Abstract
High rates of comorbidity are observed between internalizing and externalizing problems, yet the developmental dynamics of comorbid symptom presentations are not yet well understood. This study explored the developmental course of latent profiles of internalizing and externalizing symptoms across kindergarten, 1st, and 2nd grade. The sample consisted of 336 children from an urban, low-income community, selected based on relatively high (61%) or low (39%) aggressive/oppositional behavior problems at school entry (64% male; 70% African American, 20% Hispanic). Teachers reported on children’s symptoms in each year. An exploratory latent profile analysis of children’s scores on aggression/oppositionality, hyperactivity/inattention, anxiety, and social withdrawal symptom factors revealed 4 latent symptom profiles: comorbid (48% of the sample in each year), internalizing (19–23%), externalizing (21–22%), and well-adjusted (7–11%). The developmental course of these symptom profiles was examined using a latent transition analysis, which revealed remarkably high continuity in the comorbid symptom profile (89% from one year to the next) and moderately high continuity in both the internalizing and externalizing profiles (80% and 71%, respectively). Internalizing children had a 20% probability of remitting to the well-adjusted profile by the following year, whereas externalizing children had a 25% probability of transitioning to the comorbid profile. These results are consistent with the hypothesis that a common vulnerability factor contributes to developmentally stable internalizing-externalizing comorbidity, while also suggesting that some children with externalizing symptoms are at risk for subsequently accumulating internalizing symptoms.
Introduction
Statistical models of psychiatric comorbidity have consistently revealed two broad-band factors, internalizing and externalizing, that explain the majority of co-occurrence of psychiatric disorders in adulthood (Carragher, Krueger, Eaton, & Slade, 2015) and of psychiatric symptom manifestations in childhood (Achenbach & Edelbrock, 1978). The externalizing spectrum incorporates a variety of disinhibited or externally-focused behavioral symptoms including aggression, conduct problems, delinquent behavior, oppositionality, hyperactivity, and attention problems, whereas the internalizing spectrum includes a variety of over-inhibited or internally-focused symptoms including anxiety, fear, sadness/depression, social withdrawal, and somatic complaints. Despite the apparent distinctiveness between these domains, most studies of children find them to be positively correlated with one another (Bird, Gould, & Staghezza, 1993; Caron & Rutter, 1991). Because much of the epidemiological research presents only a cross-sectional view of the prevalence of child psychopathology, it is not clear how comorbidity develops over time. It is possible that comorbidity between externalizing and internalizing domains increases probabilistically over time, as initial symptoms become risk factors for the development of additional symptoms from the other domain (i.e., accumulation). Alternatively, it is possible that psychopathology is less differentiated in younger children, such that children may exhibit symptoms from both domains initially that, over time, crystallize into more “pure” internalizing or externalizing presentations in response to environmental contingencies that shape symptom manifestation (i.e., differentiation). Finally, it is possible that comorbidity is stable over time, reflecting the influence of a common underlying trait that increases vulnerability to both domains of psychopathology across the lifespan. In this study, we examine if and how children’s profiles of psychopathology change across the first 3 years of school.
Theoretical Perspectives on Comorbidity
The predominance of comorbidity has been a major concern in clinical science. One of the primary debates is whether the co-occurrence between different syndromes is appropriately termed “comorbidity,” in the medical application of this term (Lilienfeld, Waldman, & Israel, 1994). Comorbidity refers to the presence of two independent syndromes, which implies that the probability of comorbidity should equal the product of the probabilities of each individual disorder. Data, however, clearly demonstrate that rates of comorbidity between internalizing and externalizing disorders far exceed the rate that would be predicted based on chance co-occurrence of independent syndromes, suggesting that some mechanism must underlie the phenomenon of comorbidity (Beauchaine & McNulty, 2013; Caron & Rutter, 1991).
One of the primary hypotheses put forward is that a common trait imparts vulnerability for symptoms in both domains (Weiss, Süsser, & Catron, 1998). Behavioral genetics models have suggested that a substantial portion of the correlation between externalizing and internalizing disorders is accounted for by a common genetic component (Cosgrove et al., 2011; Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011). This common genetic liability appears to be at least partially mediated by trait negative affectivity (Mikolajewski, Allan, Hart, Lonigan, & Taylor, 2013; Rhee, Lahey, & Waldman, 2015; Schmitz et al., 1999; Tackett et al., 2013), which is mediated at the neural level by hyperactivation of the threat-response system (Whittle, Allen, Lubman, & Yücel, 2006). Additionally, deficient prefrontal control over limbic system activity contributes to emotion dysregulation and risk for both internalizing and externalizing psychopathology (Beauchaine, 2015). Finally, blunted responsivity of the mesolimbic reward system, which contributes to low positive affectivity and lack of motivation, is another potential common vulnerability factor for externalizing and internalizing psychopathology, particularly depression (Andrews et al., 2011; Brenner & Beauchaine, 2011; Forbes & Dahl, 2005). If a common vulnerability factor underlies both externalizing and internalizing symptoms, comorbidity is more likely to manifest earlier and evidence relative stability over time, as the vulnerability trait arguably confers risk for both conditions simultaneously, and maintains risk across development.
Other theories have posited that comorbidity arises when the symptoms of one disorder increase the risk for the development of another (Caron & Rutter, 1991). With regard to internalizing-externalizing comorbidity, there is substantial empirical evidence suggesting that children initially presenting with externalizing symptoms are at greater risk for later developing internalizing symptoms, which may emerge in response to adverse consequences of externalizing behaviors such as rejection by peers, academic difficulties, or other stressful life experiences (Burke, Loeber, Lahey, & Rathouz, 2005; Gooren, van Lier, Stegge, Terwogt, & Koot, 2011; Ladd & Troop-Gordon, 2003; Nobile et al., 2013; van Lier & Koot, 2010). In contrast, there is less evidence to suggest that the presence of internalizing symptoms imparts a risk for the emergence of externalizing symptoms (Gilliom & Shaw, 2004; Keiley, Bates, Dodge, & Pettit, 2000). If comorbidity is sequential, it is likely to follow a pattern of symptom accumulation whereby children with “pure” symptom profiles are at greater risk for developing comorbid symptoms over time, a pattern which may be more likely to occur among those initially presenting with externalizing symptoms.
An alternative possibility is that children are more likely than adults to express undifferentiated symptoms of distress that can manifest as symptoms of both externalizing and internalizing domains. Risk for psychopathology that arises from core dispositional traits may differentiate into specific symptom profiles over time through transactional shaping from environmental input (Lahey & Waldman, 2007). Over time, generalized distress may become refined into more “pure” symptom presentations, particularly in response to specific peer or parenting influences that reinforce certain behavioral patterns over others. For example, young children may manifest psychological distress as undifferentiated irritability, which can include symptoms such as temper tantrums, crying, and aggression. Chronic irritability in preschool-aged children has been shown to predict the later onset of both internalizing and externalizing disorders (Dougherty et al., 2015). This perspective of differentiation suggests that comorbidity will be higher among younger children, but will decrease over time as children develop more nuanced emotional reactions and behavioral responses, thus diverging into either an externalizing or internalizing profile.
Defining Comorbidity
One of the primary issues in the study of comorbidity is how best to define its existence. Many studies rely on pre-specified cutoffs on dimensional internalizing and externalizing symptom scales that reflect the threshold at which diagnostic “caseness” is met. In studies of comorbidity, this typically involves identifying children who are above the cutoff on both scales. However, children above the cutoff on one scale but below the cutoff on the other scale are often classified as displaying “pure” internalizing or externalizing disorders, regardless of whether their subthreshold scores reflect meaningful symptom elevation in the other domain. This is especially troubling from a developmental perspective because a restricted focus on children whose symptoms meet or exceed a diagnostic threshold may fail to capture important processes in children who may be on the verge of crossing the clinical threshold in the coming years. This approach also compromises the ability to identify factors that protect or divert high-risk (i.e. subthreshold) children from arriving at a diagnostic outcome.
Maximizing the value of continuous symptom severity can be achieved using latent profile analysis (LPA), a person-centered, multivariate analysis technique for identifying groups of individuals with similar patterns of symptom scores across measures (Collins & Lanza, 2010). This technique is similar in concept to cluster analysis, however, it differs importantly in statistical approach and underlying assumptions. Most importantly, in LPA the grouping variable is latent and individuals have a probability of membership in each latent profile based on their values on the array of indicators. In cluster analysis, individuals are assigned exclusively to one group with which they are deemed to be most similar (DiStefano & Kamphaus, 2006). Thus, in LPA, uncertainty in group assignment is explicitly modeled as measurement error (Collins & Lanza, 2010); by contrast, in cluster analysis, individuals whose profiles do not adequately match any group must either be assigned to a poorly-matched group, thus reducing cluster homogeneity, or be excluded from the analysis sample in order to maintain cluster homogeneity (Edelbrock & Achenbach, 1980).
LPA may be used in an exploratory fashion to reveal profiles of scores within the sample, potentially revealing important profiles that may not have been hypothesized a priori. By capitalizing on information available both across domains (i.e., relative magnitude of scores across a set of indicators) and within the continuum of severity (i.e., absolute magnitude of scores on some or all indicators), this technique facilitates the study of different patterns of comorbidity. For example, LPA may differentiate children with moderate internalizing from those with more severe internalizing symptoms, or identify 2 groups of children equally high in externalizing that are differentiated by their internalizing symptoms. This approach may also reveal whether specific symptoms within the internalizing and externalizing domains are more or less likely to be present in a comorbid symptom profile. For instance, internalizing-externalizing comorbidity may be characterized by high social withdrawal but lower anxiety.
It is important to note that an exploratory LPA reveals the latent groups that best represent a specific sample, and may lack the presumed generalizability of nationally-normed threshold techniques. However, whether developmental patterns of psychopathology are truly generalizable remains poorly understood, and the assessment of sample-specific profiles across a diverse range of samples is important (see Gatzke-Kopp, 2016). By providing characterizations of the development of psychopathology across a range of racially and socioeconomically diverse samples, assumptions of generalizability can ultimately be empirically tested. In examining the literature to date, it is apparent that many latent profiles do replicate across samples, with some key differences emerging as well.
Studies using cluster analysis or latent class analysis to characterize patterns of emotional-behavioral problems spanning the internalizing and externalizing domains have been conducted within large, nationally-representative samples of elementary school-aged children (Basten et al., 2013; Kamphaus et al., 1999; Kamphaus, Huberty, DiStefano, & Petoskey, 1997), samples characterized by high levels of poverty (Bulotsky-Shearer, Fantuzzo, & McDermott, 2010; Tolan & Henry, 1996) and samples of children drawn from clinical treatment centers (Edelbrock & Achenbach, 1980; Frankel, Hanna, Cantwell, Shekim, & Ornitz, 1992). Notably, all of these studies identified at least one class of children exhibiting co-occurring internalizing and externalizing symptoms (Basten et al., 2013; Bulotsky-Shearer et al., 2010; Edelbrock & Achenbach, 1980; Frankel et al., 1992; Kamphaus et al., 1999, 1997; Tolan & Henry, 1996). For many studies, the comorbid group was not only characterized by elevated levels across all internalizing and externalizing syndromes, but also by the degree of symptom severity, even relative to other psychopathology groups (Basten et al., 2013; Frankel et al., 1992; Kamphaus et al., 1999, 1997).
Somewhat surprisingly, several studies failed to identify a group of children exhibiting high levels of externalizing symptoms only. In most cases, the typical comorbid group (with high levels of both externalizing and internalizing symptoms) emerged as a separate class from children characterized by high externalizing symptoms and moderate elevations in at least a subset of internalizing symptoms (Basten et al., 2013; Bulotsky-Shearer et al., 2010; Frankel et al., 1992; Kamphaus et al., 1999, 1997). This pattern again highlights the value of examining the full spectrum of symptom expression rather than relying on arbitrary thresholds. With this approach, it becomes evident that individuals who may be classified as externalizing-only from a diagnostic perspective still evidence meaningful elevations in internalizing symptoms. These findings indicate that comorbidity may even be more prevalent than previously thought, if subthreshold symptom elevations are considered.
Although these studies found a tendency for children with externalizing symptoms to have elevation in at least one domain of internalizing symptoms, the studies were inconsistent in their findings about which internalizing symptoms were most likely to be elevated in this predominantly externalizing class. Basten and colleagues (2013) found that the externalizing group demonstrated elevated levels of social withdrawal but low levels of anxious and depressed symptoms. In contrast, another large-scale study within a U.S. nationally-representative sample that incorporated both parent- and teacher-rated scores found that the externalizing behavior problems were more likely to be comorbid with symptoms of depression than with social withdrawal or anxiety (Kamphaus et al., 1999, 1997). Other studies, however, reported moderate levels of both anxious/depressed and social withdrawal symptoms in their externalizing group, differing from the comorbid group only in severity (Bulotsky-Shearer et al., 2010; Frankel et al., 1992). These findings indicate that it may be important to examine which particular internalizing symptoms are most likely to co-occur with externalizing symptoms.
