Abstract
The goal of treatment in patients with primary hypothyroidism is to attain euthyroidism guided by the stipulated thyroid-stimulating hormone (TSH) levels range so as to minimize any potential long-term adverse effects. However, various factors may result in their Levothyroxine (T4) under and over-replacement.
Our study aimed to evaluate the mean daily dose of L-T4 replacement for Asian patients with primary hypothyroidism. The secondary aims were to determine the proportion of those who were either over or under-replaced, and the factors associated with their thyroid function status and replacement adherence.
Data collected using questionnaire survey from targeted patients managed in a typical public primary care center in Singapore: socio-demographic characteristics, clinical parameters, laboratory investigations, mean daily L-T4-replacement doses, and replacement regimens. The thyroid status of patients was classified based on thyroid function investigations.
Complete data of 229 patients were analyzed. A total of 59.8% of patients had TSH within the normal range, 27.5% and 12.7% were under and over-replaced, respectively. About 60% of Asian patients with primary hypothyroidism achieved normal TSH status requiring average of 1.1 μg of daily L-T4/kgBW (kg body weight). Subjects who were over-replaced had a higher daily L-T4 dose/kgBW when compared to the euthyroid and the under replaced groups. Those with L-T4 over-replacement were largely due to excessive dosage. Patients who were younger, from lower socioeconomic strata, and higher BMI were more likely to be over or under-replaced.
Majority of Asian patients with hypothyroidism required replacement of 1.1 μg of daily L-T4/kgBW. Their thyroid status was influenced by demographic and dosing factors.
Keywords: hypothyroidism, levothyroxine replacement therapy, thyroid function
1. Introduction
The goal of treatment in patients with primary hypothyroidism is to attain euthyroidism guided by the thyroid-stimulating hormone (TSH) levels within the stipulated range so as to minimize any potential long-term adverse effects. However, various factors may result in both under and over-replacement of L-levothyroxine (T4) in these patients, ranging from physician factors such as inadequate dosing and monitoring to patient factors such as adherence to the treatment regimen.
L-T4 is available in fixed-dose tablets. Physicians may introduce various treatment regimens for their patients to attain a state of biochemical euthyroidism with normal T4 and TSH levels. These regimens include different alternate-day doses, tiered doses during weekdays and weekends, or other permutations. Such regimens may potentially confuse the patients and interfere with their medication adherence but the impact is rarely reported in literature. Cost of treatment is another potential deterrent to medication adherence. This confounder is minimized in Singapore, a developed island-state with a highly ranked healthcare system in the world, where its population has access to subsidized medication in the local public primary care clinics (polyclinics). It is an ideal site to assess the dosage of daily L-T4 replacement required for the management of primary hypothyroidism among its resident patients.
Therefore, the primary aim of this study was to evaluate the mean daily dose of L-T4 replacement for Asian patients who attained a state of biochemical euthyroidism. The secondary aims were to determine the proportions of patients who had under and over replacement of L-T4, and to identify the demographic and therapeutic factors that influenced the adequacy of their L-T4 replacement.
2. Methods
A cross-sectional questionnaire survey was carried out on patients with primary hypothyroidism on L-T4 replacement that was managed in a primary care center in Singapore. The study was conducted in a public primary care clinic (polyclinic) located in the northeastern region of Singapore. It is an academic primary care institution that leverage on the electronic health record system to serve a population of 137,500 residents, comprising of 67.3% Chinese, 20.3% Malay, and 8.3% Indian ethnic groups in the estate.[1] The polyclinic in-house pharmacy dispenses most medications, including L-T4, directly to patients at subsidized rates as a distinguishing feature of the local fee-for-service primary healthcare system. Only L-T4 was available for replacement therapy in patients with hypothyroidism at this center and only a single brand of L-T4 was available that came in doses of 25, 50, and 100 μg tablets (Euthyrox by Merck Serono).
Potential subjects were identified by their primary care doctor during their routine consultation at the study site or when they had blood sampling performed for thyroid function test at the polyclinic in-house laboratory. They were then directed to one of the investigators on duty who briefed them on the study intent and procedure using the participant information leaflet that was approved by the local ethic committee in a private room. Written informed consent was obtained after their diagnosis was confirmed on reference to their electronic health records.
