Abstract
Stillbirth is a globally significant public health problem with many medical causes. There are also indirect causal pathways including social and cultural factors which are particularly salient in India's traditional society. The purpose of this study was to explore women's perceptions of stillbirth and to determine how issues of gender and power, social support, coping efforts, and religious beliefs influence perinatal grief outcomes among poor women in rural Chhattisgarh, India. Structured interviews were done face-to-face in 21 randomly selected villages among women of reproductive age (N = 355) who had experienced stillbirth (n = 178) and compared to those who had not (n = 177), in the Christian Hospital, Mungeli catchment area. Perinatal grief was significantly higher among women with a history of stillbirth. Greater perinatal grief was associated with lack of support, maternal agreement with social norms, and younger maternal age. These predictors must be understood in light of an additional finding—distorted sex ratios, which reflect gender discrimination in the context of Indian society. The findings of this study will allow the development of a culturally appropriate health education program which should be designed to increase social support and address social norms, thereby reducing psychological distress to prevent complicated perinatal grief. Perinatal grief is a significant social burden which impacts the health women.
Keywords: Perinatal grief, Social provision of support, Social norms, India
Introduction
Stillbirth has been acknowledged in the Global Action Agenda report as a significant global public health problem which is complex and difficult to manage [1]. Interventions are hampered by insufficient data [2] and inconsistency in the definition of stillbirths for reporting purposes [3, 4]. There are also multiple medical causes of stillbirth which are characteristically different in developed versus developing nations [5, 6], and indirect causal pathways.
Indirect causal pathways are environmental, social, and cultural factors. Environmental factors include deficient infrastructure which contributes to a lack of women receiving antenatal care [7], cooking with bio-mass fuels [8] and poverty [9].
Social norms facilitating systematic gender discrimination also contribute to stillbirths in India, which is one of four countries with the highest stillbirth rates in the world. Gender discrimination includes disparity of female education [10], son preference, early marriage [11] and low female autonomy [12, 13].
Cultural factors linked to stillbirths in India include; traditions such as seclusion of pregnant women; dissuading women from utilizing preventive services [14]; prescribing birthing practices such as dietary restrictions [15]; the type of remedies sought when problems arise, such as traditional remedies and spiritual healing [14]; and other practices such as consanguineous marriages [16].
These social and cultural factors also influence how women perceive, grieve, and cope with stillbirth. Studies in the West have resulted in understanding that perinatal grief is unique [17, 18], increasing the risk of complicated grief [19] which results in significant social and psychological burden [20]. In the West, predictors of perinatal grief include maternal coping style [21] and social support [22]. Outside of Western countries, however, little is known about how women perceive the experience of stillbirth, and what factors may inhibit or enhance their ability to cope with the loss [23].
Grief resulting from the stillbirth experience is not universally expressed. Unlike grieving over a newborn's death, some societies consider grieving for a stillbirth unacceptable [24], potentially prolonging the grief reaction. In this context, women have been found to experience delayed grief for stillbirths 20 years after the event [2].
In India, the medical community has viewed perinatal grief as a Western phenomenon, however, Mammen [25] showed that Indian women experience similar psychological distress. Additionally, factors unique to non-western countries may actually put these women at higher risk for mental health problems resulting from perinatal grief. The role of women in developing countries is often defined by fertility [26, 27], therefore, the experience of stillbirth can result in social isolation [17, 28], at a time when a women is in need of social support. India is a very religious society [29], with well over 80 percent of the population identified as Hindu [30]. Hindu women are excluded from death rituals and the burial of their stillborn child [31], which may potentiate their perinatal grief [32]. Intrinsic religiosity, on the other hand, may have a protective effect [33].
The purpose of this mixed methods study was to explore women's perceptions of stillbirth and to determine how issues of gender and power, social support, coping efforts, and religious beliefs may uniquely influence perinatal grief outcomes among poor women in rural Chhattisgarh, India. Phase one is described elsewhere [34] and included review of de-identified medical records of all 2010 deliveries at Christian Hospital, Mungeli, in Chhattisgarh, qualitative key informant interviews and validation focus groups to explore the context of stillbirth in this region. This paper concentrates on phase two, the quantitative phase of the study and explores predictors of perinatal grief among 355 poor rural women living in Chhattisgarh, India; some of whom had experienced stillbirth and others who had not.
Methods
Study Population
Women of reproductive age in the Mungeli area of the Bilaspur district, a rural region of the northwestern sector of Chhattisgarh, were selected by convenience sampling in randomly selected villages. Reproductive age was considered to be ages 15–49, as defined in the 2005–2006 National Family Health Survey-3, India [35].
The population of Chhattisgarh is 33.1% tribal [36], 12.2% scheduled castes [37], primarily Hindus [30], with a female literacy rate of 51.85% reported for the state [30], though averages obscure vast variations in India's urban versus rural areas and rich or poor people, caste and tribe [38]. Primarily Hindi and Chhattisgarhi are the languages of the region [30]. Among women of reproductive age, 50% have no education, and only 8% of rural women have their deliveries in a facility [39]. The mean age of marriage for rural women is 18.7, but 23 percent were married before the age of 18 [40].
De-Identified Medical Records Review
Christian Hospital, Mungeli is a 100 bed rural hospital in the Bilaspur district in north Chhattisgarh. Records review of all deliveries occurring in 2010 was performed for the purpose of identifying key areas of concern and identifying trends. The information, from 536 deliveries in 2010, guided avenues of inquiry for the qualitative interviews in phase one of the study. Themes that emerged in the qualitative interviews and focus groups were linked to current literature. These themes and validated scales, when available, were used to develop a structured interview.
Structured Interviews
The one-on-one structured interviews were used to explore demographics, risk factors for stillbirth, cultural norms, access to facilities, women's experiences and their perceptions regarding stillbirths, as well as coping techniques and perinatal grief, and consisted of both closed-ended and open-ended general questions and Likert type scales.
The informed consent and structured interview guide were written in both English and Hindi. Translation was done by a bilingual committee. Independent forward and backward translation was employed to ensure cultural and functional equivalence beyond literal translation, a time consuming but imperative process [41]. Verbal translation from Hindi to Chhattisgarhi (a dialect of Hindi) was undertaken when required.
