Introduction
Mycosis fungoides (MF) is the most common type of cutaneous T-cell lymphoma (CTCL). The neoplastic T cells in MF are usually mature CD4+ T cells, and CD8+ phenotype expression is rarely observed.1 There are 2 categories of CD8+ CTCL, one with aggressive behavior and one with indolent behavior.2 We report a rare case of suddenly aggravated CD8+ MF that was found to be associated with a hidden adenocarcinoma in the colon.
Case report
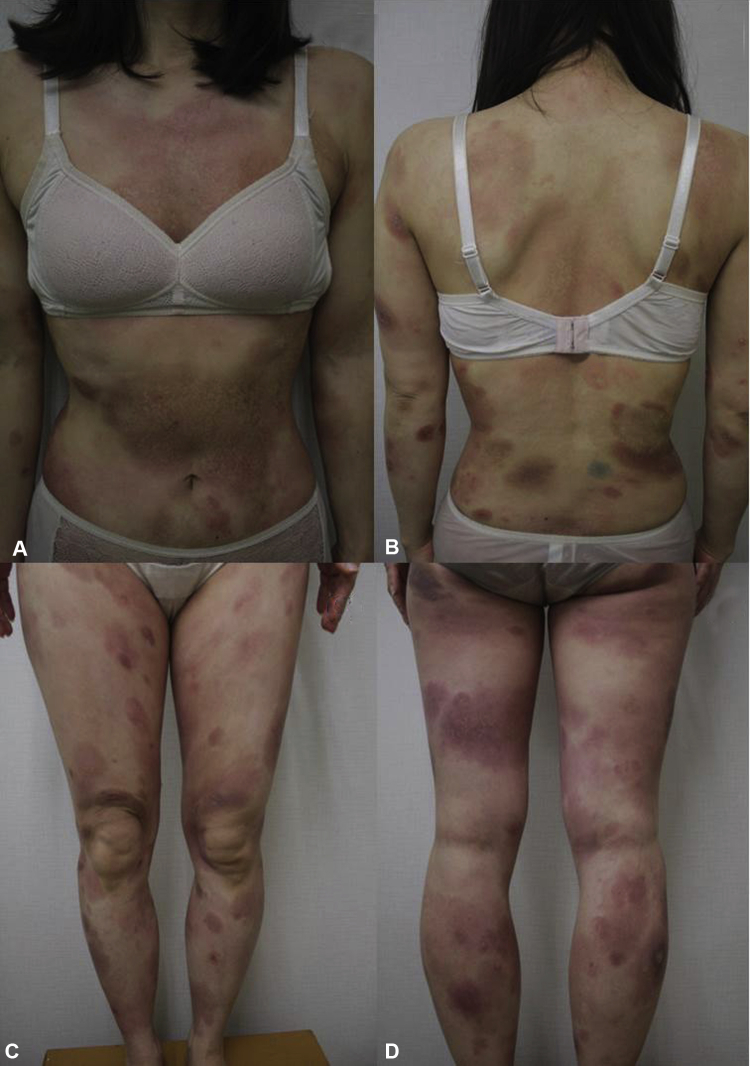
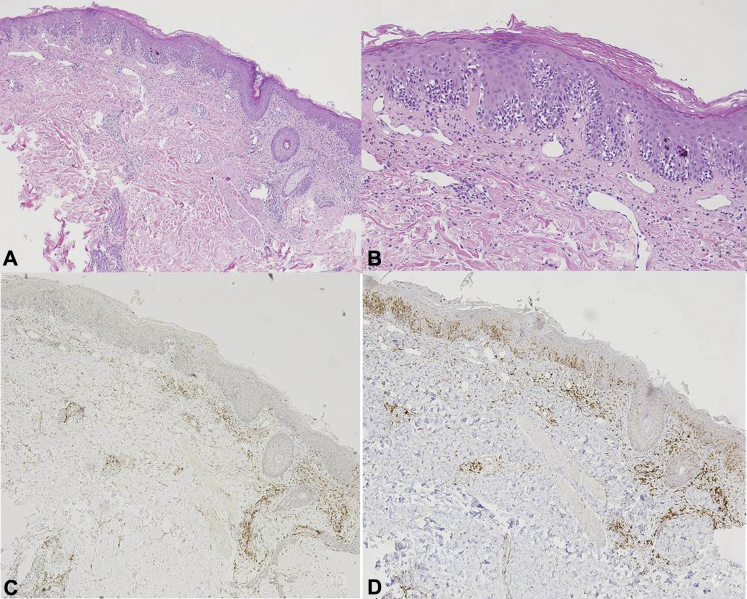
A 40-year-old woman visited our clinic because of erythematous and poikilodermatous patches of various sizes on the extremities and trunk of 1 years' duration (Fig 1, A through D). The affected body surface area was calculated by 2 dermatologists to be 40%. Skin biopsy examination of the lesions indicated atypical lymphocytes that were surrounded by a clear halo located along the dermoepidermal junction and on the epidermis (Fig 2, A and B). The skin lesions remained stationary during low-dose systemic steroid treatment. However, they were suddenly aggravated and increased size, and vegetative plaques were seen 2 months later (Fig 3, B through D). Because of the aggravation of the lesions, an additional skin biopsy found similar features of the previous condition (epidermotropism with haloed cells). Immunohistochemical analysis found CD4 negativity and CD8, CD30, and Ki-67 positivity (Fig 2, C and D). Monoclonality of the T-cell receptor gene rearrangement was found, and CD8+ MF was diagnosed. Although the patient had been treated with phototherapy, a systemic retinoid, and methotrexate for 2 months, the skin lesions were more aggravated and had a thick crust with eroded and vegetative plaques. The patient underwent further examinations to determine systemic involvement of extracutaneous lymphoma. Bone marrow biopsy results showed no evidence of lymphoma involvement, but a sigmoid colon mass was detected by abdominal computed tomography (Fig 3, A); biopsy of the mass found an adenocarcinoma. Stage IIIc sigmoid colon cancer with stage IB of MF was finally diagnosed and she underwent surgical resection and treatment with 12 cycles of FOLFOX chemotherapy (folinic acid, fluorouracil, oxaliplatin). After colon cancer treatment, the aggravated skin lesions improved and the vegetative plaques resolved to brownish patches, similar to their appearance during the first visit. Since then, her MF has been well controlled with phototherapy.
