Abstract
Theory and research on HIV and among men who have sex with men (MSM) have long suggested the importance of non-residential locations in defining structural exposures. Despite this, most studies within these fields define place as a residential context, neglecting the potential influence of non-residential locations on HIV-related outcomes. The concept of activity spaces, defined as a set of locations to which an individual is routinely exposed, represents one theoretical basis for addressing this potential imbalance. Using a one-time online survey to collect demographic, behavioral, and spatial data from MSM, this paper describes activity spaces and examines correlates of this spatial variation. We used latent class analysis to identify categories of activity spaces using spatial data on home, routine, potential sexual risk, and HIV prevention locations. We then assessed individual and area-level covariates for their associations with these categories. Classes were distinguished by the degree of spatial variation in routine and prevention behaviors (which were the same within each class) and in sexual risk behaviors (i.e., sex locations and locations of meeting sex partners). Partner type (e.g. casual or main) represented a key correlate of the activity space. In this early examination of activity spaces in an online sample of MSM, patterns of spatial behavior represent further evidence of significant spatial variation in locations of routine, potential HIV sexual risk, and HIV prevention behaviors among MSM. Although prevention behaviors tend to have similar geographic variation as routine behaviors, locations where men engage in potentially high-risk behaviors may be more spatially focused for some MSM than for others.
Keywords: HIV, activity space, spatial epidemiology, latent class analysis, men who have sex with men
INTRODUCTION
Despite recent global and national declines in new HIV infections, HIV incidence has increased among young MSM and both geographic and racial/ethnic disparities remain (Centers for Disease Control and Prevention, 2015a; Lieb et al., 2011; Prejean et al., 2011). These continued disparities suggest that, relative to other high-risk groups, large-scale HIV prevention efforts focusing on individual behavior change have been less effective in slowing the HIV epidemic among MSM (Sullivan et al., 2012). In response, the role of place, including network and structural factors, in patterning risk and prevention behaviors has received renewed attention (Baral et al., 2013; Buot et al., 2014; Frye et al., 2006; Millett et al., 2012).
However, most studies within the HIV literature define place as a residential context, neglecting the potential influence of non-residential locations on HIV-related outcomes (Bowleg et al., 2014; Buttram and Kurtz, 2013; Carpiano et al., 2011; Jeffries et al., 2013; Latkin et al., 2013; Surratt et al., 2015; Vaughan et al., 2014). Place-based theory and research on HIV and among MSM have long suggested the importance of non-residential locations in defining structural exposures (Baral et al., 2013; Buot et al., 2014; Frye et al., 2006; Lansky et al., 2000; Verghese et al., 1989). Non-residential locations may be especially critical in health research among MSM, for whom routine behaviors may be separate from HIV risk and prevention behaviors due to either stigmatization or the spatial distribution of resources (Carrel et al., 2014; Oster et al., 2013, 2011; Rothenberg et al., 2005; Sibley, 1995; Tobin et al., 2014, 2013).
In response, the concept of activity spaces, defined as a set of locations to which an individual is routinely exposed, has been developed. This concept formally acknowledges the potential influence of non-residential locations (Inagami et al., 2007; Matthews and Yang, 2013; Perchoux et al., 2013) and has recently entered the MSM health literature (Duncan et al., 2014a; Koblin et al., 2013). With these initial descriptions, these studies employed the geographic overlap of neighborhoods to show that MSM largely socialize and have sex outside of their residential neighborhoods. The natural next step in this emerging body of research is to more fully describe spatial patterns in these locations. That is, given the existence of this geographic overlap in these behaviors, we may now explore where this geographic overlap of behaviors occurs.
Describing these spatial patterns may inform the geographic targeting of interventions to where relevant behaviors occur, rather than where individuals live (Aral et al., 2015; Lasry et al., 2012; Nunn et al., 2014). Additionally, this descriptive work sets the stage for future research into potential associations with non-residential contexts and activity spaces on HIV sexual risk and prevention behaviors of MSM. Therefore, using a one-time survey to collect demographic, behavioral, and spatial data from an online sample of MSM, this analysis describes activity spaces of MSM and examines correlates of these spatial patterns.
METHODS
Recruitment
Participants were recruited using Facebook banner ads targeted to users based on geography and interests, with ads running from September 21 through October 5, 2015 (Appendix A). This method yields samples similar to venue-based methods of recruiting MSM (Hernandez-Romieu et al., 2014; Sullivan et al., 2014, 2011). A $3 donation to a charity the participant selected from a pre-defined list was provided as incentive.
Eligible participants were required to be: male at birth, aged 18+ years, report at least one male sex partner in the past 6 months, able to read and write English, and to reside in one of nine metropolitan statistical areas (MSA) with the largest numbers of new diagnoses in 2013 (New York City, Miami, Los Angeles, Washington, DC, Atlanta, Chicago, Houston, Dallas, and Philadelphia). In the United States, these MSAs represent half of all new HIV cases (Centers for Disease Control and Prevention, 2015a) and approximately 35% of the MSM population (Grey et al., 2016). MSA boundaries were defined using the U.S. Census Bureau’s 2013 delineations.
Collection of Place-Based Data
Consenting participants completed an online survey containing demographic and behavioral questions, including residential ZIP code at the time of data collection. In addition to these questions, participants indicated specific locations by dropping a pin onto a Google map embedded within the survey. This tool is valid and reliable for a broad sample of MSM (Dasgupta et al., 2014; Vaughan et al., 2016). The requested locations may be grouped into those associated with routine behaviors, with potential HIV sexual risk behaviors, and with HIV prevention behaviors as follows (Appendix B):
Routine locations: Home; work or school location (if the participant reported working at least part time or being a student); two socialization locations; primary care physician (if the participant reported having a regular primary care physician); pharmacy (if the participant reported having a regular pharmacy).
Potential sexual risk locations: For the past three sex partners within the past six months, the location where the participant met the partner and the location of the most recent sexual encounter. The locations of meeting sex partners are included in this category since these types of locations may connect sexual networks and be associated with high-risk sexual behaviors (Kelly et al., 2012; Oster et al., 2013; Tobin et al., 2014). Participants were allowed to report meeting sex partners online or using a mobile app. Since these are not physical locations, they were not considered in this analysis.
Prevention locations: Location of last HIV test, within the past year; location of last test for another sexually transmitted infection (STI), within the past year; primary care physician and pharmacy (if the participant reported currently receiving HIV treatment or regularly taking pre-exposure prophylaxis (PrEP)). Pharmacy and physician locations included as prevention locations were excluded as routine locations.
Covariate Measures
Individual-Level Covariates
As an individual’s activity space may be defined by either the individual’s choices or by constraints placed upon the individual (Matthews and Yang, 2013), covariates included in the study represented demographic variables, transportation-related variables, HIV-related variables, and geographic factors that could spatially influence an individual’s activity space. Demographic variables were: age, race, education, and recent immigration. Age was categorized into three groups with breaks at ages 30 and 51, with the age 30 representing the age division between increasing and stable rates of new HIV diagnosis and age 51 reflecting the Centers for Disease Control and Prevention’s reporting of HIV surveillance data (Centers for Disease Control and Prevention, 2015a, 2015b). Self-reported race/ethnicity was categorized as Hispanic/Latino, non-Hispanic black (“black”), non-Hispanic white (“white”), or non-Hispanic other (“other”). Education was categorized as high school diploma or less, any college, or college degree. Participants were also asked when they moved to their current town.
Transportation-related variables included primary mode of transportation and transportation instability. Primary mode of transportation was dichotomized into primarily using a car or primarily using other, non-car transportation. Transportation instability was defined as any reported instance within the past six months of being unable to do something necessary because of not having a way to get there.
