Abstract
Chronic inflammation contributes to a wide variety of human disorders. In the stomach, longstanding gastritis often results in structural alterations in the gastric mucosa, including metaplastic changes and gastric cancers. Therefore, it is important to elucidate factors that are involved in gastric inflammation. Nardilysin (N-arginine dibasic convertase; Nrdc) is a metalloendopeptidase of the M16 family that promotes ectodomain shedding of the precursor forms of various growth factors and cytokines by enhancing the protease activities of a disintegrin and metalloproteinase (ADAM) proteins. Here, we have demonstrated that Nrdc crucially regulates gastric inflammation caused by Helicobacter felis infection or forced expression of prostaglandin E2 in K19-C2mE mice. Metaplastic changes following gastric inflammation were suppressed by the deletion of Nrdc. Furthremore, the deletion of Nrdc significantly suppressed N-methyl-N-nitrosourea (MNU)-induced gastric tumorigenesis in the murine stomach. These data may lead to a global therapeutic approach against various gastric disorders by targeting Nrdc.
Chronic inflammation contributes to a wide variety of human disorders. In the stomach, most lifelong chronic gastritis is caused by Helicobacter pylori infection1, although other etiologies, such as non-steroidal anti-inflammatory drugs or autoimmunity, are also prevalent2. Longstanding gastritis can result in structural alterations in the gastric mucosa, including metaplastic changes and gastric cancers. Metaplastic changes in the stomach are associated with an increased risk of gastric cancer3. Therefore, it is important to elucidate factors that are involved in gastric inflammation for effective prevention of various gastric diseases, including gastric cancer4.
The local microenvironment influences the development of chronic gastritis and metaplastic changes regardless of causative factors, and inflammatory cytokines participate in constructing this environment. There are a number of factors regulating inflammatory cytokines. A disintegrin and metalloproteinase (ADAM) family proteins are involved in ectodomain shedding, and regulate the biological activities of structurally and functionally diverse inflammatory cytokines in a context-dependent manner5,6. Indeed, dysregulation of ectodomain shedding of those factors can be profoundly involved in the pathogenesis of a serial development of gastritis, metaplasia, and gastric cancer7.
Nardilysin (N-arginine dibasic convertase; NRDC), a zinc peptidase of the M16 family that selectively cleaves dibasic sites8, is diffusely localized in the cytoplasm, and is secreted to the cell surface by undetermined mechanisms9. We previously identified NRDC as a specific binding partner of heparin-binding epidermal growth factor-like growth factor (HB-EGF)10. NRDC also enhances the shedding of tumor necrosis factor-α (TNF-α) through activation of ADAM1711,12. TNF-α is produced as a membrane-anchored protein, shed from the cell surface by proteolytic cleavage, and subsequently activated. The proinflammatory genotype of TNF-α is associated with more than twice the risk of non-cardia gastric cancer13. In this respect, we previously demonstrated that NRDC regulates activation of TNF-α and subsequent production of inflammatory cytokines in gastric cancer cells14. These findings suggest that NRDC regulates chronic inflammation and tumorigenesis in the stomach; however, the in vivo role of NRDC in the stomach is still unclear.
In this study, we examined the role of Nrdc during the development of chronic gastritis and metaplastic changes in the stomach using Nrdc knockout mice. We also investigated the effect of Nrdc in chemically-induced gastric tumorigenesis.
