Abstract
Introduction:
Bilateral common iliac artery (CIA) aneurysm (CIAA) is a rare entity. In the past decade, different endovascular approaches have been adopted for patients with several comorbidities or unfit for open repair (OR). Recently, the use of iliac branch stent graft has been proposed, resulting in satisfactory patency rates and decrease in morbidity. Currently, according to instruction for use, the iliac branch stent graft is to be used with aortobi-iliac stent graft conjunction. We describe a case of a successful endovascular repair of bilateral CIAAs using the GORE Excluder iliac branch endoprosthesis (IBEs) without aortobi-iliac stent graft conjunction.
Case presentation:
An 83-year-old man was admitted with abdominal pain and presence of pulsatile mass in the right and left iliac fossa. Computed tomographic (CT) angiography showed the presence of large bilateral CIAAs (right CIA = 66 mm; left CIA = 38 mm), without concomitant thoracic or abdominal aorta aneurysm. Moreover, CT scan demonstrated the presence of bilateral lower accessory renal artery close to the aortic bifurcation. Due to the high operative risk, the patient was scheduled for endovascular repair with bilateral IBEs, without the aortobi-iliac stent graft conjunction to avoid the renal ischemia as a consequence of renal arteries covering. The procedure was completed without complications and duplex ultrasound demonstrated the complete exclusion of both aneurysms without any type of endoleaks at 1 month of follow-up.
Conclusions:
GORE IBEs without aortobi-iliac stent graft conjunction seem to be a feasible and effective procedure for the treatment of isolated CIAAs in patients with highly selected anatomical conditions.
Keywords: aneurysm, case report, common iliac artery aneurysm, endovascular, iliac branch device
1. Introduction
Common iliac artery (CIA) aneurysm (CIAA) is defined by a transverse diameter greater than 18.5 mm for men, and ≥15 mm for women.[1,2] The prevalence of isolated CIA aneurysm is around 0.008% to 0.03% in autopsy studies and 3% of all kind of aneurysms,[3,4] and they may be associated to an abdominal aorta aneurysm up to 20% of patients.[1,2] Common iliac aneurysm may be bilateral in 70% of isolated iliac artery aneurysms.[1] Currently, elective repair is indicated when CIAA transverse diameter is greater than 30 mm, due to an increased chance of developing symptoms or complications, including rupture with high risk of mortality (50%–100%).[5,6]
Open repair (OR), compared with endovascular procedures, is associated with more blood loss, longer operative time, and higher morbidity and mortality rate.[6,7] Endovascular techniques, with the off-label use of commercially available devices, have been proposed as a safe alternative to open surgery for the treatment of CIAAs patients with severe comorbidities and high risk, or unfit for OR.[6] Usually, the endovascular approaches include embolization and endoluminal stenting of one or both internal iliac artery (IIA) in order to create a distal landing zone in the external iliac artery (EIA). However, the IIA embolization may result in erectile dysfunction, buttock or thigh claudication, paraplegia, and sphincter dysfunction.[8] To address these issues, several endovascular strategies have been proposed to preserve at least 1 internal iliac artery, including the Bell Bottom technique,[9,10] Chimney technique,[11] Sandwich technique,[12] and Parallel Endograft technique.[13]
The off-the shelf iliac branch stent graft offers the possibility to create a distal landing zone both in IIA and EIA, therefore maintaining the IIA patency and pelvic perfusion, resulting in satisfactory patency rates and decrease in mortality.[6] Currently, the main available devices are: the Zenith Iliac Branched Device (IBD, Cook, Inc., Bloomington, IN); the GORE Excluder iliac branch endoprosthesis (IBE, W.L. GORE & Associates, Flagstaff, AZ); and the JOTEC E-iliac stent graft (Lotzenäcker, Hechingen, Germany).
The main anatomical indications for the treatment of aorto-iliac and CIA aneurysms using GORE IBE are resumed in Table 1.
