Abstract
Background—
Provisional stenting is effective for anatomic simple bifurcation lesions. Double kissing crush stenting reduces the 1-year rate of target lesion revascularization. This study aimed to investigate the 5-year clinical results of the DKCRUSH-II study (Randomized Study on Double Kissing Crush Technique Versus Provisional Stenting Technique for Coronary Artery Bifurcation Lesions).
Methods and Results—
A total of 370 patients with coronary bifurcation lesions who were randomly assigned to either the double kissing crush or provisional stenting group in the DKCRUSH-II study were followed for 5 years. The primary end point was the occurrence of a major adverse cardiac event at 5 years. Patients were classified by simple and complex bifurcation lesions according to the DEFINITION criteria (Definitions and Impact of Complex Bifurcation Lesions on Clinical Outcomes After Percutaneous Coronary Intervention Using Drug-Eluting Stents). At 5 years, the major adverse cardiac event rate (23.8%) in the provisional stenting group was insignificantly different to that of the double kissing group (15.7%; P=0.051). However, the difference in the target lesion revascularization rate between 2 groups was sustained through the 5-year follow-up (16.2% versus 8.6%; P=0.027). The definite and probable stent thrombosis rate was 2.7% in each group (P=1.0). Complex bifurcation was associated with a higher rate of target lesion revascularization (21.6%) at 5 years compared with 11.1% in patients with a simple bifurcation (P=0.037), with an extremely high rate in the provisional stenting group (36.8% versus 12.5%, P=0.005) mainly because of final kissing balloon inflation (19.4% versus 5.2%; P=0.036).
Conclusions—
The double kissing crush stenting technique for coronary bifurcation lesions is associated with a lower rate of target lesion revascularization. The optimal stenting approach based on the lesions’ complexity may improve the revascularization for patients with complex bifurcations.
Clinical Trial Registration—
URL: http://www.chictr.org. Unique identifier: ChiCTR-TRC-0000015.
Keywords: angiography, aspirin, coronary artery bifurcation lesions, double kissing crush, myocardial infarction, stents, thrombosis
WHAT IS KNOWN
Provisional side branch stenting is effective for the majority of coronary artery bifurcation lesions.
Double kissing crush stenting technique is reported to be associated with lower risk of 1-year clinical events.
Long-term results after double kissing crush are unknown.
WHAT THE STUDY ADDS
Our data showed that the benefits of double kissing crush stenting for true coronary bifurcation lesions were sustained through 5-year follow-up.
This was also true for complex bifurcation lesions.
Several studies1–4 have pointed out that provisional stenting (PS), stenting the main vessel (MV) with provisional side branch (SB) stenting if suboptimal results (Thrombolysis in Myocardial Infarction <3 or greater than type B dissection or a higher grade residual stenosis) in SB occur, is comparable to systematic 2-stent techniques for coronary bifurcation lesions in terms of short-term1–4 or 5-year5 clinical outcomes. However, the wide discrepancy in inclusion/exclusion criteria, criteria for stenting SB, and lesion complexity6 is reminders of the caution when translating these studies to individual patients. In the randomized DKCRUSH-II study (Randomized Study on Double Kissing Crush Technique Versus Provisional Stenting Technique for Coronary Artery Bifurcation Lesions),7 we compared the double kissing (DK) crush and PS techniques for real true coronary bifurcation lesions and for the first time observed <1-year target lesion revascularization (TLR) in the DK crush group. Unfortunately, there are no data showing the long-term clinical outcomes of the DK crush technique, particularly TLR and safety end point stent thrombosis (ST). Accordingly, the aim of this study was to evaluate the 5-year clinical outcomes after DK crush and PS for the patient population from the DKCRUSH-II study. The outcome in these patients was also compared in a subgroup stratified by DEFINITION criteria (Definitions and Impact of Complex Bifurcation Lesions on Clinical Outcomes After Percutaneous Coronary Intervention Using Drug-Eluting Stents),6 a stratification system to differentiate simple from complex coronary bifurcation lesions.
Methods
Study Design and Patient Population
The DKCRUSH-II study was an international, multicenter, and randomized study designed to compare the DK crush and the PS techniques for patients with Medina 1,1,1 and 0,1,1 bifurcation lesions.8 The primary end point of the primary publication was the 12-month composite major adverse cardiac event (MACE), including cardiac death, myocardial infarction (MI), and target vessel revascularization, whereas angiographic follow-up was performed 8 months after the indexed procedures. The study protocol was approved by the Ethics Committee in 7 participating centers, and written consent was obtained from all patients or their legally authorized representatives. The clinical follow-up was scheduled ≤5 years as shown in Figure 1. Finally, between April 2007 and June 2009, a total of 370 patients were enrolled (185 in each group). In brief, patients were eligible if they had ischemic symptoms or evidence of myocardial ischemia in the presence of a Medina8 1,1,1 or 0,1,1 de novo coronary bifurcation lesions. For inclusion, the maximum treatable lesion length by visual estimation for each individual branch had to be completely covered by 2 Excel stents (JW Medical Systems, Weihai, China). Excel stent is a rapamycin-coated stent with biodegradable polymer launched in 2004 in China. The exclusion criteria have been described in detail previously.7 Patients were randomly assigned to the study groups in a 1:1 ratio before undergoing balloon dilation. The main stenting techniques have been described previously.7 Final kissing balloon inflation (FKBI) was recommended for all DK crush and some of the PS group after ballooning SB.
Figure 1.