Results
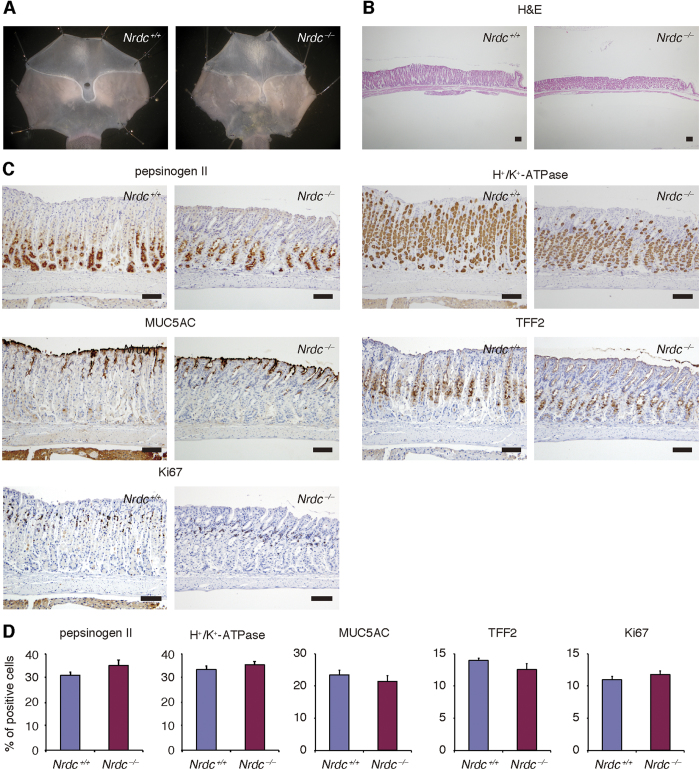
Nrdc did not alter the differentiation status of gastric mucosa under physiological conditions
We first examined the effects of Nrdc deletion in the stomach under physiological conditions. Nrdc−/− mice tend to maintain lower body weights than Nrdc+/+ mice15. Therefore, the mean stomach size of Nrdc−/− mice was slightly smaller than that of Nrdc+/+ mice (Fig. 1A). Other than the stomach size, there were no macroscopic differences between Nrdc+/+ and Nrdc−/− mice. Although the gastric mucosa was slightly thinner in Nrdc−/− mice (Fig. 1B), there were no significant differences in the differentiation status of gastric mucosal cells (Fig. 1C). Immunohistochemistry showed that the percentages of pepsinogen II-positive cells within gastric glands were not significantly different between Nrdc+/+ and Nrdc−/− mice. This indicated that chief cell differentiation was not affected by Nrdc status (Fig. 1C and D). Further, immunostainings for H+/K+-ATPase, Muc5ac, and TFF2 did not show significant differences between Nrdc+/+ and Nrdc−/− mice, indicating that differentiation of parietal, pit, and mucous neck cells was not regulated by Nrdc under physiological conditions, respectively (Fig. 1C and D). Furthermore, the proportion of Ki67-positive cells in the gastric glands of Nrdc−/− mice was similar to that of Nrdc+/+ mice. Therefore, deletion of Nrdc did not alter epithelial cell proliferation under physiological conditions (Fig. 1C and D).
Figure 1. Stomachs of Nrdc+/+ and Nrdc−/− mice under physiological conditions.
(A) Representative macroscopic views of the stomachs of Nrdc+/+ and Nrdc−/− mice. (B) H&E staining of Nrdc+/+ and Nrdc−/− mouse stomachs. Bars = 100 μm. (C) Immunohistochemistry for pepsinogen II, H+/K+-ATPase, Muc5ac, TFF2, and Ki67 in Nrdc+/+ and Nrdc−/− mice. Bars = 100 μm. (D) Percentages of epithelial cells immunostained with pepsinogen II, H+/K+-ATPase, Muc5ac, TFF2, and Ki67 in Nrdc+/+ and Nrdc−/− mice.
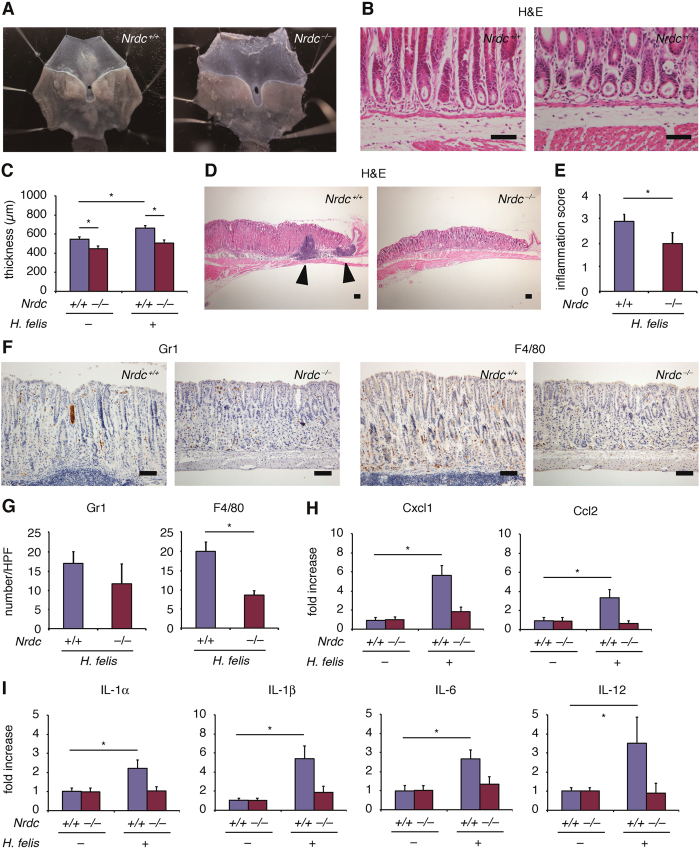
Gastritis caused by Helicobacter felis infection was attenuated by Nrdc deletion
Helicobacter felis infection is a well-characterized mouse model that mimics chronic Helicobacter pylori infection in the human stomach16. Based on a previous report16, we administered suspending water containing Helicobacter felis to Nrdc+/+ and Nrdc−/− mice for three days. Mice were sacrificed 20 weeks after the end of administration. Regardless of Nrdc gene status, Helicobacter felis was infected successfully into the gastric mucosae (Fig. 2A and B). The thickness of the mucosa of gastric corpus in Nrdc+/+ mice with Helicobacter felis infection was significantly different from mice without the infection, but was not significantly different from Nrdc−/− mice regardless of Helicobacter felis infection (Fig. 2C). Of note, formation of lymphoid follicles, a characteristic of Helicobacter felis infection, was scarce in Nrdc−/− mice (Fig. 2D), and the inflammation score was more severe in Nrdc+/+ than in Nrdc−/− mice with Helicobacter felis infection (Fig. 2E). Consistent with these findings, infiltration of Gr1-positive neutrophils was not prominent in Nrdc−/− mice, and that of F4/80-positive macrophages was significantly decreased compared to Nrdc+/+ mice (Fig. 2F and G). The mRNA expression of Cxcl1 and Ccl2, factors that recruit neutrophils and macrophages, respectively, was also decreased in Nrdc−/− mice (Fig. 2H). Notably, mRNA levels of interleukin (IL)-1α, IL-1β, IL-6, and IL-12, that can contribute to chronic gastritis in humans13,14,15,16,17, were not significantly increased in Nrdc−/− mice (Fig. 2I). Thus, the deletion of Nrdc attenuates gastric inflammation caused by Helicobacter infection.
