Abstract
OBJECTIVE
We investigated the association of cardiovascular risk factors and myocardial fibrosis with early cardiac dysfunction in type 1 diabetes.
RESEARCH DESIGN AND METHODS
Participants with type 1 diabetes aged 13–39 years without a known history of cardiovascular disease (CVD) (n = 1,441) were recruited into the Diabetes Control and Complications Trial (1983–1993) and subsequently followed in the Epidemiology of Diabetes Interventions and Complications study (1994 to present). Seven hundred fourteen participants underwent cardiac magnetic resonance (CMR) imaging (2007–2009) with late gadolinium enhancement sequences to assess ischemic and nonischemic scars and tagging sequences to evaluate circumferential strain. CMR-derived T1 mapping also was used to assess interstitial fibrosis. The influence of cardiovascular risk factors and myocardial scar on circumferential strain was assessed using linear regression.
RESULTS
Circumferential dysfunction was consistently associated with older age, male sex, smoking history, obesity, higher blood pressure, lower HDL cholesterol, and higher mean HbA1c. Participants with nonischemic scars (n = 16) had the worst circumferential function compared with those without scars (β ± SE 1.32 ± 0.60; P = 0.03). In sex-adjusted models, the correlation between T1 times and circumferential strain was not significant. In the fully adjusted models, a trend toward circumferential dysfunction in participants with nonischemic scars was found. Left ventricular ejection fraction was not associated with risk factors but was significantly lower if a myocardial scar was present.
CONCLUSIONS
Traditional CVD risk factors and elevated HbA1c levels are major factors related to early cardiac dysfunction in type 1 diabetes. Nonischemic myocardial scar, possibly as a marker of chronic exposure to known risk factors, may predict early cardiac dysfunction mediated by diffuse myocardial fibrosis as seen in diabetic cardiomyopathy.
Introduction
Diabetes is strongly associated with the incidence and progression of heart failure (HF), although this relationship is not as well studied for type 1 compared with type 2 diabetes (1). The high risk of HF in patients with diabetes is partly explained by the elevated risk of coronary artery disease but may also be related to the presence of diabetic cardiomyopathy (DCM) (2). Controversy exists about the role of diabetes as a cardiomyopathic entity (3–5), but myocardial fibrosis appears to contribute importantly to both ischemic and diabetic heart disease (6). However, whether established risk factors of HF affect early subclinical cardiac dysfunction in individuals with type 1 diabetes is unclear.
Cardiac magnetic resonance (CMR) techniques allow for the assessment of replacement (scar) and diffuse myocardial fibrosis, identifying distribution patterns and estimating the amount of extension in the heart. In the presence of a myocardial scar, CMR may also identify patterns of nonischemic and ischemic myocardial disease, which have been associated with an unfavorable prognosis in patients with diabetes (7,8).
The assessment of left ventricular (LV) myocardial deformation (strain) by CMR tagging has been validated in diverse populations and shown to be robust and reproducible (9). In addition, strain measurements may be more sensitive to changes in contractile function during the early phases of DCM than traditional parameters of cardiac function (10).
We investigated the influence of cardiovascular risk factors on early cardiac dysfunction, as measured by cardiac strain, in patients with type 1 diabetes participating in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) study. We also assessed how measures of myocardial fibrosis affect these relationships by investigating the association of myocardial scar and diffuse fibrosis with circumferential strain.
Research Design and Methods
Study Sample
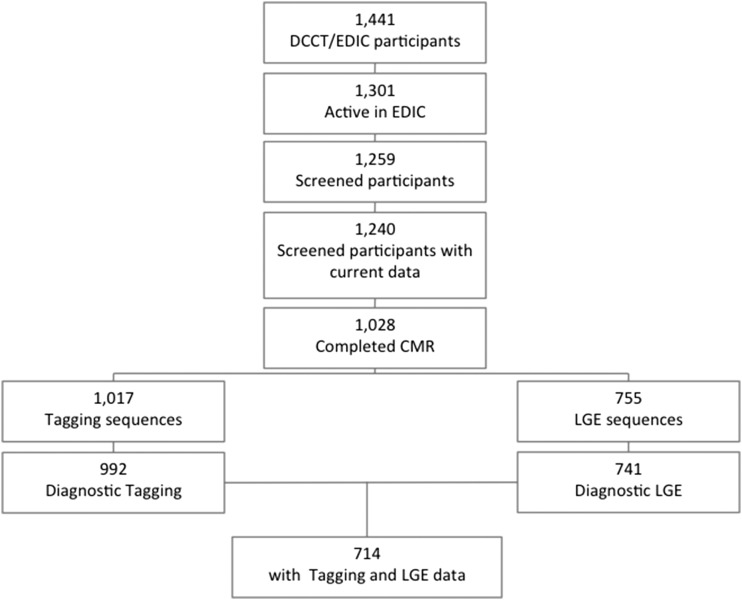
The DCCT/EDIC study has been previously described in detail (11,12). Briefly, between 1983 and 1989, the DCCT recruited 1,441 patients (aged 13–39 years) with type 1 diabetes who were free of cardiovascular disease (CVD), hypertension, and hypercholesterolemia. DCCT participants were randomly assigned to either intensive or conventional diabetes treatment (1983–1993). The EDIC study (1994 to present) is the observational follow-up of the DCCT cohort. We included EDIC participants who had contrast-enhanced CMR examinations during the 14th year of the EDIC study, with an average total (DCCT and EDIC) follow-up of 21 years. A total of 1,301 participants (94% of the surviving DCCT cohort) were active in EDIC at the time of the CMR assessment. Of those, 714 had complete data on cardiovascular risk factors and the main parameters of CMR (12). Participant selection procedures are summarized in Fig. 1. Institutional review committees of all participating centers (www.nejm.org/doi/full/10.1056/nejmoa1409463#t=article) approved the study, and all participants gave informed consent.
