Abstract
Purpose:
This study aimed to evaluate the safety and efficacy of retropupillary fixation of an iris-claw intraocular lens (IOL; Verisyse polymethyl methacrylate IOL, Abbott Medical Optics [AMO], Netherlands) for the surgical correction of aphakia in microspherophakic eyes without sufficient capsular support.
Design:
This was a prospective, interventional, noncomparative case series.
Methods:
This interventional case series comprised 17 eyes of 9 microspherophakic patients. Retropupillary fixation of the Verisyse iris-claw IOL (AMO) was performed in all cases. The surgical time was measured. Corrected distance visual acuity, astigmatism, intraocular pressure (IOP), tissue reaction, pigment dispersion, and stability of the IOL were studied 1 day, 3 days, 1 week, 2 weeks, 1 month, and 6 months postoperatively.
Results:
Eight patients had familial microspherophakia and one patient had Marfan's syndrome. Eighty-two percent of the cases achieved a visual acuity of 0.3 or better. There was no significant postoperative inflammatory reaction. Transient elevation of IOP was recorded in two cases in the 1st week only. One IOL developed disengagement of one of the haptics from the iris and was successfully re-engaged. All the other IOLs were well centered and stable. The mean surgical time was 18.0 ± 4.5 min.
Conclusions:
Retropupillary fixation of an iris-claw IOL is a safe and effective procedure that provides early visual recovery. It is also a time-saving method for correcting aphakia in microspherophakic eyes without sufficient capsular support.
Keywords: Aphakia, iris-claw lens, microspherophakia
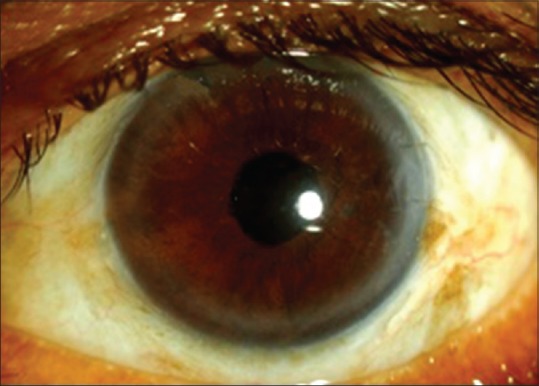
Microspherophakia is a rare autosomal recessive condition. It usually presents as lenticular myopia. Glaucoma is sometimes the presenting complication, which is most likely due to a pupillary block. There is typically no associated buphthalmos or angle anomalies. The microspheric lens is liable to dislocation into the vitreous cavity or the anterior chamber (AC). The condition may be isolated or associated with a number of disorders including Peter's anomaly, Marfan's syndrome, and Weill–Marchesani syndrome.[1] The spherical shape, as shown in Fig. 1, is attributed to the underdeveloped zonules of Zinn, which do not exert enough force on the lens to maintain its usual oval shape.[1,2,3,4] This condition is the result of a homozygous mutation to the LTBP2 gene. Parental consanguinity was present in the reported families.[5]
Figure 1.
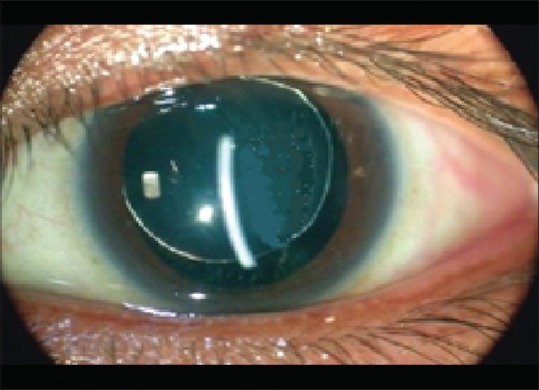
A slit-lamp optical section showing a small, thick spherical lens with stretched zonules
The surgical modalities available for correcting aphakia in such cases are unusual and depend mainly on the ability to preserve the lens capsule during surgery. In fact, this is not typically an easy task, especially in underdeveloped lens zonules that, in many cases, result in the absence of adequate capsular support for intraocular lens (IOL) implantation. The surgical options for optical correction of aphakia in eyes with no capsular support include angle-supported AC IOLs, sclerally fixed IOLs, and iris-sutured IOLs. In addition to the surgical difficulty of some of these techniques, each has its own limitations and complications.[6,7,8,9]
Posterior iris fixation of iris-claw IOLs has the advantage of a retropupillary posterior chamber (PC) location and a relatively simple surgical approach with a low rate of postoperative complications.[9] We conducted this study to analyze the stability, safety, and efficacy of retropupillary posterior iris fixation of iris-claw IOLs in microspherophakic eyes with inadequate capsular support.
