Abstract
Background:
The Rhesus (Rh) blood group system is one of the most polymorphic and immunogenic systems known in humans, because of its immunogenicity along with ABO grouping, RhD antigen testing was made mandatory before issuing a compatible blood. At present, there are five major antigens, i.e., D, C, E, c, and e in Rh blood group system.
Aims:
The aim of this study is to provide essential data about the distribution of the major Rh antigens and the most common phenotype among the Saudi population.
Materials and Methods:
This is a retrospective study to evaluate the Rh grouping and Rh sub-groups performed among some donors who donated blood or blood products at the department of donation center at King Abdulaziz Medical City Riyadh, Saudi Arabia from January 1, 2014 to December 31, 2014. Sample size included 600 donors. Donors are males and females and their ages are above 18 years.
Results:
The incidence of RhD was 84.8% and only 15.2% of samples were negative for D antigen. The Incidence of other Rh antigens C, E, c, and e were 62.3%, 23.5%, 74.3%, and 95.0%, respectively. The most common phenotype among RhD positive donors was DCcee (28.7%) and among RhD negative donors was dccee (13.7%). However, three donors (0.5%) were negative for antithetical antigens C and c.
Conclusion:
This study shows that there is a wide racial and geographical variation in the distribution of Rh antigens and phenotypes among study participants. The Rh blood group system has a vital role in population genetic study and in resolving medical legal issues and more importantly in transfusion medicine practice.
Key words: Antigens, blood group, phenotypes, Rhesus
INTRODUCTION
Study of Rhesus (Rh) blood group antigens, phenotype, and Rh antibodies is very useful in routine and advanced clinical practice in blood transfusion centers. Moreover, it can be used for population genetic studies.[1,2] The typing of blood group antigens and determination of phenotype for blood and blood components are a prerequisite for an efficient and safe blood transfusion.[3,4] Rh antibodies are usually immunoglobulin G, and they are produced early during life.[5,6,7]
The frequency of Rh antigens and developed Rh antibodies in patients after blood transfusion or after adverse transfusion reactions have been the theme of research in blood transfusion medicine.[8,9,10,11] Blood group antigens issues related to blood transfusion medicine are very interesting and complex. In addition, the investigation of those antigens have much to offer to blood banking, making the role of workers in transfusion medicine more important in clinical practice.[5,10,11]
Unfortunately, there are few systematic search for antigens C, c, e, E, and Rh phenotypes in the donor and recipient, thereby exposing the transfused patient to high risk of alloimmunization.[12]
Based on available information and reviewing of published papers, the occurrences of alloimmunization in massive transfusion patients are <4%.[13] Recipients and patients who develop alloantibodies due to incompatible blood transfusion in their blood are at risk. This risk can be avoided by transfusing blood units that are negative for the antigens, which the alloantibodies have been produced and developed against. Blood units that have been antigen detected and cross-matched for these important Rh antigens will reduce the possibility of the complications and adverse transfusion reactions. Most of the alloantibodies are encountered during compatibility testing procedure in clinical practice and in most transfusion donation centers, are originally due to antigens that belong to Rh blood grouping systems.[14,15]
It is very important to study the frequencies of the different Rh antigens and Rh phenotypes concerning those who have developed multiple alloantibodies due to massive previous transfusions. This information is necessary to check the availability of blood units that lack the corresponding antigen(s). The current practice of providing compatible blood to patients in many areas is still depending on random cross matching of available units in the donation centers or availability of blood units from recipient relatives.
This study was conducted to provide sufficient data on the distribution of Rh blood groups antigens, their frequency, and the most common Rh phenotype among donors who donated blood or blood components at King Abdulaziz Medical City – Riyadh. These findings would assist in the planning and coordinating blood-transfusion services in the Kingdom of Saudi Arabia.
MATERIALS AND METHODS
This is a retrospective chart review study conducted to determine the frequency of Rh antigens and Rh phenotypes among donors donating blood or blood products at King Abdulaziz Medical City – Riyadh in the year 2014. Participants in this study included six hundred donors. Donors are males and females and their ages are above 18 years. The selection criteria are based on donating blood or blood products. Donors who did not donate blood or blood products were excluded. Finally, the raw data of RhD and Rh sub-groups antigens obtained were analyzed using SPSS version 20 (BM Corporation, Armonk, NY, USA) computer program.
