Abstract
Objectives
We sought to examine whether there are systematic differences in ascertainment of preexisting maternal medical conditions and pregnancy complications from three common data sources used in epidemiologic research.
Methods
Diabetes mellitus, chronic hypertension, gestational diabetes mellitus (GDM), gestational hypertensive disorders (GHD), placental abruption and premature rupture of membranes (PROM) among 4821 pregnancies were identified via birth certificates, maternal self-report at approximately 4 months postpartum and by discharge codes from the Statewide Planning and Research Cooperative System (SPARCS), a mandatory New York State hospital reporting system. The kappa statistic (k) was estimated to ascertain beyond chance agreement of outcomes between birth certificates with either maternal self-report or SPARCS.
Results
GHD was under-ascertained on birth certificates (5.7 %) and more frequently indicated by maternal report (11 %) and discharge data (8.2 %). PROM was indicated more on birth certificates (7.4 %) than maternal report (4.5 %) or discharge data (5.7 %). Confirmation across data sources for some outcomes varied by maternal age, race/ethnicity, prenatal care utilization, preterm delivery, parity, mode of delivery, infant sex, use of infertility treatment and for multiple births. Agreement between maternal report and discharge data with birth certificates was generally poor (kappa < 0.4) to moderate (0.4 ≤ kappa < 0.75) but was excellent between discharge data and birth certificates for GDM among women who underwent infertility treatment (kappa = 0.79, 95 % CI 0.74, 0.85).
Conclusions for Practice
Prevalence and agreement of conditions varied across sources. Condition-specific variations in reporting should be considered when designing studies that investigate associations between preexisting maternal medical and pregnancy-related conditions with health outcomes over the life-course.
Keywords: Birth certificates, Hospital discharge datasets, Maternal report, Pregnancy complications, Positive predictive value, Agreement, Infertility treatment
Introduction
Evidence linking preexisting maternal medical conditions and pregnancy complications with maternal and child health over the life-course (Malcolm 2012; Brown et al. 2013; Ray et al. 2001; Yeung et al. 2014) is fueling an interest to uncover their underlying causes and effects. Consequently, there is a demand for data sources that can accurately ascertain outcomes during pregnancy such as gestational diabetes, cardiovascular disease and hypertension. Common sources for preexisting medical conditions and pregnancy complications in epidemiological studies include maternal report, birth certificates and hospital discharge data.
Previous studies indicate that birth certificates, maternal self-report and hospital discharge data can underestimate the prevalence of preexisting maternal medical conditions and pregnancy complications (Lain et al. 2012; Roberts et al. 2008; Yasmeen et al. 2006). Reliability of these data sources can also vary by level of socio-demographic factors and/or the severity of the outcome of interest (e.g. pre-eclampsia) (Lain et al. 2012; Lydon-Rochelle et al. 2005; Rice et al. 2007; Coolman et al. 2010). A proposed strategy to improve the ascertainment of these outcomes is to combine information from various sources (i.e. birth certificates, hospital discharge data) (Lydon-Rochelle et al. 2005). Due to their availability and cost-effectiveness these data sources will remain widely used in research to describe trends or to identify risk factors of maternal and perinatal morbidity and mortality. Understanding and measuring the variability in the reporting of outcomes across data sources is needed (Ananth 2005; Kirby 2001) and can aid researchers considering potential systematic error while designing epidemiological studies for which multiple sources are not available.
The first aim of this study was to examine agreement among birth certificates, maternal self-report and hospital discharge data for the presence of preexisting maternal medical conditions and pregnancy complications in a population of women who delivered in New York State between July 2008 and May 2010. Second, since they are followed more thoroughly during pregnancy due to their increased risk, we also examined agreement of reporting of outcomes among women whose pregnancies were conceived via infertility treatment and pregnancies that resulted in multiple births. Lastly, we investigated if verification of reporting across sources differed by type of pregnancy (i.e. infertility treatment or multiple births) and other maternal factors.
Methods
Study Sample
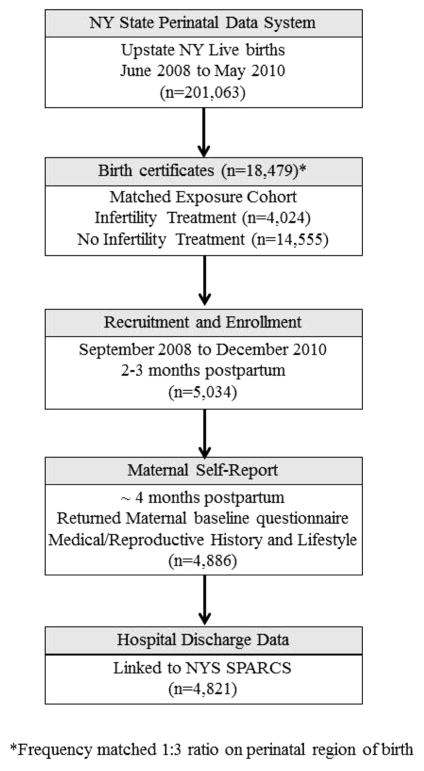
The Upstate KIDS Study is a matched exposure birth cohort focused on examining the association between infertility treatment and child development (Buck Louis et al. 2014) (Fig. 1). Briefly, birth certificates were used to identify a representative sample of live births conceived by infertility treatment from New York State (excluding the five boroughs of New York City) between July 2008 and May 2010. Singleton live births conceived with infertility treatment were then frequency matched on region (at 1:3 ratio) to a random sample of births conceived without infertility treatment. All twins and higher order multiples were also invited to enroll. Mothers were provided a baseline questionnaire at enrollment, including the option of a Spanish translation if they preferred. We excluded mothers from the current analysis if they were missing information from one of the data sources we examined. Of the 5034 mothers who enrolled, 4886 (97 %) returned the questionnaire and of these 4821 (99 %) mothers were also successfully linked to hospital discharge records. The linkage process has been previously described (Wang et al. 2011). Briefly, the NYS department of health assigns a four-digit Permanent Facility Identity (PFI) to hospitals and this in combination with the medical record number creates a unique identifier for which only 3 % of records remain unmatched. Women missing the maternal questionnaire (n = 148) did not differ in race/ethnicity, educational level, age or use of infertility treatment compared to those who returned a questionnaire. However, compared to questionnaire respondents, the pregnancies of non-respondents more frequently resulted in multiple births (22 vs. 33 %). The New York State Department of Health (NYSDOH) and the University of Albany Institutional Review Board (IRB) approved the study (NYSDOH IRB #07–097; University of Albany #08-179) and served as the IRB designated by the National Institutes of Health for this study under a reliance agreement. All participants provided written informed consent.
Fig. 1.