2.1. Patients
The population studied included both gender, age 21 to 80 years from the multiethnic Asian population, who were either Singaporean or permanent residents with known diagnosis of primary hypothyroidism that was confirmed from the electronic health record system. The study subjects need to be on a stable dose of L-T4 with a minimal duration of treatment of 6 months and were capable of providing informed consent without cognitive, visual, and auditory impairment.
2.2. Measurements
The questionnaire collected data on demographic characteristics, details on the background of the hypothyroidism, comorbidities and specific information on L-T4 regimen, and concomitant medications. It was noted that the L-T4 regimen varies from same dose daily to variable dose on alternate days (eg, 3 days of dose A; 4 days of dose B) to segmented weekday/weekend dose (eg, Monday to Friday—dose A; Saturday and Sunday—dose B).
Body weight, body mass index (BMI), systolic and diastolic blood pressure, heart rate, and the patients’ latest thyroid function test results (serum free levothyroxine [FT4] and TSH levels) were obtained. The data were then coded and entered into the study Excel spread sheet that was later passed on to a data management officer who deidentified the dataset before handling it to the biostatistician for statistical analysis.
2.3. Reagents
All thyroid function tests were performed at the Clinical Biochemistry laboratory in the Department of Clinical Pathology at a tertiary hospital in Singapore using the Beckman Coulter Unicel Dxl 800 immunoassay analyzer as per manufacturer's recommended protocol. The coefficients of variation for the assays were 3.6% and 5.5% for FT4 and TSH, respectively. Blood samples were transferred from the polyclinic study site to the hospital laboratory twice daily.
2.4. Sample size calculation
One of the outcomes of the study was to determine the proportion of patients with primary hypothyroidism with either over or under-replacement of L-T4. In the absence of local data, the study by Okosieme et al[2] was selected to compute the sample size. Using their report of 17.4% of patients with inadequate T4-replacement, the sample size was computed to be 217 subjects, with a margin of error of 5%. To allow for an estimation of 5% dropout and missing data, we targeted 230 eligible subjects for recruitment.
2.5. Definitions
The subjects were classified into 3 groups based on their TSH level: over-replaced (TSH < 0.65 mU/L), euthyroid (TSH from 0.65 to 3.70 mU/L), and under-replaced (TSH > 3.70 mU/L).
From clinical perspectives, patients with overt hyperthyroid will have a TSH below normal range and an FT4 that is over the normal range. Therefore, even though TSH in this group of patients may not be suppressed below 0.01 mU/L, a raised FT4 could lead to potential harmful consequences. Similarly, those with overt hypothyroid status may be of clinical concern even if TSH is below 10 mU/L. Hence, further classification to overt and subclinical hyper- and hypothyroid status were carried out in our subclass analysis: overt hyperthyroid was defined as TSH below normal range and FT4 above normal range, subclinical hyperthyroid was defined as TSH below normal range and FT4 within normal range, euthyroid was defined as both TSH and FT4 within normal range, subclinical hypothyroid was defined as TSH above normal range and FT4 within normal range, and overt hypothyroid was defined as TSH above normal range and FT4 below normal range.
2.6. Statistical analysis
The mean T4 dosage per day per body weight was derived using the total T4 dosage per week divided by 7 and their respective body weight. To compare factors affecting L-T4 replacement in the 3 groups, analysis of variance was used to compare data showing a Gaussian distribution, while in data where distribution between individuals violated the assumptions of normality when tested using the Kolmogorov–Smirnov test, Kruskal–Wallis was used. For factors affecting medication adherence to L-T4, independent t test was used for parametric data while Mann–Whitney U test was used for nonparametric continuous data. Chi-square or Fisher exact test was used for categorical variables. Analyses were done using Statistical Package for the Social Sciences version 23.0. A P-value of 0.05 was considered significant.
2.7. Ethics approval
All subjects gave their informed written consent that had been approved by the local research ethics committee, SingHealth Centralized Institution Review Board (CIRB 2015/2891).
3. Results
A total of 300 potential subjects were approached by the investigators, of which 49 did not satisfy the eligibility criteria. Twenty-two of the remaining 251 eligible subjects refused consent, attaining a response rate of 91%. Eventually the complete data of 229 patients with hypothyroidism was analyzed.
Table 1 showed the categories of patients based on their biochemical classifications using TSH levels, in comparison with those defined by conventional clinical thyroid status.
Table 1.
Distribution of patients according to current FT4 and TSH concentrations.

