Abstract
Historically, obesity was thought to be advantageous for maintaining healthy bones due to the greater BMD observed in overweight individuals. However, recent observations of increased fracture in some obese individuals has led to concern that common metabolic complications of obesity, such as type 2 diabetes, metabolic syndrome, impaired glucose tolerance, insulin resistance, hyperglycemia, and inflammation may be associated with poor bone health. In support of this hypothesis, greater visceral fat, a hallmark of insulin resistance and metabolic syndrome, is associated with lower BMD. Research is needed to determine if and how visceral fat and/or poor metabolic health are causally associated with bone health. Clinicians should consider adding a marker metabolic health, such as waist circumference or fasting plasma glucose concentration, to other known risk factors for osteoporosis and fracture.
Keywords: obesity, visceral fat, bone mineral density, fracture
Introduction
Historically, obesity was thought to be advantageous for maintaining healthy bones (1). Heavier individuals have greater bone mineral content (BMC) and bone mineral density (BMD), and statistically are at lower risk for osteoporosis. These observations were attributed to increased “loading” and characteristics of the endocrine environment. However, recent observations have indicated that in some cases obesity is associated with elevated fracture risk (2). We propose that these apparently discrepant observations are explained by the confounding effect of poor metabolic health. Obesity is associated with perturbations of metabolic health, including type 2 diabetes mellitus (T2DM), metabolic syndrome, impaired glucose tolerance, impaired fasting glucose, insulin resistance, hyperglycemia, and inflammation, as well as disruptions of the endocrine system (e.g., the growth factor and reproductive axes). Although greater body weight may be beneficial regarding bone size and density, the metabolic complications associated with obesity, particularly abdominal/visceral obesity, are likely to have adverse effects on qualitative aspects of bone health, such as structure and function. In this article, we will review and synthesize recent literature regarding obesity and bone health, including BMD, fracture risk, and qualitative aspects including geometry, strength, and microarchitecture. We will focus on articles that lend insight into the role of metabolic health, and interpret the results in the context of the characteristics of the study participants.
Children and adolescents
The effect of body fat on skeletal maturation has only recently emerged as an important area of investigation. Because bone integrity in childhood is likely to have biologically relevant effects on skeletal competence in advanced age (3), it is important to understand the factors, including obesity, that determine bone mass, geometry, and strength in childhood. An obligatory level of fat is required for the initiation of skeletal maturation, however excess adiposity, while associated with increased bone size may have an adverse effect on bone quality. Across the pubertal years, body fat has been associated with larger bones in boys, and larger and denser bones in girls (4). However, accelerated skeletal growth and greater bone size may not translate into reduced fracture risk. In fact, two recent studies reviewing the medical records of patients aged 2 to 19 yr showed that overweight and obese children had an increased odds ratio of fracture, with the association strongest in the 6-11 year-old age group (5, 6). Gender may affect the association between obesity and bone outcomes. In adolescents, fat mass was independently associated with cortical bone mass in girls but not boys (7). In girls, the prevalence of overweight/obesity was greater in individuals presenting with fracture at either upper or lower limb, but in boys, prevalence was greater only with fracture at the lower limb (8). Fat distribution and/or metabolic health may affect the association between adipose tissue and bone. Although total body fat was positively associated with BMC in overweight children, visceral fat and subcutaneous abdominal fat were inversely associated, and children with prediabetes had lower BMC than children who were normal glucose tolerant (9). During puberty, expansion of bone marrow adipose tissue (BMAT) is associated with bone anabolism. However in adults, greater BMAT is associated with lower BMD (10). Thus, whether obesity in childhood affects the trajectory of BMAT expansion, and thereby compromises bone strength, is a topic that requires research.