Flow chart of data linkage for study population
Data Sources
Electronic birth certificates were obtained from the New York Statewide Perinatal Data System, a maternal and newborn data collection and analysis system maintained by the NYSDOH. New York State also captures diagnoses from all inpatient, outpatient and emergency room visits via the Statewide Planning and Research Cooperative System (SPARCS). Pregnancy complications for obstetric patients delivering in New York State hospitals are reported to SPARCS using the International Classification of Disease, nineth Revision (ICD-9) codes. Up to 15 diagnoses could have been reported on hospital discharge summaries for pregnancies. A matching algorithm utilizing unique key personal identifiers (i.e. hospital identification number, maternal last name, date of discharge, date of admission, street address and zip code) was used to match birth certificates from the Upstate KIDS study population to maternal hospital discharge records in SPARCS. Upon enrollment, self-administered questionnaires were sent to query mothers on average 4 months postpartum regarding socio-demographic factors, medical and reproductive histories.
Assessment of Preexisting Maternal Medical Conditions and Pregnancy Complications
We examined agreement for conditions that were reported on birth certificates, by maternal self-report on questionnaires and identifiable through hospital discharge codes in a comparable manner; including two preexisting maternal medical conditions: diabetes mellitus and chronic hypertension; two pregnancy complications: gestational diabetes mellitus (GDM) and gestational hypertensive disorders (GHD); and two complications of labor and delivery: placental abruption and premature rupture of membranes (PROM). Given their comorbid nature, analyses for pregnancy complications or complications of labor and delivery are not mutually exclusive.
The presence of preexisting maternal medical conditions and pregnancy complications were identified by checkboxes on the birth certificate. If a check-box for a given outcome was marked, then the outcome was coded as being present, otherwise they were coded as absent. For mothers whose pregnancies resulted in multiple births and subsequently multiple birth certificates, we used the first birth certificate encountered in our dataset to ascertain pregnancy complications. Maternal diagnoses in hospital discharge data were ascertained by ICD-9 codes. Self-administered questionnaires prompted mothers to review a list of pregnancy complications followed by their brief descriptions. Mothers were asked to mark all complications diagnosed by a health care professional during the index pregnancy. Similarly, a medical history section required mothers to indicate preexisting chronic medical conditions. A list of ICD-9 codes and questionnaire responses used to identify outcomes can be found in Supplementary Table 1. We used contingency tables to verify that cases of GDM and GHD did not have concomitant indications of preexisting diabetes or chronic hypertension, respectively. To examine reporting of outcomes across levels of pregnancy and maternal factors, we grouped women according to whether conditions were identified among all three data sources, in two sources or only one.
Pregnancy and Maternal Factors
To examine the influence of maternal factors on the reporting of conditions, we obtained information on maternal age, race/ethnicity (Non-Hispanic Whites, Other) and education (≤ High School degree, Some Technical/College, College degree, Graduate/Professional degree), parity, prenatal care utilization via the Revised-Graduated Prenatal Care Utilization Index (R-GINDEX) (Alexander and Kotelchuck 2001) (≥ adequate prenatal care, inadequate prenatal care), infant’s sex, preterm delivery (yes/no), mode of delivery (spontaneous, cesarean, forceps/vacuum), infertility treatment, and multiple births from birth certificates. We chose to examine these factors because previous research has shown that they can affect the accuracy with which preexisting maternal chronic health conditions and pregnancy complications are reported (Lain et al. 2012; Zollinger et al. 2006; Northam and Knapp 2006; Reichman and Hade 2001). We dichotomized race/ethnicity for sufficient sample size to make comparisons as the majority of the cohort was non-Hispanic white. When covariate information such as maternal race/ethnicity was missing on the birth certificate we supplemented data using information from maternal questionnaires.
Statistical Analyses
Descriptive statistics were calculated to summarize socio-demographic factors of the study population. We present the overall frequency of preexisting maternal medical conditions and pregnancy complications by data source. We also present the overall frequency of outcomes stratified for groups who reported infertility treatment or whose pregnancies resulted in a multiple birth. Chi square tests of independence or analysis of variance were used to examine associations between pregnancy and maternal factors and the degree to which preexisting maternal medical conditions and pregnancy complications were confirmed (by number of data sources: all three, any two, only one). Our results did not differ when we examined confirmation of outcomes for only those women that had undergone infertility treatment or whose pregnancies resulted in multiple births (data not shown). We therefore present these results for the entire study population. These analyses were conducted using SAS 9.3.
The Upstate KIDS study oversampled birth certificates that reported infertility treatment or that resulted in multiples, two groups more likely to experience preexisting maternal chronic health conditions or pregnancy complications. To account for this sampling strategy and to avoid verification bias, we conditioned measures of agreement based on birth certificate report (Katki et al. 2012). Therefore, we used birth certificate data to determine the overall prevalence of outcomes in NYS (excluding New York City) during the study period, as well as for births conceived via infertility treatment or that resulted in multiple births. The prevalence of each preexisting maternal medical condition or pregnancy complication was used to create inverse probability weights to estimate agreement statistics and predictive values (Katki et al. 2012) for the overall study population and for women whose pregnancies resulted from infertility treatment or in multiples.
The kappa statistic (k) was estimated to ascertain beyond chance agreement of outcomes between birth certificates and maternal self-report or SPARCS. We used kappa values to designate agreement between sources as excellent (k ≥ 0.75), moderate (0.4 ≤ k < 0.75) or poor (k < 0.4) (Woodward 2014). To examine the proportion of preexisting maternal medical conditions and pregnancy complications that were or were not also identified by birth certificates, we estimated the positive (PPV) and negative predictive values (NPV), respectively for maternal self-report and SPARCS. NPVs were omitted from tables because as expected, NPVs for maternal self-report and for SPARCS were high (range 0.95–0.99). We calculated agreement, PPV and NPV estimates and their 95 % confidence intervals in R (R Development Core Team, http://www.R-project.org) using CompareTests (Katki and Edelstein 2011).
Results
Study Population and Prevalence of Preexisting Maternal Medical Conditions and Pregnancy Complications
Mothers that participated in study are described elsewhere (Buck Louis et al. 2014) and their characteristics are similar to those for which data were available for these analyses. Mothers were on average 30 years old (SD = 6.0) and predominately Non-Hispanic White (81 %). Fifty-one % reported having a college degree or higher, 26 % indicated the use of infertility treatment and 22 % gave birth to multiples (96 % twins). As expected, the frequency of preexisting maternal medical conditions and pregnancy complications appeared to be higher in groups whose pregnancies were conceived via infertility treatment or had multiple births (Table 1). These findings were observed regardless of data source.
Table 1.