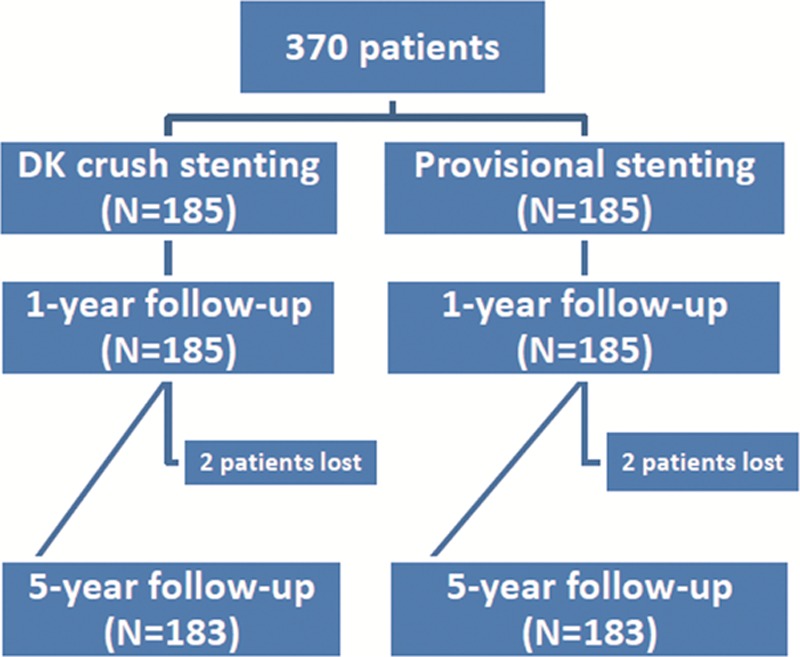
Study flowchart of the DKCRUSH-II study (Randomized Study on Double Kissing Crush Technique Versus Provisional Stenting Technique for Coronary Artery Bifurcation Lesions). Eight months after an indexed stenting procedure, 91.6% of patients underwent angiographic follow-up. DK indicates double kissing.
Medications
A 300-mg loading dose of clopidogrel was administered before the index procedure if the patient was not pretreated. After the intervention, all patients received 300 mg per day aspirin for 1 month; thereafter, they received 100 mg per day indefinitely for life. Clopidogrel (75 mg per day) was continued for at least 12 months. After 1 year, clopidogrel was not routinely prescribed and left at the discretion of the patients’ physician.
Definition of Study End Points
The primary end point was the occurrence of a MACE at 5 years, which included MI, cardiac death, and clinically driven target vessel revascularization. Repeat angiography was performed only after the recurrence of symptoms after the indexed stenting procedure. The rate of definite and probable ST served as a safety end point. MI was diagnosed if the plasma level of creatine kinase (CK)-MB and troponin I/T increased to >3× the upper normal limit in no fewer than 2 blood samples. All deaths were considered as cardiac in origin unless noncardiac reasons were indicated. TLR and target vessel revascularization were defined as any repeat revascularization (percutaneous coronary intervention or coronary artery bypass graft) for target lesions and target vessels, respectively, in the presence of symptoms or objective signs of ischemia. ST was defined according to the Academic Research Consortium definition.9
Statistical Analysis
The calculation of the patient sample size has been described previously.7 The treatment group differences were evaluated with a t test or the Wilcoxon rank-sum score for continuous variables when appropriate. The χ2 test or Fisher exact test was used to analyze categorical variables. Survival rates free from events were generated by the Kaplan–Meier analysis and were compared using the log-rank test. Patients were classified by simple and complex subgroups according to DEFINITION criteria.6 Briefly, complex bifurcation was defined as SB diameter stenosis minimal 90% and SB lesion length ≥10 mm, plus at least 2 minor criteria (including MV lesion length ≥25 mm, MV reference diameter <2.5 mm, moderate or severe calcification, a bifurcation angle ≤45° or ≥70°, multiple lesions, and thrombus-containing lesions). Statistical significance was taken as a 2-sided P value <0.05. All analyses were performed with the statistical program SPSS 16.0 (SPSS Institute Inc, Chicago, IL).
Results
Baseline Characteristics
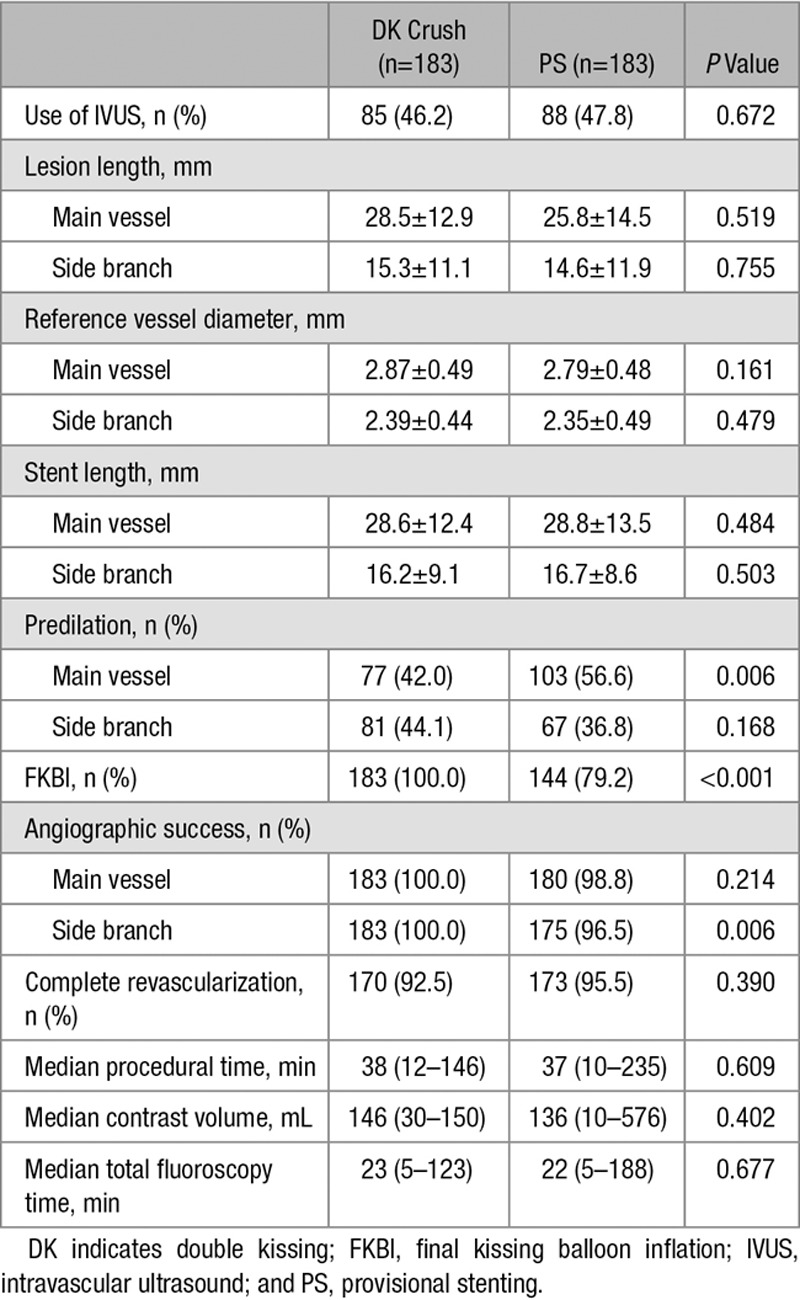
Four patients were lost to the 5-year follow-up, with 2 patients in each group. Finally, 366 patients (183 in each group) formed the basis of this study. Baseline clinical and procedural characteristics are shown in Tables 1 and 2. In brief, of 366 patients, 16.5% had recent MI (>2 weeks), 33.5% had 3 vessel diseases, and 16.6% localized at the distal left main. Intravascular ultrasound (IVUS) assessment was used in >46% of patients. FKBI was not performed in 38 (27.7%) cases in the PS group. Angiographic success was achieved in >99% of the patients. Complete revascularization was achieved in 92.4% of the DK group and 97.8% of the PS group. An 8-month angiographic follow-up after indexed procedures was available for 91.6% (n=337) of the patients.
