Abstract
Introduction:
Tuberculosis (TB) is a significant cause of morbidity and mortality among children. The vague symptoms, the uncertain diagnostic tests and lack of adequate awareness among families all contributed in masking the actual prevalence of the disease. The objective of this study was to describe the epidemiology of childhood TB in River Nile State (RNS), North Sudan.
Methods:
All registered cases of TB aged 15 years and below, at the 13 management units in RNS during 3 years, 2011–2013 were included. The records included epidemiological, clinical, and microbiological data.
Results:
Out of the 1221 total TB notified cases, children were 187 (15.3%); almost equally distributed across the 3 years of the study period. Males were 56.7%. Most of the cases (89.9%) were newly diagnosed; among them, pulmonary TB (PTB) constituted 61.5%. Sputum specimen was tested in 59.4% (111/187) of cases, and only 15.3% (17/111) of specimens were sputum smear positive for new cases. The cure rate was (76.5%), and the treatment success rate was (88.2%). The death rate was 6.1% among PTB cases and 5.6% among extra-pulmonary cases. All the 20 (10.7%) children tested for HIV were negative.
Conclusion:
TB is under-reported in RNS and treatment outcomes are sub-optimal. Strategies to identify the active case-detection among children are recommended.
Key words: Childhood tuberculosis, River Nile State, Sudan
INTRODUCTION
Tuberculosis (TB) is one of the major infections affecting children worldwide.[1] It causes significant morbidity and mortality, especially in infants and young children. However, accurate information on the extent and distribution of disease in children is not available for most of the world.[1,2] Factors such as overcrowding, poverty, and the HIV epidemic have all contributed to the resurgence of TB globally.[2] Indeed, the highest rates of TB occur in resource-poor countries.[3]
Sudan alone carries 11–15% of the TB burden in the Eastern Mediterranean Region of the World Health Organization (WHO).[4] The estimated incidence of new TB cases in 2010 was 119/100,000 populations, and the estimated prevalence was 209/100,000 causing an overall death rate of 24/100,000 annually.[4] The exact number of deaths among children is not known, but its important to emphasize that TB is an important disease affecting child survival.[5]
The natural history and clinical expression of infection of TB differ substantially in children compared with adults.[6] It is difficult to confirm the diagnosis of TB by current microbiological methods. Even in industrialized countries, the triad of a positive tuberculin skin test, radiographic and/or clinical manifestations consistent with TB, and establishing a recent link to a known infectious case of TB is the “gold standard” for diagnosis.[7]
Furthermore, poor ascertainment and reporting of cases of TB prevent accurate estimation of the global burden of disease among children. While overdiagnosis is a possibility, the majority of cases is not diagnosed, especially where children with TB can access services only through referral hospitals.[8] It is important to mention that TB in young children indicates recent infection rather than secondary reactivation.[1,2,3,4,5,6,7,8]
The aim of this work was to describe the epidemiology of TB among children in RNS, North Sudan; we believe that, in low-resource settings, such as our country, epidemiological data can be used to monitor TB transmission in the community and to evaluate the effectiveness of the National TB Control programme.
METHODS
Settings
River Nile State (RNS) lies in North Sudan, (32–36° N and 16–22° E), covering an area of 124,000 km2, and the population is about 1,250,000 composed of different ethnic groups. The most important cities are Ed Damer, Atbara, Shendi, Berber and Abu Hamad. There are seven working TB Management Units (TBMUs), integrated within the general health system and distributed over the seven localities of the state, staffed with medical and nursing personnel, and social workers. TBMUs are the institutions where suspected TB patients are diagnosed and treated.
Data collection tools
Data were collected from the TB records, at the TBMUs. The records included the following epidemiological, clinical, and microbiological data: Name, age, sex, residence, centre of diagnosis and management, referral source, date of presentation, site of the disease, signs and symptoms with duration, whether new or re-treatment case, sputum microscopy tests initially and periodically, other diagnostic methods, treatment category, time of sputum conversion, treatment outcomes, and HIV status. In RNS, TB is diagnosed using a combination of a patient history, physical examination, and diagnostic tests, including sputum microscopy, chest X-ray, and tissue samples.
