Abstract
Purpose:
The purpose of this study was to evaluate functional and anatomical outcomes of posterior iris-claw intraocular lens (IOL) implant for correction of aphakia in eyes with inadequate capsular support.
Materials and Methods:
Prospective case series of 108 aphakic eyes with inadequate capsular support which underwent posterior iris-claw IOL with a 6-month follow-up period was conducted. The cases belonged to two clinical settings: elective secondary implantation and those with intraoperative posterior dislocation of cataractous lens or IOL. Main outcome measures were visual acuity, anterior chamber reaction, stability of IOL, endothelial cell count, intraocular pressure (IOP), and cystoid macular edema (CME).
Results:
The mean best-corrected visual acuity was LogMAR 0.25. None had chronic anterior chamber inflammation. The mean difference in central endothelial counts before surgery and 1 month after surgery was 104.21 cell/mm2 (4.92%). There was no statistically significant difference in central endothelial cell count at 1 and 6 months (P = 0.91) and also in the central macular thickness at preoperative and after 6 months suggestive of CME (P = 0.078). Three eyes had raised IOP which were managed with neodymium-doped yttrium aluminum garnet laser peripheral iridotomy. There were no IOL dislocations or other adverse events in our series.
Conclusion:
Posterior chamber iris-claw lenses are a good option in eyes with inadequate posterior capsular support. Chronic inflammation, poor lens stability, or significant central endothelial cell loss was not observed during the 6-month follow-up period.
Keywords: Inadequate posterior capsule, posterior iris-claw lenses, secondary intraocular lens implantation
The presently available options for lens implantation in eyes with inadequate capsular support are far from perfect. Various intraocular lens (IOL) implants available for fixation in this scenario are anterior chamber (ACIOL), scleral fixated (SFIOL), glued IOL, anterior iris fixated IOL, and posterior iris-fixated IOL.[1,2,3]
Although ACIOLs have been used extensively, they are known to have a high risk of corneal decompensation and glaucoma.[4] The surgical technique for implanting SFIOLs and glued IOLs has a steep learning curve and needs more intraocular maneuvering.
Few studies of posterior iris-claw lenses in Indian population exist in literature.
Materials and Methods
This prospective study included patients with surgical aphakia with poor capsular support at our tertiary eye care center during September 2013 to January 2015. The Ethical Committee approval was taken before beginning the study.
The cases belonged to two clinical settings: Elective secondary implantation and those with intraoperative posterior dislocation of the cataractous lens or IOL either due to large posterior capsular rupture or zonular dehiscence.
Preoperative assessment included thorough clinical examination including LogMAR visual acuity, slit-lamp examination of the anterior and posterior segment, and intraocular pressure (IOP) on Goldman applanation tonometer.
Patients underwent specular microscopy (Konan Specular Microscope X, model NSP-9900, Konan Medical Inc., Japan) for central endothelium cell count (ECC) and optical coherence tomography (OCT; Topcon 3D OCT 2000, Software 4.2 X, Topcon Corporation, Tokyo, Japan) for central macular thickness preoperatively.
Surgical technique
All cases were operated by a single surgeon under peribulbar block with 0.5% lignocaine anesthesia after a written informed consent of patients was obtained. The lens used in our study was Excelens (Excel Optics Pvt. Ltd., Chennai, India) polymethyl methacrylate single-piece biconvex iris-claw IOL with a total length of 8 mm and 5.5 mm optic size. The recommended A constant by the manufacturer was 117.2. We preferred SRK-T formula for achieving postoperative emmetropia.
In elective secondary implantation, a 5.5 mm scleral tunnel was made or revised according to duration from primary surgery using a crescent knife. Two paracenteses were made at 3 and 9 O'clock position and pilocarpine (0.5%) was injected intracamerally. The anterior chamber was entered after injecting viscoelastic material. This was followed by anterior vitrectomy. Posterior iris-fixated IOL was implanted using an iris-claw IOL holding forceps and Sinskey hook and enclaved on the posterior surface of the iris at 3 and 9 O'clock meridian [Fig. 1 and 2]. The lens optic was firmly held with the forceps and positioned in the center, posterior to the pupil [Fig. 3]. The mid-peripheral iris was gently enclaved in the claw using Sinskey hook. Peripheral iridectomy was done at 11 or 1 O'clock position. Viscoelastic material was removed. A suture was placed if needed to seal the wound.
Figure 1.