Number and % of pregnancy complications identified by each data source and stratified by whether pregnancy resulted from infertility treatment or involved a multiple birth, Upstate KIDS, 2008–2010
| All participants (n = 4821)
|
Infertility treatment (n = 1271)
|
Multiples (n = 1063)
|
||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Birth certificates | ||||||
| Diabetes | 42 | 0.9 | 17 | 1.3 | 7 | 0.7 |
| Gestational diabetes | 323 | 6.7 | 109 | 8.6 | 74 | 7.0 |
| Chronic hypertension | 98 | 2.0 | 40 | 3.1 | 27 | 2.5 |
| Pregnancy related hypertensive disorders | 276 | 5.7 | 101 | 7.9 | 106 | 10.0 |
| Premature rupture of membranes | 356 | 7.4 | 113 | 8.9 | 110 | 10.3 |
| Placental abruption | 34 | 0.7 | 14 | 1.1 | 13 | 1.2 |
| Maternal report | ||||||
| Diabetes | 119 | 2.5 | 34 | 2.7 | 28 | 2.6 |
| Gestational diabetes | 370 | 7.7 | 118 | 9.3 | 94 | 8.8 |
| Chronic hypertension | 199 | 4.1 | 60 | 4.7 | 48 | 4.5 |
| Pregnancy related hypertensive disorders | 530 | 11.0 | 168 | 13.2 | 206 | 19.4 |
| Premature rupture of membranes | 217 | 4.5 | 71 | 5.6 | 96 | 9.0 |
| Placental abruption | 60 | 1.2 | 24 | 1.9 | 16 | 1.5 |
| SPARCSa | ||||||
| Diabetes | 52 | 1.1 | 17 | 1.3 | 11 | 1.0 |
| Gestational diabetes | 328 | 6.8 | 115 | 9.0 | 83 | 7.9 |
| Chronic hypertension | 134 | 2.8 | 49 | 3.9 | 35 | 3.3 |
| Pregnancy related hypertensive disorders | 396 | 8.2 | 128 | 10.1 | 151 | 14.4 |
| Premature rupture of membranes | 274 | 5.7 | 94 | 7.4 | 88 | 8.4 |
| Placental abruption | 54 | 1.1 | 21 | 1.7 | 22 | 2.1 |
Pregnancy complications are not mutually exclusive
The New York State Department of Health, Statewide Planning and Research Cooperative System
All conditions except for PROM were more frequently reported by mothers or recorded on discharge summaries than on birth certificates. This difference in prevalence was observed regardless of whether the pregnancy resulted from infertility treatment or involved a multiple birth. The frequency that mothers reported chronic hypertension and pregnancy related hypertensive disorders was approximately twice the number indicated by birth certificates (Table 1). In contrast, the frequencies of preexisting diabetes mellitus and gestational diabetes reported to SPARCS were similar to those reported on birth certificates.
Verification of Preexisting Maternal Medical Conditions and Pregnancy Complications for Pregnancies Conceived via Infertility Treatment, Multiple Births and Maternal Factors
Results suggest that the frequency with which conditions were confirmed (by all three, any two, or only one data source) differed by certain pregnancy and maternal factors (Tables 2, 3, 4). Except for GDM (Table 2), most conditions were identified only by one source and were not confirmed by other data sources (Tables 3, 4). We examined further the number and % of preexisting maternal medical conditions and pregnancy complications by data source for outcomes identified by any two or only one data source (see Supplement Table 2). Except for PROM, the majority (range 54–75 %) of preexisting maternal medical conditions and pregnancy complications identified by only one source were indicated by maternal report alone. Preexisting diabetes mellitus, GHD and chronic hypertension indicated by any two data sources were most often indicated by hospital discharge data and maternal report.
Table 2.
Number and % of gestational diabetes and preexisting diabetes mellitus identified among data sources by pregnancy and maternal characteristics, Upstate KIDS, 2008–2010
| Gestational diabetes (n = 469)
|
Preexisting diabetes mellitus (n = 148)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| All 3 | Any 2 | Only 1 | p value | All 3 | Any 2 | Only 1 | p value | |
| n (%) | 211 (45) | 130 (28) | 128 (27) | – | 23 (16) | 19 (13) | 106 (71) | – |
| Maternal race | ||||||||
| Non-hispanic white | 178 (48) | 106 (28) | 88 (24) | 0.002 | 18 (17) | 12 (11) | 77 (72) | 0.547 |
| Other | 33 (34) | 24 (25) | 40 (41) | 5 (12) | 7 (17) | 29 (71) | ||
| Maternal education | ||||||||
| ≤High school | 28 (13) | 30 (23) | 23 (18) | 0.262 | 5 (14) | 5 (14) | 25 (71) | 0.752 |
| Some technical/college | 79 (47) | 44 (26) | 45 (27) | 9 (16) | 10 (18) | 37 (66) | ||
| College | 50 (51) | 20 (21) | 27 (28) | 3 (14) | 1 (5) | 17 (81) | ||
| Graduate/professional | 54 (44) | 36 (29) | 33 (27) | 6 (17) | 3 (8) | 27 (75) | ||
| Parity | ||||||||
| 1 | 41 (43) | 28 (29) | 27 (28) | 0.818 | 12 (22) | 8 (15) | 34 (63) | |
| 2 | 68 (42) | 49 (31) | 44 (27) | 4 (14) | 5 (18) | 19 (68) | 0.095 | |
| 3+ | 38 (40) | 24 (26) | 32 (34) | 2 (6) | 2 (6) | 31 (88) | ||
| Prenatal care utilization | ||||||||
| ≥Adequate prenatal care | 180 (44) | 119 (29) | 112 (27) | 0.034 | 19 (15) | 15 (12) | 95 (74) | 0.977 |
| Inadequate prenatal care | 5 (36) | 1 (7) | 8 (57) | 1 (14) | 1 (14) | 5 (72) | ||
| Infertility treatment | ||||||||
| No | 133 (42) | 93 (29) | 94 (29) | 0.087 | 13 (12) | 14 (13) | 78 (75) | 0.253 |
| Yes | 78 (52) | 37 (25) | 34 (23) | 10 (23) | 5 (12) | 28 (65) | ||
| Multiple birth | ||||||||
| No | 163 (46) | 89 (25) | 103 (29) | 0.062 | 17 (15) | 16 (14) | 84 (71) | 0.714 |
| Yes | 48 (42) | 41 (36) | 25 (22) | 6 (19) | 3 (10) | 22 (71) | ||
| Infant’s sex | ||||||||
| Female | 104 (44) | 65 (27) | 68 (29) | 0.783 | 12 (17) | 8 (12) | 49 (71) | 0.799 |
| Male | 107 (46) | 65 (28) | 60 (26) | 11 (14) | 11 (14) | 57 (72) | ||
| Preterm delivery | ||||||||
| Yes | 60 (45) | 43 (32) | 30 (23) | 0.229 | 9 (27) | 6 (18) | 18 (55) | 0.040 |
| No | 151 (45) | 87 (26) | 98 (29) | 14 (12) | 13 (11) | 88 (77) | ||
| Mode of delivery | ||||||||
| Spontaneous | 96 (53) | 41 (23) | 43 (24) | 0.0568 | 7 (13) | 5 (9) | 44 (79) | 0.511 |
| Cesarean section | 109 (39) | 86 (31) | 83 (30) | 16 (18) | 14 (15) | 60 (67) | ||
| Forceps/vacuum | 5 (50) | 3 (30) | 2 (20) | 0 (0) | 0 (0) | 2 (100) | ||
| Maternal age (mean (SD)) | 32.3 (5) | 32.5 (6) | 31.6 (6) | 0.427 | 29.4 (6) | 32.7 (6) | 31.1 (6) | 0.219 |
Pregnancy complications are not mutually exclusive
Table 3.