Table 1.
Baseline Clinical and Angiographic Characteristics
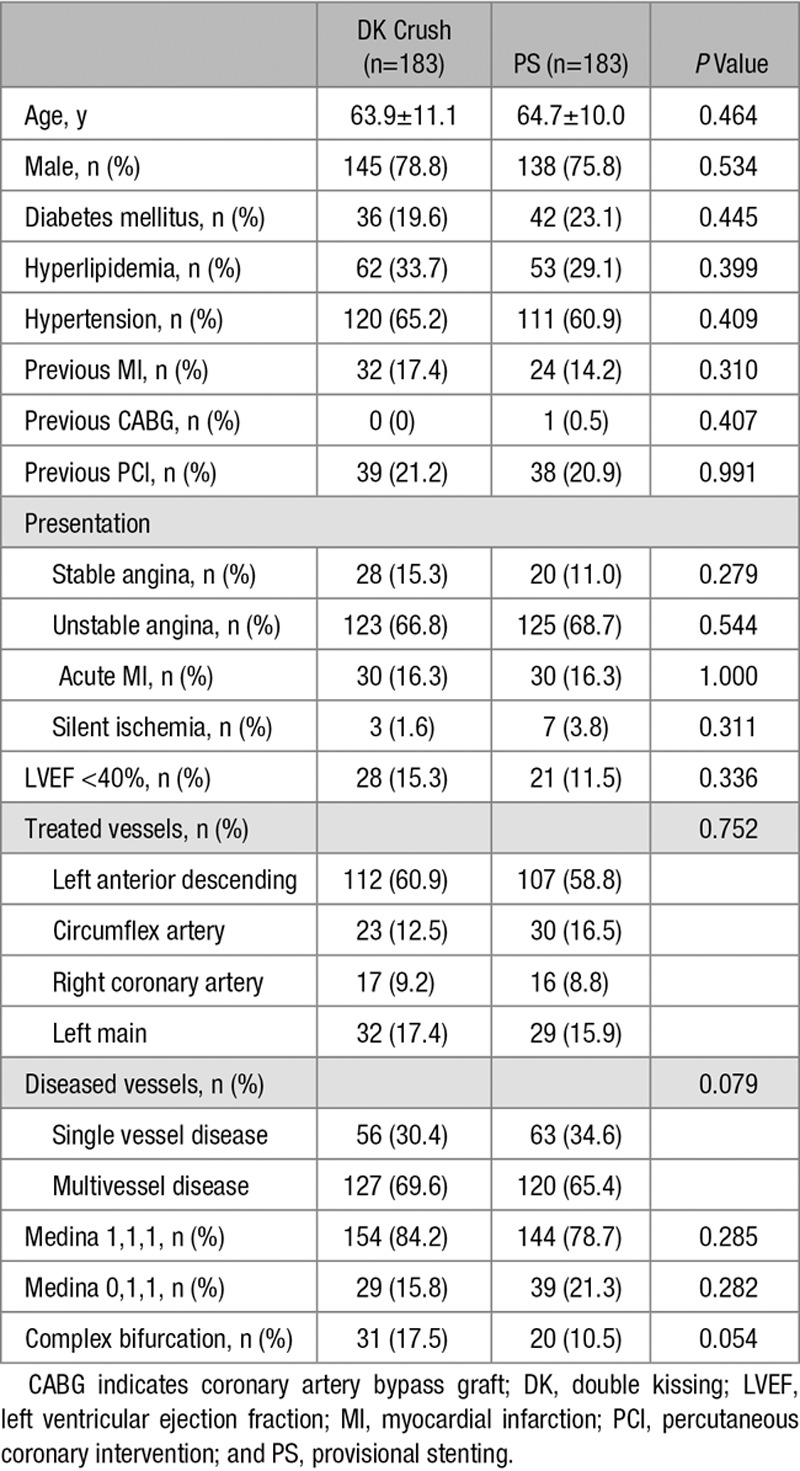
Table 2.
Procedural Characteristics
Medication
No patient was intolerable to 300 mg per day of aspirin in the first month after the stenting procedure. At the end of the 5-year follow-up, aspirin was not taken by 36 (19.7%) patients in the DK group and 35 (19.1%) patients in the PS group (P=1.0) because patients who had no ST were intolerable to aspirin-induced gastrointestinal symptoms. For these patients, traditional Chinese medicine was used to replace aspirin. Dual antiplatelet therapy (DAPT) was prescribed in 70 (37.8%) patients in the DK group and to 74 (40.0%) patients in the PS group, and the difference was not significant (P=0.749).