Based on the definitions in the method section, Fig. 1 shows that about half of the patients (53%) attained euthyroid status; 7% were overt hyperthyroid, 7.1% subclinical hyperthyroid, 30.1% subclinical hypothyroid, and 1.1% overt hypothyroid status. Forty-six cases were excluded as they did not fall into the defined categories.
Figure 1.

Percentages were based on 183 cases. A total of 46 cases which did not fall into the above categories were excluded from the bar chart. The following categories were excluded: FT4 > 14.4 pmol/L, TSH > 3.70 mU/L, FT4 > 14.4 pmol/L, TSH from 0.65 to 3.70 mU/L, FT4 < 8.8 pmol/L, TSH from 0.65 to 3.70 mU/L, and FT4 < 8.8 pmol/L, TSH < 0.65 mU/L. FT4 = free levothyroxine, TSH = thyroid-stimulating hormone.
The study population consisted of 79.0% females, 74.2% Chinese, 10.0% Malay, 13.1% Indian, and 2.6% of other ethnic groups, with an overall median age of 57 years. A total of 79.5% of them were married, 34.9% had postsecondary or higher education, and 65.9% lived in public housing. Table 2: their median weight (interquartile range [IQR]) was 62.4 kg (55.8–71.3 kg) with median BMI of 25.1 (22.2–27.9).
Table 2.
Factors affecting levothyroxine replacement therapy.
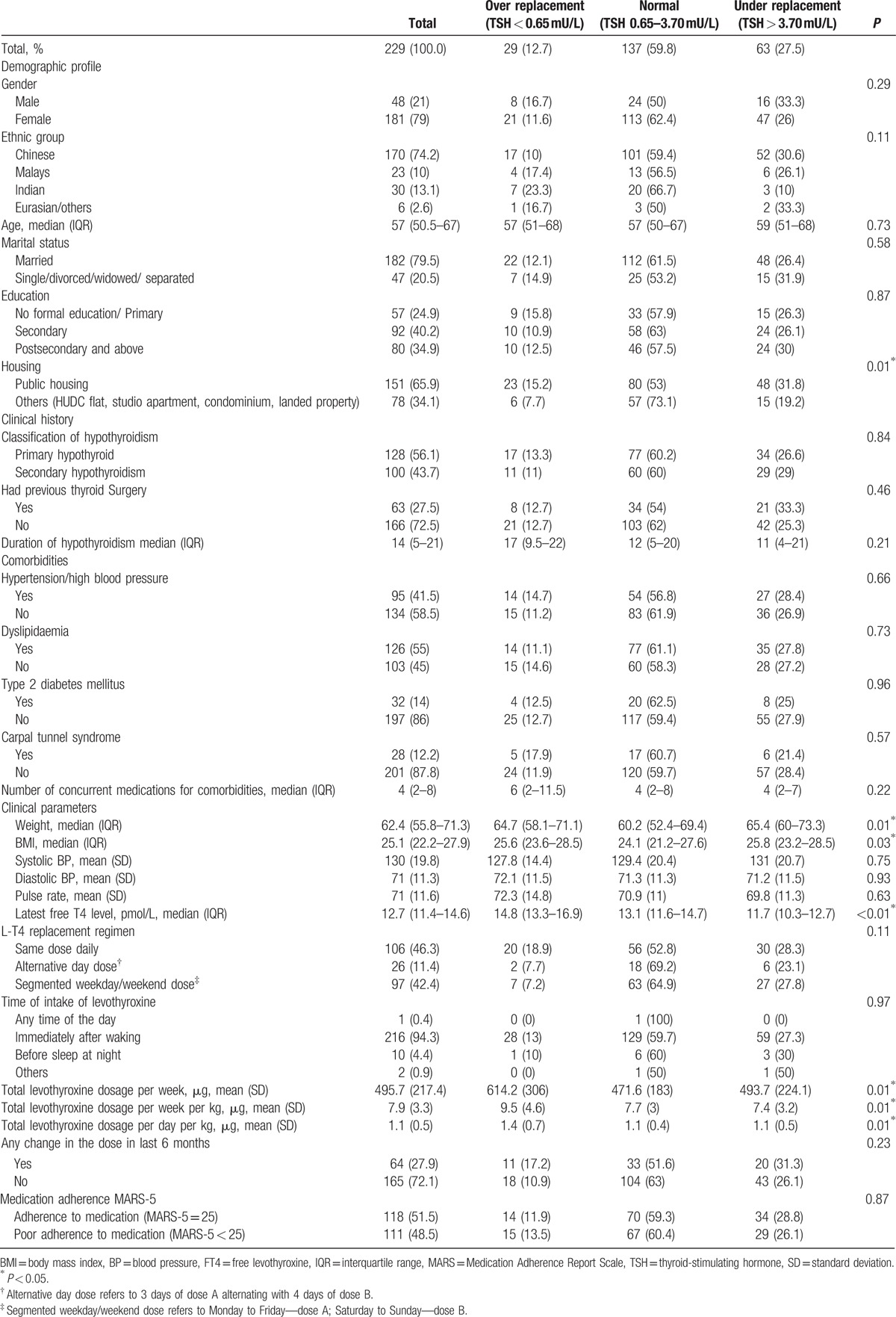
Overall, 59.8% of the sampled population had TSH within the euthyroid range, 12.7% of them were over-replaced and 27.5% were under-replaced. Gender, ethnicity, age, marital status, highest educational level attained, etiology and duration of hypothyroidism, comorbidities, and number of concurrent medications were not associated with the replacement status. We found that patients living in private estates, which are a proxy for their higher socioeconomic status, were more likely to attain euthyroid status (P = 0.01).