HIV-related factors included HIV-status, partner type, and outness. HIV status was self-reported. Participants were allowed to respond to questions about up to three sex partners in the last six months. Each sex partner was identified as a main or casual partner. The degree to which the participant’s sexual orientation was known to others (“outness”) was assessed using a seven-point scale, with values of 6 or 7 categorized as highly out (Pachankis et al., 2008).
Area-Level Covariates
We also included geographic factors that represent higher-level social context and the spatial distribution and availability of resources. MSA was defined as the MSA where the participant reported currently living. Residential poverty and residential population density were defined based on the census tract of the reported residential location. Poverty was obtained from the US Census Bureau’s 2009–2013 5-Year American Community Survey estimates and categorized as low (<20% poverty) or high (≥20% poverty), based on federal poverty definitions. Population density was based on 2010 population estimates from the US Census Bureau. For each MSA, high density was defined as the top quartile of census tracts. Categories of poverty and population density were then combined into a single variable representing the distribution and availability of resources.
Categorizing Activity Spaces
To define activity spaces of MSM for analytic purposes and public health action, we must reduce the dimensionality of multiple locations into a single, concise, meaningful categorization. Research in other fields (such as obesity and environmental epidemiology) has focused on geometric relationships between points (Perchoux et al., 2013; Rainham et al., 2010; Sherman et al., 2005), or on visual inspection of spatial patterns (Basta et al., 2010; Wiebe et al., 2016). However, since a lack of physical activity and movement are not direct risk factors for HIV, these measures may be less applicable to HIV epidemiology and subsequent public health application.
Consequently, recent studies of HIV-related activity spaces have used the overlap of areas defined by that individual’s behaviors, either administratively-defined areas (e.g. counties) (Duncan et al., 2014a) or participant-defined neighborhoods (Koblin et al., 2013). The presence of overlapping areas in which an individual engages in specific behaviors established the existence of geographic separation among specific behaviors, but lacks more nuanced information about the degree and spatial structure of that geographic separation. By exploring where geographic overlap occurs instead of simply if geographic overlap occurs, we may better understand the spatial structure of behaviors and better target interventions. For example, we could consider whether an individual’s home and doctor are in the same census tract, county, or MSA, creating a measure of the degree of spatial variation across these locations.
Additionally, as opposed to potential geometric measures, using administratively-defined areas to define the degree of overlap (or concordance) may also inform geographic targeting of interventions and resources (Aral et al., 2015; Lasry et al., 2012; Nunn et al., 2014). For example, interventions, funding, and policy decisions at different governmental levels may reach different populations in the presence of large geographic variation in behaviors.
We measured the concordance of administratively-defined areas by first geocoding all locations to a census tract, county, and MSA. We then determined the smallest geographic level (census tract, county, MSA, or out of the MSA) for which the locations were concordant. To account for varying sizes of census tracts across levels of urbanicity and across MSAs, census tracts were considered to be concordant if they were immediately adjacent or, for the smallest quartile of census tracts, were second-order adjacent (e.g. neighbors of neighbors).
Given these measures of concordance for all pairs of locations, we then used latent class analysis (LCA) to create an activity space categorization. LCA posits that the observed data reflect unobserved underlying structure, and creates categories reflecting this latent structure (Collins and Lanza, 2010; Hagenaars and McCutcheon, 2002).
As LCA inputs, we selected specific measures of concordance that allowed for the spatial separation of locations that may be stigmatized or may have limited spatial distribution (Baral et al., 2013; Buot et al., 2014; Cummins et al., 2007; Frye et al., 2006; Sibley, 1995). The LCA inputs also acknowledged the centrality of home as a geographic reference point. With the exception of the last variable below, these inputs took one of four values (census tract, county, MSA, or beyond the MSA). These inputs were defined as follows:
Concordance of routine locations: The smallest geographic level (i.e. census tract, county, MSA, beyond MSA) containing two-thirds of six possible routine locations. This variable represents the geographic area in which the participant performs most routine activities, but does not require the centrality of home.
Concordance of home and work/school: The smallest geographic level containing both home and work/school.
Concordance of home and socialization locations: The smallest geographic level containing home and either reported socialization location.
Concordance of home and testing locations: The smallest geographic level containing home and the location of the HIV or STI test.
Concordance of home and treatment locations: The smallest geographic level containing home and either the physician or pharmacy locations for HIV-positive participants or participants regularly using PrEP.
Concordance of sex locations: The smallest geographic level containing all sex locations.
Concordance of locations of meeting sex partners: The smallest geographic level containing all locations where sex partners were met. Online locations were not considered in this measure.
Concordance between home and sex locations: Whether all, some, or no sex was reported at home.
Using these eight variables, we fit latent class models with 2 to 10 classes. We assessed model fit using change in log-likelihood, Bayesian information criterion (BIC), and entropy (Collins and Lanza, 2010; Nylund et al., 2007). We also considered interpretability of the model results in determining the number of classes (Muthén and Muthén, 2000). After selecting the LCA model, the posterior probability of each participant’s membership in each class was obtained.
Associations between Covariates and LCA Class Membership
We then used logistic regression to describe characteristics of individuals composing the activity space classes. Given the multi-level, unordered measure of activity space, we could have used polytomous logistic regression (Kleinbaum and Klein, 2010). However, interpreting results from these models is not intuitive as they require defining both exposure and outcome reference groups. Consequently, we used logistic regression to model the odds of an individual being in a given class compared to not being in that class. Potential correlation of participants within MSAs was accounted for using a random intercept for each MSA. All covariates described above were included in the model.
To account for uncertainty in the assignment of participants to LCA classes, logistic regression models were run for 1000 replications, with the LCA class for each participant assigned using the posterior probability of class membership. We then used combining equations to calculate the summary OR and 95% confidence intervals (CI) (Reiter, 2003).
Analysis Software
Data management and analysis were performed using SAS v9.4 (SAS Institute, Cary, NC). Latent class analysis was performed using proc LCA v1.3.2 (Lanza et al., 2007). Geocoding and spatial data manipulation were completed in R v3.2.1 (R Foundation for Statistical Computing, Vienna, Austria).