The 5-Year Follow-Up
At 5-year follow-up, the cumulative incidence of MACE was 23.8% in the PS group and 15.7% in the DK group (hazard ratio, 1.679; 95% confidence interval, 0.997–2.827; P=0.051; Table 3; Figure 2). The significant difference in TLR between the DK group (8.6%) and the PS group (16.2%, P=0.027) was sustained through the 5-year follow-up. Among 183 patients in the PS group, 144 (72.3%) underwent FKBI, and it was associated with a higher rate of TLR (19.4%, n=28) compared with 38 patients who had no FKBI (5.2%, n=2; P=0.036). Similarly, for all 366 patients, an IVUS assessment had a lower rate of MI (1.8%) compared with 5.4% in the angiographic guidance subgroup (P=0.043).
Table 3.
The 5-Year Clinical Outcomes After DK Crush and PS
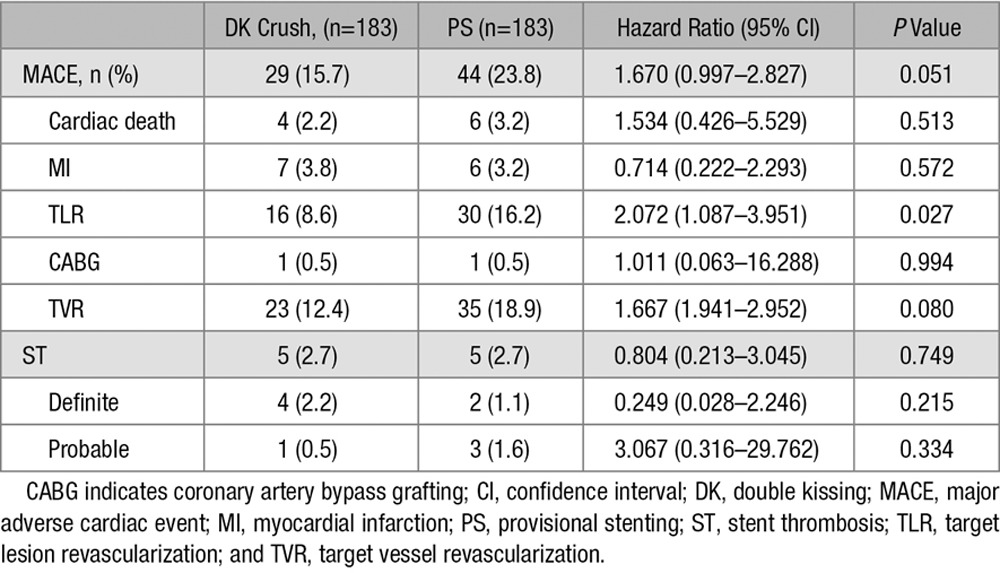
Figure 2.
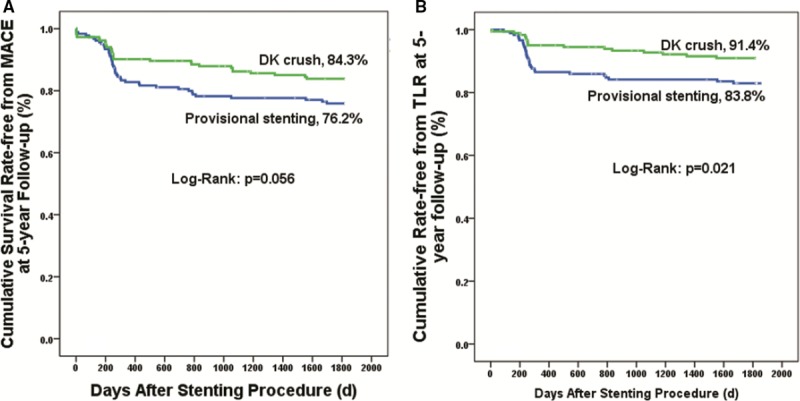
Kaplan–Meier analysis. The cumulative survival rate free from major adverse cardiac event (MACE; A) and target lesion revascularization (TLR; B) at a 5-year follow-up after the double kissing (DK) crush and provisional stenting techniques.
By 5 years after the indexed procedures, the rate of definite and probable ST was 2.7% (n=5) in both groups (P=1.0). The rates of event-free survival of definite and probable ST are shown in Figure 3. The rate of early (<30 days), late (within 1 year), and very late (>1 year) ST was 0.5%, 1.1%, and 1.1% in the PS group, and 2.2%, 0.5%, and 0% in the DK group, respectively, and the difference was not significant (all P>0.05). Three patients (2 in the DK group and 1 in the PS group) had a definite or probable ST while not taking DAPT.
Figure 3.
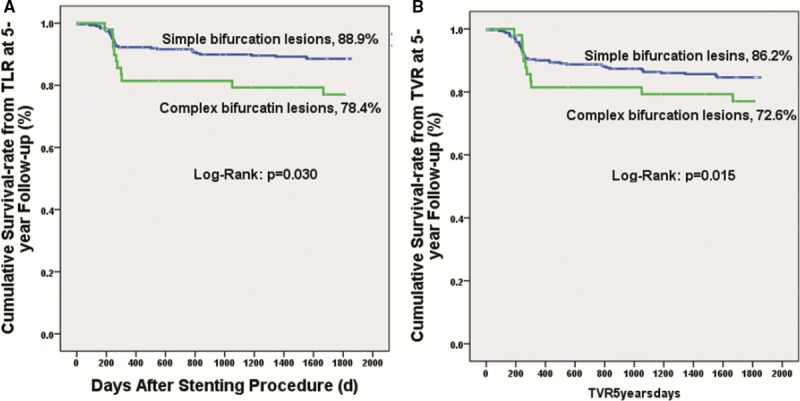
Kaplan–Meier analysis. The cumulative survival rate from target lesion revascularization (TLR; A) and target vessel revascularization (TVR; B) at a 5-year follow-up in patients with complex and simple bifurcation lesions after stent implantation.
