Abstract
Background:
The objective of this study was an investigation of the association between depression and sleep quality.
Materials and Methods:
This cross-sectional study was performed on 360 delivered women that referred to thirty health-care centers in Ardabil, Iran. The Standard Pittsburgh Sleep Quality Index questionnaire was used to the investigation of sleep quality. We used the Edinburgh Postnatal Depression Questionnaire to assess postpartum depression. Logistic regression was used to examine the association of sleep quality with postpartum depression.
Results:
Chance of depression in women with poor sleep quality was 3.34 times higher than those with good sleep quality (odds ratio = 3.34; 95% confidence interval: 2.04–5.48; P < 0.001). After controlling for some risk factors, an association observed between sleep quality and depression in postpartum women.
Conclusion:
we found an association between sleep quality in women who had given birth in the last 3 months and symptoms of postpartum depression.
Keywords: Postpartum depression, pregnancy, sleep quality
INTRODUCTION
Postpartum depression with symptoms such as anxiety, depressed mood, forgetfulness, and irritability is similar to depression in other periods of life,[1] but its incidence is three times more in the first 5 weeks after delivery.[2] Postpartum depression has serious consequences on the quality of life of the mothers and their children. It can also seriously affect the quality of the relationship between the mother and her newborn baby[3] as well as damage the emotional, cognitive, motor, and behavioral development of the growing baby.[4] According to several studies conducted in Iran, the prevalence of postpartum depression varies from 15.5%[5] to 37.7%.[6] Some factors such as socioeconomic factors, maternal age, education and sex of the infant,[7] previous history of depression, occupation, and number of children[8,9] were reported to be effective in the development of postpartum depression. Sleep patterns and sleep deprivation are other potential factors which can be associate with postpartum depression.[10] Delivery has physical, physiological, and psychological effects on women's sleep, also taking care of a newborn with irregular sleep patterns will result in sleep disturbances during the postpartum period[11] and women in the postpartum period experience high levels of sleep disturbances, especially in the first three postpartum months.[12] On the other hand, insufficient and disrupted sleep affects memory, decision-making, psychomotor, and mood.[13,14] The association between depression and sleep can be bilateral. Depression may lead to disturbed sleep while sleep disorder can also be an independent risk factor for depression. The association between sleep status and depression may result from a neurological or psychological function which is similar in both cases.[15,16] The previous studies showed sleep quality was associated with postpartum depression.[17,18]
Because of the high prevalence of depression in this region and their serious side effects of this disorder and the limited number of studies which have been done on relation with sleep quality, we aimed to investigate the association between postpartum depression and sleep quality to add cross-cultural understandings of prenatal sleep and mental health.
MATERIALS AND METHODS
Study design and participants
This was a cross-sectional study that was performed on a representative sample of 360 delivered women attending thirty health-care centers in Ardabil, Iran in 2012. We included subjects who had delivered in the last 3 months and had a live birth. Delivered women with the previous history of self-reported depression and other psychiatric disorders were excluded from the study. Participants were selected based on a systematic random sampling method. After preparing the list of eligible individuals in each health-care center, subjects were sorted based on the date of their delivery. The sampling starts by selecting a recorded number from the list at random and then, every fourth recorded number in the frame was selected.
Study instrument and variables assessment
Required data were collected from participants through their medical records such as age, education, type of delivery, the interval of the previous delivery, occupation, sex of the infant, birth order, physical activity, height and weight before pregnancy. Other information collected from the questionnaires including the Standard Pittsburgh Sleep Quality Index (PSQI), Food Frequency Questionnaire (FFQ), and Edinburgh Postnatal Depression Questionnaire (EPDS).
The PSQI questionnaire was used for assessing sleep quality. The questionnaire is consisted of nine questions, and the fifth question contains 10-items. On the whole, the questions contain 18-items which can be classified into seven components which asses the seven aspects of sleep during the last 1 month of pregnancy including sleep quality, sleep onset latency, sleep duration, sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each component has a score range of 0–3 and the total score scale varies from 0 to 21. A total score of 5 or greater is indicative of poor sleep quality. The sensitivity and specificity of the questionnaire have been reported as 98.7% and 84.4%, respectively.[19]
For calculation of energy intake, a 106-item Willett-format dish-based semi-quantitative FFQ that was specifically designed for the Iranian adults was used to assess usual dietary intakes of study subjects throughout their pregnancy.[20]
EPDS was used to assess postpartum depression. It is a 10-item self-report scale, with four response categories for each item, ranging from a score of 0 (no presence of the symptom) to 3 (marked presence or change). The global score of the questionnaire is between 0 and 30. Those who scored 13 or more were considered as depressed delivered women. Validity and reliability of the questionnaire have been reported earlier. The questionnaire has a sensitivity of 78%, specificity of 75%, and reliability of 0.79.[21]
After the selection of the sample from the list of eligible women, subjects were called by trained staff from the health-care centers and then, the objectives of the study were explained to them in detail. We explained to the participants that there is no obligation to participate in the study. In addition, questionnaires were distributed anonymously.