Figure 1.
DCCT/EDIC study participant selection.
Assessment of Cardiac Risk Factors
The methods used to characterize complications and risk factors have been described in detail (13). In brief, during the DCCT and EDIC, all participants underwent a complete evaluation annually that included measurements of blood pressure (BP), weight, height, and serum creatinine level and an electrocardiogram. HbA1c was measured by high-performance liquid chromatography every 3 months during DCCT and annually during the EDIC study. Albumin excretion rates and fasting lipid levels were measured annually during DCCT and in alternate years during EDIC. Hypertension was defined as BP ≥140/90 mmHg or use of an antihypertensive medication. Hypercholesterolemia was defined as LDL cholesterol ≥130 mg/dL or use of a lipid-lowering medication.
CMR Protocol
The CMR protocol in EDIC has been described (7). In summary, a uniform CMR protocol was performed at 27 centers between July 2007 and April 2009 that used 1.5-T magnets in 26 centers and a 3-T magnet in 1 center (Espree or Avanto [Siemens Medical Systems, Erlangen, Germany], Intera [Philips Medical Systems, Best, the Netherlands], or SIGNA [GE Medical Systems, Waukesha, WI]). The general CMR protocol included CMR tagging sequences. Late gadolinium enhancement (LGE) was performed by using a 0.15–0.20 mmol/kg dose of gadopentetate dimeglumine (Magnevist; Bayer Healthcare Pharmaceuticals, Whippany, NJ) as the contrast agent. Participants with an estimated glomerular filtration rate <60 mL · min−1 · 1.73 m−2, a history of dialysis or renal transplantation, or a known allergy to gadolinium were not recruited to the LGE protocol. Experienced readers masked to treatment assignment and participant clinical information analyzed all CMR examinations for cardiac structure and function (e.g., LV mass, volumes, ejection fraction) in a central reading center. In addition, the readers performed 100 reanalyzes to calculate intraclass correlation (0.917–0.978) for the cardiac function variables, as previously described (7).
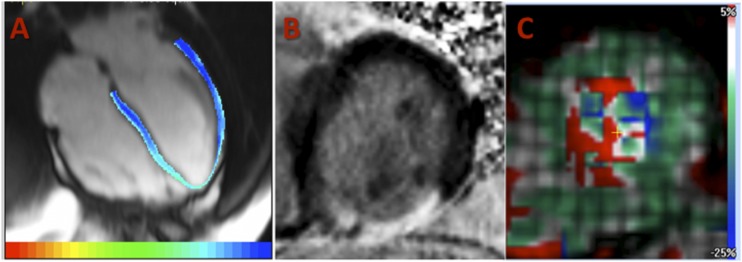
CMR LGE
LGE CMR sequences were used to assess LV replacement fibrosis (scar). Myocardial scar was defined as focal enhancement either in two adjacent short-axis images or in one short-axis image and a long-axis image at a corresponding location and then classified into two categories (types): 1) ischemic when involving the subendocardium in a coronary artery territory or 2) nonischemic when involving predominantly the midwall or subepicardial location without subendocardial involvement in a noncoronary distribution (Fig. 2) (7). The percentage of LV scar was calculated by dividing scar mass by total LV mass (7).
Figure 2.
Images from the CMR protocol in the DCCT/EDIC study. A: T1 mapping assessment of the LV from a four-chamber view using a TI scout Look-Locker sequence. B: LGE image in a short-axis view of the LV (presence of transmural scar in the inferior wall). C: Assessment of LV deformation (strain map) from tagging sequences in a midventricular short-axis view.
CMR T1 Mapping
CMR sequence–acquired T1 mapping images were used to assess diffuse fibrosis in participants without evidence of myocardial scar in LGE images (Fig. 2). We included participants who underwent TI scout scans with 1.5-T scanners after the infusion of gadolinium-based contrast agent. A detailed description of the protocol has been previously reported (14). Briefly, TI scout images were obtained by true fast imaging with steady-state free precession Look-Locker acquisition sequences in four-chamber images or LV midventricle short-axis views. Images were analyzed using MASS research software (MASS V2010-EXP; Leiden University Medical Center, Leiden, the Netherlands). The postcontrast T1 times were then normalized according to the gadolinium dose, glomerular filtration rate, and infusion-acquisition delay times (14). Lower T1 times are associated with higher diffuse fibrosis.