Importantly, a small number of studies did identify a class of children characterized by high levels of externalizing symptoms and low levels of internalizing symptoms (Edelbrock & Achenbach, 1980; McDermott & Weiss, 1995; Tolan & Henry, 1996). Among a large community sample of urban poor children, a class characterized by clinical-level externalizing severity and low internalizing symptoms consisted of 6% of the sample (Tolan & Henry, 1996). Membership in this class was related to residence in neighborhoods with a higher density of household poverty, whereas poverty density was not related to membership in the comorbid aggressive-anxious/depressed class. Thus, the inconsistency with which studies have identified an externalizing-only class may be a function of the demographic nature of the sample under study. However, since these authors dichotomized the CBCL scale scores according to whether or not the score fell above the recommended cutoff for clinical significance, it is still possible that the children in this externalizing-only class might have shown elevated but subthreshold levels of anxiety/depression or withdrawal.
Finally, most studies have consistently identified a class of children with high levels of internalizing symptoms including depression, anxiety, and social withdrawal, and with low levels of externalizing symptoms (Basten et al., 2013; Bulotsky-Shearer et al., 2010; Edelbrock & Achenbach, 1980; Kamphaus et al., 1999). This class tended to be more clearly delineated among studies incorporating parent versus teacher ratings, which is consistent with the nature of internalizing symptoms, which may be more difficult for a teacher to detect.
Developmental Perspective on Comorbidity
To date, the majority of research on comorbid symptom profiles has been conducted cross-sectionally. Although studies have been conducted spanning the full range of childhood, little research has examined if/how individuals transition in symptom profiles over time. In the present study, children were first assessed in kindergarten, and followed annually through 2nd grade. Kindergarten represents a valuable starting point because it reflects an age in the earliest phase of reliable symptom identification, as many rating scales are designed to assess children older than age 4. Assessing children at the school age also enables the use of teacher-reported symptoms, which may be beneficial as teachers have extensive experience with same-aged children and are more likely to rate a child in reference to an appropriate comparison group than parents. This developmental step also marks the introduction of new cognitive, social and regulatory demands on children, creating a backdrop of normative development against which pathological symptoms are more readily apparent. Finally, the ongoing affective and cognitive changes underway, as well as the expanding environmental contexts (e.g., the unselected peer group) create the setting for dynamic developmental changes across these years.
In order to gain insight into the developmental course of emotional and behavioral symptoms, it is important to move beyond the characterization of static symptom profiles to study continuity and discontinuity of symptoms over time (Beauchaine & McNulty, 2013; Sroufe, 1997). This goal is met by latent transition analysis (LTA), which is a longitudinal extension of LCA that models the conditional probabilities of latent class membership at a later time point, given class membership at the earlier time point (Collins & Lanza, 2010; Collins & Wugalter, 1992). When emotional and behavioral symptoms are used to define the classes, this method reveals the likelihood that children exhibiting a particular pattern of symptoms at one time point will exhibit a similar pattern of symptoms at a later time point (continuity), as well as the likelihood that they will transition to exhibiting any of the other empirically-identified symptom patterns at the later time point (discontinuity).
Little research has been conducted longitudinally to assess developmental continuity and discontinuity in empirically-identified profiles or clusters of symptoms. Only one of the studies described above conducted a follow up of the participants examined in the initial cross-sectional study (Tolan & Henry, 1996). From the initial study of children in 1st – 6th grade, these researchers re-assessed a subset of the 1st-, 2nd-, and 4th-grade samples two years later (n = 946) in order to test for classification stability. Not surprisingly, 83% of the subsample was in the low probability of clinical-level problems class at both time points, indicating a high level of stability among typically developing children. Among children classified with a clinical diagnosis initially, however, only between 21 and 63 percent of children remained in these same classes at the second time point, indicating at least a moderate degree of change in symptom class over time. Unfortunately, the authors did not elaborate on which classes had the highest or lowest stability, nor did they provide the transition probabilities between specific classes. Furthermore, this study utilized clinical threshold classifications, making it difficult to determine whether subthreshold symptoms at earlier time points contributed to the probability of changing symptom classification.
Present Study
The present study builds on the sparse pre-existing literature on continuity and discontinuity of childhood emotional-behavioral symptom profiles spanning both externalizing and internalizing symptom domains. LTA (Collins & Lanza, 2010; Collins & Wugalter, 1992) was used to quantify the probabilities of transitioning between latent profiles of psychopathology in a sample of high-risk children, 61% of whom were selected based on early-onset aggressive behaviors. Children were assessed by teacher report in kindergarten, 1st, and 2nd grade. Because aggression has been shown to be associated with higher levels of internalizing and externalizing, this sample is well suited to the study of comorbidity. Symptom profiles were based on multiple externalizing (aggression/oppositionality and hyperactivity/inattention) and internalizing (anxiety and social withdrawal) factors in order to examine whether comorbidity is more likely to occur between specific syndromes within the broader internalizing and externalizing domains.
We hypothesized that continuity would be high among children exhibiting a low-symptom profile initially, since these children’s behaviors should be reinforced by socialization practices in the classroom and at home. We also expected that children exhibiting a comorbid profile would show high continuity over time, with a particularly low probability of transitioning to a low-symptom profile, since internalizing-externalizing comorbidity has been associated with severe and chronic behavior problems (Ialongo, Edelsohn, Werthamer-Larsson, Crockett, & Kellam, 1996; Sourander et al., 2007). We hypothesized that children with an externalizing profile would be at increased risk of developing comorbid internalizing symptoms, reflecting the symptom accumulation hypothesis reviewed above. Finally, we expected that children exhibiting an internalizing profile would be most likely to transition toward a low-symptom profile, reflecting a positive adjustment to school.
Following the developmental models of comorbidity described above, we propose that the shared latent vulnerability model would be supported by a pattern of relatively high stability in a comorbid symptom profile across time with few transitions into the comorbid profile between years, whereas the undifferentiated distress model would be supported by a reduction in the relative size of the comorbidity group across the three years with a moderate probability of children transitioning from the comorbid profile toward more clearly delineated externalizing and internalizing symptom profiles. Finally, the accumulation model would be supported by higher transition probabilities from individual symptom groups toward a comorbid group across time, although this is predicted to be more likely to occur among those with initial externalizing presentations.
Methods
Participants
The sample consists of children who participated in the PATHS to Success study, which included a randomized controlled trial of a multi-component preventive intervention targeting kindergarten children with early-onset aggressive/oppositional behaviors, as well as a developmental study of a comparison group of children with relatively low levels of aggressive/oppositional behaviors. All children were recruited from elementary schools within a single urban school district in central Pennsylvania. More details regarding recruitment can be found in Gatzke-Kopp et al. (2012). Briefly, at the beginning of the school year in 2008 (Cohort I) and 2009 (Cohort II), all kindergarten teachers completed a 10-item aggressive/oppositional behavior screening questionnaire for each child in their class. For purposes of the intervention, 207 children who had screened in the upper quartile of aggressive/oppositional behaviors within their classroom were enrolled in the study, 100 of whom were randomly assigned to the experimental condition. Children in the experimental group participated in weekly “friendship groups” along with a rotating selection of peers. These sessions took place during the second half of the kindergarten school year and the first half of the 1st-grade school year. In addition, parents of children in the experimental group received home visits by a trained parenting coach approximately once per month during this same period. Additionally, 132 comparison children who scored in the lowest quartile on the screening instrument were selected to be matched with children in the high-aggression groups on sex and classroom. For the present study, all available participants are included in the analysis sample in order to maximize sample size, which impacts the reliability of the latent class and latent transition analysis solutions (Yang, 2006). The full study sample thus consists of 339 children, 61% of whom displayed elevated aggressive/oppositional behaviors relative to their classmates at study entry. The analyses were conducted on the 336 children with teacher survey data in any year (see below). Parents provided informed consent and children gave verbal assent for all study procedures. The study procedures were approved by the Pennsylvania State University Internal Review Board.
Sixty-four percent of the children in the sample were male. Consistent with the demographics of the region, 70% of the children were African American, 20% were Hispanic or Latino, 9% were Caucasian, and 1% were Asian. The average age at initial screening was 5.6 years (SD = .35, range = 5.0 – 7.0). Sample children lived in a community with very low socioeconomic resources; 79% of students in the district were classified as low-income (qualifying for free or reduced-price school meals), the majority of households were headed by a single mother (69%), and 79% of parents were estimated to have no more than a high school education. Regional statistics indicated that property crimes were twice as high and violent crimes were 4.5 times as high as comparable statistics for the entire state.
Measures
Teacher Ratings
Teachers were asked to complete questionnaires regarding each participating child in the winter of the child’s kindergarten school year and in the spring of the child’s 1st- and 2nd-grade years. Teachers who returned their questionnaires received a $15 gift card as compensation for their time. Teacher surveys were completed for 301 children (89% of the sample) in kindergarten, 272 children (80%) in 1st grade, and 240 children (71%) in 2nd grade. One hundred and ninety-two children (57% of the sample) had teacher questionnaire data across all three school years, while another 93 children had data from all but one year. Only three children had no teacher questionnaire data from any school year. Participating children were equally distributed across classrooms such that all teachers had both high- and low-aggression risk children, as well as children in the experimental and control groups. When teachers declined to complete questionnaires, they did so unilaterally for all participants, and thus there is no built-in selection bias for missing teacher reports.
The present analyses utilized teacher reports of children’s externalizing symptoms, including aggressive/oppositional and hyperactive/inattentive behaviors, and internalizing symptoms, including anxiety, emotional distress, and social withdrawal. Since each of these constructs was measured across multiple survey scales (described below), an exploratory factor analysis was conducted on the individual scale items (29 in total) to identify cohesive dimensions of behavior across all survey items. These factor scores were then entered as indicators in the latent profile analysis.
Strengths and Difficulties Questionnaire (SDQ)
Teachers responded to four behavior-problem subscales from Goodman’s (1997) SDQ: emotional symptoms, conduct problems, hyperactivity/inattention, and peer problems. Each subscale includes 5 items rated on a 3-point scale from 0 (not true) to 2 (certainly true). The emotional symptoms subscale includes items assessing worry and fearfulness (e.g., “Many worries or often seems worried”), somatic complaints (“Often complains of headaches, stomach-aches or sickness”), and emotional distress (“Often unhappy, depressed, or tearful”). The conduct problems subscale assesses aggression (“Often fights with other children or bullies them”), oppositionality (e.g., “Generally well behaved, usually does what adults request”), and antisocial behaviors (e.g., “Often lies or cheats”). The hyperactivity/inattention subscale assesses hyperactivity (e.g., “Constantly fidgeting or squirming”), impulsivity (e.g., “Thinks things out before acting”), and concentration problems (e.g., “Easily distracted, concentration wanders”). The peer problems subscale assesses the quality of children’s relationships with their peers, including social withdrawal (“Rather solitary, prefers to play alone”), peer acceptance (e.g., “Generally liked by other children”), and victimization (“Picked on or bullied by other children”). The exploratory factor analysis includes all items from the emotional symptoms, conduct problems, and hyperactivity/inattention SDQ subscales, as well as the single item assessing social withdrawal from the peer problems subscale. These items are supplemented by additional items assessing aggression/oppositionality and internalizing symptoms, particularly social withdrawal, drawn from other survey subscales (described below).
Although the SDQ subscale scores were not utilized in the exploratory factor analysis or in the subsequent latent profile analysis, the means and ranges for these scores at each assessment are presented in Table 1 in order to provide insight into the level and range of behavior problems exhibited by children in the analysis sample. Sample means suggested moderate symptom elevations on average, with particularly high mean levels of hyperactivity/inattention, and relatively high standard deviations indicated a substantial amount of heterogeneity in symptom levels. Symptom scores ranged across the full spectrum of severity on both the conduct problems and hyperactivity subscales in all 3 years. Scores on the peer problems and emotional symptoms scales had a maximum of 9 or 10, out of 10 possible points, in each year.
Table 1.