Local outreach workers were selected with language, gender, and cultural matching, then trained to protect human research participants using the modules developed by the National Institute of Health (NIH) Office of Extramural Research, and finally trained to uniformly conduct the interviews.
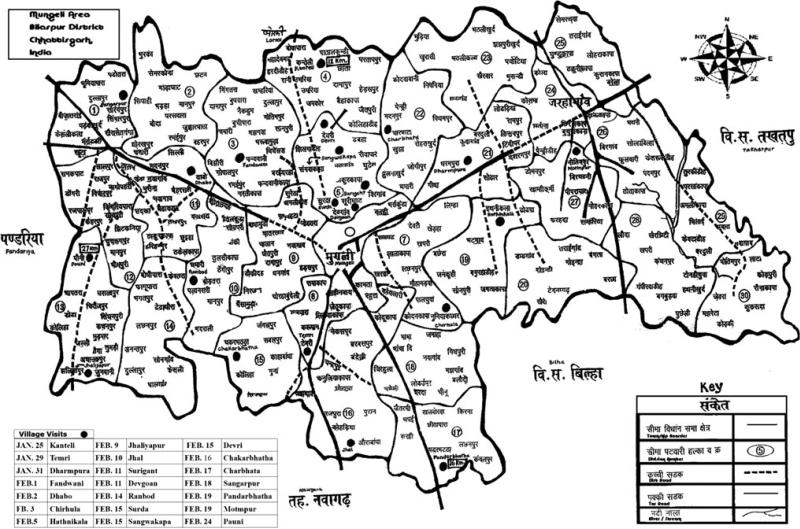
A list of villages within the Christian Hospital, Mungeli catchment area was compiled from the de-identified medical records review, and from this list villages within the Mungeli area were randomly selected. The order of visitation for the selected villages was determined by transportation availability. See Fig. 1 for a map of the Mungeli area and the villages visited.
Fig. 1.
Map of the Mungeli area, Bilaspur District, Chhattisgarh, India. Villages visited: 1 Kanteli, 2 Temri, 3 Dharmpura, 4 Fandwani, 5 Dhabo, 6 Chirhula, 7 Hathnikala, 8 Jhaliyapur, 9 Jhal, 10 Surigaht, 11 Devgoan, 12 Ronbod, 13 Surda, 14 Sangwakapa, 15 Devri, 16 Chakarbhatha, 17 Charbatha, 18 Sangarpur, 19 Pandarbhatha, 20 Motinpur, 21 Pauni
The structured interview guide was pilot tested among 14 village women in Kanteli, a village with a population of 3,500–4,000 approximately 12 km from Christian Hospital, Mungeli. Based on the performance of the pilot the final structured interview guide required only two minor wording and time frame changes.
The structured interview consisted of demographic and general health questions, questions pertaining specifically to the event of stillbirth, and the following validated scales which were analyzed for reliability within this sample. The Social Provision Scale—this 12-item version assesses several components of the perceptions that social support is received from others [42]. A 4-point Likert-type scale with possible responses ranging from (1) strongly agree to (4) strongly disagree is summed for an index score of 12–48 with higher scores reflecting more social support (Cron-bach's alpha = 0.74). The Shortened Ways of Coping-Revised scale is a 14-item Likert-type scale which contains two subscales measuring two distinct ways of coping—wishful thinking and practical coping [43]. Each subscale is summed, resulting in two index scores with higher scores indicating more frequent use of that particular coping strategy [44]. Possible responses ranged from never to daily (Cronbach's alpha = 0.88). The Perinatal Grief Scale is a 33-item 5-point Likert scale ranging from (5) strongly agree to (1) strongly disagree [45]. Items are summed for an index score of 33 to 165, with higher scores representing more intense grief (Cronbach's alpha = 0.91). Reverse coded items were reversed before summing the index scores.
An autonomy scale and a social norms for progressiveness scale were created from questions asked in previous studies in India related to these topics. The autonomy scale questions were specific to women who typically have low autonomy, for example to ascertain who decides if she should get health care for herself, and whether she can go to the market without permission. It is a 4-item scale, summed for an index score of 0–8 (Cron-bach's alpha 0.54). The social norms for progressiveness scale is designed to measure women's attitudes toward social norms on a continuum of very traditional to progressive. It is a 7-item scale, summed for an index score of 0–14; Cronbach's alpha of 0.50. Measurement of intrinsic religiosity was accomplished using a one-item measure which Gorsuch and McPherson [46] identified as having the highest correlation with the intrinsic religiosity factor in a 20 item scale and “showed the same pattern of correlations with the other scales as did the total scale” (p. 352).
Women who had not had stillbirth were compared to women with a history of stillbirth on all measures except questions specifically related to stillbirth. (The questions pertaining to the stillbirth included antenatal care, place of delivery, type of attendee, length of labor, sex of baby, gestational age, maternal age at the time, and appearance of the baby). They were asked to consider how they thought they would feel if they were to experience stillbirth in relation to the perinatal grief questions, for trending purposes.
In total, 21 villages were visited, with populations ranging from approximately 300–8,000, averaging 2,475. Women from 35 different villages actually participated in the structured interviews because those visiting relatives in their natal villages or otherwise present in the villages visited were not excluded and three structured interviews were conducted with patients at Christian Hospital, Mungeli.
Analysis
SPSS version 17 was used for statistical analysis, including descriptive statistics, factor analyses, scale development, significance tests between sets of variables of interests, and multiple linear regression equations. Data was collected from 355 structured interviews, 178 from women who had experienced stillbirth and 177 from women who had not had a stillbirth.