RESULTS
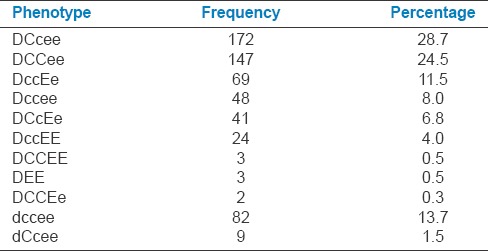
Participants in this study included 600 donors; donors are males and females and their ages above 18 years. The incidence of RhD positive was 84.8% and only 15.2% of samples were negative for D antigen. The Incidence of other Rh antigens, i.e., C, E, c, and e were 62.3%, 23.5%, 74.3%, and 95.0%, respectively [Figure 1 and Table 1]. The most common Rh phenotype among RhD positive donors was DCcee (28.7%) followed by DCCee (24.5%), and the lowest Rh phenotype among RhD positive was DCCEe (0.3%). The most common Rh phenotype among RhD negative donors was dccee (13.7%). Three donors (0.5%) were negative for antithetical antigens C and c [Table 2].
Figure 1.
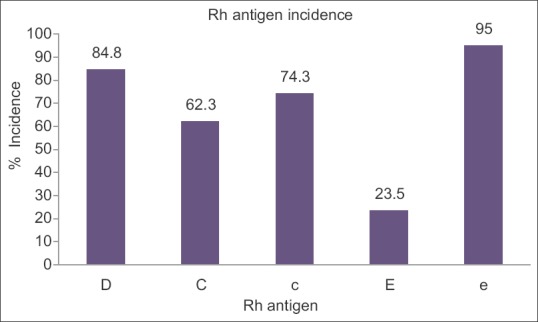
The incidence of Rhesus antigen in present study
Table 1.
The incidence of Rhesus antigen positive/negative in present study
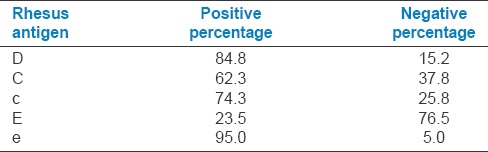
Table 2.
The frequency and percentage of Rhesus phenotypes
DISCUSSION
Rh antigens, Rh phenotypes, and Rh genes are different from one group of population to another due to ethnic variations as well as across different races.[9,10]
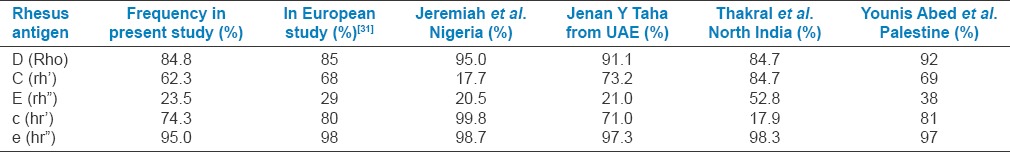
Rh antigens, Rh phenotypes, and Rh genes are different [Table 3] from one group of population to another due to ethnic variations as well as across different races.[9,10]
Table 3.
The frequency of Rhesus antigens in present study compared with different populations
Rh antigens and Rh phenotypes are stable during the human life, and the frequency of Rh blood group antigens and Rh phenotypes are very important among population. They could help in determining the availability of blood matching and the occurrence of hemolytic diseases in neonates. In addition, they could help in paternity and maternity testing for forensic purposes.[9,10] Therefore, frequency of different Rh antigens and Rh phenotypes are important and useful for proper management of blood transfusion medicine services.[11]
The Rh blood group system includes many immunogenic antigens that are located on variant forms of RhD and RhCE proteins. The genes responsible for the Rh proteins are located on the short arm of chromosome number one.[1,16,17] The immunologic responses to the major Rh antigens will be beneficial in the management and treatment of hemolytic disease.[17,18,19]
The frequency of D antigen in this study is 84.8% as compared to the findings in the US, France, and Nigeria where it was shown that the respective prevalence was 85.4%, 85%, and 81.5%, respectively.[20,21,22] D antigen frequency is higher in other sub and non-Saharan Africa countries.[23,24,25,26,27]
The frequency of the RhD negative in this study is 15.2%. These results disagree with the work of Joseph[28] who found that the D antigen negative is 7.28%, whereas Cabannes found that the D antigen negative values were ranging between 1.70 and 9.3% in sub-Saharan Africa.[29,30]
The frequencies of c and e antigens in this study are high (74.3 and 95%), whereas the frequencies of C and E antigens are lower 62.3% and 23.5%, respectively. Among whites European, and Asian people, e antigen is the most common, and next comes c antigen.[31] With regards to C and E antigens, their frequencies are higher than the results obtained in this study, which showed 62.3% and 23.5%, respectively.[22,25,31,32]
The most frequently encountered phenotype in this study is the phenotype DCcee (28.7%) among RhD positive blood donors and dccee 13.7% among RhD negative blood donors. This profile is different from that observed in the whites European where the phenotype DCCee or DCCEE are the most common ones.[22,33]
This study revealed that Rh antigenic profile, phenotype, and genotype along with antibody screening and their identification are very important factors before blood transfusion, especially in patients with history of massive transfusion and multi-parity females.