RESULTS
Sample Characteristics
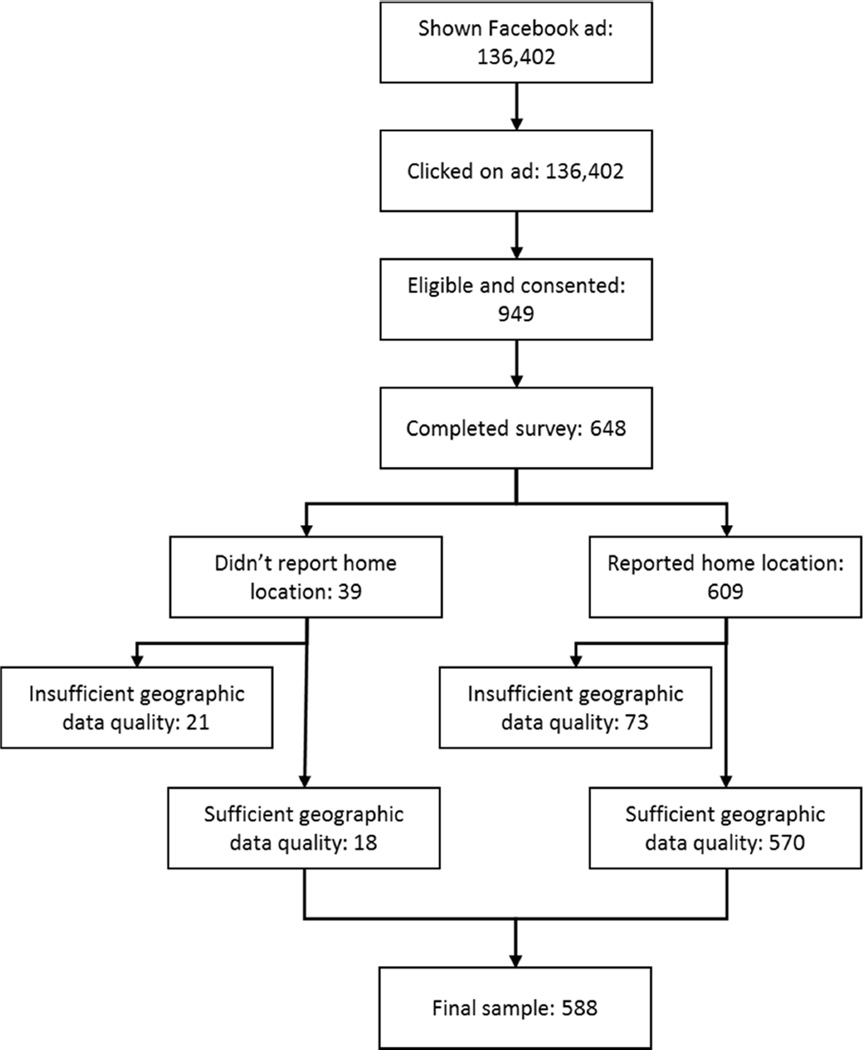
Of 136,402 men presented with the Facebook ad, 5,281 men (3.9%) clicked on the ad to enter the eligibility screening (Figure 1). Of these, 949 men (18.0%) were eligible and consented to participate in the study. 648 men (68.3%) completed the survey.
Figure 1.
Recruitment and study inclusion among MSM in this study
To reduce misclassification of locations, participants were further restricted based on the quality of the reported spatial data. Of 446 participants who placed a home location in the reported ZIP code, the range of distances between the ZCTA centroid and the home location was 0.1 to 9.3 km. Using this range as a threshold for data quality, 73 participants indicating a home location >9.3 km from the reported ZCTA centroid were excluded. 18 participants not reporting a home location and providing data of sufficient quality were also included. Therefore, the final sample included 588 participants.
Our sample represented a wide range of ages and incomes, living in both high and low poverty census tracts (Table 1). Our sample was young and highly educated. Roughly 26% of the sample was non-white.
Table 1.
Characteristics of an online sample of 588 participating men who have sex with men (MSM) from 9 United States metropolitan statistical areas (MSA) in 2015
| Covariate | n (%) |
|---|---|
| Age | |
| 18–29 | 214 (36.4) |
| 30–50 | 286 (48.6) |
| 51 and over | 88 (15.0) |
| Race | |
| White | 430 (73.1) |
| Black | 37 (6.3) |
| Hispanic | 60 (10.2) |
| Other | 61 (10.4) |
| Education | |
| High school or less | 28 (4.8) |
| Some college | 131 (22.3) |
| College degree | 429 (73.0) |
| Employment Status | |
| Employed part-time or full-time | 465 (79.1) |
| Student | 73 (12.4) |
| Unemployed | 14 (2.4) |
| Other | 36 (6.1) |
| Car as primary mode of transportation | 341 (58.0) |
| Any transportation instability | 152 (25.8) |
| Moved to the city in the past 6 months | 45 (7.7) |
| Reported HIV positive | 45 (7.7) |
|
Reporting regular PrEP use (among those not reporting being HIV positive) |
59 (10.9) |
| Sex partners | |
| Main partners only | 179 (30.4) |
| Main and casual partners | 203 (34.5) |
| Casual partners only | 206 (35.0) |
| Highly out | 465 (79.1) |
| Metropolitan statistical area (MSA) | |
| Atlanta | 40 (6.8) |
| Chicago | 71 (12.1) |
| Dallas | 37 (6.3) |
| Houston | 32 (5.4) |
| Los Angeles | 91 (15.5) |
| Miami | 26 (4.4) |
| New York | 179 (30.4) |
| Philadelphia | 41 (7.0) |
| Washington, DC | 71 (12.1) |
| Residential density and poverty | |
| Average density–Low poverty | 232 (39.5) |
| Average density–High poverty | 52 (8.8) |
| High density–Low poverty | 192 (32.7) |
| High density–High poverty | 112 (19.1) |
Activity Space Categories
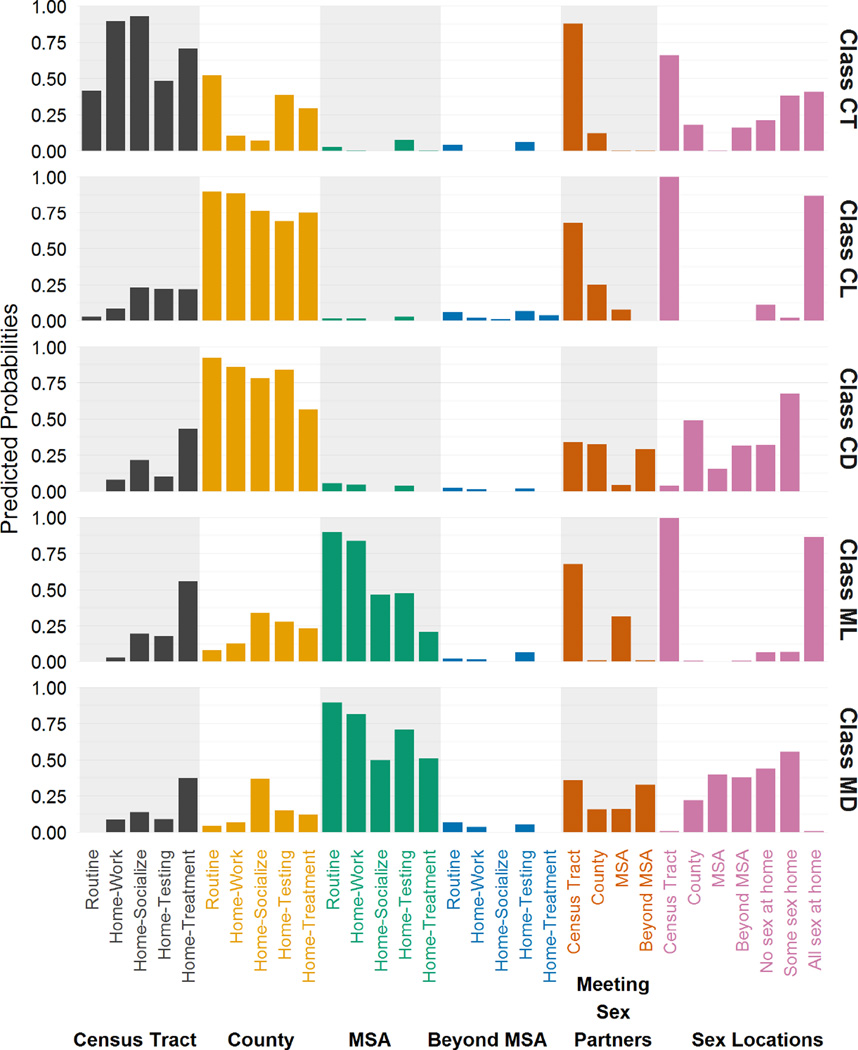
Using a combination of model fit and interpretability, the five-class model was considered most appropriate (Table 2). Figure 2 shows item-response probabilities corresponding to each class. These values represent the probability of a particular response to a particular variable being included in a given latent class.
Table 2.