Data analysis
A descriptive analysis for the selected variables was performed using SPSS computer program version 20.0 (IBM Statistics, Chicago, IL). The frequency distribution of the different variables and the percentages of cases with data on these variables was calculated. Age was characterized by mean and standard deviation. P < 0.05 was considered statistically significant for comparing proportions.
Ethical issues
Ethical approval was obtained from the Ethical Committee of the Faculty of Medicine and Health Sciences, Nile Valley University.
RESULTS
During the 3-year period of study, 187 children (15 years and below) were registered in the records of the TB control program in RNS, out of the 1221 total cases during the same period, representing (15.3%). Almost equal number of cases were diagnosed every year, 62, 60, 65 in the years 2011, 2012, and 2013, respectively. This distribution gives a rough case notification rate of 5/100000 population. Males constituted 56.7% with a male to female ratio of 1.3:1. Seven TMBUs cases were diagnosed. However, most cases in this study, 53.5% (100/187) were diagnosed in Atbara center [Table 1]. Concerning the type of patients at the start of treatment, 89.9% (168/187) were new TB cases, 3.2% (6/187) were relapses, and only one case (0.5%) was a defaulter [Table 2].
Table 1.
Sociodemographic characteristics of registered children with tuberculosis in River Nile State, Sudan 2011-2013 (n=187)
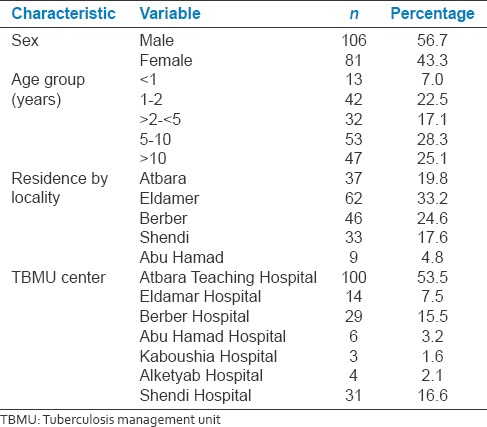
Table 2.
The clinical characteristics of children with tuberculosis in River Nile State, Sudan 2011-2013 (n=187)
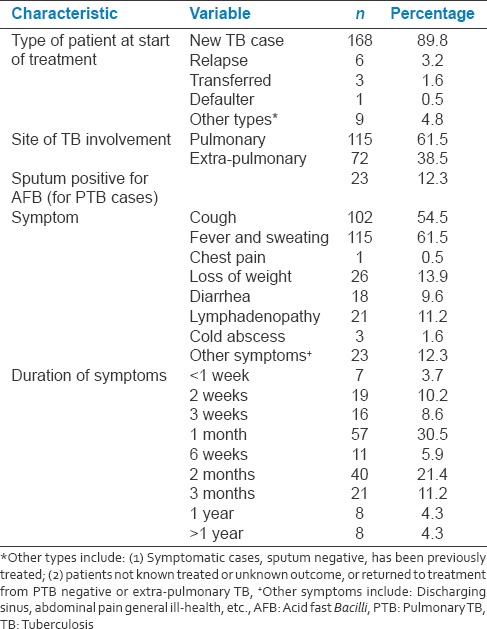
Pulmonary TB (PTB) cases were 61.5% (115/187) and extra-pulmonary cases were 38.5% (72/187).
The total number of children tested for sputum were 59.4% (111/187); among them, only 15.3% (17/111) were sputum smear-positive new cases and 84.7% (94/111) were new sputum smear-negative cases.
The treatment outcome for children was displayed in Table 3. However, due to the limited number of new sputum smear-positive cases, all indicators of the control program were sub-optimal. When considering the WHO indicators for the assessment of the control program outcomes that takes into account only new sputum smear-positive cases as a denominator; the cure rate was (76.5%), and the treatment success rate was (88.2%). For comparison, when considering the whole cohort of PTB cases, the cure rate was 12.2%, and treatment completion rate was 63.5%.
Table 3.
