Abstract
Objective
Chronic rhinosinusitis with nasal polyposis (CRSwNP) is a disease process that is driven, in part, by intrinsic mucosal inflammation. Surgery plus continued medical therapy is commonly elected by medically recalcitrant, symptomatic patients. The objective was to evaluate the prevalence of nasal polyp recurrence up to 18-months after endoscopic sinus surgery (ESS) with congruent continuing medical management.
Study Design
Prospective, multi-center cohort of adult patients undergoing ESS for medically recalcitrant CRSwNP performed between August, 2004 and February, 2015.
Methods
All patients received baseline nasal endoscopy quantified using Lund-Kennedy grading. All patients included for final analysis provided at least 6-month postoperative endoscopy examinations. Multivariate analysis was used to identify risk factors for polyp recurrence.
Results
363 CRSwNP patients having undergone ESS involving polypectomy were enrolled. A total of 244 (67%) participants had graded postoperative endoscopies with average of follow-up of 14.3[±7.0] months. Surgery plus postoperative medical management significantly improved endoscopy total scores at 6-months (p<0.001). The recurrence of nasal polyposis 6-months after ESS was 35% (68/197), compared to 38% (48/125) after 12-months, and 40% (52/129) after 18-months. Multivariate analysis identified both prior ESS (OR=2.6, 95% CI: 1.5–4.6; p=0.001) and worse preoperative polyposis severity (OR=1.4, 95% CI: 1.1–1.8; p=0.016) as risk factors for recurrent polyposis.
Conclusions
Polyp recurrence is common after ESS with control of polyps up to 18-months found in approximately 60–70% of patients. Investigation into both surgical and medical management strategies is warranted to improve upon the observed prevalence of recurrence.
MeSH Key Words: Nasal Polyps, Recurrence, Sinusitis, Chronic Disease, Endoscopy, Edema
INTRODUCTION
Modern treatments of chronic rhinosinusitis with nasal polyposis (CRSwNP) seek to reduce the burden of symptoms and future interventions for patients, commonly requiring multi-modality therapy including endoscopic sinus surgery (ESS) followed by continued appropriate medical therapy. Disease-specific quality-of-life (QOL) measures demonstrate surgical efficacy in the short-term (eg. 18-month follow-up)1–3 with multi-institutional cohort data, but long-term follow-up (eg. 5-year) has shown revision polypectomy rates range between 20–50% across single institution,4 multi-institutional5 and administrative data.6
Controlling polypoid sinus disease is, in part, measured by symptom severity but also through endoscopic analysis. Although the primary outcome of ESS is QOL improvement, endoscopic evaluation does allow for an objective measure of sinonasal disease. Beyond establishing diagnoses, endoscopic findings are used, in part, to guide continued medical therapy and monitor disease progression. Furthermore, although aggregate endoscopy and QOL scores do not historically associate, optimized and weighted endoscopic grading scores have accounted for ~33% of the explained variability in sinus-specific symptoms; largely driven by the polyp and edema severity.7
Despite standard use of endoscopy exams for CRSwNP, inadequate data exists for endoscopic findings of recurrent polyposis following ESS. One comprehensive analysis of a single-institutional cohort revealed short-term polyp recurrence in ~50% of patients 12-months following ESS.8 Aspirin-exacerbated disease and comorbid asthma were associated with an increased likelihood of polyp recurrence while Draf-III frontal sinusotomy was protective against polyp recurrence. Our prospective, multi-institutional investigation examined polyp and edema recurrence in patients with CRSwNP after ESS and identified clinical factors associated with relapse.
MATERIALS & METHODS
Patient Population and Inclusion Criteria
Adult study participants (≥18 years old) were prospectively enrolled into a previously described, non-randomized, multi-center, observational cohort investigation into treatment outcomes following ESS.2,9–12 Patients were diagnosed with medically recalcitrant CRSwNP defined by the temporally relevant criteria.13–15 Study participants voluntarily elected ESS as subsequent treatment of CRSwNP after initial therapeutics including, but not limited to, at least one course of either topical corticosteroids (≥21-days) or a 5+ day course of oral corticosteroid therapy and at least one course (≥14-days) of broad spectrum or culture-directed antibiotics.
