Abstract
Background:
The aim of this study was to validate the Farsi version of Rome III modular questionnaire which contains all functional gastrointestinal disorders (FGIDs).
Materials and Methods:
We used Rome foundation guidelines for translation of English version into Farsi, and all the steps were performed. In the first step, 2 forward translations into Farsi were completed by two authors separately, and then translators, who participated in Step 1, together with our monitor, compared the two target-language versions and made some changes. The product of Phase 2 was translated back into English by an American-Iranian physician. The final step was comparison of the two English versions and validation of the translation. In this step, we compared the final version item by item, and also we used focus groups of patients after pretesting.
Results:
Our results showed that FGIDs questionnaire diagnosed 153 patients among 169 patients who were diagnosed to have different types of FGIDs. The sensitivity of this questionnaire was 90.5%. It was determined that the odd questions' values of Cronbach’s alpha was 0.77 (very reliable), and it was 0.71 (very reliable) in other sections. The split-half test reliability of whole items value was 0.72, which is statistically significant.
Conclusion:
Our findings showed that the Farsi version of Rome III diagnostic questionnaire for the adult functional gastrointestinal disorders demonstrated good validity and reliability and could be used in clinical studies.
Keywords: Farsi, functional gastrointestinal disorders, Iran, Rome III criteria, validity
INTRODUCTION
Functional gastrointestinal disorders (FGIDs) are a class of gastrointestinal (GI) disorders that include different chronic and/or recurrent GI symptoms. Irritable bowel syndrome (IBS) and functional dyspepsia (FD) are the most common disorders between these categories, which are diagnosed using Rome III criteria.[1] FGIDs are not be explained by the structural or biochemical abnormalities. There are no specific objective findings in FGIDs, and we can observe a lot of overlaps between these disorders. Therefore, these entities are defined as syndromes such as IBS.[2,3]
Dyspeptic symptoms are seen in organic diseases such as reflux esophagitis, gastroduodenal ulcer, and malignancy. However, dyspepsia without organic causes is more prevalent in individuals seeking medical care.[4]
There are completely different epidemiologic reports about FGIDs. For example, the incidence of gastroesophageal reflux was reported from 0.05% to 4.3% and from 0.8% to 10.3% for dyspepsia and from 0.2% to 10% for IBS.[2]
A meta-analysis which is published in 2004 determined that frequency of dyspepsia was 10–40; however, this frequency was 5–12% when they exclude concurrent symptoms such as heartburn. Diagnostic criteria in this study included Rome II which is published in 1999; in Rome II criteria, symptoms of reflux were excluded from the diagnostic criteria of FD, and when IBS symptoms were present, FD was diagnosed as IBS.[5,6]
The prevalence of FD in the general population using Rome III criteria which is published in 2006 has been reported to be 5.3–20.4%.[6]
In a systematic review which is published in 2002, the prevalence of IBS was reported 3–20%, but the most estimates range was from 10% to 15%.[7]
Japanese studies determined that the prevalence of IBS defined by Rome II was 6.1–35.5%; other reports based on Rome III criteria revealed that the prevalence of IBS was 1.1–29.2%.[6]
Miwa used both Rome III and Rome II criteria for diagnosis of IBS patients; the prevalence of IBS was 13.1% using Rome III criteria and 9.8% using Rome II criteria. The author determined that Rome III criteria was more sensitive for diagnosis of IBS patients and it is a better tool for picking up more masked IBS cases.[8]
Diagnosis of FGIDs is based on self-reported symptoms, and definition of the symptoms may be varying by countries and geographic areas and these are culture-based symptoms.[9]
Drossman declared that Rome foundation introduced a standard for the classification and diagnosis of the FGIDs which is called the Rome criteria. A series of documents were published in 1990s and it was eventually compiled as a book in 1994. Rome criteria were then updated as Rome II criteria in 2000 and their final update was published in 2006 as Rome III. Rome III criteria were published due to different explanations such as availability of new data from scientific progress, the advent of new drugs, the necessity to develop new therapies, and the shift of paradigm in medical conceptualization.[10]
There are four major differences between Rome II and Rome III criteria: change of chronological criteria, changes in classification categories, creation of two pediatric categories, and criteria changes.[10]
Rome III criteria were used in many epidemiologic and clinical studies worldwide in different languages.[11]
A cross-cultural research in FGIDs is a term which is used in epidemiologic studies, for example, in comparative reports of IBS prevalence in different countries. The validity of these comparisons was a methodological challenge in research studies. In addition to epidemiologic studies, cross-cultural studies can make a great contribution in areas such as molecular studies, genetics, psychosocial factors, symptom presentation, comorbid diseases, diagnosis, and treatment which can be influenced by culture, ethnicity, and race.[12]
The goal of this study was to validate the Rome III Diagnostic Questionnaire in Farsi, as a base for future research in Iran.