Pre-menopausal women
Studies in healthy premenopausal women indicate that fat distribution is associated with several measures of bone health, independently of obesity per se (11–15). Abdominal fat, visceral fat (VAT), and BMAT are adversely associated with bone health, conferring lower BMD, lower trabecular bone volume and stiffness, higher cortical porosity, and lower bone formation rate. In contrast, subcutaneous adipose tissue may be positively associated, or not associated, with measures of bone health. Although the mechanism for these divergent associations is not clear, it is possible that differential production of leptin, adiponectin, aromatase, or proinflammatory molecules could play a role. The observation that abdominal fat, VAT, and BMAT are associated with each other suggests coordinate regulation. It is possible that a metabolic insult, such as inflammation or oxidative stress, or an endocrine perturbation precipitates a global shift in allocation of resources from bone to fat, perhaps at the stage of mesenchymal stem cell differentiation. In support of a role for the endocrine system, serum concentrations of insulin-like growth factor-1 (IGF-1) were positively associated with BMD and a marker of bone formation (procollagen type 1 amino-terminal propeptide, P1NP), and inversely associated with VAT and BMAT. In premenopausal women, thigh muscle cross-sectional area and density were positively associated with BMD, suggesting that lean mass (not fat mass) is responsible for the positive association between obesity and BMD (11).
Postmenopausal women
Menopause is associated with an acute increase in bone remodeling that further increases with advancing age. Increased remodeling has been associated with increased skeletal fragility, and may in part explain greater fracture risk in older women. How obesity, with its suppressive impact on remodeling, interacts with the novel physiology of the postmenopausal years is not clear. Some reports suggest that obesity is protective against osteoporosis due to its promotion of greater BMD (16). Areal and volumetric BMD at multiple sites was noted to be higher in obese vs normal-weight postmenopausal women and positively associated with body fat (15, 17). Likewise, cortical thickness, trabecular number, trabecular distribution, and bone strength estimated by pQCT and micro-finite element analysis were more favorable in obese women. However, all differences were reversed after normalizing for body weight, suggesting that the apparent absolute advantage of obesity may not be in proportion to the excess of weight, possibly leading to relative bone fragility. In support of this hypothesis, data from the Global Longitudinal Study of Osteoporosis in Women (GLOW), which involved >60,000 postmenopausal women in 10 countries, indicated that obesity was associated with increased risk of ankle and upper leg fractures (18). In a medical-record-based study of over 800,000 postmenopausal women, the association between obesity and fracture was site-specific, being lower in the hip/pelvic area but 30% higher in the proximal humerus (19). Although it can be speculated that adipose tissue may protect the hip region during a fall, the source of higher arm fractures in obesity is not clear. It is possible that the adverse effects of obesity on BMD or bone architecture are more apparent in the arm, which does not benefit from the mechanical (loading) stimuli associated with increased body weight. Alternatively, the additional body weight in obesity may increase the force of a fall beyond that which can be accommodated by the arm. The ratio of VAT to subcutaneous fat was adversely associated with measures of bone density and architecture after accounting for confounding factors (15). Thus, whether the greater BMD in obesity confers any advantage or disadvantage to bone health in this group is not clear; further research is needed to examine aspects of bone quality in obesity, and to determine whether body fat distribution or metabolic health clarifies associations among obesity, bone health, and fracture risk.
Men
Gender differences may exist between the association of fat mass with bone quantity and/or quality. In a study that included both sexes and carefully adjusted for the confounding effect of body size, fat mass was significantly associated with BMD in women, but only weakly associated in men (20). However, the association of body composition with bone density in men may depend on age and energy balance (gaining vs losing weight). Among older men aged 70-97 y who were gaining weight, the increase in lean mass (but not fat mass) predicted increase in BMD, whereas among those who were losing weight, loss of fat (but not lean mass) predicted decrease in BMD, suggesting a protective effect of fat (21). Similarly in men aged >50 y, the ratio of VAT to subcutaneous fat was positively and independently associated with femoral neck BMD (15). However, in younger men, this ratio was inversely associated with both areal and volumetric BMD of the femoral neck, suggesting that age modifies the association between visceral fat and bone.