Treatment outcome of children with tuberculosis in River Nile State, Sudan 2011-2013 (n=187)
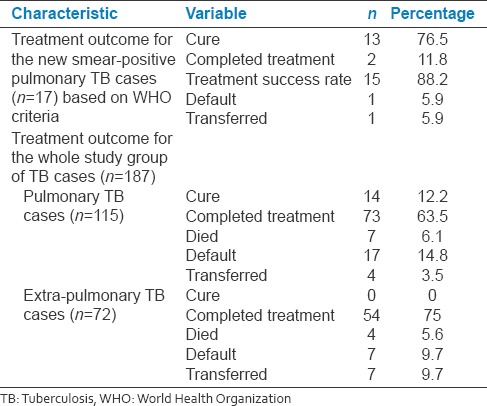
The death rate was 6.1% among PTB cases and 5.6% among extra-pulmonary cases [Table 3]. All 20 (10.7%) children tested for HIV were negative.
DISCUSSION
TB is one of the greatest challenges for all health authorities across the globe. In this study, among the 1221 total cases of TB reported in RNS, children were 187 (15.3%). It is to be mentioned that globally, the WHO estimated the prevalence of childhood TB is around 6% of total cases.[9] Our finding is higher than the reported global burden of TB in children. For instance, among the 4,452,860 new cases reported in 2010 by the 22 countries with the highest burden of TB, only 157,135, (3.5%) (range, 0.1–15.0%), of the cases were children. There is general agreement in literature that the best estimates suggest that children account for approximately 11% of the burden of disease from TB.[1,7] In addition, it is estimated that only 50% of cases of childhood TB was notified to the National Control programmes. This low notification rate was attributed to many factors, including the nonspecific symptoms in children, the uncertain diagnosis, poor accessibility to health facilities, poverty, and unawareness among families.[10] It is plausible to suggest that these same factors are also contributing to the high incidence of childhood TB expected in Sudan and to the low reporting rate as well.
To overcome this obstacle, the WHO launched the “roadmap for childhood TB” to improve case-detection, diagnosis, and treatment outcome, and also advocates for better commitment and accountability at all levels of the health system and the community.[11] In this context, active case finding activities of proven yield included: Household contact screening, private-public mix services, mobile health chest maps, community home-based care visits, and screening of children at school in addition to safe motherhood health services.[10]
It is to be mentioned that age per se has an important impact in the natural history of disease progression. For instance, in our study, children < 2 years were minority (7.6%) when compared to those more than 5 years (45%). This finding has been attributed to the natural history of TB in children which differs substantially in the two age groups.[12] Primary infection before 2 years of age frequently progresses to serious disease within the first 12 months without significant prior symptoms. Whereas primary infection between 2 and 10 years of age rarely progresses to serious disease, and such progression was associated with significant clinical symptoms. In children aged more than 3 years, the presence of symptoms represented a high chance to establish a clinical diagnosis before serious disease progression. Primary infection after 10 years of age frequently progresses to adult-type disease.[13]
In this study, cough was reported in 54.5% while fever and sweating were reported in 61.5%. It has been stated that with airway involvement, the usual presenting symptom is a persistent, nonremitting cough that is unresponsive to the treatment for the likely alternative causes.[13] Clinical signs are often subtle, and no diagnostic scoring system has been adequately verified.[14]
The duration of symptoms varies, but most cases (96.3%) run a chronic coarse (more than 2 weeks) before establishing diagnosis while only (3.7%) were diagnosed within 1 week duration. This delay could be explained by the natural history of TB and both the variations in susceptibility to disease and the diverse spectrum of clinical manifestations observed in children due to the sequence of events that follows primary infection with Mycobacterium tuberculosis.[13]
Microscopical examination of sputum for bacteriologic confirmation was only used in (27.3%) of the studied children; this could be due to the difficulty of collecting spontaneously produced sputum in children. In addition, a gastric aspiration that needs training, and hospital setting was not feasible at the diagnostic centers in our settings. DOTS/STOP TB strategies have been effective epidemiological tools in targeting sputum smear-positive cases in adults. However, children deemed to be ignored as they are unable to produce sputum. Therefore, children contribute very little to transmission within communities.[15,16,17]
Chest radiography was used in 44.9% of cases as X-ray has always been highly suggestive of a diagnosis of PTB but it depends on technical quality and facilities which are major challenges in developing countries. Another investigation used in the studied children was fine-needle aspiration biopsy, which was used in (5.9%). This technique was proven useful in children with a peripheral lymph-node mass.[18,19]
In our study, we identified PTB in 61.5% of the cases while the remaining 38.5% were extra-PTB. This percentage is less than that reported in South Africa, 76.7% for pulmonary and 25% for extra-thoracic TB while in the USA 73.6% was PTB and 18.7% were extra-PTB.[20,21] These variations may be attributed to disease prevalence as well as the availability of methods of early diagnosis and early notification. Furthermore, many studies highlighted the difficulty in confirmation of the disease in children that resulted in poor reporting, especially in endemic areas with limited resources.[22,23] This poor reporting has been identified as a major factor contributing to the poor treatment indicators.[8]
The outcome of treatment in this study was generally sub-optimal. For the new smear-positive pulmonary cases, the cure rate and treatment completion rate were 76.5% and 88.2% respectively. However, due to the scarcity of new smear-positive cases among children, we also calculated the treatment outcome for the whole cohort, i.e., all cases underwent sputum testing as a denominator and not only the new cases. By doing so, the cure rate and treatment completion rate dropped to 12.2% and 63.5%, respectively.
