Abstract
Background
Vesicovaginal fistulas (VVF) are the most commonly acquired fistulas of the urinary tract, but we lack a standardized algorithm for their management. Surgery is the most commonly preferred approach to treat women with primary VVF following benign gynaecologic surgery.
Objective
To carry out a systematic review and meta-analysis on the effectiveness of operative techniques or conservative treatment for patients with postsurgical VVF. Our secondary objective was to define the surgical time and determine the types of study designs.
Methods
PubMed, Old Medline, Embase and Cochrane Central Register of Controlled Trials were used as data sources. This systematic review was modelled on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement, including a registration number (CRD42012002097).
Results
We reviewed 282 full text articles to identify 124 studies for inclusion. In all, 1379/1430 (96.4%) patients were treated surgically. Overall, the transvaginal approach was performed in the majority of patients (39%), followed by a transabdominal/transvesical route (36%), a laparoscopic/robotic approach (15%) and a combined transabdominal-transvaginal approach in 3% of cases. Success rate of conservative treatment was 92.86% (95%CI: 79.54–99.89), 97.98% in surgical cases (95% CI: 96.13–99.29) and 91.63% (95% CI: 87.68–97.03) in patients with prolonged catheter drainage followed by surgery. 79/124 studies (63.7%) provided information for the length of follow-up, but showed a poor reporting standard regarding prognosis. Complications were studied only selectively. Due to the inconsistency of these data it was impossible to analyse them collectively.
Conclusions
Although the literature is imprecise and inconsistent, existing studies indicate that operation, mainly through a transvaginal approach, is the most commonly preferred treatment strategy in females with postsurgical VVF. Our data showed no clear odds-on favorite regarding disease management as well as surgical approach and current evidence on the surgical management of VVF does not allow any accurate estimation of success and complication rates. Standardisation of the terminology is required so that VVF can be managed with a proper surgical treatment algorithm based on characteristics of the fistula.
Introduction
Vesicovaginal fistula (VVF) is an abnormal fistulous tract extending between the bladder and the vagina that allows the continuous involuntary discharge of urine into the vaginal vault. In addition to the medical sequelae from these fistulas, they affect physical, mental, social and sexual life of the patients [1]. In developing countries, the predominant cause of VVF is prolonged obstructed labour (97%) [1]. Conversely, in industrial countries iatrogenic injury to the urinary tract is the most common cause of VVF and the majority are consequences of benign gynaecological surgery [2]. It is estimated that 0.8 per 1000 of all hysterectomies are complicated by the development of a VVF [3]. Other causes in the developed world include malignant disease and pelvic irradiation [4]. In contrast to obstetric and irradiation fistulas, the typical postsurgical (post hysterectomy) fistula is the result of more direct and localised trauma to healthy tissue [5].
Although vesicovaginal fistulas (VVF) are the most commonly acquired fistulas of the urinary tract, we lack a standardized algorithm for their management [6]. Conservative management including prolonged bladder drainage, glue/fibrin injections, fulguration and so on is a reasonable option in cases with small, clean and non-malignant VVF [3,7]. Beside that, an operation is by far the most commonly preferred approach for affected women and the success rate varies between 75–95% with various different techniques in literature [3,8–13]. Multiple different surgical routes like Latzko repair, open transabdominal, transvaginal, laparoscopic, robotic, transurethral endoscopic with or without tissue interposition have been described [8,9,13], but no studies have compared surgical with conservative procedures and their outcomes in patients with VVFs following benign gynaecologic surgery. Furthermore, there is no general consensus regarding surgical time for a successful repair [7]. However, the evidence concerning treatment outcome with well-documented success and complication rates as well as the optimal surgical timing is lacking. To our knowledge, this is the first systematic review and meta-analysis investigating this topic. Primary outcome of interest was to review and summarize the current body of literature regarding effectiveness of disease management in patients with VVF following benign gynaecologic surgery. Our secondary objective was to define the most commonly reported time point for treatment and determine the types of study designs.
Materials and methods
This study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [14]. Before data extraction, the protocol of this review was registered with the PROSPERO International Prospective Register of Systematic Reviews (CRD42012002097) following the PRISMA guidelines for protocols (PRISM-P) [15]. The following PICO question was defined and is shown in Fig 1.
Fig 1. PICO question.
Literature search
Literature search included 4 data sources using the retrieval systems DIMDI Classic search or OvidSp. In detail, we performed a computerised English-language Medline, Pub med, Cochrane Central Register of Controlled trials (CENTRAL) and Embase literature search using the MeSH terms *vesicovag* AND *fistul* AND (*management* OR *iatrogenic* OR *surgery* OR repair*), respectively. Our search ranged from 1947 to March 2016.
Study selection
The limits for literature search were adult human females. Studies were included if they reported on a) vesicovaginal fistula b) which occurred after a benign gynaecologic surgery c) with clearly described conservative or surgical management. In screening process we excluded studies focusing on other types of urogenital fistulas (UGF), congenital fistulas or fistulas due to malignancy/irradiation or foreign bodies. Studies dealing with obstetrical VVF or trials, which did not clearly separate outcome parameters regarding fistula cause, were also excluded. Congress proceedings of international society meetings, textbooks, and review articles did not meet the inclusion criteria. Reports including men, neonates or adolescents despite the search limits were not included. Non-English articles with English abstracts were included if they provided information not found in English-language literature.
Data extraction and study characteristics
Two investigators (BBA and KB) independently reviewed random titles and abstracts to establish reliable, reproducible inclusion criteria. All pertinent references from the manuscripts were obtained and reviewed. General characteristics were recorded from each study. Two authors (BBA and KB) independently abstracted study design, number of included patients, type or size of the VVF, different types of treatment (surgical/conservative), route and type of surgical treatment, cause of fistula and time point of surgical repair. The following outcome parameters were measured: time between fistula occurrence and repair (= surgical time), complete resolution of symptoms, success rate and treatment complications: postoperative leakage, de-novo stress incontinence, de novo urgency, urinary tract infection, number of attempts/repair, new-onset of pain/dyspareunia, recurrent VVF immediately (failure) or at any time postoperatively and long-term consequences on pelvic health including sexual function immediately or at any time after treatment. Terminology for success was inconsistent among included studies. We used terminology for success when success was either defined as “anatomical cure–fistula closed, healed or cured” or “absence of urinary loss, resolution of symptoms”. A total of 12 publications showed disagreement between the two reviewers. This was resolved by discussion with a third person (EH or HK). The findings of all relevant studies were abstracted, categorized and summarized by study design and outcomes measured. Furthermore, two of the authors (BBA and KB) independently rated the quality of the studies, using criteria from US Preventive Services Task Force and the NHS Centre for Reviews and Dissemination [16]. Studies received a poor rating if they were case reports, case series without adequate control group or comparative studies where the groups were not comparable.
Risk of bias (RoB) assessment
Risk of bias between included studies was independently assessed and evaluated by two of the authors (BBA and KB). Due to the types of study design of included studies the Newcastle Ottowa Scale for risk of bias assessment for comparative studies was used (Table 1) [17]. This considers 3 criteria (selection of study groups, comparability of groups and ascertainment of outcome of interest) for quality assessment. Discrepancy between the review authors over the risk of bias was resolved by discussion, with involvement of a third author where necessary.
Table 1. Quality assessment (Newcastle Ottowa Scale) for comparative studies.
| Author, year | Selection | Comparability | Outcome/Exposure |
|---|---|---|---|
| Gupta N, 2010 | *** | * | *** |
| Ou CS, 2004 | *** | ** | *** |
| Pshak T, 2013 | ** | * | *** |
| Rajamaheswari N, 2012 | *** | ** | *** |
| Miklos JR, 2015 | ** | * | ** |
A study can be awarded a maximum of one star for each numbered item within the selection and outcome categories. A maximum of two stars can be given for comparability.
*: poor quality
**: moderate quality
***: high quality
Synthesis of results
The meta-analysis was conducted on individual patient level using random-effect logistic regression models to calculate the probability of success for every type of therapy (conservative, surgical, combined) and every route and type of surgical treatment. 95% confidence intervals for the estimated proportion of successful treatments were calculated based on profile likelihood. To show the amount of heterogeneity the between trial variance τ² is presented for every model. Random- effects logistic regression models were used to manage study heterogeneity. Furthermore, calculation of the meta-analysis was also extended to random-effect logistic regression models. No odds ratios for the comparison between the different types of therapy were calculated as only 4 out of the 124 trials had a comparative study design while 120 studies reported uniform treatment for all documented patients. Therefore the differences in the outcome might be mainly influenced by the heterogeneity of the study populations. All statistical calculations were performed using the R-project for statistical computing (Version R-3.2.5) [18].