The present study was approved by the Ethics Committee of Isfahan University of Medical Sciences, Isfahan, Iran (research number 392078).
Statistical analysis
SPSS software (version 18, PASW Statistics for Windows, Chicago: SPSS Inc.) was used for data analysis. Continuous variables were expressed as means ± standard deviation. For initial analysis, the Student's t-test was used to determine statistical differences in continuous variables between the two groups (depressed and nondepressed also qualified and nonqualified sleep). The nonparametric Mann–Whitney U-test was used if appropriate. Categorical variables were examined using Chi-square test and finally to examine the association of sleep quality with postpartum depression (as a binomial independent variable), we applied the logistic regression model controlling for age, physical activity, education, house owner, body mass index (BMI), sex of the infant, child order, delivery type, and total energy. P values were two-tailed and <0.05 was taken as a significance level.
RESULTS
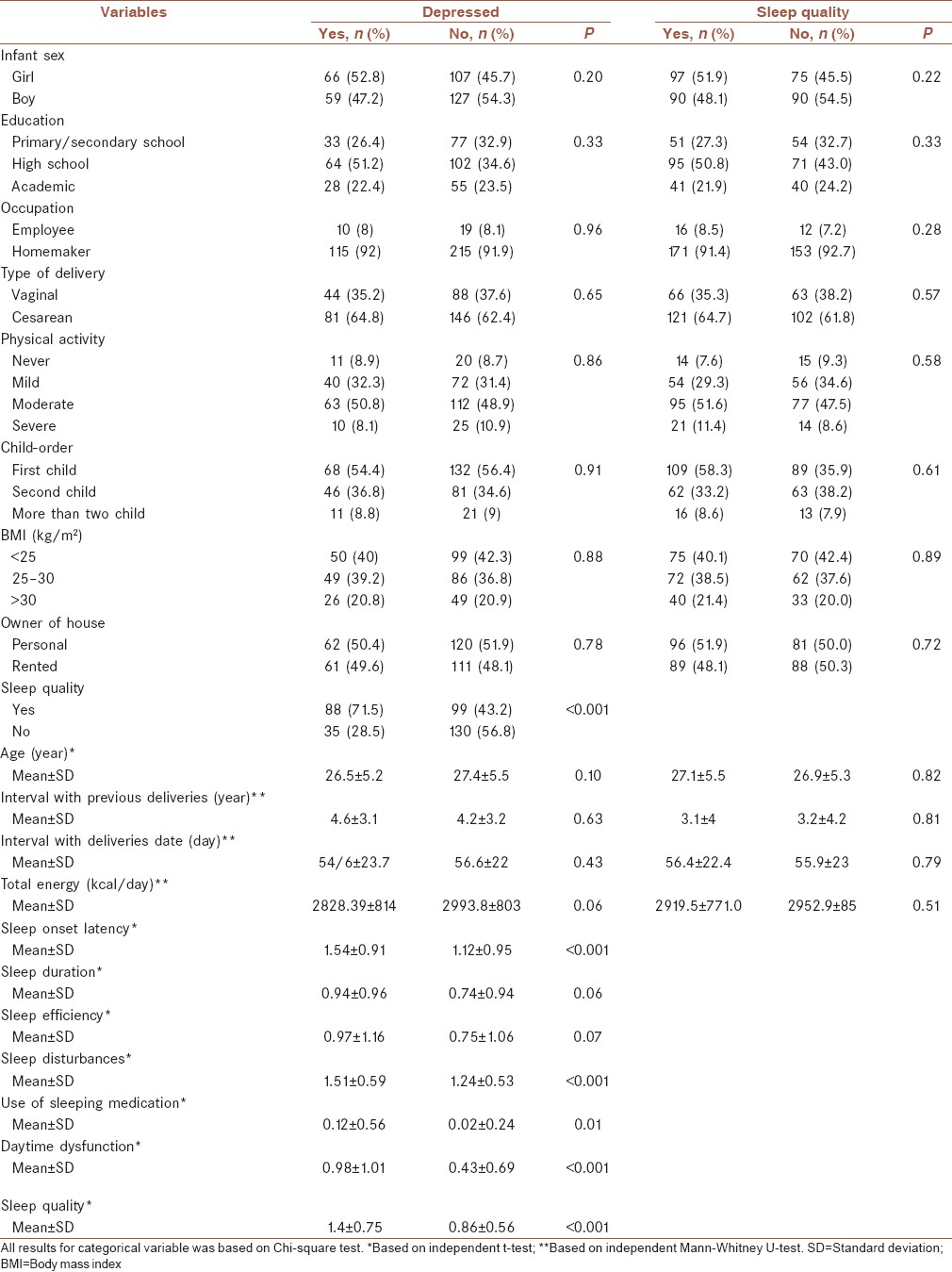
A total of 360 participants were enrolled, one participant did not complete the EPDS questionnaire, and seven subjects did not complete the PSQI questionnaire. In 359 participants who filled out the EPDS, 125 (34.8%) subject had EPDS score 13 or more and was considered as depressed subjects. Demographic characteristic and other Variables were compared between depressed and nondepressed women [Table 1]. The association between the components of sleep quality and postpartum depression is shown in Table 1. There were significant associations between postpartum depression and sleep onset latency (P > 0.001), sleep quality (P > 0.001), sleep disturbances (P > 0.001), use of sleeping medication (P = 0.019), and daytime dysfunction (P > 0.001). There were no significant associations between postpartum depression and other components such as sleep duration and sleep efficiency.
Table 1.
Frequency (%) distribution and mean±standard deviation of characteristics’ postpartum women based on depression and sleep quality, Ardebil, Iran in 2012
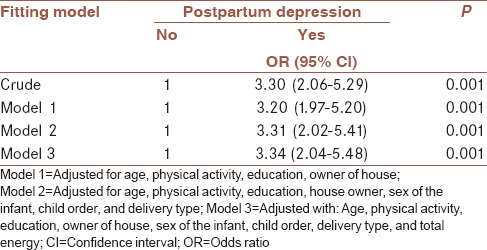
Of the 353 participants those who had filled out the PSQI, 187 (53.1%) scored more than five that is indicative of poor sleep quality. Demographic characteristic and other variables were compared between those who have low sleep quality and good sleep quality [Table 1]. In the crude model and after controlling for covariates such as age, physical activity, education, owner of house, and BMI, we found a statistically significant association between postpartum depression and