Model fit statistics for LCA models with 2 to 10 classes
| Number of classes |
Log-likelihood | BIC | Entropy |
|---|---|---|---|
| 2 | −3118 | 1526 | 0.92 |
| 3 | −3007 | 1459 | 0.84 |
| 4 | −2953 | 1502 | 0.86 |
| 5 | −2869 | 1487 | 0.87 |
| 6 | −2857 | 1616 | 0.86 |
| 7 | −2838 | 1731 | 0.84 |
| 8 | −2809 | 1828 | 0.86 |
| 9 | −2797 | 1956 | 0.87 |
| 10 | −2776 | 2067 | 0.89 |
Figure 2.
Item-response probabilities corresponding to each LCA class. All items except those related to potential sexual risk are grouped by the geographic level containing the given behaviors.
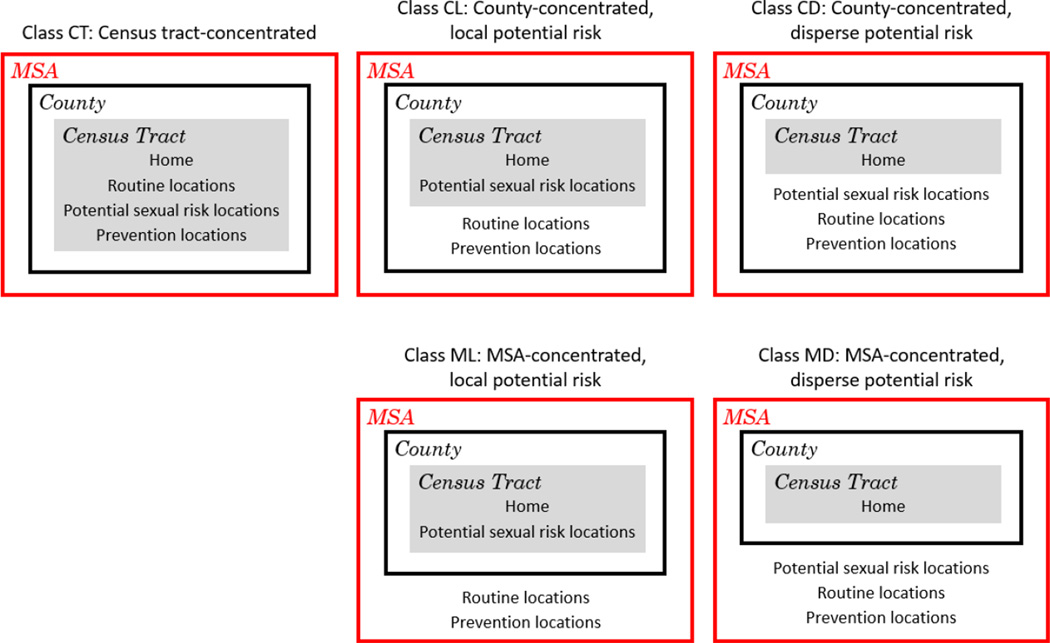
Table 3 summarizes the characteristics of each class; Figure 3 provides a high-level graphical representation of the nesting of behaviors within geographic areas for each class. Classes were distinguished by the geographic level of concordance in routine and prevention behaviors (which were the same within each class) and in potential sexual risk behaviors (i.e., sex locations and locations of meeting sex partners). Based on the item-response probabilities, we labeled the five classes as: “census tract-concentrated” (abbreviated as CT, 16% of the sample using most likely class membership), “county-concentrated, local potential risk” (CL, 30%), “county-concentrated, disperse potential risk” (CD, 24%), “MSA-concentrated, local potential risk” (ML, 15%), “MSA-concentrated, disperse potential risk” (MD, 15%). Men in the “census tract-concentrated” class generally reported all locations including locations of sex and meeting sex partners, close to home (i.e. in the same or adjacent census tracts). Men in the “county-concentrated, local potential risk” and “MSA-concentrated, local potential risk” classes generally reported routine and prevention behaviors farther from home (i.e., within in the same county and MSA, respectively, as their home), with potential sexual risk behaviors limited to a small area surrounding the home. Conversely, men in the “county-concentrated, disperse potential risk” and “MSA-concentrated, disperse potential risk” classes generally reported routine, prevention, and sexual risk behaviors far from home, in the same county and MSA, respectively.
Table 3.
Description of latent classes from the five-class model
| Class (Abbreviation) |
Size of class (n)* |
Description |
|---|---|---|
| Census tract-concentrated (CT) |
16% (94) | Routine behaviors are contained within a census tract or county. Routine, risk, and prevention behaviors occur in the same or adjacent census tract as home. Sex partners are met within the same or adjacent census tracts. Sex occurs within the same census tract, with at least some sex occurring at home. |
| County-concentrated, local potential risk (CL) |
30% (176) |
Routine behaviors are contained within the county. Routine, risk, and prevention behaviors occur in the same county as home. Sex partners are met within the same or adjacent census tracts. Sex occurs only at home. |
| County-concentrated, disperse potential risk (CD) |
24% (141) |
Routine behaviors are contained within the county. Routine and prevention behaviors occur in the same county as home. Sex partners are met across the county, including locations outside the MSA. Sex occurs across the county and outside the home, including outside the MSA. |
| MSA-concentrated, local potential risk (ML) |
15% (88) | Routine behaviors are contained within the MSA. Routine and prevention behaviors occur in the same MSA as home. Sex partners are met within the same or adjacent census tracts. Sex occurs only at home. |
| MSA-concentrated, disperse potential risk (MD) |
15% (88) | Routine behaviors are contained within the MSA. Routine and prevention behaviors occur in the same MSA as home. Sex partners are met in multiple locations, including locations outside the MSA. Sex occurs across the MSA and outside the home, including outside the MSA. |
Based on most likely class membership
Figure 3.
Summary of latent classes from the five-class model
Associations between LCA Classes and Covariates
Table 4 presents modeled associations between each class and the covariates of interest. Compared to all other classes combined, members of the Census Tract-Concentrated class had greater odds of being less educated, living in poorer areas, recently moving to town, and not using a car. Individuals in this class had twice the odds of having both main and casual partners (OR: 1.9, 95% CI: 1.1–3.5) as having only main partners.
Table 4.
Adjusted odds ratios (aOR) and 95% CI for associations between membership in each latent class compared to membership in all other latent classes. aOR for all variables are adjusted for all other variables and account for potential correlation within MSA. Counts are based on most likely class membership.
