Abstract
Background
Public health breakdown from the Syrian government's targeting of healthcare systems in politically unsympathetic areas has yielded a resurgence of infectious diseases. Suspected cholera recently reappeared but conflict-related constraints impede laboratory confirmation. Given the government's previous under-reporting of infectious outbreaks and the reliance of the WHO on government reporting, we sought to assess the reliability of current surveillance systems.
Methods
We compared weekly surveillance reports of waterborne diseases from the Syrian government's (WHO-associated) Early Warning and Response System (EWARS), based in Damascus, and the independent, non-governmental Early Warning and Response Network (EWARN) headquartered in Gaziantep, Turkey. We compared raw case rates by EWARS and EWARN and assessed the quality of reporting against the WHO benchmarks.
Results
We identified significant under-reporting and delays in the government's surveillance. On average, EWARS reports were published 24 days (range 12–61) after the reference week compared with 11 days (5–21) for EWARN. Average completeness for EWARS was 75% (55–84%), compared with 92% for EWARN (85–99%). Average timeliness for EWARS was 79% (51–100%), compared with 88% for EWARN (70–97%). EWARS made limited use of rapid diagnostic tests, and rates of collection of stool samples for laboratory cholera testing were well below reference levels.
Conclusions
In the context of the current Syrian war, the government's surveillance is inadequate due to lack of access to non-government held territory, an incentive to under-report the consequence of government attacks on health infrastructure, and an impractical insistence on laboratory confirmation. These findings should guide the WHO reform for surveillance in conflict zones.
Key questions.
What is already known about this topic?
Cholera outbreaks occur in settings of poor sanitation, inadequate surveillance and weak infrastructure.
Cholera presents a serious threat to Syria and other countries in conflict.
The current WHO case definition of cholera and other waterborne disease requires reference laboratory confirmation.
What are the new findings?
Significant deficiencies in the identification and follow up of suspected cholera cases has been identified.
Reliance on the Syrian state surveillance system is likely to lead to a significant underestimation of the threat posed by cholera and other contagious diseases.
Independent non-governmental surveillance is more timely and comprehensive but undermined by lack of access to laboratories.
Recommendations for policy
For effective surveillance in conflict settings, global recommendations for the WHO reform must address the need for operational independence from governments, especially those like Syria's that are trying to undermine public health for part of its population.
In conflicts where timely laboratory confirmation of cholera and other contagious diseases is unfeasible, screening tests and clinical diagnosis should be used as supplements.
Cholera vaccination should be implemented as a pragmatic and cost-effective preventive strategy in areas of Syria and in other humanitarian crises where the risk of outbreak is established and control of national and cross-border spread cannot be guaranteed.
Background
The conflict in Syria has now entered its sixth year. While global attention is focused on the war trauma and the exodus of refugees to Europe, the public health crisis is escalating rapidly. In February 2016, after 5 years of war, the United Nations (UN) Office for the Coordination of Humanitarian Affairs (OCHA) estimated that 13.5 million Syrians need humanitarian assistance, including 4.6 million civilians living in hard-to-reach areas.1 An estimated 12 million need water, sanitation and hygiene (WASH) services.2 Of the 6.5 million internally displaced persons, 520 000 civilians—predominantly women and children—are forced to live in the unhygienic conditions of overcrowded camps and collective shelters, at risk of cholera and other diseases spread by contaminated water.2
Cholera is a barometer of public health. It was last reported in Syria in 2009 when an epidemic in the governorates of Deir Ezzor and Raqqa infected more than 1000 people and killed several children.3 Statements by the Syrian Ministry of Health (MoH) at the time first denied both the widespread watery diarrhoea and cholera as the cause of the outbreak (one dozen patients suffering normal diarrhoea only) and then downplayed the number, speaking of only 30 cholera cases.3 The outbreak was not reported to the Program for Monitoring Emerging Diseases (ProMED), the most important internet-based reporting system for the timely dissemination of information on outbreaks of infectious disease and other global threats. It was acknowledged only recently for the first time by the MoH in its Cholera Epidemic Preparedness and Response Plan, published by the WHO in November 2015.4
Health professionals on the front line have long been concerned that cholera would follow the same pattern as polio, another waterborne disease (WBD), which re-emerged in Syria in July 2013 after an 18-year absence.5 Denial by the Syrian government, lack of official acknowledgement by the WHO, flawed results from the national laboratory and difficulties of surveillance caused by insecurity allowed polio to spread widely. Transmitted by contaminated water and person-to-person contact, poliovirus was ultimately documented in more than half of the country's governorates, and by early 2014 had spread to Iraq, crippling children as far away as Baghdad.5 Following an extensive vaccination campaign across northern Syria, wild poliovirus was last documented in Syria in early 2014, but concerns remain given the increasing difficulties of surveillance and vaccination against a backdrop of widespread malnutrition. These concerns are heightened for the 1.1 million civilians living under siege, more than 900 000 of whom are besieged by the Syrian government, denied safe water, food, basic medical care and vaccinations.6
Cases of suspected cholera began appearing in northern Syria in October 2015.7 On 20 October, a 5-year-old boy in eastern Aleppo presented with acute watery diarrhoea (AWD) and severe dehydration, dying shortly after he tested positive for cholera on a rapid diagnostic test (RDT).8 In the same week, two children in Deir Ezzor with AWD tested positive on RDTs and also died, according to direct communication from medical colleagues in Deir Ezzor.
