Abstract
Objectives
1) Compare post-operative bleeding in the CHEER (Creating Healthcare Excellence through Education and Research) network between different age groups, diagnoses, and practice types 2) Report the incidence of bleeding by individual CHEER practice site based on practice guidelines.
Study Design
Retrospective data collection (RDC) database review of the CHEER network using ICD-9 and CPT codes related to tonsillectomy patients.
Setting
Multisite practice based network.
Subjects and Methods
8347 subjects underwent tonsillectomy as determined by procedure code within the RDC database and 107 had post-operative hemorrhage. These subjects had demographic information and related diagnoses based on CPT and ICD-9 codes collected. Post-operative ICD-9 codes and CPT codes were used to identify patients who also had post-operative bleed. Variables included age (<12 years vs. ≥ 12 years), diagnoses (infectious vs. non-infectious), and practice type (community vs. academic). Statistical analysis included multivariate logistic regression variables predictive of post-operative bleeding with p=<0.05 considered significant.
Results
Thirteen sites contributed data to the study (7 academic, 6 community). There was a post-operative bleeding for an overall bleed rate of 1.3%. Patients ≥12 years had a significantly increased bleed rate compared with the younger group (odds ratio 5.98: 95% CI [3.79, 9.44] p<0.0001). There was no significant difference in bleed rates when comparing practice or diagnoses.
Conclusion
A site descriptor database built to expedite clinical research can be used for practice assessment and quality improvement. These data was also useful to identify patient risk factors for post tonsillectomy bleed.
Keywords: tonsillectomy bleed rates, tonsillectomy complications, guidelines, academic sites, community sites, practice based network
Introduction
Tonsillectomy is one of the most common procedures performed in the field of otolaryngology-head and neck surgery. This procedure is primarily done for recurrent infections as well as for obstructive symptoms in both adults and pediatric patients and over 500,000 tonsillectomies are performed each year on patients under the age of 15.1 The procedure not only can decrease bacterial tonsillitis but also improve overall quality of life in patients.2 The procedure, however, is not without risk and one of the most significant risks is bleeding either during or after the procedure. There has been reported a 0.2%–2% risk of primary bleeding (within 24 hours of the procedure) and a 0.1%–3% risk of secondary bleeding (>24 hours from the procedure).3 This may result in readmission for control of the bleeding in hospital or the operative room. Although rare, post-tonsillectomy bleeding can be severe enough to result in death.4,5
Guidelines have been published by the American Academy of Otolaryngology—Head and Neck Surgery Foundation regarding indications for tonsillectomy in children.3 One of the recommendations put forth included the following: Clinicians who perform tonsillectomy should determine their rate of primary and secondary post-tonsillectomy hemorrhage at least annually (Statement 10). Currently, there is a need to obtain and assess data regarding this common procedure and rates of post-operative bleeding in current practices, both academic and community. In order to make meeting this recommendation feasible, the process to obtain and assess data cannot be onerous and labor intensive.
CHEER (Creating Healthcare Excellence through Education and Research) is a practice-based research network that was established to facilitate advancements in otolaryngology-head and neck surgery, and is funded through the National Institute on Deafness and other Communication Disorders (NIDCD). As a network, it has grown to currently encompass 30 sites that spans 19 states includes over 200 otolaryngologists, 100 audiologists, and 50 Speech Language Pathologists. As its vital component, the retrospective data collection (RDC) project serves as a capacity descriptor and holds more than 277,519 unique patients with demographics, ICD-9, and CPT codes. Published in 2011, the CHEER Otology Data Collection project further demonstrated the network’s capacity to move from retrospective RDC data to effectively recruit and quickly gather patient-related data for future prospective studies.6
The CHEER RDC database holds many of the variables that could potentially be queried to explore practice performance metrics for national guidelines, such as post-tonsillectomy bleeding rates. This could also provide the catalyst to improve quality of patient care though examining ways to lower the rate. For example, those practices that have a significantly lower rate of bleeding can be asked about their practices/technique to identify “best practices” (positive deviants) that could improve other practices to decrease their site bleeding rates.7
The overall objective is to report the incidence of post-tonsillectomy bleeding in patients at CHEER sites, as recommended by national guidelines. We postulated that there would be differences in bleeding rates among CHEER sites. These differences could be due to variability among clinical diagnosis and patient ages. We hypothesized that practitioners can use CHEER RDC database to identify risk factors for post-tonsillectomy bleeding. We anticipate that this work will not only provide opportunities to evaluate national guidelines, but also begin to identify areas of quality improvement regarding post-tonsillectomy bleeding rates for CHEER sites.
Methods
This study was evaluated by the Duke University School of Medicine IRB and deemed to be exempt research. The CHEER retrospective data collection (RDC) database was utilized. The RDC database includes de-identified patient data of at least one calendar year (2011–2012 or 2012–2013) from participating CHEER sites. These data include administrative, demographic (i.e. age, gender), diagnostic, and procedural data.6
The RDC was queried for patients with a tonsillectomy procedure. Tonsillectomy could be done solely or also done in conjunction with other procedures such as adenoidectomy. These included both CPT codes (ie, 42820, 42821, 42825, 42826) and ICD-9 codes (ie, 28.2, 28.3).
From the initial dataset of patients undergoing tonsillectomy procedure, patients with codes indicative of post-operative bleeding requiring hospital stay or operative intervention were queried (ie, ICD-9 28.7, 998.11 and CPT 42960, 42961, 42962). This indicates clinically significant bleeding that would require reevaluation in the clinical setting resulting in hospital stay or operative intervention. Each bleed was counted individually, not by patient. There were no patients with multiple bleeds. 129–130 Patients were grouped based by those ≥12 years and those <12 years of age. The 12 year mark was based on the CPT codes for tonsillectomy (ie, 42820 vs. 42821). The included CHEER sites were also divided into the type of practice (academic vs. community).