CMR Tagging Protocol
Tagging CMR assessed LV strain through a standard protocol (9) (Fig. 2). Tagged images were acquired from short-axis slices at the LV base, mid, and apex. Circumferential strain was acquired from 12 segments and three slices in each study by using the harmonic phase technique. Peak systolic circumferential strain (Ecc) at the midventricular level was acquired by averaging four segments. By convention, Ecc values are negative during systole with circumferential shortening. Thus, a less-negative Ecc value indicates diminished regional LV function.
Statistical Analysis
Sex-specific clinical and CMR-derived measures were assessed. The distribution of Ecc was individually assessed according to sex, age, treatment group (intensive/conventional), study cohort (primary/secondary), smoking status, alcohol use, obesity status (BMI ≥ or <30 kg/m2), renal dysfunction parameters, hypertension, lipids profile, metabolic syndrome criteria, and presence/type of myocardial scar (Supplementary Data). Spearman correlation was used to evaluate the association between diffuse fibrosis assessed by T1 values and Ecc, adjusting for sex. For myocardial scar, the presence (binary: yes/no) and the type of scar (two patterns: ischemic and nonischemic) were assessed as independent variables. The associations between covariates and circumferential deformation (Ecc as the dependent variable) were assessed using minimally adjusted linear regression models, which included a basic model and minimally adjusted risk factor models. Finally, a multivariate linear regression model that tested the influence of cardiovascular risk factors and myocardial scar on Ecc and LV ejection fraction values was assessed, adjusting for anthropometrics, cardiovascular risk factors, and presence/type of myocardial scar.
Results
Of the 1,017 DCCT/EDIC study participants who underwent diagnostic CMR imaging, 714 were included in the analysis. The mean age of the included participants was 49 years; 42% were female; and the mean duration of type 1 diabetes was 28 years (Supplementary Table 1).
Circumferential deformation was worse (less-negative Ecc values) in participants who were male, older, smokers, and obese and with hypertension, hypercholesterolemia, the metabolic syndrome, proliferative diabetic retinopathy, and impaired renal function (Table 1). These relationships were consistent in all age strata, although the differences between men and women tended to converge in the oldest age-groups (Supplementary Fig. 1). Compared with women, men had greater LV mass, a higher prevalence of myocardial scar, and more interstitial fibrosis as measured by postcontrast T1 times (Supplementary Table 1).
Table 1.
Distribution of LV circumferential strain
| n | Ecc (%) | P value | |
|---|---|---|---|
| Sex | |||
| Female | 303 | −19.2 ± 2.4 | |
| Male | 411 | −18.3 ± 2.4 | <0.0001 |
| Age | |||
| <50 years | 390 | −18.9 ± 2.4 | |
| ≥50 years | 324 | −18.4 ± 2.4 | 0.0064 |
| Treatment group | |||
| Intensive | 371 | −18.8 ± 2.4 | |
| Conventional | 343 | −18.6 ± 2.4 | 0.3183 |
| Study cohort | |||
| Primary | 353 | −18.8 ± 2.4 | |
| Secondary | 361 | −18.6 ± 2.4 | 0.2351 |
| Current smoker | |||
| No | 631 | −18.8 ± 2.4 | |
| Yes | 83 | −18.1 ± 2.6 | 0.0097 |
| Alcohol | |||
| No | 385 | −18.7 ± 2.5 | |
| Yes | 329 | −18.7 ± 2.3 | 0.4766 |
| BMI ≥30 kg/m2 | |||
| No | 488 | −18.9 ± 2.4 | |
| Yes | 226 | −18.3 ± 2.4 | 0.0025 |
| AER ≥300 μg/min or ESRD | |||
| No | 679 | −18.7 ± 2.4 | |
| Yes | 35 | −17.8 ± 2.2 | 0.0150 |
| Sustained AER ≥30 μg/min or ESRD | |||
| No | 565 | −18.8 ± 2.4 | |
| Yes | 149 | −18.2 ± 2.5 | 0.0030 |
| Any proliferative diabetic retinopathy* | |||
| No | 596 | −18.8 ± 2.4 | |
| Yes | 118 | −18.2 ± 2.5 | 0.0256 |
| Hypertension† | |||
| No | 373 | −19.0 ± 2.3 | |
| Yes | 341 | −18.4 ± 2.4 | 0.0004 |
| Hypercholesterolemia‡ | |||
| No | 248 | −19.0 ± 2.4 | |
| Yes | 466 | −18.5 ± 2.4 | 0.0030 |
| Metabolic syndrome§ | |||
| No | 460 | −18.9 ± 2.4 | |
| Yes | 226 | −18.1 ± 2.4 | <0.0001 |
| Myocardial scar | |||
| None | 682 | −18.7 ± 2.4 | |
| Any | 32 | −17.7 ± 2.7 | 0.0294 |
| Ischemic | 16 | −18.4 ± 2.7 | 0.0205 |
| Nonischemic | 16 | −17.0 ± 2.4 | (df = 2) |
Data are mean ± SD unless otherwise indicated. More-negative Ecc values indicate more myocardial circumferential deformation. AER, albumin excretion rate; ESRD, end-stage renal disease.
*During the DCCT/EDIC study.
†Defined as BP ≥140/90 mmHg or treatment with an antihypertensive medication.
‡Defined as LDL ≥130 mg/dL or treatment with a lipid-lowering medication.