| Class CT: Census tract- concentrated (n=94) |
Class CL: County- concentrated local potential risk (n=177) |
Class CD: County- concentrated disperse potential risk (n=141) |
Class ML: MSA- concentrated local potential risk (n=88) |
Class MD: MSA- concentrated disperse potential risk (n=88) |
|
|---|---|---|---|---|---|
| Age | |||||
| 18–29 | 0.9 (0.6, 1.6) | 0.9 (0.6, 1.5) | 1.6 (1.0, 2.5) | 0.6 (0.3, 1.0) | 1.0 (0.6, 1.8) |
| 30–50 | Ref | Ref | Ref | Ref | Ref |
| 51 and over | 0.9 (0.5, 1.9) | 2.2 (1.2, 4) | 1.1 (0.6, 1.9) | 0.6 (0.3, 1.3) | 0.4 (0.2, 1.0) |
| Race | |||||
| Black | 1.3 (0. 5, 3.3) | 1.7 (0 .7, 4) | 0.4 (0.1, 1.2) | 0.8 (0.3, 2.3) | 0.9 (0. 3, 2.6) |
| Hispanic | 0.7 (0.3, 1.7) | 1.5 (0.8, 2.8) | 0.9 (0.4, 1.9) | 1.5 (0.7, 3.3) | 0.6 (0.2, 1.7) |
| Other | 0.7 (0.3, 1.6) | 1.2 (0.6, 2.4) | 0.8 (0.4, 1.5) | 1.3 (0.6, 3.1) | 1.3 (0.6, 2.9) |
| White | Ref | Ref | Ref | Ref | Ref |
| Education | |||||
| High school or less | 2.2 (0. 8, 5.8) | 1.2 (0. 5, 3.1) | 1.0 (0.4, 2.6) | 0.6 (0.1, 2.5) | 0.3 ( 0, 2) |
| Some college | 1.6 (0.9, 2.8) | 0.9 (0.5, 1.5) | 0.8 (0.5, 1.3) | 1.2 (0.7, 2.2) | 0.9 (0.5, 1.6) |
| College degree | Ref | Ref | Ref | Ref | Ref |
|
Non-car primary mode of transportation |
2.1 (1.2, 3.7) | 1.1 (0.6, 1.8) | 0.7 (0.4, 1.2) | 0.7 (0.4, 1.2) | 0.7 (0.4, 1.4) |
|
Any transportation instability |
0.6 (0.3, 1.1) | 1.5 (0.9, 2.6) | 0.7 (0.4, 1.1) | 0.7 (0.4, 1.3) | 1.9 (1.1, 3.3) |
|
Moved to town in the past six months |
2.1 (1.0, 4.4) | 1.2 (0.6, 2.6) | 0.2 (0.1, 0.6) | 1.7 (0.7, 4) | 0.8 (0.3, 2.1) |
| Not highly out | 1.3 (0.7, 2.2) | 0.7 (0.4, 1.1) | 1.2 (0.7, 1.9) | 0.9 (0.5, 1.8) | 1.4 (0.8, 2.5) |
| Reported HIV positive | 0.6 (0.2, 1.7) | 1.0 (0.4, 2.2) | 0.9 (0.4, 2.1) | 0.8 (0.3, 2.2) | 2.1 (0.9, 5) |
| Sex partners | |||||
| Main partner only | Ref | Ref | Ref | Ref | Ref |
| Both main and casual | 1.9 (1.1, 3.5) | 0.1 (0.1, 0.3) | 8.9 (4.4, 18) | 0.3 (0.2, 0.6) | 4.0 (1.9, 8.2) |
| Only casual | 1.4 (0.7, 2.5) | 0.3 (0.2, 0.5) | 7.4 (3.6, 15) | 0.3 (0.2, 0.6) | 3.4 (1.7, 7) |
|
Population Density and Poverty |
|||||
| Average density-Low poverty |
Ref | Ref | Ref | Ref | Ref |
| Average density-High poverty |
2.0 (0.9, 4.4) | 1.2 (0.6, 2.4) | 0.6 (0.2, 1.4) | 1.6 (0.7, 3.8) | 0.4 (0.1, 1.2) |
| High density-Low poverty |
1.0 (0.5, 1.8) | 1.9 (1.1, 3.2) | 1.6 (0.9, 2.8) | 0.7 (0.4, 1.3) | 0.4 (0.2, 0.8) |
| High density-High poverty |
0.8 (0.4, 1.6) | 2.5 (1.4, 4.5) | 1.4 (0.8, 2.6) | 0.9 (0.4, 1.8) | 0.2 (0.1, 0.5) |
Membership in the County-Concentrated, Local Potential Risk class reflected greater odds of living in highly urban areas, especially the Los Angeles and New York City MSAs (Table 5), and greater odds of being older. Participants in this class had much lower odds of reporting any casual partners than participants in other classes combined (OR for both main and casual partners: 0.1, 95% CI: 0.1–0.3, OR for only casual partners: 0.3, 95% CI: 0.2–0.5).
Table 5.
Random intercepts and 95% CI for membership in each latent class compared to membership in all other latent classes. Counts are based on most likely class membership.
| MSA | Class CT: Census tract- concentrated (n=94) |
Class CL: County- concentrated local potential risk (n=177) |
Class CD: County- concentrated disperse potential risk (n=141) |
Class ML: MSA- concentrated local potential risk (n=88) |
Class MD: MSA- concentrated disperse potential risk (n=88) |
|---|---|---|---|---|---|
| Atlanta | 0.0 (−0.4, 0.5) | −0.3 (−1.1, 0.5) | −0.4 (−0.9, 0.2) | 0.5 (−0.5, 1.4) | 1.1 (0.1, 2.1) |
| Chicago | 0.0 (−0.4, 0.5) | 0.5 (−0.2, 1.2) | 0.0 (−0.5, 0.5) | −0.8 (−1.9, 0.2) | −0.2 (−1.3, 0.8) |
| Dallas | −0.3 (−0.7, 0.2) | 0.2 (−0.6, 1.0) | 0.2 (−0.4, 0.7) | 0.5 (−0.5, 1.5) | 0.0 (−1.1, 1.1) |
| Houston | 0.2 (−0.2, 0.7) | 0.7 (−0.1, 1.5) | −0.1 (−0.7, 0.5) | −0.9 (−2.2, 0.3) | −1.0 (−2.3, 0.4) |
| Los Angeles | 0.0 (−0.4, 0.5) | 0.7 (0, 1.3) | 0.4 (0, 0.9) | −1.4 (−2.5, −0.3) | −1.4 (−2.5, −0.3) |
| Miami | 0.1 (−0.4, 0.6) | 0.2 (−0.6, 1.0) | 0.2 (−0.4, 0.7) | −0.1 (−1.2, 1.0) | −0.8 (−2.2, 0.5) |
| New York | −0.2 (−0.6, 0.2) | −1.0 (−1.6, −0.3) | −0.3 (−0.7, 0.2) | 1.2 (0.4, 2) | 1.2 (0.4, 2.1) |
| Philadelphia | 0.0 (−0.4, 0.5) | −0.4 (−1.1, 0.4) | −0.1 (−0.6, 0.5) | 0.2 (−0.8, 1.2) | 0.8 (−0.2, 1.8) |
| Washington, DC | 0.0 (−0.4, 0.4) | −0.6 (−1.3, 0.1) | 0.1 (−0.4, 0.6) | 0.9 (0, 1.8) | 0.3 (−0.7, 1.3) |
Members of the County-Concentrated, Disperse Potential Risk class had greater odds of being younger and living in the Los Angeles and New York City MSAs. Importantly, relative to other classes combined, the odds of reporting casual sex partners were much greater for this class (OR for both main and casual partners: 8.9, 95% CI: 4.4–18.0, OR for only casual partners: 7.4, 95% CI: 3.6–15.0).
Conversely, members of the MSA-Concentrated, Local Potential Risk class had much lower odds of reporting casual partners (OR: 0.3, 95% CI: 0.2–0.6, OR for only casual partners: 0.3, 95% CI: 0.2–0.6). This class also had greater odds of living in the New York City or Washington, DC MSAs and lower odds of living in the Los Angeles MSA.
Finally, members of the MSA-Concentrated, Disperse Potential Risk class had lower odds of being older and higher odds of transportation instability. These men had greater odds of living in low density neighborhoods, especially the New York City or Atlanta MSAs and lower odds of living in the Los Angeles MSA. Members of this class also had much greater odds of reporting casual sex partners (OR for both main and casual partners: 4.0, 95% CI: 1.9–8.2, OR for only casual partners: 3.4, 95% CI: 1.7–7.0).
DISCUSSION
Using LCA, we explored spatial variation in the locations of routine activities, HIV-related potential sexual risk, and prevention behaviors among an online sample of MSM. Specifically, this analysis reduced a large number of locations important in the lives of MSM into a single, concise variable that could be used analytically and had relevance for public health action. The identified categories of activity spaces ranged from those in which men remained near home for all behaviors to those in which behaviors spanned multiple counties. Overall, the activity spaces of 84% of participants were defined by behaviors occurring outside of the home census tract.