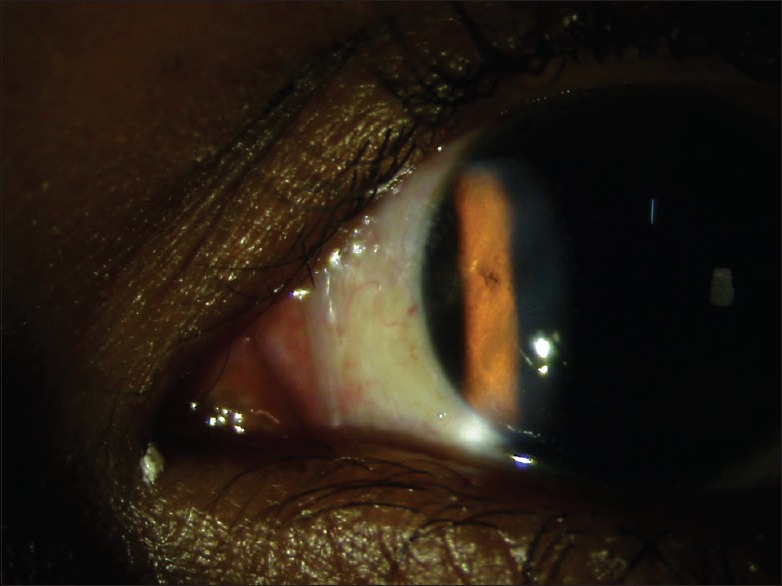
Nasal enclavation: Seen as dimples on anterior iris surface
Figure 2.
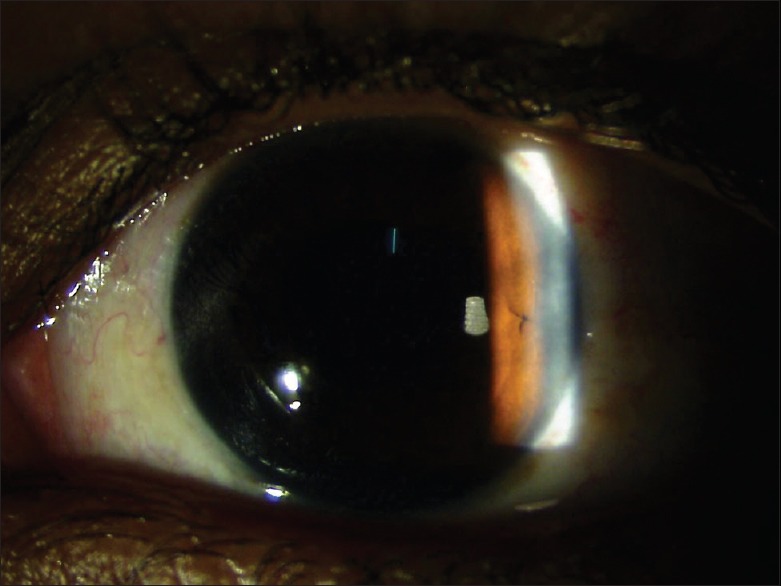
Temporal enclavation: Seen as dimples on anterior iris surface
Figure 3.
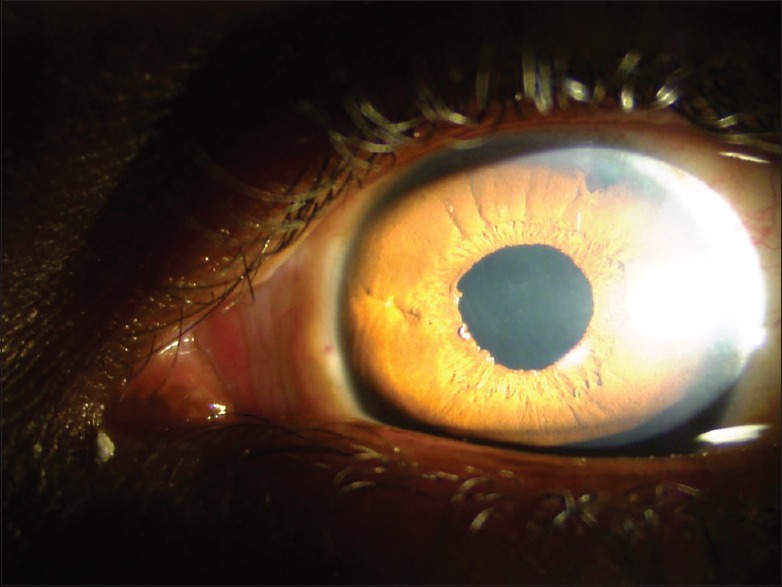
Retropupillary iris-claw intraocular lens: Enclavation at 3 O’clock and 9 O’clock position. Peripheral iridectomy at 1 O’clock position
In eyes with intraoperative large posterior capsular rupture or zonular dehiscence with a posterior lens or IOL dislocation, implantation of posterior iris fixated IOL as explained above was preceded by standard three port 20-gauge pars plana vitrectomy (PPV) for posteriorly dislocated cataractous lens or IOL. The infusion was kept off during implantation of IOL as it does generate turbulence when the wound is open for implantation. However, it is kept in place in the unlikely event that IOL falls back into the vitreous cavity because insertion of infusion cannula in a soft eyeball can be challenging. Therefore, infusion cannula is disconnected only at the end of surgery.