Results
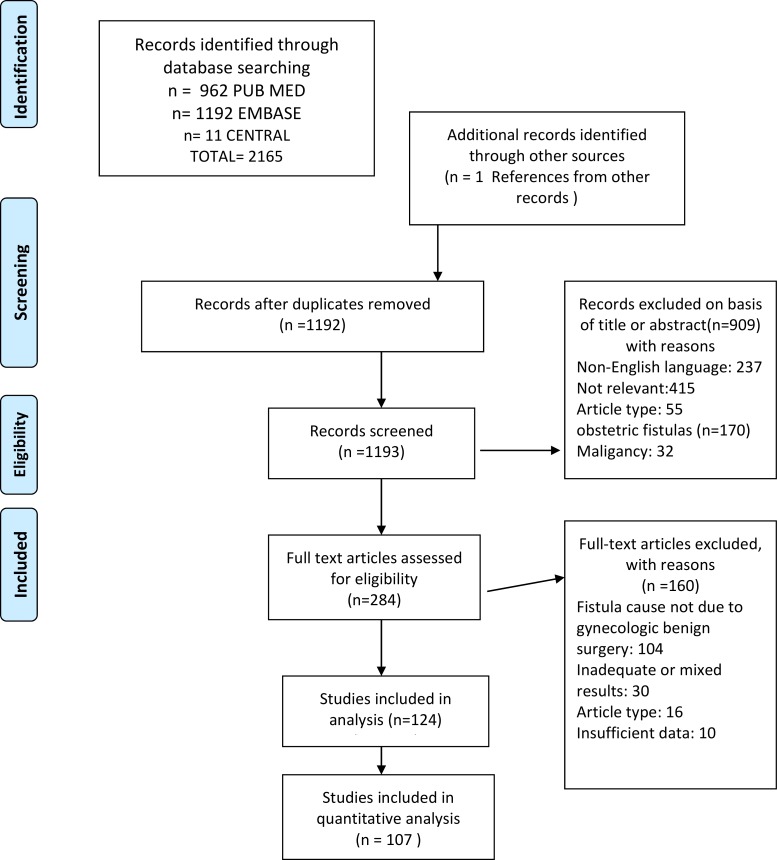
We identified 2165 citations, reviewed 282 full text articles, and identified 124 studies for inclusion [1,4,8,10,13,19–137]. We excluded 1018 studies because they did not meet the inclusion criteria. The results of the search and screening procedure are presented as a PRISMA Flow Chart in Fig 2. The final analysis included 23 case reports, 95 retrospective case series, 5 comparative studies and 1 uncontrolled prospective study involving 1430 patients in all. There were no randomized controlled trials and no case-control studies. Case series contained between 2 and 110 patients. Detailed information of each included study (author, year, type of procedure and success rate) is summarized in Table 2.
Fig 2. PRISMA Flow Chart.
Table 2. Included studies, type of procedure/approach and reported success rates.
| Author, year | Type of procedure | sucess rate(%) | |
|---|---|---|---|
| Ansquer et al, 200618 | transvaginal | 100% | |
| Abdel-Karim et al, 201119 | Laparoscopic | 100% | |
| Ayed et al, 200620 | combined vaginal and suprapubic | 41% | |
| Aycinena et al, 197721 | conservative (curretage) | 100% | |
| Agrawal et al, 201522 | Robotic | 100% | |
| Blandy et al, 199123 | Transabdominal | 100% | |
| Badenoch et al, 198724 | Transabdominal | 100% | |
| Baumrucker et al, 197125 | rubber ball | not stated | |
| Bramhall et al., 195026 | Transabdominal | not stated | |
| Bajory et al, 201127 | Transvaginal | 100% | |
| Brandt et al, 199828 | Transvesical | 96% | |
| Bragayrac et al, 201429 | Robotic | not stated | |
| Clark et al, 197530 | combined vaginal and transvesical | 100% | |
| Chibber et al, 200531 | Laparoscopic | 100% | |
| Chien W-H et al, 200632 | Transvaginal | 100% | |
| Chapron et al, 199533 | Transabdominal | 100% | |
| Cruikshank et al, 198734 | Transvaginal | 82% | |
| Chu Lei et al, 201535 | Laparoscopic | 100% | |
| Dogra Prem et al, 201136 | YAG laser weldging | 88% | |
| Dorsey et al, 196037 | Transabdominal | 100% | |
| Daley et al, 200638 | conservative (fibrin sealant) | 100% | |
| Dos Santos et al, 200839 | Laparoscopic | not stated | |
| Dorairajan et al, 200840 | Transvaginal | not stated | |
| Dalela et al, 200641 | Transabdominal | 100% | |
| Ezzat et al, 2009 42 | combined abdominal and vaginal | 88% | |
| Falk et al, 1957 43 | conservative (electrocoagulation) | 100% | |
| Fourie et al, 198344 | Transabdominal | 88% | |
| Flynn et al, 200445 | Transvaginal | 100% | |
| Fearl et al, 196846 | transvesical or transvaginal | 90% | |
| Fang et al, 201547 | transvaginal (with foley catheter) | 100% | |
| Fleischmann et al, 198848 | Transabdominal | 100% | |
| Gupta et al, 201049 | transabdominal versus robotic | 100% | |
| Gözen et al, 200950 | Laparoscopic | 100% | |
| Goodwin et al, 198051 | Transvaginal | 100% | |
| Grange et al, 201452 | combined vaginal and vesicoscopic | 100% | |
| Harrow et al, 196853 | Transvesical | not stated | |
| Hong HM et al, 201054 | pointed electrocoagulation | 100% | |
| Hessami et al, 200755 | Transadominal | 100% | |
| Hellenthal et al, 200756 | Transabdominal | 95% | |
| Hemal et al, 200857 | Robotic | 100% | |
| Henriksson et al, 198258 | combined vaginal and suprapubic | 78% | |
| Hsieh CH et al, 200859 | Transvaginal | 1005% | |
| Immergut et al, 195060 | Transvesical | 67% | |
| Iselin et al, 199813 | Transvaginal | 100% | |
| James et al, 201361 | conservative (bladder drainage) | 1005% | |
| Javali et al, 201462 | Laparoscopic | 100% | |
| Kostakopoulos et al, 199863 | transvaginal and transabdomnal | 100% | |
| Krissi et al, 200164 | fistulectomy & closure | not stated | |
| Keettel et al, 197865 | transvaginal and combined | 94% | |
| Kristensen et al, 66 | Transabdominal | not stated | |
| Ledniowska et al, 201267 | transvaginal with modifications | not stated | |
| Lazarou et al, 200668 | Transvaginal | 100% | |
| Llueca et al, 201569 | Laparoscopic | 100% | |
| Landes et al, 197970 | Transvesical | 100% | |
| Dutto et al, 201371 | Robotic | 1005 | |
| Liao et al, 20124 | Transvaginal | 83,30% | |
| Morgan et al, 195072 | Transabdominal | not stated | |
| DasMahapatra et al, 200773 | Laparoscopic | 100% | |
| Modi et al, 200674 | Laparoscopic | 100% | |
| Muto et al, 200575 | conservative (glue) | 66.6% | |
| El-Lateef et al, 200376 | Retropubic | 100% | |
| McKay et al, 200177 | Cystorrhaphy | not stated | |
| Milicic et al, 200178 | Transvaginal | 95.2% | |
| McKay et al, 199779 | Cystorrhaphy | 100% | |
| Miklos et al, 199980 | Transvaginal | not stated | |
| Malin et al, 196781 | gold leaf | not stated | |
| Moriel et al, 199382 | Transvesical | 100% | |
| Mohseni et al, 201283 | Transabdominal | 86% | |
| Macalpine et al, 194084 | Transvesical | 100% | |
| Malmström et al, 195585 | Conservative | 100% | |
| Mallikarjuna et al, 201586 | laparoscopic (AINU) | 100% | |
| Miklos et al, 201587 | Laparoscopic | 97%(primary)100%(recurrent) | |
| Nagraj et al, 200788 | Laparoscopic | not stated | |
| Nabi et al, 200189 | Laparoscopic | 100% | |
| Nesrallah et al, 199990 | Transabdominal | 100% | |
| Nezhat et al, 199491 | Laparoscopic | 100% | |
| Nerli et al, 201092 | Transvesicoscopic | 100% | |
| Otsuko et al, 200893 | Laparoscopic | not stated | |
| Ou et al, 200410 | combined /vag./abd./laparosc.) | 83%/100%/100% | |
| Ostad et al, 199894 | Transabdominal | 100% | |
| Phipps et al, 199695 | Laparoscopic | 100% | |
| Persky et al, 197996 | Transvesical | 83% | |
| Pietersma et al, 201497 | Robotic | 100% | |
| Persky et al, 197398 | Transabdominal | 100% | |
| Pontes et al, 197499 | Transabdominal | 100% | |
| Peikoff et al, 1956100 | Transabdominal | 100% | |
| Phsak et al, 2013101 | Transvaginal | not stated | |
| Rizvi et al, 2010102 | Laparoscopic | 100% | |
| Reynolds et al, 2008103 | Transabdominal | 100% | |
| Radopoulos et al, 2008104 | Transvaginal | 100% | |
| Raz et al, 19938 | Transvaginal | 82% | |
| Roslan et al, 2012105 | LESS | 100% | |
| Razi et al, 2015106 | combined(transvag./transabd.) | 100% | |
| Rader et al, 1975107 | Transvaginal | 100% | |
| Rajamaheswari et al, 2012108 | transvag. versus transabd. | 95% vs.100% | |
| Szendi et al, 1959109 | Transvaginal | 100% | |
| Schneidermann et al, 1958110 | Suprapubic | 100% | |
| Shah et al, 2010111 | conservative (fulguration) | not stated | |
| Roen et al, 1960112 | combined (transvag.,transvesic.) | not stated | |
| Robles et al, 2009113 | Transvaginal | not stated | |
| Schimpf et al, 2007114 | Robotic | 100% | |
| Sears et al, 2007115 | Robotic | 100% | |
| Sundaram et al, 2006116 | Robotic | 100% | |
| Starkman et al, 2007117 | Transvaginal | 100% | |
| Singh RB et al, 2005118 | Transabdominal | 100% | |
| Soong et al, 1997119 | Transabdominal | 67% | |
| Sharma et al, 20141 | Laparoscopic | 100% | |
| Singh V et al, 2013120 | Laparoscopic | 100% | |
| Shirvan et al, 2013121 | conservative (plasma/glue) | 100% | |
| Simforoosh et al, 2012122 | Laparoscopic | 75% | |
| Sharifiaghdas et al, 2012123 | Transabdominal | 90% | |
| Singh et al, 2012124 | Transabdominal | 89% | |
| Tancer et al, 1992125 | Transvaginal | 89% | |
| Toledo et al, 2013126 | Observation | 100% | |
| Tsivian et al, 2006127 | Transvaginal | 100% | |
| Tiong et al, 2007128 | Laparoscopic | 100% | |
| Theobald et al, 1998129 | Laparoscopic | 100% | |
| Taylor et al, 19481230 | Transvesical | 100% | |
| Udea et al, 1977131 | Suprapubic | 100% | |
| Wong et al, 2006132 | Laparoscopic | 100% | |
| Wein et al, 1980133 | Transabdominal | 91% | |
| Xu et al, 2005134 | Transabdominal | 100% | |
| Zhang et al, 2013135 | Laparoscopic | 100% | |
| Zumrutbas et al, 2014136 | Cystoscopy | 100% | |
| Transvag.: transvaginal | transabd.: transabdominal | transvesic.: transvesical | |
Study characteristics
Fistula type was documented only in 58/124 (47%) studies. Of these, the majority of trials 35/58 (60%) dealed with simple fistulas, 21/58 (36%) with complex VVF and in a small percentage of studies (4%) complicated VVF were investigated. The majority of studies (66/124; 53%) did not comment on fistula type. Mean fistula size could not be calculated due to heterogeneity and insufficiency of data documentation. The majority of VVF occurred after a transabdominal hysterectomy (n = 943/1430; 66%), followed by vaginal hysterectomy (n = 126/1430; 9%), laparoscopic hysterectomy (n = 38/1430; 3%) and other benign gynaecologic operations (n = 72/1430; 5%). The remaining studies (17%) did not mention the type of hysterectomy causing the fistula. 46/124 (37%) studies included only patients who underwent a primary fistula repair (n = 221), 16/124 (13%) studies investigated patients who had previous attempts of fistula repair (n = 54) and 41/124 (33%) trials described a mixed collective of cases (n = 979). Remaining 21 studies (17%) did not give any information. Number of attempts varied between 1 and 3 repairs in average.