Simple Versus Complex Lesions
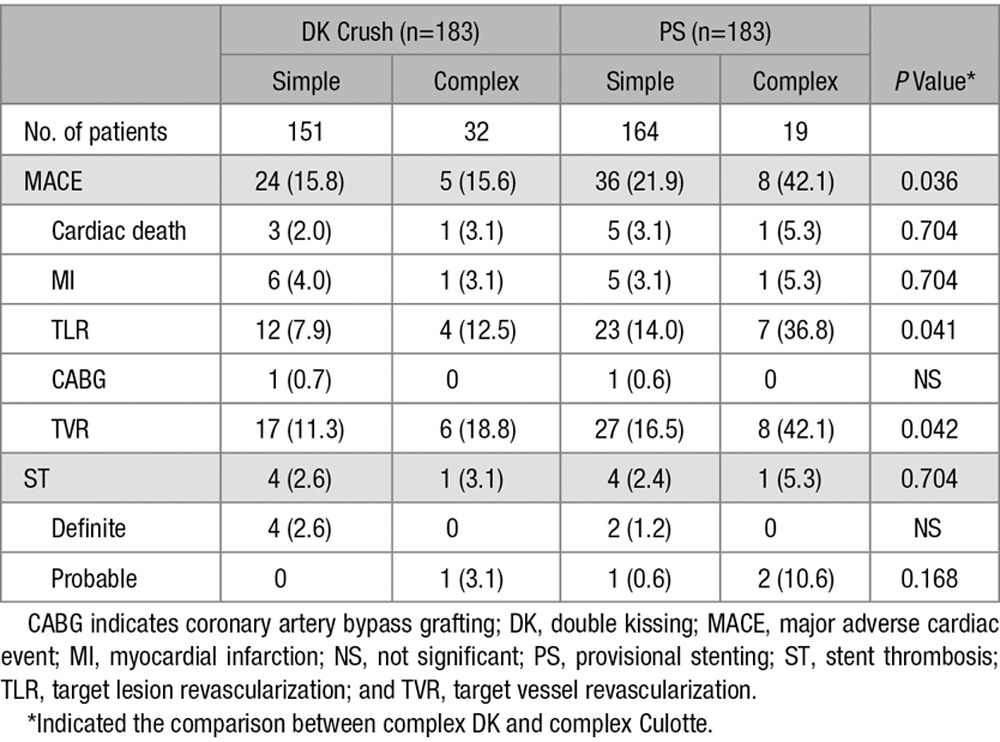
According to the DEFINITION criteria,6 51 (13.9%) patients were classified by complex subgroup, and 315 (86.1%) were included in the simple bifurcation subgroup. There was a significant difference in the 5-year rates of TLR between simple (11.1%) and complex (21.6%, P=0.037; Table 4; Figure 4), particularly in patients with complex bifurcation lesions treated by PS (Table 5).
Table 4.
The 5-Year Clinical Outcomes After Stenting in Patients With Complex and Simple Coronary Bifurcation Lesions From 366 Patients
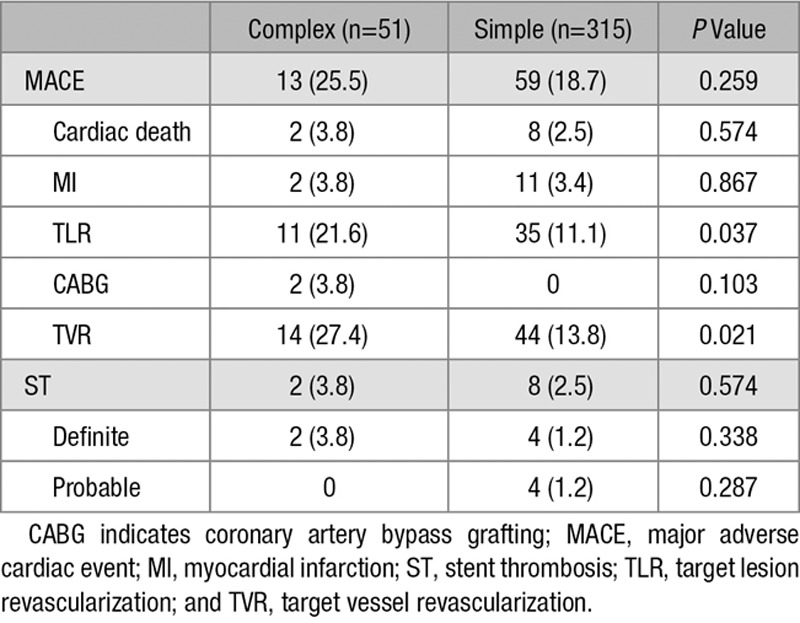
Figure 4.
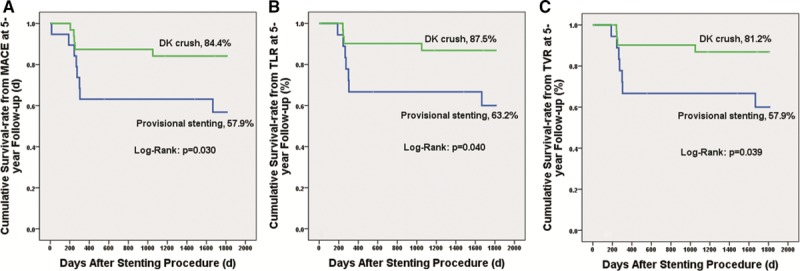
Kaplan–Meier analysis. The survival rate free from major adverse cardiac event (MACE; A), target lesion revascularization (TLR; B), and target vessel revascularization (TVR; C) of patients with complex bifurcations after double kissing (DK) crush vs provisional stenting.
Table 5.
The 5-Year Clinical Outcomes in Simple and Complex Bifurcation Lesions After Either DK Crush or PS
Replacing MI by target vessel MI to perform a post hoc analysis, the rate of target lesion failure at the end of the 5-year follow-up was 11.4% in the DK group and 20.4% in the PS group (P=0.011).
Discussion
To our knowledge, this is the first report of long-term follow-up results from a multicenter and randomized study comparing DK crush and PS for patients with real true coronary bifurcation lesions. We found that a significant difference in TLR between the 2 strategies was sustained through the 5-year follow-up, with the data favoring DK crush, even though the 5-year MACE rate did not achieve statistical significance.
