that go into the surgical decision making process, many surgeons are only willing to consider TKR at advanced severity among persons who have failed conservative treatment.29,30 Coupled with a potential greater willingness on the part of the US population to undergo surgery to treat their knee pain, the substantial size of the population at risk may explain the rapid increase in the annual number of TKRs performed among all age groups, including younger and middle-aged adults.12
Among the two million persons with knee OA under 45 years of age, many likely have obesity-associated or post-traumatic OA.31,32 This early age of diagnosis poses a troubling public health burden. Accounting for comorbidities,22 a 45-year-old obese non-Hispanic white woman who has just developed knee OA has a 61% lifetime risk of undergoing TKR and a 7% lifetime risk of needing a revision TKR.33 The societal burden of knee OA can be alleviated by the promotion of weight loss, which has consistently been shown to be effective as secondary prevention for knee OA and holds significant promise for primary prevention as well.34,35 The large burden of knee OA further emphasizes the need for large-scale trials and community-based programs to manage the musculoskeletal effects of the obesity epidemic. Additionally, much basic science OA research currently focuses on evaluating the long-term impact of trauma on OA development. The large current burden of knee OA on younger persons, which is only expected to grow, highlights the importance of increasing the pace of translating research from bench to bedside.
Several methodologic choices underpinning our estimates were driven by the availability of data and merit comment. Data on both obesity as well as symptomatic knee OA prevalence were derived from cross-sectional studies, which did not permit us to evaluate whether there was a relationship between the time lived with extra body mass and the likelihood of developing OA. To evaluate knee OA prevalence by race/ethnicity group, we assumed that any variation from national age-sex-stratified prevalences was directly related to that group's obesity rate. While we were able to determine robust estimates of obesity prevalence for non-Hispanic whites, non-Hispanic blacks and Hispanics, estimates for other non-Hispanic persons comprise a small proportion of the NHANES cohort and should be treated with caution. Several factors are associated with the development of knee OA including genetics, occupational exposure and early structural changes such as cartilage defects, meniscal tear, and bone marrow lesions.1,36-39 Since we chose to present the number of persons affected by symptomatic knee OA from a public health perspective, we did not present the data stratified by these risk factors; however, we caution that some of these factors are likely associated with demographic characteristics under study.
We assumed that rates of KL progression were associated with obesity, as has been observed in some cohort studies,40,41 but we did not stratify such rates by age or race/ethnicity, finding insufficient evidence with regards to the extent that such characteristics have an independent effect on progression. The KL grading scale focuses exclusively on radiographically-visible damage to the tibiofemoral joint and ignores the patellofemoral joint;42,43 however, population-level progression rates using other measures of OA severity are lacking. These areas of uncertainty deserve future examination.
We also note that published estimates suggest that there are about four to five million persons who are currently living with a TKR implant,4,44 almost exclusively for advanced OA.45-47 As TKR recipients often experience periodic knee pain in the years following surgery,48 some such persons will be considered to have symptomatic knee OA in our analysis. Our estimate will over-count individuals with diagnosed arthritis of another joint who have knee pain unrelated to that arthritis, while it will undercount persons with knee OA who have not yet been diagnosed by a health professional as well as persons with diagnosed OA in addition to another rheumatic condition. Bolen et al. estimate that among Americans with chronic joint pain who have not been diagnosed with arthritis, only 6% would describe their symptoms in a manner that would suggest that they do in fact have arthritis.49
Our data support the evolving contemporary view of OA as a disease that affects not just older adults but also millions of younger and middle-aged adults. Additionally, over half of all persons with symptomatic knee OA have advanced disease. Policymakers should recognize that extant therapies and future treatments for knee OA, such as cost-effective disease-modifying drugs,50 may have a larger potential patient pool than previously realized. These data also underscore the urgency of developing treatment programs with proven long-term efficacy to assist the growing number of younger persons who will live with symptomatic knee OA for the majority of their adult lives.
SIGNIFICANCE AND INNOVATION.
Fourteen million individuals in the United States have symptomatic knee OA.
This includes nearly two million persons under the age of 45 years and six million persons between 45 and 64 years.
Although the racial/ethnic minority population is substantially younger than whites; over three million racial/ethnic minorities have symptomatic knee OA, a number that is expected to rise.
Over half of all individuals with diagnosed symptomatic knee OA have had sufficient progression of their OA such that they would be eligible for knee replacement if they had severe symptoms.