CONCLUSION
Our study shows that there is a wide range of racial and geographical variation in the distribution of Rh antigens and phenotypes. The Rh blood group system has vital role in population genetic study in resolving medical legal issues and more importantly in transfusion practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Levine P, Stetson RE. An unusual case of intra-group agglutination. JAMA. 1939;113:126–7. doi: 10.1001/jama.251.10.1316. [DOI] [PubMed] [Google Scholar]
- 2.Scott ML. The complexities of the Rh system. Vox Sang. 2004;87(Suppl 1):58–62. doi: 10.1111/j.1741-6892.2004.00431.x. [DOI] [PubMed] [Google Scholar]
- 3.Worlledge S, Ogiemudia SE, Thomas CO, Ikoku BN, Luzzatto L. Blood group antigens and antibodies in Nigeria. Ann Trop Med Parasitol. 1974;68:249–64. doi: 10.1080/00034983.1974.11686948. [DOI] [PubMed] [Google Scholar]
- 4.Jeremiah ZA, Buseri FI. Rh antigen and phenotype frequencies and probable genotypes for the four main ethnic groups in Port Harcourt, Nigeria. Immunohematology. 2003;19:86–8. [PubMed] [Google Scholar]
- 5.Mollison PL, Engelfriet CP, Marcela C. Blood Transfusion in Clinical Medicine. 10th ed. United Kingdom: Oxford Blackwell Scientific Publications; 1997. [Google Scholar]
- 6.Mouro I, Colin Y, Chérif-Zahar B, Cartron JP, Le Van Kim C. Molecular genetic basis of the human Rhesus blood group system. Nat Genet. 1993;5:62–5. doi: 10.1038/ng0993-62. [DOI] [PubMed] [Google Scholar]
- 7.Hoffbrand AV, Pettit AE. Postgraduates Hematology. 4th ed. London: British Library; 2001. [Google Scholar]
- 8.Elsayid M, Aseeri YY, Saqri FA, Alanazi A, Qureshi S. A study of prevalence of blood group of Saudi Patients in King Abdulaziz Medical City, Riyadh. Sci J Public Health. 2015;3:559–62. [Google Scholar]
- 9.Reddy KS, Sudha G. ABO and Rh(D) blood groups among the Desuri Reddis of Chittur District, Andhra Pradesh. Anthrapologists. 2009;11:237–8. [Google Scholar]
- 10.Brown TA. Genetics: A molecular approach. Singapore: Fong and sons printers; pp. 309–27. [Google Scholar]
- 11.Dacie JV, Lewis SM. Practical hematology. In: Lewis SM, Bain BJ, Bates I, editors. Practical Hematology. 9th ed. London: Churchill Livingstone, Harcourt Publishers Limited; 2001. pp. 444–51. [Google Scholar]
- 12.Akre DP, Seka-Seka J, Dassew SR. Alloimmunisation anti-erythrocytes post transfusion – Among sickle cell disease followed at the CHU OF Cocody Abidjan. J Sci Pharm Biol. 2008;9:64–70. [Google Scholar]
- 13.Schonewille H. Red Blood Cell Alloimmunization After Blood Transfusion. Leiden: University Press; 2008. [Google Scholar]
- 14.Frohn C, Dümbgen L, Brand JM, Görg S, Luhm J, Kirchner H. Probability of anti-D development in D- patients receiving D+RBCs. Transfusion. 2003;43:893–8. doi: 10.1046/j.1537-2995.2003.00394.x. [DOI] [PubMed] [Google Scholar]
- 15.Klein HG, Anstee D, editors. Mollison's blood transfusion in clinical medicine. 11th ed. Oxford, United Kingdom: Blackwell Publishing Ltd; 2005. pp. 163–208. The Rh blood group system (and LW) [Google Scholar]
- 16.Sharma DC, Rai S, Iyenger S, Jain B, Sao S. Prevalence and distribution of ABO and Rh-D Antigens along with its Subgroups and rare types in greater Gwalior Region. OJBD. 2013;2:69–73. [Google Scholar]
- 17.Landsteiner K, Wiener AS. An agglutinable factor in human blood recognized by immune sera for rhesus blood. Proc Soc Exp Biol Med. 1940;43:223. [Google Scholar]
- 18.Fisk RT, Foord AG. Observations on the Rh agglutinogen of human blood. Am J Clin Pathol. 1942;12:545–52. [Google Scholar]
