Abstract
Objective
The very early engagement in bulimic behaviors, such as binge eating, may be influenced by factors that dispose individuals to impulsive action as well as by factors that dispose individuals to depressive symptomatology. Using a longitudinal design, we conducted the first test of the simultaneous operation of both risk factors as children transition from elementary to middle school.
Method
In a sample of 1,906 children, we assessed risk for impulsive action (negative urgency, which is the tendency to act rashly when distressed, and eating expectancies, which are learned anticipations that eating will alleviate negative mood) and risk for depression (negative affect and depressive symptomatology) and binge eating behavior at three time points using a longitudinal design: the end of fifth grade (last year of elementary school: T0), the beginning of sixth grade (first year of middle school: T1), and the end of sixth grade (T2).
Results
Both the impulsive action and depression pathways predicted very early engagement in binge eating: each accounted for variance beyond the other. Mediation tests found that T1 eating expectancies mediated the predictive influence of T0 negative urgency on T2 binge eating (z = 2.45, p < .01) and that T1 depressive symptoms mediated the influence of T0 negative affect on T2 binge eating (z = 2.04, p < .05).
Discussion
In children, elevated levels of both negative urgency and negative affect predict early binge eating. This finding has important clinical implications because there are different interventions for the two different risk processes.
Keywords: risk, development, personality, youth, binge eating
Introduction
Binge eating (consuming unambiguously large amounts of food in a discrete period of time while feeling a sense of loss of control),1 along with other eating disorder symptoms, are often present at the beginning of adolescence (e.g., Ref. 2). It is important to develop risk models for children this young because binge eating at the beginning of adolescence is highly predictive of adult bulimia nervosa (BN) and anorexia nervosa2,3 and is associated with a range of physical and mental health problems.1,2 Research suggests that there are two different risk pathways for binge eating: one characterized by a disposition toward impulsive action and another characterized by a disposition toward depression. The intent of the current research was to conduct the first tests of (a) whether both pathways are indeed present, and present in children at the earliest stages of binge eating behavior, and (b) whether each pathway predicted binge eating over and above the other. We next briefly review each risk pathway and then introduce our model test.
Impulsivity Risk Pathway
We used the trait of negative urgency, which is the tendency to act rashly or impulsively when distressed, to measure risk for impulsive action. This trait appears to play an important role in risk for binge eating4 and for other behaviors characterized by impulsive acts (e.g., Refs. 5 and 6). For individuals high in negative urgency, rash action when distressed appears to help manage negative mood through avoidance or distraction.7 When a wide range of impulsivity-related traits were considered in a meta-analysis, only negative urgency had a substantial relationship to binge eating.8 Changes in levels of negative urgency are associated with changes in BN symptoms,9 and negative urgency concurrently and prospectively predicts BN behaviors in elementary school-aged girls and boys.4,10,11
The Acquired Preparedness (AP) model of risk describes one transactional mechanism by which negative urgency results in binge eating.4,6,12 According to AP, children high in negative urgency are disposed to act, often in rash ways, to alleviate distress. When these children are exposed to learning experiences that involve eating when distressed, they are biased to form expectancies associating eating with distress relief. This expectancy, in turn, increases the likelihood of binge eating.13 Thus, negative urgency predicts future binge eating through endorsement of eating expectancies. This process has been shown cross-sectionally in the fifth graders10,11 and prospectively in early adolescents.4 Although this risk pathway involves relief from distress, it does not involve high levels of negative mood or depression. These children are not particularly distressed, and the AP model holds while controlling for depression levels.4 The distress simply reflects a dip in the adolescent’s routine affective fluctuations.
Depression Risk Pathway
A second pathway of risk has identified negative affect and depression as risk factors for early onset binge eating. Negative affect has consistently been associated with eating disorder symptoms.14 Major depressive disorders frequently co-occur with binge eating disorder or BN, and there is evidence that depression predicts eating disorder onset and loss of control eating in adolescent girls.2,15 Moreover, elevated depressive symptoms, but not anxiety or anger, predicts binge eating onset in longitudinal samples of high school girls16 and college girls.17 It thus appears that individuals who are high on negative affect are at risk to develop depressive symptomatology, which in turn increases the likelihood of binge eating. To date, however, no research has been conducted on depressive symptom-related risk pathways in children as young as fifth grade.
The Current Study
The current study has two primary aims. The first is to test the two risk processes simultaneously to determine whether each has incremental predictive power over the other. Past studies have only investigated each pathway in isolation; therefore, it is not known if the apparent presence of one pathway is really an artifact of the presence of the other. The current study is the first to test them conjointly.
The second goal is to conduct this test in youth who are making the important developmental transition from elementary school to middle school. Middle school children encounter larger, more impersonal school contexts, and they experience a new level of independence from their parents.18 Even if they have not experienced pubertal onset themselves, many middle schoolers have, which contributes to a setting in which the needs and drives associated with physically mature bodies are manifest. For these reasons, this transition has been described as a potential turning point in development,19 that is, a period characterized by significant behavioral and developmental change. Additionally, because early disordered eating is highly associated with later diagnosable eating disorders,3 the prediction of this behavior from characteristics of elementary school children helps to clarify the developmental risk process and could suggest appropriate ages for preventive interventions.