Fig 1.
Multiple erythematous and poikilodermatous patches on the entire body.
Fig 2.
Atypical lymphocytes characterized by hyperchromatic nuclei and clear halos infiltrating the basal layers (A, B). Immunohistochemical staining showed neoplastic lymphocytes with CD4 negativity (C) and CD8 positivity (D). (A and B, Hematoxylin-eosin stain. C, CD4 stain. D, CD8 stain. Original magnifications: A, C, and D, ×40; B, ×100.)
Fig 3.
A, Positron emission tomography–computed tomography shows a hypermetabolic lesion on the sigmoid colon. B through D, Skin lesions aggravated to eroded and vegetative plaques on the erythematous base, with thick crust on the preexisting patches.
Discussion
MF is the most common type of CTCL. It is clinically categorized in patch, plaque, and tumor stages. During the early patch stage, there are single or multiple erythematous macules and patches that vary in size and color.1 Histologically, the epidermis shows epidermotropism, which comprises small to medium atypical lymphocytes with enlarged hyperchromatic and clear cytoplasm (haloed cells). The neoplastic T cells in MF are usually mature CD4+ T cells, and approximately 20% of cases of early MF involve the CD8+ phenotype.2 The clinical behavior of CD8+ MF is similar to that of the CD4+ type, which is indolent.1 The condition may remain in the early patch stage or plaque stage for months or years before progressing to the tumor stage. Therefore, the diagnosis of early-stage MF is often challenging because of its overlapping clinical and histologic findings with various reactive dermatoses.1 In contrast to the indolent course, according to the World Health Organization– European Organisation for Research and Treatment of Cancer classification,2 there are CD8+ cutaneous lymphomas with aggressive behavior and poor prognoses that are categorized as primary aggressive epidermotropic CD8+ cytotoxic CTCL.