Characteristics of the analysis sample in all years.
| Kindergarten
|
1st Grade
|
2nd Grade
|
||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | |
| Age | 6.1 (0.4) | 5.4 – 7.5 | 7.2 (0.4) | 6.6 – 8.6 | 8.2 (0.3) | 7.5 – 9.3 |
| SDQ Subscale Scores | ||||||
| Emotional Symptoms | 1.9 (2.3) | 0 – 10 | 1.4 (1.9) | 0 – 10 | 1.5 (2.0) | 0 – 9 |
| Conduct Problems | 2.5 (2.8) | 0 – 10 | 2.7 (2.9) | 0 – 10 | 2.7 (2.8) | 0 – 10 |
| Hyperactivity/Inattention | 4.6 (3.3) | 0 – 10 | 4.4 (3.5) | 0 – 10 | 4.2 (3.3) | 0 – 10 |
| Peer Problems | 1.8 (1.9) | 0 – 9 | 1.7 (1.8) | 0 – 9 | 2.0 (2.0) | 0 – 9 |
| CBQ Subscale Scores | ||||||
| Aggressive/Oppositional | 2.4 (1.2) | 1 – 5.7 | 2.2 (1.2) | 1 – 5.7 | 2.3 (1.2) | 1 – 6.0 |
| Internalizing | 2.3 (0.9) | 1 – 5.5 | 2.2 (0.8) | 1 – 4.8 | 2.3 (0.9) | 1 – 5.2 |
Note. SDQ = Strengths and Difficulties Questionnaire. CBQ = Child Behavior Questionnaire (items compiled for the present study). The SDQ subscales have possible score range of 0 – 10. The CBQ subscales have a possible score range of 1 – 6.
Child Behavior Questionnaire (CBQ)
In addition to the SDQ, teachers completed a second behavior questionnaire with many similarly targeted items compiled for the present study. An aggression/oppositionality scale was created using seven items assessing children’s physical aggression (e.g., “Hits, pushes, or shoves”), verbal aggression (e.g., “Yells at others”), and oppositionality (e.g., “Ignores or refuses to obey adults”) drawn from the Teacher Observation of Classroom Adaptation – Revised (TOCA-R; Werthamer-Larsson, Kellam, & Wheeler, 1991). An internalizing scale was created using six items assessing children’s socially withdrawn behaviors (e.g., “Avoids playing with other children”) and internalizing symptoms (e.g., “Sad, unhappy”) drawn from an internalizing/withdrawn scale compiled for the Head Start REDI Project (http://headstartredi.ssri.psu.edu/). All items were rated on a 6-point scale from 1 (almost never) to 6 (almost always) and scale scores were computed as the average across items.
Sample means and ranges for each year on the CBQ scales are also reported in Table 1. Means were very similar on both the aggression and internalizing scales and reflected moderately elevated symptoms. The range of observed scores on the aggression scale nearly covered the entire possible range of scores in each year, indicating that the sample reflects a very wide range of symptom severity. Maximum scores on the internalizing scales were slightly lower, ranging from 4.8 – 5.7 (out of a maximum possible score of 6) across years.
Results
Factor analyses
As a preliminary step, exploratory factor analyses were conducted on the 29 symptom items separately for each grade level to determine the number of factors that optimally account for the pattern of correlations among the teacher survey items. All factor analyses were conducted in Mplus 7.3 on the polychoric correlation matrix of survey items, modeling the full range of observed response categories for each variable, with pairwise deletion of missing data. Two items that exhibited substantial cross-loadings on two or more factors were removed from the analyses, yielding 27 total items contributing to the factor solutions. The appropriate number of factors to retain in each grade level was assessed using parallel analysis (Horn, 1965) and Velicer’s minimum average partial (MAP) test (Velicer, 1976) as implemented in the R psych package by William Revelle (http://personality-project.org/r/psych/). These statistics generally pointed towards a 4-factor solution in all grade levels. In each grade level, these 4 factors could be clearly interpreted as aggression/oppositionality, hyperactivity/inattention, anxiety, and withdrawal.
In order to test the measurement invariance of the 4-factor solution across grade levels, an exploratory structural equation model (ESEM; Asparouhov & Muthén, 2009; Marsh, Morin, Parker, & Kaur, 2014) was fit in Mplus in which four factors were freely estimated for each grade level simultaneously. This method essentially embeds multiple sets of exploratory factor analyses within a single structural equation model. Unlike a traditional confirmatory factor analysis approach in which items are constrained to have zero loadings on the non-hypothesized factors, in ESEM item cross-loadings are freely estimated within the specified sets of factors, allowing for a closer fit of the model to the data (Marsh et al., 2014). Furthermore, within ESEM parameter constraints may be imposed to test hypotheses such as measurement invariance, which is not possible in a traditional EFA.
For the ESEM model, the 27 ordinal survey items were entered in three grade-level blocks with four factors being freely estimated for each block of items, thus yielding three sets of four factors each. The model was conducted on the polychoric correlation matrix including all children with data in any year (n = 336). The model was estimated using WLSMV and the resulting factors were rotated using the CF-varimax rotation algorithm (the factor solution using the oblimin rotation algorithm was very similar). Items were allowed to cross-load on all factors within a grade-level set, but item loadings on factors outside the grade-level set were fixed to 0 and no residual correlations were estimated between items within or across grade levels.
In the baseline model, the factor loadings and item thresholds were freely estimated across grade levels, and factor correlations were freely estimated among all 12 factors both within and across grade levels. For model identification purposes, all latent factors and the latent item response variables were standardized to a mean of 0 and standard deviation of 1. The fit of this model was compared to that of a model in which all factor loadings and item response thresholds were constrained to be invariant across grade levels, and the factor variances were fixed to 1 in kindergarten and freely estimated in 1st and 2nd grade. The means of the factors and the means and variances of the latent item response variables remained fixed in all grade levels. A model with invariant factor loadings and freely estimated item thresholds was not examined since the latent item response probability curve is jointly determined by these two parameters (L. K. Muthén & Muthén, 2012, p. 485), and thus both loading and threshold invariance are required if the factors are to be interpreted as reflecting the same construct over time (Marsh et al., 2014; B. Muthén & Asparouhov, 2002). In contrast, invariance of the item residuals over time is not necessary for common interpretation of the underlying factor scores (Marsh et al., 2014), and thus the fit of a model in which the residuals are held invariant over time was not examined.
The fit statistics for the baseline model and the loading- and threshold-invariant model are reported in Table 2. Although the χ2 test indicated that neither model fit the data exactly, the RMSEA, CFI, and TLI fit statistics all indicated that both models provided a close approximation of the data (RMSEAs ≤ .02, CFIs > .98, TLIs > .98). Additionally, although the χ2 test of change in model fit was statistically significant, the magnitude of change in the model fit statistics from the baseline to the measurement-invariant model was very small (ΔRMSEA = 0.002, ΔCFI = −0.004, ΔTLI = −0.003). The χ2 difference test is known to be overly sensitive to minor model misfit in large samples, and therefore it has been suggested that fit statistics assessing the degree of closeness of the model’s fit, such as RMSEA and CFI, provide more practically useful information (Browne & Cudeck, 1992; Cheung & Rensvold, 2002). Cheung and Rensvold (2002) suggest that it is reasonable to impose measurement invariance if the ΔCFI between the baseline and measurement-invariant model is less than or equal to −0.01, which was indeed the case in the present comparison. Accordingly, the loading- and threshold-invariant model was accepted as providing an acceptable fit to the data.
Table 2.
Fit statistics for the baseline and measurement-invariant exploratory structural equation models for the factor structure across all three years.
| # Free Parameters | χ2 | df | p | p-diff | RMSEA (95% CI) | CFI | TLI | |
|---|---|---|---|---|---|---|---|---|
| Baseline model | 624 | 3205.4 | 2886 | 0.00 | .018 (.014, .022) | .992 | .991 | |
| Measurement-invariant model | 260 | 3698.4 | 3250 | 0.00 | 0.00 | .020 (.017, .023) | .988 | .988 |
Notes. In the baseline model, all factor loadings and item thresholds were freely estimated, and factor variances were fixed to 1 for model identification purposes. In the measurement-invariant model, all factor loadings and item thresholds were constrained to be equal over time, and the factor variances were fixed to 1 in kindergarten and freely estimated in 1st and 2nd grade. χ2 = model chi-squared test statistic for goodness of fit; df = error degrees of freedom; p = probability value of the χ2 test statistic; p-diff = p-value of the χ2 difference between the baseline and measurement-invariant models; RMSEA = Root Mean Square Error of Approximation; CFI = Comparative Fit Index; TLI = Tucker-Lewis Fit Index.
The factor loadings for the loading- and threshold-invariant model are provided in Table 3. The results replicated the overall factor structure that emerged from the within-grade EFAs, with clearly interpretable factors measuring the behavioral dimensions of aggression/oppositionality, hyperactivity/inattention, anxiety, and withdrawal. Item cross-loadings on non-primary factors were generally below 0.4, with the exception of the item assessing the child’s attention span, which loaded primarily on the hyperactivity/inattention factor (λ = −0.748) with a moderate cross-loading on the withdrawal factor (λ = −0.419).
Table 3.
Factor loadings.
| AGG | HYP | ANX | WITH | |
|---|---|---|---|---|
| Loses temper | 0.805 | 0.098 | 0.057 | 0.099 |
| Fights or bullies other children | 0.927 | 0.039 | 0.127 | −0.083 |
| Lies or cheats | 0.638 | 0.294 | 0.208 | −0.080 |
| Steals | 0.575 | 0.163 | 0.291 | −0.232 |
| Breaks things on purpose | 0.537 | 0.358 | −0.065 | 0.168 |
| Stubborn | 0.668 | 0.178 | −0.054 | 0.241 |
| Yells at others | 0.778 | 0.126 | −0.027 | 0.069 |
| Breaks rules | 0.636 | 0.356 | 0.022 | 0.112 |
| Fights with other children | 0.829 | 0.082 | 0.115 | 0.038 |
| Disobeys adults | 0.651 | 0.277 | −0.026 | 0.243 |
| Hits, pushes | 0.701 | 0.226 | 0.011 | 0.074 |
| Restless/overactive | 0.094 | 0.941 | 0.096 | −0.174 |
| Fidgets | 0.061 | 0.916 | 0.197 | −0.218 |
| Easily distracted | −0.056 | 0.884 | 0.011 | 0.245 |
| Thinks before acting | −0.308 | −0.515 | 0.049 | −0.267 |
| Good attention span | 0.003 | −0.748 | 0.127 | −0.419 |
| Acts young | 0.081 | 0.538 | 0.051 | 0.334 |
| Somatic complaints | 0.225 | 0.013 | 0.464 | 0.034 |
| Worries | 0.077 | −0.099 | 0.810 | 0.098 |
| Unhappy, tearful | 0.355 | 0.005 | 0.490 | 0.345 |
| Nervous, clingy | −0.166 | 0.230 | 0.714 | 0.158 |
| Fearful | −0.095 | 0.059 | 0.893 | 0.088 |
| Prefers to play alone | −0.110 | −0.011 | 0.276 | 0.737 |
| Invites others to play | −0.207 | −0.090 | −0.073 | −0.638 |
| Low energy | −0.104 | −0.033 | 0.218 | 0.677 |
| Keeps to self, withdraws | −0.070 | −0.109 | 0.366 | 0.724 |
| Avoids playing with others | 0.216 | −0.046 | 0.298 | 0.481 |
Notes. Item-factor loadings > 0.400 are in bold text. AGG = aggression/oppositionality; HYP = hyperactivity/inattention; ANX = anxiety; WITH = withdrawal.
Factor scores were calculated from the latent factor model using Mplus. Although factor scores fail to account for measurement error in the factor model, they are generally preferable to simple scale scores because they more closely approximate the dimensions of behavior represented by the latent factors (Marsh et al., 2014). In order to reduce the degree of uncertainty and bias in the estimated factor scores when used as independent variables in the latent profile analyses, factor scores were dropped if over half of the items with a loading of 0.6 or higher on that factor were missing.
Univariate statistics for these factor scores are provided in Table 4, and the correlations among factor scores are provided in Table 5. Within years, all factor scores tended to be positively correlated (suggesting the presence of a general behavior-problems factor), although the highest correlations were found between the aggression/oppositionality and hyperactivity/inattention factors (r’s = .55 –.65) and between the anxiety and withdrawal factors (r’s = .47-.59). Across years, there was moderately high stability in children’s aggression (kindergarten to 1st grade: r = .68; 1st to 2nd grade: r = .77) and hyperactivity/inattention (kindergarten to 1st grade: r = .71; 1st to 2nd grade: r = .82). Relatively lower cross-year stability was observed for children’s anxiety (kindergarten to 1st grade: r = .36; 1st to 2nd grade: r = .50) and withdrawal (kindergarten to 1st grade: r = .53; 1st to 2nd grade: r = .56).
Table 4.