The median weight and BMI were lowest for those with normal TSH level at 60.2 kg and 24.1 kg/m2, respectively, compared with 64.7 kg and 25.1 kg/m2 in the over replaced and 65.4 kg and 25.8 kg/m2 in the under replaced group.
Correspondingly, the mean replacement dosages in the over replaced, euthyroid, and under replaced groups were 1.4, 1.1, and 1.1 μg of L-T4 per day per kg body weight (kgBW), respectively (Table 2).
Comparison between the 3 major ethnic groups in Singapore, that is, Chinese, Malay, and Indians, showed that in those with abnormal TSH value, the Chinese and Malays were more likely to be under-replaced with 30.6% and 26.1% respectively while the Indians were less likely to be under-replaced with only 10% of them in this group. The Indians were however more likely to be over-replaced with 23% of them in this group. The median dose requirement per day per kgBW in the euthyroid group for the 3 ethnic groups (Chinese, Malay, and Indian) were 1.2, 1.2, and 0.9 μg, respectively (P = 0.24).
Less than half of the patients (46.3%) were on the same dose of L-T4 daily. A total of 42.4% of them were on segmental regimen and 11.4% were on alternate day regimen. The type of L-T4 replacement regimen, change in doses in previous 6 months, and their medication adherence using the Medication Adherence Report Scale (MARS) instrument were not significantly associated with their thyroid status.
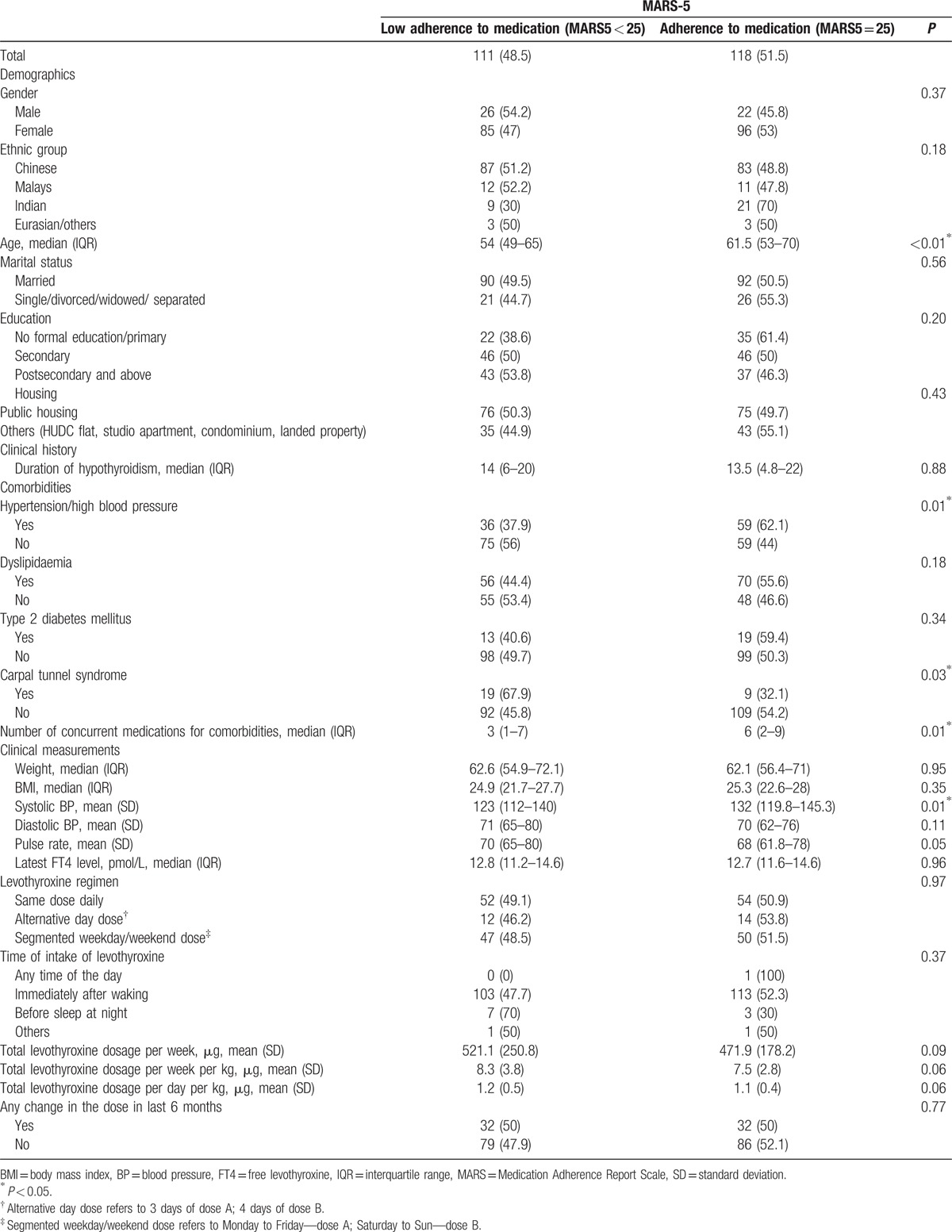
Table 3 showed that younger patients had lower adherence to L-T4 replacement based on their MARS-5 scores. Those who had higher medication adherence were more likely to have hypertension and correspondingly their systolic blood pressures were significantly higher compared to those with lower L-T4 adherence. In contrast, patients with carpal tunnel syndrome were more likely to have lower adherence to L-T4 replacement. The specific L-T4 regimens were not associated with medication adherence. However, those with more concomitant medications were more likely to have higher adherence to L-T4 replacement therapy. Patients who had low adherence to replacement therapy were more likely to receive higher doses of L-T4, although the L-T4 dosages between the 2 groups did not reached statistical significance.
Table 3.
Factors affecting medication adherence to levothyroxine replacement therapy.
4. Discussion