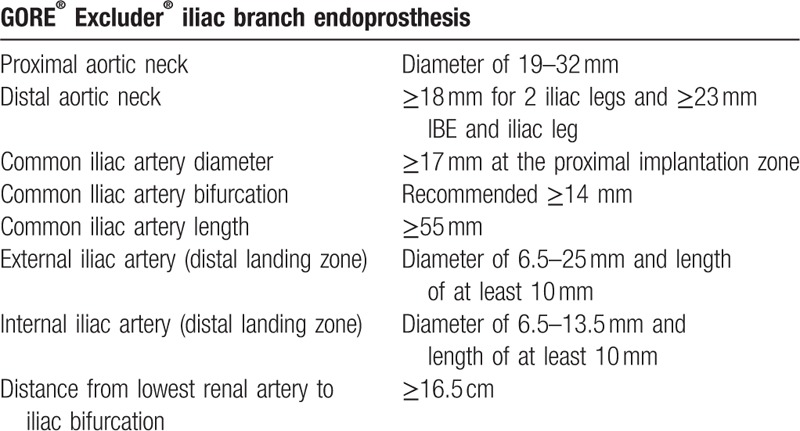
Table 1.
Anatomical criteria for the GORE® Excluder® iliac branch endoprosthesis device for the correct implantation.
According to the manufacturer instructions for use (IFU), the GORE IBE is to be used in conjunction with aortobi-iliac stent graft. Therefore, due to specific anatomical limitations, not every patient is always eligible for the standard approach.
We report a treatment of bilateral CIAAs by endovascular positioning of bilateral GORE IBEs, without the need of aortobi-iliac stent graft conjunction.
2. Case presentation
An 83-year-old man was admitted with 3-day history of abdominal pain. The patient had clinical history of hypertension, coronary artery disease, diabetes mellitus, severe chronic pulmonary disease requiring permanent O2 therapy, and moderate renal failure (serum creatinine 1.5 mg/dL). Physical examination revealed the presence of a pulsatile mass in the right and left iliac fossa. Computed tomographic (CT) angiography demonstrated the presence of a large bilateral CIAAs (right CIA = 66 mm; left CIA = 38 mm) (Fig. 1A). There were no concomitant aneurysms of thoracic or abdominal aorta, but CT angiography showed the presence of a bilateral accessory lower renal artery, 2 cm above the aortic bifurcation (Fig. 1B, C). The length and diameter of the right CIA proximal neck were 23 and 17 mm, respectively. The total length of the right CIA was 104 mm and the diameter of the right external iliac artery (EIA) was 9.5 mm. The right CIA diameter at iliac bifurcation was 15 mm. The internal iliac artery diameter and length to first bifurcation were 9.3 and 27 mm, respectively. The length of the left CIA proximal neck was 27 mm and its diameter ranged between 15.5 and 18 mm. The total length of the left CIA was 85 mm and the diameter of the right EIA was 10 mm. The left CIA diameter at iliac bifurcation was 15.3 mm. The left internal iliac artery diameter and length to first bifurcation were 7.6 and 23 mm, respectively. Taking in consideration the advanced age and the significant comorbidities, the patient was considered not suitable for open repair and scheduled for endovascular treatment. Because of the 2 accessories renal arteries close to the aortic bifurcation, the bilateral CIAAs were treated with bilateral isolated IBE, without an aortic main body endograft support, to avoid the likely renal ischemia as a consequence of polar arteries covering by the endograft. The procedure was performed under local anesthesia and was approached from a bilateral antegrade common femoral artery puncture using sonography guidance and introducer sheaths of appropriate size. After sheath insertion, 5000 units of heparin were administered, and a BER II diagnostic catheter (4 F, 100 cm, Cordis Corporation, Bridgewater, NJ) was advanced into the left CIA with the support of a 0.035″ Terumo guide wire (Terumo Medical). The contralateral access was used for the angiography. The GORE IBE was introduced over a 0.035″ stiff guide wire and “through-and-through” wire, and deployed at the level of the left CIA bifurcation. A 12 F crossover sheath was advanced over the “through-and-through” wire and placed at the level of the side branch. A 0.035″ short tip stiff guide wire (Amplatz, Boston Scientific) was introduced inside 12 F sheath, and internal iliac component was advanced over the wire and deployed in the ipsilateral internal iliac artery. A proximal cuff was deployed to achieve an adequate sealing zone. The angiography confirmed the complete exclusion of left CIAA and the absence of endoleak (Fig. 2A). The procedure was then performed in the right CIA, where a GORE Excluder IBE was deployed at the level of bifurcation (Fig. 2B), while an internal component was deployed in the right internal iliac artery. Also in this case, 2 proximal cuffs were deployed to achieve an adequate sealing zone. At the end of the procedure, angiography confirmed the complete exclusion of the 2 aneurysms without any signs of endoleaks (Fig. 2C). Postoperative course was uneventful and the patient was discharged on the 3rd postoperative day with a stable renal function (serum creatinine 1.4 mg/dL).