Methods
This study was conducted in Egypt between June 2011 and November 2013. It was a prospective interventional noncomparative case series. Seventeen eyes of nine microspherophakic patients were studied.
Preoperatively, all patients provided informed consent and underwent a complete ophthalmologic evaluation including uncorrected visual acuity, subjective refraction, and best-corrected visual acuity (BCVA). Other evaluation criteria included slit-lamp examination, Goldmann applanation tonometry, keratometry, an ultrasonography scan, posterior segment evaluation with a 90 D lens, and indirect ophthalmoscopy.
A lensectomy was performed in all cases, either with an anterior approach or a pars plana approach for posteriorly dislocated lenses. Antiglaucoma medications and cycloplegics were given for cases of pupillary block. Retropupillary fixation of the iris-claw IOL (Verisyse polymethyl methacrylate [PMMA] IOL, Abbott Medical Optics [AMO], Netherlands) was carried out in all cases by one of the two surgeons (Mahmoud A. Al Aswad and Sameh Mosaad Fouda). The IOL model VRSA54 has an overall diameter of 8.5 mm with an optic diameter of 5.4 mm and an A constant ultrasound of 115.0 recommended by the manufacturer for AC placement; for retropupillary fixation, an A constant of 116.9 and SRK-T formula were used for IOL calculation. Biometry was done using the optical method (IOL master, Zeiss, Germany). This PMMA IOL for aphakia is available in powers of 2 D to 30 D. Fig. 2 shows the schematic representation of the Verisyse aphakic IOL.
Figure 2.
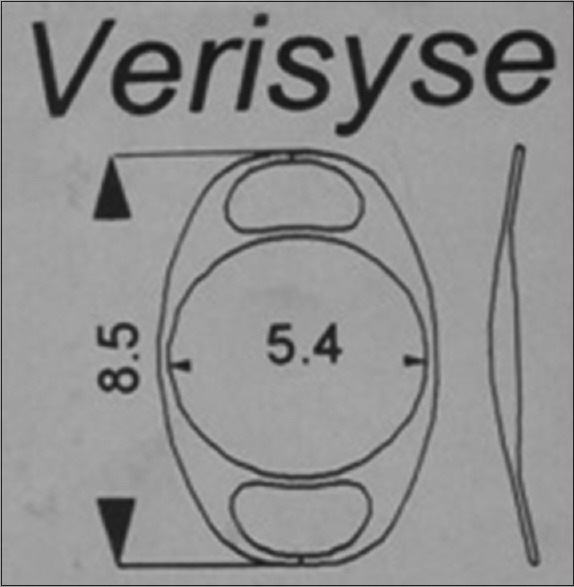
Schematic representation of the Verisyse aphakic lens
Surgical technique
Peribulbar anesthesia or general anesthesia was given according to the patient's condition. An automated lensectomy and anterior vitrectomy were performed with an anterior approach through two opposing paracentesis incisions that were located 90° from the scleral section on each side. A pars plana lensectomy was used for the posteriorly dislocated lens. In the case in which a pars plana lensectomy was performed, AC incisions were created after completing the pars plana lensectomy to implant the lens. An anterior capsulorrhexis was performed using a vitrectomy cutter at a speed of 800 cps (anterior vitreorrhexis), and removal of the lens matter was performed using the aspiration function only with the aim of preserving the integrity of the posterior capsule as long as possible (this helps to minimize the risk of loss of lens matter into the vitreous cavity). In the case of vitreous prolapse, an anterior vitrectomy was performed with preservation of as much of the capsular remnants as possible, as they may add more stability to the iris-claw lens. Intracameral pilocarpine was injected to constrict the pupil. A cohesive high molecular weight viscoelastic (Healon GV®, AMO, USA) was repeatedly injected to deepen the AC and maintain space; it was carefully removed at the end of the procedure to avoid a postoperative rise of intraocular pressure (IOP). The iris-claw IOL was introduced into the AC through a 6-mm scleral tunnel. With gentle manipulation, one haptic was tilted down and pushed under the iris while holding the optic with a lens forceps, and then it was tilted up to produce an indent in the iris. Simultaneously, a Sinskey hook was passed through the paracentesis of the same side, and the iris was enclosed into the haptic claw with a gentle push using the Sinskey hook. With a similar maneuver, the other haptic enclosure was carried out. One or more iridotomies were performed to reduce the risk of pupillary block. The scleral wound was sutured with interrupted 10-0 nylon sutures.