We used three different time points to test the two pathways during this transition: The end of elementary school in fifth grade (T0), 6 months later at the beginning of middle school in sixth grade (T1), and 12 months after baseline at the end of sixth grade (T2). To our knowledge, this study is the first to (a) test the depression pathway in such a young population sample and (b) test the two pathways simultaneously.a For the impulsivity pathway, we anticipate that T0 negative urgency will predict T2 binge eating, and this effect will be mediated by T1 expectancies that eating helps to manage negative affect. For the depression pathway, we anticipate that T0 negative affect will predict T2 binge eating, and this effect will be mediated by T1 depressive symptomatology. We anticipate that each effect will be present when controlling for the other.
Method
Participants and Procedure
Participants
The participants were 1,906 students (50.2% boys, 49.8% girls) from Midwestern urban, suburban, and rural settings. They were assessed at three different time points, each 6 months apart: (a) the end of their fifth grade year in elementary school (T0), (b) the beginning of their sixth grade year in middle school (T1), and (c) the end of their sixth grade year in middle school (T2). At the initiation of the study, the mean age of the participants was 10.86 years. The ethnic breakdown of the sample was as follows: European American (60.9%), African American (18.7%), Hispanic (8.2%), Asian (2.9%), Middle Eastern (0.4%), and other (8.8%).
Data Collection
The university’s Institutional Review Board and participating school systems approved the following procedure, which was used for all three time points of the study. The questionnaires were administered in school cafeterias or classrooms during school hours in 23 public elementary schools for the first time point and in 19 public middle schools for the second and third time points. A passive consent procedure was used: each family was sent a letter through the U.S. Mail to introduce the study and was asked to return an enclosed, stamped letter or call a phone number if they did not want their child to participate. Of 1,988 fifth grade students in the participating schools, 95.8% (1,906) of the students participated in the study. Nonparticipation was due to parents declining participation for their child, students declining assent, or language disabilities that precluded completing the questionnaires.
Students were assured that their responses on the questionnaires would be kept confidential and that no one outside of the research team would see them. Students were required to sign assent forms before receiving the questionnaire. Except for those who moved out of district (these participants were contacted, asked to complete the forms through a secure website or by regular mail and were paid $30 for doing so), there was no compensation for participation. Total questionnaire administration took 60 min or less.
Data Analytic Method
As we describe below, we used a model building approach to test the incremental significance of each hypothesized risk pathway. To test the models, we used structural equation modeling (SEM) with maximum likelihood parameter estimates and an adjusted χ2 statistic that is robust to non-normality (the multiple linear regression (MLR) method). To test mediation, we used the indirect test provided by Mplus,20 which computes the product of the two regression coefficients. We measured model fit using four common indices: the Comparative Fit Index (CFI), the Tucker Lewis Index (TLI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). Guidelines for these indices vary: CFI and TLI values of .90 or .95 are described as representing good fit.21 RMSEA values of .06 are considered to indicate a close fit, .08 a fair fit, and .10 a marginal fit,21 and SRMR values of approximately .09 tend to indicate good fit.21 Overall evaluation of model fit is made by considering the values of each of the four fit indices; models that fit well on most indices are generally considered well-fitting. We used p < .01 to determine statistical significance for the bivariate correlations. The SEM model involved tests of the net effects of each variable, over and above the effects of other variables. We therefore included pathways significant at p < .05. We also tested whether the two risk pathways varied by sex.
Measures
Pubertal Development Scale
This Likert-type rating scale consists of five different questions for girls and boys. The Pubertal Development Scale22 correlates highly with physician ratings and other forms of self-report.23 This scale allows for dichotomous classification: following prior research, we rated scores of 2.5 or higher as reflective of pubertal onset.
Eating Expectancy Inventory
The Eating Expectancy Inventory24 is a five-factor measure that assesses expectancies for reinforcement from eating. For the current study, we used the scale of the expectancy that eating helps one manage negative mood states. As with past samples, the scale was internally consistent (α = .93 at T0 and was higher in subsequent time points).
Center for Epidemiologic Studies-Depression
This is a 20-item scale measuring depression with scores ranging from 0 to 60. The items are answered on a scale of four frequency ratings [“Less than 1 day” to “Most or all (5–7) days”]. Because our purpose was to measure the degree of depressive symptomatology, rather than diagnose depression, we used total Center for Epidemiologic Studies-Depression scores and treated them as interval scale. This scale has proven reliable (α = .85 in T0; higher in subsequent time points) and valid in numerous studies; it is frequently used with children, adolescents, and adults.25
Positive Affect, Negative Affect Scale
The Positive Affect, Negative Affect Scale26 measures dimensions of positive and negative affectivity. The scales are internally consistent (alpha values range from .84 to .90), stable, and have impressive evidence for their validity. We used only the negative affect scale. Concerning reliability, α = .90 in T0 and was higher in subsequent time points.