Despite the fact that children with TB respond well to and tolerate the same basic treatment regimens as used for adults,[7] the situation is sub-optimal in our settings. This was evidenced by the fewer number of children achieving required treatment targets. Here, poor compliance with treatment may constitute a contributing factor.
This study has some limitations. The cross-sectional design may reflect only temporal associations. In addition, a health facility-based study is another limitation that may not allow generalizations to be made about the exact situation in the community. However, with the limited resources in our setting, other alternative ways to survey the community are not feasible. It is possible to consider the small sample size as one limitation of this study; however, this was the total number of cases notified to the control program during study period. It is well reported in literature that diagnosis of TB in children is an ambiguous area[15,23] in addition to problems of data recording in TB registries at TBMUs. Despite these limitations, we assume that this study is the first of its kind in Sudan, reflecting the epidemiology of childhood TB with special emphasis on the assessment indicators of the control program of DOTS/STOP TB strategies. We recommend further studies to explore the whole picture in our country, hopefully, using “intensified case-detection” strategies.
CONCLUSION
The epidemiology of childhood TB in RNS as in many other developing countries is masked by many factors that result in low case-detection rate, poor ascertainment of diagnosis, and sub-optimal treatment outcome.
Financial support and sponsorship
This study was partially funded by the Swiss Embassy in Khartoum, Small Action Fund 2013.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
we are thankful to the Swiss Embassy for financing this work. Our thanks are extended to the administrators and statisticians at the State Ministry of Health, RNS for their collaboration.
REFERENCES
- 1.Nelson LJ, Wells CD. Global epidemiology of childhood tuberculosis. Int J Tuberc Lung Dis. 2004;8:636–47. [PubMed] [Google Scholar]
- 2.Walls T, Shingadia D. Global epidemiology of paediatric tuberculosis. J Infect. 2004;48:13–22. doi: 10.1016/s0163-4453(03)00121-x. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Styblo K, Rouillon A. Tuberculosis in developing countries: Burden, intervention and cost. Bull Int Union Tuberc Lung Dis. 1990;65:6–24. [PubMed] [Google Scholar]
- 4.World Health Organization. WHO/HTM/TB/2004.344. Geneva, Switzerland: World Health Organization; 2004. Compendium of indicators for monitoring and evaluating national tuberculosis programs. [Google Scholar]
- 5.Graham SM, Sismanidis C, Menzies HJ, Marais BJ, Detjen AK, Black RE. Importance of tuberculosis control to address child survival. Lancet. 2014;383:1605–7. doi: 10.1016/S0140-6736(14)60420-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shingadia D, Novelli V. Diagnosis and treatment of tuberculosis in children. Lancet Infect Dis. 2003;3:624–32. doi: 10.1016/s1473-3099(03)00771-0. [DOI] [PubMed] [Google Scholar]
- 7.Marais BJ, Hesseling AC, Gie RP, Schaaf HS, Beyers N. The burden of childhood tuberculosis and the accuracy of community-based surveillance data. Int J Tuberc Lung Dis. 2006;10:259–63. [PubMed] [Google Scholar]
