Abstract
OBJECTIVE
Young adults with type 1 diabetes transitioning from pediatric to adult care are at risk for adverse outcomes. We developed a survey to evaluate transition experiences in two groups of young adults with type 1 diabetes, before (PEDS) and after (ADULT) transition to adult care.
RESEARCH DESIGN AND METHODS
We fielded an electronic survey to young adults (18 to <30 years) at 60 T1D Exchange Clinic Registry centers.
RESULTS
Surveys were completed by 602 young adults, 303 in the PEDS group (60% female, age 20 ± 2 years) and 299 in the ADULT group (62% female, age 24 ± 3 years). In the PEDS group, mean anticipated transition age was 22 ± 2 years; 64% remained in pediatric care because of emotional attachment to the provider. The ADULT group transitioned at age 19 ± 2 years, mainly after pediatric provider recommendation. More than 80% of respondents reported receiving counseling on type 1 diabetes self-management and screening tests from pediatric providers, but less than half (43% PEDS and 33% ADULT) reported discussing reproductive health. In the PEDS group, half had discussed transfer with pediatric providers. Of the ADULT participants, 63% received an adult provider referral, and 66% felt mostly/completely prepared to transition. ADULT participants with fewer pretransition pediatric visits or who felt unprepared for transition had increased odds of gaps >6 months between pediatric and adult care. Receipt of transition preparation counseling was not associated with self-reported hemoglobin A1c <7.0% in either group.
CONCLUSIONS
These results support the need for intensive efforts to integrate transition preparation counseling and care coordination into pediatric type 1 diabetes care.
Introduction
The stage of “emerging adulthood,” spanning from 18 to 30 years of age, encompasses a number of competing educational, social, and economic demands (1). For patients with type 1 diabetes, this developmental period is also typified by challenges in disease management compounded by decreasing parental involvement in diabetes care and transitions in providers of diabetes care (2). In the setting of these changes, adherence and glycemic control may worsen. Young adults with type 1 diabetes have been shown to be at increased risk for poor glycemic control as well as acute diabetes complications, emergence of chronic microvascular complications, and early mortality (3–9).
Health care transition has been defined as a planned, purposeful process in which adolescents and young adults move from pediatric-focused to adult-focused health care delivery (10,11). The process of transition involves three phases: transition planning and preparation, transfer to the adult-focused model, and intake into the adult-focused system (10). For young adults with type 1 diabetes, transition problems may contribute to decreased frequency of medical follow-up and increased risk for adverse outcomes (2,9,12,13).
Prior research has elucidated deficiencies in the transition process for patients with type 1 diabetes, including gaps in care (14–17), suboptimal pediatric transition preparation (15,18), increased posttransition hospitalizations (19), and patient dissatisfaction with the transition experience (14–17). However, data are limited on transition experiences in the U.S. (12,15,20,21), partly caused by the lack of a mandated transition age and regional differences in practice.
Available data suggest that many young adults in the U.S. defer transitions of medical care until the early to mid-20s (15,21), but national reports to shed light on pre- and posttransition diabetes care delivery are lacking. Because transition preparation and transfer involve a series of patient interactions with providers, obtaining reports directly from the patients about their experiences is critical to understanding gaps in transition care and areas for improvement.
This study surveyed adolescents and young adults (age 18–30 years) with type 1 diabetes enrolled in the T1D Exchange Clinic Registry regarding their views of the experience of transitioning from pediatric to adult care. The primary objectives of this study were 1) to describe diabetes transition care experiences in two groups of subjects: one group before anticipated transition to adult care and the other group after transition to the adult care setting; and 2) to evaluate the associations between health care transition preparation counseling by pediatric providers of diabetes care and young adult glycemic control within each of the two samples. Because individuals in both groups were drawn from 60 widely distributed diabetes treatment centers, the results provide a broad national view of the current strengths and weaknesses of the transition of diabetes care across the U.S.
Research Design and Methods
Survey Development
We developed the Transition Experiences Survey to characterize the transition experiences of young adults with type 1 diabetes. Initial items were based on a survey from previous single-center research (15), which was adapted by pediatric and adult providers of diabetes care and transition experts and expanded to include pre- and posttransition versions. Young adults still receiving diabetes care at a pediatric center received a version focusing on transition preparation activities in pediatric care (PEDS). Young adults who had transitioned from pediatric to adult diabetes care received a version with questions about transition preparation and the transfer process (ADULT). Both versions captured information regarding diabetes history and demographic and socioeconomic variables. Copies of the Transition Experiences Surveys are available upon reader request.