This analysis revealed two key factors defining the activity spaces of MSM recruited online: the spatial overlap of routine and prevention behaviors and the potential spatial segregation of sexual risk behaviors from routine and prevention behaviors. Although the lack of geographic concordance between home and other behaviors has been reported for MSM (Duncan et al., 2014a; Koblin et al., 2013; Oster et al., 2013, 2011), our study found that an individual’s prevention behaviors generally have similar spatial distribution as routine behaviors, but potential sexual risk behaviors may vary from this routine spatial pattern. With this variation, individuals may encounter multiple contexts, including economic, structural, and health-related, which may vary greatly from their residential context (Inagami et al., 2007).
These classes of activity space in turn reflect geographic and personal factors that may constrain or expand movement with or without the individual’s express volition. Our results first suggest the importance of geography in constraining activity spaces. As our categories are based on the overlap of administratively-defined areas, the size of the census tracts, counties, and MSAs directly determine the potential for behaviors to be in the same area. For census tracts, we accounted for this by effectively enlarging smaller tracts using their neighbors. Similarly, associations between activity space classes and specific MSAs may be markers of MSA geography. For example, two counties comprise the Los Angeles MSA, one much larger than the other, potentially restricting its residents to county-based classes. Likewise, the New York City MSA is composed of relatively small, highly-connected counties, affording its residents greater spatial variation in behaviors and thus facilitating membership in the MSA-concentrated classes.
Apart from the geography of MSAs, the spatial distribution of resources may push MSM away from or pull MSM towards specific locations. Our combined measure of population density and poverty represented a broad measure of resource availability and access. Patterns of associations between the activity space classes and this combined measure may reflect difference in both the spatial distribution and accessibility of locations where prevention and sexual risk may occur, including HIV testing, HIV treatment, and locations where MSM congregate. High poverty, average density areas of MSAs may have less availability of testing and prevention resources and men may have less access to those resources (Dasgupta et al., 2015; Kalichman et al., 2015), providing one possible explanation of a spatially restricted activity space. Men living in these high poverty, average density areas were also more likely to be members of an activity space class with local, rather than diverse, sexual risk, possibly due to the spatial distribution of MSM and limited locations where MSM may gather (Delaney et al., 2014). In contrast, individuals living in high-poverty, high-density areas may have greater access to potential locations of risk and prevention behaviors, despite having fewer resources, resulting in the county-concentrated activity spaces among men in these areas.
Within these spatial structures, the individual must engage in behaviors at specific locations to define his activity space (Baral et al., 2013; Frye et al., 2006). Spatial variation in routine and prevention behaviors, which tended to spatially overlap in this study, could be limited by recently moving to town or by transportation access (Dasgupta et al., 2015; Kalichman et al., 2015). However, as a key component of this categorization of activity space, spatial variation in an individual’s potential sexual risk behaviors may especially be shaped by individual, rather than geographic, factors. Younger MSM, who are at highest risk of acquiring HIV (Johnson et al., 2014; Sullivan et al., 2015), were more likely to engage in potential sexual risk behaviors across a county. Additionally, in this study, partner types represented a key determinant of the activity space. Having any casual partnerships may place MSM at greater sexual risk for HIV and STI acquisition (Rosenberg et al., 2013). The observed activity space categories may then serve as markers of sexual networks with elevated risk.
The spatial variation in these key behaviors has critical implications for developing and implementing HIV-related interventions among MSM. Calls have been made for increased geographic targeting of interventions in order to reach most at-risk populations (Aral et al., 2015; Lasry et al., 2012; Nunn et al., 2014). However, when informed by surveillance data, this targeting is generally based only on residential locations. Our results show that, for most MSM, interventions targeted in this manner could miss key geographic opportunities. For example, interventions could be targeted to locations where sexual risk and prevention behaviors occur, which are frequently outside the home neighborhood in high-risk groups.
However, our observed spatial variation may confer a hidden benefit to the current residence-based geographic targeting of interventions. The large observed spatial variation may give MSM greater opportunity to be exposed to interventions. By visiting locations across his county or MSA, an individual may encounter geographically-targeted interventions that were not designed to reach him. Similarly, MSM living in locations targeted by interventions may also diffuse interventions through their travels.
This study represents an early exploration of the activity spaces of internet-using MSM and attempt to quantify activity spaces for epidemiologic research. Future work will refine this view, including accounting for the time visiting each location and acquiring a more complete set of visited locations (Duncan et al., 2016). Future work may also examine variation in contextual exposures contained within these activity spaces and determine the most critical contexts for specific behaviors, since home may not be the most relevant exposure (Kwan, 2012).
This study has limitations. First, generalizability of these results is a critical concern. Our participants were largely white, educated, urban, and highly out, and may not be representative of MSM in either these MSAs or in the entire country. However, prior online studies of MSM had similar demographics (excepting race) as samples recruited using venue-time based sampling (Hernandez-Romieu et al., 2014; Sullivan et al., 2014, 2011).
Potential misidentification of locations is another limitation (Duncan et al., 2014b). Using recent locations minimizes this concern, provided participants can correctly use the map. This concern may be further minimized by using a familiar Google map in an online population which has been shown to result in valid, high quality data (Dasgupta et al., 2014; Vaughan et al., 2016). Additionally, LCA represents just one method of categorizing activity spaces, and neglects timing and other potentially relevant locations. However, as theory informed our selected inputs (Baral et al., 2013; Buot et al., 2014; Cummins et al., 2007; Frye et al., 2006; Sibley, 1995), our categorization may be used in future research.
Finally, the modifiable areal unit problem (MAUP) represents a limitation of all analyses involving geographic areas (Openshaw and Taylor, 1979). Since administratively-defined areas differ in size both within and across MSAs, the inclusion of behaviors within a given administratively-defined area depends on the spatial structure of the place. However, as these areas form a basis for reporting, policy, and interventions, their relevance remains (Centers for Disease Control and Prevention, 2016, 2015a).
Conclusions
In this early examination of the activity spaces of an online sample of MSM, we observed further evidence of significant spatial variation in locations of routine, potential HIV sexual risk, and HIV prevention behaviors among MSM. Although prevention behaviors tended to occur over the same geographic areas as routine behaviors, locations where men engaged in potentially high-risk sexual behaviors were more spatially focused for some MSM than for others. Studies linking context to HIV-related outcomes should consider the potential exposure to these varied non-residential locations. The geographic targeting of interventions should also acknowledge this potential for relevant behaviors occurring outside the home.
Supplementary Material
Highlights.
84% of activity spaces were defined by locations outside the home census tract.
Prevention behaviors generally spatially overlap routine behaviors.
Potential sexual risk behaviors may be spatially segregated.