Results
Study Population
Women who participated in the study were of reproductive age, reporting ages 16–49, resulting in an average age of 27.43, and a history of first delivery at mean age 18.87, however, figures pertaining to maternal age in this study are approximate as many of the women did not know their age and therefore an approximate age was recorded. Most were daughter-in-laws in terms of household position, at 80.3 percent. The ethnicity of the participants was 33.2% scheduled castes, 10.4% scheduled tribes, 48.2% other backwards castes, and 8.2% other groups such as high castes [Scheduled castes are a class of people designated as such according to Article 341 of the Indian Constitution empowering the President of India to do so [37]. They are the depressed classes—those born into the low castes of Hinduism, who are therefore unacceptable to those of higher caste—putting those in the low castes at great social disadvantage with little or no opportunity to improve their lot in life. According to Narayan [47] they are oppressed castes, or marginalized groups also known as Dalits.] Nearly all the participants were Hindu (99.4%). Almost half (47.9%) had no education. Anemia was the most common health problem; however, most participants reported having no health problems. The average number of pregnancies was 3.66 with a range of 1–13, family planning was rare with 84.8% not using any contraceptive method, and 80.1% had birth intervals of less than 2 years. See Table 1 for comparison of descriptive statistics pertaining to the Indian population, population of Chhattisgarh, and the study population, as well as comparison of the study population groups—women who had experienced stillbirth and those who had not.
Table 1.
Descriptive statistics of variables comparing the population of India, Chhattisgarh, and our study population
| India | Chhattisgarh | Study participants | Study participants with history of stillbirth N = 178 | Study Participants without stillbirth N = 177 | |
|---|---|---|---|---|---|
| Scheduled tribe (ST) | 8.08%a | 33.13%b | 10.4% | 14.6% (N = 26) | 6.2% (N = 11) |
| Scheduled castes (SC) | 16.48%a | 12.2%c | 33.2% | 31.5% (N = 56) | 35.0% (N = 62) |
| Other backwards castes (OBC) | 80.3% | 46.6% (N = 83) | 49.7% (N = 88) | ||
| Hindu | 80.44%a | 99.4% | 100% (N = 178) | 98.9% (N = 175) | |
| Female literacy rate among ST | 18.19%a | ||||
| Female literacy rate among SC | 25.00%a | ||||
| Female literacy rate among rural women of reproductive age | 41.1%e | ||||
| Women who used thumbprint rather than signature | 40.0% | ||||
| Women of reproductive age with no education | 50.0%d | 47.9% | 53.9%(N = 96)** | 41.8% (N = 74) | |
| Rural woman having facility births | 8.0% | 18.0% (N = 32) | |||
| Birth intervals < 2 years | 81.4% (N = 144) | 78.3% (N = 137) | |||
| Report of domestic violence | 20.3% (N = 36) | 13.6% (N = 24) | |||
| Ever had a sonogram | 43.3% (N = 77)* | 29.4% (N = 52) | |||
| Women reporting no health problems | 63.5%(N = 113)** | 81.9% (N = 145) | |||
| Tobacco and/or paan used | 25.3% (N = 45)* | 13.6% (N = 24) | |||
| Mean age of marriage for rural women | 18.7e | ||||
| Rural women married before the age of 18 | 23.0%e | ||||
| Mean age at first delivery | 18.87 | 19.01 | 18.74 | ||
| Birth Control Pill use among rural women of reproductive age | 1.4%e | 0.8% | 0.6% (N = 1) | 1.1% (N = 2) | |
| No form of contraceptive used | 84.8% | 86.0% (N = 153) | 83.6% (N = 148) | ||
| Total fertility rate | 2.62f | 2.6d | 3.6 | 4.6 | 2.7 |
| Total female to male sex ratio | 0.93f | 0.99a | 0.94 | ||
| Female to male sex ratio among rural stillborn babies reported | 0.81g | 0.53 |
The stillbirth group of women was similar to the comparison group on descriptive measures. However, the stillbirth group was significantly higher on tobacco use and the combination of tobacco and paan (a chewing mixture of areca nut and lime wrapped in a betel leaf or a similar variation), significantly more of these women had no education, and they had significantly more health problems and had sonograms. Looking at all study participants, the sex ratio of reported number of living daughters to number of living sons was 0.94. Among women who had experienced stillbirth, the sex ratio for stillborn babies reported was 0.53. The women's number of stillbirths ranged from one to five.
Christian Hospital, Mungeli Delivery Records for 2010
The mean age of the 536 mothers was 24.18, with a range of 18–40 years old, and 49.8% were primigravida. Most mothers were in the general ward, 65.2%, with only 31.9% registered in private rooms and 2.9% without ward or room designation recorded. Over 86% of the women came to the hospital for delivery unbooked (i.e., were not pre-registered for delivery at the hospital). There were 16 sets of twins, giving a total of 552 babies born. Female babies born totaled 41.1% (223), male babies 58.9% (319), giving a sex ratio at birth of 0.69 (gender was not recorded for 10 babies). Deliveries by Cesarean section totaled 61.7% and 38.3% were born by vaginal delivery with or without the use of forceps. The sex ratio for babies born by Cesarean section was 0.61. Of the women who had Cesarean section, 22.2% also had a bilateral tubal ligation done. The average baby weight was 2,639.6 grams. The lowest birth weight recorded was 980 grams and the maximum was 4,400 grams. The mean weight for male babies was higher than for female babies, 2,700 (SD 535.1) and 2,567.8 (SD 526.9) respectively, a statistically significant difference (t [490] = −0.2.70, p = 0.007). There were 57 stillbirths; equivalent to a stillbirth rate of 103 per 1,000 live births.
Structured Interviews
Mean Comparison of Women with and without a History of Stillbirth
There were significant differences in maternal age, number of pregnancies, and number of living daughters, emotion focused coping, and perinatal grief each higher in the stillbirth group. Comparative socioeconomic status and social norms for progressiveness were lower in the stillbirth group. See Table 2 for comparison of our study sample women with and without a history of stillbirth. Emotion focused coping was not as highly significant as the other significant variables.
Table 2.