Enrollment sites included sinus clinics within tertiary referral, academic hospitals in North America: Oregon Health & Science University (OHSU; Portland, OR), Stanford University (Palo Alto, CA), the Medical University of South Carolina (Charleston, SC), the University of Utah (Salt Lake City, UT), the University of Calgary (Calgary, Alberta, Canada), and the Medical College of Wisconsin (Milwaukee, WI). Patients were assured that study consent was voluntary and standard of care was not altered by study participation. An Institutional Review Board (IRB) at each enrollment center governed investigational protocols and informed consent.
During preoperative enrollment meetings participants provided demographic information, as well as social and medical history. Participants were observed up to 18-months and evaluated at ~6-month intervals during routine physician-directed postoperative clinical appointments per the standard of care.
Surgical Intervention
Surgical approach was directed by the intraoperative discretion of each enrolling physician and reflected disease progression. Study participants were either primary or revision ESS cases conducted under general anesthesia with judicious use of image guidance. Postoperative therapeutic regimens including daily 240ml. nasal saline rinses and medical therapeutics as necessary.
Exclusion Criteria
Due to potential variations in disease etiology and surgical and/or therapeutic interventions, participants with comorbid ciliary dyskinesia were excluded. Participants were excluded if less than 6-months had lapsed since ESS procedures at the time of analysis. Participants failing to return for postoperative clinical appointments within 18-months were considered lost to follow-up.
Clinical Measures of Disease Severity
Clinical measures of disease severity, collected during routine clinical assessments, were used simultaneously for investigational purposes. High resolution computed tomography (CT) with landmark navigation (Medtronic, Minneapolis, MN) was utilized to evaluate preoperative sinonasal disease severity using 1.0mm. contiguous images in the axial plane. Images were quantified by the enrolling physician in accordance with Lund-Mackay bilateral staging (score range: 0–24).16
Bilateral paranasal sinuses were evaluated preoperatively and postoperatively using rigid endoscopy (Karl Storz, Tuttlingen, Germany) and quantified using Lund-Kennedy (LK) staging (score range: 0–20) which quantifies visualized pathologic states within the paranasal sinuses.17 Higher scores on both staging systems indicate worse overall disease severity.
Data Management and Statistical Analysis
Study data was coded using unique study identification numbers to ensure confidentiality and transferred into a HIPAA compliant database (Access, Microsoft Corp., Redmond, WA). Statistical analyses were conducted using commercially available software (SPSS v.22, IBM Corp, Armonk, NY). The two primary outcome measures of interest, the prevalence of postoperative nasal polyposis and sinonasal edema, were identified using evidence from LK endoscopic staging and defined as non-zero (>0) LK scores recorded during follow-up examinations. Bilateral scores were also calculated by summarizing unilateral scores for nasal polyposis and sinonasal edema at each evaluation time point (range: 0–4). Descriptive analytics were conducted and within-subject differences in mean endoscopy scores were conducted using either paired sample t-testing or Wilcoxon signed-rank testing. Observed patient follow-up (person-months) was summarized to determine incident density rates of recurrence.
Multivariate logistic regression models were built to identify independent patient characteristics associated with nasal polyposis and sinonasal edema recurrence. Preliminary models included a binary measure of either nasal polyp or edema recurrence, as the main dependent variables of interest, and all independent cofactors (Tables 1 and 2) screened for univariate significance (p<0.250) with adjustment for enrollment site variation. Final models were built using a forward selection (p=0.010) and backwards elimination (p=0.050) technique in a manual, stepwise process. Goodness-of-fit was evaluated using Hosmer-Lemeshow (H-L) test statistics.18 Adjusted odds ratios (OR), 95% confidence intervals (CI) are reported with corresponding type-I errors.
Table 1.