In addition to the Transition Experiences Survey, the validated Self-Care Inventory (SCI) (22) and the Problem Areas in Diabetes (PAID) scale (23,24) were administered to all participants. The SCI is a self-reported measure of adherence in four domains: glucose monitoring, insulin, diet, and exercise. SCI scores range from 0 to 100, with higher scores indicating better adherence. The PAID scale measures diabetes-related distress. PAID scores range from 0 to 100, with higher scores indicating higher levels of emotional distress related to diabetes.
Survey Administration
The T1D Exchange Clinic Network has enrolled more than 30,000 individuals with type 1 diabetes across 74 U.S.-based pediatric and adult endocrinology practices. Details on the eligibility criteria, informed consent process, and data collection for the T1D Exchange Clinic Network have been previously published (25). T1D Exchange clinic registry participants 18 to <30 years of age and diagnosed with type 1 diabetes before 16 years of age were invited to participate via three e-mail waves between November 2014 and March 2015. Eligible participants who signed an electronic informed consent form completed the online survey. Respondents received their choice of a $20 electronic gift card or donation to a diabetes charity.
Supplementary T1D Exchange Clinic Registry Data
In addition to self-reported survey data, supplementary demographic and clinical data were obtained from the T1D Exchange clinic registry medical records. Clinical variables and demographics, including age at diagnosis, insulin modality, use of continuous glucose monitoring, and the most recent hemoglobin A1c (HbA1c) level, were compared in respondents and nonrespondents.
We used self-reported categorical HbA1c values for the main respondent analyses, given that a significant number of respondents did not have T1D Exchange registry HbA1c values reported in the 6 months preceding the survey. For those respondents who did have recent T1D Exchange clinical HbA1c data, registry HbA1c values agreed with self-reported HbA1c values. Specifically, 63% in the PEDS group had registry HbA1c values 6 months before or 1 month after the survey, and 68% of self-reported HbA1c data matched the registry values. In the ADULT group, 35% of respondents had registry HbA1c values, and 68% of self-reported HbA1c data matched.
Statistical Analysis
A priori, the study was designed to include up to 600 participants in the two response categories (300 PEDS and 300 ADULT). Participants reporting age at transition <13 years (n = 9) were excluded from the analysis. PEDS and ADULT participants were analyzed separately.
Descriptive analyses were completed for transition preparation items and reasons for transition. The association between the anticipated age of transition (PEDS) or the actual age of transition (ADULT) and self-reported most recent HbA1c <7.0% was assessed using a t test. The association between sex and receipt of transition preparation regarding reproductive health was assessed using a χ2 test.
The association between self-reported most recent HbA1c <7.0% and receipt of transition preparation items was assessed using multivariable logistic regression with a stepwise procedure to account for potential multicollinearity. In the ADULT cohort, the association between the self-reported most recent HbA1c <7.0% and the overall level of preparedness to transition (categorized as mostly/completely prepared and completely unprepared/mostly unprepared/neutral) was also assessed using multivariable logistic regression. Participants who indicated they were pregnant or had been pregnant in the past 12 months (n = 10) were excluded from the HbA1c analysis.
Summary scores for the PAID and SCI measures were calculated. The association between PAID and SCI scores and receipt of transition preparation items was examined through a multivariable linear regression model using a LASSO (least absolute shrinkage and selection operator) selection procedure to account for potential multicollinearity. In the ADULT cohort, the association between the PAID score or SCI score and two-category overall level of preparedness to transition was assessed through multivariable linear regression models. Spearman correlation coefficients were computed for anticipated age of transition (PEDS) and age of transition (ADULT) and the PAID and SCI scores.
The proportion with >6 months’ gap in care between receipt of care at a pediatric provider and receipt of care at an adult provider was calculated for the ADULT cohort. A multivariable logistic regression model was used to examine the association between >6 months’ gap in care and 1) the number of reported visits to a pediatric provider in the 12 months before transition and 2) the participant’s level of preparedness to transition. An ordinal logistic regression model was used to examine the association between self-reported HbA1c and >6 months’ gap in care.
Results are expressed as mean ± SD or median (interquartile range). To account for possible confounding, the following covariates were assessed for association with each model outcome through univariate analysis: race/ethnicity, age, sex, duration of diabetes, occurrence of one or more life stress events in the past 12 months, and insurance status. If an association with an outcome was present, the covariate was included in the model for the outcome. Data analyses were performed using SAS 9.4 software (SAS Institute Inc., Cary, NC). In view of the multiple comparisons, only P values <0.01 were considered significant.
Results
Between November 2014 and March 2015, 4,077 participants from 60 clinic centers were sent a survey invitation via e-mail; of these, 964 (24%) accessed the survey, and 611 (15%) from 55 of the 60 clinics completed the survey. An additional 239 participants accessed the survey after the response categories were full and were excluded from participation. Of 611 respondents, 602 met requirements for analysis (303 PEDS and 299 ADULT). Supplementary Figure 1 summarizes the survey administration.