Postoperative follow-up
Patients were examined at 1 day, 3 days, 1 week, 2 weeks, 1 month, and 6 months postoperatively. Prednisolone acetate (R/Pred Forte®-Allergan) and gatifloxacin (R/Zymar®-Allergan) eye drops were given postoperatively five times daily together with tobramycine/dexamethasone (R/Tobradex®-Allergan) ointment at bed time for 3 weeks. BCVA, IOP, tissue reaction, and stability of the IOL were studied at each follow-up visit.
Results
This interventional case series comprised 17 eyes of 9 microspherophakic patients. Eight patients, belonging to two families, had familial microspherophakia and one patient had Marfan's syndrome. The mean age of the patients was 28 ± 15 (range: 13–43) years; the majority of patients (59% of the cases) were in the age group of 18–32 years. The male to female ratio in the study was 9:8. The follow-up period ranged from 4 to 18 months (mean: 8 months). One eye of a familial microspherophakic patient had posterior dislocation of the lens and gave a history of minor trauma. Indications of surgery were an intermittent pupillary block and secondary glaucoma in four eyes, cataract in two eyes, posterior dislocation of the lens in one eye, myopic astigmatism in six eyes, corneo-lenticular touch in one eye, and prophylactic removal in the remaining three eyes.
The main outcome measures were surgical time, postoperative BCVA, mean IOP, and intra- and postoperative complications.
The mean surgical time of the operation was 18 ± 4.5 min. The mean preoperative BCVA was 0.28 ± 0.24. Postoperatively, all the cases had a BCVA better than preoperative visual acuity with a mean of 0.9 ± 0.07 after 6-month follow-up. Fig. 3 shows the change in mean BCVA over the follow-up period. The mean preoperative IOP was 19.82 ± 13.43 mmHg. Transient elevation of IOP was recorded in two cases (12%) in the 1st week only, and it was medically controlled. Early postoperative hypotony was noticed in one eye (6%). The mean IOP at the end of the 1st postoperative week was 10.82 ± 1.88 mmHg, and after 6 months following the operation, it was 13.7 ± 1.53 mmHg. Fig. 4 shows the change in the mean IOP over the follow-up period. The mean postoperative astigmatism was 1.25 ± 1.75 D which was calculated after removal of the sutures. No cases of postoperative macular edema, pigment dispersion, or corneal decompensation were encountered in this study.
Figure 3.
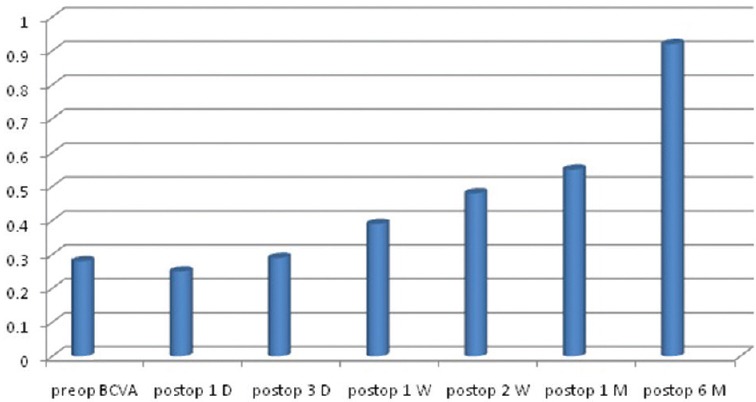
The change in mean best-corrected visual acuity over the follow-up period
Figure 4.
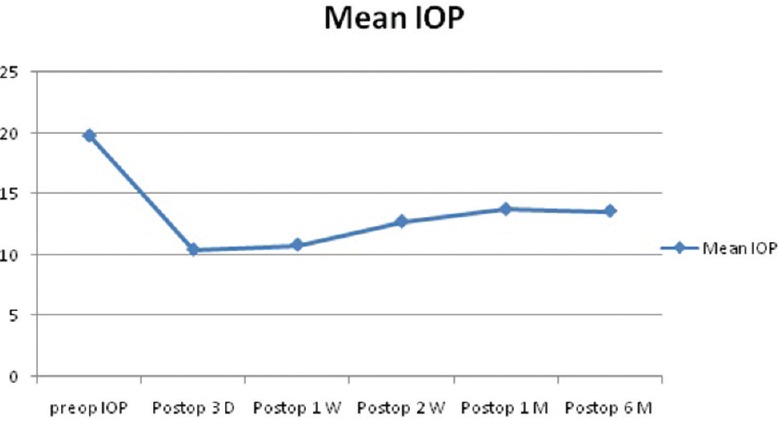
The change in mean intraocular pressure over the follow-up period
No intraoperative complications were encountered in any of the cases. Postoperative slight temporary pupil ovalization occurred in two eyes (12%). All the IOLs were well centered and stable at the end of the follow-up period. One IOL developed iris disengagement of one of the haptics, which was successfully re-engaged using the same technique as that of the primary procedure. Fig. 5 shows a postoperative photograph from the 1-month follow-up visit.