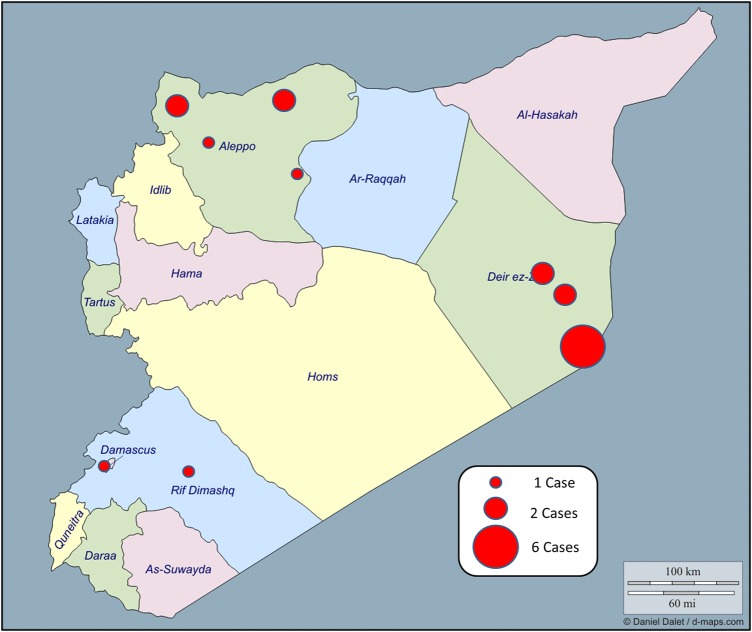
Laboratory confirmation of these and suspected cases since then (figure 1) has not been possible because of constraints on surveillance. Airstrikes by the government have destroyed all laboratories capable of confirming cholera, polio and other threats to public health in northern Syria.5 The only reference laboratory in Syria is in Damascus, effectively inaccessible to health workers serving the 11.1 million people living in areas outside of government control.9 Laboratory confirmation of cholera in the nearest reference laboratory in Ankara, Turkey, is impeded by the insecurity, the challenges of transporting specimens under controlled temperature conditions and restricted access across the border. The difficulty in collecting and transporting specimens is aggravated by the Syrian army's extensive use of land mines.5 6
Figure 1.
Cholera alerts in Syria since October 2015.
The re-emergence of suspected cholera takes place in the context of an increased incidence in WBDs documented by both the Syrian government's Early Warning and Response System (EWARS) and the independent Early Warning and Response Network (EWARN), in particular typhoid, dysentery and hepatitis A. The WHO confirmed hepatitis A in eight governorates in April 2015.10 By June, 21 773 cases of acute jaundice syndrome (AJS) had been recorded for weeks 1–21 of 201511 compared with 31 460 cases reported across all of 2014.12 These figures exclude areas outside of government surveillance. Hepatitis A and E were confirmed by independent surveillance of outbreaks of AJS in rural Damascus and northern governorates.13 WHO-supported surveillance shows increased incidence of dysentery and typhoid absent laboratory confirmation.14 In non-government territory, these diseases are predominantly diagnosed on clinical grounds.15 RDTs are available for typhoid but laboratory confirmation through the mainstay (blood culture) or the gold standard (bone marrow culture) is not available, nor is laboratory confirmation of shigellosis.
This rise in WBD occurs in the setting of long-term neglect of water and sanitation services by the government in areas considered politically unsympathetic to the regime. Since armed conflict broke out, that neglect has been compounded by the Syrian military's sustained targeting of civilians in areas held by armed forces adversarial to the government, displacing millions into crowded and unsanitary shelters, and its aggressive airstrikes on hospitals and public health infrastructure.16 Just as doctors have been criminalised for treating civilians injured at prodemocracy rallies, engineers and maintenance staff at water plants in areas outside of government control have faced arrest and had their salaries stopped.17 The International Committee for the Red Cross (ICRC) estimates that across the country half of the water infrastructure is dysfunctional or destroyed, and the availability of safe water is 5–30% of precrisis levels.18 Water plants that still function are undermined by fuel shortages while scheme water is contaminated with sewage.19 Chlorine, the primary agent for decontaminating water, has long been withheld by the government from politically unsympathetic areas, becoming an indirect agent of biological warfare, while intermittently used as a chemical weapon against civilians.20
At the same time, the government has restricted humanitarian assistance by UN agencies. Between 1 September and 30 November, the Syrian Arab Red Crescent (the UN implementing partner) delivered WASH services to only 144 000 of the 4.5 million people living in hard-to-reach areas.21 The airstrikes on water plants by the Syrian and Russian military forced the increasing use of river water and further drove the spread of WBD. One of several attacks in November alone targeted the primary water source for the Aleppo governorate, permanently cutting off water supply to 1.4 million in rural areas.22 Easily destroyed water plants are time-consuming and costly to repair. The manipulation of the water supply has in effect become a tool of war, contributing to displacement and disease.
These attacks on the civilian population and public health in areas of the country controlled by non-governmental forces should give rise to caution about the reliability of the Syrian government's reporting on public health threats in those regions.
The existing epidemics of typhoid, shigellosis and hepatitis in Syria, the cholera epidemic in Iraq, the evolving threat of cholera in Syria, and the Syrian government's history of delayed reporting and possible cover-up of WBDs in areas of the country considered politically hostile5 led us to examine the existing data on detection and reporting of WBD by the Syrian government and the independent monitoring agency conducting surveillance in areas outside government control. We sought to determine whether the official surveillance system endorsed by the WHO allows appropriate response to these threats.
Methods
We reviewed data from the two infectious disease surveillance systems operating in Syria: EWARS housed in the MoH; and EWARN set up by the Assistance Coordination Unit (ACU).
The Early Warning and Response Network
An EWARN is described as ‘a simplified system for disease surveillance that can be quickly set up in affected areas during the acute phase of an emergency with the primary purpose of rapid detection, prompt response and containment of epidemic-prone diseases among affected populations’.23 The ACU which set up the EWARN in this study was established in December 2012 by the Syrian National Coalition (the main alliance of political opposition groups) to coordinate humanitarian efforts on the basis of need alone. Its mandate is to deliver aid to all those in need ‘regardless of ethnicity, religion or political beliefs’. Aid is coordinated in accordance with international standards and human rights principles, which state that aid should be given on the basis of need alone.24 The ACU has been recognised as a humanitarian organisation since its inception, and receives support from the WHO and funding from the Bill and Melinda Gates Foundation. In 2013, the ACU was registered in Turkey as a humanitarian, non-governmental and non-political organisation, and is subject to a yearly audit by Deloitte. Its programming includes EWARN, health, information management, water and sanitation, food security, emergency shelter, education, and camp management.