Comparing women in our study who have a history of stillbirth to those who have not had stillbirth
|
N = 178 N = 177 |
Mean | SD | Sig. (2-tailed) | 95% CI for the difference in means | |
|---|---|---|---|---|---|
| Maternal age | Stillbirth | 29.29 | 7.96 | 0.000 | 2.22, 5.21 |
| No stillbirth | 25.57 | 6.27 | |||
| Number of pregnancies | Stillbirth | 4.60 | 2.32 | 0.000 | 1.48, 2.29 |
| No stillbirth | 2.71 | 1.44 | |||
| Mother's age at 1st delivery | Stillbirth | 18.74 | 2.27 | 0.241 | −0.74, 0.19 |
| No stillbirth | 19.01 | 2.15 | |||
| Comparative SES (1 = worse, 2 = same, 3 = better) | Stillbirth | 2.15 | 0.63 | 0.000 | −0.37, −0.10 |
| No stillbirth | 2.39 | 0.61 | |||
| Social provision of support (11–44, higher score indicates more social support) | Stillbirth | 37.22 | 4.12 | 0.758 | 0.97, 0.71 |
| No stillbirth | 37.36 | 3.89 | |||
| Autonomy (0–8, higher score indicates more autonomy) | Stillbirth | 4.16 | 1.55 | 0.500 | −0.21, 0.44 |
| No stillbirth | 4.05 | 1.58 | |||
| Intrinsic religiosity | Stillbirth | 1.97 | 0.18 | 0.992 | −0.04, 0.04 |
| No stillbirth | 1.97 | 0.18 | |||
| Emotion focused coping (0–14, higher score indicates more reliance on this coping method) | Stillbirth | 8.83 | 2.35 | 0.013 | 0.13, 1.10 |
| No stillbirth | 8.21 | 2.32 | |||
| Practical coping (0–14, higher score indicates more reliance on this coping method) | Stillbirth | 7.57 | 2.04 | 0.363 | −0.23, 0.63 |
| No stillbirth | 7.37 | 2.09 | |||
| Social norms for progressiveness (0–14, higher score indicates progressive attitude) | Stillbirth | 7.53 | 3.26 | 0.002 | −1.85, −0.43 |
| No stillbirth | 8.67 | 3.51 | |||
| Perinatal grief (33–165, higher score indicates more grief) | Stillbirth | 111.31 | 17.53 | 0.000 | 3.9, 10.8 |
| No stillbirth | 103.95 | 15.46 |
Perinatal Grief Trend
Overall perinatal grief scores were significantly higher (p < 0.001) for women who had experienced stillbirth compared with those who had not, 111.31 (SD 17.529) and 103.95 (SD 15.459) respectively. However, the mean perinatal grief scores were higher than expected for the comparison group, and 21.1% of the women without a history of stillbirth had lost live born children. Further analysis revealed there were significant (p < 0.001) differences in perinatal grief scores comparing women who had not had stillbirth nor lost any children, women who had not had stillbirth but had otherwise lost children, women who had a history of stillbirth but had not lost any other children and women who had a history of stillbirths and had lost other children also (Table 3). Time since stillbirth ranged from less than 1–30 years, with a mode of 2 years. Grief regressed on time since stillbirth was not significant; that is, there was no tendency for grief to drop or increase as time since the stillbirth increased.
Table 3.
Perinatal grief trend by losses suffered
| Group | Mean grief score | N | SD |
|---|---|---|---|
| Women who have nor lost any children | 102.64 | 140 | 14.91 |
| Women who have not had stillbirth but have lost at least one live born child | 108.92 | 37 | 16.68 |
| Women who have had stillbirth but have not lost any live children | 110.99 | 140 | 18.06 |
| Women who have had stillbirth and at least one live born child | 112.53 | 38 | 15.58 |
| df | 1,353 | ||
| F | 17.60** |
Total N = 355.
p < 0.01
Correlates of Perinatal Grief for Women with a History of Stillbirth
Possible correlations between perinatal grief outcomes and the independent variables of interest were explored using bivariate analysis, see Table 4. Increased social provision of support, increased social norms for progressiveness, and maternal age at stillbirth were all negatively related to perinatal grief at p < 0.01. Emotion focused coping and practical coping were significant predictors of increased perinatal grief, though the association was not as strong.
Table 4.
Single linear regressions exploring correlates of grief among rural women in Chhattisgarh, with a history of stillbirth
| Variable | Perinatal grief |
|||
|---|---|---|---|---|
| R 2 | β | B | 95% CI | |
| Social provision of support | 0.10 | −0.32** | −1.36 | −1.96, −0.76 |
| Position in household | 0.00 | 0.34 | 1.35 | −4.47, 7.16 |
| Victim of domestic violence | 0.01 | 0.07 | 3.13 | −3.32, 9.57 |
| Contraceptive use | 0.00 | 0.05 | 1.95 | −3.42, 7.32 |
| Number of living sons | 0.02 | 0.12 | 2.03 | −0.40, 4.45 |
| Number of living daughters | 0.00 | −0.04 | −0.49 | −2.22, 1.23 |
| Education | 0.00 | −0.02 | −0.42 | −3.21,2.38 |
| Comparative SES | 0.01 | 0.10 | 2.73 | −1.37, 6.83 |
| Mother's age at 1 st delivery | 0.01 | −0.12 | −0.92 | −2.07, 0.22 |
| Social norms for progressiveness | 0.24 | 0.49** | −2.62 | −3.32, −1.92 |
| Intrinsic religiosity | 0.00 | −0.05 | −5.19 | −19.58, 9.19 |
| Autonomy | 0.02 | −0.13 | −1.43 | −3.09, 0.24 |
| Maternal age | 0.00 | −0.06 | −0.13 | −0.46, 0.20 |
| Gestational age | 0.01 | 0.11 | 4.97 | −1.60, 11.54 |
| Number of pregnancies | 0.01 | 0.07 | 0.51 | −0.61, 1.63 |
| Number of stillbirths | 0.01 | 0.08 | 1.65 | −1.26, 4.57 |
| Emotion focused coping | 0.02 | 0.15* | 1.14 | 0.04, 2.23 |
| Practical coping | 0.04 | 0.19* | 1.66 | 0.41, 2.91 |
| Maternal age at stillbirth | 0.08 | −0.28** | −0.99 | −1.50, −0.50 |
p < 0.05
p < 0.01
Predictors of Perinatal Grief for Women with a History of Stillbirth
To further explore the variables that were significantly associated with perinatal grief on bivariate analysis, perinatal grief was regressed on social norms for progressiveness, social provision of support, emotion focused coping, practical coping, and maternal age at stillbirth, see Table 5. The model explained 36% of the variance in perinatal grief. Increased social norms for progressiveness, social provision of support, and maternal age at stillbirth were each highly significant predictors of reduced perinatal grief. Emotion focused coping and practical coping were not significant in this model. There were no significant interactions.