Compared with nonresponders, participants who completed the survey were more likely to be female (61% vs. 49%), non-Hispanic white (86% vs. 79%), have private health insurance (81% vs. 75%), use an insulin pump (62% vs. 52%), use a continuous glucose monitor (18% vs. 10%), and have lower HbA1c (mean 8.3% vs. 8.9%) (Supplementary Table 1).
Participants Receiving Care from Pediatric Provider
Among the 303 PEDS cohort participants, mean age was 20 ± 2 years, 182 (60%) were female, and 259 (87%) were non-Hispanic white. Mean age at diagnosis was 9 ± 4 years. For self-reported HbA1c categories, 52 participants (18%) reported HbA1c <7.0%. Most (219 [72%]) had been patients of their pediatric provider for 5 years or more. Additional characteristics of the cohort, including HbA1c distribution, are reported in Table 1.
Table 1.
Characteristics of survey completers
| Overall | Receiving care from pediatric provider | Transitioned to adult provider | |
|---|---|---|---|
| N = 602 | n = 303 | n = 299 | |
| Age (years)a | 22 ± 3 | 20 ± 2 | 24 ± 3 |
| Female | 368 (61) | 182 (60) | 186 (62) |
| Race/ethnicityb | |||
| White non-Hispanic | 521 (88) | 259 (87) | 262 (89) |
| Black non-Hispanic | 13 (2) | 5 (2) | 8 (3) |
| Hispanic or Latino | 57 (10) | 32 (11) | 25 (8) |
| Other race/ethnicity | 1 (<1) | 1 (<1) | 0 |
| Education level | |||
| High school diploma or less | 103 (17) | 79 (26) | 24 (8) |
| Vocational or college degree | 436 (72) | 214 (71) | 222 (74) |
| Graduate or professional degree | 63 (10) | 10 (3) | 53 (18) |
| Insurance status | |||
| Private insurance | 510 (85) | 247 (82) | 263 (88) |
| Other insurance | 82 (14) | 51 (17) | 31 (10) |
| No insurance | 10 (2) | 5 (2) | 5 (2) |
| Duration as patient under current provider | |||
| <6 months | 72 (12) | 11 (4) | 61 (20) |
| 6 months to <1 year | 46 (8) | 7 (2) | 39 (13) |
| 1 year to <5 years | 195 (32) | 66 (22) | 129 (43) |
| ≥5 years | 289 (48) | 219 (72) | 70 (23) |
| Self-reported most recent HbA1cc | |||
| <7.0% | 112 (19) | 52 (18) | 60 (21) |
| 7.0–7.9% | 218 (37) | 110 (37) | 108 (37) |
| 8.0–8.9% | 135 (23) | 74 (25) | 61 (21) |
| 9.0–9.9% | 68 (12) | 33 (11) | 35 (12) |
| 10.0–10.9% | 34 (6) | 18 (6) | 16 (5) |
| ≥11.0% | 21 (4) | 10 (3) | 11 (4) |
| Age at diagnosis (years) | 9 ± 4 | 9 ± 4 | 9 ± 4 |
Data are shown as the mean ± SD or as n (%).
aParticipant-reported age;
bRace/ethnicity missing for 10 participants;
cSelf-reported HbA1c information missing for 14 participants.
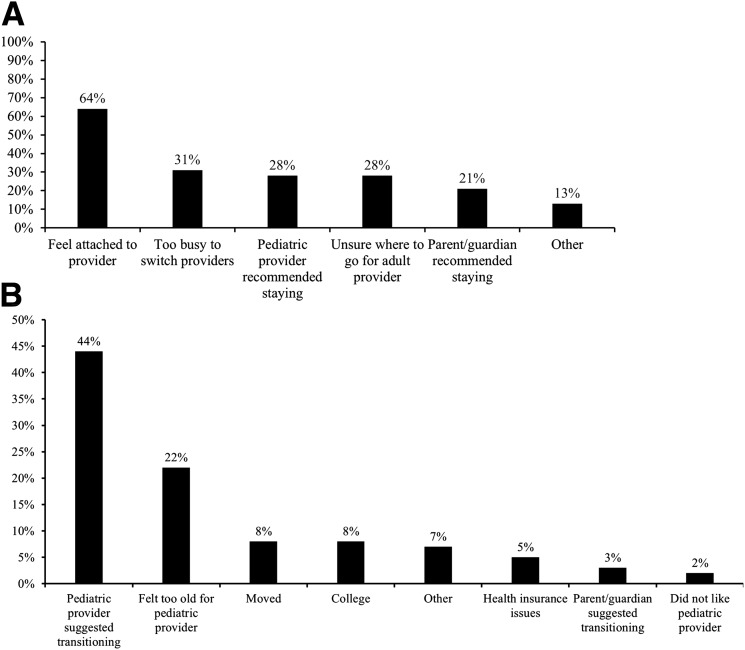
Mean anticipated age to transition to a provider of adult diabetes care was 22 ± 2 years. The anticipated age at transition did not differ between participants who reported currently achieving target HbA1c and those who did not (P = 0.24). Most participants (193 [64%]) indicated they stayed in pediatric diabetes care as a young adult because they felt attached to their pediatric provider of diabetes care (Fig. 1A).