EWARN was established by the ACU in June 2013 with the assistance of the US Centers for Disease Control and Prevention (CDC).25 It presents data on the number of WBD, including acute diarrhoea, acute bloody diarrhoea, AWD, AJS, acute flaccid paralysis and suspected typhoid fever. EWARN uses the reporting forms, case definitions and alert thresholds from the WHO's field manual. In addition to weekly bulletins, EWARN publishes a weekly surveillance of acute flaccid paralysis26 and a triweekly report on WBD and adequacy of chlorination of water sources in three districts considered high risk in Deir Ezzor.27 The ACU holds quarterly meetings with district-level officers in northern Syria, members of field response teams and water and sanitation and hygiene officers, under the supervision of its Health Department. In addition, Médecins Sans Frontières has trained officials involved in EWARN on such aspects of cholera as case definition, surveillance, rapid testing, collection of laboratory samples and vaccination.28
The Early Warning and Response System
The EWARS was established in September 2012 by the Syrian MoH, with technical support and funding provided by the WHO.29 30 The WHO-Syrian Arab Republic website describes EWARS as having two components: “[A]n immediate alert component (which signals the early stages of an outbreak); and a weekly reporting component…These complementary components ensure timely detection and verification of outbreaks and effective monitoring of morbidity patterns.”29 EWARS presents data on acute diarrhoea, acute bloody diarrhoea, AWD, AJS and acute flaccid paralysis. These clinical states serve as de facto markers for waterborne gastroenteritis; salmonellosis/campylobacter; cholera; viral hepatitis; polio. It presents data on suspected typhoid fever but is not disaggregated from an ‘others’ category, which includes, but is not limited to, typhoid, leishmaniasis, tuberculosis, brucellosis and pertussis. EWARS does not provide a breakdown of cases at the governorate level. In December 2013, the Syrian MoH and WHO officials described EWARS as: “established and functional…[having] succeeded so far in mitigating the consequences of many outbreaks, responding to a nation-wide measles outbreak, a typhoid outbreak in Deir Ezzor, and the present polio outbreak.”31
We collated case numbers and distribution of WBDs from the EWARS and EWARN data sets for the 12-month period from week 43 of 2014 through week 44 of 2015. We verified the data through correspondence with the WHO Regional and Syria offices and the ACU. We collected and triangulated additional data through field visits to the region and communication with as many of the reporting doctors inside Syria who could be contacted.
Raw numbers of EWARS and EWARN cases of AWD and WBD were compared for each time period. Where possible, the overall weekly reporting data were broken down by governorate for temporal trends by geography and with regard to the changing conflict-related circumstances in each region. We measured the time between the date of the first e-publication of each EWARS and EWARN weekly report against the last day of the reporting period of the report to determine the number of days’ delay and hence the average delay of each reporting system. We compared these rates to the 85% benchmark rate of timeliness recommended in the Syrian MoH's Cholera Epidemic Preparedness and Response Plan, developed with the support of the WHO and released in November 2015.4 Similarly, we assessed the completeness of each case report data set against these benchmarks. In situations where there appeared to be a marked increase in WBD cases, we performed an additional analysis (where data were available) to correct for the total number of consultations, to ensure that any increase in total reported numbers reflected a true increase and not just a reflection of more consultations.
Results
The analysis of the number and distribution of WBD cases reveals gaps in surveillance and discordance in reporting. Bulletins by EWARS were published on average 24.3 days (range 12–68) after the reference week compared with 11.4 days (range 5–21) by EWARN. In real time, this means that EWARS reports come out 2 weeks after EWARN reports. For weeks 36–44 of 2015, the time delay for EWARN was 7–13 days, compared with 18–29 days for EWARS.
EWARS stated that sentinel surveillance sites were established across all 14 governorates (figure 2). However, no population coverage or breakdown by governorate was provided. In addition, completeness of its reporting varied substantially, between 55% and 84% on a weekly basis. The average of 75% was well short of the requirement of 85% stated in the Syrian MoH's Cholera Epidemic Preparedness and Response Plan above.4 There were also errors and omissions in the EWARS reports. In 2014, week 47 is duplicated for week 48; in 2015, weeks 1 and 8 are absent altogether. Timeliness, a measure of the proportion of sentinel sites reporting each week's cases within an agreed timeframe, varied between 51% and 100%, with an average of 79%.
Figure 2.
Distribution of EWARS sentinel surveillance sites across Syria. EWARS, Early Warning and Response System.
EWARN surveillance covered a population of 11 795 443, from 513 sites in 12 governorates (figure 3). A breakdown of cases was provided at the governorate level. Completeness of reporting averaged 92% and varied by a range of 85–99%. Timeliness averaged 88% and varied by a range of 70–97%. Table 1 compares timeliness, completeness and availability of reporting of EWARS and EWARN.
Figure 3.
Distribution of EWARN sentinel surveillance sites across Syria. EWARN, Early Warning and Response Network.
Table 1.
Comparison of WBD reporting performance by EWARS and EWARN
| EWARS |
EWARN |
|||
|---|---|---|---|---|
| Average | Range | Average | Range | |
| Completeness (%) | 75 | 55–84 | 92 | 85–99 |
| Timeliness (%) | 79 | 51–100 | 88 | 70–97 |
| Report released (days)* | 24 | 12–61 | 11 | 5–21 |
Number of days between the end of each epidemiological survey week and when the data were first circulated or published online.
EWARN, Early Warning and Response Network; EWARS, Early Warning and Response System; WBD, waterborne disease.