- 8.Marais BJ, Gie RP, Hesseling AC, Schaaf HS, Lombard C, Enarson DA, et al. A refined symptom-based approach to diagnose pulmonary tuberculosis in children. Pediatrics. 2006;118:e1350–9. doi: 10.1542/peds.2006-0519. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization. Global Tuberculosis Report 2014. Geneva: World Health Organization; 2014. [Last accessed on 2015 Jun 07]. Available from: http://www.who.int/tb/publications/global_report/en/ [Google Scholar]
- 10.Joshi B, Chinnakali P, Shrestha A, Das M, Kumar AM, Pant R, et al. Impact of intensified case-finding strategies on childhood TB case registration in Nepal. Public Health Action. 2015;5:93–8. doi: 10.5588/pha.15.0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. WHO/HTM/TB/2013.12. Geneva, Switzerland: World Health Organization; 2013. Roadmap for childhood tuberculosis. Towards zero deaths. [Google Scholar]
- 12.Starke JR. Seminars in Respiratory and Critical Care Medicine. New York, USA: Thieme Medical Publishers, Inc.; 2004. Tuberculosis in children. [DOI] [PubMed] [Google Scholar]
- 13.Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Obihara CC, Starke JJ, et al. The natural history of childhood intra-thoracic tuberculosis: A critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004;8:392–402. [PubMed] [Google Scholar]
- 14.Hesseling AC, Schaaf HS, Gie RP, Starke JR, Beyers N. A critical review of diagnostic approaches used in the diagnosis of childhood tuberculosis. Int J Tuberc Lung Dis. 2002;6:1038–45. [PubMed] [Google Scholar]
- 15.Marais BJ, Graham SM, Maeurer M, Zumla A. Progress and challenges in childhood tuberculosis. Lancet Infect Dis. 2013;13:287–9. doi: 10.1016/S1473-3099(13)70031-8. [DOI] [PubMed] [Google Scholar]
- 16.Maher D, Mikulencak M. WHO/CDS/CP/TB/99.270. Geneva, Switzerland: World Health Organization; 1999. What is DOTS? A guide to understanding the WHO-recommended TB control strategy known as DOTS. [Google Scholar]
- 17.Raviglione MC, Uplekar MW. WHO's new stop TB strategy. Lancet. 2006;367:952–5. doi: 10.1016/S0140-6736(06)68392-X. [DOI] [PubMed] [Google Scholar]
- 18.Almobarak AO, Elhoweris MH, Ahmed AH, Haroon MS, Adam EA, Elmadhoun WM, et al. Fine needle aspiration cytology for suspected tuberculous lymphadenitis: A feasible solution for a diagnostic dilemma in Sudan. Sudan J Med Sci. 2014;9:221–4. [Google Scholar]
- 19.Wright CA, Warren RM, Marais BJ. Fine needle aspiration biopsy: An undervalued diagnostic modality in paediatric mycobacterial disease. Int J Tuberc Lung Dis. 2009;13:1467–75. [PubMed] [Google Scholar]
- 20.Marais BJ, Gie RP, Schaaf HS, Hesseling AC, Enarson DA, Beyers N. The spectrum of disease in children treated for tuberculosis in a highly endemic area. Int J Tuberc Lung Dis. 2006;10:732–8. [PubMed] [Google Scholar]
- 21.Peto HM, Pratt RH, Harrington TA, LoBue PA, Armstrong LR. Epidemiology of extrapulmonary tuberculosis in the United States, 1993-2006. Clin Infect Dis. 2009;49:1350–7. doi: 10.1086/605559. [DOI] [PubMed] [Google Scholar]
- 22.Perez-Velez CM, Marais BJ. Tuberculosis in children. N Engl J Med. 2012;367:348–61. doi: 10.1056/NEJMra1008049. [DOI] [PubMed] [Google Scholar]
- 23.Graham SM. Chest radiography for diagnosis of tuberculosis in children: A problem of interpretation. Int J Tuberc Lung Dis. 2014;18:757. doi: 10.5588/ijtld.14.0354. [DOI] [PubMed] [Google Scholar]