MATERIALS AND METHODS
This study was designed to determine the validity and reliability of the Farsi version of Rome III diagnostic questionnaire for the adult functional GI disorders. There are different methods for determining the validity and reliability of questionnaires;[13] in this study, we used Rome foundation guidelines.
Rome III diagnostic questionnaire for the adult functional
This is a self-report questionnaire which is designed to determine FGIDs based on Rome III criteria. Questionnaire was developed by expert gastroenterologists in the Rome Foundation Board and it is designed for clinical practice and research. This questionnaire contains 93 questions including esophagus, stomach and intestines, gall bladder or pancreas, rectum or anal canal, and questions about other symptoms. Response format of this questionnaire includes four types: Yes or no format, a 5- or 7-point Likert scale, and a few other response scales.
Questionnaire translation
We used Rome foundation guidelines for translation of English version into Farsi and all the steps were performed and approved by the Rome foundation.
The first step was forward translation; in this step, 2 forward translations into Farsi were completed by two authors separately. The next step was reconciliation; in this step, translators who participated in Step 1, together with our monitor (who is introduced by the Rome foundation), compared the two target-language versions and made some changes. The third step was backward translation; product of Phase 2 was translated back into English by an American–Iranian physician. The final step was comparison of the two English versions and validation of the translation. In this step, we compared the final version item by item. There were seven small changes needed in the Farsi version to be made to have a more correct and clear questionnaire after this comparison and also we used focus groups of patients after pretesting.
Study design
A total of 193 individuals were accepted to participate in the research project who were able to communicate verbally in Fars and all of them were older than 18 years.
Patients were requested to fill a data collection form and Farsi version of Rome III criteria questionnaire. Finally, 24 participants were excluded from the study due to incomplete forms. Diagnosis of FGIDs was established by a single gastroenterology specialist who was accepted as the gold standard.
Internal consistency
Test–retest was performed for the internal consistency of the questionnaire, and the item-total correlation and Cronbach’s alpha reliability coefficient (which is an indicator for internal consistency and homogeneity) were determined.
We assessed and calculated the contribution of each question of the questionnaire to the alpha coefficient and the value of Cronbach’s alpha of the questionnaire was determined by item-total correlation analysis when each item was omitted.
Internal consistency was calculated by split-test analysis. The correlation between the two semi-consistent analyses of the test was calculated by dividing the questionnaire half and half. Cronbach’s alpha values were calculated as 47 questions for the first half (odd numbers) and 46 questions (even numbers) for the second half. Information was entered into the Statistical Package for the Social Sciences (SPSS v. 20) software (SPSS Inc., Chicago, IL, USA) and analyzed.
RESULTS
We enrolled 169 patients to this study. The mean age of the patients was 38.24 ± 8.37 years, 60.9% (103 participants) were female and 39.1% (66 participants) were male. Our results determined that FGID questionnaire diagnosed 153 patients among 169 patients who were diagnosed to have different types of FGIDs. The sensitivity of this questionnaire was 90.5%.
Internal consistency
The applied scale was divided into two parts including 47 (odd numbers of questionnaire) and 46 questions (even numbers of questionnaire), and the odd questions were compared with the even questions.