§Defined as at least two of the four components: systolic BP ≥130 mmHg or diastolic BP ≥85 mmHg or any antihypertensive agent, including ACE/angiotensin receptor blocker for all reasons, female waist circumference ≥88 cm or male waist circumference ≥102 cm, female HDL cholesterol <50 mg/dL or male HDL cholesterol <40 mg/dL, and triglycerides ≥150 mg/dL.
Worse circumferential deformation was also found in participants with poor glycemic control and in the presence of myocardial scar (Table 1). Participants with nonischemic myocardial scars had less circumferential deformation (less-negative Ecc values) compared with those with ischemic scars. In sex-adjusted models, the correlation between T1 times and Ecc was not significant (β ± SE −0.002 ± 0.003 ms/%; P = 0.55).
The minimally adjusted linear regression models are shown in Table 2. Consistently, female sex was associated with more circumferential deformation (more-negative Ecc values) than male sex. Older participants had less circumferential deformation, although this relationship was attenuated in the fully adjusted model. When risk factors were individually added to the basic model, smoking, obesity, elevated BP, worse metabolic profile, higher HbA1c, proliferative diabetic retinopathy, and renal dysfunction were consistently associated with less circumferential deformation (less-negative Ecc values). However, LV mass was not a significant predictor of circumferential deformation when included in the basic model. The presence of myocardial scar was associated with marginal significance (P = 0.09) with circumferential dysfunction when added to the basic model, and the association became significant (P = 0.027) when participants with nonischemic scars were compared with those without scars. The amount of diffuse fibrosis assessed by T1 times was not a significant predictor of circumferential dysfunction when added to the basic model.
Table 2.
Minimally adjusted linear regression of circumferential strain (Ecc, %) in relation to cardiovascular risk factors
| Covariate | Estimate of β ± SE | P value |
|---|---|---|
| Basic model1 | ||
| Age (per 10 years of age) | 0.26 ± 0.13 | 0.0498 |
| Sex (female vs. male) | −0.86 ± 0.18 | <0.0001 |
| Cohort (primary vs. secondary intervention) | −0.12 ± 0.18 | 0.4906 |
| Minimally adjusted risk factor models2 (basic model + 1 covariate) | ||
| Group (intensive vs. conventional) | −0.18 ± 0.18 | 0.2997 |
| Smoking (yes vs. no) | 0.68 ± 0.27 | 0.0125 |
| BMI (kg/m2) | 0.08 ± 0.02 | <0.0001 |
| BMI ≥30 kg/m2 (yes vs. no) | 0.64 ± 0.19 | 0.0008 |
| Natural waist circumference (cm) | 0.03 ± 0.01 | <0.0001 |
| Mean systolic BP (mmHg) | 0.04 ± 0.01 | 0.0007 |
| Mean diastolic BP (mmHg) | 0.09 ± 0.02 | <0.0001 |
| Hypertension (yes vs. no) | 0.50 ± 0.18 | 0.0055 |
| Mean HDL cholesterol (mg/dL) | −0.02 ± 0.01 | 0.0014 |
| Mean LDL cholesterol (mg/dL) | 0.01 ± 0.004 | 0.0070 |
| Mean total cholesterol (mg/dL) | 0.01 ± 0.004 | 0.0326 |
| Mean triglycerides (mg/dL) | 0.01 ± 0.002 | <0.0001 |
| Hypercholesterolemia (yes vs. no) | 0.21 ± 0.19 | 0.2808 |
| HbA1c (%) | ||
| Before CMR | 0.28 ± 0.07 | 0.0002 |
| Mean during DCCT | 0.14 ± 0.07 | 0.0397 |
| Mean during the EDIC study | 0.37 ± 0.09 | <0.0001 |
| Mean during the DCCT/EDIC study | 0.38 ± 0.10 | <0.0001 |
| Metabolic syndrome (yes vs. no) | 0.81 ± 0.19 | <0.0001 |
| Sustained AER ≥30 μg/min or ESRD (yes vs. no) | 0.61 ± 0.22 | 0.0055 |
| Any PDR (yes vs. no) | 0.58 ± 0.24 | 0.0169 |
| AER ≥300 μg/min or ESRD (yes vs. no) | 0.69 ± 0.41 | 0.0915 |
| LV end-diastolic mass (g) | 0.004 ± 0.004 | 0.2993 |
| LV end-diastolic mass/BSA | 0.001 ± 0.008 | 0.8725 |
| Myocardial scar | ||
| Any scar (ischemic or nonischemic) vs. none | 0.73 ± 0.43 | 0.0904 |
| Nonischemic vs. none | 1.32 ± 0.60 | 0.0274 |
| Ischemic vs. none | 0.14 ± 0.59 | 0.8156 |
| Nonischemic vs. ischemic | 1.18 ± 0.83 | 0.1544 |
| Normalized myocardial T1 (ms) (n = 200) | −0.002 ± 0.003 | 0.5515 |
Positive regression coefficients indicate a decrease in function because Ecc has a negative value. Normalized myocardial T1: postcontrast CMR-derived T1 times were normalized by gadolinium dose, glomerular filtration rate, and infusion-acquisition delay times. Lower values are related to higher diffuse fibrosis. AER, albumin excretion rate; BSA, body surface area; ESRD, end-stage renal disease; PDR, proliferative diabetic retinopathy.