UPPS-P Negative Urgency Scale
We used the child version of the Negative Urgency Scale,27 which has recently proved to be internally consistent, have good convergent validity across assessment method, good discriminant validity from other impulsivity-related measures, and predictive of criteria in theoretically consistent ways.28 In this sample, α = .85 at T0 and was higher in subsequent time points.
Eating Disorder Examination-Questionnaire
For this study, we adapted the Eating Disorder Examination-Questionnaire (EDE-Q)29 for use with a younger population by using age-appropriate wording, defining concepts that may be difficult to understand, and shortening the length of time referred to in the questions to the past 2 weeks, per past recommendations.30 This child version is the most widely used and has generally good reliability and validity, particularly in clinical samples.30–32 We measured binge eating with loss of control: children had to endorse two items, one that assessed episodes of binge eating and one that assessed loss of control during these episodes. Endorsement of both items led to a score of 1 on our measure of binge eating. Children who endorsed neither item were given a score of 0 on binge eating. As loss of control seems to be a central feature for youth, we excluded children who endorsed overeating (binge eating but no loss of control) in order to make sure we had a clear contrast between no binge eating and binge eating; however, our findings did not change when we included overeating. The number of excluded children were T0, n = 100; T1, n = 87; and T2, n = 84.
Results
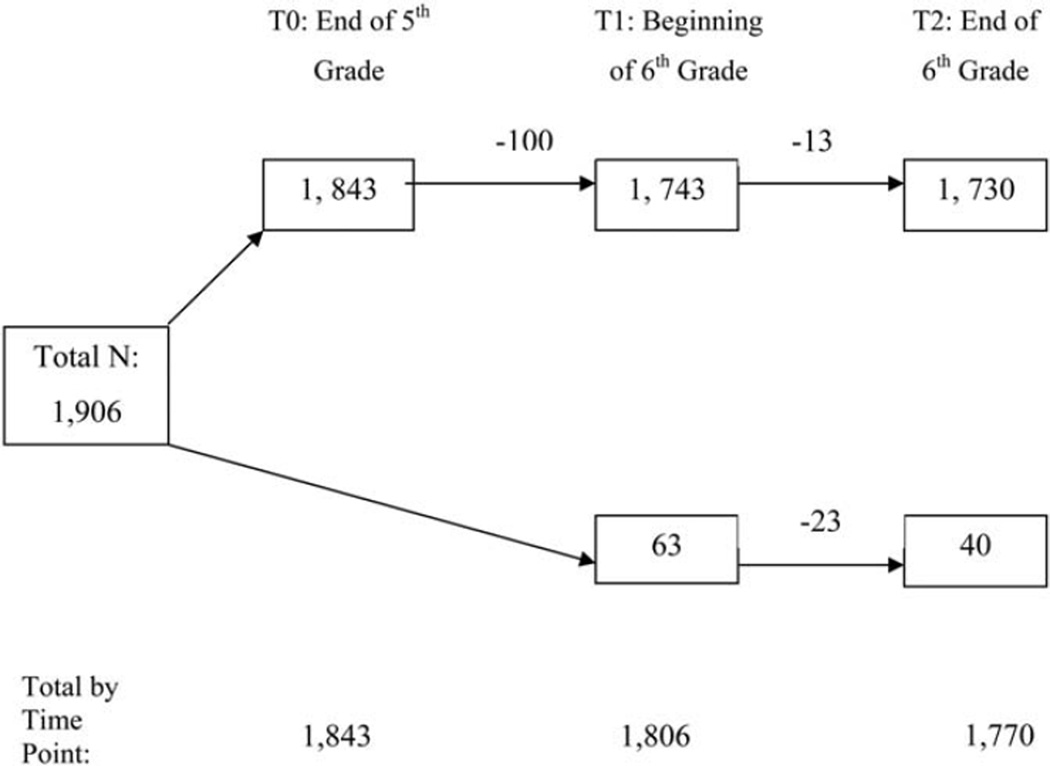
Attrition and Treatment of Missing Data
The participation rates at each time point are depicted in Figure 1. Of the 1,906 participants, 96.7% participated in T0, 94.8% participated in T1, and 92.9% participated in T2. A total of 1,730 (90.8%) participated at all three time points. Individuals who participated at all three time points of the study did not differ from those who participated in only one or two time points on any variable. We therefore assumed that data were missing at random, and we used the expectation maximization (EM) procedure to impute values for the missing data points. This procedure has been shown to produce relatively unbiased population parameter estimates and to be superior to traditional methods.33 As a result, we were able to make full use of the sample of n = 1,906.
FIGURE 1.
