Abstract
Objectives
The aims of this study were to assess psychiatrists' knowledge of and attitudes toward repetitive transcranial magnetic stimulation (rTMS) in Saudi Arabia and to determine the contributing factors.
Methods
A quantitative observational cross-sectional study was conducted using an online survey. The sample consisted of 96 psychiatrists in Saudi Arabia. A new valid and reliable questionnaire was developed.
Results
A total of 96 psychiatrists enrolled in the study, 81% of whom were men. Half of the participants were consultants. The sample mainly consisted of general psychiatrists (65%). The mean age of the participants was 37 years. The results showed that 80% of the psychiatrists had a sufficient level of knowledge about rTMS. Consultants had greater knowledge than residents. Training abroad was not significantly associated with the level of knowledge or the type of attitude. Most psychiatrists (79%) had a positive attitude toward rTMS. Only 53% of the psychiatrists said they would agree to receive rTMS if they experienced a psychotic depressive condition. A minority of psychiatrists (7%) said they would not refer their patients for rTMS.
Conclusions
Most of the psychiatrists surveyed had good knowledge of and a positive attitude toward rTMS. Those who had a high level of training and experience showed higher levels of knowledge. Articles were reported to be a better source for improving physician knowledge than textbooks. Having a family member or relative who was treated with rTMS positively affected psychiatrists' attitudes toward rTMS.
Key Words: repetitive transcranial magnetic stimulation, TMS, psychiatrists, knowledge, attitude, Saudi Arabia
Repetitive transcranial magnetic stimulation (rTMS) is a noninvasive treatment method. It works by generating a high magnetic current that enhances or suppresses cortical activity.1,2 There are multiple claimed therapeutic uses of rTMS for psychiatric disorders such as depression, bipolar disorder, hallucinations, schizophrenia, and migraine. However, rTMS has only been US Food and Drug Administration (FDA) approved for medication-refractory depression.3 Saudi FDA registers rTMS, and it is indicated for the treatment of major depressive disorder in adult patients who have failed to receive satisfactory improvement from antidepressant medications.4
Transcranial magnetic stimulation was introduced in 1984 to 1985 by Anthony Barker and colleagues.5 In 1991, Pascual-Leone et al6 published one of the first articles to reference rTMS.5 In 1995, Kolbinger et al studied the effects of rTMS on patients with drug-resistant depression. Patients who were receiving nonsham stimulation showed improvement.7 The first detailed rTMS safety and ethical guidelines were released in 1996.8
Electroconvulsive therapy (ECT) is a well-established older method to treat psychotic disorders. Being the most effective short-term therapy for major depression, it gained a huge popularity. Although it is effective, there are certain limitations such as anesthesia, risk of seizures, and relatively low tolerance rate among some patients. Comparing rTMS to ECT, rTMS considered being a safer, noninvasive therapy with inferior efficacy in treating major depression. However, rTMS has some adverse effects, such as transient headache, paresthesia, local pain, neck pain, toothache, and, rarely, seizures (occurring in less than 1% of nonepileptic patients and 1.4% of epileptic patients).9,10 Micallef-Trigona did systematic review and meta-analysis of 9 randomized clinical trials comparing ECT and rTMS in treating medication resistance depression. Both methods showed reduction in symptoms of depression measured by Hamilton Rating Scale for Depression. There was a mean reduction of 9.3 and 15.42 points in favor of ECT.11
After 60 years of opening the first psychiatric hospital in Saudi Arabia in the mid 1950s, the Saudi government passed a Mental Health Act in 2012. The main provider of mental health services is the Ministry of Health. There are around 94 public outpatient mental health facilities that serve over 1800 patients per 100,000 population per year, most of these patients are diagnosed with mood disorders, stress-related disorders, neurotic disorders, or somatoform disorders. Schizophrenia (50%), substance abuse (20%), and mood disorders (20%) are the most prevalent psychotic disorders among inpatients. However, psychotic disorders seen in outpatients and inpatients settings are similar in Saudi Arabia and United States.12,13
