Abstract
This case report aims to highlight the role of photodisruptive neodymium-doped yttrium-aluminum-garnet (Nd:YAG) (1064 nm) laser in the treatment of bleb dysesthesia, which occurs in overhanging blebs or with perilimbal spread. Although treatment of such dysesthetic blebs with laser photocoagulation has been previously described, cases where the height of bleb precludes laser penetration, desired effect might not be seen. We herein describe a technique using a combination of photocoagulative (532 nm) and photodisruptive (1064 nm) Nd:YAG laser for a high bleb migrating nasally and inferiorly along the limbus in a 64-year-old female, causing hypotony and consequent macular edema. Successful reduction could be achieved within a week of treatment. By 6 weeks, intraocular pressure improved to 8 mmHg, macular edema subsided, and visual acuity improved to 6/6. Although surgical procedures to correct bleb dysesthesia are available, laser procedures being quick outpatient modalities are more comfortable for the patients.
Keywords: Bleb dysesthesia, bleb overfiltration, bleb scarring, hypotony, photocoagulative (532 nm) neodymium-doped yttrium-aluminum-garnet laser, photodisruptive (1064 nm) neodymium-doped yttrium-aluminum-garnet laser
Despite advances in trabeculectomy, it is not uncommon to encounter elevated or migrating blebs causing dysesthesia and hypotony at times. Bleb dysesthesia refers to burning, foreign body sensation, tearing, pain, or ocular discomfort in an eye with a filtering bleb. Large blebs interfere with lid closure which leads to improper tear film distribution in the area of the bleb, thus causing corneal drying, epithelial defects, dellen, and bubble formation at the bleb-cornea interface.[1]
Topical lubrication is the initial treatment for bleb dysesthesia and it provides adequate relief of symptoms for most patients. Various surgical and nonsurgical laser treatment modalities have also been described for those not satisfactorily responding to conservative treatment.[1,2,3,4,5,6]
We hereby describe a technique for inferiorly spreading large blebs where photodisruptive neodymium-doped yttrium-aluminum-garnet (Nd:YAG) laser (1064 nm) was used for the first time in literature along with the already described photocoagulative frequency-doubled (532 nm) Nd:YAG laser.
Case Report
A 65-year-old female came to our clinic with the chief complaints of foreign body sensation and watering from her left eye (OS) for the past 2 months. She had undergone OS trabeculectomy, done elsewhere around 6 months back. The best-corrected visual acuity of the patient was 6/6 in right eye (OD) and 6/9 OS. The intraocular pressure (IOP) was 14 mmHg OD and 4 mmHg OS. On slit-lamp examination, there was a circumferential elevated and avascular bleb extending nasally and inferiorly along the limbus OS [Fig. 1a]. The anterior chamber was shallow but formed, and cornea was clear enough to allow the view of posterior segment. Bleb leak was ruled out by a negative Seidel's test. Optic disc OD revealed a vertical cup-to-disc ratio of 0.5 while the same was 0.9 OS with greater inferior neuroretinal rim loss. OD visual fields were normal but OS revealed a superior arcuate scotoma. Both eyes had an intraocular lens implant, done several years ago. The patient was instilling timolol maleate 0.5% eye drops BID OD and 2 hourly lubricating eye drops OS.
Figure 1.
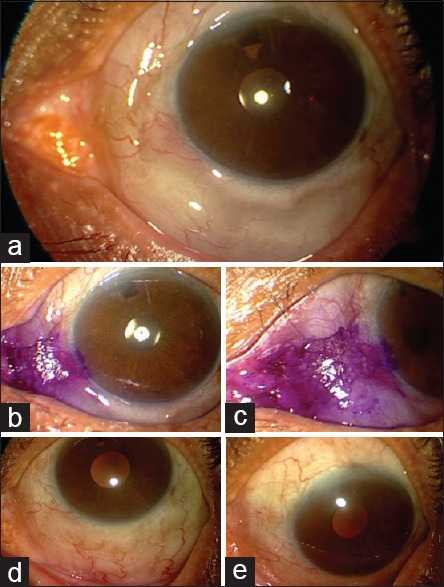
(a) Top row – slit-lamp photograph of left eye (at presentation) showing a diffuse high bleb spreading nasally and inferiorly along the limbus. (b and c) Middle row – preparation of eye for laser photocoagulation, by staining with gentian violet. Gentian violet has been shown to enhance laser penetration. (d and e) Bottom row – slit-lamp photograph of left eye (6-week postintervention) showing limitation of spread of bleb nasally as well as inferiorly
Bleb revision with a photocoagulative frequency-doubled Nd:YAG (532 nm) pea-green laser was planned the same day, in accordance to the technique previously described by the authors.[2] A few drops of topical anesthetic and antibiotic were instilled in the involved eye, and the nasal part of the bleb was painted with gentian violet (GV) to enhance the effect of the laser. A few shots were given (0.3 W for 0.15 s with a spot size of 300–500 µ) on the conjunctiva in a barrage fashion on the nasal aspect between the cornea and the canthus. However, no reduction in the bleb was seen immediately due to the excessively accumulated fluid [Fig. 1b and c]. A photodisruptive Nd:YAG (1064 nm) laser shot of 5 mJ energy in a single-burst mode was then given to puncture the inferior dependent portion of the bleb. The photocoagulative frequency-doubled Nd:YAG (532 nm) laser was then again attempted on the previous site, i.e., nasally, with success this time around. Antibiotic eye drops along with topical lubricants were used in QID dosage for the next 4 days.