1Basic model was also adjusted for CMR machine type.
2Minimally adjusted model, separate model for each covariate, was also adjusted for age, sex, primary vs. secondary cohort, and CMR machine type.
The multivariate regression model for circumferential strain and ejection fraction is shown in Table 3. Less circumferential shortening (less-negative Ecc values) was associated with older age, male sex, smoking, higher BMI, higher BP, lower HDL cholesterol, and higher HbA1c mean values during the cohort follow-up period. A trend in significance showed less circumferential deformation in participants with nonischemic myocardial scars compared with those without scars. LV ejection fraction was not associated with cardiovascular risk factors. However, compared with those without myocardial scar, ejection fraction was significantly lower in participants with either ischemic or nonischemic myocardial scars.
Table 3.
Multivariate linear regression of LV circumferential strain and ejection fraction in relation to cardiovascular risk factors
| Ecc (%) |
Ejection fraction (%) |
|||
|---|---|---|---|---|
| Covariate | β ± SE | P value | β ± SE | P value |
| Age (per 10 years of age) | 0.30 ± 0.13 | 0.0236 | 0.80 ± 0.35 | 0.0226 |
| Sex (female vs. male) | −0.44 ± 0.20 | 0.0318 | 1.77 ± 0.54 | 0.0012 |
| Cohort (primary vs. secondary intervention) | −0.15 ± 0.17 | 0.3926 | 0.34 ± 0.46 | 0.4592 |
| Smoking (yes vs. no) | 0.64 ± 0.27 | 0.0188 | −0.16 ± 0.72 | 0.8184 |
| BMI (kg/m2) | 0.04 ± 0.02 | 0.0367 | 0.05 ± 0.05 | 0.3832 |
| Mean diastolic BP (mmHg) | 0.07 ± 0.02 | 0.0002 | 0.02 ± 0.05 | 0.7521 |
| Mean HDL cholesterol (mg/dL) | −0.02 ± 0.008 | 0.0236 | 0.02 ± 0.02 | 0.2383 |
| Mean HbA1c during the DCCT/EDIC study | 0.28 ± 0.10 | 0.0043 | −0.20 ± 0.26 | 0.4343 |
| Myocardial scar | ||||
| Nonischemic vs. none | 1.13 ± 0.58 | 0.0518 | −8.93 ± 1.54 | <0.0001 |
| Ischemic vs. none | −0.04 ± 0.58 | 0.9506 | −3.67 ± 1.53 | 0.0164 |
Only the most significant lipid variable (i.e., HDL cholesterol) was included in the final model. The model was also adjusted for CMR machine type. Positive regression coefficients indicate a decrease in function because Ecc has a negative value. Boldface values indicate significance or clear trend at P ≤ 0.05.
Conclusions
This study investigated a large unique cohort of subjects with type 1 diabetes from the DCCT/EDIC study with more than two decades of follow-up who underwent a comprehensive CMR assessment. The CMR analyses included functional measures, deformation evaluation, myocardial scar identification and classification, and diffuse fibrosis quantification. In addition to the expected influence of age and sex, we show that smoking, obesity, high BP, the presence of the metabolic syndrome, and chronic high glucose levels are the main factors related to early subclinical cardiac dysfunction as assessed by circumferential deformation. The presence of myocardial scar, although infrequent, may also play a role in the cardiac dysfunction of this population, particularly in the presence of a nonischemic pattern.
This study includes data on cardiac deformation as measured by LV strain by using a validated technique that is available in clinical settings (15). The results show small differences for strain values between groups. Small differences in LV deformation are expected in groups of generally healthy participants without known clinical CVD. LV strain allows for early identification of subclinical cardiac dysfunction and relates to future clinical events (16,17). The ability to detect early dysfunction may lead to preventive strategies through clinical decision making.
Although risk factors related to the late clinical manifestation of HF are well known, we now show determinants of early subclinical cardiac dysfunction in a large cohort of participants with type 1 diabetes. These findings demonstrated that LV ejection fraction was not related to clinical risk factors but was lower when more advanced disease (as assessed by the presence of myocardial scar) was present. The findings indicate that known risk factors of cardiovascular outcomes in the general population similarly affect early cardiac dysfunction in type 1 diabetes and support approaches for primary prevention of CVD in this population.
We found that obesity and high BP were among the main factors related to early subclinical cardiac dysfunction in type 1 diabetes as assessed by circumferential deformation, which is consistent with previous studies in generally healthy populations that found obesity and hypertension to be related to cardiac measures, early ventricular dysfunction, and hard clinical events that start in early adulthood (18–20). Furthermore, increases in BMI and BP are main determinants of cardiac remodeling over decades of adulthood (21,22). In fact, more severe obesity appears to be implicated with hospitalization for HF in patients with type 1 diabetes (23). Smoking, particularly current smoking status, is known to be related to incident clinical HF (24). In the current study, smoking status also is a determinant of early subclinical LV dysfunction in type 1 diabetes.