According to a 2011 World Health Organization report regarding the availability of mental health services in Saudi Arabia, the number of psychiatrists has increased. The rate of psychiatrists working in the mental health sector in Saudi Arabia is 2.91 per 100,000, whereas the average rate of psychiatrists working in the mental health sector worldwide is 1.27 per 100,000 population. Furthermore, there are several undergraduate and postgraduate psychiatry training programs in Saudi Arabia, including residency training programs in Riyadh, Jeddah, and Dammam. The availability of psychiatric beds in Saudi Arabian general hospitals is less than the global median rate, which is 1.4 per 100,000 population. However, the number of psychiatric hospitals in Saudi Arabia has increased nearly 10-fold over the past 30 years to 20 psychiatric hospitals (0.08 per 100,000 population). Globally, the median rate of psychiatric hospitals is 0.03 per 100,000 population. The number of beds in psychiatric hospitals in Saudi Arabia is 12 per 100,000 population, which is similar to the United States (13.3 beds per 100,000 population), and higher than in the Eastern Mediterranean region (4.8 beds per 100,000 population), whereas the median rate is 7.04 beds per 100,000 population worldwide. The expenditures from health care budget on mental health in Saudi Arabia are less than what it is in the United States (4% and 5.6%, respectively).12–15 Repetitive transcranial magnetic stimulation is registered in Saudi FDA, and it is indicated for the treatment of major depressive disorder in adult patients who have failed to receive satisfactory improvement from antidepressant medications.
One of the most important factors in correcting patient misconceptions about a treatment is their physician's treatment explanation; this, in turn, is directly affected by physician knowledge.16 Psychiatrists' knowledge of and positive attitude toward ECT have been shown to significantly correlate with ECT therapeutic referral.17 Multiple studies on ECT knowledge and attitude in both patients and psychiatrists have been conducted.18,19 However, there has been limited attention paid to knowledge and attitude toward rTMS because it is a new therapy; only 1 study has been conducted with rTMS recipients. In that study, most of the participants correctly answered the question, “What do you think TMS is? (A treatment in which a magnetic field is used),” and most reported that they would agree to be treated with rTMS if recommended in the future.20,21
Unfortunately, to the best of our knowledge, there have been no studies conducted among psychiatrists regarding their knowledge of and attitude toward rTMS. In this study, rTMS knowledge and attitudes were assessed among psychiatrists in Saudi Arabia.
METHODS
A quantitative observational cross-sectional study was conducted in King Khalid University Hospital. Psychiatrists in Saudi Arabia were the study population. Institutional review board approval was granted before data collection was begun.
Questionnaire
An anonymous, self-administered online survey was completed using the Google Documents platform. Our search failed to find a validated scale to measure rTMS knowledge and attitude among professionals. Therefore, we developed a new questionnaire for this study based on other studies that have measured knowledge of and attitude toward ECT.19,22
The questionnaire contained 3 sections: demographic information, knowledge, and attitudes. The demographic and general information section included age, sex, training abroad, subspecialty, conference attendance, and other related questions. The knowledge section contained 21 items that evaluated different aspects of rTMS knowledge. These items had 3 response options: yes, no, and I don't know. The correct response was marked as 1 point, and the incorrect and “I don't know” responses were marked as zero points because both represented a lack of knowledge. The attitude section contained 13 items, including both positive and negative attitude statements. These items used a 5-point Likert scale with options of strongly agree, agree, neutral, disagree, and strongly disagree. The responses were scored from 0 to 4 based on whether the attitude statement was positive or negative. As no previous studies existed regarding knowledge and attitude toward rTMS, we decided to consider those who answered more than 50% of the items correctly to have sufficient knowledge. Those who obtained more than half of the total possible score were considered to have a positive attitude toward rTMS.
After designing the questionnaire, 7 experts in psychiatry reviewed it for validity. We made some modifications based on their comments. A pilot study with 5 participants was conducted to assess the questionnaire's reliability through the test-retest method, and feedback was then obtained. The reliability of the knowledge and attitude sections of the questionnaire was tested using Cronbach α and yielded a score of 0.74.