Figure 1.
A: Reasons for remaining with the pediatric provider. B: Main reason for leaving the pediatric provider.
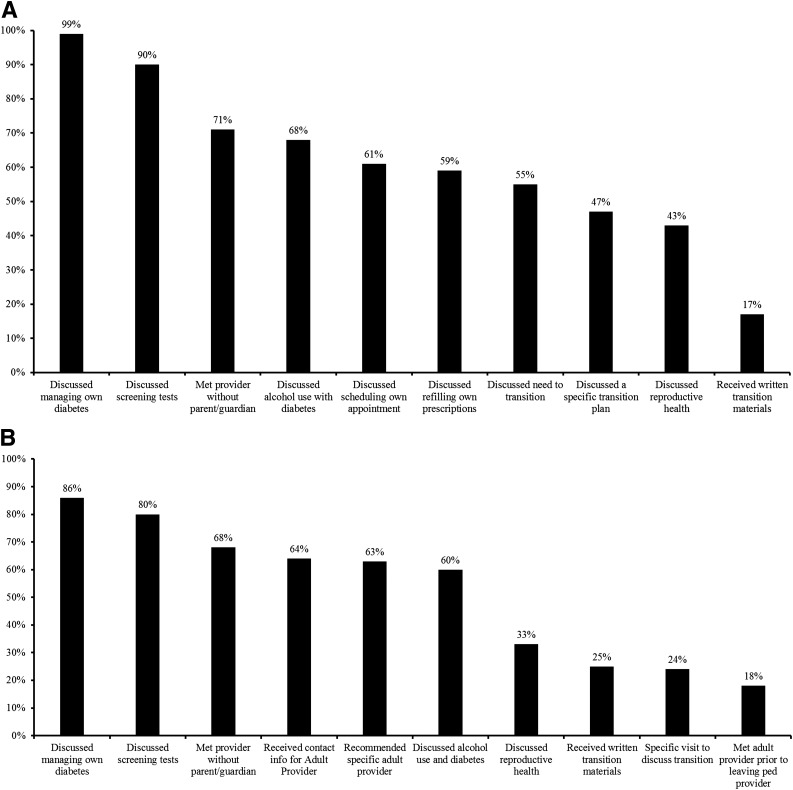
During the preceding 12 months, >90% of participants reported receiving counseling on managing their own diabetes and screening tests, 71% (n = 216) met with their provider without the participant’s parent/guardian in the room, and <50% discussed alcohol use, scheduling their own appointments, and refilling their own prescriptions (Fig. 2A). About half of participants discussed the need to transition to an adult provider of diabetes care (55%) and a specific transition plan (47%), although only 17% had received any written transition materials. Discussions about reproductive health (e.g., pregnancy planning for women or sexual function for men) were reported by 43% of participants (48% of females vs. 36% of males, P = 0.049) (Fig. 2A).
Figure 2.
A: Transition preparation in participants receiving care from a pediatric provider. B: Transition preparation in participants who have transitioned from a pediatric provider to an adult provider.
Current Self-Reported HbA1c
Fifty-two participants (18%) reported a most recent HbA1c <7.0%. Receipt of the individual transition preparation counseling items was not associated with recent HbA1c <7.0% (P > 0.05 for all items, adjusted for race/ethnicity, sex, type of insurance, and occurrence of at least one major life event in the past year).
Current Diabetes-Related Distress and Diabetes Self-Care
The mean PAID score was 27 ± 20, and the mean SCI score was 59 ± 15; PAID and SCI scores were not significantly correlated with anticipated age of transition to adult care (Spearman correlation coefficient −0.1 for both PAID and SCI scores). Receipt of transition preparation counseling items was not associated with PAID or SCI scores (P > 0.05 for all items, adjusted for sex, type of insurance, and occurrence of one or more major life events in the past year).
Participants Transitioned from Pediatric to Adult Provider
Among the 299 ADULT cohort participants, mean current age was 24 ± 3 years, 186 (62%) were female, and 262 (89%) were non-Hispanic white. The mean age at diagnosis was 9 ± 4 years. For self-reported HbA1c categories, 60 participants (21%) reported HbA1c <7.0%. Most (199 [67%]) had been patients of an adult provider for at least 1 year. Additional ADULT cohort characteristics are reported in Table 1.