Conservative treatment: Results of individual studies
10 studies described non-surgical treatment strategies as sole treatment option. These included transvaginal injection of fibrin sealant in 1 case, Yag Laser welding in 8 patients, cystoscopic electrocoagulation/fulguration/catheter method in 11 patients, endovaginal application of cyanoacrylic glue in 3 cases, platelet rich plasma/rich fibrin glue application in 6 women, curettage of fistula tract in 3 cases and ball technique with rubber/metal ball in 18 females. Success ranged between 67%-100% and the majority consisted of small VVF (<1 cm) [22,26,37,39,44,62,76,86,112,122].
239/1430 VVF (16%) were initially managed conservatively with prolonged catheter drainage (range: 2–12 weeks). Only 19/239 (8%) VVFs resolved with catheter drainage and the remaining 220/239 (92%) VVFs underwent surgical repair.
Surgical treatment
The majority of patients were treated surgically. In all, 1379 patients were managed surgically and 97.98% (95%-CI: 96.13–99.29) were cured. The most commonly reported surgical approach was the transvaginal route (n = 534/1379; 39%), followed by a transabdominal/transvesical approach (n = 493/1379; 36%), a laparoscopic/robotic route (n = 207/1379; 15%) and a combined transabdominal-transvaginal approach in 45/1379 (3%) cases. Additionally, further various surgical techniques like transvaginal transurethral pointed electrocoagulation, transurethral suture cystorraphy, suprapubic cystotomy with gold leaf and so on were reported in 41/1379 (3%) cases. In 59/1379 (4%) VVFs the surgical route was not documented. Interposition grafts like Martius flap, Gracilis muscle, omental, peritoneal, labial fat flap or bladder mucosa autograft were used in the majority of studies (66 studies including 708 cases).
Success after treatment
107/124 (86%) studies documented a success rate after treatment, describing 87 patients being completely symptom-free, 754 being completely dry and in 406 cases fistula healed completely or was cured.
Results of each meta-analysis with logistic regression model
Only studies which consistently evaluated treatment success were used for the meta-analysis. Success rate of conservative treatment was 92.86% (95%CI: 79.54–99.89), 97.98% in surgical cases (95% CI: 96.13–99.29) and 91.63% (95% CI: 87.68–97.03) in patients with prolonged catheter drainage followed by surgery. Success rates regarding surgical approaches were as follows: transabdominal/transvescial route 97.05% (95% CI: 94.55–99.18), transvaginal route 93.82% (95% CI: 89.96–97.49), laparoscopic/robotic approach 98.87% (95% CI: 96.85–99.99) and combined transabdominal/transvaginal route 90.70% (95% CI: 64.63–99.87). Use of interposition flap showed a success rate of 97.63% (95% CI: 95.31–99.22), without interposition flap reported success rate was 97.62% (95% CI: 93.63–99.91).
Reported frequency of success rates are summarised in Tables 3–8.
Table 3. Treatment modalities.
| Treatment | conservativ | surgcial | Catheter and surgery |
|---|---|---|---|
| Number of studies | 9 81,8% of 11 | 73 89,0% of 82 | 25 80,6% of 31 |
| Number of patients | 28 54,9% of 51 | 983 90,3% of 1088 | 239 82,1% of 291 |
Table 8. Frequency of success.
| Estimated proportion of successes % | 95%-CI of proportion of successes | Between trial variance τ² | |
|---|---|---|---|
| With Flap | 97,63 | 95,31–99,22 | 1,594 |
| Without Flap | 97,62 | 93,63–99,91 | 2,034 |
Table 4. Frequency of success.
| Estimated proportion of successes % | 95%-CI of proportion of successes | Between trial variance τ² | |
|---|---|---|---|
| Conservative | 92,86 | 79,54–99,89 | 0 |
| Surgical | 97,98 | 96,13–99,29 | 2,05 |
| Catheter+surgery | 91,63 | 87,68–97,03 | 0 |
Table 5. Surgcial approaches.
| Surgical approach | Abdominal | transvaginal | Laparosc.or robotic | Others | combined | n.s. | |
|---|---|---|---|---|---|---|---|
| Number of patients | 493 | 534 | 207 | 41 | 45 | 59 | |
Table 6. Frequency of success.
| Estimated proportion of successes % | 95%-CI of proportion of successes | Between trial variance τ² | |
|---|---|---|---|
| Abdominal/transvescial | 97,05 | 94,55–99,18 | 0,49 |
| Transvaginal | 93,82 | 89,96–97,49 | 0,19 |
| Laparoscopic/robotic | 98,87 | 96,85–99,99 | 0 |
| Others | 100 | ||
| Combined | 90,70 | 64,63–99,87 | 2,65 |
n.s: not stated
Laparoscp.: laparoscopic
Table 7. Use of interposition flap.
| Interposition Flap | Without | with |
|---|---|---|
| Number of studies | 21 72,41% of 29 | 62 93,94% of 66 |
| Number of patients | 217 64,98% of 334 | 695 98,16% of 708 |
Intra- and postoperative surgical outcome
Successful intraoperative or postoperative outcome was mentioned in detail in 78/124 (63%) studies. The majority of these studies defined a successful outcome as an uneventful intra- or postoperative course and no immediate complications detected. 14 studies mentioned a complicated postoperative outcome and in 24 patients this was described in detail: ileus (n = 5), postoperative fever (n = 6), intraoperative bleeding (n = 2), grad II hydroureter (n = 1), clostridium difficile atelectasis (n = 1), wound infection (n = 2), bowel injuries (n = 2), compartment syndrome (n = 1), pelvic abscess (n = 1), and occurrence of ureterovaginal (n = 1) and vesicocolonic fistula (n = 2).
Length of follow-up and complication rates
79/124 (64%) studies provided information for the length of follow-up. The remaining 45 studies did not mention any length of follow-up. The mean available follow-up time was 19.7 months. Complications were studied only selectively. Total number of studies mentioning complication outcome is shown in Table 9. Due to the inconsistency of these data it was impossible to analyse them collectively.
Table 9. Number of studies mentioning complication outcome.
| Complications | Mentioned in Studies | Patients in these studies | Observed absolute frequency | Observed relative frequency |
|---|---|---|---|---|
| Failure/Recurrence | 60 | 905 | 59 | 6,52% |
| UTI | 15 | 229 | 12 | 5,24% |
| De novo SUI | 26 | 247 | 5 | 2,02% |
| De novo pain | 5 | 72 | 1 | 1,39% |
| De novo urgency | 32 | 280 | 10 | 3,57% |
Long-term consequences and sexual function after treatment
None of the included studies documented any long-term consequences of pelvic health. Only 3 studies assessed sexual function after treatment [41,93,135]. Dorairajan et al. reported that 8/10 patients were sexual active without any signs of dyspareunia or pain [40], Nerli et al. reported that 2/4 cases were sexual active and all 3 women were sexual active in the study published by Xu et al. [93,135].