Participants
We calculated a required sample size of 93 (Zα: 1.96 for 95% confidence level, proportion: 0.6, d: 0.1). The questionnaire was e-mailed to approximately 300 psychiatrists, and those who responded were included in the study (convenience sampling), resulting in a response rate of 33%. The e-mail list was obtained from several sources, primarily the Saudi Psychiatric Association, the Saudi Commission for Health Specialties, and personal communication. Junior residents are the first- and second-year residents in the psychiatry training program, whereas senior residents are the third- and fourth-year residents in the program. Specialists who got the psychiatry training certificate and did not finish the 3 years were required after the program to be a consultant. Data were collected over 1 week. Participants provided consent, and they were informed of the objectives and aims of the research.
Data Analysis
Data were analyzed using the Statistical Package for Social Sciences23 (Armonk, NY), version 21.0. Descriptive statistical data are presented by mean values, standard deviations, and percentages. Analysis of variance (ANOVA), post hoc analysis (Scheffé method), and t tests were used to compare subgroups. In addition, Pearson correlation was used to assess the relationship between different variables. Only statistically significant differences at P < 0.05 are reported.
RESULTS
Study Subjects
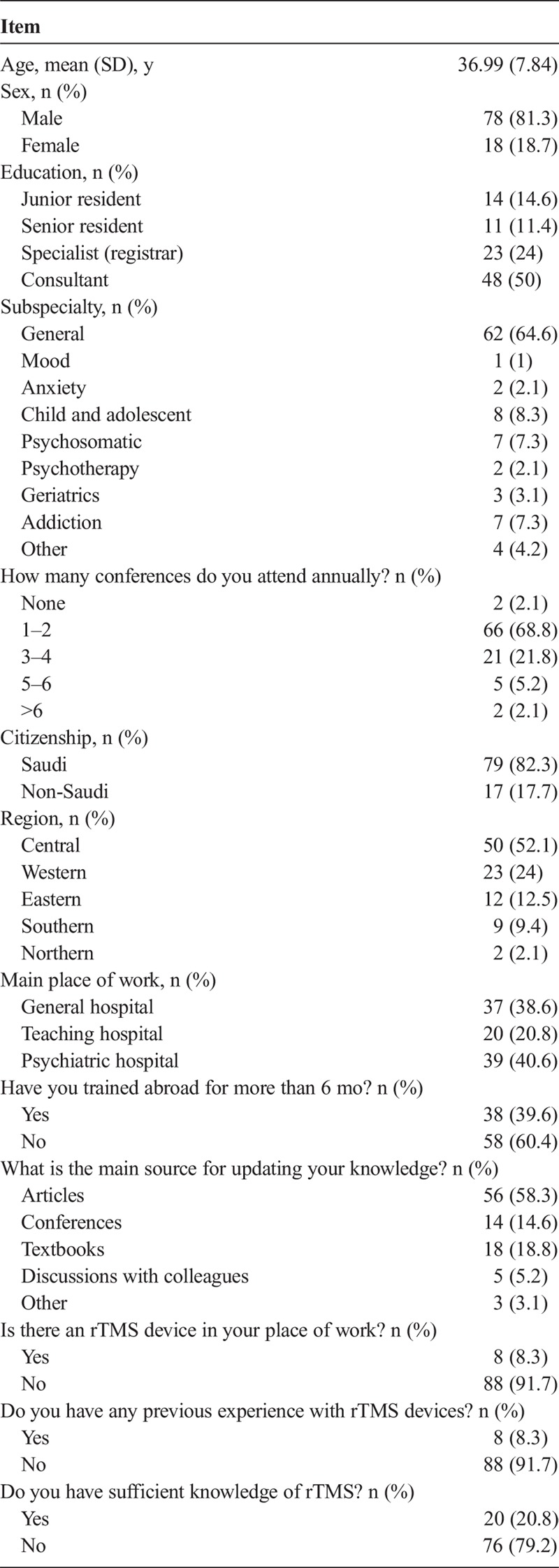
A total of 96 psychiatrists completed the questionnaire, 81% of whom were men. Consultants represented 50% (n = 48) of the participants, followed by specialists (registrars) (24%), junior residents (14.6%), and senior residents (11.5%). The sample consisted of a variety of subspecialties, primarily general psychiatrists (n = 62, 65%), child and adolescent psychiatrists (8%), psychosomatic psychiatrists (7%), and other subspecialties (20%). The Saudi–to–non-Saudi participant ratio was 5:1. The mean age of participants was 37 ± 7.84 years. The study covered all regions in Saudi Arabia, with a participation rate of 52% in the central region, 24% in the western, 13% in the eastern, 9% in the southern, and 2% in the northern region. Most psychiatrists, 79%, thought that they did not have sufficient knowledge of rTMS. Other results are shown in Table 1.