Figure 2. Stomachs of Nrdc+/+ and Nrdc−/− mice infected with Helicobacter felis.
(A) Representative macroscopic views of the stomachs of Nrdc+/+ and Nrdc−/− mice infected with Helicobacter felis. (B) Detection of Helicobacter felis in the mucosae of Nrdc+/+ and Nrdc−/− mice. Note that Helicobacter felis is detected in gastric glands of both Nrdc+/+ and Nrdc−/− mice. Bars = 100 μm. (C) Mucosal thickness of Nrdc+/+ and Nrdc−/− mice with or without Helicobacter felis infection. (D) Formation of lymphoid follicle (arrowheads) in Nrdc+/+ and Nrdc−/− mouse gastric mucosae. Bars = 100 μm. (E) Inflammation scores of Nrdc+/+ and Nrdc−/− mouse gastric mucosae. *P < 0.05. (F) Immunohistochemistry for Gr1 and F4/80 in Nrdc+/+ and Nrdc−/− mice. Bars = 100 μm. (G) Number of epithelial cells immunostained for Gr1 and F4/80 in Nrdc+/+ and Nrdc−/− mice. *P < 0.05. (H) mRNA expression of Cxcl1 and Ccl2 in the gastric mucosae of Nrdc+/+ and Nrdc−/− mouse stomachs. (I) mRNA expression of IL-1α, IL-1β, IL-6, and IL-12 in the gastric mucosae of Nrdc+/+ and Nrdc−/− mouse stomachs. *P < 0.05.
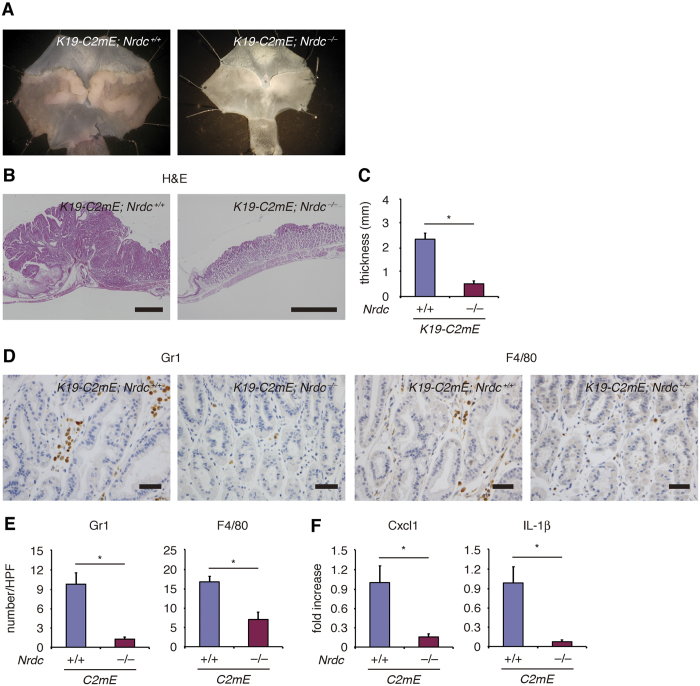
Gastritis caused by forced expression of prostaglandin (PG)E2 was attenuated by Nrdc deletion
We examined the role of Nrdc in K19-C2mE mice, another mouse model that expresses PGE2 abundantly in the gastric mucosa and mimics human gastritis16. Similar to Helicobacter felis–induced gastritis, mucosae of the gastric corpus of Nrdc+/+ mice were macroscopically thicker compared to Nrdc−/− mice at 30 weeks of age (Fig. 3A). Histologically, the mucosae of gastric corpus were remarkably hyperplastic in Nrdc+/+ mice, consistent with a previous report16. However, this hyperplastic change was not prominent in Nrdc−/− mice (Fig. 3B). Consequently, mucosae were significantly thinner in Nrdc−/− mice (Fig. 3C). Infiltration of Gr1-positive neutrophils and F4/80-positive macrophages was significantly decreased in Nrdc−/− mice compared to Nrdc+/+ mice (Fig. 3D and E). The expression of Cxcl1 and IL-1β mRNA was significantly decreased in Nrdc−/− mice compared to Nrdc+/+ mice (Fig. 3F), although we could not demonstrate alterations of Ccl2, IL-1α, IL-6, and IL-12 mRNA between Nrdc+/+ and Nrdc−/− mice in the presence of K19-C2mE alleles. Thus, like Helicobacter felis–induced gastritis, deletion of Nrdc attenuates gastric inflammation and hyperplasty caused by the forced expression of PGE2.