Of 4 major randomized clinical studies1–4 that compared PS with systematic 2-stent techniques, only the Nordic Bifurcation study5 reported long-term clinical outcomes. The authors reported that the rate of composite MACE at a 5-year follow-up after the indexed procedure was not different between the 2 groups, which is similar to but slightly different from our results (23.8% in the PS group and 15.7% in the DK group) with a P value at the marginal level (P=0.05); this implied that this difference in MACE would have become significant if the sample size was expanded. Notably, the Nordic Bifurcation study 5-year results showed that the definite (angiographically confirmed) ST in PS increased by 2× (3.0% versus 1.5%; P=0.32) although without significant difference.5 Our analysis found a catch-up phenomenon of ST in the PS group, with ST defined as late and very late. Even though 26.2% of the patients were not taking DAPT at the 5-year follow-up, only 1 patient had ST in PS, a result indicating that the progression of lesions in SB might be the main reason for the increased ST beyond 30 days. Thus far, there has been lack of studies showing the progression of lesions (particularly in SB) after PS treatment during long-term follow-up. Using analysis from the PS technique, FKBI is recommended mostly if ballooning SB is required. An intravascular study10 showed that KBI significantly reduced SB stenosis and repaired distorted stents in the MV. However, a recent randomized study did not show any significant benefit of routine KBI11 after PS. Our subgroup analysis demonstrated that FKBI induced an increase in TLR after stenting MV alone, a finding supported by the DKCRUSH-VI study,12 a randomized clinical study comparing fractional flow reserve (FFR)-guided versus angiography-guided PS, from which we found: (1) FKBI after bailed-out SB stenting or SB angioplasty alone was associated with a higher rate of ISR in distal MV, with a resultant higher TLR rate and (2) in the FFR-guided group, FKBI after ballooning SB because of decreased SB FFR after stenting MV had a 7.8% of SB FFR <0.80, indicating the development of ischemia at the area supplied by the related SB. Furthermore, a prospective, multicenter study by Burzotta et al13 showed that patients receiving the second stent as a bailout had worse survival free from MACE than those who received it as a planned technique (P = 0.045). Taking together, less FKBI (34%) and less SB stenting (4.4%) may be a possible explanation for the lower 5-year rate of TLR after PS in the Nordic Bifurcation study 5-year follow-up.5 Furthermore, even this study included more patients with multivessel disease (68%), but complete revascularization was achieved in >94% of patients. This might be 1 reason to exclude the effect of multivessel disease on the clinical outcome in our study.
When comparing the results between the DKCRUSH-II study and the Nordic Bifurcation study, it should be noted that there are wider discrepancies among these 2 studies, such as unstable angina (>67% versus 33%), acute myocardial infarction (16% versus 0%), previous MI (15.5% versus 0%), left ventricular ejection fraction <40% (13% versus 0%), Medina 1,1,1/0,1,1 (100% versus <72%), left main bifurcation (16.7% versus 1.5%), SB lesion length (15 mm versus 5 mm) and diameter stenosis (68.3% versus <50%), and FKBI after 2 stents (100% versus 74%). These anatomic characteristics reflected more high-risk patients and more complex bifurcation lesions in our study, which predicted a more frequent occurrence of TLR in line with the DEFINITION study. According to DEFINITION criteria,6 the subgroup analysis from DKCRUSH-II study (these patients not included in DEFINITION analyses) showed that stenting complex bifurcation lesions in 51 patients had worse clinical outcomes than simple bifurcated lesions, with an extremely higher TLR rate in the PS group. Consequently, the selection of stenting technique (PS versus DK crush or other 2 stents) should be expected to be based on the classification of the lesions’ complexity.6
PS is usually considered to be a simple stenting technique. In fact, PS with SB stenting is somewhat difficult if there is severe proximal tortuous, moderate to severe calcification, and an uncomfortable SB anatomy. Furthermore, the coverage of ostial SB in the case of a narrow bifurcation angle is commonly challenging.14 In a bench test, Zhang et al14 found that PS with the T and protrusion technique was always associated with 1 to 2 floating struts in the MV after FKBI for bifurcations with an angle varying from 45° to 60°, which may be at least a partial mechanism for the occurrence of late and very late ST after PS. Furthermore, diameters (balloon/vessel ratio) and patterns of balloons during FKBI (as short overlapping as possible in the MV) were not fixed in the previous studies,1–5 which also influences the short- and long-term results.14 Bench tests14,15 and clinical analysis16 have addressed the importance of the proximal optimization technique after FKBI to improve immediate and 1-year results; the technique was proposed before the start of either Nordic Bifurcation study5 or the DKCRUSH-II study. Consequently, the routine use of the proximal optimization technique should be recommended in further clinical studies. Finally, there is a lack of a randomized study showing the significance of IVUS-guided stenting bifurcation lesions. However, several reports showed the positive effect of IVUS guidance, particularly for 2-stent procedures, on the reduction of MI and cardiac death after stenting bifurcations.17–19 Obviously, almost half of the stenting procedures were guided by IVUS in the DKCRUSH-II study,7 which may be another factor reducing the requirement of revascularization after DK crush at a 5-year follow-up.
Notably, SB diameter is 1 indication for stenting technique selection.11 For bifurcation lesions with small SB (usually <2.0 mm in diameter), keep it open is recommended.11,20 In the COBIS II registry study (Korean Coronary Bifurcation Stenting),20 SB with a diameter ≥2.3 mm was enrolled, similar to previous studies1–5 and our study.7 An agreement among the studies was that a sizable SB was associated with adverse clinical outcomes.7,20 In the current analysis, the average SB diameter was <2.5 mm; however, it should be noted that a diffuse lesion (14.9 mm, Table 2) may underestimate the real SB reference diameter, which recalls the importance of IVUS to determine the anatomic features of a diseased SB.21 Furthermore, our ongoing DEFINITION 2 study, which only includes true bifurcation lesions with an SB minimally 2.5 mm in diameter, will provide new data for the difference in clinical outcomes after PS or systematic 2-stent techniques.
Study Limitations
First, 71 patients were not taking aspirin on the 5-year follow-up; however, the effect of stopping aspirin on TLR could not be excluded even if none of them had ST. Second, of 26.2% patients who were not put on DAPT, 2 in the DK group and 1 in the PS group had ST, indicating that a longer DAPT duration might be beneficial for patients with more complex bifurcation lesions. Third, IVUS data were not included in the analysis. But the higher rate of MI in angiography guidance addressed the importance of IVUS, in line with the previous reports.17–19,22 Fourth, as the angiographic follow-up was scheduled before the 1-year clinical follow-up, vision reflex could not be excluded. However, revascularization was not performed for patients with angiographic stenosis and without clinical symptoms, suggesting clinically driven TLR in this analysis. Finally, this study was not originally meant to compare complex and simple bifurcation lesions. Moreover, this study included some patients with an SB diameter <2.5 mm. Thus, our data should be very cautiously translated.