Figure 1.
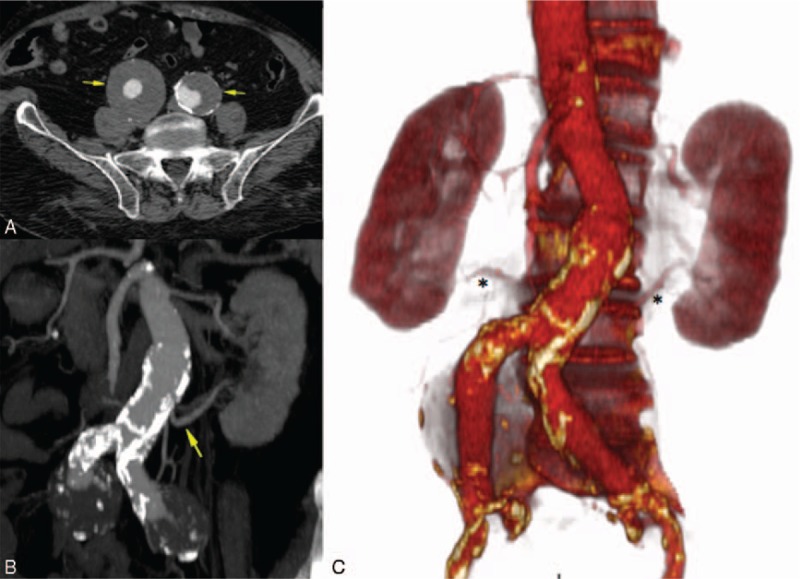
(A) Transversal slide of preoperative CT angiography image showing bilateral common iliac artery aneurysms (right CIA = 66 mm; left CIA = 38 mm). (B) Coronal slide of preoperative CT angiography image showing the presence of accessory renal artery close to the aortic bifurcation. (C) 3D CT angiography reconstruction image showing bilateral inferior accessory renal arteries (the left accessory renal artery was the lower). CIA = common iliac artery aneurysm, CT = computed tomography, 3D = three-dimensional.
Figure 2.
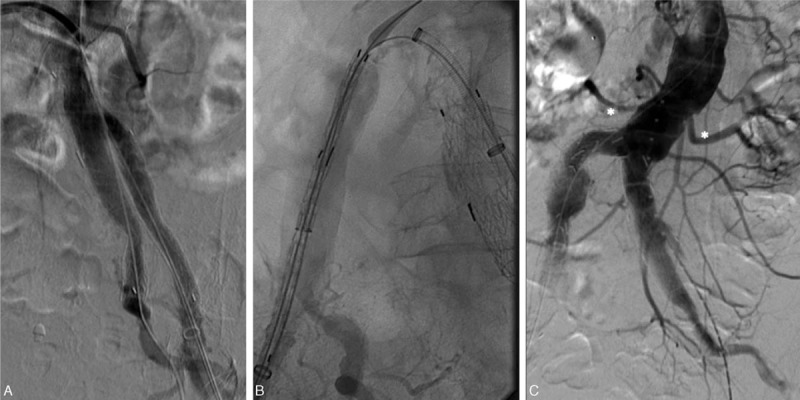
(A) Procedural angiography after correct positioning of the left GORE® Excluder® IBE and patency of the LIIC. (B) Right GORE Excluder IBE device at the level of the right iliac bifurcation. (C) Postprocedural angiography demonstrated the complete exclusion of both iliac aneurysms without signs of endoleak and patency of the left accessory renal artery. IBE = iliac branch endoprosthesis, LICC = left internal iliac component.