Acknowledgments
Supported by: National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) R01AR064320 and K24AR057827. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Author Contributions: Dr. Losina had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Obtaining of funding: Losina
Conception and design: Deshpande, Losina
Collection and assembly of data: Deshpande
Analysis and interpretation of the data: Deshpande, Katz, Solomon, Yelin, Hunter, Messier, Suter, Losina
Statistical expertise: Losina
Drafting of the article: Deshpande
Critical revision of the article for important intellectual content: Deshpande, Katz, Solomon, Yelin, Hunter, Messier, Suter, Losina
Final approval of the article: Deshpande, Katz, Solomon, Yelin, Hunter, Messier, Suter, Losina
Competing interest statement: Dr. Katz is President-Elect of the Osteoarthritis Research Society International (OARSI). Drs. Katz and Losina are Deputy Editors for Methodology and Biostatistics for the Journal of Bone and Joint Surgery. Dr. Solomon has received research support from Amgen, the Consortium of Rheumatology Researchers of North America, Eli Lilly, and Pfizer; has served in unpaid roles on studies sponsored by Bristol-Myers Squibb, Eli Lilly, Novartis, and Pfizer; has received royalties from UpToDate for contributions relating to non-steroidal anti-inflammatory drugs; and is Deputy Editor of Arthritis and Rheumatology. Dr. Hunter has received consulting fees from Abbott (<$10,000), Flexion (<$10,000), Merck Serno (<$10,000), Nestle (<$10,000), and SciMetrika (<$10,000) and royalties from DJO Global from a license agreement related to a patellofemoral sleeve. Dr. Messier has received consulting fees from Nestle (<$10,000) and SciMetrika (<$10,000) and is a Director of OARSI. The authors report no other competing interests.
Previous Presentation: A portion of this analysis was previously presented at the 2015 Annual Meeting of the American College of Rheumatology / Association of Rheumatology Health Professionals in San Francisco, CA under the title “Burden of symptomatic knee osteoarthritis in the United States: impact of race/ethnicity, age and sex.”
REFERENCES
- 1.Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP. Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:507–515. doi: 10.1016/j.joca.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 2.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, Bierma-Zeinstra SM, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22:363–388. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 3.Losina E, Paltiel AD, Weinstein AM, Yelin E, Hunter DJ, Chen SP, et al. Lifetime medical costs of knee osteoarthritis management in the United States: impact of extending indications for total knee arthroplasty. Arthritis Care Res. 2015;67:203–215. doi: 10.1002/acr.22412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weinstein AM, Rome BN, Reichmann WM, Collins JE, Burbine SA, Thornhill TS, et al. Estimating the burden of total knee replacement in the United States. J Bone Joint Surg Am. 2013;95:385–392. doi: 10.2106/JBJS.L.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol. 2012;26:649–658. doi: 10.1016/j.berh.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, Ramos E. The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage. 2011;19:1270–1285. doi: 10.1016/j.joca.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1323–1330. doi: 10.1136/annrheumdis-2013-204763. [DOI] [PubMed] [Google Scholar]
- 8.Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. J Rheumatol. 2006;33:2271–2279. [PubMed] [Google Scholar]
- 10.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 11.Ackerman IN, Bucknill A, Page RS, Broughton NS, Roberts C, Cavka B, et al. The substantial personal burden experienced by younger people with hip or knee osteoarthritis. Osteoarthritis Cartilage. 2015;23:1276–1284. doi: 10.1016/j.joca.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–207. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donnell-Fink LA, Klara K, Collins JE, Yang HY, Goczalk MG, Katz JN, et al. Effectiveness of knee injury and anterior cruciate ligament tear prevention programs: a meta-analysis. PLoS One. 2015;10:e0144063. doi: 10.1371/journal.pone.0144063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Freedman DS. Obesity - United States, 1988-2008. MMWR Surveill Summ. 2011;60(Suppl):73–77. [PubMed] [Google Scholar]
- 15.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006;443:266–272. doi: 10.1097/01.blo.0000188066.01833.4f. [DOI] [PubMed] [Google Scholar]