Subconjunctival injection of antibiotic and steroid was given in both groups. Postoperatively, topical steroid-antibiotic-mydriatic regimen was followed. The patients received 1% prednisolone acetate eye drops six times daily tapered over 6 weeks, 0.5% moxifloxacin eye drops four times daily for 6 weeks, and 0.5% cyclopentolate eye drop once a day for a week.
Postoperative assessment included LogMAR visual acuity, central ECC, IOL position, IOP, postoperative intraocular inflammation (anterior chamber reaction), central macular thickness, presence of hyphema, pigment dispersion, and hypotony.
Postoperatively, intraocular position of the IOL was assessed with ultrasound biomicroscopy (UBM) (SCAN 3000/UBM S/N UB 3-01649, OTI OPTOS, USA), central ECC was measured with specular microscope (Konan Specular Microscope X, model NSP-9900, Konan Medical Inc., Japan), and central macular thickness was measured on OCT (Topcon 3D OCT 2000, Software 4.2 X, Topcon Corporation, Tokyo, Japan) in all patients.
Postoperative follow-up was done by a single observer on day 1 (visual acuity, anterior chamber reaction) and day 7 (visual acuity, anterior chamber reaction, IOP), 1 month (visual acuity, anterior chamber reaction, IOP, UBM, specular microscopy), 3 months (visual acuity, anterior chamber reaction, IOP), and 6 months (visual acuity, anterior chamber reaction, IOP, specular microscopy, OCT) was completed by all patients.
Cells in the anterior chamber were counted using the wide beam with a 1–2 mm long slit and graded according to the method of Hogan et al. [Table 1].[5] Flare was also graded according to the scheme proposed by Hogan in 1959 [Table 2].[5] With a ray of light directed at an oblique angle to the plane of the iris with the maximum light intensity of the slit lamp through a short 1–2 mm slit, IOP was measured with Goldmann applanation tonometer.
Table 1.
Grading of cells

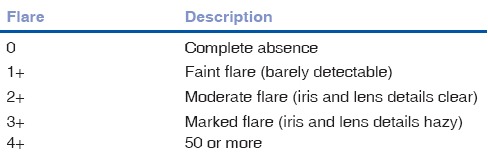
Table 2.
Grading of anterior chamber flare
Results
In total, 108 aphakic eyes were enrolled in the study, of which 99 (91.66%) eyes were for elective secondary implantation, 9 (8.33%) eyes were from the group with intraoperative posterior lens or IOL dislocation.
The case series consisted of 62 males and 46 females.
Average best-corrected visual acuity on LogMAR chart was 0.25 [Table 3]. On slit-lamp biomicroscopic examination, none of the patients had anterior chamber inflammation or hyphema or hypotony at and beyond the day 7 follow-up.
Table 3.
Postoperative LogMAR visual acuity
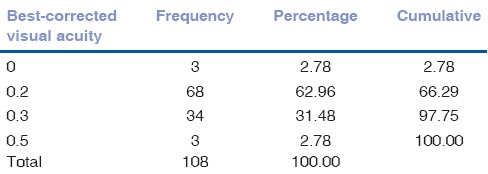
The mean difference in central endothelial counts before and 1 month after surgery was 104.21 cell/mm2 (4.92%) comparable to any other IOL surgery [Fig. 4]. The mean drop in central endothelial counts at one and 6 months after surgery was <0.5% with no statistically significant difference using the paired t-test (P = 0.91) [Figs. 5–7]. No cystoid macular edema (CME) was observed on OCT. There was no statistically significant difference in the central macular thickness at preoperative and 6 months using paired t-test (P = 0.078) [Fig. 8].