Conclusions
The 5-year clinical follow-up of the DKCRUSH-II study showed the reduction of TLR by DK crush, with a marginal difference in composite MACE when compared with PS. Given the universal acceptance of PS as recommended for simplex bifurcation lesions, patients with more complex bifurcations benefited from the DK crush technique under the IVUS guidance. Improvement of stenting techniques is crucial to achieve optimal postprocedural results and better clinical results. Further clinical study is required to compare DK crush with PS for complex bifurcated lesions.
Acknowledgments
We deeply appreciate Ling Lin, Tian Xu, Jing Kan, Hai-Mei Xu, Ying-Ying Zhao, and Ling-Ling Liu for their great contributions to data collection and remote monitoring. Most importantly, we acknowledge Bao-Xian Duan, who worked hard as an independent member for analyzing clinical events.
Sources of Funding
This study was granted by the National Natural Science Foundation of China (NSFC 81270191, NSFC 91439118, and NSFC 91639303).
Disclosures
None.
References
- 1.Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, Gunnes P, Mannsverk J, Meyerdierks O, Rotevatn S, Niemelä M, Kervinen K, Jensen JS, Galløe A, Nikus K, Vikman S, Ravkilde J, James S, Aarøe J, Ylitalo A, Helqvist S, Sjögren I, Thayssen P, Virtanen K, Puhakka M, Airaksinen J, Lassen JF, Thuesen L Nordic PCI Study Group. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006;114:1955–1961. doi: 10.1161/CIRCULATIONAHA.106.664920. doi: 10.1161/CIRCULATIONAHA.106.664920. [DOI] [PubMed] [Google Scholar]
- 2.Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, Bennett L, Holmberg S, Cotton JM, Glennon PE, Thomas MR, Maccarthy PA, Baumbach A, Mulvihill NT, Henderson RA, Redwood SR, Starkey IR, Stables RH. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010;121:1235–1243. doi: 10.1161/CIRCULATIONAHA.109.888297. doi: 10.1161/CIRCULATIONAHA.109.888297. [DOI] [PubMed] [Google Scholar]
- 3.Colombo A, Bramucci E, Saccà S, Violini R, Lettieri C, Zanini R, Sheiban I, Paloscia L, Grube E, Schofer J, Bolognese L, Orlandi M, Niccoli G, Latib A, Airoldi F. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) study. Circulation. 2009;119:71–78. doi: 10.1161/CIRCULATIONAHA.108.808402. doi: 10.1161/CIRCULATIONAHA.108.808402. [DOI] [PubMed] [Google Scholar]
- 4.Ferenc M, Gick M, Kienzle RP, Bestehorn HP, Werner KD, Comberg T, Kuebler P, Büttner HJ, Neumann FJ. Randomized trial on routine vs. provisional T-stenting in the treatment of de novo coronary bifurcation lesions. Eur Heart J. 2008;29:2859–2867. doi: 10.1093/eurheartj/ehn455. doi: 10.1093/eurheartj/ehn455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maeng M, Holm NR, Erglis A, Kumsars I, Niemelä M, Kervinen K, Jensen JS, Galløe A, Steigen TK, Wiseth R, Narbute I, Gunnes P, Mannsverk J, Meyerdierks O, Rotevatn S, Nikus K, Vikman S, Ravkilde J, James S, Aarøe J, Ylitalo A, Helqvist S, Sjögren I, Thayssen P, Virtanen K, Puhakka M, Airaksinen J, Christiansen EH, Lassen JF, Thuesen L Nordic-Baltic Percutaneous Coronary Intervention Study Group. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic Bifurcation Study 5-year follow-up results. J Am Coll Cardiol. 2013;62:30–34. doi: 10.1016/j.jacc.2013.04.015. doi: 10.1016/j.jacc.2013.04.015. [DOI] [PubMed] [Google Scholar]
- 6.Chen SL, Sheiban I, Xu B, Jepson N, Paiboon C, Zhang JJ, Ye F, Sansoto T, Kwan TW, Lee M, Han YL, Lv SZ, Wen SY, Zhang Q, Wang HC, Jiang TM, Wang Y, Chen LL, Tian NL, Cao F, Qiu CG, Zhang YJ, Leon MB. Impact of the complexity of bifurcation lesions treated with drug-eluting stents: the DEFINITION study (Definitions and Impact of Complex Bifurcation Lesions on Clinical Outcomes After Percutaneous Coronary Intervention Using Drug-Eluting Stents). JACC Cardiovasc Interv. 2014;7:1266–1276. doi: 10.1016/j.jcin.2014.04.026. doi: 10.1016/j.jcin.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 7.Chen SL, Santoso T, Zhang JJ, Ye F, Xu YW, Fu Q, Kan J, Paiboon C, Zhou Y, Ding SQ, Kwan TW. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (Double Kissing Crush versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions) trial. J Am Coll Cardiol. 2011;57:914–920. doi: 10.1016/j.jacc.2010.10.023. doi: 10.1016/j.jacc.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 8.Medina A, Suárez de Lezo J, Pan M. [A new classification of coronary bifurcation lesions]. Rev Esp Cardiol. 2006;59:183. [PubMed] [Google Scholar]
- 9.Mauri L, Hsieh WH, Massaro JM, Ho KK, D’Agostino R, Cutlip DE. Stent thrombosis in randomized clinical trials of drug-eluting stents. N Engl J Med. 2007;356:1020–1029. doi: 10.1056/NEJMoa067731. doi: 10.1056/NEJMoa067731. [DOI] [PubMed] [Google Scholar]