Patients with CIA aneurysm are usually followed by means of duplex ultrasound (DUS) and clinical examination before discharge, and after 1 and 6 months, to evaluate patency and endoleak occurrence.
Unfortunately, the patient died 3 months after the procedure due to myocardial infarction.
3. Discussion
This is the first report of endovascular repair, using GORE IBE device, of symptomatic bilateral CIAA, without the need for an aortobi-iliac stent graft conjunction. Endovascular management of CIA aneurysms with the IBE device is safe and effective in the short-term.[6,14–16] In a review on the endovascular treatment of iliac aneurysm with the Zenith iliac branched device, Karthikesalingam et al[16] reported a technical success rates ranging between 85% and 100%, with an iliac branch device occlusion in 12% of patients. Similar results were reported with the GORE IBE with a technical success of 93.3%, no 30-day mortality, and with an IIA patency rate of 91.4% at 1 and 5 years of follow-up, respectively.[17] More recently, Millon et al[6] reported their experience with the GORE IBE in 10 patients with aneurysmal CIA: technical success was 100%, with a complete aneurysm exclusion without type Ib or type II endoleak in all patients; 1 aortic type Ia endoleak was observed in the follow-up, while branch patency was 100% at 1 month and 90% at 6 months.
However, anatomical limitations exclude a large number of CIAA that could be treated with dedicated branched endovascular devices. Karthikesalingam et al[16] and Gray et al[18] reported that only one third of patients with aorto-iliac or isolated CIA aneurysms fulfilled the criteria for the use of these endovascular devices.
Several endovascular strategies have been proposed to preserve at least 1 internal iliac artery.
In 2001, Karch et al[9] described the “Bell Bottom” technique in the treatment of ectatic and nonaneurysmal iliac aneurysm. They used the larger diameter aortic extension cuff to achieve and adequate endograft to arterial wall apposition in patients with ectatic, nonaneurysmal CIAs. In 14 patients, an aortic extension cuffs were placed into 18 ectatic (>14 mm, but <20 mm) CIAs. No endoleaks, ruptures, and endograft migration related to this technique were recorded at a mean follow-up of 14 months.
In 2010 Torsello et al[10] reported a technical success rate of 97.8% in 89 patients with aorto-iliac artery aneurysm undergoing a Bell Bottom technique: after a mean follow-up of 56.5 months, 8 patients died (none aneurysm related). Cumulative survival by Kaplan–Meier analysis was 96.3% at 1 year, 85.5% at 3 years, and 83.1% at 5 years. The freedom from secondary intervention was 91.6% at 5 years.
In 2013, Wu et al[11] described the “Crossover-Chimney” technique for the treatment of CIAAs, with no recorded branch occlusion or type I endoleak from the IIA or chimney graft gutters at 6-month imaging studies.
In 2011, Lobato[12] described the sandwich technique for isolated common and IIA aneurysms or aorto-iliac aneurysms extending to the IIA. This technique consists of: insertion of an aortobi-iliac stent graft through an ipsilateral femoral approach with the iliac limb distal end positioned 1 cm above the IIA origin; catheterization of the ipsilateral IIA through a left brachial access with a long floppy tip guidewire; placement of a covered self-expanding stent inside the IIA with a 6-cm overlap into the iliac limb, followed by positioning of an iliac limb extension 1 cm below the covered stent proximal end; modeling of the iliac limb stent grafts using a latex balloon and dilation of the covered stent with an angioplasty balloon; and deployment of the contralateral iliac limb.
In 2013, Lepidi et al[13] described the “Parallel Endograft” technique in the treatment of distal aortic and common iliac aneurysms. This technique allows avoiding main body insertion, using 2 iliac limbs endografts (ILEs) that are simultaneously delivered from both femoral arteries, landing parallel into the aortic neck. Distal landing zones include external iliac arteries. A 3rd parallel covered stent graft (usually a Viabahn) is delivered from a left brachial approach in order to maintain blood flow to 1 IIA when needed. Eighteen patients were treated using this technique. Three patients required a reintervention: 1 patient needed an ILE extension to treat a type Ib endoleak and 2 for a type II endoleaks. Five patients died of nonaneurysm-related causes during follow-up. No endoleaks, graft displacements, or occlusions were observed during follow-up (median: 26 months, range 12–42 months).