Preoperative characteristics of surgical cohort with CRS with nasal polyposis (n=363)
| Characteristics: | N (%) | Mean [±SD] | Range |
|---|---|---|---|
| Age at enrollment (years) | 49.8 [±14.5] | 19 – 83 | |
| Males | 217 (60%) | ||
| Caucasian | 301 (83%) | ||
| Hispanic/Latino | 15 (4%) | ||
| Asthma | 204 (56%) | ||
| Allergy (skin prick/RAST) | 152 (42%) | ||
| Aspirin sensitivity | 80 (22%) | ||
| Prior sinus surgery | 237 (65%) | ||
| Septal deviation | 89 (25%) | ||
| Turbinate hypertrophy | 25 (7%) | ||
| Depression | 35 (10%) | ||
| Tobacco use/smoking | 22 (6%) | ||
| Alcohol consumption | 168 (46%) | ||
| Corticosteroid dependency | 31 (9%) | ||
| Diabetes mellitus (Type I/II) | 16 (4%) | ||
| Preoperative clinical measures: | |||
| Computed tomography total score | 17.1 [±4.7] | 0 – 24 | |
| LK Endoscopy total score | 10.1 [±3.7] | 1 – 20 | |
| a. Nasal polyposis score* | 3.3 [±1.0] | 1 – 4 | |
| b. Discharge score* | 2.3 [±1.3] | 0 – 4 | |
| c. Edema score* | 3.2 [±1.2] | 0 – 4 | |
| d. Scarring score* | 0.9 [±1.3] | 0 – 4 | |
| e. Crusting score* | 0.4 [±1.0] | 0 – 4 | |
CRS, chronic rhinosinusitis; SD, standard deviation; RAST, radioallergosorbent testing; LK, Lund-Kennedy;
indicates summarized bilateral severity scores
Table 2.
Unilateral and bilateral surgical procedures for patients with CRSwNP (n=363)
| Procedures: | Left side N (%) | Right side N(%) |
|---|---|---|
| Maxillary antrostomy | 337 (93%) | 330 (91%) |
| Partial ethmoidectomy | 18 (5%) | 20 (6%) |
| Total ethmoidectomy | 338 (93%) | 332 (92%) |
| Sphenoidotomy | 301 (83%) | 296 (82%) |
| Middle turbinate resection | 92 (25%) | 103 (28%) |
| Inferior turbinate reduction | 38 (11%) | 38 (11%) |
| Septoplasty | 107 (30%) | |
| Frontal sinusotomy Draf 1 | 112 (31%) | 110 (31%) |
| Frontal sinusotomy Draf 2a | 154 (42%) | 155 (43%) |
| Frontal sinusotomy Draf 2b | 27 (7%) | 29 (8%) |
| Frontal sinusotomy Draf 3 | 7 (2%) | |
| Image guidance | 303 (84%) | |
| Year of endoscopic sinus surgery: | ||
| 2004 | 19 (5%) | |
| 2005 | 26 (7%) | |
| 2006 | 64 (18%) | |
| 2007 | 39 (11%) | |
| 2008 | 29 (8%) | |
| 2009 | 9 (3%) | |
| 2011 | 24 (7%) | |
| 2012 | 66 (18%) | |
| 2013 | 50 (14%) | |
| 2014 | 36 (10%) | |
| 2015 | 1 (0.3%) | |
CRSwNP, chronic rhinosinusitis with nasal polyposis
Linear trends in mean endoscopy scores was also evaluated using repeated measures analysis of variance (ANOVA) for participants who completed all postoperative endoscopy exams. Within-subjects effects were determined using level III or IV models and corresponding F-test statistics. The prevalence of nasal polyposis and sinonasal edema were also compared between each postoperative follow-up using McNemar’s chi-square (χ2) test for matched pairs.
RESULTS
Cohort Characteristics and Postoperative Follow-up
A total of 363 study participants met inclusion criteria, completed enrollment procedures and received ESS, involving polypectomy, between August, 2004 and February, 2015. Final cohort characteristics and preoperative measures of disease severity are described in Table 1 while the prevalence of additional ESS procedures and enrollment years are described in Table 2. Postoperative endoscopy examination scores were available for 244 (67%) total participants who were followed for an average [±standard deviation] of 14.3[±7.0] months overall. A total of 197 (54%) participants returned for 6-month endoscopy while 125 (34%) and 129 (36%) participants returned for 12-month and 18-month endoscopy, respectively.
Postoperative recurrence of nasal polyposis
Overall, the proportion of study participants with CRSwNP who were found to have either unilateral or bilateral nasal polyp recurrence at some point during the follow-up period was found to be 116/244 (48%). However, a total of 27/116 of those participants (23%) with postoperative polyp recurrence were found to experience at least temporary polyp resolution via continued medical therapy or clinic-based procedures at the last follow-up examination.