Over the past three decades, the DCCT/EDIC study has documented the impact of chronic hyperglycemia on adverse outcomes in participants with type 1 diabetes (13,25). In fact, glycemic exposure appears to be a major determinant of cardiac remodeling in type 1 diabetes (26). In the current study, we found that early subclinical cardiac dysfunction in type 1 diabetes is associated with a worse lipid profile and hyperglycemia. The Swedish National Diabetes Registry assessed 20,985 patients with type 1 diabetes and found that having an HbA1c ≥10.5% increased the risk of developing clinically manifested HF by approximately fourfold compared with a well-controlled group (HbA1c <6.5%) (27). Similarly, Konduracka et al. (28) reported that longer diabetes duration and increased HbA1c levels are predictors of clinical HF in longstanding (≥10 years) type 1 diabetes. The current findings support the role of exposure to chronic hyperglycemia as a major determinant of preclinical cardiac dysfunction in type 1 diabetes. Of note, we show that the mean glucose levels over a long-term follow-up affect early cardiac dysfunction in patients with type 1 diabetes. These findings highlight the importance in clinical practice of pursuing optimal glucose control in patients with type 1 diabetes.
The difference between the DCCT treatment groups in the current study essentially reflects the long-term effects of the 2% difference in HbA1c that was maintained over an average of 6.5 years. Thus, the lack of a difference between groups reflects the weak association of the mean HbA1c over those 6.5 years of the DCCT with the CMR Ecc parameter measured 14–16 years later in the EDIC study (P = 0.04) (Table 2). In this case, the analysis of HbA1c as a quantitative variable will have greater power (smaller P value) than the qualitative treatment group comparison. Furthermore, the DCCT HbA1c is different from the weighted mean HbA1c that reflects the glycemic exposure over the total 20.5–22.5 years of follow-up that shows a strong association with Ecc (P < 0.0001). Thus, the difference between DCCT treatment groups and the DCCT HbA1c did not have a long-term effect on CMR parameters, but the overall glycemic exposure over the 20.5–22.5 years had a strong association.
Patients with type 1 diabetes are at a high risk for coronary artery disease and are therefore susceptible to ischemic cardiomyopathy (ICM) (29). In fact, both ICM and DCM share some of the same risk factors, such as smoking, hypertension, hyperlipidemia, and hyperglycemia (30,31). The presence of DCM often is a diagnosis of exclusion in patients with diabetes and clinical HF (2).
The pathophysiological mechanisms for DCM are still not clear, but myocardial fibrosis seems to be an underlying contributor in the early stages (6). Myocardial fibrosis relates to both ICM and DCM and may be seen in various histological presentations (32,33). Diffuse fibrosis seems to appear early with chronic cardiac exposure to risk factors (32,34). DCCT/EDIC study participants were shown to have higher LV diffuse fibrosis compared with low-risk volunteers without diabetes in a previous study (14). In the current study, however, T1 times (as a measure of diffuse fibrosis) did not relate to early cardiac dysfunction as assessed by circumferential deformation. The distribution of T1 times possibly is not adequate to identify small differences in the presence of diffuse fibrosis in the DCCT/EDIC study population because all participants have longstanding type 1 diabetes, which is related to increased fibrosis. In addition, the method of acquisition used in this study is not optimal, and superior methods for T1 and extracellular space quantification have been developed (34).
DCM also has been related to microangiopathy in patients with diabetes (35). In fact, this study shows that proliferative diabetic retinopathy, a known marker of diabetes-related microangiopathy, is associated with subclinical impaired deformation (Tables 1 and 2). The myocardial scar (replacement fibrosis) pattern assessed by CMR may help to differentiate the underlying etiologies for myocardial damage and identify the stage of progression of cardiac diseases (32). In a previous report by Turkbey et al. (7), myocardial scar was identified in 4.3% of the DCCT/EDIC study participants included in the LGE protocol. Scars could be further classified as nonischemic or ischemic, with one-half in each category.
In the current analysis, the presence of myocardial scar was significantly associated with circumferential deformation, particularly in participants with a nonischemic scar pattern. Nonischemic scar is a probable indicator of advanced stages of diffuse disease and a possible indicator of relevant cardiac damage seen in preclinical phases of DCM. This relationship was substantially attenuated when multivariate regression models included clinical risk factors. These findings suggest that the relationship between myocardial scar and cardiac dysfunction may be mediated by chronic exposure to known risk factors.
In summary, we assessed a large cohort of participants with type 1 diabetes with a comprehensive CMR assessment and found that older age, male sex, smoking, obesity, high BP, the presence of the metabolic syndrome, and chronic high glucose levels are the main factors related to early subclinical cardiac dysfunction in this population. Myocardial scar also appears to relate to early cardiac dysfunction, is influenced by chronic exposure to known risk factors, and is an indicator of advanced diffuse cardiac damage as seen in DCM.
Supplementary Material
Article Information
Acknowledgments. The authors thank Wanyu Hsu, Biostatistics Center, The George Washington University, for data processing and technical assistance and David M. Nathan, editor for DCCT/EDIC study publications, for help with the preparation of the manuscript.
Funding. This work was supported by cooperative agreement grants (1982–1993, 2012–2017) and contracts (1982–2012) with the Division of Diabetes Endocrinology and Metabolic Diseases of the National Institute of Diabetes and Digestive and Kidney Diseases (current grant numbers U01-DK-094176 and U01-DK-094157) and by the National Eye Institute, the National Institute of Neurological Disorders and Stroke, the General Clinical Research Centers Program (1993–2007), and the Clinical Translational Science Center Program (2006 to present), Bethesda, MD. A.C.A. was funded by Universidade Federal do Vale do São Francisco and by Johns Hopkins University.