Mean reported age of transition to adult care was 19 ± 2 years and did not differ between participants who currently met the target for HbA1c and those who did not (P = 0.12). The main reason for transitioning to an adult provider was the suggestion from the participant’s pediatric provider to transition (131 [44%]) (Fig. 1B). Overall, 183 (64%) had three or more visits to their pediatric provider during the 12 months before their transition, and 197 participants (66%) felt mostly or completely prepared for transition.
Sixty-three participants (21%) reported >6 months' gap in care when transitioning from their pediatric to adult provider of diabetes care. A gap >6 months was associated with report of fewer than three visits to the pediatric provider during the 12 months before transition (odds ratio [OR] 3.2 [95% CI 1.7, 6.1], adjusted for race/ethnicity, insurance status, and occurrence of one or more major life events in the past year) (Table 2). Participants feeling less prepared for transition (completely/mostly unprepared or neutral) were also more likely to have a gap >6 months between pediatric and adult care (adjusted OR 3.3 [95% CI 1.7, 6.3]) (Table 2). A gap >6 months was not associated with glycemic control (P = 0.69, adjusted for race/ethnicity, insurance status, sex, age, diabetes duration, and occurrence of one or more major life events in the past year).
Table 2.
Factors associated with a gap of >6 months in care between pediatric and adult providers
| Total | Gap in care >6 months | OR | |
|---|---|---|---|
| N (%) | n (%) | (95% CI)a | |
| No. of visits to pediatric provider during 12 months before transition | |||
| 0–2 visits | 101 (36) | 32 (32) | 3.2 (1.7, 6.1) |
| ≥3 visits | 183 (64) | 25 (14) | 1.0 |
| Participant-reported preparedness to transitionb | |||
| Prepared | 197 (66) | 29 (15) | 1.0 |
| Not prepared | 102 (34) | 34 (33) | 3.3 (1.7, 6.3) |
aORs were calculated from a logistic regression model including the factors of interest (number of visits to pediatric provider during the 12 months before transition and participant-reported preparedness to transition), adjusting for race/ethnicity, insurance status, and occurrence of one or more major life changes in the past year.
bPrepared to transition was assigned for participants reporting they were mostly or completely prepared to leave their pediatric provider. Not prepared to transition was assigned for participants reporting they were completely/mostly unprepared or neutral.
More than 80% of participants reported receiving counseling from their pediatric provider on managing their own diabetes and screening tests (Fig. 2B). About two-thirds reported receiving an adult provider recommendation (63%) or contact information before transition (64%). One-third discussed reproductive health with their pediatric provider (40% of females vs. 21% of males, P < 0.001). Very few had a dedicated transition visit (24%) or met their adult provider before leaving their pediatric provider (18%) (Fig. 2B).
Current Self-Reported HbA1c
Receipt of transition preparation items was not associated with recent HbA1c <7.0% (P > 0.05, adjusted for race/ethnicity, sex, age, diabetes duration, clinic site, insurance status, and occurrence of at least one major life event in the past year). In addition, participants with recent HbA1c levels in the target range did not endorse greater overall transition preparation.
Current Diabetes-Related Distress and Diabetes Self-Care
The mean PAID score was 31 ± 21 and the mean SCI score was 57 ± 15. ADULT cohort PAID and SCI scores were not significantly correlated with age of transition to adult care (Spearman correlation coefficient was −0.1 for the PAID score and 0.0 for the SCI score). Receipt of specific transition preparation counseling items was not associated with PAID or SCI scores (P > 0.05 for all items, adjusted for race/ethnicity, sex, type of insurance, and occurrence of one or more major life events in the past year). However, endorsement of overall preparation for transition (feeling completely/mostly prepared) was associated with lower PAID scores (28.3 vs. 36.1, P = 0.001) and higher SCI scores (58.7 vs. 53.5, P = 0.02).
Conclusions
This study reports contemporary experiences of transition care in a large national sample of 602 young adults with type 1 diabetes. By including both pre- and posttransition groups, we capture varied perspectives on pediatric transition preparation and the actual process of transfer from pediatric to adult clinical settings. Because the health care transition process involves a series of patient–provider interactions, obtaining reports directly from young adults about their experiences is critical to understanding areas for improvement in care delivery for this population.
The participants in the PEDS cohort were beyond the age at which, according to consensus guidelines, transition preparation counseling should be routinely incorporated into pediatric care. Consensus recommendations from the American Academy of Pediatrics, American Academy of Family Physicians, and the American College of Physicians identify 14–15 years as the ideal age to initiate the development of a patient-specific transition plan (10). A position statement of the American Diabetes Association, in collaboration with a number of professional societies, recommends that pediatric providers of diabetes care prepare patients for transition to adult care at least 1 year before transfer and likely during the early adolescent years (2). Recommended components of transition preparation include counseling on diabetes self-management and health risk behaviors, written transition plans, and specific adult provider referrals. However, even reflecting the latest advancements at centers in the T1D Exchange in the years after these consensus statements, this study documents persistent deficiencies in key components of transition preparation as reported by young adults.