Number and % of gestational hypertensive disorders and chronic hypertension identified among data sources by pregnancy and maternal characteristics, Upstate KIDS, 2008–2010
| Gestational hypertensive disorders (n = 693)
|
Chronic Hypertension (n = 278)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| All 3 | Any 2 | Only 1 | p value | All 3 | Any 2 | Only 1 | p value | |
| n (%) | 126 (18) | 257 (37) | 310 (45) | – | 48 (17) | 57 (21) | 173 (62) | – |
| Maternal race | ||||||||
| Non-hispanic white | 111 (19) | 207 (37) | 247 (44) | 0.107 | 39 (18) | 39 (18) | 133 (64) | 0.277 |
| Other | 15 (12) | 50 (39) | 63 (49) | 9 (13) | 18 (27) | 40 (60) | ||
| Maternal education | ||||||||
| ≤High school | 14 (11) | 46 (37) | 64 (52) | 0.271 | 6 (9) | 13 (20) | 46 (71) | 0.030 |
| Some technical/college | 43 (19) | 87 (39) | 94 (42) | 12 (12) | 19 (19) | 69 (69) | ||
| College | 27 (17) | 59 (38) | 71 (45) | 14 (27) | 10 (20) | 27 (53) | ||
| Graduate/professional | 42 (22) | 65 (35) | 81 (43) | 16 (26) | 15 (24) | 31 (50) | ||
| Parity | ||||||||
| 1 | 43 (23) | 72 (38) | 75 (39) | 0.011 | 10 (17) | 12 (21) | 36 (62) | 0.161 |
| 2 | 32 (18) | 50 (28) | 96 (54) | 17 (21) | 14 (17) | 51 (62) | ||
| 3+ | 12 (11) | 42 (38) | 57 (51) | 6 (8) | 21 (30) | 44 (62) | ||
| Prenatal care utilization | ||||||||
| ≥Adequate prenatal care | 112 (18) | 229 (37) | 276 (45) | 0.100 | 43 (17) | 51 (21) | 154 (62) | 0.877 |
| Inadequate prenatal care | 6 (40) | 4 (27) | 5 (33) | 1 (14) | 1 (14) | 5 (72) | ||
| Infertility treatment | ||||||||
| No | 74 (15) | 178 (37) | 227 (47) | 0.012 | 24 (13) | 42 (22) | 126 (65) | 0.007 |
| Yes | 52 (24) | 79 (37) | 83 (39) | 24 (28) | 15 (17) | 47 (55) | ||
| Multiple birth | ||||||||
| No | 79 (18) | 148 (34) | 206 (48) | 0.095 | 36 (17) | 41 (20) | 131 (63) | 0.849 |
| Yes | 47 (18) | 109 (42) | 104 (40) | 12 (17) | 16 (23) | 42 (60) | ||
| Infant’s sex | ||||||||
| Female | 57 (16) | 130 (37) | 164 (47) | 0.349 | 27 (19) | 29 (21) | 85 (60) | 0.683 |
| Male | 69 (20) | 127 (37) | 146 (43) | 21 (15) | 28 (20) | 88 (65) | ||
| Preterm delivery | ||||||||
| Yes | 44 (17) | 123 (46) | 99 (37) | 0.0004 | 16 (16) | 23 (23) | 60 (61) | 0.693 |
| No | 82 (19) | 134 (32) | 211 (49) | 32 (18) | 34 (19) | 113 (63) | ||
| Mode of delivery | ||||||||
| Spontaneous | 49 (19) | 91 (35) | 121 (46) | 0.631 | 14 (12) | 23 (20) | 77 (68) | 0.206 |
| Cesarean section | 74 (18) | 162 (39) | 180 (43) | 34 (21) | 34 (21) | 93 (58) | ||
| Forceps/vacuum | 2 (13) | 4 (27) | 9 (60) | 0 (0) | 0 (0) | 3 (100) | ||
| Maternal age (mean (SD)) | 31.4 (6) | 30.5 (7) | 30.9 (6) | 0.410 | 34.3 (5) | 33.4 (5) | 30.3 (7) | <0.0001 |
Pregnancy complications are not mutually exclusive
Table 4.
Number and % of placental abruption and premature rupture of membranes identified among data sources by pregnancy and maternal characteristics, Upstate KIDS, 2008–2010
| Placental abruption (n = 92)
|
Premature rupture of membranes (n = 574)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| All 3 | Any 2 | Only 1 | p value | All 3 | Any 2 | Only 1 | p value | |
| n (%) | 16 (17) | 24 (26) | 52 (57) | – | 41 (7) | 191 (33) | 342 (60) | – |
| Maternal race | ||||||||
| Non-hispanic white | 15 (19) | 21 (27) | 43 (54) | 0.521 | 38 (8) | 163 (35) | 260 (57) | 0.004 |
| Other | 1 (8) | 3 (23) | 9 (69) | 3 (3) | 28 (25) | 82 (72) | ||
| Maternal education | ||||||||
| ≤High school | 6 (25) | 6 (25) | 12 (50) | 0.326 | 3 (3) | 32 (30) | 73 (67) | 0.105 |
| Some technical/college | 2 (8) | 6 (25) | 16 (67) | 14 (8) | 57 (35) | 94 (57) | ||
| College | 3 (14) | 9 (41) | 10 (45) | 13 (10) | 51 (39) | 67 (51) | ||
| Graduate/professional | 5 (23) | 3 (14) | 14 (64) | 11 (6) | 51 (30) | 108 (64) | ||
| Parity | ||||||||
| 1 | 3 (18) | 2 (12) | 12 (70) | 0.131 | 11 (7) | 49 (31) | 98 (62) | 0.419 |
| 2 | 3 (9) | 13 (37) | 19 (54) | 10 (7) | 35 (24) | 100 (69) | ||
| 3+ | 6 (27) | 4 (18) | 12 (55) | 10 (11) | 28 (30) | 54 (59) | ||
| Prenatal care utilization | ||||||||
| ≥Adequate prenatal care | 16 (20) | 21 (26) | 43 (54) | 0.286 | 37 (8) | 162 (33) | 288 (59) | 0.612 |
| Inadequate prenatal care | 0 (0) | 0 (0) | 3 (4) | 1 (3) | 12 (36) | 20 (61) | ||
| Infertility treatment | ||||||||
| No | 10 (18) | 12 (21) | 35 (61) | 0.352 | 29 (7) | 118 (30) | 246 (63) | 0.051 |
| Yes | 6 (17) | 12 (34) | 17 (49) | 12 (7) | 73 (40) | 96 (53) | ||
| Multiple birth | ||||||||
| No | 11 (69) | 12 (50) | 40 (77) | 0.064 | 20 (5) | 126 (33) | 241 (62) | 0.017 |
| Yes | 5 (31) | 12 (50) | 12 (23) | 21 (11) | 65 (35) | 101 (54) | ||
| Infant’s sex | ||||||||
| Female | 14 (28) | 9 (18) | 27 (54) | 0.007 | 17 (6) | 100 (36) | 160 (58) | 0.310 |
| Male | 2 (4) | 15 (36) | 25 (60) | 24 (8) | 91 (31) | 182 (61) | ||
| Preterm delivery | ||||||||
| Yes | 14 (26) | 15 (27) | 26 (47) | 0.027 | 31 (12) | 102 (39) | 129 (49) | <0.0001 |
| No | 2 (5) | 9 (24) | 26 (71) | 10 (3) | 89 (29) | 213 (68) | ||
| Mode of delivery | ||||||||
| Spontaneous | 3 (11) | 6 (22) | 18 (67) | 0.484 | 16 (6) | 90 (32) | 176 (62) | 0.449 |
| Cesarean section | 12 (19) | 18 (29) | 33 (52) | 24 (9) | 94 (35) | 152 (56) | ||
| Forceps/vacuum | 1 (50) | 0 (0) | 1 (50) | 1 (5) | 6 (28) | 152 (67) | ||
| Maternal age (mean (SD)) | 32.1 (6) | 33.6 (5) | 31.6 (7) | 0.463 | 31.8 (5) | 30.6 (6) | 30.8 (6) | 0.507 |
Pregnancy complications are not mutually exclusive
The degree to which preexisting maternal medical conditions and pregnancy complications were confirmed with additional sources statistically differed across levels of maternal age, race/ethnicity, education, prenatal care utilization, preterm delivery, parity, infant’s sex, mode of delivery and infertility treatment (Tables 2, 3, 4). The differences observed were condition specific.