In this case, the skin lesions had a rapidly aggravated course and poor response to standard treatments. We first suggested that the condition might be primary aggressive epidermotropic CD8+ cytotoxic CTCL rather than classic MF because of the violent behavior. However, primary aggressive epidermotropic CD8+ cytotoxic CTCL does not have longstanding precursor lesions and does not follow the typical progression from the patch and plaque stages to the tumor stage, unlike MF.3, 4 The histologic appearance is different from that of classic MF in that the epidermis commonly shows keratinocyte necrosis, and atypical lymphocytes infiltrate deeply into a subcutaneous fat layer with destruction of adnexal skin structures.4 It was incidentally that we found the sigmoid colon cancer during the workup for systemic lymphoma involvement. The pathologic finding was an adenocarcinoma, not a lymphoma. We then hypothesized that the sudden aggravated skin lesions might be a cutaneous manifestation of paraneoplastic syndrome. According to the criteria proposed by Curth,5 there is a specific type of neoplasia that occurs with paraneoplasia and a high frequency of association between both conditions.6 Our patient had erythematous eroded vegetative plaques rimmed with a thick crust that resembled pyoderma gangrenosum, especially on the leg. However, paraneoplastic pyoderma gangrenosum with colorectal cancer has been rarely reported7 and the frequency of association between them is unlikely high enough. In addition, the histologic feature was different from those of pyoderma gangrenosum. We finally suggest that the skin lesions associated with indolent CD8+ MF could have been aggravated because of the hidden malignancy. Cytokine secretion and a triggered immune response to antigens expressed in the tumor are thought to be responsible for the deterioration of the cutaneous lesions.6 Several previous studies suggested that there is increased risk for secondary malignancy development in MF patients.8, 9, 10 Kantor et al10 reported the increased risks for colon cancer among patients with CTCL.10 However, in recent large cohort studies, the results did not prove an increased rate of colon cancer in MF patients.8, 9 Few reported cases describe clinical changes in MF patients with other malignancy. To our knowledge, only 1 case of MF with lung cancer has been reported that accounts for clinical features without significant change in skin lesions after surgical resection of lung cancer.11 In contrast, this patient's skin lesions were dramatically improved after resection of the colon cancer and continued to maintain improved state during FOLFOX chemotherapy. The FOLFOX agents have not been used as chemotherapy choices for MF. We considered removal of the colon mass to have contributed more to the improvement of the skin lesions than did the chemotherapy.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Song S.X., Willemze R., Swerdlow S.H., Kinney M.C., Said J.W. Mycosis Fungoides Report of the 2011 Society for Hematopathology/European Association for Haematopathology Workshop. Am J Clin Pathol. 2013;139:466–490. doi: 10.1309/AJCPOBDP2OQAJ5BR. [DOI] [PubMed] [Google Scholar]
- 2.Massone C., Crisman G., Kerl H., Cerroni L. The prognosis of early mycosis fungoides is not influenced by phenotype and T-cell clonality. Br J Dermatol. 2008;159:881–886. doi: 10.1111/j.1365-2133.2008.08761.x. [DOI] [PubMed] [Google Scholar]
- 3.Gormley R.H., Hess S.D., Anand D., Junkins-Hopkins J., Rook A.H., Kim E.J. Primary cutaneous aggressive epidermotropic CD8+ T-cell lymphoma. J Am Acad Dermatol. 2010;62:300–307. doi: 10.1016/j.jaad.2009.02.035. [DOI] [PubMed] [Google Scholar]
- 4.Nofal A., Abdel-Mawla M.Y., Assaf M., Salah E. Primary cutaneous aggressive epidermotropic CD8 T-cell lymphoma: Proposed diagnostic criteria and therapeutic evaluation. J Am Acad Dermatol. 2012;67:748–759. doi: 10.1016/j.jaad.2011.07.043. [DOI] [PubMed] [Google Scholar]
- 5.Curth HO. Skin lesions and internal carcinoma. In: Andrade R, Gumport SL, Popkin GL, Rees TD, editors. Cancer of the Skin. WB Saunders; Philadelphia: 1976. pp. 1308–1309. [Google Scholar]
- 6.Silva J.A., Mesquita Kde C., Igreja A.C. Paraneoplastic cutaneous manifestations: concepts and updates. An Bras Dermatol. 2013;88:9–22. doi: 10.1590/S0365-05962013000100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed K., Raman S., Pathma-Nathan N. Pyoderma gangrenosum: A paraneoplastic syndrome associated with occult colorectal malignancy? Report of a case and review of literature. Arch Clin Exp Surg. 2015;4:226–230. [Google Scholar]
- 8.Huang K.P., Weinstock M.A., Clarke C.A., McMillan A., Hoppe R.T., Kim Y.H. Second lymphomas and other malignant neoplasms in patients with mycosis fungoides and Sezary syndrome: evidence from population-based and clinical cohorts. Arch Dermatol. 2007;143:45–50. doi: 10.1001/archderm.143.1.45. [DOI] [PubMed] [Google Scholar]
- 9.Brownell I., Etzel C.J., Yang D.J., Taylor S.H., Duvic M. Increased malignancy risk in the cutaneous T-cell lymphoma patient population. Clin Lymphoma Myeloma. 2008;8:100–105. doi: 10.3816/CLM.2008.n.011. [DOI] [PubMed] [Google Scholar]
- 10.Kantor A.F., Curtis R.E., Vonderheid E.C. Risk of second malignancy after cutaneous T-cell lymphoma. Cancer. 1989;63:1612–1615. doi: 10.1002/1097-0142(19890415)63:8<1612::aid-cncr2820630828>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 11.Nagase K., Shirai R., Okawa T., Inoue T., Misago N., Narisawa Y. CD4/CD8 Double-negative mycosis fungoides mimicking erythema gyratum repens in a patient with underlying lung cancer. Acta Derm Venereol. 2014;94:89–90. doi: 10.2340/00015555-1618. [DOI] [PubMed] [Google Scholar]