A total of 68/197 (35%) of participants were found to have unilateral or bilateral nasal polyp recurrence at 6-month follow-up endoscopy exams, compared to 48/125 (38%) of participants at 12-month follow-up and 52/129 (40%) of participants with recurrence at 18-month follow-up. For participants with at least 6-month follow-up (n=244), average endoscopy total and polyp scores at each evaluation time are described in Figure 1. Mean total endoscopy scores improved from a preoperative score of 10.3[±3.7] to 5.1[±3.6] at 6-month follow-up (n=197; p<0.001), however no significant differences were noted between 6-month and 12-month total scores (n=96; 4.8[±3.6] vs. 4.8[±3.5]; p=0.940) or between 12-month and 18-month total scores (n=79; 5.2[±3.6] vs. 5.1[±3.7]; p=0.678). Similar over-time differences were found for matched pairings of bilateral LK polyp scores which improved in severity from a preoperative mean score of 3.4[±1.0] to 0.8[±1.3] at 6-month follow-up (p<0.001). No significant differences between either 6-month or 12-month scores (0.7[±1.2] vs. 0.8[±1.1]; p=0.701) or 12-month and 18-month LK polyp scores (0.9[±1.2] vs. 1.0[±1.4]; p=0.830) were found.
Figure 1.
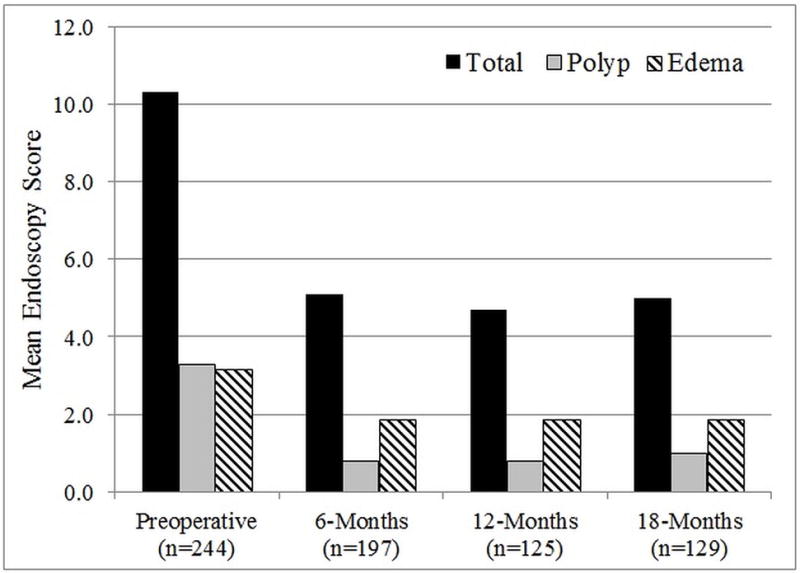
Average endoscopy total scores, bilateral nasal polyposis and sinonasal edema scores before and after endoscopic sinus surgery
Study participants with follow-up (n=244) were observed for a total of 3,478 person-months postoperatively. Participants with unilateral or bilateral polyp recurrence (n=116) had an incidence density rate of 3.3/100 person-months.
Postoperative recurrence of sinonasal edema
The proportion of participants with CRSwNP who were found to have either unilateral or bilateral edema at some follow-up period was 211/244 (87%). A total of 164/197 (83%) of participants were found to have unilateral or bilateral edema at 6-month follow-up endoscopy exams, compared to 102/125 (82%) at 12-month and 101/129 (78%) of participants with edema at 18-month follow-up. For participants with at least 6-month follow-up (n=244), average bilateral edema scores at each evaluation time are also described in Figure 1. Matched pairings of bilateral LK edema scores significantly improved from a preoperative mean score of 3.2[±1.2] to 1.9[±1.2] at 6-month follow-up (p<0.001). No significant differences in matched pairs between either 6-month or 12-month bilateral LK edema scores (1.9[±1.1] vs. 1.9[±1.2]; p=0.885) or between 12-month and 18-month edema scores (2.0[±1.2] vs. 1.9[±1.2]; p=0.490) were found. Participants with unilateral or bilateral edema recurrence (n=211) had an incidence density rate of 6.1/100 person-months.