Figure 3. Gastritis caused by forced expression of prostaglandin E2.
(A) Representative macroscopic views of the stomachs of Nrdc+/+ and Nrdc−/− mice with forced expression of PGE2 by the insertion of K19-C2mE alleles. (B) H&E staining of Nrdc+/+ and Nrdc−/− mouse stomachs with forced expression of PGE2. Bars = 1000 μm. (C) Mucosal thickness of the Nrdc+/+ and Nrdc−/− mice with forced PGE2 expression. *P < 0.05. (D) Immunohistochemistry for Gr1 and F4/80 in Nrdc+/+ and Nrdc−/− mice. Bars = 100 μm. (E) Numbers of epithelial cells immunostained for Gr1 and F4/80 in Nrdc+/+ and Nrdc−/− mice. *P < 0.05. (F) mRNA expression of Cxcl1 and IL-1β in the gastric mucosae of Nrdc+/+ and Nrdc−/− mouse stomachs. *P < 0.05.
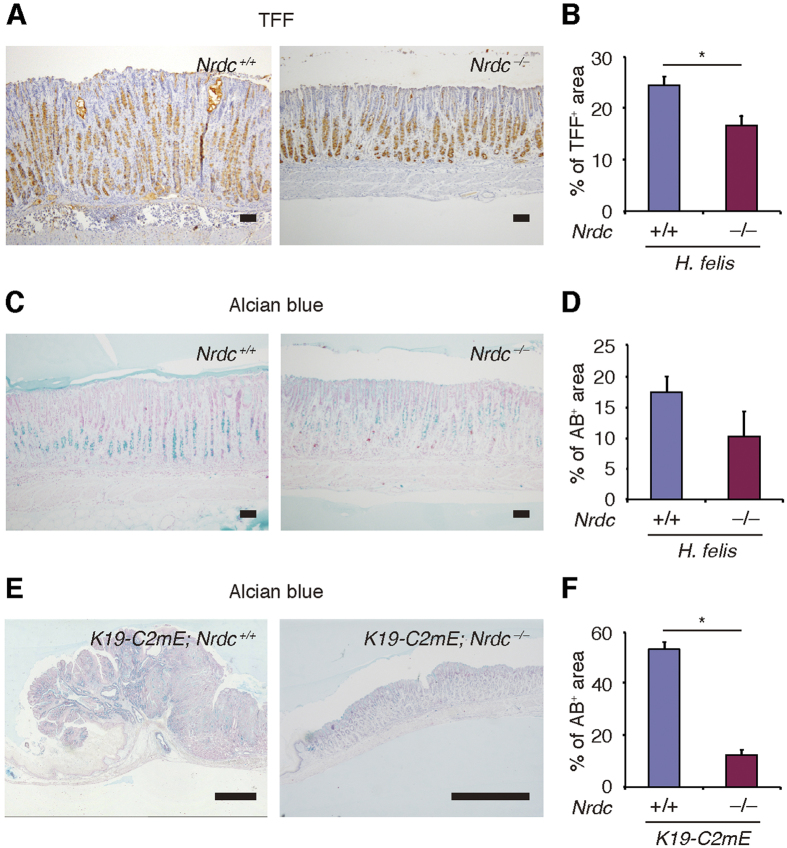
Metaplastic changes were attenuated by Nrdc deletion
We next investigated whether Nrdc plays a role in metaplastic changes following gastritis. Staining for TFF2 and/or staining with Alcian blue are widely used to detect metaplastic changes in the gastric corpus18. Upon Helicobacter felis infection for 20 weeks, the percentage of TFF2-stained cells was significantly lower in Nrdc−/− mice than in Nrdc+/+ mice (Fig. 4A and B). The percentage of Alcian blue-stained cells was also reduced in Nrdc−/− mice compared to Nrdc+/+ mice at 26 weeks of Helicobacter felis infection (Fig. 4C and D).
Figure 4. Metaplastic changes in Nrdc+/+ and Nrdc−/− mouse stomachs.
(A)Immunohistochemistry for TFF2 in Nrdc+/+ and Nrdc−/− mouse stomachs with Helicobacter felis infection. Bars = 100 μm. (B) Areas stained for TFF2 in Nrdc+/+ and Nrdc−/− mouse stomachs with Helicobacter felis infection. *P < 0.05. (C) Alcian blue staining of Nrdc+/+ and Nrdc−/− mouse stomachs with Helicobacter felis infection. Bars = 100 μm. (D) Areas stained with Alcian blue in Nrdc+/+ and Nrdc−/− mouse stomachs with Helicobacter felis infection. *P < 0.05. (E) Alcian blue staining of Nrdc+/+ and Nrdc−/− mouse stomachs with PGE2 expression. Bars = 1000 μm. (D) Areas stained with Alcian blue in Nrdc+/+ and Nrdc−/− mouse stomachs with forced PGE2 expression. *P < 0.05.