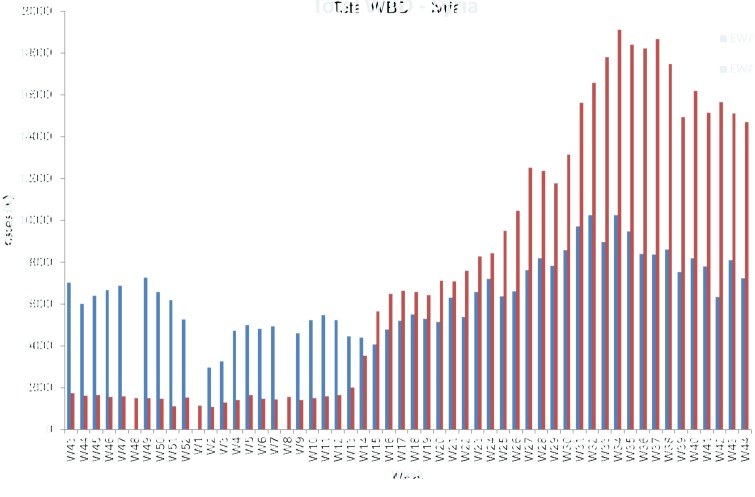
Figure 4 shows the variation in timeliness between EWARS and EWARN reporting. Total consultations for WBDs in Syria for EWARS and EWARN are reported in figure 5. Both EWARS and EWARN reported increasing WBDs after week 20 of 2015, the beginning of summer. There was, however, a decline after week 39.
Figure 4.
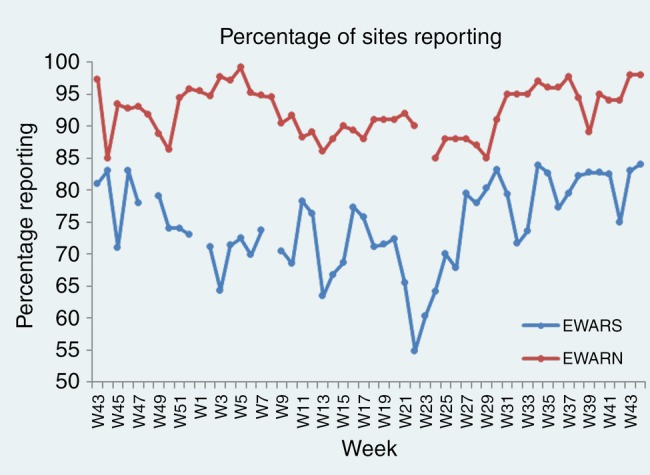
Variation in the completeness of reporting between EWARS and EWARN from week 43, 2014 through week 44, 2015. EWARN, Early Warning and Response Network; EWARS, Early Warning and Response System.
Figure 5.
Total waterborne disease consultations across Syria for EWARS and EWARN data sets. EWARN, Early Warning and Response Network; EWARS, Early Warning and Response System.
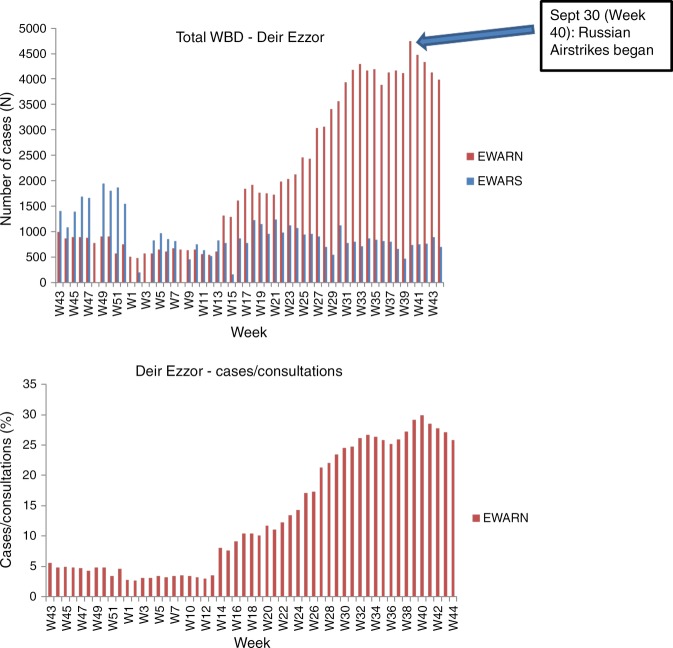
EWARN reported rising WBDs cases in Aleppo, Deir Ezzor, Al-Hassekeh, Dar'a, Homs and Idleb. Figure 6 (top) illustrates the steady rise in the number of WBD cases beginning in week 15 in Aleppo. The abrupt increase in week 15 can be attributed to the inclusion of acute diarrhoea, a new category added to the total WBD category due to the increasing number of cases, separating AWD from acute diarrhoea. EWARS reported an increase in WBD as of week 24. When we divided the number of WBD cases by the number of consultations seen each week (figure 6 bottom), the trend appears to be a true increase in WBD cases in Aleppo. A true increase in WBDs was more evident in Deir Ezzor. EWARN captured a rise in the number of WBD cases over time while the number of consultations decreased (figure 7), but EWARS showed a decline and low numbers of cases in Deir Ezzor.
Figure 6.
Total cases of waterborne disease reported in Aleppo by EWARS and EWARN (top). Rise in waterborne disease in Aleppo as analysed by cases of waterborne disease in Aleppo/total consultations in Aleppo (bottom). EWARN, Early Warning and Response Network; EWARS, Early Warning and Response System.
Figure 7.
Total number of waterborne disease cases in Deir Ezzor from week 43, 2014 through week 44, 2015 (top). Rise in waterborne disease in Deir Ezzor as analysed by cases of waterborne disease in Deir Ezzor/total consultations in Idleb (bottom). EWARN, Early Warning and Response Network; EWARS, Early Warning and Response System.