Multivariate modeling – polyposis and edema recurrence
Multivariate logistic regression was performed to identify potential independent predictors of both nasal polyposis and sinonasal edema recurrence. After preliminary screening, final modeling for polyp recurrence found that after controlling for potential variation between enrollment sites, a history of previous ESS (OR=2.6; 95% CI: 1.5–4.6; p=0.001) and higher preoperative, bilateral nasal polyposis LK endoscopy scores (OR=1.4, 95% CI: 1.1–1.8; p=0.016) were found to associate with polyp recurrence. Final modeling for edema recurrence found that, after controlling for enrollment site variation, only a history of previous ESS (OR=4.5, 95% CI: 2.1–9.8; p<0.001) was found to associate with edema recurrence. The H-L goodness-of-fit was found to be adequate for both the final nasal polyposis and sinonasal edema models (χ2=3.1 and χ2=6.1, respectively; p>0.050). Neither extent of surgery nor year of ESS was associated with polyp recurrence (p>0.050).
Longitudinal analysis –polyposis and edema recurrence
A subgroup of 63/244 (26%) participants returned for endoscopy examinations at all three study follow-up time points. Participants were found to have an average baseline LK endoscopy total score of 10.7[±3.8], a 6-month total score of 5.2[±3.6], a 12-month total score of 5.3[±3.6], and an 18-month mean total score of 5.1[±3.5]. Within-subjects effects found a significant overall improvement (F(3)=54.6; p<0.001) experienced in the first 6-months but no significant difference in mean endoscopy total scores between 6-month and 18-month follow-up (F(2)=0.1; p=0.920). Similarly participants were found to have an average preoperative bilateral polyp score of 3.5[±1.0], a 6-month bilateral score of 0.8[±1.2], a 12-month bilateral score of 1.0[±1.2], and an 18-month polyp score of 1.0[±1.4]. Within-subjects effects again found significant overall improvement (F(3)=85.3; p<0.001) experienced in the first 6-months postoperatively but no significant differences in mean LK polyp scores between 6-month and 18-months (F(2)=0.6; p=0.525). Participants also had an average preoperative bilateral LK edema score of 3.2[±1.4], a 6-month bilateral score of 1.9[±1.1], a 12-month bilateral score of 2.0[±1.1], and an 18-month edema score of 2.0[±1.2]. Within-subjects effects found significant overall improvement (F(3)=21.2; p<0.001) experienced in the first 6-months postoperatively but no significant differences in mean LK edema scores between 6-month and 18-month evaluations (F(2)=0.1; p=0.862).
The prevalence of unilateral or bilateral recurrent nasal polyposis following ESS was found to be 35% at 6-months evaluation, 46% at 12-month and 41% at 18-month follow-up evaluation (Figure 2). No significant difference in the prevalence of polyp recurrence (p≥0.143) was found between 6-months and 18-months. The prevalence of unilateral or bilateral recurrent sinonasal edema before ESS was 89%. No significant difference in the prevalence of edema, between any two evaluation time points, was found (p≥0.727) with 86% of patients having edema at 6-months, 89% at 12-months, and 86% at 18-month follow-up.
Figure 2.
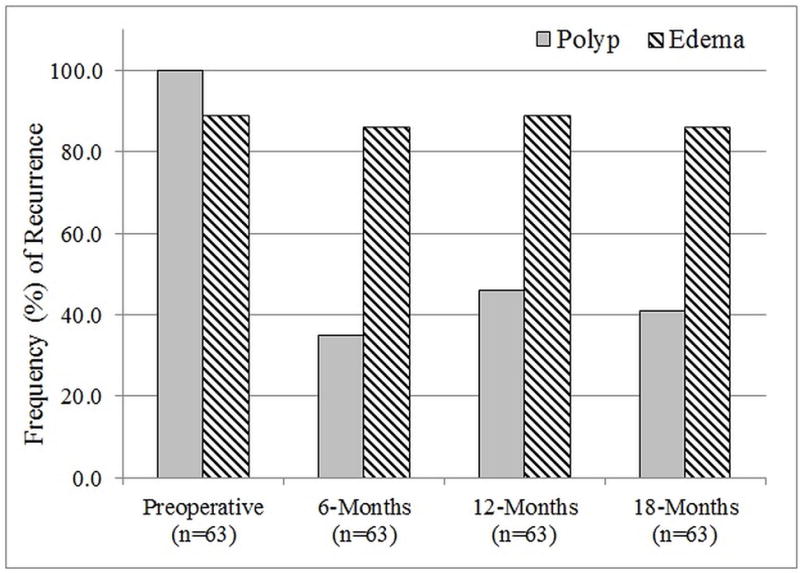
Prevalence of unilateral or bilateral nasal polyposis and sinonasal edema scores before and after endoscopic sinus surgery
DISCUSSION
This study investigated the prevalence of polyp recurrence in a large, multi-center, prospective cohort of patients with CRSwNP undergoing ESS. Despite ESS plus continued medical therapy, 40% of patients with 18-month follow-up demonstrate polyp recurrence which is comparable to or better than other cohort studies that report 50–60% recurrence rates.8,19 Evaluation of cofactors associated with polyp recurrence identified only prior ESS and worse preoperative polyposis severity to be significantly associated with recurrence. This is in contrast to prior cohorts that have identified aspirin-exacerbated respiratory disease and comorbid asthma as risk factors for recurrence. These postoperative endoscopic findings suggest that although current medical and/or surgical interventions for CRSwNP achieve significant improvement in patient reported outcome measures,1–3 a significant portion of our patients fail to achieve endoscopic control of the disease.