Surgical time: Time between fistula occurrence and repair
In 22/124 (18%) studies, including 241 patients, surgery was initiated < 12 weeks after fistula occurrence. 15/124 (12%) studies with 223 patients defined the time point of surgical repair after 12 weeks. No statistically significant difference regarding success rate could be detected between early and late repair (p>0.05). 11 (9%) studies (n = 147 cases) started surgical timing < 12 weeks as well as > 12 weeks. The majority of studies (64/124; 52%), including 531 cases did not give any comment on their surgical time and 12 studies (9%) did not document an adequate time range.
Discussion
Vesicovaginal fistulas are among the most distressing complications of obstetric and gynaecologic procedures, which can cause devasting medical, social, and psychogenic consequences [138]. The aetiology has changed, becoming more associated with hysterectomy. Despite numerous publications on this subject, the management of VVF remains a source of debate. The options of fundamental issues such as the preferred surgical approach and the optimal timing of surgery still vary widely [128].
Main findings
This systematic review and meta-analysis assessed the effectiveness of disease management in patients with postsurgical fistulas and investigated treatment outcome with success and complication rates as well as surgical timing and type of study designs. The scientific literature consists mainly of case reports and retrospective case series. Furthermore, this analysis contains only a minority of studies, which used conservative treatment options as sole fistula treatment, as the majority of patients were treated surgically (96.4%). The preferred surgical approach was a transvaginal route, followed by transabdominal/transvesical approach, laparoscopic/robotic approach and combined operation techniques with reported success rates of 93.82%, 97.05%, 98.87% and 90.70%, respectively.
Comparison with literature
Treatment of patients with VVF is currently controversial [139]. Although a trial of conservative management with prolonged bladder drainage might be tried, the spontaneous closure rate of VVF is low [51]. We found only 10 studies, which used conservative treatment as sole treatment strategy. Besides, our data confirmed that VVF resolves with prolonged catheter drainage only in a low percentage (8%). Some authors indicate that conservative treatment is only successful in smallest fistulas, and the majority of patients will require definitive surgical repair [3,44,140]. However, no studies exist comparing non surgical with surgical treatment strategies.
Although an operation is by far the most common recommendation for affected women, evidence concerning surgical treatment is lacking. Multiple different surgical techniques and approaches have been described in literature [8,9,13], but the choice mainly depends on location, severity and size of fistula [141]. Additionally, only few studies have compared the surgical procedures/approaches for VVF [10,50,102,109]. One study compared open and robotic surgical repair in patients with recurrent VVFs with no significant difference in outcome and complication rate [50]. Ou et al. evaluated three different surgical techniques (laparoscopic–open abdominal–transvaginal) in patients with primary fistula repair. Their data suggested that laparoscopic repair is feasible and results in lower morbidity than transabdominal and vaginal repair [10]. Phsak et al. compared the outcome between recurrent VVFs and primary VVFs without tissue interposition. The authors concluded that transvaginal repair of recurrent VVFs without tissue interposition is equally successful as in primary repairs [102]. Rajamaheswari et al. investigated the outcome between vaginal and transabdominal repair and reported comparable success rates between the two groups [109].
Surgical approach
The most important principle in repair is to provide tension-free, watertight closure, and the surgical route should be the one that provides the best possible chance of closure on the first attempt [142]. These principles can be achieved through a vaginal, abdominal or endoscopic approach. Although the choice of technique partly depends on the characteristics of the fistula, the surgical experience is also an important factor of successful outcome [138]. Although different surgical techniques have been described, a consensus for the ideal approach for surgical correction of VVF is still required [142].
Vaginal approach
In general, most gynaecologic surgeons prefer the vaginal approach, which has been associated with lower morbidity rates and with an equally good outcome [7,143]. The two most commonly reported vaginal repair techniques include Latzko technique and the layered closure [143]. This systematic review confirmed that vaginal fistula repair was used in the majority of cases with a reported success rate of 93.82%. Latzko operation was performed in 170 women and Tancer et al. published the largest investigation with 110 VVFs post hysterectomy. 107 patients were treated by partial colpocleises (Latzko repair) and 89% were cured at first attempt [126]. Although the included studies are inconsistent regarding characteristics of the fistula, we summarize that the vaginal approach for fistula repair is performed in the majority of female patients and therefore it is the surgical procedure with the highest level of experience in literature.
Abdominal approach
The abdominal route can be performed using a transvesical or an extravesical (bivalve technique) approach and is mainly indicated for loculated or complex fistulas [143]. We included 439 cases managed with an abdominal/transvesical approach with a reported success rate of 97.05%. Majority of these cases were treated with interposition graft. Due to the inconsistency of included trials and lack of fistula characteristics no recommendation can be made.
Laparoscopic and robotic-assisted approach
Minimally invasive laparoscopic surgery is increasingly being performed, including laparoscopic VVF repair [1,10,32,36]. In 2005, Chibber et al. described a laparoscopic approach to the O`Conor technique with reported advantages of decreased morbidity and a more rapid recovery [32]. One systematic review with 44 eligible studies compared the success rates between laparoscopic/robotic transvesical repair and extravesical laparoscopic repair techniques in patients with VVF. Due to their results, the authors summarized that extravesical VVF repair has similar cure rates compared to the traditional transvesical approach [144]. Most recent technology used in the treatment of VVF repair is the robotic-assisted approach and some authors reported excellent results with this operation technique [23,30,58,98]. Disadvantages include increased learning curve, time, costs and surgeons experience. We included 8 studies, which used a robotic-assisted approach. Success rates were excellent with 100% success, but number of included patients was small. Summarizing our data, due to the small number (n = 26 cases in all) and heterogeneity of studies, no clear statement and recommendation can be made regarding this operation technique and their success and complication rate in fistula repair.
Specified long-term outcome and complication rates
Postoperative complications are common and the most frequent postoperative complications reported in literature are de novo SUI, de novo urgency, leakage, de novo pain/dyspareunia, infection and failure [142,143]. Analysing our data, we could demonstrate that the majority of the included studies did not mention an adequate follow-up time and complications were described only selectively. We summarised 106/124 papers mentioning any complication, but from the remaining studies, which did not mention it we cannot assume that none occurred. Due to the inconsistency of these data it was impossible to analyse them collectively and no accurate prediction of complication rates can be made.
Surgical time
One of the main controversies in literature is the ideal timing for surgical intervention for postoperative VVF. Angioli et al. recommended waiting 2–4 months using continuous drainage of the bladder [143]. However, several other studies showed that, especially for small uninfected fistulae, early repair has better or at least similar success rates compared to delayed repair with additional advantage of reduced suffering and early commencement of normal life [24,25,143]. On the other hand, some reports indicate that timing of repair does not affect the outcome [145]. Our data demonstrated that 22 publications used an early repair, 15 studies started late surgical repair and 11 trials performed early as well as late repair. Due to this inconsistency, no serious recommendation can be done regarding ideal timing for surgical intervention.
Definition success rate and fistula classification
The reported cure rate of VVF varies between 75–95% with various different techniques in literature [3,8–13]. In accordance to literature, our findings revealed a success rate of 92.9% with conservative treatment, 97.98% in cases treated surgically and 91.63% in patients with prolonged catheter drainage followed by surgery. Summarising our data, no clear odds-on favorite regarding disease management as well as surgical approach could be identified and no technique was superior to any other. One major problem we faced was that success was defined in different ways, as many studies defined success as surgical closure of the fistula in place of function following surgery. In our opinion, successful surgical closure of the defect should be called ‘anatomical closure’ rather than ‘cure’, because many women suffer from on going pelvic organ, sexual and psychological dysfunction. Although this is of significant importance, only 3 studies [41,93,135] reported on sexual function after fistula treatment and the majority did not even mention this topic. Another problem that we faced when analysing the included studies was the lack of standardisation of terminology. The methodology of measuring the fistula as well as the used classification system was not clear in the majority of articles and none of the included studies stratified data by fistula type, primary repair versus previous attempts, fistula size or fistula location. Standardisation of the terminology is therefore required so that VVF can be properly managed [146]. Given the limitations of this analysis, future clinical research with a clearly defined VVF classification system, success definition better than anatomic result is needed to confirm our findings.
Quality and design of studies included
The scientific literature regarding surgical or conservative management of VVF following a benign gynaecologic surgery in female patients includes mainly case reports and retrospective case series and a variety of different surgical techniques. For this reason the majority of the included studies received a poor quality rating due to the study type. Furthermore, the reporting standard regarding surgical outcome, follow-up time and complication rate was poor. In addition to differences in reporting, an adequate documented follow-up time was not mentioned in the majority of cases, making it difficult to draw meaningful conclusions from these findings.
Strengths and limitations
One of the strengths of our study is the inclusion of study data on the effectiveness of disease management in females with VVF in a specific population, namely after a benign gynaecologic surgery. The typical postsurgical fistula is the result of a direct and localised trauma to healthy tissue and therefore not comparable with obstetric or irradiation/cancer fistula. No similar analysis was found in literature. Besides, most of the included studies had the same primary outcome parameter, to be specific success after treatment. Limitations of our study are inherent to the limitations of the included studies. None of the included studies stratified data by fistula type, size or location. The methodology of measuring the fistula as well as the used classification system was not clear in the majority of articles. As no study reported data by using a unique classification system, a subgroup analysis according to fistula characteristics was not feasible. Another limitation arises from the study design as the majority of studies consisted of case reports or case series reporting uniform treatment for all documented patients. For this reason risk of bias assessment could be performed in a minority of studies with comparative study design. Furthermore, differences in outcome might be influenced by heterogeneity of study populations.