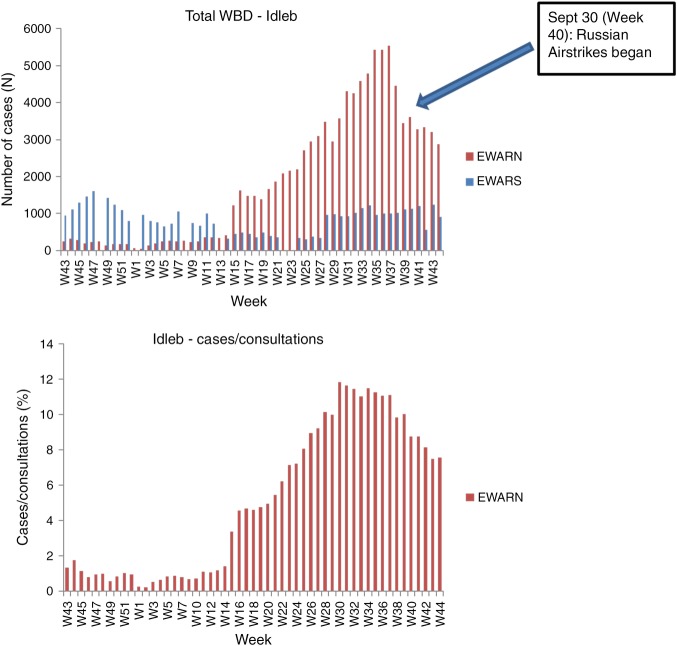
Data from Idleb governorate reported by EWARN and EWARS were consistent (figure 8). EWARS reported a sudden decrease in WBD cases in week 13, with a levelling off until the abrupt rise in cases in week 28 and a levelling off through week 41, suggesting that surveillance was compromised during these 4 months. In addition, EWARS did not report any data for the entire governorate of Idleb for weeks 13, 22 and 23 in 2015. Since EWARS did not provide a breakdown by governorate, the analysis of cases as a proportion of weekly consultations could not be performed.
Figure 8.
Total number of waterborne disease cases in Idleb from week 43, 2014 through week 44, 2015 (top). Rise in waterborne disease in Idleb as analysed by cases of waterborne disease in Idleb/total consultations in Idleb (bottom). EWARN, Early Warning and Response Network; EWARS, Early Warning and Response System.
EWARS presented little data on laboratory testing of suspect cases of cholera. Of the 31 cases of AWD reported between weeks 2 and 38 in 2015, a RDT was performed on only one (in Raqqa) and reported as negative. Only one stool sample was sent for testing in the Damascus reference laboratory and was reported as negative.32 No stool samples from the 30 other cases of AWD were sent for laboratory testing due to lack of access.27 EWARS data did not include the first RDT-positive case identified by EWARN on 20 October (week 43). In week 44, EWARS reported a case of AWD in Damascus as RDT-positive, which later showed a negative result by laboratory culture.14
In response to this case, the EWARS bulletin stated that the MoH asked all the health directorates in all governorates to ‘activate surveillance for all AWD admitted to hospitals, collect stool samples from all suspected cases and notify the directorate of communicable diseases in the MoH with laboratory results immediately’.14 However, no stool sample was taken from the next case of AWD in rural Damascus the following week (week 45); nor was a RDT used because ‘clinical investigation showed that the suspected case is not in accordance with the standard case definition of cholera’.33
Discussion
Summary and explanation of results
The findings of this study indicate that EWARS may not have the capacity to detect epidemic-prone diseases, particularly in areas outside of government control. The relatively poor quality of EWARS reports relative to EWARN and its limited geographical coverage suggest that the WHO, by relying solely on EWARS, may not be well prepared to address cholera in Syria. There are also differences in the timeliness of reporting between EWARS and EWARN. The 2-week delay in publication of EWARS weekly bulletins potentially compromises judicious analysis of alerts and limits timely comparison of aggregated data. EWARS procedure in week 45 contradicts the WHO guidelines for outbreak surveillance in humanitarian emergencies, which state that ‘all alerts must be verified and outbreaks investigated within 24 hours using a standardised case investigation form and an approved specimen collection method’.34 The absence of published laboratory reports confirming isolation of another microbe capable of causing RDT-positive AWD raises concerns that a negative report may be inconclusive or a false negative, due to factors such as an uncertain cold chain or the inadequacy of samples. No plausible alternative diagnosis to cholera for these cases has been provided.
Both EWARS and EWARN reported increasing WBDs from week 20 of 2015 (the beginning of warmer summer months typically associated with increases in cholera and other WBD) and a decline after week 39. The decline may be seasonal but it is also coincident with the onset of Russian airstrikes which may have impeded surveillance.35 Since 30 September 2015, several medical personnel have been killed in airstrikes by Syrian and Russian air forces.35
The increase in WBD cases in Aleppo may be linked to the fact that the supply of safe water for the residents of Aleppo governorate is estimated at 20% of precrisis levels.36 Likewise, the increase in WBDs in Deir Ezzor is perhaps because only 10% of water plants still function in the governorate.18 The combination of the Syrian government's targeted destruction of the plants, its withholding of chlorine, and its recurrent airstrikes make repair and rehabilitation of the plants very difficult. Furthermore, the contrasting decline and low numbers in EWARS data (compared with EWARN data) in Deir Ezzor is consistent with increasingly limited access by government employees to Deir Ezzor, and EWARS reports frequently refer to this limitation.14 33 37 In addition, EWARS reports no data for the entire governorate of Idleb for weeks 13, 22 and 23 in 2015, perhaps because the Syrian army lost control of Idleb city in late March 2015 and has little to no access to the Idleb governorate, which has been under the control of non-state armed forces since early June.38
Comparison with previous studies and significance of findings
To the best of our knowledge, this is the first published comparative assessment of WBD surveillance systems from within an area of active armed conflict. The gaps in the Syrian government surveillance system identified in this study raise concern about underdetection of WBDs by EWARS which, given the WHO's sole reliance on it, indicate the weak capacity of the WHO to respond to a potential epidemic. There is strong circumstantial evidence to suggest that cholera is re-emerging in Syria. As it did with polio, the WHO's insistence on laboratory confirmation of cholera is inappropriate in a conflict zone such as Syria where access to the one recognised national laboratory in Damascus is limited. That compounds the problem of under-reporting by government agencies. The documented failure of EWARS to follow established protocols for investigating suspected cases of cholera raises further concern. The WHO's guidelines for outbreak surveillance in humanitarian emergencies require that ‘all alerts must be verified and outbreaks investigated within 24 hours using a standardised case investigation form and an approved specimen collection method’.34
The consequence of a delayed response to a cholera outbreak can be seen in neighbouring Iraq, where cholera spread to five districts before the epidemic was officially acknowledged in September 2015.39 In cholera outbreaks, typically only 30% of cases are reported. In this particular instance, cholera cases were detected through RDTs on Iraq's western border with Syria—tests that were not accepted by the WHO because of its insistence on laboratory confirmation.