Examination of the association between surgical extent and polyp recurrence in a previous single institution cohort study found that more extensive surgery was protective against polyp recurrence. Jankowski et al.20 found that nasalization of the ethmoids (i.e., complete mucosal stripping coupled with complete marsupialization) was associated with lesser polyp recurrence compared to ‘functional’ ethmoidectomy. Bassiouni et al.8 found that Draf-III frontal sinusotomy was associated with reduced prevalence of polyp recurrence. Unfortunately, our cohort data was not adequate to capture the impact of Draf-III on polyp recurrence given that only 2% of patients underwent Draf-III procedures. Further multi-institutional study into the association between surgical extent and polyp recurrence is needed since no other variable, under the surgeon’s control, has been found to significantly associate with reduced polyp recurrence. Finally, there are vastly different reported neo-ostium patency rate outcomes21,22 and clarification of the true efficacy of this procedure would help clarify the role of Draf-III sinusotomy in managing patients with CRSwNP.
A more extensive surgical approach, including extended sinusotomy, may be an important tool to combat polyp recurrence in specific anatomic situations. Minimal investigation has been made into the impact of sphenoid marsupialization and mega-antrostomies on polyp recurrence or PROMs.23 Finally, there is evidence that middle turbinate resection is associated with a slower rate of return of nasal polyposis.4 These findings, coupled with high-level evidence showing no difference PROMs in patients, which have or have not undergone middle turbinate resection,24 suggest that middle turbinate resection should be strongly considered in CRSwNP surgery. The mucosal sparing Denker’s procedures with Draf-III’s frontal sinusotomy may also be appropriate in patients with CRSwNP.25
There has been a paradigm shift in CRS management since early the early inception of ESS in order to establish ventilation in order to surgically facilitate improved application of continued topical medical therapy. This study, unfortunately involved no therapeutic compliance data or detailed medical regimens given the difficulty in obtaining accurate and complete medication history. This data, though, does reflect a real world milieu surrounding the use of postoperative topical therapies, whatever that compliance may be. The study does also incorporate approximately 10-years of surgical intervention. During this time, evidence based research evolved to define how ESS impacts topical distributions and a paradigm shift from strict ventilation of the sinuses to the ventilation and facilitation of continued topical medical therapies. Interestingly, the year of surgery however was not significantly associated with the prevalence of polyp recurrence (p=0.860), ranging between 40% (2014) to 75% (2009). Future investigations into the recurrence of polyposis and sinonasal edema should consider evaluating the effectiveness and compliance of sinonasal irrigation, topical corticosteroid use, oral steroid use, local drug delivery, and topical steroid rinses.