Table 5.
Predictors of grief among women in Chhattisgarh with a history of stillbirth
| Variable | β | B | 95% CI |
|---|---|---|---|
| Constant | 176.19 | 151.20, 201.17 | |
| Social norms for progressiveness | −0.44** | −2.35 | −3.02, −1.69 |
| Social provision of support | −0.23** | −0.98 | −1.52, −0.44 |
| Emotion focused coping | 0.02 | −0.14 | −0.89, 1.16 |
| Practical coping | 0.05 | 0.43 | −0.76, 1.63 |
| Maternal age at stillbirth | −0.20* | −0.69 | −1.13, −0.25 |
p < 0.05
p < 0.01
Discussion
Study Sample
India is a vast country, with highly varied geography and numerous groups with different languages, customs, and culture, and additional variations in urban and rural settings. In this setting it would be inappropriate to expect the sample to be representative of the population of Chhattisgarh or India as a whole. The comparisons shown in Table 1 are provided for contextualization only. The study sample is consistent with the target population, namely, poor rural women of reproductive age in the Mungeli area.
Participants with and without stillbirths were fairly comparable on descriptive statistics. However, it is noteworthy that the stillbirth group was higher on tobacco and both tobacco and paan use, more of these women had no education, they had more health problems, and more had sonograms; known risk factors associated with stillbirth [8, 48–51].
The sex ratio of 0.94 for reported number of living daughters and number of living sons is lower than the sex ratio reported for Chhattisgarh, 0.99 [30] but similar to the national rural sex ratio of 0.93 reported by Jha, et al. [51]. In this study, the sex ratio for stillborn babies reported was 0.53, there were fewer female (N = 61) than male (N = 116) stillbirths reported. This finding is consistent with the results Jha et al. [51] reported in their analysis of 1.1 million households surveyed in India. Overall, stillbirths were more commonly reported to be male; thus the national rural stillbirth sex ratio was 0.81, though the reason for this was not explained. In fact, the authors report that female infanticide occurs early, typically the first day after birth and is presumably reported as either a stillbirth or early neonatal death. That would actually skew the stillbirth sex ratio toward a higher female to male stillbirth ratio. However, the fact remains that the low sex ratio of live births in India is a worsening trend, most likely due to sex determination followed by abortion of female babies, particularly when there are already one or more girls in the family. These abortions, if reported at all, would be categorized as miscarriages and thus would not affect the stillbirth ratio.
Christian Hospital, Mungeli Delivery Records for 2010
The high rate of unbooked deliveries reflects the culture. Typically normal deliveries are conducted at home and only once complications arise are women brought to the hospital for delivery. Women presenting to Christian Hospital, Mungeli for delivery were suffering complications such as anemia, prolonged labor, pre-eclampsia, placenta previa, abruptio placentae, and uterine rupture, as well as high risks such as breech presentations and twins. Their babies presented with complications such as hand or cord prolapse, footling breech, transverse presentation, low birth weight, fetal distress, muconium staining, and intrauterine death. Hence the high rate of Cesarean sections and stillbirths. The low sex ratio and disparity in weight for female babies is unexplained but appears to reflect gender discrimination, a well-documented problem in India [51], to which Chhattisgarh is no exception.
Structured Interviews
Mean Comparison of Women with and without a History of Stillbirth
The significant difference in average maternal age, with the stillbirth group approximately 4 years older, likely reflects that older women have had more opportunities for stillbirth to occur and women over the age of 35 are at increased risk of stillbirth [52]. The number of pregnancies and number of living daughters were both significantly higher in the stillbirth group. These variables go hand-in-hand, particularly in the Indian context where the quest for sons drives fertility up and families keep trying for a son when they have had only daughters [11] Socioeconomic status was also worse in the stillbirth group, another well documented risk factor for stillbirths [7, 48].
Perinatal Grief Trend
Perinatal grief scores were significantly higher for women who had experienced stillbirth compared with those who had not. However, perinatal grief scores were higher than expected among those who had not experienced stillbirth. These women were asked to answer the perinatal grief scale questions according to how they thought they would feel if it had happened to them. It is possible that these women were very empathetic, but another plausible explanation is that their answers were influenced by the experience of other losses and otherwise losing children. Toedter, Lasker, and Janssen reviewed 22 studies in four Western countries and found that 95% of the time perinatal grief scores will fall between 78 and 91. Therefore, for normative purposes, they stated that a score greater than 91 can be considered to reflect a high degree of grief [20]. Only 23% of our sample had perinatal grief scores below 91.
Perinatal grief scores were progressively higher for women who had lost children without a history of stillbirth, women who had experienced stillbirth but had not lost any live born children, and women who had experienced the double loss of stillbirth and loss of one or more live born children. Time since stillbirth had a 30 year variance and did not significantly relate to grief. This seems to indicate that significant grief may be experienced for many years following stillbirth, which agrees with Lawn et al. [2].
Correlates of Perinatal Grief for Women with a History of Stillbirth
Social provision of support was highly significant, with a small to medium effect size (R2 = 0.24) predicating less perinatal grief with increased social support. In this setting, social repercussions for infertility noted in the literature include abandonment, mistreatment, or divorce [28] and also determines the social hierarchy these women find themselves in within the husband's family [53]. Women in phase one of our study [34] discussed abandonment or a second wife being brought into bear children after stillbirth occurred. Such serious disruptions to the social provision of support are likely to put women at increased risk for higher levels of perinatal grief. Social norms for progressiveness was a highly significant predictor of lower grief. A woman with a progressive attitude is likely to reject traditional social norms such as early marriage and child-bearing, and son preference. Maternal age at the time of stillbirth was also highly significant; as their age increased, perinatal grief decreased. This likely reflects that older women have had more opportunities to have children, and may have other live children. Additionally, older women may hold a higher position within the household hierarchy [54] and therefore may be less vulnerable to the social repercussions of stillbirth. Emotion focused coping and practical coping were also significant, but as these coping efforts increased perinatal grief also increased. This likely reflects that coping effort is increased as a result of the stillbirth event and therefore correlates with perinatal grief. Neither coping style remained significant in the multiple regression model.