Conclusion
Although the literature on disease management of females with postsurgical VVF is imprecise and inconsistent, our data show that the majority of patients are treated surgically through a transvaginal route. The quality and design of studies reviewed were weak with a poor reporting standard, weakening the conclusions that can be drawn. In summary, these data do not allow accurate prediction of success and complication rates in female patients with VVF following benign gynaecologic surgery. Standardisation of the terminology is required so that VVF can be managed with a proper surgical treatment algorithm based on characteristics of the fistula and well designed RCT are needed in future.
Supporting information
(DOC)
Acknowledgments
We express our sincere thanks to Mag. Wildner, for her support in literature search.
Data Availability
All relevant data are available in the manuscript.
Funding Statement
This study was supported by the Department of General Gynaecology and Gynaecologic Oncology, Medical University Vienna.
References
- 1.Sharma S, Rizvi SJ, Bethur SS, Bansal J, Qadr SJ, Modi P. Laparoscopic repair of urogenital fistulae: A single center experience. J Minim Access Surg. 2014; 10(4): 180–184. 10.4103/0972-9941.141508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller EA, Webster GD. Current management of vesicovaginal fistulae. Curr Opin Urol. 2001; 11: 417–421. [DOI] [PubMed] [Google Scholar]
- 3.Bazi T. Spontaneous closure of vesicovaginal fistula after bladder drainage alone: review of the evidence. Int Urogynecol J pelvic Floor Dysfunct. 2007; 18(4): 475. [DOI] [PubMed] [Google Scholar]
- 4.Liao CY, Tasi RS, Ding DC. Gynaecological surgery caused vesicovaginal fistula managed by Latzko operation. Taiwan J Obstet Gynecol. 2012; 51(3): 359–362. 10.1016/j.tjog.2012.07.007 [DOI] [PubMed] [Google Scholar]
- 5.Arrow SS, Hamlin EC, Wall LL. Obstructed labour injury complex: Obstetric fistula formation and the multifaceted morbidity of maternal birth trauma in the developing world. Obstet Gynecol Surv. 1996; 51: 568–574. [DOI] [PubMed] [Google Scholar]
- 6.Oakley SH, Brown HW, Greer JA, Richardson ML, Adelowo A, Yurteri-Kaplan L et al. Management of vesicovaginal fistulae: a multicentre analysis from the Fellows Pelvic research Network. Female pelvic Med Reconstr Surg. 2014; 20(1): 7–13. 10.1097/SPV.0000000000000041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ghoniem GM, Warda HA. The management of genitourinary fistula in the third millennium. Arab Journal of Urology. 2014; 12: 97–105. 10.1016/j.aju.2013.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Raz S, Bregg KJ, Nitti VW, Sussman E. Transvaginal repair of vesicovaginal fistula using a peritoneal flap. J urol. 1993; 150: 56–59. [DOI] [PubMed] [Google Scholar]
- 9.McKay HA. Vesicovaginal fistula repair: Transurethral suture cystorrhaphy as a minimally invasive alternative. J Endourol. 2004; 18: 487–490. 10.1089/0892779041271427 [DOI] [PubMed] [Google Scholar]
- 10.Ou CS, Huang UC, Tsuang M, Rowbotham R. Laparoscopic repair of vesicovaginal fistula. J Lapraoendosc Adv Surg Tech A. 2004; 14: 17–21. [DOI] [PubMed] [Google Scholar]
- 11.Sims JM. On treatment of vesicovaginal fistula. Am J Med Sci. 1852; 23: 59. [Google Scholar]
- 12.Martius H. Die operative Wiederherstellung der vollkomen fehlenden Harnröhre und des Schliessmuskels derselben. Zentralbl Gynakol. 1928; 52: 480. [Google Scholar]
- 13.Iselin CE, Alsan P, Webster GD. Transvaginal repair of vesicovaginal fistulas after hysterectomy by vaginal cuff excision. J Urol. 1998; 160: 728–730. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med. 2009 [PMC free article] [PubMed] [Google Scholar]
- 15.Hamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015; 349: g7647 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 16.Khan K, Riet G, Popay J, Nixon J, Klejnen J. Study quality assessment. Undertaking systematic reviews of research effectiveness: CRD`s guidance for those carrying out or commissioning reviews. York: NHS Centre for Reviews and Dissemination, 2001. [Google Scholar]
- 17.Wells GA, Shea B, O`Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle Ottowa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. [Google Scholar]
- 18.R: Development Core team (2008). R: A language and enviroment for statistical computing. R Foundation for statistical computing, Vienna, Austria: Available: http://www.r-project.org. [Google Scholar]
- 19.Ansquer Y, Mellier G, Santulli P, Bennis M, Mandelbrot L, Madelenat P. Latzko operation for vault vesicovaginal fistula. Acta Obstetricia et Gynecologica. 2006; 85: 1248–1251. [DOI] [PubMed] [Google Scholar]
- 20.Abdel-Karim AM, Moussa A, Elsalmy S. Laparoendoscopic single-site surgery extravesical repair of vesicovaginal fistula: early experience. Urology. 2011; 78: 567–571. 10.1016/j.urology.2011.05.036 [DOI] [PubMed] [Google Scholar]
- 21.Ayed M, El Atat R, Hassine LB, Sfaxi M, Chebil M, Zmerli S. Prognostic factors of recurrence after vesicovaginal fistula repair. Int J Urol. 2006; 13(4): 345–349. 10.1111/j.1442-2042.2006.01308.x [DOI] [PubMed] [Google Scholar]
- 22.Aycinena JF. Small vesicovaginal fistula. Urology. 1977; 9(5): 543–545. [DOI] [PubMed] [Google Scholar]
- 23.Agrawal V, Kucherov V, bendana E, Joseph J, Rashid H, Wu G. Robot-assisted laparoscopic repair of vesicovaginal fistula: a single-center experience. Urology. 2015; 86(2): 276–281. 10.1016/j.urology.2015.02.074 [DOI] [PubMed] [Google Scholar]
- 24.Blandy JP, Badenoch DF, Fowler CG, Jenkins BJ, Thomas NW. Early repair of iatrogenic injury to the ureter or bladder after gynecological surgery. J Urol. 1991; 146(3): 761–765. [DOI] [PubMed] [Google Scholar]
- 25.Badenoch DF, Tiptaft RC, Thakar DR, Fowler CG, Blandy JP. Early repair of accidental injury to the ureter or bladder following gynaecological surgery. Br J Urol. 1987; 59(6): 516–518. [DOI] [PubMed] [Google Scholar]
- 26.Baumrucker GO. Ball repair of vesicovaginal fistula. Urology. 1974; 3(3): 333–336. [DOI] [PubMed] [Google Scholar]
- 27.Bramhall TC, Marshall DF. Extraperitoneal repair of vesicovaginal fistulas. Am J Obstet Gynecol. 1950; 60(4): 834–842. [DOI] [PubMed] [Google Scholar]
- 28.Bajory Z, Fekete Z, Kiraly I, Szalay I, Pajor L. Consecutive vesicovaginal fistula for transobturator sling perforations and successfull repairs with skin flap. Neurourol Urodyn. 2011; 30(8): 1530–1532. 10.1002/nau.21114 [DOI] [PubMed] [Google Scholar]
- 29.Brandt FT, Lorenzato FR, Albuquerque CD. Treatment of vesicovaginal fistula by bladder mucosa autograft. J Am Coll Surg. 1998; 186(6): 645–648. [DOI] [PubMed] [Google Scholar]
- 30.Bragayrac LA, Azhar RA, Fernandez G, Cabrera M, Saenz E, Machuca V et al. Robotic repair of vesicovaginal fistulae with transperitoneal-transvaginal approach: a case series. Int Braz J Urol. 2014; 40(6): 810–815. 10.1590/S1677-5538.IBJU.2014.06.12 [DOI] [PubMed] [Google Scholar]
- 31.Clark DH, Holland JB. Repair of vesicovaginal fistulas: simultaneous transvaginal-transvesical approach. South Med J. 1975; 68(11): 1410–1413. [DOI] [PubMed] [Google Scholar]
- 32.Chibber PJ, Shah HN, Jain P. Laparoscopic O`Conor’s repair for vesico-vaginal and vesico-uterine fistulae. BJU Int. 2005; 96(1): 183–186. 10.1111/j.1464-410X.2005.05592.x [DOI] [PubMed] [Google Scholar]
- 33.Chien W-H, Liang C-C. Iatrogenic bladder stone and associated vesicovaginal fistula after hysterectomy. Gynecological Surgery. 2006; 3(2): 134–135. [Google Scholar]
- 34.Chapron C, Dubuisson JB, Ansquer Y, Gregorakis SS, Morice P, Zerbib M. Bladder injuries during total laparoscopic hysterectomy: diagnosis, management, and prevention. J Gynecol Surg. 1995; 11(2): 95–98. 10.1089/gyn.1995.11.95 [DOI] [PubMed] [Google Scholar]