Univariate statistics for factor scores.
| n | Mean | SD | Min | Max | Skewness | Kurtosis | |
|---|---|---|---|---|---|---|---|
| Kindergarten | |||||||
| AGG | 300 | −0.017 | 0.905 | −1.80 | 2.02 | 0.15 | −0.60 |
| HYP | 299 | 0.062 | 0.834 | −1.84 | 1.96 | −0.07 | −0.63 |
| ANX | 299 | 0.210 | 0.820 | −1.48 | 2.59 | 0.38 | −0.29 |
| WITH | 300 | 0.058 | 0.832 | −1.80 | 2.65 | 0.12 | −0.12 |
| 1st Grade | |||||||
| AGG | 271 | −0.009 | 0.960 | −2.02 | 2.32 | 0.07 | −0.66 |
| HYP | 271 | −0.007 | 0.865 | −2.16 | 1.80 | 0.03 | −0.70 |
| ANX | 270 | −0.026 | 0.789 | −1.84 | 2.19 | 0.38 | −0.57 |
| WITH | 271 | −0.084 | 0.726 | −1.60 | 2.75 | 0.32 | 0.10 |
| 2nd Grade | |||||||
| AGG | 238 | 0.004 | 0.995 | −1.98 | 2.63 | 0.12 | −0.55 |
| HYP | 239 | −0.032 | 0.869 | −1.93 | 2.18 | 0.09 | −0.51 |
| ANX | 239 | 0.022 | 0.750 | −1.68 | 2.09 | 0.31 | −0.17 |
| WITH | 237 | 0.048 | 0.854 | −1.91 | 2.76 | 0.16 | −0.20 |
Notes. AGG = aggression/oppositionality; HYP = hyperactivity/inattention; ANX = anxiety; WITH = withdrawal.
Table 5.
Correlations among factor scores.
| Kindergarten | 1st Grade | 2nd Grade | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| AGG | HYP | ANX | WITH | AGG | HYP | ANX | WITH | AGG | HYP | ANX | WITH | |
| Kindergarten | ||||||||||||
| AGG | --- | |||||||||||
| HYP | 0.60 | --- | ||||||||||
| ANX | 0.22 | 0.23 | --- | |||||||||
| WITH | 0.25 | 0.31 | 0.59 | --- | ||||||||
| 1st Grade | ||||||||||||
| AGG | 0.68 | 0.44 | 0.04 | 0.14 | --- | |||||||
| HYP | 0.50 | 0.71 | −0.03 | 0.13 | 0.55 | --- | ||||||
| ANX | 0.15 | 0.01 | 0.36 | 0.26 | 0.18 | 0.17 | --- | |||||
| WITH | 0.35 | 0.33 | 0.29 | 0.53 | 0.36 | 0.29 | 0.58 | --- | ||||
| 2nd Grade | ||||||||||||
| AGG | 0.64 | 0.48 | 0.03 | 0.22 | 0.77 | 0.55 | 0.15 | 0.35 | --- | |||
| HYP | 0.47 | 0.77 | −0.11 | 0.05 | 0.47 | 0.82 | 0.02 | 0.31 | 0.65 | --- | ||
| ANX | 0.04 | 0.20 | 0.05 | 0.16 | 0.05 | 0.25 | 0.50 | 0.24 | 0.06 | 0.24 | --- | |
| WITH | 0.20 | 0.21 | 0.24 | 0.58 | 0.14 | 0.25 | 0.30 | 0.56 | 0.31 | 0.24 | 0.47 | --- |
Notes. Pearson correlation coefficients with pairwise deletion of missing cases are reported. Pairwise sample sizes across years are between 236 and 238 for kindergarten with 1st grade; between 215 and 219 for 1st grade with 2nd grade; and between 205 and 208 for kindergarten with 2nd grade. All correlation coefficients with an absolute value greater than 0.12 are significant at p < .05. AGG = aggression/oppositionality; HYP = hyperactivity/inattention; ANX = anxiety; WITH = withdrawal.
Latent transition analysis
An LTA was conducted with the 4 symptom factor scores in order to
identify latent groups of children having particular profiles of scores across these four dimensions of behavior, and
examine continuity and discontinuity in these behavioral profiles across kindergarten, 1st, and 2nd grade.
LTA model selection
The first task was to identify the number of latent profiles that best characterize the children in this sample. This question was addressed in an exploratory fashion by fitting latent profile models with increasing numbers of latent profiles and using relative model information criteria, including Akaike’s Information Criterion (AIC), the Bayesian Information Criterion (BIC), and the sample-size adjusted Bayesian Information Criterion (aBIC), to select the number of profiles that optimizes the balance between model fit and complexity (Akaike, 1974; Schwartz, 1978; Sclove, 1987).
In all models, the same number of profiles was estimated in kindergarten, 1st, and 2nd grade. The factor score means and variances were allowed to vary freely across profiles within a given year, thus allowing the profiles to be distinguished by differences in both mean factor scores and variances around these mean scores. Although LPA studies frequently constrain variances to be equal across profiles in order to reduce the number of parameters that must be estimated, this constraint yielded substantially poorer model fit in the present sample. As is typical in LPA, the correlations between factor scores within each profile were fixed to 0 (i.e., the factor scores were assumed to be independent conditional on latent profile membership).
During model selection, measurement invariance was imposed by constraining the factor score means and variances within each profile to be equal across all years (the appropriateness of this assumption was later tested for the final selected model). The number of random starts was set at 2,000 initial-stage starts and 500 final-stage optimizations in order to obtain a well-identified maximum-likelihood solution. All models were conducted on the full sample of 336 children who had data in any year using full-information maximum likelihood estimation, which uses all available data assuming data are missing at random.
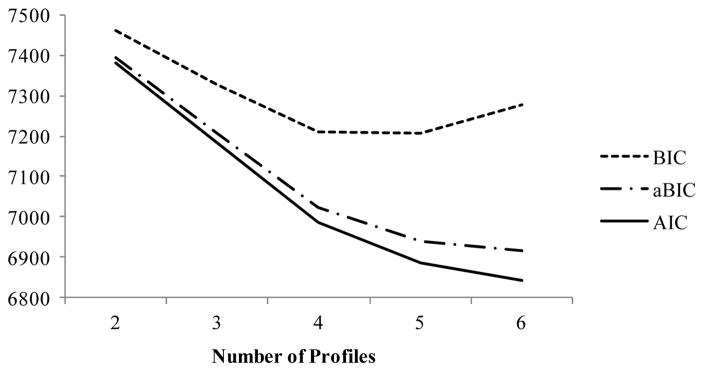
Model fit information for the 2- through 6-profile solutions are provided in Table 6 and the relative information criteria are plotted in Figure 1. BIC values decrease steadily through the 4-profile solution, are essentially the same for the 4- and 5-profile solutions, and increase in the 6-profile solution. Unlike the BIC, the AIC and aBIC values continue to decrease through the 6-profile solution; however, the rate of decrease progressively slows between the 4-, 5-, and 6-profile solutions, indicating smaller relative improvements in model fit. Thus, the relative information criteria point towards either the 4- or the 5-profile model as being optimal.
Table 6.
LTA model fit statistics for 2- through 6-profile solutions.
| # Profiles | #Free Parameters | LL | AIC | BIC | aBIC | Entropy |
|---|---|---|---|---|---|---|
| 2 | 21 | −3669.009 | 7380.0 | 7460.2 | 7393.6 | 0.870 |
| 3 | 38 | −3553.189 | 7182.4 | 7327.4 | 7206.9 | 0.828 |
| 4 | 59 | −3434.080 | 6986.2 | 7211.4 | 7024.2 | 0.831 |
| 5 | 84 | −3358.711 | 6885.4 | 7206.1 | 6939.6 | 0.820 |
| 6 | 113 | −3309.219 | 6844.4 | 7275.8 | 6917.3 | 0.840 |
Notes. Four factor scores were used as indicators of the latent profiles: aggression/oppositionality, hyperactivity/inattention, anxiety, and withdrawal. In all models, factor score means and variances were freely estimated across profiles within years, and the within-profile means and variances were constrained to be equal across years. LL = log-likelihood value; AIC = Akaike’s Information Criterion, BIC = Bayesian Information Criterion; aBIC = sample-size adjusted Bayesian Information Criterion.
Figure 1.
LTA model relative information criteria for 2- through 6-profile solutions
Notes. BIC = Bayesian Information Criterion; aBIC = sample-size adjusted Bayesian Information Criterion; AIC = Akaike’s Information Criterion.
It is common for relative information criteria to fail to unambiguously select an optimal model in latent profile analysis, and in such cases the interpretability of differences between profiles and the theoretical meaningfulness of the profile solutions must be considered. Therefore, the profile solutions yielded by the 4- and 5-profile models were compared. The 4-profile model yielded the following profiles: (1) well-adjusted, with very low scores on all internalizing and externalizing factors, (2) internalizing, with very low scores on both externalizing factors and elevated scores on both internalizing factors, (3) externalizing, with elevated scores on both externalizing factors and lower scores on both internalizing factors, and (4) comorbid, with high scores on all externalizing and internalizing factors. The 5-profile model yielded profiles that were very similar to those from the 4-profile model except that the comorbid profile was split into two profiles that were characterized by elevations in both externalizing and internalizing scores, one of which had very high externalizing scores (particularly hyperactivity/inattention) and only moderately high internalizing scores, and the other of which had very high internalizing scores, high aggression, and only moderately high hyperactivity/inattention. Thus, both the 4- and 5-profile models provided solutions with interpretable and well-separated profiles. However, the theoretical significance of the distinction between the two comorbid symptom profiles that were identified in the 5-profile solution is not entirely clear.
In order to check the robustness of the 4- and 5-profile solutions, both models were also tested in separate latent profile analyses incorporating two of the three data collection years, i.e., (1) kindergarten and 1st grade, (2) 1st and 2nd grade, and (3) kindergarten and 2nd grade. The 4-profile model was consistently replicated across all three 2-year LPAs, however the 5-profile model was not consistently replicated, with a particularly divergent solution in the 1st- and 2nd-grade LPA. Thus, the 5-profile solution did not appear to be as robust as the 4-profile solution. Based on this observation, as well as the greater parsimony of the 4-profile solution and the conclusion that the 5-profile solution did not make a strong substantive improvement on the 4-profile solution, all further analyses were conducted using the 4-profile solution.
The appropriateness of the measurement-invariance assumption, which constrains within-profile means and variances to be identical in all three years, was tested by comparing the fit of the measurement-invariant model to that of a model in which all within-profile factor score means and variances were freely estimated across all years (i.e., the unconstrained model). The likelihood-ratio test between these models was significant (Δ-2LL = 107.1, Δdf = 64, p < .001), indicating a greater-than-zero reduction in absolute model fit to the data as a result of the measurement invariance constraints. However, the AIC, BIC, and aBIC were all higher in the unconstrained model relative to the measurement-invariant model (ΔAIC =20.9, ΔBIC = 265.2, ΔaBIC = 62.2), suggesting that the measurement-invariant model was the more optimal model in terms of the balance between model fit and parsimony. Additionally, examination of the profile solutions for each year in the model without measurement invariance constraints (not reported) revealed that a remarkably similar solution is reached across all three years, and that this solution was very similar to that obtained in the measurement-invariant model. Therefore, the measurement-invariant model was used for all further analyses. This allows the interpretation of the profiles to remain constant between kindergarten, 1st, and 2nd grade.
The final question to be addressed in selecting the optimal LTA model was that of stationarity of transitions between the profiles over time. The LTA model included first-order autoregressive associations between the profiles such that profile membership probabilities in 1st and 2nd grade were estimated conditional on profile membership in the prior year. Initially, the probabilities of transitioning from a given profile in one year to each profile in the following year were freely estimated. This model was compared to a stationary model in which the corresponding profile transition probabilities were constrained to be equal across years. The stationary model did not result in significantly poorer fit to the data (Δ-2LL = 19.2, Δdf = 12, p = .08), and the AIC, BIC and aBIC were all lower in the stationary model relative to the model in which transition probabilities were freely estimated across years (ΔAIC = −4.8, ΔBIC = −50.6, ΔaBIC = −12.5), suggesting that the stationary model provided a more optimal balance between fit and parsimony. Furthermore, given the relatively short developmental duration reflected here, it is not clear whether theoretically meaningful distinctions can be drawn from changes in transition probabilities from kindergarten to 1st grade relative to 1st to 2nd grade. For these reasons, the stationary model was selected for all further analyses.
LTA results: Profile structure
The parameter estimates from the 4-profile measurement-invariant LTA solution are reported in Table 7. These estimates include the prevalence of each profile in each year and the factor score means and variances that define each profile. To facilitate interpretation of the profiles, the factor score means for each profile are also plotted in Figure 2 (for visual clarity, the factor score variances are not plotted). Tests of the statistical significance of the differences in factor score means across profiles revealed that all factor score means were significantly different between each pair of profiles (p’s < .05), with the exception of anxiety, which was equivalent in the comorbid and internalizing profiles. In interpreting the factor score means, it is important to note that each factor score has a sample mean of roughly 0. Since 61% of the children in the present study were selected based on teacher reports of early-emerging aggressive behaviors, the sample mean on the aggression/oppositionality factor score in particular reflects elevated levels of aggression relative to a non-selected community sample.
Table 7.