TABLE 1.
Demographic Factors
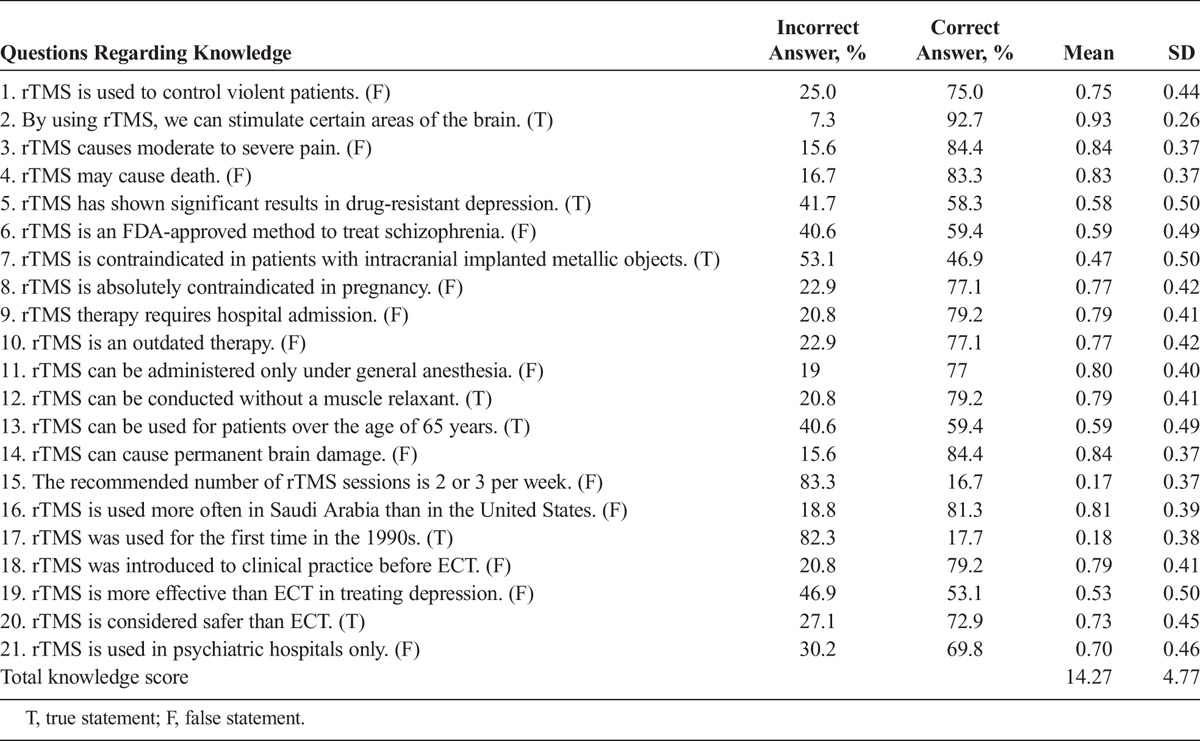
Knowledge
As seen in Table 2, 93% of the participants correctly answered the question “By using rTMS, we can stimulate certain areas of the brain.” More than two thirds did not know the correct number of rTMS therapy sessions. About half of the participants thought that rTMS is more effective than ECT for treating depression, and 59% correctly said that rTMS could be used in patients older than the age of 65 years.