Specifically, although most of the respondents in the PEDS group had discussed general diabetes self-management with their providers, 59% had discussed prescription refills and appointment scheduling, 55% had reviewed the need to transition or a specific transition plan, and <20% had received any written transition materials. These findings are similar to data from the 2007 Survey of Adolescent Transition and Health, in which approximately half of a national sample of patients aged 19–23 years with chronic health conditions reported receiving counseling around transition (26). In a 2014 study of 50 younger teens with type 1 diabetes (average age 16 years), 40% had discussed transition with their pediatric diabetes teams (20). In addition, <70% of patients in our pediatric group had discussed alcohol use, and <50% had discussed reproductive health, an area in which prior research has demonstrated adolescent knowledge deficits (2,27).
Further insights from the PEDS group include the observations that young adults remaining in pediatric care, compared with those who transition, are younger and therefore less likely to have completed college. In addition, most of the respondents in the PEDS group reported that they remained in pediatric care because they felt attached to their pediatric provider. This attachment has previously been identified as a barrier to transition in patients with type 1 diabetes (20,28) as well as more generally in pediatric patients with chronic health conditions and their parents (29) and is an important area to directly address in patient counseling. In addition, feelings of attachment experienced by pediatric providers have recently been identified as a further factor that may delay transition timing in participants with type 1 diabetes (30).
In the ADULT cohort, approximately two-thirds had received a specific referral for an adult diabetes provider. This proportion is improved relative to 2012 data from a posttransition sample of young adults with type 1 diabetes receiving care at a single specialty diabetes center providing care for adults, in which only half had received a specific adult provider referral (15). The frequency of pretransition counseling topics reported by the transitioning cohort was similar to the pediatric cohort, although the report of reproductive counseling was lower.
Of the ADULT cohort respondents, 21% reported a gap >6 months between pediatric and adult diabetes care. Respondents with fewer than three pediatric visits in the year before transition and those who overall felt unprepared to transition were more likely to report gaps in care, results that also reinforce prior findings from the single-center study (15). More robust pediatric transition preparation and enhanced engagement of pretransition patients in pediatric care may help reduce gaps in care during the transition period and ultimately improve posttransition diabetes outcomes.
Receipt of transition preparation in the ADULT cohort was not associated with lower posttransition HbA1c, also similar to single-center results. Prior longitudinal studies have demonstrated an increased risk of poor glycemic control in posttransition patients in adult care (9,12). However, the degree to which pediatric transition preparation can modify the glycemic control trajectory across transition remains unclear. Typical transition preparation activities, like those assessed in our survey, may positively affect more proximal outcomes, such as gaps in care and adherence, but may not be potent enough to affect HbA1c. More robust transition programs, for example, incorporating care navigators (31–33) or intensive patient education curricula, may be required to achieve significant improvement in posttransition metabolic outcomes and should be tested in U.S. populations with type 1 diabetes.
Participants who had transitioned to adult care and felt overall mostly/completely prepared to transition reported less diabetes-related distress (PAID) and higher adherence (SCI). No other studies, to our knowledge, have examined associations between diabetes-related distress or adherence and age of transition, or transition preparation variables. The PAID and SCI analyses are especially important given the association of both scales with depression (22,23,34,35), which is prevalent in the young adult population and associated with poor diabetes outcomes (36). Relationships between PAID/SCI scores and transition care delivery warrant further examination in prospective research models with young adults.
This study has a number of limitations. The cross-sectional design prevents conclusions about causality. Patient perceptions of transition preparation may be subject to recall bias, an effect that may be more pronounced in the ADULT cohort, depending on the duration of time between transition and survey response. Self-reported HbA1c data are also subject to bias, although results correlated well with measured T1D Exchange HbA1c data where available. Future prospective cohort study designs would allow for objective data collection on transition outcomes, including HbA1c and diabetes complications trajectories, and the relationship of these outcomes to transition timing, transition preparation, and level of educational attainment and workforce participation during transition.
Response rates cannot be calculated with traditional methods because the a priori maximum planned recruitment included 300 respondents in PEDS/ADULT cohorts, but the nonrespondent proportion was significant. Nonrespondents were more likely to be male and nonwhite, with higher HbA1c levels. Studies are needed to examine transition care experiences in patients with these characteristics. Indeed, our findings of deficiencies in transition preparation and loss to follow-up between pediatric and adult care may be magnified in more diverse populations.
Finally, although existing data suggest that most young adults with type 1 diabetes receive specialty diabetes care (37), this study did not evaluate the experiences of patients who transitioned to adult care physicians outside of the T1D Exchange network. Future studies are needed to examine the experiences of young adults with T1D receiving care from providers outside of this network (e.g., general internist or private practice endocrinologists who treat adults).