Predictors of Perinatal Grief for Women with a History of Stillbirth
When the statistically significant variables from bivariate analyses were all put into the multiple regression model, social support and social norms for progressiveness, and maternal age at the time of stillbirth repeated the same pattern as was noted above in the bivariate analyses; as these variables increased, perinatal grief decreased. However in this model, neither coping variable significantly predicted perinatal grief. This may be due to the strong correlation between practical coping and emotion focused coping (r = 0.46). However, it is possible that coping effort does not play a more definite part in perinatal grief outcomes in this context due to the overwhelming sense of fatalism that is pervasive in India [9]. Causal appraisal may not be generated at all, and therefore, coping effort may not be initiated [55]. Interestingly, gender of the stillborn did not predict perinatal grief. Mean perinatal grief scores were not significantly different for mothers with a male stillbirth compared to mothers with a female stillbirth 110.4 (SD 17.7) and 112.8 (SD 17.3) respectively, p = 0.396. Although India's son preference is well documented in the literature, it appears to occur at a societal level rather than among the mothers. Mothers in our study grieved the loss of their babies regardless of gender.
Strengths and Limitations
There are several limitations to be noted. This was a cross-sectional study, and as such, causality could not be determined for any of the associations noted. Error in recall and strong emotions related to the subject matter may have resulted in self-reporting bias. Additionally, this study was limited to poor rural women in the Mungeli area of Chhattisgarh, India and therefore is not generalizable to the rest of India with its vast variations of cultures, traditions, castes, and religions.
Strengths of the study include useable data and results. The medical records review contained in this study summarized the current delivery factors and outcomes at Christian Hospital, Mungeli. This data may be useful to monitor trends and guide future research and interventions.
The data collected in the villages and subsequent analysis, contributes to the limited literature regarding rural, central Indian women's perceptions regarding pregnancy and delivery care, how they cope with the loss of stillbirths, and their grief related to the experience. The enhanced understanding gained through this study, of the stillbirth experience including psychological distress, social burden, and factors that influence maternal coping, is particularly important for developing countries. More than half of the total global stillbirths occur in just four nations, one of which is India [24]. Understanding the way that social norms, social support, and maternal age at the time of stillbirth affect grief outcomes will guide future interventions aimed at reducing perinatal grief, a significant mental health issue and social burden.
Conclusion
Stillbirth is a complex public health problem involving medical, environmental, social, and cultural causal pathways that also factor into the aftermath of stillbirth. In India, social norms play a particularly important role in how women perceive, grieve, and cope with stillbirth.
Perinatal grief has been recognized as a significant social and psychological burden in the West. This study adds to the sparse previous evidence that Indian women also experience significant perinatal grief. Indian women in fact suffer with high levels of perinatal grief, which contributes to mental health problems and social issues—a significant public health burden requiring further attention.
It is noteworthy that only 23% of the women had “normal” perinatal grief scores using the admittedly Western based scoring for the standardized perinatal grief scale we used [20]. Those who had specifically suffered the loss of live-born children, or stillbirth, or both had progressively higher perinatal grief scores- ranging far into the highest and most risk –associated range. It is plausible that the high perinatal grief scores among these poor rural Indian women who had not suffered stillbirth are reflecting a general sense of grief. Their everyday lives are filled with loss and grief. As women, they have lost basic human rights, they have lost whatever autonomy they might have had before marriage, they have lost dignity as they must submit to the wishes of their husbands and in-laws. If, on top of all of their everyday grief they suffer the loss of stillbirth, their grief is terribly strong.
Known risk factors for stillbirth were noted at higher rates in the stillbirth group (the use of tobacco and paan, low education levels, and maternal health problems). Other findings, such as the greater use of sonograms among women with stillbirth and the link between the higher number of pregnancies with a greater number of daughters, as well as the distorted sex ratios, reflect grave social concerns in India— namely gender discrimination.
Salient results of this study indicate that women who experienced stillbirth had significantly higher grief than those who had not, regardless of the stillborn gender. However, social support and social norms for progressiveness were highly significant and negatively associated with perinatal grief, offering some protection. This has important implications for future health education interventions, which should be aimed at increasing family provision of social support and promoting social progressiveness rather than letting traditional social norms stand unchallenged. The worsening gender discrimination as evidenced by the trend in sex ratio can only be reversed through social change.
Acknowledgments
The authors gratefully acknowledge the access and introductions to Chhattisgarhi villages provided by Dr. Anil Henry, medical director of Christian Hospital Mungeli.
This work was partially supported by a LLU CHR dissertation grant award.
Footnotes
Publisher's Disclaimer: Your article is protected by copyright and all rights are held exclusively by Springer Science+Business Media, LLC. This e-offprint is for personal use only and shall not be self-archived in electronic repositories. If you wish to self-archive your work, please use the accepted author's version for posting to your own website or your institution's repository. You may further deposit the accepted author's version on a funder's repository at a funder's request, provided it is not made publicly available until 12 months after publication.
Conflict of interest No funding or financial support was received for this research, no conflict of interest to declare.
Contributor Information
Lisa R. Roberts, In Your Best Interest Medical Clinic, 1201 Brookside Ave., Redlands, CA 92373, USA
Susanne Montgomery, Behavioral Health Institute, Loma Linda University, 1898 Business Center Dr., San Bernardino, CA 92408, USA.