- 16.Leininger RE, Knox CL, Comstock RD. Epidemiology of 1.6 million pediatric soccer-related injuries presenting to US emergency departments from 1990 to 2003. Am J Sports Med. 2007;35:288–293. doi: 10.1177/0363546506294060. [DOI] [PubMed] [Google Scholar]
- 17.Esquivel AO, Bruder A, Ratkowiak K, Lemos SE. Soccer-related injuries in children and adults aged 5 to 49 years in US emergency departments from 2000 to 2012. Sports Health. 2015;7:366–370. doi: 10.1177/1941738115579854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Losina E, Weinstein AM, Reichmann WM, Burbine SA, Solomon DH, Daigle ME, et al. Lifetime risk and age at diagnosis of symptomatic knee osteoarthritis in the US. Arthritis Care Res. 2013;65:703–711. doi: 10.1002/acr.21898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Health Interview Survey. National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services; Hyattsville, MD: 2007–08. [March 1, 2015]. < http://www.cdc.gov/nchs/nhis/quest_data_related_1997_forward.htm>. [Google Scholar]
- 20.Peeters GM, Alshurafa M, Schaap L, de Vet HC. Diagnostic accuracy of self-reported arthritis in the general adult population is acceptable. J Clin Epidemiol. 2015;68:452–459. doi: 10.1016/j.jclinepi.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 21.Rasooly I, Papageorgiou AC, Badley EM. Comparison of clinical and self reported diagnosis for rheumatology outpatients. Ann Rheum Dis. 1995;54:850–852. doi: 10.1136/ard.54.10.850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Losina E, Walensky RP, Reichmann WM, Holt HL, Gerlovin H, Solomon DH, et al. Impact of obesity and knee osteoarthritis on morbidity and mortality in older Americans. Ann Intern Med. 2011;154:217–226. doi: 10.1059/0003-4819-154-4-201102150-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Holt HL, Katz JN, Reichmann WM, Gerlovin H, Wright EA, Hunter DJ, et al. Forecasting the burden of advanced knee osteoarthritis over a 10-year period in a cohort of 60-64 year-old US adults. Osteoarthritis Cartilage. 2011;19:44–50. doi: 10.1016/j.joca.2010.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bridged-Race Resident Population Estimates: United States, State and County for the years 1990-2014. Centers for Disease Control and Prevention; Atlanta, GA: [March 1, 2015]. < http://wonder.cdc.gov/wonder/help/bridged-race.html#>. [Google Scholar]
- 25.National Health and Nutrition Examination Survey. National Center for Health Statistics, Centers for Disease Control and Prevention, US Department of Health and Human Services; Hyattsville, MD: 2007–08. [March 1, 2015]. < http://wwwn.cdc.gov/nchs/nhanes/search/nhanes07_08.aspx>. [Google Scholar]
- 26.Prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation --- United States, 2007-2009. Morb Mortal Wkly Rep. 2010;59:1261–1265. [PubMed] [Google Scholar]
- 27.Cisternas MG, Murphy L, Sacks JJ, Solomon DH, Pasta DJ, Helmick CG. Alternative Methods for Defining Osteoarthritis and the Impact on Estimating Prevalence in a US Population-Based Survey. Arthritis Care Res. 2015 doi: 10.1002/acr.22721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nelson AE, Renner JB, Schwartz TA, Kraus VB, Helmick CG, Jordan JM. Differences in multijoint radiographic osteoarthritis phenotypes among African Americans and Caucasians: the Johnston County Osteoarthritis project. Arthritis Rheum. 2011;63:3843–3852. doi: 10.1002/art.30610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dowsey MM, Nikpour M, Dieppe P, Choong PF. Associations between pre-operative radiographic changes and outcomes after total knee joint replacement for osteoarthritis. Osteoarthritis Cartilage. 2012;20:1095–1102. doi: 10.1016/j.joca.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 30.Collins JE, Deshpande BR, Katz JN, Losina E. Race and sex specific incidence rates and predictors of total knee arth roplasty: Seven year cumulative data from the Osteoarthritis Initiative. Arthritis Care Res. 2015 doi: 10.1002/acr.22771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coggon D, Reading I, Croft P, McLaren M, Barrett D, Cooper C. Knee osteoarthritis and obesity. Int J Obes Relat Metab Disord. 2001;25:622–627. doi: 10.1038/sj.ijo.0801585. [DOI] [PubMed] [Google Scholar]