In summary, this study offers a national perspective of young adult diabetes care experiences on both sides of the transition. Our results suggest areas for improvement in the delivery of transition preparation education and highlight associations between transition preparation, gaps in care, and self-care adherence. Continued efforts to standardize transition education may help ensure that patients acquire the appropriate knowledge and skills for success in self-management in the adult care setting and lead to improved outcomes for this vulnerable population.
Supplementary Material
Article Information
Funding. Funding was provided by The Leona M. and Harry B. Helmsley Charitable Trust. K.C.G.’s work on this study was also supported by the National Institute for Diabetes and Digestive and Kidney Diseases (K23-DK-102655 and K12-DK-094721).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. K.C.G. contributed to data interpretation and wrote and edited the manuscript. N.C.F. performed statistical analysis and wrote and edited the manuscript. S.A., L.A.D., B.J.A., S.D.C., M.E.D., I.M.L., S.K.L., A.L.P., J.K.R., and L.M.L. contributed to data interpretation and reviewed and edited the manuscript. L.M.L. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and accuracy of the data analysis.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-1729/-/DC1.
References
- 1.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol 2000;55:469–480 [PubMed] [Google Scholar]
- 2.Peters A, Laffel L; American Diabetes Association Transitions Working Group . Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems: a position statement of the American Diabetes Association, with representation by the American College of Osteopathic Family Physicians, the American Academy of Pediatrics, the American Association of Clinical Endocrinologists, the American Osteopathic Association, the Centers for Disease Control and Prevention, Children with Diabetes, The Endocrine Society, the International Society for Pediatric and Adolescent Diabetes, Juvenile Diabetes Research Foundation International, the National Diabetes Education Program, and the Pediatric Endocrine Society (formerly Lawson Wilkins Pediatric Endocrine Society). Diabetes Care 2011;34:2477–2485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HA. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care 2003;26:1052–1057 [DOI] [PubMed] [Google Scholar]
- 4.Laing SP, Swerdlow AJ, Slater SD, et al. The British Diabetic Association Cohort Study, I: all-cause mortality in patients with insulin-treated diabetes mellitus. Diabet Med 1999;16:459–465 [DOI] [PubMed] [Google Scholar]
- 5.Jacobson AM, Hauser ST, Willett J, Wolfsdorf JI, Herman L. Consequences of irregular versus continuous medical follow-up in children and adolescents with insulin-dependent diabetes mellitus. J Pediatr 1997;131:727–733 [DOI] [PubMed] [Google Scholar]
- 6.Wills CJ, Scott A, Swift PG, Davies MJ, Mackie AD, Mansell P. Retrospective review of care and outcomes in young adults with type 1 diabetes. BMJ 2003;327:260–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, Dunger DB. Clinical and psychological course of diabetes from adolescence to young adulthood: a longitudinal cohort study. Diabetes Care 2001;24:1536–1540 [DOI] [PubMed] [Google Scholar]
- 8.Laing SP, Jones ME, Swerdlow AJ, Burden AC, Gatling W. Psychosocial and socioeconomic risk factors for premature death in young people with type 1 diabetes. Diabetes Care 2005;28:1618–1623 [DOI] [PubMed] [Google Scholar]
- 9.Lotstein DS, Seid M, Klingensmith G, et al.; SEARCH for Diabetes in Youth Study Group . Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics 2013;131:e1062–e1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cooley WC, Sagerman PJ; American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians; Transitions Clinical Report Authoring Group . Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2011;128:182–200 [DOI] [PubMed] [Google Scholar]
- 11.Blum RW, Garell D, Hodgman CH, et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health 1993;14:570–576 [DOI] [PubMed] [Google Scholar]
- 12.Helgeson VS, Reynolds KA, Snyder PR, et al. Characterizing the transition from paediatric to adult care among emerging adults with type 1 diabetes. Diabet Med 2013;30:610–615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weissberg-Benchell J, Wolpert H, Anderson BJ. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care 2007;30:2441–2446 [DOI] [PubMed] [Google Scholar]
- 14.Busse FP, Hiermann P, Galler A, et al. Evaluation of patients’ opinion and metabolic control after transfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res 2007;67:132–138 [DOI] [PubMed] [Google Scholar]