Figure 4.
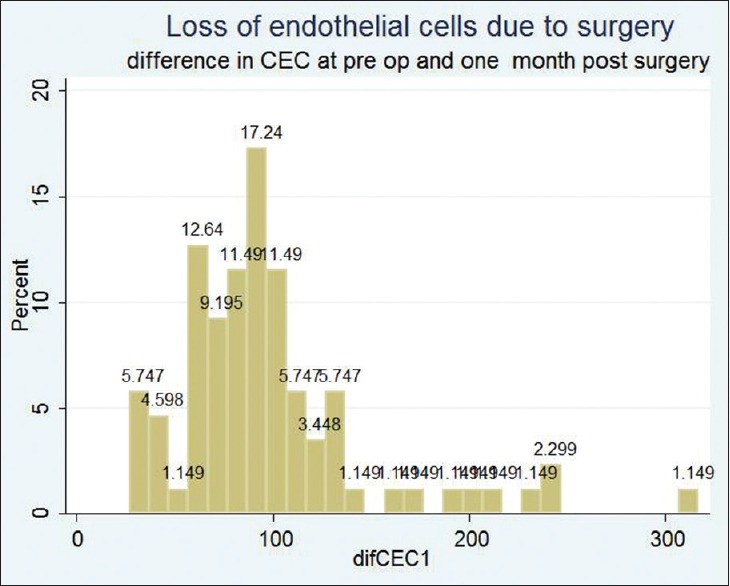
Corneal endothelial cell count: Preoperative and 1 month postoperative
Figure 5.
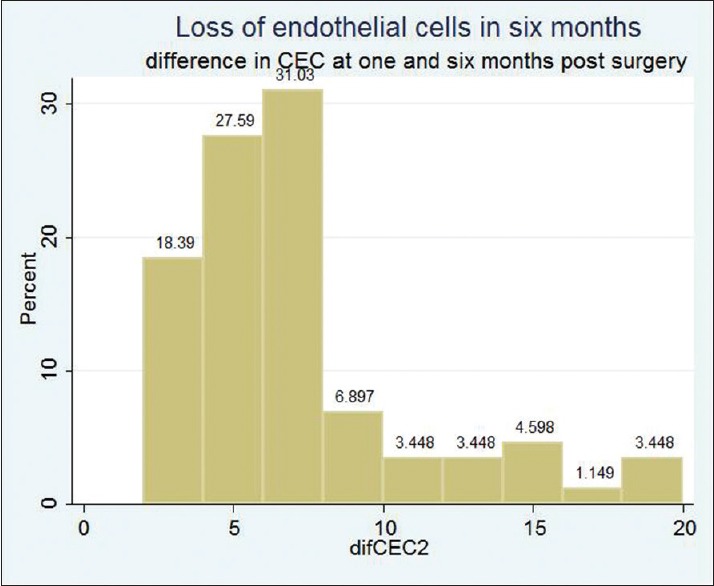
Corneal endothelial cell count: One and 6 months postoperative
Figure 7.
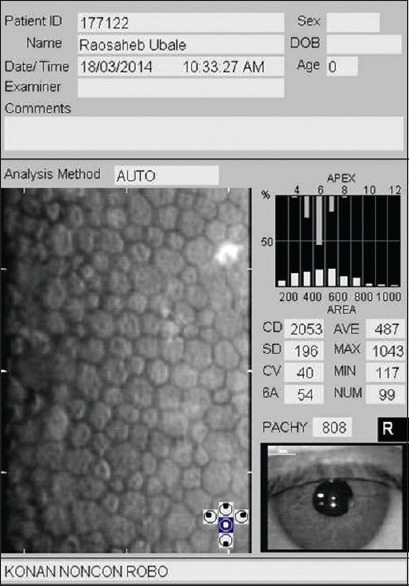
Six-month postoperative specular microscopy of the same patient
Figure 8.