In K19-C2mE mice at the age of 30 weeks, Alcian blue staining showed that the development of metaplastic changes was significantly less prominent in Nrdc−/− mice compared with Nrdc+/+ mice (Fig. 4E and F). Together, these data indicate that the deletion of Nrdc leads to the suppression of metaplastic changes in the stomach.
Formation of gastric tumors was suppressed by Nrdc deletion
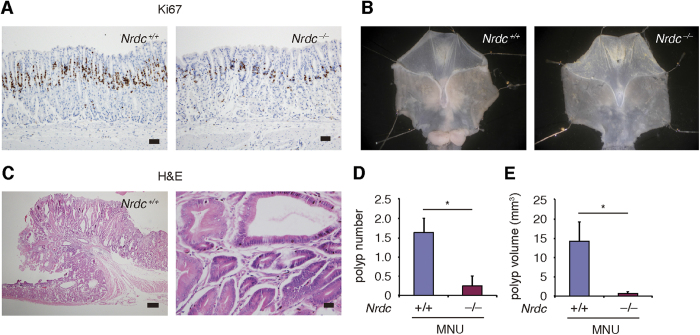
Chronic gastritis and metaplastic changes are associated with the development of gastric cancers. In both Helicobacter felis infection and the K19-C2mE chronic gastritis mouse models, we noticed that the increase in the number of Ki67-positive cells in the gastric glands of Nrdc+/+ mice was not remarkable in Nrdc−/− mice (Fig. 5A). Based on this finding, we hypothesized that the formation of gastric tumors may also be suppressed in Nrdc−/− mice. Because it requires a long period to develop tumors in Helicobacter felis-infected mouse stomach, we administered a chemical carcinogen to rapidly induce mouse gastric tumors. Administration of N-methyl-N-nitrosourea (MNU) causes polypoid tumors in the gastric antrum with inflammatory reactions in the stroma19,20,21. In Nrdc+/+ mice, MNU treatment resulted in polyp formation in the gastric antrum (Fig. 5B and C). In Nrdc−/− mice, the number and burden of gastric tumors was dramatically reduced compared with that in Nrdc+/+ mice (Fig. 5B,D and E). Thus, deletion of Nrdc attenuates gastric tumorigenesis induced by MNU.
Figure 5. Formation of gastric tumors in Nrdc+/+ and Nrdc−/− mouse stomachs.
(A) Ki67 immunostaining in Nrdc+/+ and Nrdc−/− mouse stomachs with the forced PGE2 expression. Bars = 50 μm. (B) Macroscopic views of the stomachs of Nrdc+/+ and Nrdc−/− mice treated with N-methyl-N-nitrosourea (MNU). (C) H&E staining of gastric tumor in Nrdc+/+ mouse. Bars = 200 μm (left) and 20 μm (right). (D) Polyp number in the stomachs of Nrdc+/+ and Nrdc−/− mice treated with MNU. *P < 0.05. (E) Polyp volume of Nrdc+/+ and Nrdc−/− mouse gastric tumors established by MNU treatment. *P < 0.05.
Discussion
In the present study, we demonstrated that Nrdc crucially regulates gastric inflammation caused by Helicobacter felis infection or forced expression of PGE2. Metaplastic changes following gastric inflammation were suppressed by the deletion of Nrdc. The deletion of Nrdc significantly suppressed chemically-induced tumorigenesis of the stomach.
Helicobacter pylori-induced gastritis is a primary inflammatory disorder of the human stomach, affecting about half of the global population1. Recent improvements in the hygienic environment have reduced the rate of Helicobacter pylori infection; however, other causative factors such as non-steroidal anti-inflammatory drugs or autoimmunity also contribute to the development of acute and chronic gastritis22. Regardless of the causative factors, chronic inflammation of the gastric mucosa can slowly progress to mucosal atrophy, induce metaplastic changes, and finally cause gastric cancer. In addition to the treatment of acute gastritis that may result in hemorrhagic complications, detection and therapeutic intervention in the early stages of the developmental cascade from chronic gastritis to gastric cancer is important. Therefore, it would be helpful to understand the molecular basis of chronic inflammation in the stomach.
Chronic inflammation is regulated by a feedback loop consisting of diverse inflammatory cytokines, and is closely associated with the recruitment of inflammatory cells in tissues. We previously demonstrated that the deletion of Nrdc critically suppresses ectodomain shedding, activation of TNF-α, and the production of other inflammatory cytokines in gastric cancer cells14. We also showed that the deletion of Nrdc significantly suppresses mouse steatohepatitis with attenuated inflammatory cytokine production and reduced infiltration of inflammatory cells23. Therefore, in this study, we examined the undetermined in vivo role of Nrdc during the developmental process of chronic gastritis, metaplastic changes, and gastric tumors.