TABLE 2.
Distribution of Answers Concerning Knowledge of rTMS
The survey showed that 80% of the participants answered more than half of the questions correctly, with a mean of 14.25 (out of a possible 21 points) and a standard deviation of 8.81. Approximately 73% answered 60% of the knowledge questions correctly, and 63% answered 70% correctly. Comparisons of participant knowledge based on educational level are illustrated in Figure 1 (ANOVA F3,92 = 8.839) and show that consultants had greater knowledge than both senior residents (P = 0.017) and junior residents (P < 0.001). There was no statistically significant difference in level of knowledge between consultants and specialists or between junior and senior residents. Specialists had a higher level of knowledge than junior residents (P = 0.035). In addition, the survey results indicated that older psychiatrists had more knowledge than younger psychiatrists (Pearson correlation r = 271, n = 96, P = 0.008). Physicians who used articles to keep their knowledge current had greater rTMS knowledge than those who used textbooks (ANOVA F4,91 = 3.681, P = 0.008). There was no association between the level of knowledge and either having trained abroad for more than 6 months (ANOVA F1,94 = 668, P = 0.416) or the number of conferences attended annually (ANOVA F4,91 = 0.16, P = 0.958).
FIGURE 1.
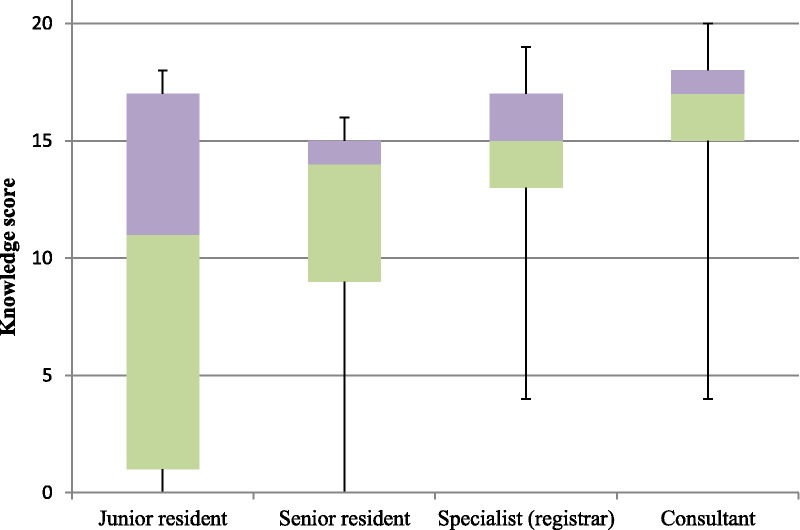
Box plots showing the knowledge scores of different subgroups.
Attitude
As seen in Table 3, 43% of the psychiatrists said that they would refer their patients for rTMS therapy, whereas only 7.3% said that they would not. More than half of the psychiatrists (53.1%) agreed with the statement, “I would consent to receive rTMS if I had a psychotic depressive condition,” whereas one fifth (21.8%) disagreed. Most participants (80.2%) thought that having knowledge of rTMS would improve the quality of care. After calculating the attitude scores, we found that 79.2% of the participants obtained more than half of the total possible score, with a mean score of 29.58 (out of a possible 52 points) and a standard deviation of 12.58. Approximately 38% and 5% answered 60% and 70% of the attitude questions positively, respectively. Those who had a family member or contact treated with rTMS (n = 12) had a more positive attitude toward rTMS (Pearson correlation r = 0.4, n = 96, P < 0.001).
TABLE 3.