A flow chart representation of participant retention at each time point. Of the 1,906 participants, 63 were not tested for the first time until time point 1 because of absences from school on each time point 0 testing occasion.
Possible Effects due to School Membership
To determine whether there was significant covariance among the study variables due to participants attending the same school, we calculated intraclass coefficients for each variable (using elementary school membership, n = 23, as the nesting variable). Intraclass coefficients ranged from .03 to .00; therefore, we concluded that school membership was essentially unrelated to study variables.
Descriptive Statistics
The sample of 1,906 comprises 949 girls and 957 boys. By the end of fifth grade (T0), 24.8% of participants (27.7% of the girls and 21.8% of the boys) had experienced pubertal onset. The means and standard deviations for negative urgency, negative affect, depression, and the expectancy that eating helps to alleviate distress at each time point for both boys and girls are given in Table 1. In the current sample, as in prior research,2 there was a change in self-reported binge eating over time, with an overall decline: 10.0% of participants reported binge eating at T0, 6.4% did at T1, and 5.7% did at T2. The change from T0 to T1 was significant (χ2 = 134.65, p < .001), as was the change from T1 to T2 (χ2 = 313.86, p < .001). Specifically, 116 children reported binge eating at T0 but not at T1, whereas 60 children reported the opposite pattern of no binge eating at T0 but the presence of the behavior at T1. Similarly, 56 children reported binge eating at T1 but not at T2, and 48 children reported no binge eating at T1 but the presence of the behavior at T2.
TABLE 1.
Descriptive statistics of negative urgency, negative affect, depression, and eating expectancies by gender
| Sex | Factor and Wave | Mean | Standard Deviation |
|---|---|---|---|
| Girls | Negative Urgency-0 | 2.21 | 0.71 |
| Negative Urgency-1 | 2.10 | 0.71 | |
| Negative Urgency-2 | 2.20 | 0.74 | |
| Boys | Negative Urgency-0 | 2.20 | 0.70 |
| Negative Urgency-1 | 2.12 | 0.65 | |
| Negative Urgency-2 | 2.10 | 0.66 | |
| Girls | Negative Affect-0 | 2.19 | 0.78 |
| Negative Affect-1 | 1.87 | 0.77 | |
| Negative Affect-2 | 1.83 | 0.76 | |
| Boys | Negative Affect-0 | 2.01 | 0.72 |
| Negative Affect-1 | 1.76 | 0.68 | |
| Negative Affect-2 | 1.66 | 0.63 | |
| Girls | Depression-0 | 10.34 | 9.00 |
| Depression-1 | 8.15 | 7.99 | |
| Depression-2 | 8.04 | 7.81 | |
| Boys | Depression-0 | 9.44 | 8.17 |
| Depression-1 | 6.90 | 6.74 | |
| Depression-2 | 6.55 | 7.00 | |
| Girls | Eating Expectancy-0 | 2.21 | 1.31 |
| Eating Expectancy-1 | 1.90 | 1.23 | |
| Eating Expectancy-2 | 1.90 | 1.26 | |
| Boys | Eating Expectancy-0 | 2.32 | 1.43 |
| Eating Expectancy-1 | 1.92 | 1.28 | |
| Eating Expectancy-2 | 1.80 | 1.18 |
Note: Each number following the variable represents the time point in which the data were collected (e.g., Negative Urgency-0 refers to negative urgency as reported at baseline). N = 1,906.
Correlations among Study Variables across all Three Time Points
The correlations among study variables are given in Table 2. As shown in Table 2, puberty was associated with all three time points of negative urgency and depression, T2 eating expectancies, T2 negative affect, and T0 and T1 binge eating. All other key study variables were significantly intercorrelated, both within and across time points.
TABLE 2.