The WHO should be particularly sensitive to timely reporting of cholera: first, because it was the epidemics of cholera in the 19th century that gave rise to the predecessor of the WHO (the Health Office of the League of Nations) and second, because poor surveillance fuelled the Seventh Pandemic, which began in 1961 and is still escalating.40 Previous reports show that the WHO surveillance consistently under-reports the global burden of cholera because the WHO acknowledges only cases reported by governments.41 42 However, reporting by member states can be influenced by national interests in trade and tourism as well as limited by problems of access to reference laboratories. Conflicting national interest has been linked to the WHO's inability to respond effectively to recent cholera outbreaks, and led to a World Health Assembly (WHA) Resolution on Cholera in 2011 which called for a stronger, more coordinated response by the WHO highlighting ‘the importance of emergency preparedness planning, surveillance strengthening, early response’ and ‘improved environmental management, improved hygiene and sanitation behaviour, and access and appropriate use of cholera vaccines’.43
However, in the 4 years since the WHA Resolution, cholera's rise has continued. For 2014, the WHO reported a total of 190 549 cases and 2231 deaths due to cholera in 42 endemic countries.41 The WHO states that these figures represent only 5–10% of the true global burden. This under-reporting is borne out by an analysis undertaken by Ali et al42 for the same year, which estimates 2.86 million cases and 95 000 deaths each year and identifies 69 endemic countries.43
Strengths and limitations of this study
This study reflects a comprehensive analysis of the currently available data reports of cholera and other WBD in Syria. Given the discrepancies between the completeness and timeliness of reporting between the government and ACU systems, it is not possible to determine how much the EWARS under-reporting is directly related to conflict-related access limitations or the product of external influence on the reporting systems by the Syrian government. Either way, it represents a warning to the WHO not to rely solely on government-produced data when alternative sources may supply a better or supplemental picture.
Recommendations for future research
Research into disease surveillance in regions of conflict is inevitably challenging. Securing multilateral support for such research and publication will not always be possible. However, Syria is not the only situation of armed conflict or civil insecurity where a combination of access limitations and lack of government concern with the public health of at least portions of its population would call into question the reliability of government-produced information. There is an ethical imperative to conduct research on vulnerable populations at risk of infectious disease, particularly diseases which pose global threats and are issues of global governance. Similar studies might be conducted in South Sudan, eastern Ukraine, Yemen and Myanmar.
Recommendations for policy and practice
The current attention to reforming the WHO to better undertake emergency surveillance44 45 presents the opportunity to review the WHO's response in conflict zones, including the need to ensure avenues for reporting that are independent from governments. The WHO's limited ability to compel member states even to implement the International Health Regulations should inform pragmatic strategies for operational emergency response in conflict zones. This study suggests that in countries in conflict, control of outbreaks and cross-border spread should allow for notification of global threats by non-state parties.
The Syrian government's conflict-related, systematic destruction of public health infrastructure including water treatment facilities, in combination with the mass displacement of a civilian population under attack, poses a major threat to regional health and security. Even if conflict abates through diplomatic efforts, the potential collaboration between EWARS and EWARN should continue to be explored. In the interim, it may be necessary for international actors operating independently of the government to legitimise and strengthen EWARN's systems of surveillance, coordination and response.
More generally, there is a need to legitimise and strengthen existing systems of surveillance, coordination and response involving local and international actors operating independently of the government. A precedent exists: since 2014, the Bill and Melinda Gates Foundation has been providing financial and technical support directly to the ACU in recognition of the effective surveillance by EWARN in documenting the polio outbreak and coordinating the cross-border vaccination campaign carried out by the Polio Task Force. An agency such as the US or European Centers for Disease Control could provide independent monitoring, merge surveillance data, ensure information sharing, and perform analysis for the timely detection and control of serious global threats.
In addition, it is time to recognise that reliance on a laboratory diagnosis of cholera, polio and other contagious disease as the sole confirmation of the presence of a disease is impractical in conflict and should be supplemented by onsite screening tests and clinical diagnosis. Research into reliable RDTs should also be pursued. Cholera vaccination should be implemented as a cost-effective preventive strategy in Syria and other humanitarian crises where the risk of outbreak is established and control of national and cross-border spread cannot be guaranteed, particularly in non-endemic countries.
Conclusions
We have shown that in the current Syrian conflict, the government's surveillance system is inadequate. In conflict zones, especially when the government is openly attacking parts of its population, surveillance should not depend solely on the reporting of a single party which may have access limitations or an incentive to colour the data. Moreover, an insistence on reference laboratory testing should be recognised as impractical and supplemented by accessible, reliable screening tests and clinical diagnosis. Given the WHO's reliance on government surveillance systems, these findings should inform the re-evaluation of its preparedness strategies in conflict zones and guide the WHO's reform for emergency response.
The UN Secretary-General's High Level Panel (HLP) is currently reviewing the WHO's response and preparedness to global health crises, but its narrow focus on what went wrong with the Ebola crisis ignores the additional complexities faced in conflict settings, despite the strong association between infectious disease and war and the abundance of contemporary conflicts.46 The HLP recognises that in West Africa governmental political concerns impeded the WHO's timely response to Ebola, but it does not address the prospect of similar governmental political concerns impeding accurate reporting in conflict zones, and hence the need for some operational independence from governments, particularly when, as in Syria, the government as a party to the conflict continues to target civilians, doctors, hospitals and public health infrastructure indispensable to the survival of civilians in areas considered hostile to the government.
Syria is not the only country where the government cannot be relied on to prioritise protecting the public health of certain segments of the population. A similar situation exists today in Yemen, Ukraine and South Sudan. In such situations, the accuracy of the WHO's reporting is likely to be compromised if, as an agency that deals primarily with governments, the WHO is not attentive to the possible limitations of governmental surveillance and reporting and thus open to alternative non-governmental sources of information. The need to ensure these alternative lines of communication and information should be part of the WHO reform strategy.