Although low (but not high) BMI was associated with elevated fracture risk (22), obesity may be associated with increased risk for some fractures. A large population study found that overweight/obese men were at higher risk for multiple rib fractures, although their risk for spine, hip, pelvis, and wrist/forearm fractures was lower (23). Data from MrOS indicated that, after adjusting for BMD, greater obesity was associated with greater risk for hip and non-spine fracture, which was explained in part by lower physical function (24). In men, poor bone microarchitecture was associated with greater VAT, and also with concentrations of a number of hormones (growth hormone, IGF-1, testosterone, estradiol), several of which are negatively impacted by obesity (25).
Type 2 diabetes
Fracture risk is increased in T2DM, often despite concomitant obesity and high BMD (26). The reason for the increased fracture risk is not entirely clear, but may be explained in part by greater falls resulting from hypoglycemic episodes, peripheral neuropathy, or retinopathy. It is also possible that, despite greater BMD, bone quality is compromised. Such qualitative aspects include the macrogeometry of cortical bone, the microarchitecture of trabecular bone, bone mineralization, and turnover (27). To illustrate this point, T2DM was associated with higher BMD at all sites, but lower lumbar spine trabecular bone score (TBS) from DXA (27). TBS reflects the density of the trabecular network, and is correlated with fracture risk. Low TBS predicted fracture independent of BMD in individuals with and without T2DM. A portion of the excess fracture risk in T2DM was statistically accounted for by TBS, but not BMD. Although the mechanism through which T2DM results in altered bone formation is not known, it may be related to cross-linking of advanced glycation endproducts (AGEs), which increases the brittle quality of bone, or to increased cortical porosity. Among non-diabetic individuals, AGEs were higher in those with a history of fracture (26), suggesting that a continuum exists in metabolic dysfunction as it pertains to bone structure. Similarly, biochemical markers of bone formation/turnover are reduced in both T2DM and obesity. Taken together, these observations suggest that indices of metabolic health must be separated from obesity to make appropriate conclusions regarding the possible impact of fat mass on bone.
Elderly
Although low body weight has long been recognized as a risk factor for fracture in the elderly, attention has only recently turned to whether overweight or obesity affects fracture risk in this age group. A meta-analysis that evaluated BMI as a risk factor for fracture in the elderly demonstrated a 17% reduction in risk at a BMI of 30 kg/m2 (obese) relative to the reference BMI of 25 kg/m2, particularly for hip fracture (22). Similarly, lower abdominal fat was associated with a higher risk for fragility fracture in women aged 57-97 yr, independent of age, lean mass, and BMD (28). These observations agree with data in older men (discussed above) indicating that fat and specifically VAT were positively associated with BMD (21)(15). Taken together, these results suggest that obesity, specifically abdominal obesity, has a protective effect on BMD and fracture in the elderly. The mechanism for these effects and the reason for their occurrence only in elderly are not known. Although in other age groups obesity is associated with greater adverse post-fracture outcomes, there is little information concerning adverse consequences of fracture in the obese elderly (e.g., functional limitation or loss of independence), and this gap in knowledge warrants examination.
Sarcopenic obesity
In addition to adversely impacting fracture risk through affects on bone, obesity may indirectly affect fracture risk through effects on muscle. The term “sarcopenic obesity” was coined to reflect the inverse association observed between accumulation of body fat and the decline in muscle mass and/or function in some individuals (29). Although the mechanism for this effect is not clear, pro-inflammatory factors emanating from adipose tissue may adversely affect muscle development or maintenance. This may occur on a local level, as adipose tissue is observed to infiltrate skeletal muscle, particularly in older adults. Alternatively, oxidative stress from chronic energy imbalance or poor diet may promote the terminal differentiation of satellite cells towards adipose at the expense of muscle. The end result is a situation where muscle function becomes impaired, leading to increased risk for fall and fracture.
Weight loss for bones?