- 32.Lotz M K, Kraus VB. New developments in osteoarthritis. Posttraumatic osteoarthritis: pathogenesis and pharmacological treatment options. Arthritis Res Ther. 2010;12:211. doi: 10.1186/ar3046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Losina E, Klara K, Michl GL, Collins JE, Katz JN. Development and feasibility of a personalized, interactive risk calculator for knee osteoarthritis. BMC Musculoskelet Disord. 2015;16:312. doi: 10.1186/s12891-015-0771-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, DeVita P, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310:1263–1273. doi: 10.1001/jama.2013.277669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bucknor MD, Nardo L, Joseph GB, Alizai H, Srikhum W, Nevitt MC, et al. Association of cartilage degeneration with four year weight gain--3T MRI data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2015;23:525–531. doi: 10.1016/j.joca.2014.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loughlin J. Genetic contribution to osteoarthritis development: current state of evidence. Curr Opin Rheumatol. 2015;27:284–288. doi: 10.1097/BOR.0000000000000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eckstein F, Collins JE, Nevitt MC, Lynch JA, Kraus VB, Katz JN, et al. Brief Report: Cartilage Thickness Change as an Imaging Biomarker of Knee Osteoarthritis Progression: Data From the Foundation for the National Institutes of Health Osteoarthritis Biomarkers Consortium. Arthritis Rheumatol. 2015;67:3184–3189. doi: 10.1002/art.39324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang F, Kumm J, Svensson F, Turkiewicz A, Frobell R, Englund M. Risk factors for meniscal body extrusion on MRI in subjects free of radiographic knee osteoarthritis: longitudinal data from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2015 doi: 10.1016/j.joca.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 39.Sharma L, Chmiel JS, Almagor O, Dunlop D, Guermazi A, Bathon JM, et al. Significance of preradiographic magnetic resonance imaging lesions in persons at increased risk of knee osteoarthritis. Arthritis Rheumatol. 2014;66:1811–1819. doi: 10.1002/art.38611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reijman M, Pols HA, Bergink AP, Hazes JM, Belo JN, Lievense AM, et al. Body mass index associated with onset and progression of osteoarthritis of the knee but not of the hip: the Rotterdam Study. Ann Rheum Dis. 2007;66:158–162. doi: 10.1136/ard.2006.053538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Felson DT, Goggins J, Niu J, Zhang Y, Hunter DJ. The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum. 2004;50:3904–3909. doi: 10.1002/art.20726. [DOI] [PubMed] [Google Scholar]
- 42.McAlindon TE, Snow S, Cooper C, Dieppe PA. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Ann Rheum Dis. 1992;51:844–849. doi: 10.1136/ard.51.7.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Petersson IF, Boegard T, Saxne T, Silman AJ, Svensson B. Radiographic osteoarthritis of the knee classified by the Ahlback and Kellgren & Lawrence systems for the tibiofemoral joint in people aged 35-54 years with chronic knee pain. Ann Rheum Dis. 1997;56:493–496. doi: 10.1136/ard.56.8.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97:1386–1397. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eckstein F, Boudreau RM, Wang Z, Hannon MJ, Wirth W, Cotofana S, et al. Trajectory of cartilage loss within 4 years of knee replacement--a nested case-control study from the Osteoarthritis Initiative. Osteoarthritis Cartilage. 2014;22:1542–1549. doi: 10.1016/j.joca.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gioe TJ, Novak C, Sinner P, Ma W, Mehle S. Knee arthroplasty in the young patient: survival in a community registry. Clin Orthop Relat Res. 2007;464:83–87. doi: 10.1097/BLO.0b013e31812f79a9. [DOI] [PubMed] [Google Scholar]
- 47.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86-A:1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 48.Bonnin MP, Basiglini L, Archbold HA. What are the factors of residual pain after uncomplicated TKA? Knee Surg Sports Traumatol Arthrosc. 2011;19:1411–1417. doi: 10.1007/s00167-011-1549-2. [DOI] [PubMed] [Google Scholar]
- 49.Bolen J, Helmick CG, Sacks JJ, Gizlice Z, Potter C. Should people who have joint symptoms, but no diagnosis of arthritis from a doctor, be included in surveillance efforts? Arthritis Care Res. 2011;63:150–154. doi: 10.1002/acr.20313. [DOI] [PubMed] [Google Scholar]
- 50.Losina E, Daigle ME, Suter LG, Hunter DJ, Solomon DH, Walensky RP, et al. Disease-modifying drugs for knee osteoarthritis: can they be cost-effective? Osteoarthritis Cartilage. 2013;21:655–667. doi: 10.1016/j.joca.2013.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]