LTA 4-profile solution.
| Comorbid | Internalizing | Externalizing | Well-Adjusted | |
|---|---|---|---|---|
| Prevalence, n (%) | ||||
| Kindergarten | 160.7 (47.8%) | 78.4 (23.3%) | 74.6 (22.2%) | 22.3 ( 6.6%) |
| 1st grade | 161.7 (48.1%) | 69.3 (20.6%) | 71.6 (21.3%) | 33.3 ( 9.9%) |
| 2nd grade | 162.0 (48.2%) | 64.5 (19.2%) | 71.2 (21.2%) | 38.4 (11.4%) |
| Factor Score Means | ||||
| AGG | 0.628 | −0.886 | −0.041 | −1.194 |
| HYP | 0.561 | −0.716 | 0.000 | −1.123 |
| ANX | 0.404 | 0.395 | −0.552 | −0.837 |
| WITH | 0.423 | 0.048 | −0.465 | −1.098 |
| Factor Score Variances | ||||
| AGG | 0.545 | 0.327 | 0.333 | 0.142 |
| HYP | 0.429 | 0.341 | 0.308 | 0.111 |
| ANX | 0.532 | 0.400 | 0.230 | 0.073 |
| WITH | 0.435 | 0.593 | 0.280 | 0.110 |
Notes. All pairs of profiles differ significantly in their mean values on all factor scores, except for the comorbid and internalizing profiles which do not differ in mean anxiety scores. AGG = aggression/oppositionality; HYP = hyperactivity/inattention; ANX = anxiety; WITH = withdrawal.
Figure 2.
Factor score means within profiles for the LTA 4-profile solution.
Notes. AGG = aggression/oppositionality; HYP = hyperactivity/inattention; ANX = anxiety; WITH = withdrawal.
The four profiles can be described as: comorbid, externalizing, internalizing, and well-adjusted. In the present sample of at-risk children, the comorbid profile had by far the highest prevalence, making up 48% of the sample in each year. This profile was characterized by elevated scores across all four internalizing and externalizing behavior-problem dimensions. Specifically, this profile exhibited the highest scores on aggression/oppositionality, hyperactivity/inattention, and withdrawal, with anxiety scores equal to those of the internalizing profile. The externalizing and internalizing profiles had similar prevalence rates, each composing roughly 20% of the sample in each year. The externalizing profile was characterized by moderate levels of aggression/oppositionality and hyperactivity/inattention, and relatively low levels of anxiety and withdrawal. More specifically, the externalizing profile had mean scores on aggression/oppositionality and hyperactivity/inattention that were lower than those of the comorbid profile but much higher than those of the internalizing and well-adjusted profiles, along with mean scores on anxiety and withdrawal that were lower than those of the comorbid and internalizing profiles but slightly higher than those of the well-adjusted profile. The internalizing profile was characterized by high levels of anxiety, moderately high withdrawal, and low levels of both aggression/oppositionality and hyperactivity/inattention. Specifically, this profile had mean scores on aggression/oppositionality and hyperactivity/inattention that were much lower than those of the comorbid and externalizing profiles but still slightly higher than those of the well-adjusted profile, mean scores on anxiety that were much higher than those of the externalizing and well-adjusted profiles and equivalent to those of the comorbid profile, and mean scores on withdrawal that were much higher than those of the externalizing and well-adjusted profiles but significantly lower than the comorbid profile. Finally, the well-adjusted profile had the lowest prevalence at just 7% to 11% of the sample in each year (ranging from 22 children in kindergarten to 38 children in 2nd grade). This profile was characterized by the lowest scores across all four internalizing and externalizing factors. In addition, the variances around the mean factor scores within this profile were markedly lower than those for any other profile, indicating higher within-profile homogeneity.
LTA results: Profile transition probabilities
Continuity and discontinuity in children’s behavioral profiles over time is reflected in the estimated probability of membership in each profile conditional on prior profile membership, i.e., the profile transition probabilities. As described above, the model assumed stationarity of profile transitions over time, and therefore only one set of profile transition probabilities was estimated across both the kindergarten to 1st-grade and the 1st-grade to 2nd-grade intervals. Sparseness of the conditional profile membership probability matrix was handled by allowing Mplus to fix regression parameters as necessary to estimate 0 probability values for extremely unlikely transitions. The resulting transition probabilities are reported in Table 8. In this table, the rows represent prior profile membership and the columns represent later profile membership. The value in each cell represents the probability of being in the column profile conditional on previous membership in the row profile. The top panel of Table 8 presents the profile transition probabilities for adjacent years (i.e., 1-year intervals, with the transition probabilities held constant across each interval), which are directly derived from the model-estimated latent logistic regression parameters regressing each year’s profile membership on the prior-year profile membership. The second panel presents the cumulative transition probabilities over the full 2-year interval between kindergarten and 2nd grade (regardless of 1st-grade profile membership). These probabilities were calculated from the cross-tabulation of profile membership probabilities in each year produced by Mplus based on the estimated model. For both panels, continuity in symptom profiles over time is reported in the diagonal cells.
Table 8.
Profile transition probabilities across adjacent years and cumulatively from kindergarten to 2nd grade
| Comorbid | Internalizing | Externalizing | Well-Adjusted | |
|---|---|---|---|---|
| 1-Year Transition Probabilities | ||||
| Comorbid | 0.892 | 0.011 | 0.098 | 0.000 |
| Internalizing | 0.000 | 0.801 | 0.000 | 0.199 |
| Externalizing | 0.248 | 0.000 | 0.705 | 0.047 |
| Well-Adjusted | 0.000 | 0.217 | 0.147 | 0.636 |
| Cumulative 2-Year Transition Probabilities | ||||
| Comorbid | 0.819 | 0.018 | 0.156 | 0.007 |
| Internalizing | 0.000 | 0.684 | 0.029 | 0.286 |
| Externalizing | 0.395 | 0.013 | 0.529 | 0.063 |
| Well-Adjusted | 0.036 | 0.311 | 0.197 | 0.455 |
Notes. The value in each cell represents the probability of being in the column profile conditional on previous membership in the row profile. Profile stability rates are in bold font on the diagonal. Transition probabilities are constrained to be equal across adjacent years.
Overall, there was high continuity in symptom profiles over time. The highest continuity was observed for the comorbid profile; from one year to the next, 89% of these children continued to exhibit comorbid symptoms and only 10% transitioned to an externalizing profile. Over the full 2-year interval, 82% of children who were comorbid in kindergarten continued to exhibit comorbidity in 2nd grade. Nearly all cases of discontinuity among children in the comorbid profile were accounted for by transitions into the externalizing profile (16% over the course of 2 years). The probability of children who manifested comorbidity differentiating toward the internalizing profile or remitting to the well-adjusted profile was effectively 0.
The internalizing profile also showed high continuity, although not as high as that of the comorbid profile. From one year to the next, 80% of internalizing children continued to exhibit this profile, with the remainder (20%) remitting to the well-adjusted profile. Across the full 2-year interval, 68% of those who had exhibited internalizing symptoms in kindergarten continued to exhibit this profile in 2nd grade, and 29% had remitted to the well-adjusted profile. The probability of internalizing children transitioning to either the externalizing or comorbid profile was effectively 0, indicating that internalizing symptoms did not predict the additional accumulation of externalizing symptoms.
Among children exhibiting an externalizing profile, from one year to the next 71% continued to exhibit this symptom profile, 25% transitioned to a comorbid profile, and 5% showed a remission of symptoms. Across the full 2-year interval, 53% of children classified as externalizing in kindergarten continued to exhibit this profile in 2nd grade. Of the 47% of externalizing children who exhibited symptom profile discontinuity over the 2-year interval, the majority (40%) transitioned to a comorbid profile, thereby evidencing an additional accumulation of internalizing symptoms. Only a small proportion (6%) transitioned from an initial externalizing presentation into the well-adjusted profile by 2nd grade, and essentially none transitioned to an internalizing profile.
Somewhat surprisingly, year-to-year continuity was lowest for the well-adjusted profile. Adjacent-year continuity for this profile was 64%, with moderate probabilities of transitioning to both the internalizing (22%) and externalizing (15%) profiles. Across the full 2-year interval, only 46% of children classified as well-adjusted in kindergarten continued to exhibit this profile in 2nd grade, while 31% had transitioned to the internalizing profile and 20% had transitioned to the externalizing profile. Not surprisingly, the probability of a direct transition from the well-adjusted profile to the comorbid profile was effectively 0. In interpreting these transition probabilities, it is important to note that only 22 children were classified as well-adjusted in kindergarten. Given this low base rate, these transition probabilities reflect the movement of just a few children (e.g., the 31% transitioning to an internalizing profile by 2nd grade reflects only 7 children). Therefore, the precision and replicability of these transition probabilities may be lower for the well-adjusted profile relative to the other profiles.
A schematic diagram of the pattern of transitions between symptom profiles is provided in Figure 3. Each symptom profile is represented by a circle positioned roughly according to the profile’s severity on the externalizing and internalizing dimensions, which constitute the axes of the graph. The size of the circle approximates the prevalence of the profile in the present sample. Transitions between profiles with a probability of at least 5% (rounding to the nearest whole number) are illustrated by arrows connecting the circles.
Figure 3.
Schematic diagram of transition pathways between latent profiles.
Notes. The size of each circle approximates the prevalence of the profile, and the position of each circle approximates the severity of internalizing and externalizing symptoms within the profile. Transitions between profiles having probabilities greater than 10% are represented with thick arrows and transitions having probabilities between 5% and 10% are represented with thin arrows. AGG = aggression/oppositionality, HYP = hyperactivity/inattention, ANX = anxiety, WITH = withdrawal.
Discussion
Results from the present analyses provide an exploratory and descriptive examination of internalizing and externalizing symptom profile dynamics across the early school years. A latent profile analysis (LPA) conducted on children’s aggression/oppositionality, hyperactivity/inattention, anxiety, and social withdrawal in kindergarten, 1st, and 2nd grade suggested that children’s patterns of symptoms across these factors coalesce into four profiles that are present in all three years. Consistent with both the high-risk sample demographics and the study design, which over-selected children evidencing higher aggressive/oppositional behaviors relative to their peers, two of the four profiles identified were characterized by elevated levels of externalizing symptoms and collectively represented about 70% of the sample. By far the most prevalent of these profiles, making up nearly 50% of the sample, was a comorbid group characterized by high levels of both externalizing and internalizing symptoms. An additional 20% of the sample fit an externalizing profile with moderate externalizing symptoms and lower internalizing symptoms. Although participants were oversampled for elevated externalizing symptoms, no criterion regarding internalizing symptoms was applied. Thus, the predominance of internalizing symptom comorbidity among children exhibiting early externalizing symptoms suggests that this type of comorbidity is the norm rather than the exception, consistent with prior research (Bird et al., 1993; Epkins, 2000). Additionally, the higher severity of externalizing symptoms in the comorbid profile relative to the externalizing profile is consistent with prior research showing that groups of children with internalizing-externalizing comorbidity tend to have the most severe symptoms (Basten et al., 2013; Frankel et al., 1992; Kamphaus et al., 1999, 1997; Polier, Vloet, Herpertz-Dahlmann, Laurens, & Hodgins, 2011).
Although no screening procedure was used to select for internalizing symptoms, a profile emerged characterized by elevated levels of anxiety and social withdrawal in the absence of externalizing symptoms, representing approximately 20% of the sample. Surprisingly, the well-adjusted profile, characterized by the absence of any internalizing or externalizing symptoms, captured only about 10% of the sample. It is possible that the sampling strategy of selecting comparison children who were low on externalizing symptoms inadvertently oversampled for children whose anxious withdrawal served to inhibit any oppositional or aggressive behavior.
A latent transition analysis (LTA) was conducted to model the probability of transitioning between each set of profiles across adjacent years. The findings revealed high levels of continuity across years for the externalizing, internalizing, and comorbid symptom profiles. This high degree of continuity is particularly notable given that a different teacher completed the symptom checklists in each year. The LTA also revealed that the externalizing profile, but not the internalizing profile, was associated with a moderately increased risk for emergent internalizing-externalizing comorbidity. Additionally, children with an internalizing profile were much more likely to show full symptom remission than were children who exhibited externalizing symptoms.
Does the developmental course of comorbidity fit a common vulnerability, accumulation, or differentiation model?
The comorbid profile comprised nearly half of the study sample in kindergarten, and this proportion did not change substantially over the years. Continuity in this profile was very high, ranging from 82% to 89% depending on the time interval. Additionally, the emergence of new comorbid cases was relatively rare; 81% of the children exhibiting a comorbid profile in 2nd grade had already exhibited a comorbid profile in kindergarten. The high prevalence and stability of the comorbid profile is consistent with the common vulnerability model. According to this model, internalizing-externalizing comorbidity would likely be present early in childhood as a result of a common vulnerability that predisposes toward the expression of symptoms in both domains. This model would likewise predict high continuity of the comorbid profile and low rates of developmentally emergent comorbidity, since the underlying vulnerability is not likely to change over time.