Given the dichotomous association between obesity and bone health, the question emerges as to whether weight loss is beneficial or harmful for bone density and quality. Based on the existing literature, in an absolute sense, weight loss by diet or surgical means is generally associated with increases in markers of bone turnover, and decreases in bone content and density (30, 31). Whether loss of bone due to negative energy balance is “bad” with respect to bone health is less clear. When BMD data were normalized to the new, reduced body weight, weight-specific BMD was actually higher following weight loss, at least in premenopausal women (32). Further, in older adults, decreased BMD associated with intentional weight loss was not associated with adverse changes in bone microarchitecture (33). Weight re-gain is associated with re-gain of bone in pre-(30, 32), but not postmenopausal (34) women, suggesting that the endocrine milieu associated with older age does not support bone growth in the context of positive energy imbalance (weight gain). This could explain the phenomenon of increased fracture risk in obese older adults; ie., it is possible that bone is not able to increase appropriately with weight gain in older adults, and may suggest that intentional weight loss (which is rarely successfully maintained) may be dangerous for long-term bone health in older adults. Studies examining whether a specific metabolic condition (e.g. visceral obesity, diabetes, metabolic syndrome) interacts with intentional weight loss on measures of bone health have not been done, and are needed. Importantly, studies examining bone quality with weight loss in multiple populations are needed to clarify whether the decrease in BMD with intentional weight loss is detrimental to bone strength.
Recommendations for clinical care
Clinicians should be aware that obesity has divergent effects on bone health. While greater body weight associated with obesity may increase bone density, poor metabolic health associated with obesity may impair bone strength and/or density at certain sites, with variation occurring across age and gender groups. It is important to consider metabolic health in obese patients. If their waist circumference exceeds published cut-points for poor metabolic health, or if they have T2DM, impaired fasting glucose, or impaired glucose tolerance, obese patients may be at risk for osteoporosis and/or fracture. At present, current guideline for estimating fracture risk (e.g., FRAX) do not consider metabolic health. Research is needed to develop guidelines for incorporating metabolic health markers into prediction algorithms such as FRAX. Until this information is available, we recommend using waist circumference, fasting plasma glucose concentration, or 2-hour plasma glucose concentration obtained from a glucose tolerance test to determine if overweight/obese patients should be evaluated for bone density and counseled regarding fracture risk (see Fig. 1 for specific criteria).
Fig. 1.

Main points
Summary and need for future research
Although obesity is associated with greater bone content and density, it is not clear that the magnitude of the increase fully compensates for the increased adipose tissue burden, and if the greater BMD/BMC necessarily protects against fracture. Unfavorable effects of obesity on bone quality may adversely affect bone strength. Gender and age differences were apparent in the association between fat mass and bone health, with some suggestion that fat could be protective in older men. However, adverse effects of obesity on bone quantity and quality that occur early in life may limit peak bone accrual and thereby have lasting effects that persist into older age. Whether weight loss is beneficial for bone health is not clear, particularly in older adults where loss of bone may be irreversible. VAT, an accepted hallmark of poor metabolic health, is associated adversely with BMD, suggesting that insulin resistance, inflammation, or other factors associated with poor metabolic health have adverse effects on bone metabolism. This hypothesis is supported by the increased fracture risk in T2DM, often despite concomitant obesity and high BMD (26). However, the cause-and-effect nature of these relationships is not clear, and it is equally likely that lifestyle factors or poor metabolic health may stimulate differentiation of stem cells towards fat at the expense of bone, leading to both accumulation of VAT and poor bone structure and function. In addition, whether visceral adiposity is associated with greater risk for fracture has not been examined. Carefully designed interventions are needed to clarify the nature of associations between specific adipose tissue depots and bone density, quality, and fracture risk (Fig. 2).
Fig. 2.