Distribution of Answers Concerning Attitudes Toward rTMS
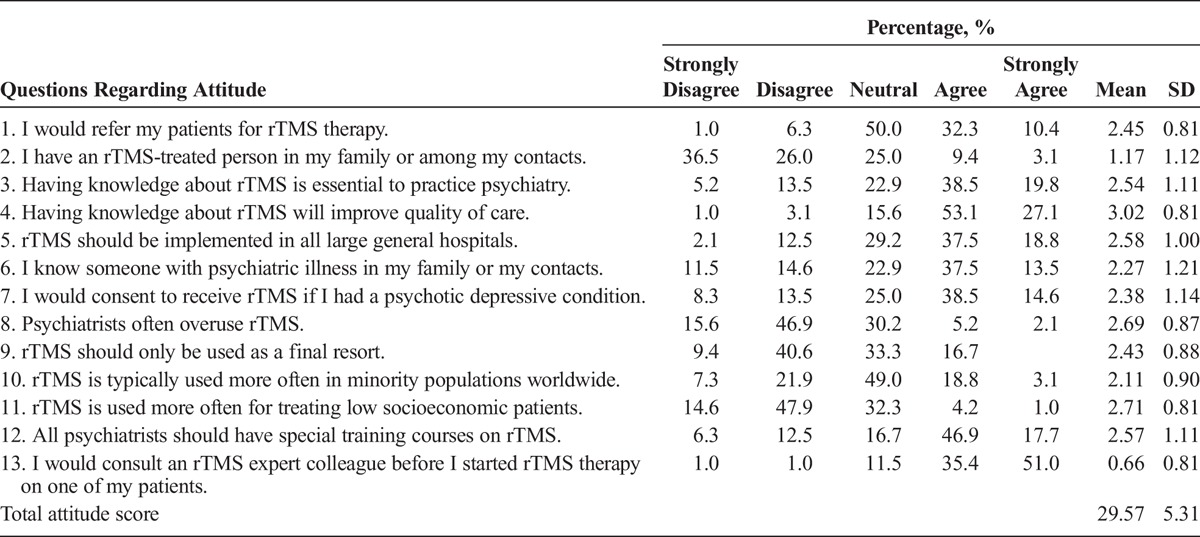
Training variables (level of training and training abroad for more than 6 months) did not show any statistically significant association with attitude (F3,92 = 0.928, P = 0.430 and F1,94 = 1.567, P = 0.214, respectively).
Reliability of the Scale
The internal consistency reliability of the overall scale was good (Cronbach α = 0.74). The knowledge section was more reliable than the attitude section, with a Cronbach α of 0.88 for knowledge and 0.61 for attitude.
DISCUSSION
This study is about psychiatrists' knowledge of and attitudes toward rTMS in Saudi Arabia. The response rate was 33%, which is similar to the average response rate to Web-based surveys.24 The e-mail accounts that we used in distributing the survey are not 100% correct or active. The ratio of male to female (5:1) in our study is similar to the ratio of psychiatrists in Saudi Arabia who are registered in the Saudi Commission for Health Specialties, the license body of health workers in Saudi Arabia.
One of the aims of the study was to assess basic rTMS knowledge among different subgroups of physicians. Consultants and specialists showed similar levels of knowledge. We assume that this is because both groups had to graduate from a residency program in which they could acquire sufficient knowledge of rTMS. On the other hand, consultants had greater rTMS knowledge than residents, as illustrated in the results. This could be because consultants were more experienced and encountered more patients with different illnesses. In addition, they had attended more conferences and exchanged experiences with other psychiatrists worldwide.
As seen in the results, physicians who used articles to keep their knowledge current had a higher level of knowledge than physicians who used textbooks. Articles have more accurate and more up-to-date information compared with textbooks and are easily accessible, which could help explain these results.
There was no relationship between the level of knowledge and training abroad for more than 6 months. We expect that this is because the rTMS device is only available in a few hospitals both locally and abroad, and thus, both groups had a similar exposure to rTMS. Approximately 40% of the sample got training abroad, and at the same time only 8% of the sample have experience with rTMS. This reflects the limited rTMS exposure.