Jerry W. Lee, Department of Health Promotion and Education, School of Public Health, Loma Linda University, Nichol Hall, Loma Linda, CA 92350, USA
Barbara A. Anderson, Doctor of Nursing Practice, Frontier Nursing University, 4263 Quail Rd., Riverside, CA 92507, USA
References
- 1.Rubens C, et al. Global report on preterm birth and stillbirth (7 of 7): Mobilizing resources to accelerate innovative solutions (Global Action Agenda). BMC Pregnancy and Childbirth. 2010;10(Suppl 1):S7. doi: 10.1186/1471-2393-10-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawn J, et al. Global report on preterm birth and stillbirth (1 of 7): Definitions, description of the burden and opportunities to improve data. BMC Pregnancy and Childbirth. 2010;10(Suppl 1):S1. doi: 10.1186/1471-2393-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woods R. Long-term trends in fetal mortality: Implications for developing countries. Bulletin of the World Health Organization. 2008;86(6):460–466. doi: 10.2471/BLT.07.043471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Facchinetti F, et al. International issues in stillbirth. Journal of Maternal-Fetal & Neonatal Medicine. 2008;21(6):425–428. doi: 10.1080/14767050802040849. [DOI] [PubMed] [Google Scholar]
- 5.Kramer MS, et al. Analysis of perinatal mortality and its components: Time for a change? American Journal of Epidemiology. 2002;156(6):493. doi: 10.1093/aje/kwf077. [DOI] [PubMed] [Google Scholar]
- 6.Nhu Thi Nguyen N, et al. Causes of stillbirths and early neonatal deaths: Data from 7993 pregnancies in six developing countries. Bulletin of the World Health Organization. 2006;84(9):699–705. doi: 10.2471/blt.05.027300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Di Mario SM, Say L, Lincetto O. Risk factors for stillbirth in developing countries: A systematic review of the literature. Sexually Transmitted Diseases. 2007;34(7):S11–S21. doi: 10.1097/01.olq.0000258130.07476.e3. [DOI] [PubMed] [Google Scholar]
- 8.Mishra V, Retherford RD, Smith KR. Cooking smoke and tobacco smoke as risk factors for stillbirth. International Journal of Environmental Health Research. 2005;15(6):397–410. doi: 10.1080/09603120500288913. [DOI] [PubMed] [Google Scholar]
- 9.Lawn J, et al. Reducing intrapartum-related deaths and disability: Can the health system deliver? International Journal of Gynecology & Obstetrics. 2009;107:S123–S142. doi: 10.1016/j.ijgo.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 10.Korde-Nayak Vaishali N, Gaikwad Pradeep R. Causes of stillbirth. The Journal of Obstetrics and Gynecology of India. 2008;58(4):314–318. [Google Scholar]
- 11.Croll E. Endangered daughters: Discrimination and development in Asia. Routledge; London: 2000. [Google Scholar]
- 12.Lee ACC, et al. Linking families and facilities for care at birth: What works to avert intrapartum-related deaths? International Journal of Gynecology & Obstetrics. 2009;107:S65–S88. doi: 10.1016/j.ijgo.2009.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yesudian PP. Synergy between women's empowerment and maternal and peri-natal care utilization. 2009;15 [Google Scholar]
- 14.Lawn J, et al. Two million intrapartum-related stillbirths and neonatal deaths: Where, why, and what can be done? International Journal of Gynecology & Obstetrics. 2009;107:S5–S19. doi: 10.1016/j.ijgo.2009.07.016. [DOI] [PubMed] [Google Scholar]
- 15.Ramakrishna J, et al. Health, illness and care in the obstetric period: A prospective study of women in rural Karnataka. In: Koenig M, et al., editors. Reproductive health in India: new evidence. Rawat Pubns; New Delhi: 2008. pp. 86–115. [Google Scholar]
- 16.Sathyanarayana Rao TS, et al. Consanguinuity: Still a challenge. Indian Journal of Psychiatry. 2009;51(1):5. doi: 10.4103/0019-5545.44896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kelly ER. Marking short lives: Constructing and sharing rituals following pregnancy loss. Peter Lang Publishing; New York, NY, USA: 2007. Marking short lives: Constructing and sharing rituals following pregnancy loss. [Google Scholar]
- 18.Rowland A, Goodnight WH. Fetal loss: Addressing the evaluation and supporting the emotional needs of parents. Journal of Midwifery & Women's Health. 2009;54(3):241–248. doi: 10.1016/j.jmwh.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 19.Bennett SM, et al. The scope and impact of perinatal loss: Current status and future directions. Professional Psychology: Research and Practice. 2005;36(2):180–187. [Google Scholar]
- 20.Toedter LJ, Lasker JN, Janssen HJEM. International comparison of studies using the Perinatal Grief Scale: A decade of research on pregnancy loss. Death Studies. 2001;25(3):205–228. doi: 10.1080/07481180125971. [DOI] [PubMed] [Google Scholar]
- 21.Engler AI, Lasker JN. Predictors of maternal grief in the year after a newborn death. Illness, Crisis & Loss. 2000;8(3):227. [Google Scholar]
- 22.Bennett SM, et al. An exploratory study of the psychological impact and clinical care of perinatal loss. Journal of Loss & Trauma. 2008;13(6):485–510. [Google Scholar]
- 23.Kelley M, Rubens C. Global report on preterm birth and stillbirth (6 of 7): Ethical considerations. BMC Pregnancy and Childbirth. 2010;10(Suppl 1):S6. doi: 10.1186/1471-2393-10-S1-S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stanton C, et al. Stillbirth rates: Delivering estimates in 190 countries. Lancet. 2006;367(9521):1487–1494. doi: 10.1016/S0140-6736(06)68586-3. [DOI] [PubMed] [Google Scholar]
- 25.Mammen OK. Women's reaction to perinatal loss in India: An exploratory, descriptive study. Infant Mental Health Journal. 1995;16(2):94–101. [Google Scholar]
- 26.Pandalangat N. Mental health services for women in third world countries and immigrant women. In: Romans S, Seeman M, editors. Women's mental health: A life-cycle approach. Lippincott Williams & Wilkins; PA: 2006. [Google Scholar]