Agreement of Complications Between Birth Certificates and Maternal Report
Generally, for the total study population, agreement between birth certificates and maternal-self report for most preexisting maternal medical conditions and pregnancy complications was poor (0.26 ≤ k ≤ 0.36) (Table 5). However, moderate agreement between these two sources was observed for gestational diabetes (k = 0.63, 95 % CI 0.59, 0.67) and placental abruption (k = 0.42, 95 % CI 0.32, 0.52). In addition, except for PROM, if mothers reported a condition, the probability that it would be indicated on the birth certificate was high (0.62 ≤ PPV ≤ 0.75).
Table 5.
Agreement and positive predictive value among pregnancy complications derived from birth certificates by data source stratified by whether pregnancy resulted from infertility treatment or involved a multiple birth, Upstate KIDS, 2008–2010
| All Participants (n = 4821)
|
Infertility Treatment (n = 1271)
|
Multiple births (n = 1063)
|
||||
|---|---|---|---|---|---|---|
| k (95 % CI) | PPV (95 % CI) | k (95 % CI) | PPV (95 % CI) | k (95 % CI) | PPV (95 % CI) | |
| Maternal report | ||||||
| Diabetes | 0.26 (0.19, 0.32) | 0.62 (0.47, 0.75) | 0.40 (0.26, 0.54) | 0.65 (0.40, 0.83) | 0.37 (0.23, 0.50) | 0.86 (0.42, 0.98) |
| Gestational diabetes | 0.63 (0.59, 0.67) | 0.75 (070, 0.79) | 0.71 (0.65, 0.78) | 0.76 (0.67, 0.83) | 0.66 (0.58, 0.74) | 0.77 (0.66, 0.85) |
| Chronic hypertension | 0.31 (0.25, 0.36) | 0.62 (0.52, 0.71) | 0.33 (0.27, 0.38) | 0.76 (0.67, 0.84) | 0.30 (0.18, 0.43) | 0.48 (0.30, 0.66) |
| Pregnancy related hypertensive disorders | 0.36 (0.33, 0.40) | 0.75 (0.70, 0.94) | 0.52 (0.45, 0.59) | 0.76 (0.67, 0.83) | 0.43 (0.37, 0.49) | 0.79 (0.70, 0.86) |
| Premature rupture of membranes | 0.29 (0.24, 0.33) | 0.28 (0.23, 0.32) | 0.31 (0.22, 0.41) | 0.29 (0.22, 0.38) | 0.43 (0.35, 0.52) | 0.46 (0.37, 0.56) |
| Placental abruption | 0.42 (0.32, 0.52) | 0.68 (0.50, 0.81) | 0.62 (0.46, 0.77) | 0.79 (0.51, 0.92) | 0.42 (0.20, 0.64) | 0.46 (0.22, 0.72) |
| SPARCSa | ||||||
| Diabetes 0.48 (0.36, 0.59) | 0.31 (0.22, 0.41) | 0.63 (0.45, 0.81) | 0.65 (0.40, 0.83) | 0.69 (0.48, 0.90) | 0.88 (0.42, 0.98) | |
| Gestational diabetes | 0.72 (0.68, 0.76) | 0.78 (0.73, 0.82) | 0.79 (0.74, 0.85) | 0.83 (0.74, 0.86) | 0.71 (0.63, 0.79) | 0.77 (0.66, 0.85) |
| Chronic hypertension | 0.41 (0.35, 0.48) | 0.60 (0.50, 0.69) | 0.56 (0.45, 0.68) | 0.65 (0.49, 0.78) | 0.48 (0.34, 0.62) | 0.59 (0.40, 0.76) |
| Pregnancy related hypertensive disorders | 0.36 (0.32, 0.40) | 0.59 (0.53, 0.65) | 0.54 (0.47, 0.62) | 0.83 (0.74, 0.86) | 0.38 (0.30, 0.45) | 0.58 (0.48, 0.67) |
| Premature rupture of membranes | 0.38 (0.33, 0.43) | 0.39 (0.34, 0.44) | 0.39 (0.30, 0.48) | 0.40 (0.31, 0.49) | 0.35 (0.26, 0.44) | 0.37 (0.29, 0.47) |
| Placental abruption | 0.48 (0.37, 0.59) | 0.71 (0.53, 0.83) | 0.39 (0.30, 0.48) | 0.64 (0.38, 0.84) | 0.59 (0.42, 0.76) | 0.77 (0.48, 0.92) |
Pregnancy complications are not mutually exclusive PPV positive predictive value
The New York State Department of Health, Statewide Planning and Research Cooperative System
Agreement was higher among groups who reported the use of infertility treatment (n = 1271) or whose pregnancies resulted in multiple births (n = 1063). Preexisting maternal medical conditions and pregnancy complications reported by mothers who underwent infertility treatment were more likely to be indicated on birth certificates (0.65 ≤ PPV ≤ 0.79) than for other mothers. The highest PPVs for preexisting diabetes mellitus (PPV = 0.86, 95 % CI 0.42, 0.98), gestational diabetes (PPV = 0.77, 95 % CI 0.66, 0.85) and pregnancy related hypertensive disorders (PPV = 0.79, 95 % CI 0.70, 0.86) were observed among those who gave birth to multiples. However, for other conditions reported by mothers who gave birth to multiples, the probability they were indicated on the birth certificate was low (Table 5).