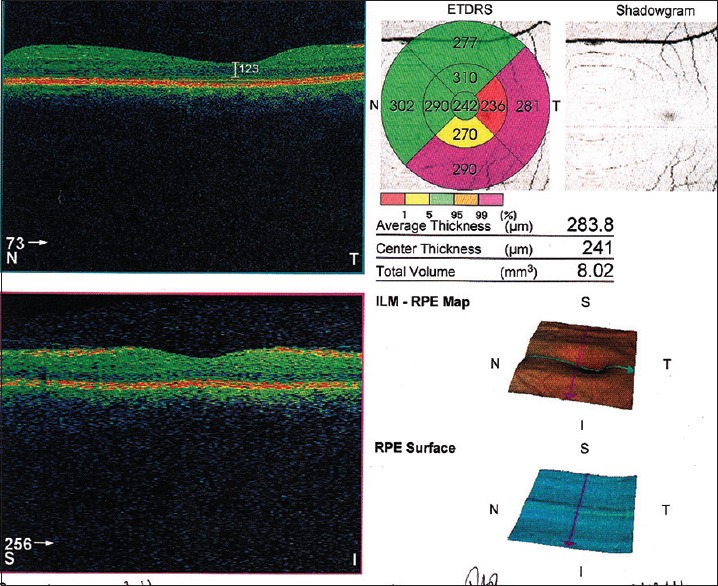
Six-month postoperative optical coherence tomography showing normal central macular architecture and thickness
Three eyes had raised IOP which were managed with neodymium-doped yttrium aluminum garnet (Nd: YAG) laser peripheral iridotomy (PI) [Fig. 9].
Figure 9.
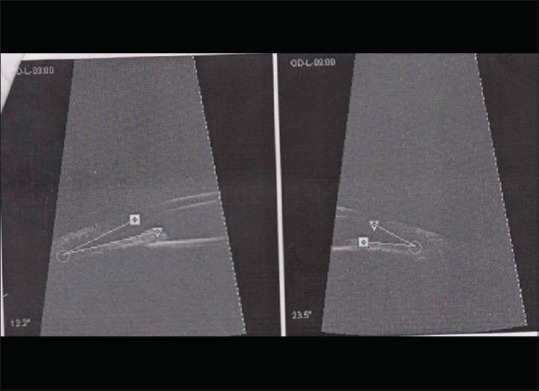
Postoperative ultrasound biomicroscopy showing wide open-angles on each side after implantation of iris-claw
There were no major postoperative adverse events, decentration or dislocation of IOL in our series [Figs. 9 and 10].
Figure 10.
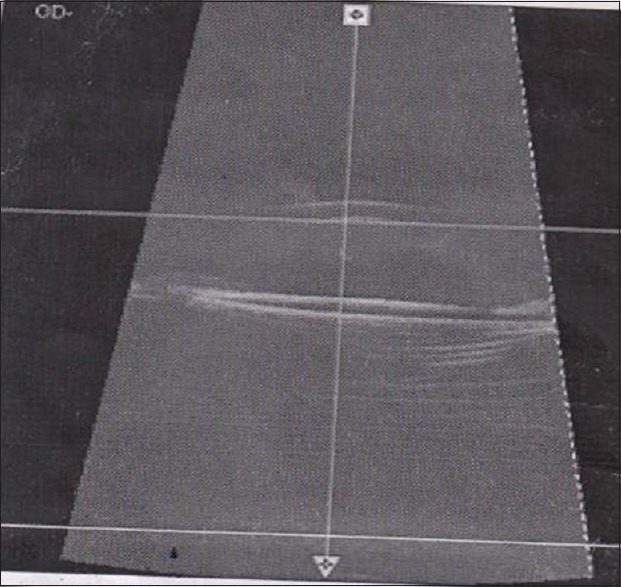
Postoperative ultrasound biomicroscopy showing intraocular lens position: well-centered intraocular lens parallel to iris plane
Discussion
While indisputably “in-the-bag” implantation is the location of choice for an IOL implant, lens implantation in the absence of adequate posterior capsular support is a challenge for a cataract surgeon. At present, ACIOLs, SFIOLs, glued IOLs, and iris-claw IOLs are being used in correction of aphakia in this scenario.[1,2,3]
Endothelial decompensation is a known complication associated with ACIOLs.[4] ACIOLs are also associated with higher inflammatory reaction. In a study conducted by Marques et al., ACIOL-related inflammation has been the main indication for IOL exchange in 53% cases.[6]
Stability of SFIOLs can be jeopardized due to degradation of suture material over time, leading to dislocation of SFIOL.[7] In a study by Vote et al., SFIOLs were associated with high complication rate and subsequent need for further surgery. Suture breakage was the main indication for 57% of re-surgeries.[8] Similarly, a study by Asadi and Kheirkhah shows that transscleral-fixated posterior chamber intraocular lenses are not just technically difficult but are also associated with higher chances of retinal detachment (4%) and suture breakage (24%).[9]
In a study published by Evereklioglu et al., SFIOLs were proved to have a better outcome than ACIOLs while another study by Bellucci et al. showed that SFIOLs had more intraoperative and postoperative complications.[3,10] At the same time, this study also reported 6% rate of sight-threatening complications in both types of IOLs. Wherein retinal detachment was seen in one out of 35 eyes implanted with ACIOLs and two out of 33 eyes implanted with SFIOLs.[3,10]
A study of glued IOLs reported CME in 1.9% eyes, pigment dispersion in 1.9% eyes, and haptic extrusion in 1.9% eyes. 3.3% cases had IOL decentration and re-surgery was required in 7.7% cases due to altered haptic position.[11]
Anterior iris-claw lenses have also gained notoriety due to postoperative problems. In a 3-year follow-up of anterior iris-claw IOLs in 72 eyes, Chen et al. reported a mean endothelial cell loss of 9.78% and pigment precipitates on IOL in 5.6% patients.[12] In another study carried by De Silva et al., postoperative complication rates in anterior iris-claw IOLs were comparable with conventional ACIOLs, with postoperative IOP rise in 9.5% eyes and corneal decompensation in 1.7% of eyes.[13] They also reported CME in 7.7% of eyes and subluxation of IOL in 6% eyes. Retinal detachment was seen in 0.8% of eyes.[13]