Although the present study does not provide insight into the nature of this common vulnerability factor, strong candidates for intermediate phenotypes include negative affectivity (Mikolajewski et al., 2013; Rhee et al., 2015; Tackett et al., 2013) or emotion dysregulation (Beauchaine, 2015), and in some cases reward insensitivity (Andrews et al., 2011; Brenner & Beauchaine, 2011; Forbes & Dahl, 2005). At the neural level, negative affectivity is associated with exaggerated reactivity of threat-response circuitry (Whittle et al., 2006), which has been linked to genetic variation in central serotonergic functioning (Canli & Lesch, 2007; Murphy et al., 2013). Indeed, genetic markers of serotonergic function have been implicated in risk for anxiety, depression, and reactive aggressive (Beitchman et al., 2006; Karg, Burmeister, Shedden, & Sen, 2011; Lesch et al., 1996; Lesch & Merschdorf, 2000). Additionally, disruptions in prefrontal-limbic connectivity are associated with emotion dysregulation and risk for both internalizing and externalizing psychopathology (Beauchaine, 2015). Finally, reward insensitivity is linked to underactivation of the mesolimbic dopamine system (Brenner & Beauchaine, 2011; Neuhaus & Beauchaine, 2013) and has been implicated in sensation-seeking behaviors in externalizing disorders (Neuhaus & Beauchaine, 2013) and in anhedonic symptoms in depression (Treadway & Zald, 2014). One or more of these underlying factors could predispose toward stable expression of both internalizing and externalizing symptoms when combined with adverse environmental circumstances (Beauchaine & McNulty, 2013; Sroufe, 1997), which are likely experienced by many children in the present study given the high-risk sample demographics.
The findings of the present study do not provide strong support for the differentiation model of comorbidity, which suggests that comorbidity early in childhood may reflect nonspecific emotional-behavioral dysregulation that differentiates over the course of development into more “pure” internalizing or externalizing symptom presentations based on the child’s experiences. Year-to-year transitions from the comorbid profile to the internalizing profile were very rare (1.1%), and transitions to the externalizing profile were only slightly more common (9.8%). It is worth noting that these transitions to the externalizing profile are likely to reflect a decrease in symptom severity across all 4 symptom factors, with an especially pronounced decrease in internalizing symptoms. This could reflect a delayed adjustment to the transition to school that may have exacerbated symptom expression during kindergarten for some children. Although these results suggest that comorbidity present in childhood is already highly stable, with very little evidence of differentiating toward single-domain profiles, participants were only followed through 2nd grade. Whether children with comorbid symptom profiles differentiate toward single-domain symptom profiles in later childhood or adolescence requires further study.
Although the findings generally support the common vulnerability model, some evidence for the accumulation hypothesis was evident specifically for the pathway whereby externalizing symptoms increase the risk for the additional acquisition of internalizing symptoms. Research has proposed that internalizing symptoms develop as the social consequences of externalizing problems, such as peer rejection, begin to take an emotional toll (Gooren, van Lier, Stegge, Terwogt, & Koot, 2011; Ladd & Troop-Gordon, 2003; van Lier & Koot, 2010), and thus this model does not necessarily imply a common mechanism underlying symptoms in both domains. In the present study, having a profile of moderate externalizing symptoms was associated with a 25% probability of transitioning to a comorbid internalizing-externalizing profile in the following year, and a 40% probability of developing comorbid symptoms within 2 years. Conversely, consistent with prior literature (Gilliom & Shaw, 2004; Keiley, Bates, Dodge, & Pettit, 2000), having an internalizing symptom profile was associated with extremely low risk of later developing comorbid symptoms. Although there was clear evidence of transitions from externalizing to comorbid profiles, it is important to note that this pathway only accounts for a small percentage of comorbid symptom presentations in the present sample, with fewer than 20% of the children classified as comorbid in 2nd grade having exhibited an externalizing profile in kindergarten.
Since 60% of kindergarten externalizing children did not develop comorbid internalizing symptoms by 2nd grade, future research should investigate the factors that predict which externalizing children are likely to develop emergent internalizing-externalizing comorbidity. It is possible that the children who do not develop comorbid internalizing symptoms may experience fewer negative consequences of their externalizing behaviors, such as peer-rejection. For instance, some children may appear hyperactive, inattentive, and oppositional from the teacher’s perspective but still manage to succeed socially with peers. It is also possible that some externalizing children are less capable of internalizing the consequences of their actions, and may not experience rejection from peers in the same way that individuals prone to anxiety do. Research has identified cognitive biases among children with externalizing problems such that their estimation of their own social standing can be highly discrepant from actual peer perceptions and social relationships (Gresham, MacMillan, Bocian, Ward, & Forness, 1998). These types of unrealistic attributional tendencies may be explained by neurobiological theories of hyperactivity/impulsivity. Dopaminergic deficiencies observed in both rodent models and human studies indicate a deficiency in the ability to identify contingent associations between behavior and adverse consequences (Gatzke-Kopp et al., 2009; Sagvolden, Johansen, Aase, & Russell, 2005). Externalizing children with such underlying deficiencies in recognizing the consequences of their behaviors may be more likely to see rejection from peers as arbitrary and unfair, and therefore be more likely to react with anger than sadness. Thus, it is possible that among children with elevated externalizing symptoms in kindergarten, different neural vulnerabilities predispose children toward or away from the likelihood of developing comorbidity.
Continuities and discontinuities in symptom profiles
The strikingly high continuity of the comorbid symptom profile across the first three years of school is consistent with prior studies suggesting that comorbidity of internalizing and externalizing symptoms is associated with particularly high risk for pervasive and persistent adjustment problems (Ialongo et al., 1996; Sourander et al., 2007). The presence of comorbidity has been associated with more severe consequences than either internalizing or externalizing symptom profiles alone. Children with internalizing-externalizing comorbidity are more likely to experience academic struggles (Yoo, Brown, & Luthar, 2009) and to be rejected and victimized by peers (Harrist, Zaia, Bates, Dodge, & Pettit, 1997; Ladd & Burgess, 1999). These adverse experiences create a positive feedback loop, reinforcing both internalizing and externalizing symptoms over time (Hymel, Rubin, Rowden, & LeMare, 1990; Ladd, 2006; Moilanen, Shaw, & Maxwell, 2010; van Lier & Koot, 2010). The developmental persistence of comorbid symptoms underscores the importance of identifying interventions that are effective for the sizable proportion of children who show mixed emotional and behavioral problems at school entry.
In the present study, moderately high continuity was also observed for the externalizing symptom profile, with 53% of externalizing kindergarteners continuing to show this same profile of symptoms in the spring of 2nd grade. Importantly, another 40% of externalizing kindergarteners transitioned into the comorbid symptom profile, which was characterized by even higher mean externalizing symptom severity along with high internalizing symptom severity. Thus, 93% of children with an externalizing profile in kindergarten continued to show externalizing symptoms, with or without comorbid internalizing symptoms, in 2nd grade. This continuity rate is higher than that typically found in studies utilizing threshold-based approaches to classify children as disordered versus non-disordered, which tend to yield externalizing disorder persistence estimates of 40 to 50% over similar time periods (Lavigne et al., 1998; McConaughy, Stanger, & Achenbach, 1992; Verhulst & Althaus, 1988). The high continuity of externalizing symptoms observed in the present study may reflect a strength of the latent transition analysis technique, which takes advantage of the richness of information available from continuous symptom scales collected over multiple occasions. Indeed, studies have shown that continuous symptom scales show higher stability over time than do threshold-based classifications of psychopathology (McConaughy et al., 1992). In the present study, the externalizing profile likely included many children who would fall below conventional cutoffs for “clinically-significant” externalizing psychopathology, yet this profile of symptoms was highly persistent over time and was associated with substantial risk for developing more severe comorbid symptoms. Had a threshold-based classification approach been used, the marked persistence of relatively moderate externalizing behaviors and the associated risk for worsening symptoms would likely have been missed.
In interpreting the low externalizing symptom remission rate in the present study, however, it is important to note that the well-adjusted profile was characterized by extremely low symptom levels, rather than by the absence of high symptom levels. Thus, children showing modest decreases in externalizing symptoms over time may still have been classified in the externalizing profile because their symptoms did not decrease to the level of the well-adjusted profile. From this perspective, the low remission rate for externalizing symptoms in the present study is consistent with prior studies that distinguish between symptom improvement and full remission of symptoms. For example, in a large-scale study of children’s emotional-behavioral symptoms over the course of two years, Verhulst and Althaus (1988) observed that 46% of children who were initially above the 90th percentile on the Child Behavior Checklist were below this cutoff two years later, indicating a substantial rate of symptom improvement, however only 5% of those initially above the cutoff were within the “normal” range (below the 50th percentile) two years later, indicating a very low rate of full symptom remission.
Finally, the continuity of externalizing symptoms in the present sample must be interpreted in light of social-contextual factors. the sample was drawn from a low-income, urban school district with high levels of neighborhood crime, low average parental education levels, and a high proportion of single-parent households. These sample characteristics are associated with heightened risk for externalizing problems (McLoyd, 1998) and are therefore likely to contribute to particularly high continuity of these problems. Research on samples from diverse socioeconomic backgrounds will be required to ascertain the generalizability of the symptom continuity rates observed in the present study.
In contrast to the extremely low rates of symptom remission observed for the externalizing and comorbid profiles, kindergarteners exhibiting an internalizing profile had a moderate (29%) probability of remitting by 2nd grade. It is possible that these remitting internalizing children had only temporarily displayed noticeable anxiety and social withdrawal as a response to the transition to school, which can be particularly stressful for children with a predisposition toward social anxiety (Coplan & Arbeau, 2008), and that these symptoms subsided as they adjusted to the social demands of school. Despite the moderate probability of remitting by 2nd grade, the continuity of internalizing symptoms observed in the present study is still substantially higher than that frequently observed in studies using “clinically-significant” threshold-based classifications (McConaughy et al., 1992; Verhulst & Althaus, 1988). This provides further evidence in support of the power of the latent transition analysis technique to detect developmentally stable symptom profiles. Interestingly, the probability of transitioning from the comorbid profile to a profile characterized by low internalizing symptoms (either externalizing or well-adjusted) was roughly half of the probability of transitioning from the internalizing profile to a profile with low internalizing symptoms, suggesting that internalizing symptoms may be more persistent when paired with co-occurring externalizing symptoms. This observation is consistent with the research cited above on the particularly high persistence of comorbid internalizing-externalizing disorders, as well as the tendency for externalizing psychopathology to be associated with increased risk for subsequent internalizing psychopathology.
It is important to note that, despite the high prevalence of the comorbid profile in all years, the chance that a child exhibiting either an internalizing or an externalizing symptom profile would transition to the other profile in a later year was exceedingly low. Thus, in addition to the hypothesized common vulnerability factor predisposing toward both internalizing and externalizing symptoms, there must also be differential risk factors that increase the risk for one domain of symptoms over the other, thereby maintaining distinct developmental trajectories among children who are either high or low on these factors. The traits of behavioral inhibition and impulsivity are clear candidates for such differential risk factors (Beauchaine, 2015). Excessive behavioral inhibition has been robustly demonstrated to be a risk factor for internalizing psychopathology (Rosenbaum, Biederman, Bolduc-Murphy, Faraone, Chaloff, Hirshfeld, & Kagan, 1993), whereas trait impulsivity is a well-established precursor to all forms of externalizing psychopathology (Beauchaine & McNulty, 2013; Clark, 2005). Comorbidity may be most likely to emerge in individuals who are high on a common vulnerability factor, such as negative affectivity or emotion dysregulation, and who exhibit moderate levels on differentiating risk factors such as behavioral inhibition versus impulsivity.
Is there an “externalizing only” profile?
Several previous studies using exploratory latent profile or cluster analysis of symptom scales have failed to identify a group of children characterized by high externalizing symptoms in the absence of internalizing symptoms (Basten et al., 2013; Bulotsky-Shearer et al., 2010; Frankel et al., 1992; Kamphaus et al., 1999, 1997). In the present study, two profiles were identified with elevated scores on externalizing factors, and notably neither of them had internalizing scores as low as those in the well-adjusted profile. The highest externalizing scores were observed within the comorbid profile, which was also characterized by high anxiety and the highest levels of social withdrawal of any profile. The majority of children with externalizing symptoms in the present sample fit this profile, suggesting that severe externalizing symptoms are most often accompanied by high levels of internalizing symptoms as well. The externalizing profile was characterized on average by more moderate levels of externalizing symptoms and lower levels of internalizing symptoms, however the mean anxiety and withdrawal scores for this profile were still significantly higher than those for the well-adjusted profile. Thus, this profile also does not appear to represent a true “externalizing-only” profile. The lack of a true externalizing-only profile may indicate that such a profile is rare, and reflective of psychopathic tendencies that occur with extremely low frequency.