The results showed a significant proportion of patients with hypothyroidism who were under or over-replaced with L-T4. Parle et al[3] did a community study in the United Kingdom that showed although L-T4 prescription is common in the general practice, almost half of the patients (47%) who were either over or under treated based on their TSH value. This was attributed largely to inappropriate dose prescription. A later study by Okosieme et al,[2] also in primary care setting in the United Kingdom, reported that 17.4% of patients with hypothyroidism in their study had over-replacement with L-T4 while 19.8% of the patients were under replaced. The study showed that only 62.9% of the population studied achieved biochemical euthyroidism.[2] Another study by Somwaru et al[4] in the American population showed a high prevalence of abnormal thyroid function tests in older people taking thyroxine hormone replacement, particularly in those with low weight and diabetes. They found that 41% of their thyroid hormone users had a low TSH, 16% had a high TSH, and 43% were euthyroid.
Both over and under replacement with L-T4, even in the subclinical states, could lead to potential harmful consequences. Hypothyroidism is associated with adverse effects on body weight,[5] lipid profile,[6,7] blood pressure,[8] and increased risk of sleep apnea[9] while hyperthyroidism is associated with increased risk of atrial fibrillation[10,11] and osteoporosis.[12,13]
Our study showed that only 59.8% of our population sampled achieved biochemical euthyroid status with L-T4 replacement. A total of 12.7% of them were over-replaced while 27.5% of them were under replaced. From clinical perspectives, 8.7% had overt hyperthyroidism and only 1.1% were regarded as overtly hypothyroid (Fig. 1). We found that socioeconomic status significantly influenced the adequacy of replacement was more likely to be either over replaced or under replaced, leading to abnormal thyroid status. Socioeconomic factors are associated with education and accessibility to healthcare services. Although public primary healthcare services offer subsidized medical consultation and medications to the general population, the awareness and understanding of patients with hypothyroidism on their needs for regular L-T4 replacement and their attending physicians’ fidelity to monitoring of their thyroid status remain to be determined. Future research should focus on patient and physician centric interventions to address these potential gaps to optimize the treatment status of patients with hypothyroidism.