Psychiatrists who had family members or relatives treated with rTMS had more relevant rTMS experience, which positively affected their attitudes. A previous study on patients who had been treated with rTMS showed that they also had positive attitudes toward rTMS.20 We can thus say that rTMS is perceived as an acceptable treatment, especially among those who have experienced it.
Repetitive transcranial magnetic stimulation is an effective, safe, noninvasive treatment with fewer adverse effects than ECT. Most participants (80.2%) thought that having rTMS knowledge would improve quality of care. Another study on ECT showed that there were fewer misconceptions and a greater acceptance of ECT among patients who obtained their information from a doctor. This emphasizes the role of physician knowledge in improving quality of care.
One fifth of the psychiatrists (22%) stated that they would not consider having rTMS therapy if they experienced psychotic depressive symptoms. Another study on attitudes toward ECT among Hungarian psychiatrists found that 32% of the participating psychiatrists would not consider undergoing ECT therapy.19 We believe that this difference is due to the different adverse effects of ECT compared with rTMS.
Approximately 79% of the psychiatrists thought that they lacked knowledge about rTMS; surprisingly, the study showed that 80% of them had a sufficient level of knowledge. We think that this is because rTMS is a new device, and thus, participants underestimated their knowledge due to a lack of experience (91.7% had no experience with rTMS). In addition, this is maybe due to physicians' perfectionism and they want to be sure about their answers. In 1 study, about one third of family medicine residents underestimate themselves and believe they are less intelligent and less competent. This is a well-known phenomenon, which is called imposter phenomenon.25
CONCLUSIONS
In summary, most psychiatrists had a sufficient level of knowledge and a positive attitude toward rTMS. Those who had a high level of training and experience showed higher levels of knowledge. Furthermore, we found that articles were a better source for improving physicians' knowledge of rTMS than textbooks. Finally, having a family member or relative who had been treated with rTMS positively affected psychiatrists' attitudes toward rTMS.
Recommendations
We recommend conducting the same study in other countries and among other specialties (eg, neurologists, family physicians) to further validate these results.
Limitations
One limitation of the study was that the test-retest assessment of the scale's reliability was only conducted with 5 participants.
Footnotes
This research was funded by the SABIC Psychological Health Research and Applications Chair, Department of Psychiatry, College of Medicine, Deanship of Post Graduate Teaching, King Saud University. The authors have no conflicts of interest or financial disclosures to report.
REFERENCES
- 1.Londero A, Langguth B, De Ridder D, et al. Repetitive transcranial magnetic stimulation (rTMS): a new therapeutic approach in subjective tinnitus? Neurophysiol Clin. 2006;36:145–155. [DOI] [PubMed] [Google Scholar]
- 2.Lefaucheur JP, André-Obadia N, Antal A, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125:2150–2206. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Food and Drug Administration. Guidance for Industry and FDA Staff - Class II Special Controls Guidance Document: Repetitive Transcranial Magnetic Stimulation (rTMS) Systems [Internet]. Available from: http://www.fda.gov/RegulatoryInformation/Guidances/ucm265269.htm. Accessed September 18, 2015.
- 4.Saudi Food and Drug Authority (SFDA) [Internet]. [cited 2016 Jan 15]. Available at: http://old.sfda.gov.sa/en/Pages/default.aspx. Accessed January 15, 2016.