Correlations among all study variables
| PUB | NU-0 | NU-1 | NU-2 | DEP-0 | DEP-1 | DEP-2 | EE-0 | EE-1 | EE-2 | NA-0 | NA-1 | NA-2 | BE-0 | BE-1 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PUB | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| NU-0 | .13** | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| NU-1 | .13** | .57** | – | – | – | – | – | – | – | – | – | – | – | – | – |
| NU-2 | .13** | .53** | .66** | – | – | – | – | – | – | – | – | – | – | – | – |
| DEP-0 | .14** | .40** | .30** | .31** | – | – | – | – | – | – | – | – | – | – | – |
| DEP-1 | .13** | .29** | .39** | .34** | .53** | – | – | – | – | – | – | – | – | – | – |
| DEP-2 | .12** | .27** | .36** | .44** | .41** | .65** | – | – | – | – | – | – | – | – | – |
| EE-0 | .03 | .22** | .20** | .19** | .24** | .22** | .11** | – | – | – | – | – | – | – | – |
| EE-1 | .04 | .20** | .29** | .20** | .19** | .28** | .25** | .51** | – | – | – | – | – | – | – |
| EE-2 | .08** | .21** | .27** | .29** | .22** | .29** | .30** | .41** | .58** | – | – | – | – | – | – |
| NA-0 | .03 | .39** | .29** | .25** | .50** | .34** | .26** | .25** | .23** | .19** | – | – | – | – | – |
| NA-1 | .04 | .23** | .32** | .24** | .35** | .58** | .37** | .22** | .34** | .25** | .47** | – | – | – | – |
| NA-2 | .07** | .20** | .28** | .35** | .36** | .45** | .57** | .15** | .23** | .28** | .38** | .55** | – | – | – |
| BE-0 | .06** | .12** | .19** | .18** | .26** | .20** | .13** | .27** | .22** | .21** | .17** | .13** | .13** | – | – |
| BE-1 | .07** | .12** | .16** | .14** | .19** | .25** | .18** | .24** | .36** | .30** | .15** | .17** | .13** | .28** | – |
| BE-2 | .06** | .12** | .15** | .16** | .21** | .21** | .31** | .17** | .25** | .35** | .12** | .14** | .20** | .22** | .42** |
Note: PUB, Puberty; NU, Negative Urgency; DEP, Depression; EE, Eating Expectancies; NA, Negative Affect; BE, Binge Eating; each number following the variable represents the time point in which the data were collected (i.e., NU-1 = Negative Urgency, T1);
p < .01,
p < .001, N = 1,906.
Model Tests
To test whether both pathways operated at the same time, one must show that a model that included both pathways improved fit with the data when compared with a model that included each pathway alone or neither pathway. Thus, we first tested a baseline model, which did not specify either pathway. The fit of the baseline model was good: χ2 (75) = 416.90, CFI = .94, TLI = .90, RMSEA = .05 (90% confidence interval: .05 to .06), SRMR = .08. It was then used for comparison purposes. Second, we tested a model that specified the impulsivity pathway to see if the model fit for the data was improved from the baseline model by including this pathway. This model fit well: χ2 (73) = 380.03, CFI = .95, TLI = .91, RMSEA = .05 (90% confidence interval: .04 to .06), SRMR = .07. It fit significantly better than the baseline model (the adjusted χ2 statistic for model comparison: Δχ2 (2) = 30.74, p < .001). Thus, a model that included the impulsivity pathway is a better fitting model than one that does not specify this pathway; the impulsivity pathway for binge eating appeared to be present. Third, we did the same thing, separately, for the depression pathway. This model fit well: χ2 (74) = 400.54, CFI = .94, TLI = .91, RMSEA = .05 (90% confidence interval: .05 to .06), SRMR = .07. It fit significantly better than the baseline model (the adjusted χ2 statistic for model comparison: Δχ2 (1) = 32.72, p < .001). Thus, a model that included the depression pathway fits the data well; this pathway appeared to be present.
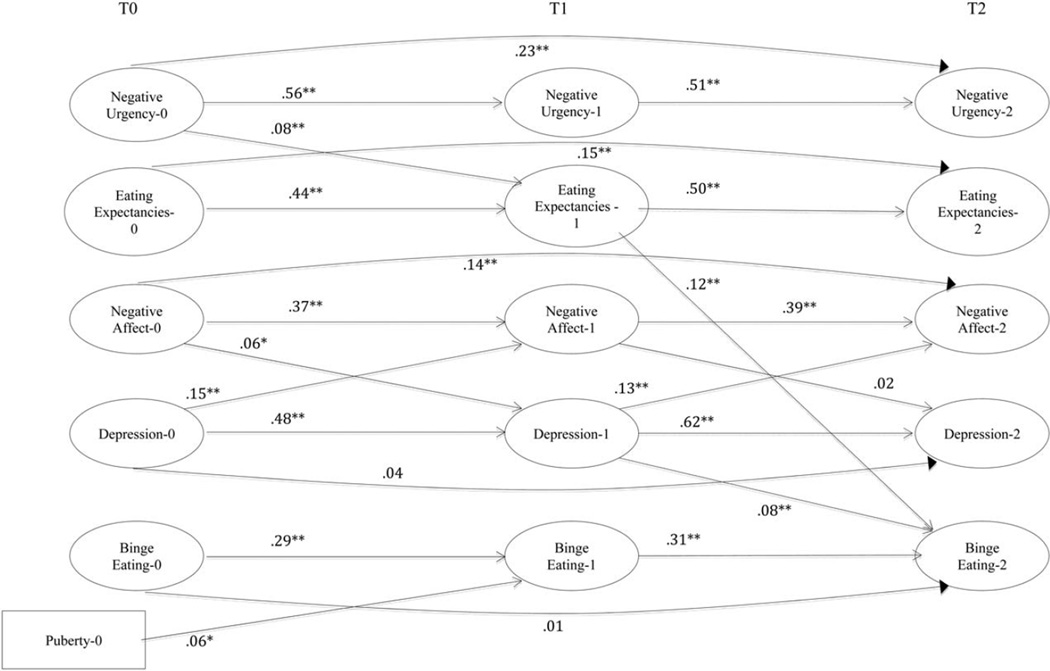
Lastly, because the model fit improved from the baseline model for each of the two pathways, we tested a model that included both the impulsivity and depression pathways. In other words, we tested whether specifying both the impulsivity and depression pathways better captured the experience of our participants than just one pathway alone or neither pathway. This model fit well: χ2 (72) = 371.25, CFI = .95, TLI = .91, RMSEA = .05 (90% confidence interval: .04 to .05), SRMR = .06. It fit significantly better than the other models: the baseline plus impulsivity model (Δχ2 (2) = 10.54, p < .001) and the baseline plus depression model (Δχ2 (1) = 39.15, p < .01). Perhaps most importantly, each predictive relationship for both the impulsivity and depression risk pathways remained significant, and statistical tests of mediation were consistent with both mediation processes operating at the same time: for the negative urgency to eating expectancy to binge eating pathway, z = 2.45, p < .01, b = .01; and for the negative affect to depression to binge eating pathway, z = 2.04, p < .05, b = .01. These findings indicate that recognizing both pathways of risk most accurately reflected the experience of our participants. This model is depicted in Figure 2.