To mimic chronic infection and inflammation in the human stomach caused by Helicobacter pylori, we used a Helicobacter felis-infected mouse model. Mucosae of the gastric corpus were thinner in Nrdc−/− than in Nrdc+/+ mice, and the inflammation score was less severe in Nrdc−/− mice. Infiltration of neutrophils and macrophages was decreased in Nrdc−/− mice concomitantly with attenuated expression of inflammatory cytokines. Although infiltration of inflammatory cells such as neutrophils may not be critical for the development of Helicobacter felis-induced gastritis24, this pattern of cytokine expression is consistent with our previous data obtained from a human gastric cancer cell line14. Notably, levels of IL-1α, IL-1β, IL-6, and IL-12, which are the main contributors to human chronic gastritis, were decreased in Nrdc−/− mice. Thus, the deletion of Nrdc attenuates gastric inflammation, indicating that Nrdc also plays a role in the intravital stomach. It is also important that the deletion of Nrdc attenuated inflammation caused by the forced expression of PGE2. This indicated that the deletion of Nrdc attenuates gastric inflammation regardless of the cause of inflammation, and a global therapeutic approach may be possible by targeting Nrdc.
We next questioned whether Nrdc plays a role in metaplastic changes and tumorigenesis. In Helicobacter felis-infected mice, metaplastic changes develop in the gastric corpus, and progress to mucous metaplasia that can be stained with Alcian blue25,26. In the present study, metaplastic changes induced by Helicobacter felis infection, or forced expression of PGE2, were significantly attenuated by the deletion of Nrdc. More importantly, gastric tumor formation was remarkably suppressed by the same genetic change. It is now becoming clear that the tumor microenvironment, which is orchestrated by inflammatory cells, is an indispensable participant during a wide-range of tumor developmental processes27.
Inflammation plays decisive roles at different stages of tumor development, including initiation, promotion, malignant conversion, invasion, and metastasis28. We previously reported that NRDC is highly expressed in the epithelium of human gastric cancer tissues14. Knockdown of NRDC attenuates gastric cancer cell growth both in vitro and in a xenograft model. These previous data showed that TNF-α secreted from gastric cancer cells themselves initiates a feedback loop to enhance inflammatory cytokine expression.
As for the pivotal role of Nrdc in vivo, we previously showed in a mouse steatohepatitis model that the production of inflammatory cytokines and recruitment of inflammatory cells are significantly suppressed concomitantly with the suppression of TNF-α release by the deletion of Nrdc23. Although we did not again examined the shedding status of TNF-α in mouse stomach in the present study, the remarkable suppressive effect of Nrdc deletion on inflammation may lead to the suppression of metaplastic changes and tumor formation. In this respect, it is worth noting that metaplastic changes were detected in Nrdc−/− mice, albeit milder than in Nrdc+/+ mice, and that gastric tumor formation was almost completely blocked in Nrdc−/− mice. This discrepancy indicates a possibility that formation of gastric tumors by MNU treatment requires inflammatory responses, and that metaplastic changes may be regulated at least partly by factors other than Nrdc. To determine the exact mechanisms underlying how Nrdc coordinates inflammation, metaplastic changes, and tumor formation, further studies are required. However, the findings obtained in available studies, including the current work, suggest that a global therapeutic approach against various gastric disorders may be possible by targeting NRDC.
Methods
Animal models
Generation of the Nrdc knockout mouse with a CBA background was described previously15. Animals were housed under specific pathogen-free conditions at the Animal Facilities of Kyoto University. All animal experiments were performed in accordance with institutional guidelines. The Review Board of Kyoto University granted ethical permission for this study, and The Kyoto University Animal Experimentation Committee approved the experimental protocol. For the infection by Helicobacter felis, suspending water containing Helicobacter felis was gavaged to Nrdc+/+ and Nrdc−/− mice for three days according to the previous report16. K19-C2mE mice were generated as previously described16. To analyze chemically-induced gastric tumorigenesis, mice at the age of 6 weeks were administered MNU (Sigma-Aldrich, St. Louis, MO, USA) in drinking water at 240 ppm on alternate weeks for five weeks as described previously19.