Patients who achieved normal TSH status had lower median weight and BMI compared to the high and low TSH groups. This suggested that patients with higher weight and BMI were more likely to be either over-replaced or under-replaced. This finding is in contrast to that reported by Somwaru et al[4] who found that abnormal thyroid function tests were more likely in those with low weight.
The mean and median daily total T4 dosage was 1.1 μg per day per kgBW in the euthyroid group. This dose is lower than that seen in the Western population, for example, the American Thyroid Association and American Association of Clinical Endocrinologists guidelines of 1.6 μg per day per kgBW on average,[14] suggesting a lower L-T4 requirement for Asian patients. The median dose requirement per day per kgBW in the euthyroid group for the 3 ethnic groups was not significantly different. This suggests that L-T4 requirement for these 3 ethnic groups are similar, and separate dosing according to ethnicity may not be necessary among the Asian patients.
Subjects who were over replaced had a higher total L-T4 dose per day per kgBW with a mean dose of 1.4 μg when compared to the euthyroid and the under replaced group that had a mean dose of 1.1 μg in both groups. This may suggest that the suppressed TSH in the over replaced group is likely to be due to over dosing of L-T4. This calls for physician vigilance to monitor and titrate their patients’ doses of L-T4 to avoid over-replacement.
The similar dose per day per kg in the euthyroid and under replaced group suggested that the under replacement may be due to factors other than dosages, such as medication adherence and reduced bioavailability due to absorption interference with food or other concurrent medications.
The overall medication adherence was 51.5% based on the MARS-5 score (Table 1). Although the 3 groups did not significantly differ in their medication adherence, a higher proportion of them (59.3%) in the normal TSH seemed to have higher adherence to their replacement therapy (Table 1). The younger patients had lower adherence, which could be related to interruptions from work and distraction from other social activities.
Subclass analysis showed that 8.7% of the subjects were in overt hyperthyroid status that is significant enough to be of concern in view of the potential health hazard associated with overt hyperthyroidism.[15] Stall et al[15] had shown that patients with low TSH level of 0.3 to less than 0.1 mU/L despite receiving l-T4 replacement, experienced accelerated decline of bone mineral density in the spine, hip, and radius. One subject had normal TSH and FT4 below normal range suggesting either recent reduction in dose of LT4, or poor L-T4 adherence, or concomitant use of food or medication which might have interfered with the absorption of LT4. Thirty-nine subjects had normal TSH and FT4 above normal range, which could be related to possible recent increase in dose of medication. Six cases with TSH above normal and FT4 above normal range, which could be attributed to possible earlier insufficient dosing of LT4, coupled with recent overdosing of LT4.
4.1. Strength and limitations
This is one of the few studies on multiethnic Asian patients with primary hypothyroidism from Southeast Asia in a primary care setting, where the condition is commonly treated. It provided an insight into the challenges in the management of hypothyroidism, and highlighted the magnitude of L-T4 over and under-replacement in this population.
Nonetheless, the study had its limitations. Classification of the thyroid status based on laboratory investigations of FT4 and TSH levels of patients is arbitrary but a necessary step in any study to avoid ambiguity. We had taken an additional step to subclassify the study population based on their current thyroid status, which was clinically significant. However, 46 subjects did not fit into the categories but probable reasons for patients in these gray areas were provided.
The cross-sectional nature of the data provides a snapshot of the state of the management of primary hypothyroidism in primary care. It did not reflect the dynamic nature of the clinical practices amongst the primary care physicians who were adjusting their patients’ L-T4 doses to attain a state of euthyroidism.
Finally, the data from the MARS-5 instrument relied on self-reporting by patients, which the investigators were not able to verify in this study. However, the questions are easily understood and paralleled the pragmatic approach used by physicians to assess medication adherence in clinical practice. Other form of medication adherence assessment such as the use of electronic pill counter will be considered for the next prospective study on the same topic.