Findings suggest importance of considering context of non-residential locations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Aral SO, Torrone E, Bernstein K. Geographical targeting to improve progression through the sexually transmitted infection/HIV treatment continua in different populations. Curr. Opin. HIV AIDS. 2015;10:477–482. doi: 10.1097/COH.0000000000000195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13:482. doi: 10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basta LA, Richmond TS, Wiebe DJ. Neighborhoods, daily activities, and measuring health risks experienced in urban environments. Soc. Sci. Med. 2010;71:1943–1950. doi: 10.1016/j.socscimed.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, Neilands TB, Tabb LP, Burkholder GJ, Malebranche DJ, Tschann JM. Neighborhood Context and Black Heterosexual Men’s Sexual HIV Risk Behaviors. AIDS Behav. 2014;18:2207. doi: 10.1007/s10461-014-0803-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buot MLG, Docena JP, Ratemo BK, Bittner MJ, Burlew JT, Nuritdinov AR, Robbins JR. Beyond race and place: Distal sociological determinants of HIV disparities. PLoS One. 2014;9:e91711. doi: 10.1371/journal.pone.0091711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttram ME, Kurtz SP. Risk and protective factors associated with gay neighborhood residence. Am. J. Mens. Health. 2013;7:110–118. doi: 10.1177/1557988312458793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpiano RM, Kelly BC, Easterbrook A, Parsons JT. Community and drug use among gay men: the role of neighborhoods and networks. J. Health Soc. Behav. 2011;52:74–90. doi: 10.1177/0022146510395026. [DOI] [PubMed] [Google Scholar]
- Carrel M, Eron JJ, Emch M, Hurt CB. Spatial epidemiology of recently acquired HIV infections across rural and urban areas of North Carolina. PLoS One. 2014;9:e88512. doi: 10.1371/journal.pone.0088512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [accessed 4.5.16];Enhanced Comprehensive HIV Prevention Planning and Implementation for Metropolitan Statistical Areas Most Affected by HIV/AIDS [WWW Document] 2016 URL http://www.cdc.gov/hiv/research/demonstration/echpp/index.html.
- Centers for Disease Control and Prevention. HIV surveillance report: Diagnoses of HIV infection in the United States and dependent areas, 2013. Atlanta, GA: 2015a. [Google Scholar]
- Centers for Disease Control and Prevention. [accessed 1.8.15];HIV Among People Aged 50 and Older [WWW Document] 2015b URL http://www.cdc.gov/hiv/risk/age/olderamericans/index.html.
- Collins LM, Lanza ST. Latent Class and Latent Transition Analysis With Applications in the Social, Behavioral, and Health Sciences. 1st. Hoboken, NJ: John Wiley and Sons; 2010. [Google Scholar]
- Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing “place” in health research: a relational approach. Soc. Sci. Med. 2007;65:1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- Dasgupta S, Kramer MR, Rosenberg ES, Sanchez TH, Reed L, Sullivan PS. The Effect of Commuting Patterns on HIV Care Attendance Among Men Who Have Sex With Men (MSM) in Atlanta, Georgia. JMIR Public Heal. Surveill. 2015;1:e10. doi: 10.2196/publichealth.4525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta S, Vaughan AS, Kramer MR, Sanchez TH, Sullivan PS. Use of a Google map tool embedded in an internet survey instrument: Is it a valid and reliable alternative to geocoded address data? JMIR Res. Protoc. 2014;3:e24. doi: 10.2196/resprot.2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delaney KP, Kramer MR, Waller LA, Flanders WD, Sullivan PS. Using a geolocation social networking application to calculate the population density of sex-seeking gay men for research and prevention services. J. Med. Internet Res. 2014;16:e249. doi: 10.2196/jmir.3523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Kapadia F, Halkitis PN. Examination of spatial polygamy among young gay, bisexual, and other men who have sex with men in New York City: The P18 cohort study. Int. J. Environ. Res. Public Health. 2014a;11:8962–8983. doi: 10.3390/ijerph110908962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Kapadia F, Regan SD, Goedel WC, Levy MD, Barton SC, Friedman SR, Halkitis PN. Feasibility and Acceptability of Global Positioning System (GPS) Methods to Study the Spatial Contexts of Substance Use and Sexual Risk Behaviors among Young Men Who Have Sex with Men in New York City: A P18 Cohort Sub-Study. PLoS One. 2016;11:e0147520. doi: 10.1371/journal.pone.0147520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Kawachi I, Subramanian S, Aldstadt J, Melly SJ, Williams DR. Examination of how neighborhood definition influences measurements of youths’ access to tobacco retailers: a methodological note on spatial misclassification. Am. J. Epidemiol. 2014b;179:373–381. doi: 10.1093/aje/kwt251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frye V, Latka MH, Koblin B, Halkitis PN, Putnam S, Galea S, Vlahov D. The urban environment and sexual risk behavior among men who have sex with men. J. Urban Heal. 2006;83:308–324. doi: 10.1007/s11524-006-9033-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grey JA, Bernstein KT, Sullivan PS, Purcell DW, Chesson HW, Gift TL, Rosenberg ES. Estimating the Population Sizes of Men Who Have Sex With Men in US States and Counties Using Data From the American Community Survey. JMIR Public Heal. Surveill. 2016;2:e14. doi: 10.2196/publichealth.5365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagenaars JA, McCutcheon AL. Applied Latent Class Analysis. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
- Hernandez-Romieu AC, Sullivan PS, Sanchez TH, Kelley CF, Peterson JL, Del Rio C, Salazar LF, Frew PM, Rosenberg ES. The comparability of men who have sex with men recruited from venue-time-space sampling and facebook: a cohort study. JMIR Res. Protoc. 2014;3:e37. doi: 10.2196/resprot.3342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagami S, Cohen Da, Finch BK. Non-residential neighborhood exposures suppress neighborhood effects on self-rated health. Soc. Sci. Med. 2007;65:1779–1791. doi: 10.1016/j.socscimed.2007.05.051. [DOI] [PubMed] [Google Scholar]
- Jeffries WL, Marks G, Lauby J, Murrill CS, Millett GA. Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS Behav. 2013;17:1442–1453. doi: 10.1007/s10461-012-0189-y. [DOI] [PubMed] [Google Scholar]
- Johnson AS, Hall HI, Hu X, Lansky A, Holtgrave DR, Mermin J. Trends in diagnoses of HIV infection in the United States, 2002–2011. JAMA. 2014;312:432–434. doi: 10.1001/jama.2014.8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Hernandez D, Kegler C, Cherry C, Kalichman MO, Grebler T. Dimensions of poverty and health outcomes among people living with HIV infection: Limited resources and competing needs. J. Community Health. 2015;40:702–708. doi: 10.1007/s10900-014-9988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly BC, Carpiano RM, Easterbrook A, Parsons JT. Sex and the community: the implications of neighbourhoods and social networks for sexual risk behaviours among urban gay men. Sociol. Health Illn. 2012;34:1085–1102. doi: 10.1111/j.1467-9566.2011.01446.x. [DOI] [PubMed] [Google Scholar]
- Kleinbaum DG, Klein M. Logistic Regression: A Self-Learning Text. New York: Springer; 2010. Polytomous Logistic Regression, in; pp. 429–488. [Google Scholar]
- Koblin BA, Egan JE, Rundle A, Quinn J, Tieu H-V, Cerdá M, Ompad DC, Greene E, Hoover DR, Frye V. Methods to measure the impact of home, social, and sexual neighborhoods of urban gay, bisexual, and other men who have sex with men. PLoS One. 2013;8:e75878. doi: 10.1371/journal.pone.0075878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwan M-P. The Uncertain Geographic Context Problem. Ann. Assoc. Am. Geogr. 2012;102:958–968. [Google Scholar]