Histological and immunohistochemical analyses
Mouse stomach was resected, fixed in 4% buffered paraformaldehyde solution, embedded in paraffin, and cut into sections 5-μm thick. For immunostaining, the sections were incubated overnight with the primary antibodies at 4 °C, after which the secondary antibodies were added. The primary antibodies used were rat anti-F4/80 (Abcam, Cambridge, MA, USA), rat anti–Gr-1 (eBioscience, San Diego, CA, USA), sheep anti-pepsinogen II (Abcam), mouse anti-H+/K+-ATPase α subunit (MBL, Nagoya, Japan), mouse anti-Muc5AC (Abcam), mouse-anti-spasmolytic polypeptide (TFF2) (R&D Systems, Minneapolis, MN, USA), and rat anti-Ki67 (Dako, Glostrup, Denmark). All immunohistochemical analyses were performed with immunoglobulin isotype controls. For Alcian blue staining, deparaffinized sections were incubated with Alcian blue solution for 30 minutes, followed by counterstaining with Nuclear Fast Red. To determine the differentiation status of the gastric mucosa under physiological conditions, stained cells were counted in 10 randomly selected gastric glands per mouse in 6 Nrdc+/+ and 4 Nrdc−/− mice. In Helicbacter felis infection experiments, we used 12 Nrdc+/+ and 6 Nrdc−/− mice. In addition, 6 Nrdc+/+; K19-C2mE and 3 Nrdc−/−; K19-C2mE mouse samples were subjected to the analyses. Using these mice, to analyze histology and count inflammatory cells, eight high power field sections from each mouse were selected randomly. To investigate gastric tumorigenesis, 12 Nrdc+/+ and 6 Nrdc−/− mice were treated with MNU. Inflammation scores were determined according to the previous report24.
Real-time quantitative reverse transcription-polymerase chain reaction (qRT-PCR)
Total RNA was extracted using Trizol (Life Technologies, Carlsbad, CA, USA). Single-strand complementary DNA was synthesized using a First Strand SYBR Green Master Mix (Roche Applied Science, Basel, Switzerland). qRT-PCR was performed using FastStart SYBR Green Master (Roche Applied Science) and the LightCycler 480 system (Roche Applied Science). Values are expressed as arbitrary units relative to the expression of glyceraldehyde 3-phosphate dehydrogenase (GAPDH) expression. The primer sets used were: interleukin (IL)-1α-forward, CTGATGAAGCTCGTCAGGCAG; IL-1α-reverse, TGGTGCTGAGATAGTGTTTGTC; IL-1β-forward, GCAACTGTTCCTGAACTCAACT; IL-1β-reverse, ATCTTTTGGGGTCCGTCAACT; IL-6-forward, TAGTCCTTCCTACCCCAATTTCC; IL6-reverse, TTGGTCCTTAGCCACTCCTTC; IL-12-forward, ACTCTGCGCCAGAAACCTC; IL-12-reverse, CACCCTGTTGATGGTCACGAC; Cxcl1-forward, CTGGGATTCACCTCAAGAACATC; Cxcl1-reverse, CAGGGTCAAGGCAAGCCTC; Ccl2-forward, ATCCACGGCATACTATCAACATC; Ccl2-reverse, CAAGGCTCACCATCATCGTAG; Gapdh-forward, AGGTCGGTGTGAACGGATTTG; and Gapdh-reverse, TGTAGACCATGTAGTTGAGGTCA. In each experiment, 3–6 samples were subjected to the reactions.
Statistical analyses
Results are expressed as means ± standard error unless stated otherwise. Differences between treatments, groups, and strains were analyzed by the two-tailed Student’s t-test.
Additional Information
How to cite this article: Kimura, Y. et al. Nardilysin regulates inflammation, metaplasia, and tumors in murine stomach. Sci. Rep. 7, 43052; doi: 10.1038/srep43052 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
This work was supported in part by Grants-in-Aid KAKENHI (25112707, 26293068, 26293173, 26116715, 16K09394, 16K15216, 16K15427, 16K15216) and a research program of the Project for Development of Innovative Research on Cancer Therapeutics (P-Direct) from the Ministry of Education, Culture, Sports, Science and Technology/the Japan Society for the Promotion of Science. It was also supported by Health Labour Sciences Research Grants from the Ministry of Health, Labour and Welfare (The development of innovative therapeutic drug for the intractable inflammatory bowel disease/Comprehensive Research on Lifestyle-Related Diseases including Cardiovascular Diseases and Diabetes Mellitus); the Kobayashi Foundation for Cancer Research; the Naito Foundation; Princess Takamatsu Cancer Research Fund 13-24514; the Takeda Science Foundation; the Uehara Memorial Foundation.
Footnotes
The authors declare no competing financial interests.
Author Contributions Y.K., E.N., and H.S. designed the studies and wrote the manuscript; Y.K. and K.I. performed experiments and were involved in data analysis; H.O. and M.O. provided essential materials; T.K. and T.C. supervised all studies.