It was determined that the odd questions' values of Cronbach’s alpha was 0.77 (very reliable), and it was 0.71 (very reliable) in other section. If we omit 7 questions (3 from odd and 4 from even groups), Cronbach’s Alpha will be 0.81 versus 0.77. The split-half test reliability of whole items value was 0.72, which is statistically significant [Table 1 summarized internal consistency findings].
Table 1.
Cronbach's alpha of Rome III criteria
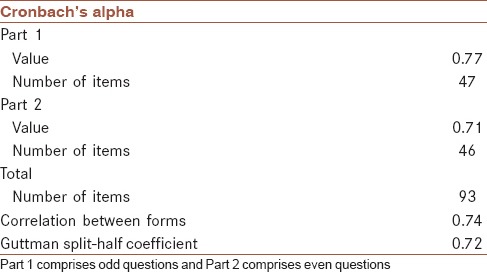
Cronbach’s alpha coefficient was approximately +1.00, which indicates that the internal consistency of this 93-item questionnaire was high. In addition, this coefficient evaluation determined that the Farsi version of Rome III questionnaire has a homogeneous structure.
DISCUSSION
Farsi version of Rome III diagnostic questionnaire for the adult functional GI disorders was translated into Farsi, and we used the guidelines recommended by the Rome foundation for this process, and finally, the translated questionnaire was reviewed and approved by the Rome foundation.
As it was mentioned in the results section, the split-half test reliability of whole items value was 0.72, which is statistically significant. The results of the current study determined that the Farsi version of Rome III diagnostic questionnaire for the adult functional GI disorders is a valid and reliable instrument in Iran, which indicates that it can be used in clinical research studies.
Uran et al. in 2014 designed a study to determine the validity and reliability of the Turkish version of Rome III criteria for IBS. Cronbach’s alpha of the questionnaire was calculated as 0.90 in their study. IBS questionnaire is a summarized form of Rome III diagnostic questionnaire for the adult functional GI disorders with same questions.[14]
Reisswitz et al. reported that Portuguese version of Rome III Diagnostic Questionnaire for FD is a valid tool. This questionnaire contains 18 questions. They enrolled 109 patients to their study who answered to their questionnaire. Cronbach’s α coefficient was 0.79.[15]
Kanazawa et al. enrolled 49 patients with IBS patients and 32 patients with FD to check the Japanese version of Rome III diagnostic questionnaire for IBS and FD. Finally, they reported that the IBS and FD diagnostic modules on the Japanese version of Rome III diagnostic questionnaire are valid and reliable tools.[16]
Ghoshal et al. designed a study to determine development, translation, and validation of enhanced Asian Rome III questionnaires (EAR3Qs) for the diagnosis of functional bowel diseases in major Asian languages. EAR3Q was developed by the Asian experts following Rome foundation guidelines. EAR3Q was translated into Chinese, Indian (Hindi and Telugu), Indonesian, Korean, and Thai. They reported that Chinese, Hindi, and Telugu translations were performed well but Korean and Indonesian versions were not.[16]
According to our findings and previous reports, Rome III criteria are a sensitive and specific tool with a high predictive value and because of these characteristics the compliance between the Rome III criteria and the gastroenterologist is very good.
CONCLUSION
Our findings show that the Farsi version of Rome III diagnostic questionnaire for the adult functional GI disorders demonstrated good validity and reliability and could be used in clinical studies.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors have no conflicts of interest.
AUTHORS’ CONTRIBUTION
AT carried out the design, coordinated the study, participated in most of the experiments, and prepared the manuscript. IM carried out the design and participated in most of the experiments. HA provided assistance in the design of the study, coordinated, and participated in manuscript preparation. AK carried out all the experiments and participated in manuscript preparation. All authors have read and approved the content of the manuscript.
Acknowledgments
The authors would like to thank Prof. Peyman Adibi and Dr. Ehsan Kheradmand for their assistance in this study.