Duality of Interest. Industry contributors have had no role in the DCCT/EDIC study but have provided free or discounted supplies or equipment to support participants’ adherence to the study: Abbott Diabetes Care (Alameda, CA), Animas (West Chester, PA), Bayer Diabetes Care (North America Headquarters, Tarrytown, NY), Becton Dickinson (Franklin Lakes, NJ), Eli Lilly (Indianapolis, IN), Extend Nutrition (St. Louis, MO), Insulet Corporation (Bedford, MA), LifeScan (Milpitas, CA), Medtronic Diabetes (Minneapolis, MN), Nipro Home Diagnostics (Ft. Lauderdale, FL), Nova Diabetes Care (Billerica, MA), Omron (Shelton, CT), Perrigo Diabetes Care (Allegan, MI), Roche Diabetes Care (Indianapolis, IN), and Sanofi (Bridgewater, NJ). No other potential conflicts of interest relevant to this article were reported.
Author Contributions. A.C.A. contributed to the study conception and design, data analysis and interpretation, and drafting of the manuscript. B.A.-V., E.T., S.D., and E.C. contributed to the study conception and design, data interpretation, and critical revision of the manuscript for important intellectual content. J.-Y.B., P.C., J.L., D.A.B., and J.A.C.L. contributed to the study conception and design, data analysis and interpretation, and critical revision of the manuscript for important intellectual content. A.C.A. and J.A.C.L. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the American Heart Association Scientific Sessions, Chicago, IL, 15–19 November 2014.
Footnotes
Clinical trial reg. nos. NCT00360893 and NCT00360815, clinicaltrials.gov.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-1889/-/DC1.
A complete list of participants in the DCCT/EDIC Research Group can be found at www.nejm.org/doi/full/10.1056/nejmoa1409463#t=article.
References
- 1.Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA 1979;241:2035–2038 [DOI] [PubMed] [Google Scholar]
- 2.Tarquini R, Lazzeri C, Pala L, Rotella CM, Gensini GF. The diabetic cardiomyopathy. Acta Diabetol 2011;48:173–181 [DOI] [PubMed] [Google Scholar]
- 3.Karamitsos TD, Tsapas A, Arnold JR. Diabetic cardiomyopathy: a controversial entity. Eur Heart J 2008;29:564; author reply 565 [DOI] [PubMed] [Google Scholar]
- 4.Rijzewijk LJ, van der Meer RW, Lamb HJ, et al. . Altered myocardial substrate metabolism and decreased diastolic function in nonischemic human diabetic cardiomyopathy: studies with cardiac positron emission tomography and magnetic resonance imaging. J Am Coll Cardiol 2009;54:1524–1532 [DOI] [PubMed] [Google Scholar]
- 5.Fagan A, Asghar O, Pearce K, et al. . Medalists with extreme duration of type 1 diabetes exhibit only mild diastolic dysfunction and myocardial fibrosis. Diabetes Care 2015;38:e5–e6 [DOI] [PubMed] [Google Scholar]
- 6.Jellis C, Wright J, Kennedy D, et al. . Association of imaging markers of myocardial fibrosis with metabolic and functional disturbances in early diabetic cardiomyopathy. Circ Cardiovasc Imaging 2011;4:693–702 [DOI] [PubMed] [Google Scholar]
- 7.Turkbey EB, Backlund JY, Genuth S, et al.; DCCT/EDIC Research Group . Myocardial structure, function, and scar in patients with type 1 diabetes mellitus. Circulation 2011;124:1737–1746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwong RY, Sattar H, Wu H, et al. . Incidence and prognostic implication of unrecognized myocardial scar characterized by cardiac magnetic resonance in diabetic patients without clinical evidence of myocardial infarction. Circulation 2008;118:1011–1020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castillo E, Osman NF, Rosen BD, et al. . Quantitative assessment of regional myocardial function with MR-tagging in a multi-center study: interobserver and intraobserver agreement of fast strain analysis with harmonic phase (HARP) MRI. J Cardiovasc Magn Reson 2005;7:783–791 [DOI] [PubMed] [Google Scholar]
- 10.Karamitsos TD, Karvounis HI, Didangelos T, Parcharidis GE, Karamitsos DT. Impact of autonomic neuropathy on left ventricular function in normotensive type 1 diabetic patients: a tissue Doppler echocardiographic study. Diabetes Care 2008;31:325–327 [DOI] [PubMed] [Google Scholar]
- 11.The DCCT Research Group The Diabetes Control and Complications Trial (DCCT). Design and methodologic considerations for the feasibility phase. Diabetes 1986;35:530–545 [PubMed] [Google Scholar]
- 12.Epidemiology of Diabetes Interventions and Complications (EDIC) Epidemiology of Diabetes Interventions and Complications (EDIC). Design, implementation, and preliminary results of a long-term follow-up of the Diabetes Control and Complications Trial cohort. Diabetes Care 1999;22:99–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nathan DM, Bayless M, Cleary P, et al.; DCCT/EDIC Research Group . Diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: advances and contributions. Diabetes 2013;62:3976–3986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gai N, Turkbey EB, Nazarian S, et al. . T1 mapping of the gadolinium-enhanced myocardium: adjustment for factors affecting interpatient comparison. Magn Reson Med 2011;65:1407–1415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donekal S, Ambale-Venkatesh B, Berkowitz