Agreement of Pregnancy Complications Between Birth Certificates and SPARCS
For the total study population, moderate agreement (0.41 ≤ k ≤ 0.72) was observed for most preexisting maternal chronic conditions and pregnancy complications between birth certificates and SPARCS. In general, agreement of conditions increased for women who underwent infertility treatment or whose pregnancies resulted in multiple births.
The probabilities that pregnancy complications reported to SPARCS were also indicated on birth certificates were generally high. However, some exceptions occurred. For example, the PPVs for PROM were low across groups (0.35 ≤ PPVs ≤ 0.39) (Table 5).
Discussion
We demonstrate in a NY state-wide birth cohort that the prevalence of preexisting maternal medical conditions and pregnancy complications can differ across commonly used epidemiologic data sources. In addition, pregnancy and maternal factors (e,g. maternal race/ethnicity, age, use of infertility treatment, plurality) were associated with differences in ascertainment and confirmation of complications across data sources. Agreement for maternal self-report and hospital discharge codes with birth certificates regarding the presence of complications was generally poor to moderate. Among groups who reported infertility treatment or whose pregnancies resulted in multiple births, agreement across sources tended to improve. Increases in kappa may be due to the greater prevalence of conditions among subgroups (22). These variations in reporting were condition-specific and should be considered when designing studies especially given recent recommendations to combine information from data sources to improve the ascertainment of outcomes (Lain et al. 2012; Lydon-Rochelle et al. 2005).
In general, previous studies support the use of birth certificates (DiGiuseppe et al. 2002; Vinikoor et al. 2010; Roohan et al. 2003), hospital discharge data (Lain et al. 2012; Yasmeen et al. 2006; Lydon-Rochelle et al. 2005) and maternal self-report (Troude et al. 2008; Buka et al. 2004; Bat-Erdene et al. 2013) as sources of information for pediatric and perinatal research given that their limitations are acknowledged and results interpreted accordingly. However, caution should be exercised when using these data as sole sources in research for identifying pre-existing maternal medical and pregnancy-related conditions. Our findings suggest that the likelihood that maternal report or hospital discharge data captured an outcome varies and is condition-specific. Also, for the conditions examined it appears that outcomes were reported less on birth certificates compared to hospital discharge data and/or by maternal report. A previous study conducted in Washington State (Lydon-Rochelle et al. 2005) found that compared against medical records as the gold standard, combining birth certificate and hospital discharge data resulted in higher true positive fractions. Researchers therefore concluded that combining birth certificate and hospital discharge data to identify conditions was superior to using one source alone. However, the true positive fractions (TPF) for birth certificate and hospital discharge data for gestational diabetes (TPF = 64.4, 95 % CI 49.7, 79.0), preexisting diabetes mellitus (52.2, 95 % CI 17.2, 87.1), chronic hypertension (47.1, 9 % CI 29.2, 65.0) and pregnancy-induced hypertension (48.6, 95 % CI 40.4, 56.7) varied.
A systematic review of ten epidemiological studies examining maternal recall of GHD concluded that the clinical utility of maternal report of these conditions was limited by low sensitivity and positive predictive values (Stuart et al. 2013). In examining the presence of recall bias, it was also shown that length of recall (48 h to 30 years) was not associated with sensitivity or specificity of maternal recall of gestational hypertension or preeclampsia. We found in particular, that the identification of some conditions such as PROM was poor for maternal report. However, for many of the outcomes examined, we found that among women whose conditions were only indicated by one source, maternal report was more often responsible for their identification. While maternal report has been shown to be limited for gestational hypertensive disorder (Stuart et al. 2013), maternal report should not be dismissed as a crucial source of information for other pregnancy outcomes.
These discrepancies in reporting may be attributed to several factors. Unless preexisting maternal medical conditions or other pregnancy-related conditions complicate delivery, they are not required elements for hospital discharge records and therefore are likely to be under-represented in hospital discharge summaries. Previous studies have also observed differential reporting of pregnancy complications and chronic conditions by socio-demographic and reproductive factors. For example, maternal recall of hypertensive disorder was found to vary by level of maternal education (Stuart et al. 2013). Moreover, some diagnoses, such as PROM may not be communicated to mothers in a comprehensible manner. Information on birth certificates has also varied by socio-demographic factors and rare events like pregnancy complications have been shown to be under-reported on birth certificates (Lydon-Rochelle et al. 2005). These factors may have also contributed to the observed discordance between sources in this study.
This study has several strengths and allowed us to examine the concordance of pregnancy complications across three common epidemiologic sources in general and among women who underwent infertility treatment or who gave birth to multiples. We also were able to examine changes in predictive values for pregnancy complications by combining information from birth certificates with both hospital discharge data and maternal self-report, a strategy that has been suggested in the literature to improve ascertainment of pregnancy complications for research (Lydon-Rochelle et al. 2005; Savitz et al. 2008; Gong et al. 2012; Campbell et al. 2013). While, other studies have shown low sensitivity of reporting of infertility treatment on birth certificates from Massachusetts (Se = 28.9 %) and Florida (Se = 41.4 %) (Cohen et al. 2014), we have found in the Upstate KIDS study that reporting of infertility treatment was high and concordant with birth certificates (Buck Louis et al. 2014). In addition, we have also shown that maternal report was highly sensitive (Se = 0.93) when validated using data obtained from the Society for Assisted Reproductive Technology Clinic Outcome Report System (SART CORS) (Buck Louis et al. 2015). The results of our study can help inform the design of epidemiologic studies that rely on these common administrative and subject-based data sources.
However, several limitations should be considered when interpreting the results of our study. Since we wanted to examine agreement across data sources in this study population, we were limited to examining those pregnancy complications and conditions for which comparable data were collected. Given the rarity of these complications, we may have lacked the power to detect how concordance of complications differed across categories of socio-demographic factors. For instance, the small number of cases required us to group all hypertensive disorders of pregnancy into one category. Furthermore, the majority of our study population was non-Hispanic White. Our study did not recruit from New York City which is more racially diverse but is under the purview of a separate department of health from the rest of the state. Given the race/ethnic characteristics of our study population and the rarity of some of the complications examined, our results should be cautiously generalized to areas with higher non-white/immigrant populations. For this study we were able to use statistical methods to correct for possible verification bias due to sampling framework by using CompareTests in R to adjust our estimates. While maternal questionnaires were created using questions available in the literature or from previous studies they were not formally pilot tested. Medical record data were not available for this study. Although medical records are often considered the gold standard in epidemiological studies of pregnancy outcomes, our sampling frame was birth certificates and we were limited to examining concordance using the birth certificate as the standard.