sleep quality based on the Model 1 (odds ratio [OR] =3.302; 95% confidence interval [CI]: 2.062–5.287; P = 0.001). It was not attenuated in the Model 2 which was adjusted for covariates using in the Model 1 plus sex of the infant, child order, and delivery type and also in Model 3 adjusted for covariates using the Model 2 plus total energy. The results confirm that the chance of depression in women suffering from low sleep quality is three times higher than in those who are not (OR = 3.34; 95% CI: 2.04–5.48; P = 0.001) [Table 2].
Table 2.
Odds ratio (95% confidence intervals) of postpartum depression according to sleep quality
DISCUSSION
Our findings suggest that there is an association between postpartum depression and sleep quality. A cross-sectional population-based study showed sleep disturbances and poor subjective sleep quality was associated with depression in postpartum.[17] Findings of cohort study on 156 pregnant women in Iran showed that the quality of sleep in weeks between the 28th and 38th week of pregnancy was significantly associated with postpartum depression.[18] The cohort study that was applied on 51 nondepressed women with a history of postpartum major depression showed a significant association between sleep quality in late pregnancy and raped recurrence of depression in postpartum period.[22] A prospective study on 273 women reported a significant correlation between sleep quality and depression during pregnancy.[23] These studies have shown findings which are consistent with the results of the present study. There are bilateral relationships between depression and sleep quality. Low sleep quality can lead to depression, and depression can also lead to low sleep quality.[24] The relationship between depression and sleep quality could be related to the various psychoneuroimmunologic and psychoneuroendocrinologic mechanisms.[25,26,27,28,29]
A major strength of this study is its potential to add to cross-cultural understandings of perinatal sleep and mental health. It was conducted in all areas of the city of Ardebil. The sampling scheme may avoid selection bias.
One of the limitations of the present study was the use of self-report questionnaires (EPDS) instead of using interviewers with the subjects by psychologists. However, this questionnaire has been widely used for the screening of postpartum depression.[30,31] Other limitations of the study are factors such as unplanned pregnancy and also taking supplements such as folic acid which were prescribed by health center employees or physicians that could also have an impact on postpartum depression but were not included in the study.