- 27.Fottrell E, et al. Risk of psychological distress following severe obstetric complications in Benin: The role of economics, physical health and spousal abuse. The British Journal of Psychiatry. 2010;196(1):18. doi: 10.1192/bjp.bp.108.062489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joshi A, Dhapola M, Pelto PJ. Gynaecological problems: Perceptions and treatment-seeking behaviors of rural Gujarati women. In: Koenig M, et al., editors. Reproductive health in India: New evidence. Rawat Publications; New Delhi: 2008. pp. 133–158. [Google Scholar]
- 29.Bauman C. Grand Rapids. Eerdmans Pub Co.; Michigan: 2008. Christian identity and Dalit religion in Hindu India, 1868–1947. [Google Scholar]
- 30.Mathew KM. Manorama yearbook. Malayala Manorama Press; Kottayam, Kerela, India: 2010. [Google Scholar]
- 31.Gatrad AR, Ray M, Sheikh A. Hindu birth customs. Archives of Disease in Childhood. 2004;89(12):1094–1097. doi: 10.1136/adc.2004.050591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lasker JN, Toedter LJ. Satisfaction with hospital care and interventions after pregnancy loss. Death Studies. 1994;18(1):41. doi: 10.1080/07481189408252642. [DOI] [PubMed] [Google Scholar]
- 33.McIntosh DN, Silver RC, Wortman CB. Religion's role in adjustment to a negative life event: Coping with the loss of a child. Journal of Personality and Social Psychology. 1993;65(4):812–821. doi: 10.1037//0022-3514.65.4.812. [DOI] [PubMed] [Google Scholar]
- 34.Roberts LR, et al. Grief and women: Inextricable in the Indian social context. 2011 [Google Scholar]
- 35.Kavitha N. The effect of adolescent pregnancy on poor birth outcomes: Does it differ between rural and urban areas? In: James KS, et al., editors. Gender population health in India: Methods, processes, policies. Academic Foundation; New Delhi: 2010. pp. 333–347. [Google Scholar]
- 36.Mandal H, Mukherjee S, Datta A. India: An illustrated atlas of tribal world. Anthropological Survey of India Calcutta, Ministry of Tourism and Culture, Dept. of Culture, Govt. of India; India: 2005. [Google Scholar]
- 37.Mandal H, et al. India, an illustrated atlas of scheduled castes. Anthropological Survey of India, Ministry of Culture, Govt. of India; India: 2005. [Google Scholar]
- 38.UNICEF . Maternal and perinatal death inquiry and response: Empowering communities to avert maternal deaths in India. UNICEF, Department of International Development; New Delhi: 2008. p. 84. [Google Scholar]
- 39.IIPS. 2005–2006 national family health survey (NFHS-3) fact sheet Chhattisgarh. International Institute for Population Sciences; Mumbai: 2008. [Google Scholar]
- 40.Cassidy T. All work and no play: A focus on leisure time as a means for promoting health. Counselling Psychology Quarterly. 1996;9(1):77–90. [Google Scholar]
- 41.Jones P, et al. An adaptation of Brislin's translation model for cross-cultural research. Nursing Research. 2001;50(5):300. doi: 10.1097/00006199-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 42.Mosley Williams A, et al. Barriers to treatment adherence among African American and white women with systemic lupus erythematosus. Arthritis Care & Research. 2002;47(6):630–638. doi: 10.1002/art.10790. [DOI] [PubMed] [Google Scholar]
- 43.Hatton C, Emerson E. The development of a shortened’ ways of coping’ questionnaire for use with direct care staff in learning disability services. Mental Handicap Research. 1995;8(4):237–251. [Google Scholar]
- 44.Mascha K. Staff morale in day care centres for adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities. 2007;20(3):191–199. [Google Scholar]
- 45.Potvin L, Lasker J, Toedter L. Measuring grief: A short version of the Perinatal Grief Scale. Journal of Psychopathology and Behavioral Assessment. 1989;11(1):29–45. [Google Scholar]
- 46.Gorsuch RL, McPherson SE. Intrinsic/extrinsic measurement: I/E-Revised and single-item scales. Journal for the Scientific study of Religion. 1989;28(3):348–354. [Google Scholar]
- 47.Narayan B. Women heroes and Dalit assertion in north India: Culture, identity and politics. Cultural Subordination and the Dalit Challenge. Sage Publications Pvt. Ltd.; CA: 2006. [Google Scholar]
- 48.McClure EM, Nalubamba-Phiri M, Goldenberg RL. Stillbirth in developing countries. International Journal of Gynecology & Obstetrics. 2006;94(2):82–90. doi: 10.1016/j.ijgo.2006.03.023. [DOI] [PubMed] [Google Scholar]
- 49.Claeson M, et al. Reducing child mortality in India in the new millennium. Bull World Health Organ. 2000;78:1192–1199. [PMC free article] [PubMed] [Google Scholar]
- 50.Coker AL, Sanderson M, Dong B. Partner violence during pregnancy and risk of adverse pregnancy outcomes. Paediatric and Perinatal Epidemiology. 2004;18(4):260–269. doi: 10.1111/j.1365-3016.2004.00569.x. [DOI] [PubMed] [Google Scholar]
- 51.Jha P, et al. Low male-to-female sex ratio of children born in India: National survey of 1.1 million households. Lancet. 2006;367(9506):211–218. doi: 10.1016/S0140-6736(06)67930-0. [DOI] [PubMed] [Google Scholar]
- 52.Huang L, et al. Maternal age and risk of stillbirth: A systematic review. CMAJ: Canadian Medical Association Journal. 2008;178(2):165–172. doi: 10.1503/cmaj.070150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Barua A, Kurz K. Reproductive health-seeking by married adolescent girls in Maharashtra. In: Koenig M, et al., editors. Reproductive health in India: New evidence. Rawat Publications; New Delhi: 2001. pp. 32–46. [DOI] [PubMed] [Google Scholar]
- 54.Mistry R, Galal O, Lu M. Women's autonomy and pregnancy care in rural India: A contextual analysis. Social Science and Medicine. 2009;69(6):926–933. doi: 10.1016/j.socscimed.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 55.Glanz K, Schwartz MD. Stress, coping, and health behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health behavior and health education; theory, research, practice. Jossey-Bass; San Francisco: 2008. pp. 211–236. [Google Scholar]
- 56.IIPS. District level household and facility survey (DLHS-3) 2007–2008 fact sheet Chhattisgarh. International Institute for Population Sciences; India: 2009. [Google Scholar]
- 57.CIA. The world factbook: South Asia—India 5/6/11; population: Total fertility rate. 2011 Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/in.html.