It should be noted that these approaches are often used only in the case of aorto-iliac aneurysm and considered off-label and not always feasible.
The GORE IBE device provides very conformable technology and accurate positioning thanks to its repositionable delivery system, and the internal iliac component is a fully supported sinusoidal stent designed for kink resistance, with proven long-term results in iliac patency preservation.[19,20]
Currently, according to GORE IFU, IBE is to be used together with an aortobi-iliac stent graft in order to obtain a reconstruction of the healthy proximal portion of the CIA,[14] and to avoid the possible migration of the device due to the large proximal diameter of the CIA.[15]
In this case report, we have demonstrated the feasibility of a bilateral CIAA repair with isolated GORE IBEs, preserving the patency of both IIAs. Due to the presence of the bilateral polar renal arteries close to the aortic bifurcation, the use of aortobi-iliac stent graft has to be avoided due to the likely renal ischemia. The main body extensions were used bilaterally in order to increase the size of the available landing zone and to avoid proximal endoleaks. The main limitation of this case report is the absence of an adequate follow-up because to patient died 3-month after intervention. Nevertheless, the aim of this case report was to assess the feasibility of the GORE IBE implantation, without aortobi-iliac stent graft conjunction, for the treatment of patients with isolated bilateral CIAAs.
4. Conclusions
Bilateral, isolated GORE Excluder IBEs seem to be a feasible and safe procedure in the treatment of isolated CIAA, maintaining the patency of IIA and reducing the risk of pelvic complications. This case report may suggest a possible IFU extension of this device, in high selected patients, in the near future. However, a larger number of patients with a longer follow-up are needed to better define suitable anatomical characteristics and determine the effective efficacy and durability of this device.
Footnotes
Abbreviations: CIA = common iliac artery, CIAA = common iliac artery aneurysm, CT = computed tomography, DUS = duplex ultrasound, EIA = external iliac artery, IBE = iliac branch endoprosthesis, IFU = instruction for use, IIA = internal iliac artery, ILE = iliac limb endograft, OR = open repair.
Ethical approval: The endovascular procedure was performed according to the institution's ethical guidelines and the patient gave informed consent to all the procedures. This case report was exempt from the Institutional Review Board standards at University of Catania.
Authorship: VA collected the data and wrote the manuscript, performed surgery, and prepared the figures and tables. AG participated in the preparation and correction of the manuscript. MV, AS, and CV collected the data and formatted the manuscript. GDA performed surgery. PV performed surgery, gave the approval to the final version of the manuscript. All authors read and approved the final manuscript.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kotsis T, Louizos LA, Pappas E, et al. Complex common and internal iliac aneurysm and current approach: individualised open-endovascular or combined procedures. Int J Vasc Med 2014;178610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Johnston KW, Rutherford RB, Tilson MD, et al. Suggested standards for reporting on arterial aneurysms. Subcommittee on Reporting Standards for Arterial Aneurysms, Ad Hoc Committee on Reporting Standards, Society for Vascular Surgery and North American Chapter, International Society for Cardiovascular Surgery. J Vasc Surg 1991;13:452–8. [DOI] [PubMed] [Google Scholar]
- [3].Brunkwall J, Hauksson H, Bengtsson H, et al. Solitary aneurysms of the iliac arterial system: an estimate of their frequency of occurrence. J Vasc Surg 1989;10:381–4. [DOI] [PubMed] [Google Scholar]