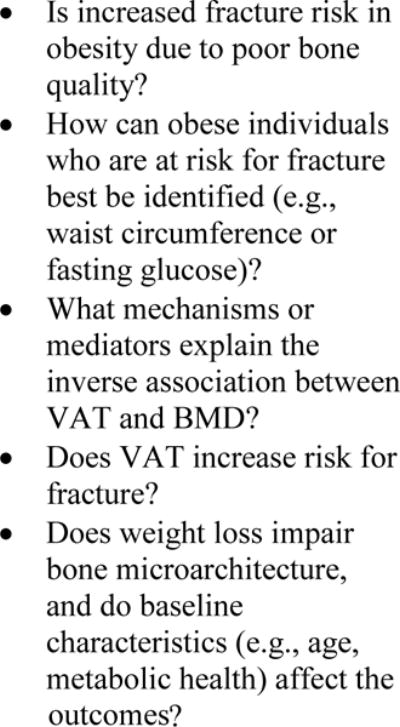
Research is needed to address the following questions:
Contributor Information
Barbara A Gower, Professor, Department of Nutrition Sciences, School of Health Professions, The University of Alabama at Birmingham, Birmingham, AL
Krista Casazza, Assistant Professor, Department of Nutrition Sciences, School of Health Professions, The University of Alabama at Birmingham, Birmingham, AL
References
- 1.Reid IR. Fat and bone. Arch Biochem Biophys. 2010;503:20–27. doi: 10.1016/j.abb.2010.06.027. [DOI] [PubMed] [Google Scholar]
- 2.Nielson CM, Srikanth P, Orwoll ES. Obesity and fracture in men and women: an epidemiologic perspective. J Bone Miner Res. 2012;27:1–10. doi: 10.1002/jbmr.1486. [DOI] [PubMed] [Google Scholar]
- 3.Cooper C, Westlake S, Harvey N, Javaid K, Dennison E, Hanson M. Review: developmental origins of osteoporotic fracture. Osteoporos Int. 2006;17:337–347. doi: 10.1007/s00198-005-2039-5. [DOI] [PubMed] [Google Scholar]
- 4.Streeter AJ, Hosking J, Metcalf BS, Jeffery AN, Voss LD, Wilkin TJ. Body fat in children does not adversely influence bone development: a 7-year longitudinal study (EarlyBird 18) Pediatr Obes. 2013 doi: 10.1111/j.2047-6310.2012.00126.x. [DOI] [PubMed] [Google Scholar]
- 5.Kessler J, Koebnick C, Smith N, Adams A. Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res. 2013;471:1199–1207. doi: 10.1007/s11999-012-2621-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fornari ED, Suszter M, Roocroft J, Bastrom T, Edmonds EW, Schlechter J. Childhood obesity as a risk factor for lateral condyle fractures over supracondylar humerus fractures. Clin Orthop Relat Res. 2013;471:1193–1198. doi: 10.1007/s11999-012-2566-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sayers A, Tobias JH. Fat mass exerts a greater effect on cortical bone mass in girls than boys. J Clin Endocrinol Metab. 2010;95:699–706. doi: 10.1210/jc.2009-1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valerio G, Galle F, Mancusi C, Di Onofrio V, Guida P, Tramontano A, Ruotolo E, Liguori G. Prevalence of overweight in children with bone fractures: a case control study. BMC Pediatr. 2012;12:166. doi: 10.1186/1471-2431-12-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pollock NK, Bernard PJ, Wenger K, Misra S, Gower BA, Allison JD, Zhu H, Davis CL. Lower bone mass in prepubertal overweight children with prediabetes. J Bone Miner Res. 2010;25:2760–2769. doi: 10.1002/jbmr.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shen W, Chen J, Punyanitya M, Shapses S, Heshka S, Heymsfield SB. MRI-measured bone marrow adipose tissue is inversely related to DXA-measured bone mineral in Caucasian women. Osteoporos Int. 2007;18:641–647. doi: 10.1007/s00198-006-0285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bredella MA, Torriani M, Ghomi RH, Thomas BJ, Brick DJ, Gerweck AV, Harrington LM, Breggia A, Rosen CJ, Miller KK. Determinants of bone mineral density in obese premenopausal women. Bone. 2011;48:748–754. doi: 10.1016/j.bone.2010.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bredella MA, Torriani M, Ghomi RH, Thomas BJ, Brick DJ, Gerweck AV, Rosen CJ, Klibanski A, Miller KK. Vertebral bone marrow fat is positively associated with visceral fat and inversely associated with IGF-1 in obese women. Obesity (Silver Spring) 2011;19:49–53. doi: 10.1038/oby.2010.