REFERENCES
- 1.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377–90. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Adibi P, Behzad E, Shafieeyan M, Toghiani A. Upper functional gastrointestinal disorders in young adults. Med Arh. 2012;66:89–91. doi: 10.5455/medarh.2012.66.89-91. [DOI] [PubMed] [Google Scholar]
- 3.Adibi P, Mazdak H, Derakhshandeh A, Toghiani A. Change in functional bowel symptoms after prostatectomy: A case-control study. J Res Med Sci. 2011;16:130–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Emami MH, Arjmandpour A, Daghaghzadeh H, Rahimi H, Toghiani A, Adibi P. Adding diclofenac to Helicobacter pylori eradication regimen. Adv Biomed Res. 2015;4:143. doi: 10.4103/2277-9175.161551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.El-Serag HB, Talley NJ. Systemic review: The prevalence and clinical course of functional dyspepsia. Aliment Pharmacol Ther. 2004;19:643–54. doi: 10.1111/j.1365-2036.2004.01897.x. [DOI] [PubMed] [Google Scholar]
- 6.Oshima T, Miwa H. Epidemiology of functional gastrointestinal disorders in Japan and in the world. J Neurogastroenterol Motil. 2015;21:320–9. doi: 10.5056/jnm14165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saito YA, Schoenfeld P, Locke GR., 3rd The epidemiology of irritable bowel syndrome in North America: A systematic review. Am J Gastroenterol. 2002;97:1910–5. doi: 10.1111/j.1572-0241.2002.05913.x. [DOI] [PubMed] [Google Scholar]
- 8.Miwa H. Prevalence of irritable bowel syndrome in Japan: Internet survey using Rome III criteria. Patient Prefer Adherence. 2008;2:143–7. [PMC free article] [PubMed] [Google Scholar]
- 9.Koloski NA, Jones M, Young M, Talley NJ. Differentiation of functional constipation and constipation predominant irritable bowel syndrome based on Rome III criteria: A population-based study. Aliment Pharmacol Ther. 2015;41:856–66. doi: 10.1111/apt.13149. [DOI] [PubMed] [Google Scholar]
- 10.Drossman DA, Dumitrascu DL. Rome III: New standard for functional gastrointestinal disorders. J Gastrointestin Liver Dis. 2006;15:237–41. [PubMed] [Google Scholar]
- 11.Adibi P, Keshteli AH, Esmaillzadeh A, Afshar H, Roohafza H, Bagherian-Sararoudi R, et al. The study on the epidemiology of psychological, alimentary health and nutrition (SEPAHAN): Overview of methodology. J Res Med Sci. 2012;17:S291–7. [Google Scholar]
- 12.Reisswitz PS, Mazzoleni LE, Sander GB, Francisconi CF. Portuguese validation of the Rome III diagnostic questionnaire for functional dyspepsia. Arq Gastroenterol. 2010;47:354–60. doi: 10.1590/s0004-28032010000400007. [DOI] [PubMed] [Google Scholar]
- 13.Maleki I, Taghvaei T, Barzin M, Amin K, Khalilian A. Validation of the Persian version of the inflammatory bowel disease questionnaire (IBDQ) in ulcerative colitis patients. Caspian J Intern Med. 2015;6:20–4. [PMC free article] [PubMed] [Google Scholar]
- 14.Ozgürsoy Uran BN, Vardar R, Karadakovan A, Bor S. The Turkish version of the Rome III criteria for IBS is valid and reliable. Turk J Gastroenterol. 2014;25:386–92. doi: 10.5152/tjg.2014.4774. [DOI] [PubMed] [Google Scholar]
- 15.Kanazawa M, Nakajima S, Oshima T, Whitehead WE, Sperber AD, Palsson OS, et al. Validity and reliability of the Japanese version of the Rome III diagnostic questionnaire for irritable bowel syndrome and functional dyspepsia. J Neurogastroenterol Motil. 2015;21:537–44. doi: 10.5056/jnm15016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghoshal UC, Gwee KA, Chen M, Gong XR, Pratap N, Hou X, et al. Development, translation and validation of enhanced Asian Rome III questionnaires for diagnosis of functional bowel diseases in major Asian languages: A Rome Foundation-Asian Neurogastroenterology and Motility Association working team report. J Neurogastroenterol Motil. 2015;21:83–92. doi: 10.5056/jnm14045. [DOI] [PMC free article] [PubMed] [Google Scholar]