- 15.Garvey KC, Wolpert HA, Rhodes ET, et al. Health care transition in patients with type 1 diabetes: young adult experiences and relationship to glycemic control. Diabetes Care 2012;35:1716–1722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kipps S, Bahu T, Ong K, et al. Current methods of transfer of young people with Type 1 diabetes to adult services. Diabet Med 2002;19:649–654 [DOI] [PubMed] [Google Scholar]
- 17.Pacaud D, Yale J, Stephure D, Trussell R, Davies HD. Problems in transition from pediatric to adult care in individuals with diabetes. Can J Diabetes 2005;29:13–18 [Google Scholar]
- 18.Raymond JK, Duke DC, Shimomaeda L, Harris MA; on behalf of the Harold Schnitzer Diabetes Health Center Transition Committee. Looking forward to transition: perspectives on transition from pediatric to adult diabetes care. Diabetes Manag (London, England) 2013;3:10.2217/dmt.13.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a Universal Health Care System. Pediatrics 2009;124:e1134–e1141 [DOI] [PubMed] [Google Scholar]
- 20.Hilliard ME, Perlus JG, Clark LM, et al. Perspectives from before and after the pediatric to adult care transition: a mixed-methods study in type 1 diabetes. Diabetes Care 2014;37:346–354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lotstein DS, Kuo AA, Strickland B, Tait F. The transition to adult health care for youth with special health care needs: do racial and ethnic disparities exist? Pediatrics 2010;126(Suppl. 3):S129–S136 [DOI] [PubMed] [Google Scholar]
- 22.Weinger K, Butler HA, Welch GW, La Greca AM. Measuring diabetes self-care: a psychometric analysis of the Self-Care Inventory-Revised with adults. Diabetes Care 2005;28:1346–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polonsky WH, Anderson BJ, Lohrer PA, et al. Assessment of diabetes-related distress. Diabetes Care 1995;18:754–760 [DOI] [PubMed] [Google Scholar]
- 24.Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care 1997;20:760–766 [DOI] [PubMed] [Google Scholar]
- 25.Beck RW, Tamborlane WV, Bergenstal RM, Miller KM, DuBose SN, Hall CA; T1D Exchange Clinic Network . The T1D Exchange clinic registry. J Clin Endocrinol Metab 2012;97:4383–4389 [DOI] [PubMed] [Google Scholar]
- 26.Sawicki GS, Whitworth R, Gunn L, Butterfield R, Lukens-Bull K, Wood D. Receipt of health care transition counseling in the national survey of adult transition and health. Pediatrics 2011;128:e521–e529 [DOI] [PubMed] [Google Scholar]
- 27.Charron-Prochownik D, Sereika SM, Wang SL, et al. Reproductive health and preconception counseling awareness in adolescents with diabetes: what they don’t know can hurt them. Diabetes Educ 2006;32:235–242 [DOI] [PubMed] [Google Scholar]
- 28.Ritholz MD, Wolpert H, Beste M, Atakov-Castillo A, Luff D, Garvey KC. Patient-provider relationships across the transition from pediatric to adult diabetes care: a qualitative study. Diabetes Educ 2014;40:40–47 [DOI] [PubMed] [Google Scholar]
- 29.Fernandes SM, O’Sullivan-Oliveira J, Landzberg MJ, et al. Transition and transfer of adolescents and young adults with pediatric onset chronic disease: the patient and parent perspective. J Pediatr Rehabil Med 2014;7:43–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Agarwal S, Garvey KC, Raymond JK, Schutta MH. Perspectives on care for young adults with type 1 diabetes transitioning from pediatric to adult health systems: a national survey of pediatric endocrinologists. Pediatr Diabetes 2016. Aug 31. doi: 10.1111/pedi.12436. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cadario F, Prodam F, Bellone S, et al. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol (Oxf) 2009;71:346–350 [DOI] [PubMed] [Google Scholar]
- 32.Holmes-Walker DJ, Llewellyn AC, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with type 1 diabetes aged 15-25 years. Diabet Med 2007;24:764–769 [DOI] [PubMed] [Google Scholar]
- 33.Van Walleghem N, Macdonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care 2008;31:1529–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.La Greca AM, Bearman KJ. Adherence to pediatric treatment regimens. In Handbook of Pediatric Psychology. 3rd ed. Roberts MC, Ed. New York, The Guilford Press, 2003, p. 119–140 [Google Scholar]
- 35.La Greca AM, Swales T, Klemp S, Madigan S. Self care behaviours among adolescents with diabetes (Abstract). In Ninth Annual Sessions of the Society of Behavioral Medicine. Baltimore, MD, Society of Behavioral Medicine 1988. p. A42 [Google Scholar]
- 36.Hislop AL, Fegan PG, Schlaeppi MJ, Duck M, Yeap BB. Prevalence and associations of psychological distress in young adults with type 1 diabetes. Diabet Med 2008;25:91–96 [DOI] [PubMed] [Google Scholar]
- 37.Waitzfelder B, Pihoker C, Klingensmith G, et al.; SEARCH for Diabetes in Youth Study Group . Adherence to guidelines for youths with diabetes mellitus. Pediatrics 2011;128:531–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.