Acknowledgments
The authors acknowledge the assistance of the Health Department of the Syrian Assistance Coordination Unit, in particular the hundreds of field officers in the EWARN, as well as the EWARS programmes performing surveillance of public health threats under exigent conditions. They thank both the Syria Office and the Eastern Mediterranean Regional Office of the WHO for its correspondence and collaboration on cholera concerns. The authors also thank the front-line practitioners—their colleagues from the Interim Directorates of Health across Syria, especially those in Eastern Ghouta and other besieged areas who continue to work in extremely dangerous conditions to provide healthcare to the 11.1 million people living in territory outside government control, in line with the humanitarian principles of neutrality, impartiality and humanity and in accordance with the Geneva Conventions governing the conduct of war. Most important, the authors acknowledge their colleagues who have been killed during the past 5 years in the line of humanitarian duty, risking their lives to protect children from death or disability due to vaccine-preventable diseases, to treat the sick and the wounded, and to fulfil the right of all civilians in need to receive humanitarian assistance as enshrined in international humanitarian law. Two such staff members include laboratory technicians, Alaa Nahhas and Zakaria Hijazy, killed on 26 October 2015.
Footnotes
Handling editor: Seye Abimbola
Twitter: Follow Annie Sparrow at @annie_sparrow and Paul Langton at @WAProfLang
Contributors: All authors contributed to the design of the work. Data acquisition was primarily performed by KA, BT and NT. All authors contributed to the analysis and interpretation. The report was drafted by AS, NT and PL. All authors revised the final article and agree to be accountable for the content. They also approve the version published.
Competing interests: The Icahn School of Medicine at Mount Sinai supports costs associated with field research by AS. Disclosure forms by the authors are provided to BMJ Global Health. AS is a member of the BMJ Global Health editorial board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.OCHA: Syrian Arab Republic. http://www.unocha.org/syria (accessed Mar 2016).
- 2.Needs and Population Monitoring Report POPULATION BASELINE ROUND IV OCTOBER 2015. https://www.humanitarianresponse.info/sites/www.humanitarianresponse.info/files/assessments/npm_report_round_iv_october_2015_1.pdf (accessed 19 Dec 2015).
- 3.IWPR. Cholera Epidemic Fears Rise. SYR Issue 72. 21 Aug 09. https://iwpr.net/global-voices/cholera-epidemic-fears-rise (accessed Mar 2016).
- 4.Epidemic preparedness and response plan for cholera in Syria 30 November 2015. http://www.emro.who.int/images/stories/syria/Epidemic_preparedness_cholera_plan_of_Syria.1_November_2015.pdf?ua=1 (accessed Mar 2016).
- 5.Tajaldin B, Almilaji K, Langton P et al. . Defining polio: closing the gap in global surveillance. Ann Glob Health 2015;81:386–95. 10.1016/j.aogh.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 6.The Syria Institute: Siege Watch First Quarterly Report on Besieged Areas in Syria—February 2016. http://siegewatch.org/wp-content/uploads/2015/10/PAX-RAPPORT-SIEGE-WATCH-FINAL-SINGLE-PAGES-DEF.pdf (accessed Mar 2016)
- 7.Shah S. The Next Cholera Epidemic. Foreign Affairs. https://www.foreignaffairs.com/articles/syria/2015-11-10/next-cholera-epidemic (accessed 11 Oct 2015).
- 8.Suspected case of Cholera in N Syria Assistance Coordination Unit. http://www.acu-sy.org/en/suspected-case-of-cholera-in-n-syria/ (accessed Oct Mar 2016).
- 9.Needs and Population Monitoring (NPM)—Mobility Dynamic-Report-3 (Dec-2015). https://www.humanitarianresponse.info/en/operations/whole-of-syria/assessment/needs-and-population-monitoring-npm-mobility-dynamic-report-3 (accessed Mar 2016).
- 10.Hepatitis A cases in Syria. Weekly Epidemiological Monitor Volume 8 Issue 14 & 15 12 April 2015 Published by World Health Organization (WHO) Eastern Mediterranean Regional Office (EMRO) http://applications.emro.who.int/dsaf/epi/2015/Epi_Monitor_2015_8_14-15.pdf?ua=1 (accessed Mar 2016).
- 11. EWARS Weekly Bulletin Week No 21. (17–23 May 2015). http://www.emro.who.int/images/stories/syria/documents/EWARS_Week_21_Bulletin_2015.pdf?ua=1.
- 12. WHO Syrian Arab Republic Annual Report 2014 http://applications.emro.who.int/dsaf/EMROPUB_2015_EN_1837.pdf?ua=1.
- 13. Acute Jaundice Syndrome in Rural Damascus week 11 2015 http://www.acu-sy.org/en/wp-content/uploads/2015/06/Ext-Week11-Acute-Jaundice-Syndrome-in-Rural-Damascus_EN.pdf.
- 14.EWARS Weekly Bulletin Week No 44. October 2015. http://www.emro.who.int/images/stories/syria/documents/EWARS_Week_-44-Bulletin_2015__-_.pdf?ua=1 (accessed Mar 2016).
- 15. Water-borne Disease Assessment in Idleb week 26 2015 Brief Epidemiological review of Waterborne Diseases in Idleb Governorate between June 2014 and June 2015. http://www.acu-sy.org/en/wp-content/uploads/2015/07/Ext13-Week26-WBD_Assessment_Idleb.pdf.
- 16.Sparrow A. Syria the Other Threat New York Review of Books Blog August 12, 2014. http://www.nybooks.com/daily/2014/08/12/syria-threat-polio/ (accessed Oct 2015).
- 17.An overview of WASH, Water, Sanitation and Hygiene. http://www.acu-sy.org/en/wash-water-sanitation-hygiene/ (accessed Nov 2015).