- 35.Cruikshank SH, Pixley RL. Methods of vaginal cuff closure and preservation of vaginal depth during transvaginal hysterectomy. Obstet Gynecol. 1987; 70(1)): 61–63. [PubMed] [Google Scholar]
- 36.Chu L, Wang JJ, Li L, Tong XW, Fan BZ, Guo Y et al. Laparoscopic repair of iatrogenic vesicovaginal and rectovaginal fistula. Int J Clin Exp med. 2015; 8(2): 2364–2370. [PMC free article] [PubMed] [Google Scholar]
- 37.Dogra PN, Saini AK. Laser welding of vesico-vaginal fistula- outcome analysis and long-term outcome: single-centre experience. Int Urogynecol J. 2011; 22(8): 981–984. 10.1007/s00192-011-1389-0 [DOI] [PubMed] [Google Scholar]
- 38.Dorsey JW. The repair of vesicovaginal fistula by the transperitoneal transvesical approach. J Urol. 1960; 83: 404–408. [DOI] [PubMed] [Google Scholar]
- 39.Daley SM, Lallas CD, Swanson SK, Novicki DE, Itano NB. Fibrin sealant closure of a persistent vesicovaginal fistula after failed transabdominal closure. Journal of Pelvic Medicine and Surgery. 2006; 12(4): 229–230. [Google Scholar]
- 40.Dos Santos A, Tanaka M, Abreu SCD, Kawano PR, Yamamoto H, Pereira O et al. Laparoscopic management of iatrogenic lesions. Journal of Endourology. 2008; 22(6): 1279–1283. 10.1089/end.2008.0050 [DOI] [PubMed] [Google Scholar]
- 41.Dorairajan LN, Khattar N, Kumar S, Pal BC. Latzko repair for vesicovaginal fistula revisisted in the era of minimal-access surgery. Int Urol Nephrol. 2008; 40(2): 317–320. 10.1007/s11255-007-9252-4 [DOI] [PubMed] [Google Scholar]
- 42.Dalela D, Ranjan P, Sankhwar PL, Sankhwar SN, Naja V, Goel A. Supratrigonal VVF repair by modified O’Conor’s technique: an experience of 26 cases. European Urology. 2006; 46: 551–556. [DOI] [PubMed] [Google Scholar]
- 43.Ezzat M, Ezzat MM, Tran VQ, Aboseif SR. Repair of giant veiscovaginal fistula. J Urol. 2009; 181(3): 1184–1188. 10.1016/j.juro.2008.10.152 [DOI] [PubMed] [Google Scholar]
- 44.Falk HC, Orkin LA. Nonsurgical closure of vesicovaginal fistula. Obstet Gynecol. 1957; 9(5): 538–541. [PubMed] [Google Scholar]
- 45.Fourie T, Early surgical repair of post-hysterectomy vesicovaginal fistulas. S Afr Med J. 1983; 63(23): 889–90. [PubMed] [Google Scholar]
- 46.Flynn MK, Peterson AC, Amundsen CL, Webser GD. Fuctional outcomes of primary and secondary repairs of vesicovaginal fistulae via vaginal cuff scar excision. Int Urogynecol J Pelvic Floor Dysfunct. 2004; 15(6): 394–398. 10.1007/s00192-004-1188-y [DOI] [PubMed] [Google Scholar]
- 47.Fearl CL, Keizur LW. Optimum time interval from occurrence of vesicovaginal fistula. Trans Pac Coast Obstet Gynecol Soc. 1968; 36: 57–60. [PubMed] [Google Scholar]
- 48.Fang G, Hong L, Li B, Liu C, Wu D, Hong S et al. Transvaginal genital fistula repair with insertion of Foley catheter via fistula tract. J Obstet Gynaecol Res. 2015; 41(7): 1049–1055. 10.1111/jog.12664 [DOI] [PubMed] [Google Scholar]
- 49.Fleischmann J, Picha G. Abdominal approach for gracilis muscle interposition and repair of recurrent vesicovaginal fistulas. J Urol. 1988; 140(3): 552–554. [DOI] [PubMed] [Google Scholar]
- 50.Gupta NP, Mishra S, Hemal AK, Mishra A, Seth A, Dogra PN. Comparative analysis of outcome between open and robotic surgical repair of recurrent supratrigonal vesicovaginal fistula. J Endourol. 2010; 24(11): 1779–1182. 10.1089/end.2010.0049 [DOI] [PubMed] [Google Scholar]
- 51.Gözen AS, Teber D, Canda AE, Rassweiler J. Transperitoneal laparoscopic repair of iatrogenic vesicovaginal fistulas: Heilbronn experience and review of the literature. J Endourol. 2009; 23(3): 475–479. 10.1089/end.2008.0236 [DOI] [PubMed] [Google Scholar]
- 52.Goodwin WE, Scardino PT. Vesicovaginal and ureterovaginal fistulas: a summary of 25 years of experience. J Urol. 1980; 123(3): 370–374. [DOI] [PubMed] [Google Scholar]
- 53.Grange P, Giarenis I, Rouse P, Kouriefs C, Robinson D, Cardozo L. Combined vaginal and vesicoscopic collaborative repair of complex vesicovaginal fistulae. Urology. 2014; 84(4): 950–954. 10.1016/j.urology.2014.06.020 [DOI] [PubMed] [Google Scholar]
- 54.Harrow B. Conservative and surgical management of bladder injuries following pelvic operations. Obstetrics and Gynecology. 1968; 33(6): 852–855. [PubMed] [Google Scholar]
- 55.Hong HM, Lee JW, Han DY, Jeong JH. Vesicovaginal fistula repair using a transurethral pointed electrode. Int Neurourol J. 2010; 14(1): 65–68. 10.5213/inj.2010.14.1.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hessami SH, Chang DT. Use of biomaterial as interposition graft in the treatment of vesicovaginal fistula. Journal of Pelvic medicine and surgery. 2007; 13(1): 39–42. [Google Scholar]
- 57.Hellenthal NJ, Nanigian DK, Ambert L, Stone AR. Limited anterior cystotomy: a useful alternative to the vaginal approach for vesicovaginal fistula repair. Urology. 2007; 70(4): 797–798. 10.1016/j.urology.2007.07.064 [DOI] [PubMed] [Google Scholar]
- 58.Hemal AK, Kolla SB, Wadhwa P. Robotic reconstruction for recurrent supratrigonal vesicovaginal fistulas. J Urol. 2008; 180(3): 981–985. 10.1016/j.juro.2008.05.020 [DOI] [PubMed] [Google Scholar]
- 59.Henriksson CH, Khiel B, Pettersson S. Urethrovaginal and vesicovaginal fistula: A review of 29 patients. Acta Obstet Gynecol Scand. 1982; 61(2): 143–148. [DOI] [PubMed] [Google Scholar]
- 60.Hsieh CH. Surgical repair of a vesicovaginal fistula guided by a braided silk suture line. Int Urogynecol J Pelvic Floor Dysfunct. 2008; 19(11): 1577–1579. 10.1007/s00192-008-0611-1 [DOI] [PubMed] [Google Scholar]
- 61.Immergut S, Cottler ZR. Transvesical repair of vesicovaginal fistula. J Urol. 1950; 63(5): 865–871. [DOI] [PubMed] [Google Scholar]
- 62.James R, Mahajan ST. Concurrent vesicoperitoneal and vesicovaginal fistula. International Urogynecology Journal and pelvic Floor Dysfunction. 2013; 24(1): 173–174. [DOI] [PubMed] [Google Scholar]
- 63.Javali TD, Katti A, Nagaraj HK. A simplified laparoscopic approach to repair vesicovaginal fistula: the M.S. Ramaiah technique. Urology. 2015; 85(3): 544–546. 10.1016/j.urology.2014.11.014 [DOI] [PubMed] [Google Scholar]
- 64.Kostakopoulos A, Deliveliotis C, Louras G, Giftopoulos A, Skolaricos A. Early repair of injury to the ureter or bladder after hysterectomy. Int Urol Nephrol. 1998; 30(4): 445–450. [DOI] [PubMed] [Google Scholar]
- 65.Krissi H, Levy T, Ben-Rafael Z, Levavi H. Fistula formation after large loop excision of the transformation zone in patients with cervical intraepihelial neoplasia. Acta Obstet Gynecol Scand. 2001; 80: 1137–1138. [DOI] [PubMed] [Google Scholar]
- 66.Keettel WC, Sehring FG, deProsse CA, Scott JR. Surgical management of urethrovaginal and vesicovaginal fistulas. Am J Obstet Gynecol. 1978; 131(4): 425–431. [DOI] [PubMed] [Google Scholar]
- 67.Kristensen JK, Lose G. Vesicovaginal fistulas: the transperitoneal repair revisited. Scand J Urol Nephrol. 157; 101–105. [PubMed] [Google Scholar]
- 68.Ledniowska A, Ledniowska G, Karon J, Karon P. An evaluation of the efficiency of different surgery techniques in the treatment of vesicovaginal fistulas- own experience. New Medicine. 2012; 122–124. [Google Scholar]
- 69.Lazarou G, Grigorescu B, Powers K, Mikhail MS. Transvaginal injection of fibrin sealant for closure of vesicovaginal fistula. Pelvic Medicine and Surgery. 2006; 12(6): 335–337. [Google Scholar]
- 70.Llueca A, Herraiz JL, Rodrigo M, Mazzouzi Y, Piquer D, Guijarro M et al. Intravesical mini-laparoscopic repair of vesicovaginal fistulas. Gynecological Surgery. 2015; 12(4): 323–326. [Google Scholar]
- 71.Landes RR. Simple transvesical repair of vesicovaginal fistula. J Urol. 1979; 122(5): 604–606. [DOI] [PubMed] [Google Scholar]