- 10.Rahman S, Leesar T, Cilingiroglu M, Effat M, Arif I, Helmy T, Leesar MA. Impact of kissing balloon inflation on the main vessel stent volume, area, and symmetry after side-branch dilation in patients with coronary bifurcation lesions: a serial volumetric intravascular ultrasound study. JACC Cardiovasc Interv. 2013;6:923–931. doi: 10.1016/j.jcin.2013.04.019. doi: 10.1016/j.jcin.2013.04.019. [DOI] [PubMed] [Google Scholar]
- 11.Leesar MA, Hakeem A, Azarnoush K, Thuesen L. Coronary bifurcation lesions: present status and future perspectives. Int J Cardiol. 2015;187:48–57. doi: 10.1016/j.ijcard.2015.03.183. doi: 10.1016/j.ijcard.2015.03.183. [DOI] [PubMed] [Google Scholar]
- 12.Chen SL, Ye F, Zhang JJ, Xu T, Tian NL, Liu ZZ, Lin S, Shan SJ, Ge Z, You W, Liu YQ, Qian XS, Li F, Yang S, Kwan TW, Xu B, Stone GW. Randomized comparison of FFR-guided and angiography-guided provisional stenting of true coronary bifurcation lesions: the DKCRUSH-VI trial (Double Kissing Crush Versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions VI). JACC Cardiovasc Interv. 2015;8:536–546. doi: 10.1016/j.jcin.2014.12.221. doi: 10.1016/j.jcin.2014.12.221. [DOI] [PubMed] [Google Scholar]
- 13.Burzotta F, Summaria F, Latib A, De Vita M, Fantoni C, Benedetto S, Turturo M, Larosa C, Manzoli A, Trani C. Prospective multicentre clinical performance evaluation of second and third generation zotarolimus-eluting stents to treat patients with bifurcated coronary lesions. Catheter Cardiovasc Interv. 2016;87:15–22. doi: 10.1002/ccd.25954. doi: 10.1002/ccd.25954. [DOI] [PubMed] [Google Scholar]
- 14.Zhang JJ, Tan H, Ye F, Tan HC, Chen SL. Bench test of bifurcation stenting techniques. J Clin Innov Cardiol. 2016;1:16–22. [Google Scholar]
- 15.Finet G, Derimay F, Motreff P, Guerin P, Pilet P, Ohayon J, Darremont O, Rioufol G. Comparative analysis of sequential proximal optimizing technique versus kissing balloon inflation technique in provisional bifurcation stenting: Fractal Coronary Bifurcation Bench Test. JACC Cardiovasc Interv. 2015;8:1308–1317. doi: 10.1016/j.jcin.2015.05.016. doi: 10.1016/j.jcin.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 16.Mylotte D, Routledge H, Harb T, Garot P, Hovasse T, Benamer H, Unterseeh T, Chevalier B, Morice MC, Louvard Y, Lefèvre T. Provisional side branch-stenting for coronary bifurcation lesions: evidence of improving procedural and clinical outcomes with contemporary techniques. Catheter Cardiovasc Interv. 2013;82:E437–E445. doi: 10.1002/ccd.24901. doi: 10.1002/ccd.24901. [DOI] [PubMed] [Google Scholar]
- 17.Sakata K, Koo BK, Waseda K, Nakatani D, Yock PG, Whitbourn R, Worthley SG, Ormiston J, Webster M, Wilkins GT, Honda Y, Meredith IT, Fitzgerald PJ. A Y-shaped bifurcation-dedicated stent for the treatment of de novo coronary bifurcation lesions: an IVUS analysis from the BRANCH trial. EuroIntervention. 2015;10:e1–e8. doi: 10.4244/EIJY14M08_16. doi: 10.4244/EIJY14M08_16. [DOI] [PubMed] [Google Scholar]
- 18.Kang SJ, Kim WJ, Lee JY, Park DW, Lee SW, Kim YH, Lee CW, Mintz GS, Park SW, Park SJ. Hemodynamic impact of changes in bifurcation geometry after single-stent cross-over technique assessed by intravascular ultrasound and fractional flow reserve. Catheter Cardiovasc Interv. 2013;82:1075–1082. doi: 10.1002/ccd.24956. doi: 10.1002/ccd.24956. [DOI] [PubMed] [Google Scholar]
- 19.Chen SL, Ye F, Zhang JJ, Tian NL, Liu ZZ, Santoso T, Zhou YJ, Jiang TM, Wen SY, Kwan TW. Intravascular ultrasound-guided systematic two-stent techniques for coronary bifurcation lesions and reduced late stent thrombosis. Catheter Cardiovasc Interv. 2013;81:456–463. doi: 10.1002/ccd.24601. doi: 10.1002/ccd.24601. [DOI] [PubMed] [Google Scholar]
- 20.Hahn JY, Chun WJ, Kim JH, Song YB, Oh JH, Koo BK, Rha SW, Yu CW, Park JS, Jeong JO, Choi SH, Choi JH, Jeong MH, Yoon JH, Jang Y, Tahk SJ, Kim HS, Gwon HC. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II registry (Coronary Bifurcation Stenting). J Am Coll Cardiol. 2013;62:1654–1659. doi: 10.1016/j.jacc.2013.07.041. doi: 10.1016/j.jacc.2013.07.041. [DOI] [PubMed] [Google Scholar]
- 21.Costa RA, Feres F, Staico R, Abizaid A, Costa JR, Jr, Siqueira D, Tanajura LF, Damiani LP, Sousa A, Sousa JE, Colombo A. Vessel remodeling and plaque distribution in side branch of complex coronary bifurcation lesions: a grayscale intravascular ultrasound study. Int J Cardiovasc Imaging. 2013;29:1657–1666. doi: 10.1007/s10554-013-0263-1. doi: 10.1007/s10554-013-0263-1. [DOI] [PubMed] [Google Scholar]
- 22.Chen SL, Xu B, Han YL, Sheiban I, Zhang JJ, Ye F, Kwan TW, Paiboon C, Zhou YJ, Lv SZ, Dangas GD, Xu YW, Wen SY, Hong L, Zhang RY, Wang HC, Jiang TM, Wang Y, Chen F, Yuan ZY, Li WM, Leon MB. Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. 2013;61:1482–1488. doi: 10.1016/j.jacc.2013.01.023. doi: 10.1016/j.jacc.2013.01.023. [DOI] [PubMed] [Google Scholar]