Figure 5.
Postoperative photograph from the 1-month follow-up visit
Discussion
Faulty development of lens zonules during embryogenesis is believed to be the cause of microspherophakia, which can cause pupillary block glaucoma, high myopia, corneo-lenticular touch, and other complications in the eye.
Regardless of the indication for lens extraction in such cases, the method of extraction is more relevant to the surgeon. Clear lens phacoemulsification with IOL implantation carries many risks and surgical challenges. Capsulorhexis is difficult, and iris hooks are required to stabilize the bag during lens matter removal. The option of stabilizing the capsular bag with a capsular tension ring is an additional challenging issue because of the small capsular bag. Moreover, phacodonesis typically persists after surgery unless a sclerally fixed capsule tension ring is used, which requires more time and surgical skills.[10] In this study, an automated anterior vitreorrhexis and lensectomy were performed in all cases to avoid these surgical challenges. The removal of lens matter was performed by automated aspiration, without the vitrectomy function, to maintain the posterior capsule integrity as much as possible, with the aim of reducing the risk of intraoperative loss of lens matter into the vitreous cavity and adding more stability to the IOL after its implantation. This maintained the integrity of the posterior capsule, which actually helped to prevent posterior dislocation of the IOL in one of our cases when one of the haptics became disengaged from the iris a few days after surgery.
The surgical options to correct aphakia in cases with inadequate capsular support include an AC IOL, scleral-sutured PC IOL, or an iris-sutured PCIOL.[11]
Although it is technically easier to implant an ACIOL, these IOLs have the disadvantage of having a physical location closer to the endothelium and inability to be implanted in eyes with angle pathologies. In addition, appropriate sizing is a concern, as angle-to-angle dimensions vary considerably between patients, thus leading to inherent risks of corneal decompensation, new-onset or worsening glaucoma, and chronic inflammation.[12]
Scleral-sutured PCIOLs have the advantage of being anatomically closer to the original lens location, enjoying good visual results, and are appropriate for young aphakic patients. However, they are technically challenging to insert, with an increased risk of IOL tilt, intraocular hemorrhage, suture breakage, and endophthalmitis.[13]
Iris suturing positions the IOL near where a capsular IOL would be, without the risk of scleral suture pass. Although less demanding than scleral suturing, iris fixation can be technically challenging through a limbal incision and there is a potential for iris chafing, pigment dispersion, and chronic inflammation.[12,14] As with any sutured IOL, suture breakage and slippage of the haptic through the suture knot are also concerns.
Jose et al. studied the safety, efficacy, and stability of retropupillary iris fixation of iris-claw lenses. Most of the problems and complications with iris-fixated IOL were solved with improved design, manufacturing techniques, and surgical techniques.[15] More than 80% of the cases in our series achieved a postoperative visual acuity of 0.3 or better.