We had been treating aphakics with ACIOL and SFIOL in our center earlier; however, chances of corneal endothelial decompensation in case of ACIOLs and longer learning curve and more intraocular maneuvering in cases of SFIOLs made us settle in favor of posterior iris-fixated IOLs. In a retrospective case series by Gonnermann et al., posterior chamber iris-claw aphakic IOL implantation was done in eyes without adequate capsule support.[14] They reported a good visual outcome with a favorable complication rate in terms of CME (8.7%), hyphema (2.1%), and elevated IOP (4.3%). In the study carried out by Baykara M, retropupillary iris-claw IOL provided good visual outcomes with a favorable complication rate and it was suggested that it can be used for a wide range of indications in eyes without adequate capsule support.[15] PPV with posterior iris-claw implantation for posteriorly dislocated nucleus and IOL was studied by Patil et al.[16] In this study, 13.3% patients developed postoperative CME while remaining patients achieved a good visual outcome.
The 1980 decade saw the use of iris-claw lenses being implanted anterior to the iris as a primary option in patients undergoing uneventful cataract surgery. This concept was popularized by Prof. Jan Worst from Holland and Dr. Daljeet Singh from India.[17,18] The anterior location of the IOL resulted in corneal decompensation and CME in a significant number of patients. While designing our study protocol, we specifically chose these two possible problems to analyze after positioning the lens behind the iris. Specular endothelial microscopy is the best indicator of the endothelial cell change. Loss during surgery and the 6-month period was carefully documented. OCT is noninvasive and can be performed serially to study any macular change.
The rationale behind preferring posterior iris-claw IOL over anterior one is that posterior iris-fixated IOL is retropupillary and has a lesser risk of endothelial decompensation.[19] Posterior iris-claw lenses also have the advantage of a simpler procedure, positioning near the nodal point, and no need for extra sutures or glue.[19] There are very few studies supporting the use of posterior iris-claw IOL in aphakic patients with good postoperative results in terms of visual acuity. Our results were comparable to other studies of posterior iris-claw IOL implantation.[5,16,19,20]
All our patients had completed the 6-month follow-up period. Average best-corrected visual acuity on LogMAR was 0.25.
None of our patients had chronic anterior chamber inflammation. Similar to a study by Forlini et al., none of our patients had uveitis.[21] The mean difference in central endothelial counts before surgery and 1 month after surgery was 104.21 cell/mm2 (4.92%) comparable to any other IOL surgery. There was no statistically significant difference in central endothelial cell count at one and 6 months using paired t test. (P - 0.91). We found posterior iris-fixated IOL to be safe regarding the corneal endothelial cell loss as in other studies [Figs. 6 and 7].[21,22,23,24]
Figure 6.