- 5.Horvath JC, Perez JM, Forrow L, et al. Transcranial magnetic stimulation: a historical evaluation and future prognosis of therapeutically relevant ethical concerns. J Med Ethics. 2011;37:137–143. [DOI] [PubMed] [Google Scholar]
- 6.Pascual-Leone A, Gates JR, Dhuna A. Induction of speech arrest and counting errors with rapid-rate transcranial magnetic stimulation. Neurology. 1991;41:697–702. [DOI] [PubMed] [Google Scholar]
- 7.Kolbinger HM, Höflich G, Hufnagel A, et al. Transcranial magnetic stimulation (TMS) in the treatment of major depression—a pilot study. Hum Psychopharmacol Clin Exp. 1995;10(4):305–310. [Google Scholar]
- 8.Wassermann EM. Risk and safety of repetitive transcranial magnetic stimulation: report and suggested guidelines from the International Workshop on the Safety of Repetitive Transcranial Magnetic Stimulation, June 5–7, 1996. Electroencephalogr Clin Neurophysiol. 1998;108:1–16. [DOI] [PubMed] [Google Scholar]
- 9.Ren J, Li H, Palaniyappan L, et al. Repetitive transcranial magnetic stimulation versus electroconvulsive therapy for major depression: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2014;51:181–189. [DOI] [PubMed] [Google Scholar]
- 10.Rossi S, Hallett M, Rossini PM, et al. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120:2008–2039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Micallef-Trigona B. Comparing the effects of repetitive transcranial magnetic stimulation and electroconvulsive therapy in the treatment of depression: a systematic review and meta-analysis. Depress Res Treat. 2014;2014:135049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koenig HG, Al Zaben F, Sehlo MG, et al. Mental Health Care in Saudi Arabia: Past, Present and Future. Open J Psychiatry. Scientific Research Publishing. 2014;4:113–130. [Google Scholar]
- 13.Alkhamis A. Health care system in Saudi Arabia: an overview. East Mediterr Heal J. 2012;18:1078–1079. [DOI] [PubMed] [Google Scholar]
- 14.Mental Health Atlas 2011. World Health Organization. 2011. Available at: http://whqlibdoc.who.int/publications/2011/9799241564359_eng.pdf. Accessed January 15, 2016.
- 15.Mental Health Atlas 2011, Saudi Arabia. World Health Organization. 2011. Available at: http://www.who.int/mental_health/evidence/atlas/profiles/sau_mh_profile.pdf?ua=1. Accessed January 15, 2016.
- 16.Dowman J, Patel A, Rajput K. Electroconvulsive therapy: attitudes and misconceptions. J ECT. 2005;21:84–87. [DOI] [PubMed] [Google Scholar]
- 17.Dauenhauer LE, Chauhan P, Cohen BJ. Factors that influence electroconvulsive therapy referrals: a statewide survey of psychiatrists. J ECT. 2011;27:232–235. [DOI] [PubMed] [Google Scholar]
- 18.Dan A, Grover S, Chakrabarti S. Knowledge and attitude of patients with psychiatric disorders and their relatives toward electroconvulsive therapy. Indian J Psychol Med. 2014;36:264–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gazdag G, Kocsis N, Tolna J, et al. Attitudes towards electroconvulsive therapy among Hungarian psychiatrists. J ECT. 2004;20:204–207. [DOI] [PubMed] [Google Scholar]
- 20.Walter G, Martin J, Kirkby K, et al. Transcranial magnetic stimulation: experience, knowledge and attitudes of recipients. Aust N Z J Psychiatry. 2001;35:58–61. [DOI] [PubMed] [Google Scholar]
- 21.Mayer G, Faivel N, Aviram S, et al. Repetitive transcranial magnetic stimulation in depressed adolescents: experience, knowledge, and attitudes of recipients and their parents. J ECT. 2012;28:104–107. [DOI] [PubMed] [Google Scholar]
- 22.Lutchman RD, Stevens T, Bashir A, et al. Mental health professionals' attitudes toward and knowledge of electroconvulsive therapy. J Ment Heal [Internet]. Rampton Hospital, Woodbeck. Nottinghamshire. 2001;10:141–150. [Google Scholar]
- 23.IBM. IBM SPSS Statistics for Windows. Armonk, NY: IBM Corporation; 2011. [Google Scholar]
- 24.Cunningham CT, Quan H, Hemmelgarn B, et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol. 2015;15:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oriel K, Plane MB, Mundt M. Family medicine residents and the impostor phenomenon. Fam Med. 2004;36:248–252. [PubMed] [Google Scholar]