FIGURE 2.
A structural model of all study variables of significant pathways. Each number following the variable represents the time point in which the data were collected (i.e., Negative Urgency-1 = Negative Urgency, T1); *p < .01, **p < .001, N = 1,906. Cross-sectional associations are omitted for clarity of presentation.
We then tested whether this final model varied across the sex of the child. There was no drop in fit from the final model when a two-group model by sex was specified, even when the predictive pathways for both the impulsivity and depression models were held equal across the sexes. Thus, the final risk model was invariant across sex.
Discussion
Validated risk models can help researchers and clinicians to understand the etiology of disordered eating in youth and can also suggest effective avenues for intervention. The current study tested whether two risk pathways, one impulsive and one depressive, led to binge eating in youth transitioning into middle school. We found that a risk model that included both pathways, as opposed to just one pathway or neither pathway, better captured the experience of the youth in our sample. Clinicians should address both impulsivity and depressive symptoms in adolescents with binge eating behavior.
The impulsivity pathway described a process in which elevated levels of negative urgency predicted elevated expectancies that eating helps to manage negative affect, which in turn predicted binge eating behavior. This process, known as the AP model of risk, has also been identified for other problem behaviors.5,6 In each case, elevations in negative urgency increase risk, together with disorder-specific expectancies (e.g., smoking provides the negative reinforcement of distress relief). Thus, there appears to be a general process in which a high-risk personality trait can bias learning to lead to the formation of high-risk expectancies, resulting in a problematic, pathological behavior. Some youth disposed to act in rash, impulsive ways when distressed have learned that eating alleviates negative mood and are thus at increased risk for binge eating.
The depression pathway is characterized by negative affect leading to depressive symptomatology, which in turn predicts binge eating behavior. Research on emotional eating has highlighted the role of negative affect in loss of control eating,2 and numerous researchers have identified depressive symptomatology as a risk factor for binge eating behavior in youth.15–17 The current study is the first to document a sequential risk process in which negative affect predicted subsequent depressive symptoms, which in turn predicted binge eating behavior. This is also the first study to examine such a process in youth as young as in fifth and sixth grades.
In this younger population sample, we found no sex differences in the risk model. Given the similar rates of binge eating across adult women and men, this finding may not be particularly surprising. Of course, it is also quite possible that sex differences will emerge over the course of development. In particular, puberty (a) appears to influence the heritability of disordered eating in girls but not boys34 and (b) appears to increase risk in depression among girls.35 Further investigation of the risk process by sex is clearly warranted.
These findings have important clinical implications. Different risk processes in youth are likely to require different preventive and treatment interventions. For example, youth who are high in negative urgency may respond well to a focus on reducing impulsive actions when distressed. Learning skills like those in dialectical behavior therapy36 may prove fruitful for these youth to reduce risk and/or treat binge eating behavior. Youth high in the expectancy that eating helps to alleviate negative affect may benefit from cognitive behavioral therapy to challenge that expectation (success for an intervention challenging expectancies for thinness has been shown; Ref. 37). For those youth who are better characterized by the negative affect and depression pathway, interventions designed to alleviate negative affect, such as behavior therapy, cognitive behavior therapy, and pharmacotherapy (for a review, see Ref. 38), may be indicated.
The findings from this study suggest several future avenues of research. First, it seems likely that the risk process for disordered eating is quite complex. Thus, perhaps there are more complex transactional processes, such as between depression, negative urgency, and eating expectancies, that could further clarify who is at the greatest risk to binge eat. Second, because different children reported different directions of change in their binge eating behavior over time, person-centered analytic approaches may prove informative with more time points of data.