Several important limitations to this study are worth discussing. Variation in the prevalence of follow-up may introduce a potential source of selection bias as those patients who experience symptom resolution may be less likely to follow-up compared to patients with recurrence. This may overestimate the reported frequency of polyp recurrence. Alternatively, true recurrence may be greater since patients with polyposis relapse may either pursue treatment in other health systems or lose faith in current medical and surgical treatment methods to improve QOL. Regardless, even if every patient lost to follow-up did not experience recurrence of polyps and edema, the reported prevalence of recurrence indicates a significant need for improvement in surgical approach and/or postoperative therapy. Lastly, the semi-quantitative nature of LK endoscopy scoring may produce some degree of inter-rater or intra-rater discordance, however agreement for endoscopic attributes has been previously reported as “fair” for sinonasal edema (Kf=0.214) and “moderate” for sinonasal polyposis (Kf=0.693) within other patient populations.26
CONCLUSION
Endoscopic sinus surgery is an important treatment option for symptomatic medically recalcitrant patients with CRSwNP. Although long-term control of patient reported outcome measures is achieved in the majority of patients, endoscopic control of sinonasal inflammation is low with recurrent polyposis seen in approximately 40% of subjects 6-months after ESS. There has been no improvement in endoscopic polyp control in the last 10-years of ESS with concomitant medical therapy. No clinical risk factors predicted polyp recurrence except for previous ESS and preoperative polyposis severity. These findings highlight the need to clarify which surgical intervention is most appropriate for patients with recurrent CRSwNP as well as the need for innovative medical therapies to mitigate recurrence.
Acknowledgments
Financial Disclosures: Timothy L. Smith, Jess C. Mace, and Jeremiah A. Alt are supported by a grant for this investigation from the National Institute on Deafness and Other Communication Disorders (NIDCD), one of the National Institutes of Health, Bethesda, MD., USA (R01 DC005805; PI/PD: TL Smith). Public clinical trial registration (www.clinicaltrials.gov) ID# NCT01332136. This funding organization did not contribute to the design or conduct of this study; collection, management, analysis, or interpretation of the data; preparation, review, approval or decision to submit this manuscript for publication. Adam S. DeConde and Jeremiah A. Alt are consultants for IntersectENT, (Menlo Park, CA.). Adam S. DeConde is a consultant for Stryker Endoscopy (San Jose, CA.), and Jeremiah A. Alt is a consultant for Medtronic (Jacksonville, FL), neither of which are affiliated with this investigation. Luke Rudmik is a consultant for BioInspire (Peoria, AZ). There are no financial disclosures for Joshua M. Levy.
Footnotes
Potential Conflicts of Interest: None
References
- 1.Hopkins C, Gillett S, Slack R, Lund VJ, Browne JP. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin Otolaryngol. 2009;34(5):447–54. doi: 10.1111/j.1749-4486.2009.01995.x. [DOI] [PubMed] [Google Scholar]
- 2.Smith TL, Litvack JR, Hwang PH, et al. Determinants of Outcomes of Sinus Surgery: A Multi-Institutional Prospective Cohort Study. Otolaryngol Head Neck Surg. 2010;142(1):55–63. doi: 10.1016/j.otohns.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith TL, Kern R, Palmer JN, et al. Medical therapy vs surgery for chronic rhinosinusitis: a prospective, multi-institutional study with 1-year follow-up. Int Forum Allergy Rhinol. 2013;3(1):4–9. doi: 10.1002/alr.21065. [DOI] [PubMed] [Google Scholar]
- 4.Wu AW, Ting JY, Platt MP, Tierney HT, Metson R. Factors affecting time to revision sinus surgery for nasal polyps: a 25-year experience. Laryngoscope. 2014;124(1):29–33. doi: 10.1002/lary.24213. [DOI] [PubMed] [Google Scholar]
- 5.Hopkins C, Slack R, Lund V, Brown P, Copley L, Browne J. Long-term outcomes from the English national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Laryngoscope. 2009;119(12):2459–65. doi: 10.1002/lary.20653. [DOI] [PubMed] [Google Scholar]
- 6.Mendelsohn D, Jeremic G, Wright ED, Rotenberg BW. Revision rates after endoscopic sinus surgery: a recurrence analysis. Ann Otol Rhinol Laryngol. 2011;120(3):162–6. doi: 10.1177/000348941112000304. [DOI] [PubMed] [Google Scholar]