- 72.Dutto L, O’Reilly B. Robotic repair of vesico-vaginal fistula with perisigmoid fat flap interposition: state of the art for a challenging case? Int Urogynecol J. 2013; 24(12): 2029–2030. 10.1007/s00192-013-2081-3 [DOI] [PubMed] [Google Scholar]
- 73.Morgan EK, Santare VJ. Technic for repair of vesicovaginal fistula following total hysterectomy. American Journal of Surgery. 1950; 383–385. [DOI] [PubMed] [Google Scholar]
- 74.DasMahapatra P, Bhattacharyya P. Laparoscopic intraperitoneal repair of high-up urinary bladder fistula: a review of 12 cases. Int Urogynecol J Pelvic Floor Dysfunction. 2007; 18(6): 635–639. [DOI] [PubMed] [Google Scholar]
- 75.Modi P, Goel R, Dodia S. Laparoscopic repair of vesicovaginal fistula. Urol Int. 2006; 76(4):374–376. 10.1159/000092068 [DOI] [PubMed] [Google Scholar]
- 76.Muto G, D’Urso L, Castelli E, Formiconi A, Bardari F. Cyanoacrylic glue: a minimally invasive nonsurgical first line approach for the treatment of some urinary fistulas. J Urol. 2005; 174(6):2239–2243. 10.1097/01.ju.0000181809.51544.20 [DOI] [PubMed] [Google Scholar]
- 77.El-Lateef Moharram AA, El-Raouf MA. Retropubic repair of genitourinary fistula using a free supporting graft. BJU International. 2003; 93: 581–583. [DOI] [PubMed] [Google Scholar]
- 78.McKay HA. Transurethral suture cystorrhaphy for repair of vesicovaginal fistulas: evolution of a technique. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(4):282–287. [DOI] [PubMed] [Google Scholar]
- 79.Milicic D, Sprem M, Bagovic D. A method for the repair of vesicovaginal fistulas. Int J Gynaecol Obstet. 2001;73(1):35–39. [DOI] [PubMed] [Google Scholar]
- 80.McKay HA. Vesicovaginal and vesicocutaneous fistulas: transurethral suture cystorrhaphy as a new closure technique. J Urol. 1997;158(4):1513–1516. [DOI] [PubMed] [Google Scholar]
- 81.Miklos JR, Sobolewski C, Lucente V. Laparoscopic management of recurrent vesicovaginal fistula. Int Urogynecol J. 1999; 10: 116–117. [DOI] [PubMed] [Google Scholar]
- 82.Malin JM, Quiambao VR, Evans AT. Gold leaf in the treatment of urinary fistulas. Invest Urol. 1967;4(4):346–350. [PubMed] [Google Scholar]
- 83.Moriel EZ, Meirow D, Zilberman M, Farkas A. Experience with the immediate treatment of iatrogenic bladder injuries and the repair of complex vesico-vaginal fistulae by the transvesical approach. Arch Gynecol Obstet. 1993;253(3): 127–130. [DOI] [PubMed] [Google Scholar]
- 84.Mohseni MG, Hosseini SR, Alizadeh F, Gooran S, Valikhani N. Bladder mucosal autograft: An effective method for repair of vesicovaginal fistula. Adv Biomed Res. 2012; 1:77 10.4103/2277-9175.102984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Macalpine JB. Repair of a Vesico-vaginal Fistula by a New Technique. Br Med J. 1940; 2(4170): 778–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Malmström L, Sjovall A. Operative treatment of small vesicovaginal fistulae. Urol Int. 1955;1(1): 66–71. [DOI] [PubMed] [Google Scholar]
- 87.Mallikarjuna C, Nayak P, Reddy KP, Ghouse SM, Ragoori D, Bendigeri MT et al. The AINU Technique for Laparoscopic Vesico-Vaginal Fistula Repair: A Preliminary Report. Urol Int. 2015; 95(3): 357–360. 10.1159/000439355 [DOI] [PubMed] [Google Scholar]
- 88.Miklos JR, Moore DM. Laparoscopic extravesical vesicovaginal fistula repair: our technique and 15 –year experience. Int Urogynecol J. 2015; 26: 441–446 10.1007/s00192-014-2458-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nagraj HK, Kishore TA, Nagalaksmi S. Early laparoscopic repair for supratrigonal vesicovaginal fistula. Int Urogynecol J Pelvic Floor Dysfunct. 2007; 18(7): 759–762. 10.1007/s00192-006-0232-5 [DOI] [PubMed] [Google Scholar]
- 90.Nabi G, Hemal AK. Laparoscopic repair of vesicovaginal fistula and right nephrectomy for nonfunctioning kidney in a single session. J Endourol. 2001;15(8): 801–803. 10.1089/089277901753205780 [DOI] [PubMed] [Google Scholar]
- 91.Nesrallah LJ, Srougi M, Gittes RF. The O'Conor technique: the gold standard for supratrigonal vesicovaginal fistula repair. J Urol. 1999; 161(2): 566–568. [DOI] [PubMed] [Google Scholar]
- 92.Nezhat CH, Nezhat F, Nezhat C, Rottenberg H. Laparoscopic repair of a vesicovaginal fistula: a case report. Obstet Gynecol. 1994; 83(5 pt2): 899–901. [PubMed] [Google Scholar]
- 93.Nerli RB, Reddy M. Transvesicoscopic repair of vesicovaginal fistula. Diagn Ther Endosc. 2010; 2010: 760348 10.1155/2010/760348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Otsuko RA, Amaro JL, Tanaka MT, Epacagnan E, Mendes JB, Kawano PR et al. Laparoscopic repair of vesicovaginal fistula. J Endourol. 2008; 22(3): 525–527. 10.1089/end.2006.9846 [DOI] [PubMed] [Google Scholar]
- 95.Ostad M, Uzzo RG, Coleman J, Young GP. Use of a free bladder mucosal graft for simple repair of vesicovaginal fistulae. Urology. 1998; 52(1): 123–126. [DOI] [PubMed] [Google Scholar]
- 96.Phipps J. Laparoscopic repair of posthysterectomy vesicovaginal fistula: two case reports. Gynecological Endoscopy. 1996; 5(2): 123–124. [Google Scholar]
- 97.Persky L, Herman G, Guerrier K. Nondelay in vesicovaginal fistula repair. Urology. 1979; 13(3): 273–275. [DOI] [PubMed] [Google Scholar]
- 98.Pietersma CS. Robotic-assisted laparoscopic repair of a vesicovaginal fistula: a time-consuming novelty or an effective tool? BMJ Case reports. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Persky L, Rabin R. Experiences with vesicovaginal fistulas. Am J Surg. 1973;125(6): 763–766. [DOI] [PubMed] [Google Scholar]
- 100.Pontes EJ. Rotation of bladder flap for repair of vesicovaginal fistula. Urology. 1974; 4(1): 109–111. [DOI] [PubMed] [Google Scholar]
- 101.Peikoff SS, Wall MB. Surgical treatment of large vesicovaginal fistula; report of a case. J Int Coll Surg. 1956; 26(6): 718–724. [PubMed] [Google Scholar]
- 102.Phsak T, Nikolavsky D, Terlecki R, Flynn BJ. Is tissue interposition always necessary in transvaginal repair of benign, recurrent vesicovaginal fistulae? Urology. 2013; 82(3): 707–712. 10.1016/j.urology.2013.03.076 [DOI] [PubMed] [Google Scholar]
- 103.Rizvi SJ, Gupta R, Patel S, Trivedi A, Trivedi P, Modi P. Modified laparoscopic abdominal vesico-vaginal fistula repair-"Mini-O'Conor" vesicotomy. J Laparoendosc Adv Surg Tech A. 2010; 20(1): 13–15. 10.1089/lap.2009.0176 [DOI] [PubMed] [Google Scholar]
- 104.Reynolds S, Gottlieb LJ, Lucioni A, Rapp DE, Song DH, Bales GT. Vesicovaginal fistula repair with rectus abdominis myofascial interposition flap. Urology. 2008; 71: 1119–1123. 10.1016/j.urology.2007.12.057 [DOI] [PubMed] [Google Scholar]
- 105.Radopoulos DK, Dimitriadis GP, Vakalopoulos IK, Ioannidis SS, Tzakas KA, Vasilakakis IE. Our experience with salvage genitourinary fistulae repair: technique and outcomes. Int Urol Nephrol. 2008; 40(1): 57–63. 10.1007/s11255-007-9218-6 [DOI] [PubMed] [Google Scholar]
- 106.Roslan M, Markuszewski MM, Baginska J, Krajka K. Suprapubic transvesical laparoendoscopic single-site surgery for vesicovaginal fistula repair: a case report. Wideochir Inne Tech Maloinwazyjne. 2012; 7(4): 307–310. 10.5114/wiitm.2011.30816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Razi A, Mazloomfard MM, Ajami H, Moeini A. Combined vagino-abdominal approach for management of vesicovaginal fistulas: a 10 years' experience. Arch Gynecol Obstet. 2015; 292(1):121–5. 10.1007/s00404-014-3589-6 [DOI] [PubMed] [Google Scholar]
- 108.Rader ES. Post-hysterectomy vesicovaginal fistula: treatment by partial colpocleisis. J Urol. 1975; 114(3): 389–390. [DOI] [PubMed] [Google Scholar]
- 109.Rajamaheswari N, Chhikara AB, Seethalakshmi K, Bail A, Agarwal S. Trans-vaginal repair of gynecological supratrigonal vesicovaginal fistulae: A worthy option! Urol Ann. 2012; 4(3): 154–157. 10.4103/0974-7796.102660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Szendi B. Repair of vesicovaginal fistulas according to Latzko. Acta Med Acad Sci Hung. 1959;14: 133–139. [PubMed] [Google Scholar]