5. Conclusion
In summary, about 60% of patients achieved normal TSH status requiring average of 1.1 μg of L-T4 daily per kg of body weight. A total of 53% of them would be considered euthyroid based on clinical criteria. Subjects who were over-replaced had a higher total L-T4 dose per day per kgBW when compared to the euthyroid and the under replaced groups, where the latter 2 groups had similar dosing per day per kgBW. The result suggested that those who were over replaced were largely due to excessive dosage while those who were under replaced were likely due to other factors. Patients who were younger, from lower socioeconomic strata, and higher BMI were more likely to be over or under replaced.
Acknowledgments
The authors thank the doctors, laboratory and other polyclinic staff at the study site who had rendered their assistance during the recruitment phase of the study, Caris and Patricia for their administrative support, and Lakshmi K for her effort in carrying out part of the survey. The authors also thank the thyroid function assay details from CP Ravikiran from the Singapore General Hospital Central Laboratory.
Footnotes
Abbreviations: BMI = body mass index, FT4 = free Levothyroxine, kgBW = kg body weight, MARS = Medication Adherence Report Scale, T4 = levothyroxine, TSH = thyroid-stimulating hormone.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Statistics Singapore—Geographic Distribution http://www.singstat.gov.sg/statistics/browse-by-theme/geographic-distribution [Accessed April 20, 2016]. [Google Scholar]
- [2].Okosieme OE, Belludi G, Spittle K, et al. Adequacy of thyroid hormone replacement in a general population. QJM 2011;104:395–401. [DOI] [PubMed] [Google Scholar]
- [3].Parle JV, Franklyn JA, Cross KW, et al. Thyroxine prescription in the community: serum thyroid stimulating hormone level assays as an indicator of undertreatment or overtreatment. Br J Gen Pract 1993;43:107–9. [PMC free article] [PubMed] [Google Scholar]
- [4].Somwaru LL, Arnold AM, Joshi N, et al. High frequency of and factors associated with thyroid hormone over-replacement and under-replacement in men and women aged 65 and over. J Clin Endocrinol Metab 2009;94:1342–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Baron DN. Hypothyroidism; its aetiology and relation to hypometabolism, hypercholesterolaemia, and increase in body-weight. Lancet 1956;271:277–81. [DOI] [PubMed] [Google Scholar]
- [6].Duntas LH. Thyroid disease and lipids. Thyroid 2002;12:287–93. [DOI] [PubMed] [Google Scholar]
- [7].Franklyn JA, Daykin J, Betteridge J, et al. Thyroxine replacement therapy and circulating lipid concentrations. Clin Endocrinol 1993;38:453–9. [DOI] [PubMed] [Google Scholar]
- [8].Fommei E, Iervasi G. The role of thyroid hormone in blood pressure homeostasis: evidence from short-term hypothyroidism in humans. J Clin Endocrinol Metab 2002;87:1996–2000. [DOI] [PubMed] [Google Scholar]
- [9].Jha A, Sharma SK, Tandon N, et al. Thyroxine replacement therapy reverses sleep-disordered breathing in patients with primary hypothyroidism. Sleep Med 2006;7:55–61. [DOI] [PubMed] [Google Scholar]
- [10].Sawin CT, Geller A, Wolf PA, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med 1994;331:1249–52. [DOI] [PubMed] [Google Scholar]
- [11].Flynn RW, Bonellie SR, Jung RT, et al. Serum thyroid-stimulating hormone concentration and morbidity from cardiovascular disease and fractures in patients on long-term thyroxine therapy. J Clin Endocrinol Metab 2010;95:186–93. [DOI] [PubMed] [Google Scholar]
- [12].Stall GM, Harris S, Sokoll LJ, et al. Accelerated bone loss in hypothyroid patients overtreated with L-thyroxine. Ann Intern Med 1990;113:265–9. [DOI] [PubMed] [Google Scholar]
- [13].Paul TL, Kerrigan J, Kelly AM, et al. Long-term L-thyroxine therapy is associated with decreased hip bone density in premenopausal women. JAMA 1988;259:3137–41. [PubMed] [Google Scholar]
- [14].Jonklaas J, Bianco AC, Bauer AJ, et al. Guidelines for the treatment of hypothyroidism: prepared by the American Thyroid Association task force on thyroid hormone replacement. Thyroid 2014;24:1670–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Stall GM, Harris S, Sokoll LJ, et al. Accelerated bone loss in hypothyroid patients overtreated with L-thyroxine. Ann Intern Med 1990;113:265–9. [DOI] [PubMed] [Google Scholar]