It is important to note that frequent failure of studies using exploratory latent profile or cluster analysis techniques to identify an externalizing-only profile is in contrast to studies that employ threshold-classification approaches, and highlights the descriptive value of these exploratory techniques, which maximize symptom information along a full continuum. Indeed, since the mean externalizing factor scores in the externalizing profile were not significantly higher than the sample mean for these factors in the present study, if a threshold/diagnostic classification approach had been used this group may have been classified as typically developing or excluded due to the subthreshold elevations in externalizing symptoms. Such an approach would have missed important distinctions between this moderately-externalizing group and truly well-functioning children, such as their heightened risk for developing comorbid internalizing-externalizing symptoms.
Syndrome-level patterns of co-occurrence
In the present study, the internalizing domain was represented by anxiety and social withdrawal factors, and the externalizing domain was represented by aggression/oppositionality and hyperactivity/inattention factors. These factors reflect well-recognized emotional-behavioral syndromes that are often examined independently. By measuring multiple syndromes within the broader internalizing and externalizing domains, it is possible to address the question of whether certain syndromes are particularly likely to exhibit cross-domain comorbidity (Vaidyanathan, Patrick, & Iacono, 2011).
The profiles that emerged in the present study were generally characterized by similar levels on the two factors within each domain, consistent with a view of these syndromes as reflecting underlying, perhaps genetically mediated, internalizing and externalizing factors (Carragher et al., 2015). The comorbid profile in this sample was equally elevated on aggression/oppositionality, hyperactivity/inattention, anxiety and social withdrawal, indicating that none of these syndromes was differentially likely to exhibit cross-domain comorbidity. The only potential case of within-domain syndrome differentiation was observed for the internalizing profile, which exhibited slightly higher elevations in anxiety than in social withdrawal. In fact, this profile had significantly lower social withdrawal scores than did the comorbid profile, despite the two sharing very similar elevations on the anxiety factor. This finding is consistent with prior research showing that children with internalizing-externalizing comorbidity are particularly likely to experience peer rejection and victimization (Harrist et al., 1997; Ladd & Burgess, 1999), which may increase their inclination to withdraw from social interactions as a defensive strategy. Peer rejection of children exhibiting comorbid symptoms is likely to be a consequence of these children’s inappropriate social behaviors. In contrast, it is possible that elevated anxiety symptoms in the absence of comorbid externalizing symptoms could motivate a desire to engage in appropriate social behavior, thereby partially counteracting the fear of social interaction experienced by many anxious children. Anxiety has been associated with increased sensitivity to negative social feedback (Cremers, Veer, Spinhoven, Rombouts, & Roelofs, 2014), which could enhance the rate at which anxious children learn through experience how to adjust their behaviors to improve their social interactions and gain acceptance by their peers. In contrast, anxious children with comorbid externalizing symptoms may lack this social awareness and motivation.
Limitations
The high demographic risk of the population from which the participants were selected likely had a significant effect on the prevalence of the different profiles, as well as rates of continuity in symptom profiles over time. This raises important issues related to generalization and representation. If study results can only be interpreted to represent the very specific sample from which the data were drawn, the proliferation of descriptive studies may not suffice to propel the field forward. However, if findings cannot be assumed to generalize, it is imperative that the literature represent a diverse range of populations, with guidance as to whom specific studies can be considered to represent (Gatzke-Kopp, 2016). It is very likely, however, that core classifications are largely consistent across populations, with sample-specific factors directly influencing the prevalence of profile membership rather than the structure of the latent profiles themselves. For instance, epidemiological research with an adult sample found the structure of a dimensional and multivariate model of comorbidity fit equally well for both males and females, with sex affecting only the prevalence of specific dimensions (Eaton et al., 2012). Similarly, the structure of psychiatric comorbidity has been shown to be invariant across ethnic categories, with ethnicity affecting only the prevalence of symptoms (Eaton et al., 2013). It is also likely that the general pattern of transitions between profiles over time is generalizable across samples, even if the specific transition probabilities may vary.
Additionally, when comparing the present results to other studies, the age range and sampling interval of the present study must be considered. This study examined continuity and discontinuity in symptom profiles over the first few years of formal schooling. Studies over longer time intervals are likely to find lower continuity rates than those observed here. Additionally, the developmental patterns observed in the present study cannot be assumed to generalize across different age ranges. In particular, key periods of developmental change, such as puberty, may be expected to alter these developmental processes. The developmental dynamics of children’s latent symptom profiles over longer time intervals or across different developmental periods require further investigation.
Summary
This study is one of the first to employ LTA to characterize latent profiles of continuous externalizing and internalizing symptom factors and quantify the dynamics in internalizing-externalizing symptom profile membership across the early school years. This sample was assessed at the start of formal schooling, thus capturing early developmental manifestations of symptom expression. These results indicate a strong degree of continuity for psychopathology, and do not clearly support the hypothesis that symptom presentation is in flux among younger children. In contrast, comorbid internalizing-externalizing symptoms at this age appear to be highly stable and prevalent as early as kindergarten, providing support for a common vulnerability model of comorbidity. However, moderate externalizing symptoms do appear to increase the risk for the development of comorbidity in a subset of participants, providing some support for a symptom accumulation model of comorbidity by which externalizing symptoms indirectly increase the risk of developing internalizing symptoms.
Acknowledgments
Data collection for this project was funded by grants from the Pennsylvania Department of Health and The Social Science Research Institute at The Pennsylvania State University to the 2nd author. This paper was also supported by grant R305B090007 from the Institute of Education Sciences to the 1st author and grants P50-DA10075 and P50-DA039838 from the National Institute on Drug Abuse to the 3rd author.
The authors also wish to thank Jennifer Ford for her extensive work in managing the complex data collection in this project, the numerous research assistants who contributed to this endeavor, and Jim Stieben for his generosity with the task software. The authors also would like to acknowledge Mark Greenberg, Karen Bierman, and Robert Nix, for their roles in designing, executing, overseeing, and managing the project from which these data are drawn.
References
- Achenbach TM, Edelbrock CS. The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletin. 1978;85(6):1275–1301. [PubMed] [Google Scholar]
- Akaike H. A new look at the statistical model identification. IEEE Transactions on Automatic Control. 1974;19:716–723. [Google Scholar]
- Andrews MM, Meda SA, Thomas AD, Potenza MN, Krystal JH, Worhunsky P, … Pearlson GD. Individuals family history positive for alcoholism show functional magnetic resonance imaging differences in reward sensitivity that are related to impulsivity factors. Biological Psychiatry. 2011;69(7):675–683. doi: 10.1016/j.biopsych.2010.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T, Muthén B. Exploratory structural equation modeling. Structural Equation Modeling: A Multidisciplinary Journal. 2009;16(3):397–438. [Google Scholar]
- Basten MMGJ, Althoff RR, Tiemeier H, Jaddoe VWV, Hofman A, Hudziak JJ, … van der Ende J. The dysregulation profile in young children: Empirically defined classes in the Generation R study. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(8):841–850. doi: 10.1016/j.jaac.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP. Future directions in emotion dysregulation and youth psychopathology. Journal of Clinical Child & Adolescent Psychology. 2015;44(5):875–896. doi: 10.1080/15374416.2015.1038827. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, McNulty T. Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology. Development and Psychopathology. 2013;25(4):1505–1528. doi: 10.1017/S0954579413000746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beitchman JH, Baldassarra L, Mik H, De Luca V, King N, Bender D, … Kennedy JL. Serotonin transporter polymorphisms and persistent, pervasive childhood aggression. The American Journal of Psychiatry. 2006;163(6):1103–1105. doi: 10.1176/ajp.2006.163.6.1103. [DOI] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza BM. Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(2):361–368. doi: 10.1097/00004583-199303000-00018. [DOI] [PubMed] [Google Scholar]
- Brenner SL, Beauchaine TP. Pre-ejection period reactivity and psychiatric comorbidity prospectively predict substance use initiation among middle-schoolers: A pilot study. Psychophysiology. 2011;48(11):1588–1596. doi: 10.1111/j.1469-8986.2011.01230.x. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods & Research. 1992;21(2):230–258. [Google Scholar]
- Bulotsky-Shearer RJ, Fantuzzo JW, McDermott PA. Typology of emotional and behavioral adjustment for low-income children: A child-centered approach. Journal of Applied Developmental Psychology. 2010;31(2):180–191. [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46(11):1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Canli T, Lesch KP. Long story short: the serotonin transporter in emotion regulation and social cognition. Nature Neuroscience. 2007;10(9):1103–1109. doi: 10.1038/nn1964. [DOI] [PubMed] [Google Scholar]
- Caron C, Rutter M. Comorbidity in child psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry. 1991;32(7):1063–1080. doi: 10.1111/j.1469-7610.1991.tb00350.x. [DOI] [PubMed] [Google Scholar]
- Carragher N, Krueger RF, Eaton NR, Slade T. Disorders without borders: Current and future directions in the meta-structure of mental disorders. Social Psychiatry and Psychiatric Epidemiology. 2015;50(3):339–350. doi: 10.1007/s00127-014-1004-z. [DOI] [PubMed] [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal. 2002;9(2):233–255. [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114(4):505–521. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent Class and Latent Transition Analysis. Hoboken, NJ: John Wiley & Sons, Inc; 2010. [Google Scholar]
- Collins LM, Wugalter SE. Latent class models for stage-sequential dynamic latent variables. Multivariate Behavioral Research. 1992;27(1):131–157. [Google Scholar]
- Coplan RJ, Arbeau KA. The stresses of a “Brave New World”: Shyness and school adjustment in kindergarten. Journal of Research in Childhood Education. 2008;22(4):377–389. [Google Scholar]
- Cosgrove VE, Rhee SH, Gelhorn HL, Boeldt D, Corley RC, Ehringer MA, … Hewitt JK. Structure and etiology of co-occurring internalizing and externalizing disorders in adolescents. Journal of Abnormal Child Psychology. 2011;39(1):109–123. doi: 10.1007/s10802-010-9444-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cremers HR, Veer IM, Spinhoven P, Rombouts SARB, Roelofs K. Neural sensitivity to social reward and punishment anticipation in social anxiety disorder. Frontiers in Behavioral Neuroscience. 2015;8 doi: 10.3389/fnbeh.2014.00439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiStefano C, Kamphaus RW. Investigating subtypes of child development: A comparison of cluster analysis and latent class cluster analysis in typology creation. Educational and Psychological Measurement. 2006;66(5):778–794. [Google Scholar]
- Dougherty LR, Smith VC, Bufferd SJ, Kessel E, Carlson GA, Klein DN. Preschool irritability predicts child psychopathology, functional impairment, and service use at age nine. Journal of Child Psychology and Psychiatry. 2015;56(9):999–1007. doi: 10.1111/jcpp.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Balsis S, Skodol AE, Markon KE, … Hasin DS. An invariant dimensional liability model of gender differences in mental disorder prevalence: Evidence from a national sample. Journal of Abnormal Psychology. 2012;121(1):282–288. doi: 10.1037/a0024780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Keyes KM, Krueger RF, Noordhof A, Skodol AE, Markon KE, … Hasin DS. Ethnicity and psychiatric comorbidity in a national sample: Evidence for latent comorbidity factor invariance and connections with disorder prevalence. Social Psychiatry and Psychiatric Epidemiology. 2013;48(5):701–710. doi: 10.1007/s00127-012-0595-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelbrock C, Achenbach TM. A typology of child behavior profile patterns: Distribution and correlates for disturbed children aged 6–16. Journal of Abnormal Child Psychology. 1980;8(4):441–470. doi: 10.1007/BF00916500. [DOI] [PubMed] [Google Scholar]