- 18.Bled dry: How war in the Middle East is bringing the region's water supplies to breaking point. An ICRC report. http://www.icrcproject.org/app/water-in-middle-east/PDF/full_report-water-middle-east-icrc.pdf (accessed Nov 2015).
- 19.Eastern Aleppo Household Assessment: Water Security August 2015 (REACH). http://www.reachresourcecentre.info/system/files/resource-documents/reach_syr_profile_easternaleppo_watersecurity_aug2015.pdf (accessed Mar 2016).
- 20.Sparrow A. Syria: Death from Assad's Chlorine. New York Review of Books. May 7 2015 http://www.nybooks.com/articles/2015/05/07/syria-death-assads-chlorine/ (accessed Oct 2015).
- 21.Report of the Secretary-General on the implementation of Security Council resolutions 2139 (2014), 2165 (2014) and 2191 (2014) December 15 2015. http://www.un.org/en/ga/search/view_doc.asp?symbol=S/2015/962 (accessed Dec 2015).
- 22.Triebert C. Syria's Bombed Water Infrastructure: an OSINT Inquiry December 11 2015 https://www.bellingcat.com/news/mena/2015/12/11/syrias-bombed-water-infrastructure/
- 23. A field manual—communicable disease control in emergencies. World Health Organization 2005. http://apps.who.int/iris/bitstream/10665/96340/1/9241546166_eng.pdf.
- 24. Assistance Coordination Unit Annual Report 2014. http://www.acu-sy.org/en/wp-content/uploads/2015/12/Annual-Report-2014-English.pdf.
- 25.EWARN: The Early Warning Alert and Response Network. http://www.acu-sy.org/en/early-warning-alert-and-response-network/ (accessed Nov 2015).
- 26. Acute Flaccid Paralysis Surveillance 2015–2016. http://www.acu-sy.org/en/afp-reports/
- 27. WASH-Related Diseases Reports 2015–2016 (ACU-EWARN) http://www.acu-sy.org/en/wash-reports/
- 28. November Quarterly DLOs Training Extension- Syria EWARN- Epi week 47- 2015. http://www.acu-sy.org/en/wp-content/uploads/2015/12/Ext-47-November-Quarterly-DLOS-training-EN.pdf.
- 29.Syrian Arab Republic. EWARS: The Early Warning System. http://www.emro.who.int/syr/publications-other/ewars-weekly-bulletin.html (accessed Nov 2015).
- 30.Syrian Epidemiological Bulletin Quarterly bulletin published by MoH in Syria Vol 7 No. 2 2014 http://www.moh.gov.sy/pages/EpidemicBulletin/201304/indexe.html (accessed Nov 2015).
- 31.Muhjazi G, Bashour H, Abourshaid N et al. . An early warning and response system for Syria. Lancet 2013;382:2066 10.1016/S0140-6736(13)62691-4 [DOI] [PubMed] [Google Scholar]
- 32.EWARS Weekly Bulletin Week No 26. June 2015. http://www.emro.who.int/images/stories/syria/documents/EWARS_Week-26-Bulletin_2015.pdf?ua=1 (accessed Mar 2016)
- 33.EWARS Weekly Bulletin Week No 45. November 2015. http://www.emro.who.int/images/stories/syria/documents/EWARS_Week_-45-Bulletin_2015__-_1_-_Copy.pdf?ua=1 (accessed Mar 2016).
- 34.Outbreak Surveillance and Response in Humanitarian Emergencies. WHO guidelines for EWARN implementation. Geneva: World Health Organization, 2012. http://www.who.int/diseasecontrol_emergencies/publications/who_hse_epr_dce_2012.1/en/ [Google Scholar]
- 35.Russian military intervention in the Syrian War. https://en.wikipedia.org/wiki/Russian_military_intervention_in_the_Syrian_Civil_War (accessed Mar 2016).
- 36.Water and Violence: Crisis of Survival in the Middle East. Strategic Foresight Group 2014. http://www.strategicforesight.com/publication_pdf/63948150123-web.pdf (accessed Mar 2016)
- 37.EWARS Weekly Bulletin Week No 38. September 2015. http://www.emro.who.int/images/stories/syria/documents/EWARS_Week_-38-Bulletin_2015__-.pdf?ua=1 (accessed Mar 2016).
- 38.Second Battle of Idlib. https://en.wikipedia.org/wiki/Second_Battle_of_Idlib (accessed Mar 2016).
- 39.WHO Emergencies preparedness response—Cholera—Iraq. http://www.who.int/csr/don/26-november-2015-iraq-cholera/en/ (accessed Mar 2016).
- 40.Shah S. Pandemic: tracking contagions from cholera to Ebola and beyond. New York: Sarah Crichton Books, 2016:169–72. [Google Scholar]
- 41.Weekly epidemiological record. World Health Organization 2 October 2015, 90th year / No 40, 2015,90, 517–544. http://www.who.int/wer/2015/wer9040.pdf (accessed 30 Dec 2015).
- 42.Ali M, Nelson AR, Lopez AL et al. . Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis 2016;9:e0003832 10.1371/journal.pntd.0003832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cholera: mechanism for control and prevention. Sixty-fourth World Health Assembly WHA 64.15 Agenda item 13.9 24 May 2011. http://www.who.int/cholera/technical/Resolution_CholeraA64_R15-en.pdf (accessed Nov 2015).
- 44. Advisory Group On Reform Of WHO's Work In Outbreaks and Emergencies First Report November 15th 2015. http://www.who.int/about/who_reform/emergency-capacities/first-report-advisory-group.pdf?ua=1.
- 45.Moon S, Sridhar D, Pate MA et al. . Will Ebola change the game? Ten essential reforms before the next pandemic. The report of the Harvard-LSHTM Independent Panel on the Global Response to Ebola. Lancet 2015;386:2204–21. 10.1016/S0140-6736(15)00946-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. doi: 10.1136/bmj.i469. Checchi F, Waldman RJ, Roberts LF, et al. World Health Organization and emergency health: if not now, when? BMJ 2016;352:i469. [DOI] [PubMed] [Google Scholar]