References
- Pounder R. E. & Ng D. The prevalence of Helicobacter pylori infection in different countries. Aliment Pharmacol Ther. 9, Suppl 2, 33–39 (1995). [PubMed] [Google Scholar]
- Nishiura H. et al. Interleukin-21 and tumor necrosis factor-α are critical for the development of autoimmune gastritis in mice. J Gastroenterol Hepatol. 28, 982–991 (2013). [DOI] [PubMed] [Google Scholar]
- Choi E., Hendley A. M., Bailey J. M., Leach S. D. & Goldenring J. R. Expression of Activated Ras in Gastric Chief Cells of Mice Leads to the Full Spectrum of Metaplastic Lineage Transitions. Gastroenterology 150, 918–930 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J. G. & Wang T. C. Inflammation, atrophy, and gastric cancer. J Clin Invest. 117, 60–69 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blobel C. P. ADAMs: key components in EGFR signalling and development. Nat Rev Mol Cell Biol. 6, 32–43 (2005). [DOI] [PubMed] [Google Scholar]
- Seals D. F. & Courtneidge S. A. The ADAMs family of metalloproteases: multidomain proteins with multiple functions. Genes Dev. 17, 7–30 (2003). [DOI] [PubMed] [Google Scholar]
- Murphy G. The ADAMs: signalling scissors in the tumour microenvironment. Nat Rev Cancer. 8, 929–941 (2008). [DOI] [PubMed] [Google Scholar]
- Pierotti A. R. et al. N-arginine dibasic convertase, a metalloendopeptidase as a prototype of a class of processing enzymes. Proc Natl Acad Sci USA 91, 6078–6082 (1994). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hospital V. et al. N-arginine dibasic convertase (nardilysin) isoforms are soluble dibasic-specific metalloendopeptidases that localize in the cytoplasm and at the cell surface. Biochem J. 349, 587–597 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishi E., Prat A., Hospital V., Elenius K. & Klagsbrun M. N-arginine dibasic convertase is a specific receptor for heparin-binding EGF-like growth factor that mediates cell migration. EMBO J. 20, 3342–3350 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishi E., Hiraoka Y., Yoshida K., Okawa K. & Kita T. Nardilysin enhances ectodomain shedding of heparin-binding epidermal growth factor-like growth factor through activation of tumor necrosis factor-alpha-converting enzyme. J Biol Chem. 281, 31164–31172 (2006). [DOI] [PubMed] [Google Scholar]
- Hiraoka Y. et al. Ectodomain shedding of TNF-alpha is enhanced by nardilysin via activation of ADAM proteases. Biochem Biophys Res Commun. 370, 154–158 (2008). [DOI] [PubMed] [Google Scholar]
- El-Omar E. M. et al. Increased risk of noncardia gastric cancer associated with roinflammatory cytokine gene polymorphisms. Gastroenterology 124, 1193–1201 (2003). [DOI] [PubMed] [Google Scholar]
- Kanda K. et al. Nardilysin and ADAM proteases promote gastric cancer cell growth by activating intrinsic cytokine signalling via enhanced ectodomain shedding of TNF-α. EMBO Mol Med. 4, 396–411 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohno M. et al. Nardilysin regulates axonal maturation and myelination in the central and peripheral nervous system. Nat Neurosci. 12, 1506–1513 (2009). [DOI] [PubMed] [Google Scholar]
- Oshima H. et al. Prostaglandin E2 signaling and bacterial infection recruit tumor-promoting macrophages to mouse gastric tumors. Gastroenterology 140, 596–607 (2011). [DOI] [PubMed] [Google Scholar]
- Yuzhalin A. The role of interleukin DNA polymorphisms in gastric cancer. Hum Immunol. 72, 1128–1136 (2011). [DOI] [PubMed] [Google Scholar]
- Hoffmann W. TFF2, a MUC6-binding lectin stabilizing the gastric mucus barrier and more. Int J Oncol. 47, 806–816 (2015). [DOI] [PubMed] [Google Scholar]
- Yamachika T. et al. N-methyl-N-nitrosourea concentration-dependent, rather than total intake-dependent, induction of adenocarcinomas in the glandular stomach of BALB/c mice. Jpn J Cancer Res. 89, 385–91 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsukamoto T., Mizoshita T. & Tatematsu M. Animal models of stomach carcinogenesis. Toxicol Pathol. 35, 636–648 (2007). [DOI] [PubMed] [Google Scholar]
- Leung W. K. et al. Transgenic cyclooxygenase-2 expression and high salt enhanced susceptibility to chemical-induced gastric cancer development in mice. Carcinogenesis 29, 1648–1654 (2008). [DOI] [PubMed] [Google Scholar]
- Hirschowitz B. I. Nonsteroidal antiinflammatory drugs and the gastrointestinal tract. Gastroenterologist. 2, 207–223 (1994). [PubMed] [Google Scholar]
- Ishizu-Higashi S. et al. Deletion of nardilysin prevents the development of steatohepatitis and liver fibrotic changes. PLoS One 29, e98017 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A. B. Histologic scoring of gastritis and gastric cancer in mouse models. Methods Mol Biol. 921, 189–203 (2012). [DOI] [PubMed] [Google Scholar]
- Fox J. G. et al. Hypertrophic gastropathy in Helicobacter felis-infected wild-type C57BL/6 mice and p53 hemizygous transgenic mice. Gastroenterology 110, 155–166 (1996). [DOI] [PubMed] [Google Scholar]
- Wang T. C. et al. Mice lacking secretory phospholipase A2 show altered apoptosis and differentiation with Helicobacter felis infection. Gastroenterology 114, 675–689 (1998). [DOI] [PubMed] [Google Scholar]
- Coussens L. M. & Werb Z. Inflammation and cancer. Nature 420, 860–867 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grivennikov S. I., Greten F. R. & Karin M. Immunity, inflammation, and cancer. Cell. 140, 883–899 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]