Differential reporting and -ascertainment of chronic disease during pregnancy and pregnancy related complications by pregnancy and maternal factors provide evidence that reporting of complications is nonrandom across data sources. Differential reporting of outcomes can be a significant source of bias in reproductive and perinatal epidemiological studies. As clinical epidemiologic research moves forward to examine the association between preexisting maternal medical conditions and pregnancy complications with maternal and child health over the life-course, it is essential for researchers to (1) clearly describe the data sources used in future research studies (2) attempt to select the most appropriate data to test a hypothesis and (3) consider how the sources of epidemiologic data that they use may impact their findings. Our results suggest that the reporting of maternal chronic disease and pregnancy related complications should ideally be augmented with data from another source even if it is from birth certificates, especially in cases where the condition (e.g. PROM) than others (e.g., GDM). We also provide evidence that common data sources may be adequate in identifying complications among groups followed more thoroughly during pregnancy, for example, births after infertility treatment.
In summary, a consensus exists among researchers that using more than one source for outcomes can improve ascertainment of pregnancy complications for research. However, our findings also echo the results of previous studies examining the agreement of multiple sources for perinatal health data. More often than not, sources provide discordant information and the degree of discordance can be nonrandom for some groups such as those undergoing infertility treatment. This cohort also allowed us to examine how reporting differs between sources among women who conceived using infertility treatment or experienced multiple births, groups for whom more comprehensive information on preexisting maternal medical and pregnancy-related conditions are needed.
Nonrandom and differential reporting of preexisting maternal medical conditions and pregnancy complications should be considered in studies attempting to ascertain the impact of these conditions with maternal and child health over the life-course. For researchers using multiple sources in which reporting can vary by socio-demographic and health factors, we recommend researchers provide a thorough description of data sources used, and the comparability of assessment methods when more than one group is being examined (von et al. 2008). Researchers should also attempt to conduct sensitivity analyses in an attempt to critically evaluate the impact that misclassification (Greenland 1996) or missing data (Sterne et al. 2009) could have on study results. We provide information that could inform sensitivity analyses on the magnitude of differential reporting for women who have undergone infertility treatment or had a multiple birth.
Supplementary Material
Significance.
Our findings suggest that the prevalence and agreement of maternal medical and pregnancy-related conditions (i.e., diabetes mellitus, chronic hypertension, gestational diabetes mellitus (GDM), pregnancy-related hypertensive disorders (PHD), placental abruption and premature rupture of membranes) vary when ascertained using birth certificates, maternal report and/or hospital discharge data. Our findings are relevant to epidemiologists and condition-specific variations in reporting should be considered when designing studies that investigate the impact of these conditions over the life-course. We also discuss practical strategies for designing studies of specific conditions.
Acknowledgments
This work was supported by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD; contracts #HHSN275201200005C, #HHSN267200700019C). We also would like to acknowledge and thank the Upstate KIDS families and staff for their important contributions.
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s10995-016-2177-8) contains supplementary material, which is available to authorized users.
Compliance with Ethical Standards
Conflict of Interest The authors declare no conflict of interest.
References
- Alexander GR, Kotelchuck M. Assessing the role and effectiveness of prenatal care: History, challenges, and directions for future research. Public Health Reports (Washington, DC: 1974) 2001;116(4):306–316. doi: 10.1016/S0033-3549(04)50052-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ananth CV. Perinatal epidemiologic research with vital statistics data: Validity is the essential quality. American Journal of Obstetrics and Gynecology. 2005;193(1):5–6. doi: 10.1016/j.ajog.2005.05.064. [DOI] [PubMed] [Google Scholar]
- Bat-Erdene U, Metcalfe A, McDonald SW, Tough SC. Validation of canadian mothers’ recall of events in labour and delivery with electronic health records. BMC Pregnancy and Childbirth. 2013;13(suppl 1):S3. doi: 10.1186/1471-2393-13-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown MC, Best KE, Pearce MS, Waugh J, Robson SC, Bell R. Cardiovascular disease risk in women with pre-eclampsia: Systematic review and meta-analysis. European Journal of Epidemiology. 2013;28(1):1–19. doi: 10.1007/s10654-013-9762-6. [DOI] [PubMed] [Google Scholar]
- Buck Louis GM, Hediger ML, Bell EM, Kus CA, Sundaram R, McLain AC, Yeung E, Hills EA, Thoma ME, Druschel CM. Methodology for establishing a population-based birth cohort focusing on couple fertility and children’s development, the Upstate KIDS Study. Paediatric and Perinatal Epidemiology. 2014;28(3):191–202. doi: 10.1111/ppe.12121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck Louis GM, Druschel C, Bell E, Stern JE, Luke B, McLain A, Sundaram R, Yeung E. Use of assisted reproductive technology treatment as reported by mothers in comparison with registry data: The Upstate KIDS study. Fertility and Sterility. 2015;103(6):1461–1468. doi: 10.1016/j.fertnstert.2015.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buka SL, Goldstein JM, Spartos E, Tsuang MT. The retrospective measurement of prenatal and perinatal events: Accuracy of maternal recall. Schizophrenia Research. 2004;71(2–3):417–26. doi: 10.1016/j.schres.2004.04.004. [DOI] [PubMed] [Google Scholar]
- Campbell KH, Savitz D, Werner EF, Pettker CM, Goffman D, Chazotte C, Lipkind HS. Maternal morbidity and risk of death at delivery hospitalization. Obstetrics and Gynecology. 2013;122(3):627–633. doi: 10.1097/AOG.0b013e3182a06f4e. [DOI] [PubMed] [Google Scholar]
- Cohen B, Bernson D, Sappenfield W, Kirby RS, Kissin D, Zhang Y, Copeland G, Zhang Z, Macaluso M. Accuracy of assisted reproductive technology information on birth certificates: Florida and Massachusetts, 2004–06. Paediatric and Perinatal Epidemiology. 2014;28(3):181–190. doi: 10.1111/ppe.12110. [DOI] [PubMed] [Google Scholar]