We have used the term “risk factor” to describe the variables in the two risk pathways that we studied, following the classic terminology as described by Jacobi et al.,39 because negative urgency, negative affect, and the other variables precede and have statistical and clinical associations with binge eating. We do consider it quite possible that the two risk pathways we have described exert a causal influence on binge eating. However, we neither tested nor showed the operation of causal processes. The results of this study are consistent with, but of course not proof of, the causal processes implied in our model. It is also very likely that these processes work in conjunction with other factors not tested in this study to increase risk.
The results of this study should be understood in the context of the study’s limitations. First, we did not test any specific process or mechanism of influence. Second, despite our low attrition rates and use of the EM method for addressing missing data, there is a chance that the results could have differed with even higher retention. Third, we relied on questionnaires to assess each attribute and behavior in our sample. The EDE-Q has good reliability and validity data for clinical samples30; however, there is minimal data on its validity in community based, preadolescent samples. Fourth, we did not assess the context of the eating disorder behavior; as a result, we know very little about the nature of these early binge eating experiences.
In summary, eating disorder behavior begins at a very young age and is of obvious clinical concern. The current study found that two separate risk processes operate simultaneously in youth: one that is impulsivity-based and one that is depression based. This finding suggests that clinicians should select different, appropriate interventions for youth based on which risk process better characterizes the youth.
Acknowledgments
Supported by:R01 AA 016166 from National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Footnotes
The current study used the sample reported on in Pearson et al.4 With respect to the impulsivity pathway, we are presenting a pathway very similar to the one described in that prior study: T0 negative urgency’s predictive influence on T2 binge eating was mediated by T1 expectancies that eating helps manage negative affect. The analyses described in the current paper differ from those prior analyses in three important ways. First, the current study is the first to test whether the impulsivity pathway is present when controlling for the depression pathway, and whether the depression pathway is present when controlling for the impulsivity pathway. It is also the first to test the incremental value of each pathway in youth at the earliest stages of binge eating behavior. Second, in the current study we have defined binge eating as including loss of control, whereas in Pearson et al.4 we included binge eating without loss of control. Third, in this study we define binge eating dichotomously, so the key outcome variable reflects the presence or absence of loss of control binge eating.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders—Text Revised. 4th. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Tanofsky-Kraff M, Shomaker LB, Olsen C, Rozan CA, Wolkoff LE, Columbo KM, et al. A prospective study of pediatric loss of control eating and psychological outcomes. J Abnorm Psychol. 2011;120:108–118. doi: 10.1037/a0021406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kotler LA, Cohen P, Davies M, Pine DS, Walsh BT. Longitudinal relationships between childhood adolescent and adult eating disorders. J Am Acad Child Psychiatry. 2001;40:1434–1440. doi: 10.1097/00004583-200112000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Pearson CM, Combs JL, Zapolski TCB, Smith GT. A longitudinal transactional risk model for early eating disorder onset. J Abnorm Psychol. 2012;121:707–718. doi: 10.1037/a0027567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doran N, Khoddam R, Sanders PE, Schweizer CA, Trim RS, Myers MG. A prospective study of the acquired preparedness model: The effects of impulsivity and expectancies on smoking initiation in college students. Psychol Addict Behav. 2013;27:714–722. doi: 10.1037/a0028988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Settles RF, Cyders MA, Smith GT. Longitudinal validation of the acquired preparedness model of drinking risk. Psychol Addict Behav. 2010;24:198–208. doi: 10.1037/a0017631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cyders MA, Smith GT. Emotion-based dispositions to rash action: Positive and negative urgency. Psychol Bull. 2008;134:807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fischer S, Smith GT, Cyders MA. Another look at impulsivity: A meta-analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clin Psychol Rev. 2008;28:1413–1425. doi: 10.1016/j.cpr.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anestis MD, Selby EA, Joiner TE. The role of urgency in maladaptive behaviors. Behav Res Ther. 2007;45:3018–3029. doi: 10.1016/j.brat.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 10.Combs JL, Pearson CM, Smith GT. A risk model for pre-adolescent disordered eating. Int J Eat Disord. 2011;44:596–604. doi: 10.1002/eat.20851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pearson CM, Combs JL, Smith GT. A risk model for pre-adolescent disordered eating in boys. Psychol Addict Behav. 2010;24:696–704. doi: 10.1037/a0020358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Combs JL, Smith GT. Personality factors and acquired expectancies: Effects on and prediction for binge eating. In: Chambers N, editor. Binge Eating: Psychological Factors, Symptoms, and Treatment. New York: Nova Science Publishers; 2009. pp. 55–86. [Google Scholar]