- 111.Schneidermann C, Strean Gj. Vesicovaginal fistula. Canad M.A.J. 1958; 79: 801–805. [PMC free article] [PubMed] [Google Scholar]
- 112.Shah SJ. Role of day care vesicovaginal fistula fulguration in small vesicovaginal fistula. J Endourol. 2010; 24(10): 1659–1660. 10.1089/end.2009.0557 [DOI] [PubMed] [Google Scholar]
- 113.Roen P. Combined vaginal and transvesical approach in successful repair of vesicovaginal fistula. AMA Arch Surg. 1960; 80(4): 628–633. [DOI] [PubMed] [Google Scholar]
- 114.Robles JE, Saiz A, Rioja J, Brugarolas X, Berian JM. Collagen graft interposition in vesicovaginal fistula treatment. Urol Int. 2009; 82(1):116–118. 10.1159/000176038 [DOI] [PubMed] [Google Scholar]
- 115.Schimpf MO, Morgenstern JH, Tulikangas PK, Wagner JR. Vesicovaginal fistula repair without intentional cystotomy using the laparoscopic robotic approach: a case report. JSLS. 2007; 11(3): 378–380. [PMC free article] [PubMed] [Google Scholar]
- 116.Sears CL, Schenkman N, Lockrow EG. Use of end-to-end anastomotic sizer with occlusion balloon to prevent loss of pneumoperitoneum in robotic vesicovaginal fistula repair. Urology. 2007; 70(3): 581–582. 10.1016/j.urology.2007.05.026 [DOI] [PubMed] [Google Scholar]
- 117.Sundaram BM, Kalidasan G, Hemal AK. Robotic repair of vesicovaginal fistula: case series of five patients. Urology. 2006; 67: 970–973. 10.1016/j.urology.2005.11.014 [DOI] [PubMed] [Google Scholar]
- 118.Starkman JS, Meints L, Scarpero HM, Dmochowski RR. Vesicovaginal fistula following a transobturator midurethral sling procedure. Int Urogynecol J. 2007; 18: 113–115. [DOI] [PubMed] [Google Scholar]
- 119.Singh RB, Pavithran NM, Khatri HL, Nanda S.Technical aspects in the management of complex vesicovaginal fistulae. Trop Doct. 2005; 35(1): 40–41. 10.1258/0049475053001994 [DOI] [PubMed] [Google Scholar]
- 120.Soong Y, Lim PHC. Urological Injuries in Gynecological practice–when is the optimal time for repair? Singapur Med J. 1997; 38(11): 475–478. [PubMed] [Google Scholar]
- 121.Singh V, Sinha R, Mehrotra S, Gupta DK, Gupta S. Transperitoneal transvesical laparoscopic repair of vesicovaginal fistulae: experience of a tertiary care center in northern india. Curr Urol. 2013; 7: 75–82. 10.1159/000356253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Shirvan MK, Alamdari DH, Ghoreifi A. A novel method for iatrogenic vesicovaginal fistula treatment: autologous platelet rich plasma injection and platelet rich fibrin glue interposition. J Urol. 2013; 189(6): 2125–2129. 10.1016/j.juro.2012.12.064 [DOI] [PubMed] [Google Scholar]
- 123.Simforoosh N, Soltani MH, Lashay A, Ojand A, Nikkar MM, Ahanian A et al. Laparoscopic vesicovaginal fistula repair: report of five cases, literature review, and pooling analysis. J Laparoendosc Adv Surg Tech A. 2012; 22(9): 871–875. 10.1089/lap.2012.0141 [DOI] [PubMed] [Google Scholar]
- 124.Sharifiaghdas F, Taheri M. The use of a rotational bladder flap for the repair of recurrent mixed trigonal-supratrigonal vesicovaginal fistulas. Int J Gynaecol Obstet. 2012; 119(1):18–20. 10.1016/j.ijgo.2012.04.026 [DOI] [PubMed] [Google Scholar]
- 125.Singh V, Sinha RJ, Mehrotra S, Sankhwar SN, Bhatt S. Repair of vesicovaginal fistula by the transabdominal route: outcome at a north Indian tertiary hospital. Int Urogynecol J. 2012; 23: 411–416. 10.1007/s00192-011-1544-7 [DOI] [PubMed] [Google Scholar]
- 126.Tancer ML. Observations on prevention and management of vesicovaginal fistula after total hysterectomy. Surg Gynecol Obstet. 1992; 175(6): 501–506. [PubMed] [Google Scholar]
- 127.Toledo LG, Santos VE, Maron PEG, Vedovato BC, Fucs M, Perez MDC. Continent vesicovaginal fistula. Einstein. 2013; 11(1): 119–121. 10.1590/S1679-45082013000100022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tsivian A, Uchvatkin G, Shtricker A, Yacobi Y, Kurenkov A, Sidi A. In support of early treatment of postoperative vesicovaginal fistulas. Journal of Pelvic Medicine and Surgery. 2006; 12(4): 197–200. [Google Scholar]
- 129.Tiong HY, Shim T, Lee YM, Tan JKN. Laparoscopic repair of vesicovaginal fistula. Int Urol Nephrol. 2007; 39: 1085–1090. 10.1007/s11255-006-9168-4 [DOI] [PubMed] [Google Scholar]
- 130.von Theobald Peter, Hamel P, Febbraro W. Laparoscopic repair of a vesicovaginal fistula using an omental flap. British Journal of Obstetrics and Gynecology. 1998; 105: 1216–1218. [DOI] [PubMed] [Google Scholar]
- 131.Taylor WM. The transvesical repair of vesico vaginal fistula. The Journal of Urology. 1948; 61(3): 488–492. [DOI] [PubMed] [Google Scholar]
- 132.Udea T, Iwatsubo E, Osada Y, Hirano H, Iwakawa A. Closure of a vesicovaginal fistula using a vaginal flap. The Journal of Urology. 1977; 119: 742–743. [DOI] [PubMed] [Google Scholar]
- 133.Wong C, Lam PN, Lucente VR. Laparoscopic transabdominal transvesical vesicovaginal fistula repair. J Endourol. 2006; 20(4): 240–243. 10.1089/end.2006.20.240 [DOI] [PubMed] [Google Scholar]
- 134.Wein AJ, Malloy TR, Carpiniello VL, Greenberg SH, Murphy JJ. Repair of vesicovaginal fistula by a suprapubic transvesical approach. Surg Gynecol Obstet. 1980; 150(1): 57–60. [PubMed] [Google Scholar]
- 135.Xu Z, Fu Q. Bulbocavernosus muscle flap in the repair of complicated vesicovaginal fistula. International Journal of Urology. 2005; 12: 1037–1040. 10.1111/j.1442-2042.2005.01200.x [DOI] [PubMed] [Google Scholar]
- 136.Zhang Q, Ye Z, Liu F, Qi X, Shao C, He X et al. Laparoscopic transabdominal transvesical repair of supratrigonal vesicovaginal fistula. Int Urogynecol J. 2013; 24: 337–342. 10.1007/s00192-012-1850-8 [DOI] [PubMed] [Google Scholar]
- 137.Zumrutbas AE, Ozlulerden Y, Alkis O, Baser A, Aybek Z. Optic-guided vaginal repair of vesicovaginal fistula. J Endourol. 2014; 28(3): 275–279. 10.1089/end.2013.0435 [DOI] [PubMed] [Google Scholar]
- 138.Kocharkarn W, Pummangura W. A new dimension in vesicovaginal fistula management: an 8-year experience at Ramathibodi hospital. Asian J Surg. 2007; 30(4): 267–271 10.1016/S1015-9584(08)60037-8 [DOI] [PubMed] [Google Scholar]
- 139.Wesolowski S, Bulinski W. Vesico-intestinal fistula and rectourethral fistulae. Br J Urol. 1973; 45: 34–38. [DOI] [PubMed] [Google Scholar]
- 140.Gerber GS, Schoenberg HW. Female urinary tract fistulas. J Urol. 1993; 149(2): 229–236. [DOI] [PubMed] [Google Scholar]
- 141.Sotelo R, Garcia A, Yaime H, Rodriguez E, Dubois R, Andrade RD et al. Laparoscopic rectovesical fistula repair. J Endourol. 2005; 19: 603–607. 10.1089/end.2005.19.603 [DOI] [PubMed] [Google Scholar]
- 142.Mellano EM, Tarney Cm. Management of genitourinary fistula. Curr Opin Obstet Gynecol. 2014; 26(5): 415–423. 10.1097/GCO.0000000000000095 [DOI] [PubMed] [Google Scholar]
- 143.Angioli R, Penalver M, Muzii L, Mendez L, Mirhashemi R, bellati F et al. Guidelines of how to manage vesicovaginal fistula. Crit Rev Oncol Hematol. 2003; 48(3): 295–304. [DOI] [PubMed] [Google Scholar]
- 144.Miklos JR, Moore RD, Chinthakanan O. Laparoscopic and robotic-assisted vesicovaginal fistula repair: A systematic review of the literature. J Minim Invasive Gynecol. 2015; 22(5): 727–736. 10.1016/j.jmig.2015.03.001 [DOI] [PubMed] [Google Scholar]
- 145.Melah GS, el-Nafaty AU, Bukar M. Early versus late closure of vesicovaginal fistulas. Int J Gynaecol Obstet. 2006; 93: 252–253. 10.1016/j.ijgo.2006.02.017 [DOI] [PubMed] [Google Scholar]
- 146.Javed A, Abdullah A, Faruqui N, Syed SS, Mehdi B, Pirzada AJ. Doctor! Will I be dry? Factors determining recurrence after vesicovaginal fistula repair. J Pak Med Assoc. 2015; 65(9): 954–959. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
Data Availability Statement
All relevant data are available in the manuscript.