- Coolman M, de Groot CJ, Jaddoe VW, Hofman A, Raat H, Steegers EA. Medical record validation of maternally reported history of preeclampsia. Journal of Clinical Epidemiology. 2010;63(8):932–937. doi: 10.1016/j.jclinepi.2009.10.010. [DOI] [PubMed] [Google Scholar]
- DiGiuseppe DL, Aron DC, Ranbom L, Harper DL, Rosenthal GE. Reliability of birth certificate data: A multi-hospital comparison to medical records information. Maternal and Child Health Journal. 2002;6(3):169–179. doi: 10.1023/a:1019726112597. [DOI] [PubMed] [Google Scholar]
- Gong J, Savitz DA, Stein CR, Engel SM. Maternal ethnicity and pre-eclampsia in New York city, 1995–2003. Paediatric and Perinatal Epidemiology. 2012;26(1):45–52. doi: 10.1111/j.1365-3016.2011.01222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland S. Basic methods for sensitivity analysis of biases. International Journal of Epidemiology. 1996;25(6):1107–1116. [PubMed] [Google Scholar]
- Katki HA, Edelstein DW. Compare tests: Estimating agreement and diagnostic accuracy when one test is not conducted on all specimens. r package version 1 0. 2011 doi: 10.1002/sim.4422. Available from http://dceg.cancer.gov/bb/tools/CompareTests. [DOI] [PMC free article] [PubMed]
- Katki HA, Li Y, Edelstein DW, Castle PE. Estimating the agreement and diagnostic accuracy of two diagnostic tests when one test is conducted on only a subsample of specimens. Statistics in Medicine. 2012;31(5):436–448. doi: 10.1002/sim.4422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby RS. Invited commentary: Using vital statistics databases for perinatal epidemiology: does the quality go in before the name goes on? American Journal of Epidemiology. 2001;154(10):889–890. doi: 10.1093/aje/154.10.889. [DOI] [PubMed] [Google Scholar]
- Lain SJ, Hadfield RM, Raynes-Greenow CH, Ford JB, Mealing NM, Algert CS, Roberts CL. Quality of data in perinatal population health databases: A systematic review. Medical Care. 2012;50(4):e7–e20. doi: 10.1097/MLR.0b013e31821d2b1d. [DOI] [PubMed] [Google Scholar]
- Lydon-Rochelle MT, Holt VL, Cardenas V, Nelson JC, Easterling TR, Gardella C, Callaghan WM. The reporting of pre-existing maternal medical conditions and complications of pregnancy on birth certificates and in hospital discharge data. American Journal of Obstetrics and Gynecology. 2005;193(1):125–134. doi: 10.1016/j.ajog.2005.02.096. [DOI] [PubMed] [Google Scholar]
- Malcolm J. Through the looking glass: Gestational diabetes as a predictor of maternal and offspring long-term health. Diabetes/Metabolism Research and Reviews. 2012;28(4):307–311. doi: 10.1002/dmrr.2275. [DOI] [PubMed] [Google Scholar]
- Northam S, Knapp TR. The reliability and validity of birth certificates. Journal of Obstetric, Gynecologic, and Neonatal Nursing: JOGNN/NAACOG. 2006;35(1):3–12. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- Ray JG, Burrows RF, Burrows EA, Vermeulen MJ. MOS HIP: McMaster outcome study of hypertension in pregnancy. Early Human Development. 2001;64(2):129–143. doi: 10.1016/s0378-3782(01)00181-5. [DOI] [PubMed] [Google Scholar]
- Reichman NE, Hade EM. Validation of birth certificate data. A study of women in New Jersey’s healthstart program. Annals of Epidemiology. 2001;11(3):186–193. doi: 10.1016/s1047-2797(00)00209-x. [DOI] [PubMed] [Google Scholar]
- Rice F, Lewis A, Harold G, van den BM, Boivin J, Hay DF, Owen MJ, Thapar A. Agreement between maternal report and antenatal records for a range of pre and peri-natal factors: The influence of maternal and child characteristics. Early Human Development. 2007;83(8):497–504. doi: 10.1016/j.earlhumdev.2006.09.015. [DOI] [PubMed] [Google Scholar]
- Roberts CL, Bell JC, Ford JB, Hadfield RM, Algert CS, Morris JM. The accuracy of reporting of the hypertensive disorders of pregnancy in population health data. Hypertension in Pregnancy: Official Journal of the International Society for the Study of Hypertension in Pregnancy. 2008;27(3):285–297. doi: 10.1080/10641950701826695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roohan PJ, Josberger RE, Acar J, Dabir P, Feder HM, Gagliano PJ. Validation of birth certificate data in New York state. Journal of Community Health. 2003;28(5):335–346. doi: 10.1023/a:1025492512915. [DOI] [PubMed] [Google Scholar]
- Savitz DA, Janevic TM, Engel SM, Kaufman JS, Herring AH. Ethnicity and gestational diabetes in New York city, 1995–2003. BJOG: An International Journal of Obstetrics and Gynaecology. 2008;115(8):969–978. doi: 10.1111/j.1471-0528.2008.01763.x. [DOI] [PubMed] [Google Scholar]
- Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: Potential and Pitfalls. BMJ (Clinical Research ed) 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart JJ, Bairey Merz CN, Berga SL, Miller VM, Ouyang P, Shufelt CL, Steiner M, Wenger NK, Rich-Edwards JW. Maternal recall of hypertensive disorders in pregnancy: A systematic review. Journal of Women’s Health (2002) 2013;22(1):37–47. doi: 10.1089/jwh.2012.3740. [DOI] [PubMed] [Google Scholar]
- Szklo M, Nieto JF. Epidemiology: beyond the basics. Jones & Bartlett Publishers; 4 A.D. [Google Scholar]
- Troude P, L’Helias LF, Raison-Boulley AM, Castel C, Pichon C, Bouyer J, de La RE. Perinatal factors reported by mothers: Do they agree with medical records? European Journal of Epidemiology. 2008;23(8):557–564. doi: 10.1007/s10654-008-9268-9. [DOI] [PubMed] [Google Scholar]
- Vinikoor LC, Messer LC, Laraia BA, Kaufman JS. Reliability of variables on the North Carolina birth certificate: A comparison with directly queried values from a cohort study. Paediatric and Perinatal Epidemiology. 2010;24(1):102–112. doi: 10.1111/j.1365-3016.2009.01087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von EE, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Journal of Clinical Epidemiology. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Wang Y, Caggana M, Sango-Jordan M, Sun M, Druschel CM. Long-term follow-up of children with confirmed newborn screening disorders using record linkage. Genetics in Medicine: Official Journal of the American College of Medical Genetics. 2011;13(10):881–886. doi: 10.1097/GIM.0b013e31821e485b. [DOI] [PubMed] [Google Scholar]
- Woodward M. Epidemiology: study design and data analysis. Boca Raton, FL: Taylor and Francis Group, LLC; 2014. [Google Scholar]
- Yasmeen S, Romano PS, Schembri ME, Keyzer JM, Gilbert WM. Accuracy of obstetric diagnoses and procedures in hospital discharge data. American Journal of Obstetrics and Gynecology. 2006;194(4):992–1001. doi: 10.1016/j.ajog.2005.08.058. [DOI] [PubMed] [Google Scholar]
- Yeung E, Robledo C, Boghossian N, Zhang C, Mendola P. Developmental origins of cardiovascular disease. Current Epidemiology Reports. 2014;1:9–16. doi: 10.1007/s40471-014-0006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zollinger TW, Przybylski MJ, Gamache RE. Reliability of Indiana birth certificate data compared to medical records. Annals of Epidemiology. 2006;16(1):1–10. doi: 10.1016/j.annepidem.2005.03.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.