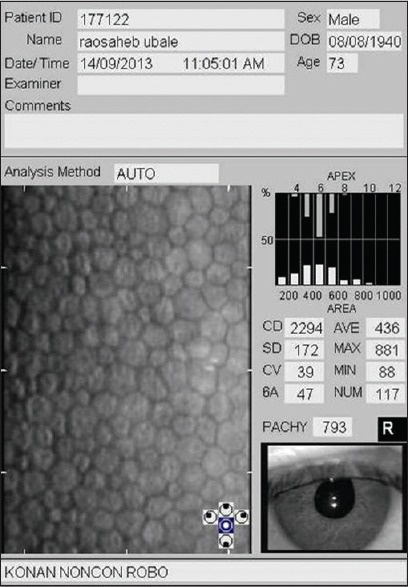
Preoperative specular microscopy of a representative patient
In our study, there was no statistically significant difference in the central macular thickness at preoperative and 6-month follow-up (P - 0.078). No CME was seen on OCT similar to studies by Forlini et al. and Schallenberg et al.[21,23] On UBM, we found all lenses to be parallel to iris plane. Similar findings were noted by Baykara et al. in 32 eyes.[15] First three eyes in our study had raised IOP in the 1st week postoperatively, which were managed with Nd: YAG PI. We included surgical peripheral iridectomy as a routine in every case of posterior iris-fixated IOL. Similarly, raised IOP was observed in one out of 31 patients by Schallenberg et al.[23]
Forlini et al. have reported three cases of disenclavation, one case of spontaneous posterior dislocation, and one case of CME out of total 320 eyes operated for posterior iris-claw IOL,[21] while Gonnermann et al. have reported disenclavation in 8.7% eyes and CME in 8.7% eyes.[14] Although spontaneous disenclavation of one or both iris-claw haptics with or without dislocation of IOL has been reported, we encountered no such case in our series.[21] None of our patients had hyphema, hypotony, or pigment dispersion.
Shortcomings of our study lie in a fact that all surgeries were performed by a single surgeon. The present publication reports the findings at the end of 6 months. The study, however, will continue to follow-up the cohort for a longer duration, notwithstanding the loss to follow-up expected over an extended period.
Conclusion
The effect of anterior claw lenses on the corneal endothelium had created a psychological barrier to the use of iris-claw lenses in general. The 6-month results of this prospective study with adequate sample size and objective evaluation of endothelial count, CME, lens stability, and visual acuity validate the role of posterior iris-fixated lenses in aphakic patients, in the absence of capsular support. In our view, technique of SFIOL insertion is more comfortable for vitreoretinal surgeons. In our experience, insertion of posterior iris-fixated IOL is well within the skill sets and maneuvers familiar to a cataract surgeon and provides a very easy, simple, and affordable option with no serious adverse effect during the follow-up period.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rao R, Sasidharan A. Iris claw intraocular lens: A viable option in monocular surgical aphakia. Indian J Ophthalmol. 2013;61:74–5. doi: 10.4103/0301-4738.107198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gicquel JJ, Langman ME, Dua HS. Iris claw lenses in aphakia. Br J Ophthalmol. 2009;93:1273–5. doi: 10.1136/bjo.2009.159871. [DOI] [PubMed] [Google Scholar]
- 3.Evereklioglu C, Er H, Bekir NA, Borazan M, Zorlu F. Comparison of secondary implantation of flexible open-loop anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2003;29:301–8. doi: 10.1016/s0886-3350(02)01526-2. [DOI] [PubMed] [Google Scholar]
- 4.Snellingen T, Shrestha JK, Huq F, Husain R, Koirala S, Rao GN, et al. The South Asian cataract management study: Complications, vision outcomes, and corneal endothelial cell loss in a randomized multicenter clinical trial comparing intracapsular cataract extraction with and without anterior chamber intraocular lens implantation. Ophthalmology. 2000;107:231–40. doi: 10.1016/s0161-6420(99)00008-1. [DOI] [PubMed] [Google Scholar]
- 5.Hogan MJ, Kimura SJ, Thygeson P. Signs and symptoms of uveitis. I. Anterior uveitis. Am J Ophthalmol. 1959;47(5 Pt 2):155–70. doi: 10.1016/s0002-9394(14)78239-x. [DOI] [PubMed] [Google Scholar]
- 6.Marques FF, Marques DM, Osher RH, Freitas LL. Longitudinal study of intraocular lens exchange. J Cataract Refract Surg. 2007;33:254–7. doi: 10.1016/j.jcrs.2006.10.036. [DOI] [PubMed] [Google Scholar]
- 7.Price MO, Price FW, Jr, Werner L, Berlie C, Mamalis N. Late dislocation of scleral-sutured posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31:1320–6. doi: 10.1016/j.jcrs.2004.12.060. [DOI] [PubMed] [Google Scholar]