S, et al. . Inter-study reproducibility of cardiovascular magnetic resonance tagging. J Cardiovasc Magn Reson 2013;15:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Choi EY, Rosen BD, Fernandes VR, et al. . Prognostic value of myocardial circumferential strain for incident heart failure and cardiovascular events in asymptomatic individuals: the Multi-Ethnic Study of Atherosclerosis. Eur Heart J 2013;34:2354–2361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ambale-Venkatesh B, Armstrong AC, Liu CY, et al. . Diastolic function assessed from tagged MRI predicts heart failure and atrial fibrillation over an 8-year follow-up period: the Multi-Ethnic Study of Atherosclerosis. Eur Heart J Cardiovasc Imaging 2014;15:442–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Armstrong AC, Jacobs DR Jr, Gidding SS, et al. Framingham score and LV mass predict events in young adults: CARDIA study. Int J Cardiol 2014;172:350–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kishi S, Armstrong AC, Gidding SS, et al. . Association of obesity in early adulthood and middle age with incipient left ventricular dysfunction and structural remodeling: the CARDIA study (Coronary Artery Risk Development in Young Adults). JACC Heart Fail 2014;2:500–508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Armstrong AC, Liu K, Lewis CE, et al. . Left atrial dimension and traditional cardiovascular risk factors predict 20-year clinical cardiovascular events in young healthy adults: the CARDIA study. Eur Heart J Cardiovasc Imaging 2014;15:893–899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Armstrong AC, Gidding SS, Colangelo LA, et al. . Association of early adult modifiable cardiovascular risk factors with left atrial size over a 20-year follow-up period: the CARDIA study. BMJ Open 2014;4:e004001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gidding SS, Liu K, Colangelo LA, et al. . Longitudinal determinants of left ventricular mass and geometry: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Circ Cardiovasc Imaging 2013;6:769–775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vestberg D, Rosengren A, Olsson M, Gudbjörnsdottir S, Svensson AM, Lind M. Relationship between overweight and obesity with hospitalization for heart failure in 20,985 patients with type 1 diabetes: a population-based study from the Swedish National Diabetes Registry. Diabetes Care 2013;36:2857–2861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, et al. . Cigarette smoking exposure and heart failure risk in older adults: the Health, Aging, and Body Composition Study. Am Heart J 2012;164:236–242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group Intensive diabetes treatment and cardiovascular outcomes in type 1 diabetes: the DCCT/EDIC study 30-year follow-up. Diabetes Care 2016;39:686–69326861924 [Google Scholar]
- 26.Genuth SM, Backlund JY, Bayless M, et al.; DCCT/EDIC Research Group . Effects of prior intensive versus conventional therapy and history of glycemia on cardiac function in type 1 diabetes in the DCCT/EDIC. Diabetes 2013;62:3561–3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lind M, Bounias I, Olsson M, Gudbjörnsdottir S, Svensson AM, Rosengren A. Glycaemic control and incidence of heart failure in 20,985 patients with type 1 diabetes: an observational study. Lancet 2011;378:140–146 [DOI] [PubMed] [Google Scholar]
- 28.Konduracka E, Cieslik G, Galicka-Latala D, et al. . Myocardial dysfunction and chronic heart failure in patients with long-lasting type 1 diabetes: a 7-year prospective cohort study. Acta Diabetol 2013;50:597–606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nyström T, Holzmann MJ, Eliasson B, Kuhl J, Sartipy U. Glycemic control in type 1 diabetes and long-term risk of cardiovascular events or death after coronary artery bypass grafting. J Am Coll Cardiol 2015;66:535–543 [DOI] [PubMed] [Google Scholar]
- 30.Dale AC, Midthjell K, Nilsen TI, Wiseth R, Vatten LJ. Glycaemic control in newly diagnosed diabetes patients and mortality from ischaemic heart disease: 20-year follow-up of the HUNT study in Norway. Eur Heart J 2009;30:1372–1377 [DOI] [PubMed] [Google Scholar]
- 31.Seferović PM, Paulus WJ. Clinical diabetic cardiomyopathy: a two-faced disease with restrictive and dilated phenotypes. Eur Heart J 2015;36:1718–1727, 1727a–1727c [DOI] [PubMed]
- 32.Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 2011;57:891–903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garot J, Lima JA, Gerber BL, et al. . Spatially resolved imaging of myocardial function with strain-encoded MR: comparison with delayed contrast-enhanced MR imaging after myocardial infarction. Radiology 2004;233:596–602 [DOI] [PubMed] [Google Scholar]
- 34.Liu CY, Liu YC, Wu C, et al. . Evaluation of age-related interstitial myocardial fibrosis with cardiac magnetic resonance contrast-enhanced T1 mapping: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2013;62:1280–1287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Adameova A, Dhalla NS. Role of microangiopathy in diabetic cardiomyopathy. Heart Fail Rev 2014;19:25–33 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.