At 1-week follow-up, bleb was found to have flattened both on the nasal as well as the inferior aspects [Fig. 1d and e]. Till the last follow-up at 3 months, visual acuity was noted 6/6 and the IOP had stabilized at 8 mm OS without any antiglaucoma medication. The macular edema had subsided by 6 weeks.
Discussion
Bleb dysesthesia is a commonly encountered problem in good filtering blebs due to the widespread use of antifibrotic agents, which at times may be severe enough to warrant a definitive intervention.[3] Nonsurgical and surgical techniques for the management of these symptomatic blebs include the use of lasers (Nd:YAG,[2,4] and argon[5] in the past), compression sutures, bleb window cryopexy, and bleb reduction. Overhanging blebs can also be surgically trimmed from the cornea with successful relief of symptoms and improvement in visual acuity. A procedure termed as bleb-limiting conjunctivoplasty for the treatment of circumferential filtering blebs has also been described.[6]
The authors have also previously described successfully a technique to reduce overhanging as well as nasally spreading blebs in a small series of patients.[2] The same technique was attempted in a similar way in this patient. However, due to height of the bleb, the effect of scarring did not get registered. An attempt to decrease height of the bleb on the nasal side was then made by draining the fluid out through a YAG puncture at the inferior dependent site, using photodisruptive Nd:YAG laser (1064 nm). This proved to be helpful, and as soon as the inferior bleb was drained, frequency-doubled Nd:YAG (532 nm) laser, i.e., photocoagulative laser along with the dye was again given on the nasal aspect, with success. It is important to watch for a scleral melt, in which case the anterior chamber is in direct communication with the bleb. The scleral melt is invariably seen in eyes with old trabeculectomy, and the area of scleral absence can usually be visualized subconjunctivally. In such a situation or where conjunctival bogginess precludes a proper view of scleral bed, inspite of attempting conjunctival blanching by applying pressure, this procedure should be avoided. Since this was not seen, rest of the procedure could be carried out in the described manner and required flattening achieved. In addition, the clinician should be prepared to deal with a loss of IOP control. IOP might rise due to limitation of the bleb area. Furthermore, a risk of infection and endophthalmitis exists due to creation of an iatrogenic leak. All of these should be discussed with the patient beforehand.
Though the surgical techniques have been well described to correct the condition, there is an inherent risk of bleb failure, need for IOP-lowering medications,[3] bleb leaks,[1] suture infection, and endophthalmitis.[7] In addition, laser treatment, being a quick outpatient procedure, is preferable for both the surgeon and patient. However, it is not uncommon to encounter high blebs precluding laser penetration leading to need for multiple treatment sessions[4] and also occasional failures. Use of photodisruptive Nd:YAG laser (1064 nm) can be considered in such cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Anis S, Ritch R, Shihadeh W, Liebmann J. Surgical reduction of symptomatic, circumferential, filtering blebs. Arch Ophthalmol. 2006;124:890–4. doi: 10.1001/archopht.124.6.890. [DOI] [PubMed] [Google Scholar]
- 2.Sony P, Kumar H, Pushker N. Treatment of overhanging blebs with frequency-doubled Nd:YAG laser. Ophthalmic Surg Lasers Imaging. 2004;35:429–32. [PubMed] [Google Scholar]
- 3.Lloyd M, Giegengack M, Morrison JC. Surgical reduction of dysesthetic blebs. 2008;126:1759–64. doi: 10.1001/archophthalmol.2008.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lynch MG, Roesch M, Brown RH. Remodeling filtering blebs with the neodymium: YAG laser. Ophthalmology. 1996;103:1700–5. doi: 10.1016/s0161-6420(96)30443-0. [DOI] [PubMed] [Google Scholar]
- 5.Fink AJ, Boys-Smith JW, Brear R. Management of large filtering blebs with the argon laser. Am J Ophthalmol. 1986;101:695–9. doi: 10.1016/0002-9394(86)90772-5. [DOI] [PubMed] [Google Scholar]
- 6.Rahman R, Thaller VT. Bleb-limiting conjunctivoplasty for symptomatic circumferential trabeculectomy blebs. J Glaucoma. 2003;12:272–4. doi: 10.1097/00061198-200306000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Quaranta L, Pizzolante T. Endophthalmitis after compression sutures for enlarged conjunctival filtration bleb following trabeculectomy. Ophthalmic Surg Lasers Imaging. 2009;40:432–3. doi: 10.3928/15428877-20096030-17. [DOI] [PubMed] [Google Scholar]