- [4].Boules TN, Selzer F, Stanziale SF, et al. Endovascular management of isolated iliac artery aneurysms. J Vasc Surg 2006;44:29–37. [DOI] [PubMed] [Google Scholar]
- [5].Huang Y, Gloviczki P, Duncan AA, et al. Common iliac artery aneurysm: expansion rate and results of open surgical and endovascular repair. J Vasc Surg 2008;47:1203–10. [DOI] [PubMed] [Google Scholar]
- [6].Millon A, Della SN, Arsicot M, et al. Preliminary experience with the GORE® EXCLUDER® iliac branch endoprostesis for common iliac aneurysm endovascular treatment. Ann Vasc Surg 2016;33:11–7. [DOI] [PubMed] [Google Scholar]
- [7].Melas N, Saratzis A, Dixon H, et al. Isolated common iliac artery aneurysms: a revised classification to assist endovascular repair. J Endovasc Ther 2011;18:697–715. [DOI] [PubMed] [Google Scholar]
- [8].Wyers MC, Schermerhorn ML, Fillinger MF, et al. Internal iliac occlusion without coil embolization during during endovascular abdominal aortic aneurysm repair. J Vasc Surg 2002;36:1138–45. [DOI] [PubMed] [Google Scholar]
- [9].Karch LA, Hodgson KJ, Mattos MA, et al. Management of ectatic, nonaneurysmal iliac arteries during endoluminal aortic aneurysm repair. J Vasc Surg 2001;33:S33–8. [DOI] [PubMed] [Google Scholar]
- [10].Torsello G, Schönefeld E, Osada N, et al. Endovascular treatment of common iliac artery aneurysms using the bell-bottom technique: long-term results. J Endovasc Ther 2010;17:504–9. [DOI] [PubMed] [Google Scholar]
- [11].Wu IH, Chan CY, Chen YS, et al. Crossover chimney technique to preserve the internal iliac artery in abdominal aortic aneurysm with commoniliac artery aneurysms. J Endovasc Ther 2013;20:298–302. [DOI] [PubMed] [Google Scholar]
- [12].Lobato AC. Sandwich technique for aortoiliac aneurysms extending to the internal iliac artery or isolated common/internal iliac artery aneurysms: a new endovascular approach to preserve pelvic circulation. J Endovasc Ther 2011;18:106–11. [DOI] [PubMed] [Google Scholar]
- [13].Lepidi S, Piazza M, Scrivere P, et al. Parallel endografts in the treatment of distal aortic and common iliac aneurysms. Eur J Vasc Endovasc Surg 2014;48:29–37. [DOI] [PubMed] [Google Scholar]
- [14].Schönhofer S, Mansour R, Ghotbi R. Initial results of the management of aortoiliac aneurysms with GORE® Excluder® Iliac Branched Endoprosthesis. J Cardiovasc Surg (Torino) 2015;56:883–8. [PubMed] [Google Scholar]
- [15].Kassaian SE, Abbasi K, Al-Sibaie AA. Endovascular treatment of isolated bilateral internal iliac artery aneurysms with a branched endograft: a case report. J Tehran Heart Cent 2013;8:116–8. [PMC free article] [PubMed] [Google Scholar]
- [16].Karthikesalingam A, Hinchliffe RJ, Holt PJ, et al. Endovascular aneurysm repair with preservation of the internal iliac artery using the iliac branch graft device. Eur J Vasc Endovasc Surg 2010;39:285–94. [DOI] [PubMed] [Google Scholar]
- [17].Parlani G, Verzini F, De Rango P, et al. Long-term results of iliac aneurysm repair with iliac branched endograft: a 5-year experience on 100 consecutive cases. Eur J Vasc Endovasc Surg 2012;43:287–92. [DOI] [PubMed] [Google Scholar]
- [18].Gray D, Shahverdyan R, Jakobs C, et al. Endovascular aneurysm repair of aortoiliac aneurysms with an iliac side-branched stent graft: studying the morphological applicability of the Cook device. Eur J Vasc Endovasc Surg 2015;49:283–8. [DOI] [PubMed] [Google Scholar]
- [19].Bos WT, Tielliu IF, Van Den Dungen JJ, et al. Results of endovascular abdominal aortic aneurysm repair with selective use of the Gore Excluder. J Cardiovasc Surg 2009;50:159–64. [PubMed] [Google Scholar]
- [20].Bastos Goncalves F, Rouwet Ellen V, Metz R, et al. Device-specific outcomes after endovascular abdominal aortic aneurysm repair. J Cardiovasc Surg 2010;51:515–31. [PubMed] [Google Scholar]