- Epkins CC. Cognitive specificity in internalizing and externalizing problems in community and clinic-referred children. Journal of Clinical Child Psychology. 2000;29(2):199–208. doi: 10.1207/S15374424jccp2902_6. [DOI] [PubMed] [Google Scholar]
- Forbes EE, Dahl RE. Neural systems of positive affect: Relevance to understanding child and adolescent depression? Development and Psychopathology. 2005;17(3):827–50. doi: 10.1017/S095457940505039X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankel F, Hanna GL, Cantwell DP, Shekim W, Ornitz E. Cluster analysis of child behavior checklists of 6 to 11-year-old males with varying degrees of behavior disorders. Child Psychiatry and Human Development. 1992;23(2):69–85. doi: 10.1007/BF00709751. [DOI] [PubMed] [Google Scholar]
- Gatzke-Kopp LM. Diversity and representation: Key issues for psychophysiological science. Psychophysiology. 2016;53(1):3–13. doi: 10.1111/psyp.12566. [DOI] [PubMed] [Google Scholar]
- Gatzke-Kopp LM, Beauchaine TP, Shannon KE, Chipman J, Fleming AP, Crowell SE, … Aylward E. Neurological correlates of reward responding in adolescents with and without externalizing behavior disorders. Journal of Abnormal Psychology. 2009;118(1):203. doi: 10.1037/a0014378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gatzke-Kopp LM, Greenberg MT, Fortunato CK, Coccia MA. Aggression as an equifinal outcome of distinct neurocognitive and neuroaffective processes. Development and Psychopathology. 2012;24(3):985–1002. doi: 10.1017/S0954579412000491. [DOI] [PubMed] [Google Scholar]
- Gilliom M, Shaw DS. Codevelopment of externalizing and internalizing problems in early childhood. Development and Psychopathology. 2004;16(2):313–333. doi: 10.1017/s0954579404044530. [DOI] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Gooren EMJC, van Lier PAC, Stegge H, Terwogt MM, Koot HM. The development of conduct problems and depressive symptoms in early elementary school children: The role of peer rejection. Journal of Clinical Child & Adolescent Psychology. 2011;40(2):245–253. doi: 10.1080/15374416.2011.546045. [DOI] [PubMed] [Google Scholar]
- Gresham FM, MacMillan DL, Bocian KM, Ward SL, Forness SR. Comorbidity of hyperactivity-impulsivity-inattention and conduct problems: Risk factors in social, affective, and academic domains. Journal of Abnormal Child Psychology. 1998;26(5):393–406. doi: 10.1023/a:1021908024028. [DOI] [PubMed] [Google Scholar]
- Harrist AW, Zaia AF, Bates JE, Dodge KA, Pettit GS. Subtypes of social withdrawal in early childhood: Sociometric status and social-cognitive differences across four years. Child Development. 1997;68(2):278–294. [PubMed] [Google Scholar]
- Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30(2):179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- Hymel S, Rubin KH, Rowden L, LeMare L. Children’s peer relationships: Longitudinal prediction of internalizing and externaliziing problems from middle to late childhood. Child Development. 1990;61(6):2004–2021. [Google Scholar]
- Ialongo N, Edelsohn G, Werthamer-Larsson L, Crockett L, Kellam S. The course of aggression in first-grade children with and without comorbid anxious symptoms. Journal of Abnormal Child Psychology. 1996;24(4):445–456. doi: 10.1007/BF01441567. [DOI] [PubMed] [Google Scholar]
- Kamphaus RW, Huberty CJ, DiStefano C, Petoskey MD. A typology of teacher-rated child behavior for a national U.S. sample. Journal of Abnormal Child Psychology. 1997;25(6):453–463. doi: 10.1023/a:1022681630818. [DOI] [PubMed] [Google Scholar]
- Kamphaus RW, Petoskey MD, Cody AH, Rowe EW, Huberty CJ, Reynolds CR. A typology of parent rated child behavior for a national U.S. sample. Journal of Child Psychology and Psychiatry. 1999;40(4):607–616. [PubMed] [Google Scholar]
- Karg K, Burmeister M, Shedden K, Sen S. The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: Evidence of genetic moderation. Archives of General Psychiatry. 2011;68(5):444–454. doi: 10.1001/archgenpsychiatry.2010.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keiley MK, Bates JE, Dodge KA, Pettit GS. A cross-domain growth analysis: Externalizing and internalizing behaviors during 8 years of childhood. Journal of Abnormal Child Psychology. 2000;28(2):161–179. doi: 10.1023/a:1005122814723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladd GW. Peer rejection, aggressive or withdrawn behavior, and psychological maladjustment from ages 5 to 12: An examination of four predictive models. Child Development. 2006;77(4):822–846. doi: 10.1111/j.1467-8624.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- Ladd GW, Burgess KB. Charting the relationship trajectories of aggressive, withdrawn, and aggressive/withdrawn children during early grade school. Child Development. 1999;70(4):910–929. doi: 10.1111/1467-8624.00066. [DOI] [PubMed] [Google Scholar]
- Ladd GW, Troop-Gordon W. The role of chronic peer difficulties in the development of children’s psychological adjustment problems. Child Development. 2003;74(5):1344–1367. doi: 10.1111/1467-8624.00611. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Van Hulle CA, Singh AL, Waldman ID, Rathouz PJ. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry. 2011;68(2):181–189. doi: 10.1001/archgenpsychiatry.2010.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID. Personality dispositions and the development of violence and conduct problems. In: Flannery DJ, Vazsonyi AT, Waldman ID, editors. Behavior and Aggression. New York, NY: Cambridge University Press; 2007. pp. 260–287. [Google Scholar]
- Lavigne JV, Arend R, Rosenbaum D, Binns HJ, Christoffel KK, Gibbons RD. Psychiatric disorders with onset in the preschool years: I. Stability of diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37(12):1246–1254. doi: 10.1097/00004583-199812000-00007. [DOI] [PubMed] [Google Scholar]
- Lesch KP, Bengel D, Heils A, Sabol SZ, Greenberg BD, Petri S, … Murphy DL. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science. 1996;274(5292):1527–1531. doi: 10.1126/science.274.5292.1527. [DOI] [PubMed] [Google Scholar]
- Lesch KP, Merschdorf U. Impulsivity, aggression, and serotonin: A molecular psychobiological perspective. Behavioral Sciences & the Law. 2000;18(5):581–604. doi: 10.1002/1099-0798(200010)18:5<581::aid-bsl411>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Lilienfeld SO, Waldman ID, Israel AC. A critical examination of the use of the term and concept of comorbidity in psychopathology research. Clinical Psychology: Science and Practice. 1994;1(1):71–83. [Google Scholar]
- Marsh HW, Morin AJS, Parker PD, Kaur G. Exploratory structural equation modeling: An integration of the best features of exploratory and confirmatory factor analysis. Annual Review of Clinical Psychology. 2014;10(1):85–110. doi: 10.1146/annurev-clinpsy-032813-153700. [DOI] [PubMed] [Google Scholar]
- McConaughy SH, Stanger C, Achenbach TM. Three-year course of behavioral/emotional problems in a national sample of 4- to 16-year-olds: I. Agreement among informants. Journal of the American Academy of Child. 1992;31(5):932–940. doi: 10.1097/00004583-199209000-00023. [DOI] [PubMed] [Google Scholar]
- McDermott PA, Weiss RV. A normative typology of healthy, subclinical, and clinical behavior styles among American children and adolescents. Psychological Assessment. 1995;7(2):162–170. [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53(2):185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- Mikolajewski AJ, Allan NP, Hart SA, Lonigan CJ, Taylor J. Negative affect shares genetic and environmental influences with symptoms of childhood internalizing and externalizing disorders. Journal of Abnormal Child Psychology. 2013;41(3):411–423. doi: 10.1007/s10802-012-9681-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moilanen KL, Shaw DS, Maxwell KL. Developmental cascades: Externalizing, internalizing, and academic competence from middle childhood to early adolescence. Development and Psychopathology. 2010;22(3):635–653. doi: 10.1017/S0954579410000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy SE, Norbury R, Godlewska BR, Cowen PJ, Mannie ZM, Harmer CJ, Munafò MR. The effect of the serotonin transporter polymorphism (5-HTTLPR) on amygdala function: A meta-analysis. Molecular Psychiatry. 2013;18(4):512–520. doi: 10.1038/mp.2012.19. [DOI] [PubMed] [Google Scholar]
- Muthén B, Asparouhov T. Latent variable analysis with categorical outcomes: Multiple-group and growth modeling in Mplus. Mplus Web Notes no 4. 2002 Dec 9;5 Retrieved from http://www.statmodel.com/examples/webnote.shtml. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- Neuhaus E, Beauchaine T. Impulsivity and vulnerability to psychopathology. In: Beauchaine TP, Hinshaw SP, editors. Child and Adolescent Psychopathology. 2. Hoboken, N.J: John Wiley & Sons; 2013. pp. 197–226. [Google Scholar]
- Nobile M, Colombo P, Bellina M, Molteni M, Simone D, Nardocci F, … Battaglia M. Psychopathology and adversities from early- to late-adolescence: A general population follow-up study with the CBCL DSM-Oriented Scales. Epidemiology and Psychiatric Sciences. 2013;22(1):63–73. doi: 10.1017/S2045796012000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polier GG, Vloet TD, Herpertz-Dahlmann B, Laurens KR, Hodgins S. Comorbidity of conduct disorder symptoms and internalising problems in children: Investigating a community and a clinical sample. European Child & Adolescent Psychiatry. 2011;21(1):31–38. doi: 10.1007/s00787-011-0229-6. [DOI] [PubMed] [Google Scholar]
- Rhee SH, Lahey BB, Waldman ID. Comorbidity among dimensions of childhood psychopathology: Converging evidence from behavior genetics. Child Development Perspectives. 2015;9(1):26–31. doi: 10.1111/cdep.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum JF, Biederman J, Bolduc-Murphy EA, Faraone SV, Chaloff J, Hirshfeld DR, Kagan J. Behavioral inhibition in childhood: A risk factor for anxiety disorders. Harvard Review of Psychiatry. 1993;1(1):2–16. doi: 10.3109/10673229309017052. [DOI] [PubMed] [Google Scholar]
- Sagvolden T, Johansen EB, Aase H, Russell VA. A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive/impulsive and combined subtypes. Behavioral and Brain Sciences. 2005;28(03):397–419. doi: 10.1017/S0140525X05000075. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitz S, Fulker DW, Plomin R, Zahn-Waxler C, Emde RN, DeFries JC. Temperament and problem behaviour during early childhood. International Journal of Behavioral Development. 1999;23(2):333–355. [Google Scholar]
- Schwartz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52:333–343. [Google Scholar]
- Sourander A, Jensen P, Davies M, Niemelä S, Elonheimo H, Ristkari T, … Almqvist F. Who is at greatest risk of adverse long-term outcomes? The Finnish From a Boy to a Man study. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(9):1148–1161. doi: 10.1097/chi.0b013e31809861e9. [DOI] [PubMed] [Google Scholar]
- Sroufe LA. Psychopathology as an outcome of development. Development and Psychopathology. 1997;9(2):251–268. doi: 10.1017/s0954579497002046. [DOI] [PubMed] [Google Scholar]
- Tackett JL, Lahey BB, van Hulle C, Waldman I, Krueger RF, Rathouz PJ. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. Journal of Abnormal Psychology. 2013;122(4):1142–1153. doi: 10.1037/a0034151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tolan PH, Henry D. Patterns of psychopathology among urban poor children: Comorbidity and aggression effects. Journal of Consulting and Clinical Psychology. 1996;64(5):1094–1099. doi: 10.1037//0022-006x.64.5.1094. [DOI] [PubMed] [Google Scholar]
- Treadway MT, Zald DH. Translational models of dopaminergic mechanisms for motivational deficits in anhedonic patients. In: Ritsner MS, editor. Anhedonia: A Comprehensive Handbook (Vol. 1: Conceptual Issues and Neurobiological Advances) New York, NY: Springer; 2014. pp. 107–117. [Google Scholar]
- Vaidyanathan U, Patrick CJ, Iacono WG. Patterns of comorbidity among mental disorders: A person-centered approach. Comprehensive Psychiatry. 2011;52(5):527–35. doi: 10.1016/j.comppsych.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Lier PAC, Koot HM. Developmental cascades of peer relations and symptoms of externalizing and internalizing problems from kindergarten to fourth-grade elementary school. Development and Psychopathology. 2010;22(3):569–582. doi: 10.1017/S0954579410000283. [DOI] [PubMed] [Google Scholar]
- Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976;41(3):321–327. [Google Scholar]
- Verhulst FC, Althaus M. Persistence and change in behavioral/emotional problems reported by parents of children aged 4–14: An epidemiological study. Acta Psychiatrica Scandinavica. 1988;77:1–28. doi: 10.1111/j.1600-0447.1988.tb10567.x. [DOI] [PubMed] [Google Scholar]
- Weiss B, Süsser K, Catron T. Common and specific features of childhood psychopathology. Journal of Abnormal Psychology. 1998;107(1):118–127. doi: 10.1037//0021-843x.107.1.118. [DOI] [PubMed] [Google Scholar]
- Werthamer-Larsson L, Kellam S, Wheeler L. Effect of first-grade classroom environment on shy behavior, aggressive behavior, and concentration problems. American Journal of Community Psychology. 1991;19(4):585–602. doi: 10.1007/BF00937993. [DOI] [PubMed] [Google Scholar]
- Whittle S, Allen NB, Lubman DI, Yücel M. The neurobiological basis of temperament: Towards a better understanding of psychopathology. Neuroscience & Biobehavioral Reviews. 2006;30(4):511–525. doi: 10.1016/j.neubiorev.2005.09.003. [DOI] [PubMed] [Google Scholar]
- Yang CC. Evaluating latent class analysis models in qualitative phenotype identification. Computational Statistics & Data Analysis. 2006;50(4):1090–1104. [Google Scholar]
- Yoo JP, Brown PJ, Luthar SS. Children with co-occurring anxiety and externalizing disorders: Family risks and implications for competence. American Journal of Orthopsychiatry. 2009;79(4):532–540. doi: 10.1037/a0017848. [DOI] [PMC free article] [PubMed] [Google Scholar]