CONCLUSION
The prevalence of both postpartum depression and low sleep quality were relatively high in our study population. There is an association between some components of sleep quality and postpartum depression. This association was remain after controlling of confounders.
Financial support and sponsorship
Nil.
Conflicts of interest
The authors have no conflicts of interest.
AUTHORS’ CONTRIBUTIONS
MRM contributed in the conception of the work, conducting the study, analysis and interpretation of data for the work, revising the draft, approval of the final version of the manuscript, and agreedfor all aspects of the work.
SI contributed in the design of the work, conducting the study, analysis of data for the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
GRK contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
MH contributed in the design of the work, analysis of data for the work revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
AE contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
REFERENCES
- 1.Stuchbery M, Matthey S, Barnett B. Postnatal depression and social supports in Vietnamese, Arabic and Anglo-Celtic mothers. Soc Psychiatry Psychiatr Epidemiol. 1998;33:483–90. doi: 10.1007/s001270050083. [DOI] [PubMed] [Google Scholar]
- 2.Cox JL, Murray D, Chapman G. A controlled study of the onset, duration and prevalence of postnatal depression. Br J Psychiatry. 1993;163:27–31. doi: 10.1192/bjp.163.1.27. [DOI] [PubMed] [Google Scholar]
- 3.Cooper PJ, Tomlinson M, Swartz L, Woolgar M, Murray L, Molteno C. Post-partum depression and the mother-infant relationship in a South African peri-urban settlement. Br J Psychiatry. 1999;175:554–8. doi: 10.1192/bjp.175.6.554. [DOI] [PubMed] [Google Scholar]
- 4.Beck CT. The effects of postpartum depression on child development: A meta-analysis. Arch Psychiatr Nurs. 1998;12:12–20. doi: 10.1016/s0883-9417(98)80004-6. [DOI] [PubMed] [Google Scholar]
- 5.Bagherzadeh R, Zahmatkeshan N, Moatamed N, Khorramroudi R, Ganjoo M. Prevalence of maternal blues, postpartum depression and their correlation with premenstrual syndrome in women refferred to health centers affiliated to Bushehr University of Medical Sciences. Iran J Obstet Gynecol Infertil. 2009;12:9–15. [Google Scholar]
- 6.Mousavi SG, Sabahi-Bidgoli M, Omidi A, Kosha Z, Ghavami M, Gorji Z, et al. Prevalence of postpartum depression and its relation to some psychosocial factors in mothers referred to health centers of Kashan during 2007-8. KAUMS J (FEYZ) 2011;15:247–53. [Google Scholar]
- 7.Hosseini SH, Naghibi A, Khademlou M. Postpartum depression and its relationship with some related factors. J Babol Univ Med Sci. 2008;10:76–81. [Google Scholar]
- 8.Kheirabadi GR, Maracy MR. Perinatal depression in a cohort study on Iranian women. J Res Med Sci. 2010;15:41. [PMC free article] [PubMed] [Google Scholar]
- 9.Choi SK, Park YG, Park IY, Ko HS, Shin JC. Impact of antenatal depression on perinatal outcomes and postpartum depression in Korean women. J Res Med Sci. 2014;19:807–12. [PMC free article] [PubMed] [Google Scholar]
- 10.Chang JJ, Pien GW, Duntley SP, Macones GA. Sleep deprivation during pregnancy and maternal and fetal outcomes: Is there a relationship? Sleep Med Rev. 2010;14:107–14. doi: 10.1016/j.smrv.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee KA. Alterations in sleep during pregnancy and postpartum: A review of 30 years of research. Sleep Med Rev. 1998;2:231–42. doi: 10.1016/s1087-0792(98)90010-7. [DOI] [PubMed] [Google Scholar]
- 12.Montgomery-Downs HE, Insana SP, Clegg-Kraynok MM, Mancini LM. Normative longitudinal maternal sleep: The first 4 postpartum months. Am J Obstet Gynecol. 2010;203:465.e1–7. doi: 10.1016/j.ajog.2010.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Walker MP. A refined model of sleep and the time course of memory formation. Behav Brain Sci. 2005;28:51–64. doi: 10.1017/s0140525x05000026. [DOI] [PubMed] [Google Scholar]
- 14.Harrison Y, Horne JA. The impact of sleep deprivation on decision making: A review. J Exp Psychol Appl. 2000;6:236–49. doi: 10.1037//1076-898x.6.3.236. [DOI] [PubMed] [Google Scholar]