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen A, Dempster DW, Recker RR, Lappe JM, Zhou H, Zwahlen A, Muller R, Zhao B, Guo X, Lang T, Saeed I, Liu XS, Guo XE, Cremers S, Rosen CJ, Stein EM, Nickolas TL, McMahon DJ, Young P, Shane E. Abdominal fat is associated with lower bone formation and inferior bone quality in healthy premenopausal women: a transiliac bone biopsy study. J Clin Endocrinol Metab. 2013 doi: 10.1210/jc.2013-1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilsanz V, Chalfant J, Mo AO, Lee DC, Dorey FJ, Mittelman SD. Reciprocal relations of subcutaneous and visceral fat to bone structure and strength. J Clin Endocrinol Metab. 2009;94:3387–3393. doi: 10.1210/jc.2008-2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng AC, Melton LJ, 3rd, Atkinson EJ, Achenbach SJ, Holets MF, Peterson JM, Khosla S, Drake MT. Relationship of adiposity to bone volumetric density and microstructure in men and women across the adult lifespan. Bone. 2013 doi: 10.1016/j.bone.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Albala C, Yanez M, Devoto E, Sostin C, Zeballos L, Santos JL. Obesity as a protective factor for postmenopausal osteoporosis. Int J Obes Relat Metab Disord. 1996;20:1027–1032. [PubMed] [Google Scholar]
- 17.Sornay-Rendu E, Boutroy S, Vilayphiou N, Claustrat B, Chapurlat R. In obese postmenopausal women, bone microarchitecture and strength are not commensurate to greater body weight. The OFELY study. J Bone Miner Res. 2013 doi: 10.1002/jbmr.1880. [DOI] [PubMed] [Google Scholar]
- 18.Compston JE, Watts NB, Chapurlat R, Cooper C, Boonen S, Greenspan S, Pfeilschifter J, Silverman S, Diez-Perez A, Lindsay R, Saag KG, Netelenbos JC, Gehlbach S, Hooven FH, Flahive J, Adachi JD, Rossini M, Lacroix AZ, Roux C, Sambrook PN, Siris ES, Glow I. Obesity is not protective against fracture in postmenopausal women: GLOW. Am J Med. 2011;124:1043–1050. doi: 10.1016/j.amjmed.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prieto-Alhambra D, Premaor MO, Fina Aviles F, Hermosilla E, Martinez-Laguna D, Carbonell-Abella C, Nogues X, Compston JE, Diez-Perez A. The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. J Bone Miner Res. 2012;27:294–300. doi: 10.1002/jbmr.1466. [DOI] [PubMed] [Google Scholar]
- 20.Reid IR, Plank LD, Evans MC. Fat mass is an important determinant of whole body bone density in premenopausal women but not in men. J Clin Endocrinol Metab. 1992;75:779–782. doi: 10.1210/jcem.75.3.1517366. [DOI] [PubMed] [Google Scholar]
- 21.Bleicher K, Cumming RG, Naganathan V, Travison TG, Sambrook PN, Blyth FM, Handelsman DJ, Le Couteur DG, Waite LM, Creasey HM, Seibel MJ. The role of fat and lean mass in bone loss in older men: findings from the CHAMP study. Bone. 2011;49:1299–1305. doi: 10.1016/j.bone.2011.08.026. [DOI] [PubMed] [Google Scholar]
- 22.De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ, 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A. Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int. 2005;16:1330–1338. doi: 10.1007/s00198-005-1863-y. [DOI] [PubMed] [Google Scholar]