- 8.Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006;141:308–12. doi: 10.1016/j.ajo.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Asadi R, Kheirkhah A. Long-term results of scleral fixation of posterior chamber intraocular lenses in children. Ophthalmology. 2008;115:67–72. doi: 10.1016/j.ophtha.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 10.Bellucci R, Pucci V, Morselli S, Bonomi L. Secondary implantation of angle-supported anterior chamber and scleral-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 1996;22:247–52. doi: 10.1016/s0886-3350(96)80227-6. [DOI] [PubMed] [Google Scholar]
- 11.Kumar DA, Agarwal A, Packiyalakshmi S, Jacob S, Agarwal A. Complications and visual outcomes after glued foldable intraocular lens implantation in eyes with inadequate capsules. J Cataract Refract Surg. 2013;39:1211–8. doi: 10.1016/j.jcrs.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Chen Y, Liu Q, Xue C, Huang Z, Chen Y. Three-year follow-up of secondary anterior iris fixation of an aphakic intraocular lens to correct aphakia. J Cataract Refract Surg. 2012;38:1595–601. doi: 10.1016/j.jcrs.2012.04.037. [DOI] [PubMed] [Google Scholar]
- 13.De Silva SR, Arun K, Anandan M, Glover N, Patel CK, Rosen P. Iris-claw intraocular lenses to correct aphakia in the absence of capsule support. J Cataract Refract Surg. 2011;37:1667–72. doi: 10.1016/j.jcrs.2011.03.051. [DOI] [PubMed] [Google Scholar]
- 14.Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM, Bertelmann E, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012;38:2139–43. doi: 10.1016/j.jcrs.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 15.Baykara M, Ozcetin H, Yilmaz S, Timuçin OB. Posterior iris fixation of the iris-claw intraocular lens implantation through a scleral tunnel incision. Am J Ophthalmol. 2007;144:586–91. doi: 10.1016/j.ajo.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 16.Patil KB, Meleth P, Shanker MP. Pars plana vitrectomy with posterior iris claw implantation for posteriorly dislocated nucleus and intraocular lens. Indian J Ophthalmol. 2011;59:497–500. doi: 10.4103/0301-4738.86321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Worst JG. Iris claw lens. J Am Intraocul Implant Soc. 1980;6:166–7. doi: 10.1016/s0146-2776(80)80016-4. [DOI] [PubMed] [Google Scholar]
- 18.Singh D. Iris claw lens – Six years' experience. Indian J Ophthalmol. 1986;34:181–2. [PubMed] [Google Scholar]
- 19.Hazar L, Kara N, Bozkurt E, Ozgurhan EB, Demirok A. Intraocular lens implantation procedures in aphakic eyes with insufficient capsular support associated with previous cataract surgery. J Refract Surg. 2013;29:685–91. doi: 10.3928/1081597X-20130723-02. [DOI] [PubMed] [Google Scholar]
- 20.Farrahi F, Feghhi M, Haghi F, Kasiri A, Afkari A, Latifi M. Iris claw versus scleral fixation intraocular lens implantation during pars plana vitrectomy. J Ophthalmic Vis Res. 2012;7:118–24. [PMC free article] [PubMed] [Google Scholar]
- 21.Forlini M, Soliman W, Bratu A, Rossini P, Cavallini GM, Forlini C. Long-term follow-up of retropupillary iris-claw intraocular lens implantation: A retrospective analysis. BMC Ophthalmol. 2015;15:143. doi: 10.1186/s12886-015-0146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anbari A, Lake DB. Posteriorly enclavated iris claw intraocular lens for aphakia: Long-term corneal endothelial safety study. Eur J Ophthalmol. 2015;25:208–13. doi: 10.5301/ejo.5000527. [DOI] [PubMed] [Google Scholar]
- 23.Schallenberg M, Dekowski D, Hahn A, Laube T, Steuhl KP, Meller D. Aphakia correction with retropupillary fixated iris-claw lens (artisan) – Long-term results. Clin Ophthalmol. 2014;8:137–41. doi: 10.2147/OPTH.S55205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsing YE, Lee GA. Retropupillary iris claw intraocular lens for aphakia. Clin Exp Ophthalmol. 2012;40:849–54. doi: 10.1111/j.1442-9071.2012.02808.x. [DOI] [PubMed] [Google Scholar]