Gonnermann et al. in 2012 concluded that the retropupillary iris-claw IOL provided good visual outcomes with a favorable complication rate and can be used for a wide range of indications in eyes without adequate capsule support.[16]
Acar et al. studied the use of secondary iris-claw IOL implantation for the correction of aphakia after pars plana vitrectomy, and they concluded that this technique is clinically safe and effective for the correction of aphakia in vitrectomized eyes without capsular support.[17]
Conclusion
The retropupillary iris-claw lens has the advantage of being a simple technique with a true PC IOL location and few intra- and post-operative complications. We believe it is a better option than an angle-supported, scleral- or iris-sutured IOL. This technique is promising and is suggested to be the preferred method of PC lens implantation in eyes with compromised zonular or capsular support.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ben Yahia S, Ouechtati F, Jelliti B, Nouira S, Chakroun S, Abdelhak S, et al. Clinical and genetic investigation of isolated microspherophakia in a consanguineous Tunisian family. J Hum Genet. 2009;54:550–3. doi: 10.1038/jhg.2009.75. [DOI] [PubMed] [Google Scholar]
- 2.Nirankari MS, Maudgal MC. Microphakia. Br J Ophthalmol. 1959;43:314–6. doi: 10.1136/bjo.43.5.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaushik S, Sachdev N, Pandav SS, Gupta A, Ram J. Bilateral acute angle closure glaucoma as a presentation of isolated microspherophakia in an adult: Case report. BMC Ophthalmol. 2006;6:29. doi: 10.1186/1471-2415-6-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Haddad C, Khatib L. Vitrectorhexis and lens aspiration with posterior chamber intraocular lens implantation in spherophakia. J Cataract Refract Surg. 2012;38:1123–6. doi: 10.1016/j.jcrs.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 5.Kumar A, Duvvari MR, Prabhakaran VC, Shetty JS, Murthy GJ, Blanton SH. A homozygous mutation in LTBP2 causes isolated microspherophakia. Hum Genet. 2010;128:365–71. doi: 10.1007/s00439-010-0858-8. [DOI] [PubMed] [Google Scholar]
- 6.Burakgazi AZ, Ozbek Z, Rapuano CJ, Rhee DJ. Long-term complications of iris-claw phakic intraocular lens implantation in Weill-Marchesani syndrome. Cornea. 2006;25:361–3. doi: 10.1097/01.ico.0000178724.04070.ce. [DOI] [PubMed] [Google Scholar]
- 7.Simões PS, Ferreira TB. Iris-fixated intraocular lenses for ametropia and aphakia. Med Hypothesis Discov Innov Ophthalmol. 2014;3:116–22. [PMC free article] [PubMed] [Google Scholar]
- 8.Yasar T. Lensectomy in the management of glaucoma in spherophakia: Is it enough? J Cataract Refract Surg. 2003;29:1052–3. doi: 10.1016/s0886-3350(03)00397-3. [DOI] [PubMed] [Google Scholar]
- 9.Hsu HY, Edelstein SL, Lind JT. Surgical management of non-traumatic pediatric ectopia lentis: A case series and review of the literature. Saudi J Ophthalmol. 2012;26:315–21. doi: 10.1016/j.sjopt.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhattacharjee H, Bhattacharjee K, Medhi J, DasGupta S. Clear lens extraction and intraocular lens implantation in a case of microspherophakia with secondary angle closure glaucoma. Indian J Ophthalmol. 2010;58:67–70. doi: 10.4103/0301-4738.58477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wagoner MD, Cox TA, Ariyasu RG, Jacobs DS, Karp CL American Academy of Ophthalmology. Intraocular lens implantation in the absence of capsular support: A report by the American Academy of Ophthalmology. Ophthalmology. 2003;110:840–59. doi: 10.1016/s0161-6420(02)02000-6. [DOI] [PubMed] [Google Scholar]
- 12.Condon GP, Masket S, Kranemann C, Crandall AS, Ahmed II. Small-incision iris fixation of foldable intraocular lenses in the absence of capsule support. Ophthalmology. 2007;114:1311–8. doi: 10.1016/j.ophtha.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 13.Cellini M, Strobbe E, Toschi PG, Campos EC. Secondary IOL implantation without capsular support: A laser flare cell meter study. ISRN Ophthalmol 2011. 2012:653246. doi: 10.5402/2011/653246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaiura TL, Seedor JA, Koplin RS, Rhee MK, Ritterband DC. Complications arising from iris-fixated posterior chamber intraocular lenses. J Cataract Refract Surg. 2005;31:2420–2. doi: 10.1016/j.jcrs.2005.06.048. [DOI] [PubMed] [Google Scholar]
- 15.Jose JC, Velasco F, Manaro F. Secondary Artisan-Verisyse aphakic lens implantation. J Cataract Refract Surg. 2005;31:2266–71. doi: 10.1016/j.jcrs.2005.06.047. [DOI] [PubMed] [Google Scholar]
- 16.Gonnermann J, Klamann MK, Maier AK, Rjasanow J, Joussen AM, Bertelmann E, et al. Visual outcome and complications after posterior iris-claw aphakic intraocular lens implantation. J Cataract Refract Surg. 2012;38:2139–43. doi: 10.1016/j.jcrs.2012.07.035. [DOI] [PubMed] [Google Scholar]
- 17.Acar N, Kapran Z, Altan T, Kucuksumer Y, Unver YB, Polat E. Secondary iris claw intraocular lens implantation for the correction of aphakia after pars plana vitrectomy. Retina. 2010;30:131–9. doi: 10.1097/IAE.0b013e3181b32eef. [DOI] [PubMed] [Google Scholar]