- Lansky A, Nakashima AK, Diaz T, Fann SA, Conti L, Herr M, Smith D, Karon JM, Jones JL, Ward JW. Human immunodeficiency virus infection in rural areas and small cities of the southeast: contributions of migration and behavior. J. Rural Heal. 2000;16:20–30. doi: 10.1111/j.1748-0361.2000.tb00433.x. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Collins LM, Lemmon DR, Schafer JL. Proc LCA: A SAS procedure for latent class analysis. Struct. Equ. Model. 2007;14:671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasry A, Sansom SL, Hicks KA, Uzunangelov V. Allocating HIV prevention funds in the United States: Recommendations from an optimization model. PLoS One. 2012:7. doi: 10.1371/journal.pone.0037545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin CA, German D, Vlahov D, Galea S. Neighborhoods and HIV: A social ecological approach to prevention and care. Am. Psychol. 2013;68:210–224. doi: 10.1037/a0032704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieb S, Prejean J, Thompson DR, Fallon SJ, Cooper H, Gates GJ, Liberti TM, Friedman SR, Malow RM. HIV prevalence rates among men who have sex with men in the Southern United States: Population-based estimates by race/ethnicity. AIDS Behav. 2011;15:596–606. doi: 10.1007/s10461-010-9820-y. [DOI] [PubMed] [Google Scholar]
- Matthews SA, Yang T-C. Spatial Polygamy and Contextual Exposures (SPACEs): Promoting activity space approaches in research on place and health. Am. Behav. Sci. 2013;57:1057–1081. doi: 10.1177/0002764213487345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WL, Wilson PA, Rourke SB, Heilig CM, Elford J, Fenton KA, Remis RS. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol. Clin. Exp. Res. 2000;24:882–891. [PubMed] [Google Scholar]
- Nunn A, Yolken A, Cutler B, Trooskin S, Wilson P, Little S, Mayer K. Geography should not be destiny: focusing HIV/AIDS implementation research and programs on microepidemics in US neighborhoods. Am. J. Public Health. 2014;104:775–780. doi: 10.2105/AJPH.2013.301864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Struct. Equ. Model. 2007;14:535–569. [Google Scholar]
- Openshaw S, Taylor PJ. A million or so correlated coefficients: three experiments on the modifiable areal unit problem. Stat. Appl. Spat. Sci. 1979;21:127–144. [Google Scholar]
- Oster AM, Pieniazek D, Zhang X, Switzer WM, Ziebell Ra, Mena La, Wei X, Johnson KL, Singh SK, Thomas PE, Elmore Ka, Heffelfinger JD. Demographic but not geographic insularity in HIV transmission among young black MSM. AIDS. 2011;25:2157–2165. doi: 10.1097/QAD.0b013e32834bfde9. [DOI] [PubMed] [Google Scholar]
- Oster AM, Wejnert C, Mena La, Elmore K, Fisher HH, Heffelfinger JD. Network analysis among HIV-infected young black men who have sex with men demonstrates high connectedness around few venues. Sex. Transm. Dis. 2013;40:206–212. doi: 10.1097/OLQ.0b013e3182840373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Goldfried MR, Ramrattan ME. Extension of the rejection sensitivity construct to the interpersonal functioning of gay men. J. Consult. Clin. Psychol. 2008;76:306–317. doi: 10.1037/0022-006X.76.2.306. [DOI] [PubMed] [Google Scholar]
- Perchoux C, Chaix B, Cummins S, Kestens Y. Conceptualization and measurement of environmental exposure in epidemiology: Accounting for activity space related to daily mobility. Heal. Place. 2013;21:86–93. doi: 10.1016/j.healthplace.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, Lin LS, An Q, Mermin J, Lansky A, Hall HI. Estimated HIV Incidence in the United States, 2006–2009. PLoS One. 2011;6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rainham D, McDowell I, Krewski D, Sawada M. Conceptualizing the healthscape: contributions of time geography, location technologies and spatial ecology to place and health research. Soc. Sci. Med. 2010;70:668–676. doi: 10.1016/j.socscimed.2009.10.035. [DOI] [PubMed] [Google Scholar]
- Reiter JP. Inference for partially synthetic, public use microdata sets. Surv. Methodol. 2003;29:181–188. [Google Scholar]
- Rosenberg ES, Rothenberg RB, Kleinbaum DG, Stephenson RB, Sullivan PS. The implications of respondent concurrency on sex partner risk in a national, web-based study of men who have sex with men in the United States. J. Acquir. Immune Defic. Syndr. 2013;63:514–521. doi: 10.1097/QAI.0b013e318294bcce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothenberg R, Muth SQ, Malone S, Potterat JJ, Woodhouse DE. Social and Geographic Distance in HIV Risk. Sex. Transm. Dis. 2005;32:506–512. doi: 10.1097/01.olq.0000161191.12026.ca. [DOI] [PubMed] [Google Scholar]
- Sherman JE, Spencer J, Preisser JS, Gesler WM, Arcury Ta. A suite of methods for representing activity space in a healthcare accessibility study. Int. J. Health Geogr. 2005;4:24. doi: 10.1186/1476-072X-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibley D. Geographics of Exclusion: Society and Difference in the West. London: Routledge; 1995. [Google Scholar]
- Sullivan PS, Carballo-Diéguez A, Coates T, Goodreau SM, McGowan I, Sanders EJ, Smith A, Goswami P, Sanchez J. Successes and challenges of HIV prevention in men who have sex with men. Lancet. 2012;380:388–399. doi: 10.1016/S0140-6736(12)60955-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Khosropour CM, Luisi N, Amsden M, Coggia T, Wingood GM, DiClemente RJ. Bias in online recruitment and retention of racial and ethnic minority men who have sex with men. J. Med. Internet Res. 2011;13:e38. doi: 10.2196/jmir.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Peterson J, Rosenberg ES, Kelley CF, Cooper H, Vaughan AS, Salazar LF, Frew P, Wingood G, Diclemente R, Del Rio C, Mulligan MJ, Sanchez TH. Understanding Racial HIV/STI Disparities in Black and White Men Who Have Sex with Men: A Multilevel Approach. PLoS One. 2014;9:e90514. doi: 10.1371/journal.pone.0090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, Diclemente RJ, Wingood GM, Frew PM, Salazar LF, Mulligan MJ, Peterson JL. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta , GA: A prospective observational cohort study. Ann. Epidemiol. 2015;25:445–454. doi: 10.1016/j.annepidem.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt HL, Kurtz SP, Levi-Minzi MA, Chen M. Environmental Influences on HIV Medication Adherence: The Role of Neighborhood Disorder. Am. J. Public Health. 2015;105:1660–1666. doi: 10.2105/AJPH.2015.302612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Cutchin M, Latkin CA, Takahashi LM. Social geographies of African American men who have sex with men (MSM): a qualitative exploration of the social, spatial and temporal context of HIV risk in Baltimore, Maryland. Health Place. 2013;22:1–6. doi: 10.1016/j.healthplace.2013.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Latkin CA, Curriero FC. An examination of places where African American men who have sex with men (MSM) use drugs/drink alcohol: A focus on social and spatial characteristics. Int. J. Drug Policy. 2014;25:591–597. doi: 10.1016/j.drugpo.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan AS, Kramer MR, Cooper HLF, Rosenberg ES, Sullivan PS. Completeness and Reliability of Location Data Collected on the Web: Assessing the Quality of Self-Reported Locations in an Internet Sample of Men Who Have Sex With Men. J. Med. Internet Res. 2016;18:e142. doi: 10.2196/jmir.5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaughan AS, Rosenberg ES, Sullivan PS. Spatial relationships between gay stigma, poverty, and HIV infection among black and white men who have sex with men in Atlanta. AIDS Res. Hum. Retroviruses. 2014;30:740–741. doi: 10.1089/aid.2014.0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verghese A, Berk SL, Sarubbi F. Urbs in rure: Human immunodeficiency virus infection in rural Tennessee. J. Infect. Dis. 1989;160:1051–1055. doi: 10.1093/infdis/160.6.1051. [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Richmond TS, Guo W, Allison PD, Hollander JE, Nance ML, Branas CC. Mapping Activity Patterns to Quantify Risk of Violent Assault in Urban Environments. Epidemiology. 2016;27:32–41. doi: 10.1097/EDE.0000000000000395. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.