- 15.Marques M, Bos S, Soares MJ, Maia B, Pereira AT, Valente J, et al. Is insomnia in late pregnancy a risk factor for postpartum depression/depressive symptomatology? Psychiatry Res. 2011;186:272–80. doi: 10.1016/j.psychres.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 16.Germain A, Thase ME. Sleep dysregulation and related regulatory models. In: Dobson KS, Dozois DJA, editors. Risk factors in depression. USA: Academic Press, Elsevier; 2008. pp. 91–117. [Google Scholar]
- 17.Dørheim SK, Bondevik GT, Eberhard-Gran M, Bjorvatn B. Sleep and depression in postpartum women: A population-based study. Sleep. 2009;32:847–55. doi: 10.1093/sleep/32.7.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alipour Z, Lamyian M, Hajizadeh E. Sleep quality in late pregnancy and postpartum depression. Iran J Obstet Gyneocol Infertil. 2012;14:39–47. [Google Scholar]
- 19.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–40. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 20.Adibi P, Keshteli AH, Esmaillzadeh A, Afshar H, Roohafza H, Bagherian-Sararoudi H, et al. The study on the epidemiology of psychological, alimentary health and nutrition (SEPAHAN): Overview of methodology. J Res Med Sci. 2012;17:292–8. [Google Scholar]
- 21.Kheirabadi GR, Maracy MR, Akbaripour S, Masaeli N. Psychometric properties and diagnostic accuracy of the edinburgh postnatal depression scale in a sample of Iranian women. Iran J Med Sci. 2012;37:32. [PMC free article] [PubMed] [Google Scholar]
- 22.Okun ML, Hanusa BH, Hall M, Wisner KL. Sleep complaints in late pregnancy and the recurrence of postpartum depression. Behav Sleep Med. 2009;7:106–17. doi: 10.1080/15402000902762394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skouteris H, Germano C, Wertheim EH, Paxton SJ, Milgrom J. Sleep quality and depression during pregnancy: A prospective study. J Sleep Res. 2008;17:217–20. doi: 10.1111/j.1365-2869.2008.00655.x. [DOI] [PubMed] [Google Scholar]
- 24.Kendall-Tackett K. A new paradigm for depression in new mothers: The central role of inflammation and how breastfeeding and anti-inflammatory treatments protect maternal mental health. Int Breastfeed J. 2007;2:6. doi: 10.1186/1746-4358-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Groer MW, Morgan K. Immune, health and endocrine characteristics of depressed postpartum mothers. Psychoneuroendocrinology. 2007;32:133–9. doi: 10.1016/j.psyneuen.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Miller GE, Rohleder N, Stetler C, Kirschbaum C. Clinical depression and regulation of the inflammatory response during acute stress. Psychosom Med. 2005;67:679–87. doi: 10.1097/01.psy.0000174172.82428.ce. [DOI] [PubMed] [Google Scholar]
- 27.Maes M, Christophe A, Bosmans E, Lin A, Neels H. In humans, serum polyunsaturated fatty acid levels predict the response of proinflammatory cytokines to psychologic stress. Biol Psychiatry. 2000;47:910–20. doi: 10.1016/s0006-3223(99)00268-1. [DOI] [PubMed] [Google Scholar]
- 28.Konsman JP, Parnet P, Dantzer R. Cytokine-induced sickness behaviour: Mechanisms and implications. Trends Neurosci. 2002;25:154–9. doi: 10.1016/s0166-2236(00)02088-9. [DOI] [PubMed] [Google Scholar]
- 29.Motivala SJ, Sarfatti A, Olmos L, Irwin MR. Inflammatory markers and sleep disturbance in major depression. Psychosom Med. 2005;67:187–94. doi: 10.1097/01.psy.0000149259.72488.09. [DOI] [PubMed] [Google Scholar]
- 30.Bunevicius A, Kusminskas L, Pop VJ, Pedersen CA, Bunevicius R. Screening for antenatal depression with the Edinburgh Depression Scale. J Psychosom Obstet Gynaecol. 2009;30:238–43. doi: 10.3109/01674820903230708. [DOI] [PubMed] [Google Scholar]
- 31.Jardri R, Pelta J, Maron M, Thomas P, Delion P, Codaccioni X, et al. Predictive validation study of the Edinburgh Postnatal Depression Scale in the first week after delivery and risk analysis for postnatal depression. J Affect Disord. 2006;93:169–76. doi: 10.1016/j.jad.2006.03.009. [DOI] [PubMed] [Google Scholar]