- 23.Premaor MO, Compston JE, Aviles FF, Pages-Castella A, Nogues X, Diez-Perez A, Prieto-Alhambra D. The association between fracture site and obesity in men: A population-based cohort study. J Bone Miner Res. 2013 doi: 10.1002/jbmr.1878. [DOI] [PubMed] [Google Scholar]
- 24.Nielson CM, Marshall LM, Adams AL, LeBlanc ES, Cawthon PM, Ensrud K, Stefanick ML, Barrett-Connor E, Orwoll ES, Osteoporotic Fractures in Men Study Research G BMI and fracture risk in older men: the osteoporotic fractures in men study (MrOS) J Bone Miner Res. 2011;26:496–502. doi: 10.1002/jbmr.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bredella MA, Lin E, Gerweck AV, Landa MG, Thomas BJ, Torriani M, Bouxsein ML, Miller KK. Determinants of bone microarchitecture and mechanical properties in obese men. J Clin Endocrinol Metab. 2012;97:4115–4122. doi: 10.1210/jc.2012-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leslie WD, Rubin MR, Schwartz AV, Kanis JA. Type 2 diabetes and bone. J Bone Miner Res. 2012;27:2231–2237. doi: 10.1002/jbmr.1759. [DOI] [PubMed] [Google Scholar]
- 27.Leslie WD, Aubry-Rozier B, Lamy O, Hans D, Manitoba Bone Density P TBS (trabecular bone score) and diabetes-related fracture risk. J Clin Endocrinol Metab. 2013;98:602–609. doi: 10.1210/jc.2012-3118. [DOI] [PubMed] [Google Scholar]
- 28.Yang S, Nguyen ND, Center JR, Eisman JA, Nguyen TV. Association between abdominal obesity and fracture risk: a prospective study. J Clin Endocrinol Metab. 2013;98:2478–2483. doi: 10.1210/jc.2012-2958. [DOI] [PubMed] [Google Scholar]
- 29.Stenholm S, Harris TB, Rantanen T, Visser M, Kritchevsky SB, Ferrucci L. Sarcopenic obesity: definition, cause and consequences. Current Opinion in Clinical Nutrition and Metabolic Care. 2008;11:693–700. doi: 10.1097/MCO.0b013e328312c37d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Compston JE, Laskey MA, Croucher PI, Coxon A, Kreitzman S. Effect of diet-induced weight loss on total body bone mass. Clin Sci (Lond) 1992;82:429–432. doi: 10.1042/cs0820429. [DOI] [PubMed] [Google Scholar]
- 31.Brzozowska MM, Sainsbury A, Eisman JA, Baldock PA, Center JR. Bariatric surgery, bone loss, obesity and possible mechanisms. Obes Rev. 2013;14:52–67. doi: 10.1111/j.1467-789X.2012.01050.x. [DOI] [PubMed] [Google Scholar]
- 32.Hamilton KC, Fisher G, Roy JL, Gower BA, Hunter GR. The effects of weight loss on relative bone mineral density in premenopausal women. Obesity (Silver Spring) 2013;21:441–448. doi: 10.1002/oby.20052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Villareal DT, Kotyk JJ, Armamento-Villareal RC, Kenguva V, Seaman P, Shahar A, Wald MJ, Kleerekoper M, Fontana L. Reduced bone mineral density is not associated with significantly reduced bone quality in men and women practicing long-term calorie restriction with adequate nutrition. Aging Cell. 2011;10:96–102. doi: 10.1111/j.1474-9726.2010.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Villalon KL, Gozansky WS, Van Pelt RE, Wolfe P, Jankowski CM, Schwartz RS, Kohrt WM. A losing battle: weight regain does not restore weight loss-induced bone loss in postmenopausal women. Obesity (Silver Spring) 2011;19:2345–2350. doi: 10.1038/oby.2011.263. [DOI] [PMC free article] [PubMed] [Google Scholar]