- 13.Smith GT, Simmons JR, Flory K, Annus AM, Hill KK. Thinness and eating expectancies predict subsequent binge eating and purging behavior among adolescent girls. J Abnorm Psychol. 2007;116:188–197. doi: 10.1037/0021-843X.116.1.188. [DOI] [PubMed] [Google Scholar]
- 14.Stice E. Risk and maintenance factors for eating pathology: A meta-analytic review. Psychol Bull. 2002;128:825–848. doi: 10.1037/0033-2909.128.5.825. [DOI] [PubMed] [Google Scholar]
- 15.Stice E, Burton E, Shaw H. Prospective relations between bulimic pathology, depression, and substance abuse: Unpacking comorbidity in adolescent girls. J Consult Clin Psych. 2004;72:62–71. doi: 10.1037/0022-006X.72.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychol. 2002;21:131–138. [PubMed] [Google Scholar]
- 17.Spoor STP, Stice E, Bekker MHJ, Van Strien T, Croon MA, Van Heck GL. Relations between dietary restraint, depressive symptoms, and binge eating: A longitudinal study. Int J Eat Disord. 2006;39:700–707. doi: 10.1002/eat.20283. [DOI] [PubMed] [Google Scholar]
- 18.Barber BK, Olsen JA. Assessing the transition to middle and high school. J Adolesc Res. 2004;19:3–30. [Google Scholar]
- 19.Graber JA, Brooks-Gunn J. Reproductive transitions: The experience of mothers and daughters. In: Ryff CD, Seltzer MM, editors. The Parental Experience in Midlife. Chicago, IL: University of Chicago; 1996. pp. 255–299. [Google Scholar]
- 20.Muthén LK, Muthén BO. User’s Guide, Version 6. Los Angeles, CA: Muthén & Muthén; 2010. Mplus: Statistical Analysis with Latent Variables. [Google Scholar]
- 21.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equation Model. 1999;6:1–55. [Google Scholar]
- 22.Petersen AC, Crockett L, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. J Youth Adolesc. 1988;17:117. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- 23.Coleman L, Coleman J. The measurement of puberty: A review. J Adolesc. 2002;25:535–550. doi: 10.1006/jado.2002.0494. [DOI] [PubMed] [Google Scholar]
- 24.Hohlstein LA, Smith GT, Atlas JG. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychol Assess. 1998;10:49–58. [Google Scholar]
- 25.Clarke G, Debar L, Lynch F, Powell J, Gale J, O’Connor E, et al. A randomized effectiveness trial of brief cognitive-behavioral therapy for depressed adolescents receiving antidepressant medication. J Am Acad Child Adolesc Psychiatry. 2005;44:888–898. [PubMed] [Google Scholar]
- 26.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 27.Lynam D, Smith GT, Cyders MA, Fischer S, Whiteside SA. The UPPS-P: A multidimensional measure of risk for impulsive behavior. Technical Report. 2007
- 28.Zapolski TCB, Stairs AM, Settles RF, Combs GL, Smith GT. The measurement of dispositions to rash action in children. Assessment. 2010;17:116–125. doi: 10.1177/1073191109351372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? Int J Eat Disord. 1994;16:363–370. [PubMed] [Google Scholar]
- 30.Carter JC, Stewart DA, Fairburn CG. Eating disorder examination questionnaire: Norms for young adolescent girls. Behav Res Ther. 2001;39:625–632. doi: 10.1016/s0005-7967(00)00033-4. [DOI] [PubMed] [Google Scholar]
- 31.Luce KH, Crowther JH. The reliability of the eating disorder examination-self-report questionnaire version (EDE-Q) Int J Eat Disord. 1999;25:349–351. doi: 10.1002/(sici)1098-108x(199904)25:3<349::aid-eat15>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 32.Mond JM, Hay P, Rodgers B, Owen C, Beumont PJV. Temporal stability of the eating disorder examination questionnaire. Int J Eat Disord. 2004;36:195–203. doi: 10.1002/eat.20017. [DOI] [PubMed] [Google Scholar]
- 33.Enders CK. A primer on the use of modern missing-data methods in psychosomatic medicine research. Psychosom Med. 2006;68:427–436. doi: 10.1097/01.psy.0000221275.75056.d8. [DOI] [PubMed] [Google Scholar]
- 34.Klump KL, Culbert KM, Slane JD, Burt SA, Sisk CL, Nigg JT. The effects of puberty on genetic risk for disordered eating: Evidence for a sex difference. Psychol Med. 2011;22:1–11. doi: 10.1017/S0033291711001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates of major depression—A theoretical model. Arch Gen Psychiatry. 2000;57:21–27. doi: 10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- 36.Linehan MM. Cognitive Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press; 1993. [Google Scholar]
- 37.Annus AM, Smith GT, Masters K. Manipulation of thinness and restricting expectancies: Further evidence for a causal role of thinness and restricting expectancies in the etiology of eating disorders. Psychol Addict Behav. 2008;22:278–287. doi: 10.1037/0893-164X.22.2.278. [DOI] [PubMed] [Google Scholar]
- 38.Chambless DL, Ollendick TH. Empirically supported psychological interventions: Controversies and evidence. Annu Rev Psychol. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- 39.Jacobi C, Hayward C, de Zwann M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychol Bull. 2004;130:19–65. doi: 10.1037/0033-2909.130.1.19. [DOI] [PubMed] [Google Scholar]