- 19.Levine P, Celano MJ, Wallace J, Sanger R. A human “D-like” antibody. Nature. 1963;198:596–7. doi: 10.1038/198596a0. [DOI] [PubMed] [Google Scholar]
- 20.Falusi AG, Ademowo OG, Latunji CA, Okeke AC, Olatunji PO, Onyekwere TO, et al. Distribution of ABO and RH genes in Nigeria. Afr J Med Med Sci. 2000;29:23–6. [PubMed] [Google Scholar]
- 21.Garratty G, Glynn SA, McEntire R. Retrovirus Epidemiology Donor Study. ABO and Rh (D) phenotype frequencies of different racial/ethnic groups in the United States. Transfusion. 2004;44:703–6. doi: 10.1111/j.1537-2995.2004.03338.x. [DOI] [PubMed] [Google Scholar]
- 22.Bogui LS, Dembele B, Sekongo Y, Abisse S, Konaté S, Sombo M. Phenotypic Profile of Rh and Kell Blood Group Systems among Blood Donors in Cote d'Ivoire, West Africa. J Blood Transfus. 2014;2014:4. doi: 10.1155/2014/309817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamed CT, Bollahi MA, Abdelhamid I, Med Mahmoud MA, Ba B, Ghaber S, et al. Frequencies and ethnic distribution of ABO and Rh (D) blood groups in Mauritania: Results of first nationwide study. Int J Immunogenet. 2012;39:151–4. doi: 10.1111/j.1744-313X.2011.01064.x. [DOI] [PubMed] [Google Scholar]
- 24.Mandengue SH, Lehman Leopold G, Assomo-Ndemba P, Mbangue G. Distribution of antigens M” of systems ABO, rhesus MNSs, Kell, and Duffy in blood donors drepanocytaires and blood volunteers to Douala (Cameroon): Risks of adverse transfusion reactions, “medicine of black Africa. 2003;50:22–4. [Google Scholar]
- 25.Loua A, Lamah MR, Haba NY, Camara M. Frequency of blood groups ABO and rhesus D in the Guinean population. Transfus Clin Biol. 2007;14:435–9. doi: 10.1016/j.tracli.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 26.Randriamanantany ZA, Rajaonatahina DH, Razafimanantsoa FE, Rasamindrakotroka MT, Andriamahenina R, Rasoarilalamanarivo FB, et al. Phenotypic and allelic profile of ABO and Rhésus D blood group system among blood donor in Antananarivo. Int J Immunogenet. 2012;39:477–9. doi: 10.1111/j.1744-313X.2012.01120.x. [DOI] [PubMed] [Google Scholar]
- 27.Keramati MR, Shakibaei H, Kheiyyami MI, Ayatollahi H, Badiei Z, Samavati M, et al. Blood group antigens frequencies in the northeast of Iran. Transfus Apher Sci. 2011;45:133–6. doi: 10.1016/j.transci.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Joseph SS. Contribution to the study of blood groups to the erythrocyte in Côte d'Ivoire. Inventory and repartition according to ethnic origin [Thesis medicine], Faculty of Medicine, Abidjan, Côte d'Ivoire. 1985 [Google Scholar]
- 29.Cabannes R. Hematology of the ethnic background of the Côte d'Ivoire. Its contribution to the knowledge of the populations of this country, of Medicine of black Africa, 1981;28:65–72. [Google Scholar]
- 30.Cabannes R, Senarail has Pene F, Sangare has, Sombo Mr. Kple hémotypologique Faget, Study of the populations of the West Africa. Particular reference to Ivorian population and Peulh of West Africa. Annals of the University of Abidjan. Series B, Medicine. 1979;13:11–6. [Google Scholar]
- 31.Kahar MA, Patel RD. Phenotype frequencies of blood group systems (Rh, Kell, Kidd, Duffy, MNS, P, Lewis, and Lutheran) in blood donors of South Gujarat, India. Asian J Transfus Sci. 2014;8:51–5. doi: 10.4103/0973-6247.126693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agarwal N, Thapliyal RM, Chatterjee K. Blood group phenotype frequencies in blood donors from a tertiary care hospital in North India. Blood Res. 2013;48:51–4. doi: 10.5045/br.2013.48.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daniels G. Human Blood Group. 2nd ed. Hoboken, NJ, USA: John Willey & Sons; 2002. [Google Scholar]