- 7.DeConde AS, Bodner TE, Mace JC, Alt JA, Rudmik L, Smith TL. Development of a clinically relevant endoscopic grading system for chronic rhinosinusitis using canonical correlation analysis. Int Forum Allergy Rhinol. 2016;6(5):478–85. doi: 10.1002/alr.21683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bassiouni A, Wormald P-J. Role of frontal sinus surgery in nasal polyp recurrence. Laryngoscope. 2013;123(1):36–41. doi: 10.1002/lary.23610. [DOI] [PubMed] [Google Scholar]
- 9.Smith TL, Mendolia-Loffredo S, Loehrl TA, Sparapani R, Laud PW, Nattinger AB. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2005;115(12):2199–205. doi: 10.1097/01.mlg.0000182825.82910.80. [DOI] [PubMed] [Google Scholar]
- 10.DeConde AS, Suh JD, Mace JC, Alt JA, Smith TL. Outcomes of complete vs targeted approaches to endoscopic sinus surgery. Int Forum Allergy Rhinol. 2015;5(8):691–700. doi: 10.1002/alr.21541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rudmik L, Soler ZM, Mace JC, DeConde AS, Schlosser RJ, Smith TL. Using preoperative SNOT-22 score to inform patient decision for Endoscopic sinus surgery. Laryngoscope. 2015;125(7):1517–22. doi: 10.1002/lary.25108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alt JA, Smith TL, Schlosser RJ, Mace JC, Soler ZM. Sleep and quality of life improvements after endoscopic sinus surgery in patients with chronic rhinosinusitis. Int Forum Allergy Rhinol. 2014;4(9):693–701. doi: 10.1002/alr.21364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lanza DC, Kennedy DW. Adult rhinosinusitis defined. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):S1–7. doi: 10.1016/S0194-59989770001-9. [DOI] [PubMed] [Google Scholar]
- 14.Rosenfeld RM, Andes D, Neil B, et al. Clinical practice guideline: Adult sinusitis. Otolaryngol Head Neck Surgery. 2007;137(3 suppl):S1–31. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- 15.Orlandi RR, Kingdom TT, Hwang PH, et al. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis. Int Forum Allergy Rhinol. 2016;6(Suppl 1):S22–209. doi: 10.1002/alr.21695. [DOI] [PubMed] [Google Scholar]
- 16.Lund VJ, Mackay IS. Staging in rhinosinusitus. Rhinology. 1993;31(4):183–4. [PubMed] [Google Scholar]
- 17.Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg. 1997;117(3 Pt 2):S35–40. doi: 10.1016/S0194-59989770005-6. [DOI] [PubMed] [Google Scholar]
- 18.Hosmer DW, Lemeshow S. Applied Logistic Regression. 2nd. Hoboken, NJ: John Wiley & Sons; 2000. [Google Scholar]
- 19.Wynn R, Har-El G. Recurrence rates after endoscopic sinus surgery for massive sinus polyposis. Laryngoscope. 2004;114(5):811–3. doi: 10.1097/00005537-200405000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Jankowski R, Pigret D, Decroocq F, Blum A, Gillet P. Comparison of radical (nasalisation) and functional ethmoidectomy in patients with severe sinonasal polyposis. A retrospective study. Rev Laryngol Otol Rhinol (Bord) 2006;127(3):131–40. [PubMed] [Google Scholar]
- 21.Ting JY, Wu A, Metson R. Frontal sinus drillout (modified Lothrop procedure): Long-term results in 204 patients. Laryngoscope. 2014;124(5):1066–70. doi: 10.1002/lary.24422. [DOI] [PubMed] [Google Scholar]
- 22.Naidoo Y, Bassiouni A, Keen M, Wormald PJ. Long-term outcomes for the endoscopic modified Lothrop/Draf III procedure: a 10-year review. Laryngoscope. 2014;124(1):43–9. doi: 10.1002/lary.24258. [DOI] [PubMed] [Google Scholar]
- 23.Cho D-Y, Hwang PH. Results of endoscopic maxillary mega-antrostomy in recalcitrant maxillary sinusitis. Am J Rhinol. 2008;22(6):658–62. doi: 10.2500/ajr.2008.22.3248. [DOI] [PubMed] [Google Scholar]
- 24.Soler ZM, Hwang PH, Mace J, Smith TL. Outcomes after middle turbinate resection: revisiting a controversial topic. Laryngoscope. 2010;120(4):832–7. doi: 10.1002/lary.20812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Videler WJM, van Drunen CM, van der Meulen FW, Fokkens WJ. Radical surgery: effect on quality of life and pain in chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2007;136(2):261–7. doi: 10.1016/j.otohns.2006.08.010. [DOI] [PubMed] [Google Scholar]
- 26.Raithatha R, Anand VK, Mace JC, et al. Interrater agreement of nasal endoscopy for chronic rhinosinusitis. Int Forum Allergy Rhinol. 2012;2(2):144–50. doi: 10.1002/alr.21009. [DOI] [PubMed] [Google Scholar]