Associated diagnoses were grouped into infectious vs. non-infectious. The infectious diagnoses included chronic maxillary sinusitis (473.0), chronic adenotonsillitis (474.9), chronic tonsillitis (474.00) and peritonsillar abscess (474). Non-infectious diagnoses included otitis media with effusion (381.10), adenoid hypertrophy (474.12), adenoid and tonsil hypertrophy (474.10), tonsil hypertrophy (474.11), sleep apnea (780.52), and snoring (786.09).
Statistical Analysis
Statistically analysis of bleeding rates using multivariate logistic regression included comparisons between the following variables: age (<12 and ≥12), site type (academic vs. community), and diagnosis type (infectious vs. non-infectious). A p-value < 0.05 was considered significant. Odds ratio and 95% confidence intervals (95% CI) were also calculated. A distribution graph was also generated to plot the bleed rate among the individual sites.
Results
A total of 13 sites met inclusion criteria and had evaluable data regarding patients having tonsillectomy. Seven sites were academic practices while six were community practices. There were total of 8347 tonsillectomy patients with 107 patients having post-operative bleeding for an overall bleed rate of 1.3%.
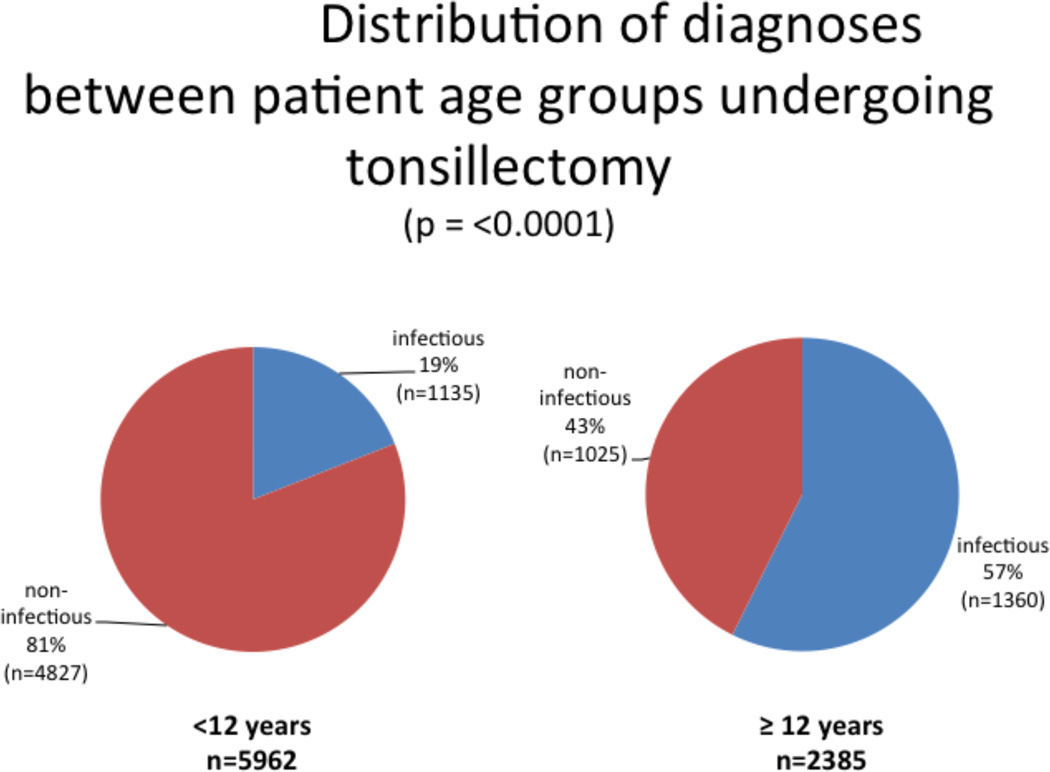
In the younger group, 81% (n=4827) of the total patients (n=5962) had non-infectious diagnoses while 19% (n=1135) of patients had infectious diagnoses. In the older group, there were a total of 2385 patients of which 43% (n=1025) had non-infectious diagnoses and 57% (n=1360) had infectious diagnoses. The diagnoses distribution between age groups was statistically significant (p=<0.0001). Figure 1 demonstrates the distribution of diagnoses (infectious vs. non-infectious) among the different age groups.
Figure 1.
Distribution of diagnoses between patient age groups undergoing tonsillectomy. The distribution of infectious and non-infectious diagnoses among older patients (≥ 12 years) and young patients (< 12 years) is significantly different (p=0.0001).
There were 30 bleeds from a total of 5962 tonsillectomy patients < 12 years old (0.5%) while there were 77 bleeds from 2385 patients ≥12 years (3.2%). Comparing age groups, patients ≥12 years had a significantly increased bleed rates compared with the younger group (p=<0.0001, odds ratio 5.98 95%CI [3.79, 9.44])
Analysis of bleed rates for diagnoses type resulted in 59 bleeds from a total of 2841 infectious related diagnoses (2.4%). There were 48 bleeds from 5506 non-infectious related diagnoses (0.9%). There was no statistical difference among these rates (p=0.16).
The RDC database demonstrated 64 post-operative bleeds in 4521 patients treated at community sites (1.4%). In comparison, there were 43 postoperative bleeds in 3835 patients treated at academic sites (1.1%). There was no statistical difference between practice type in which the tonsillectomy was performed (p=0.61). The multivariate logistic regression data for the age, diagnosis, and site type are listed in the table.
Table.
| Obs | Variable | Odds Ratio | 95% Lower Confidence Limit |
95% Upper Confidence Limit |
p-value |
|---|---|---|---|---|---|
| 1 | Age | 5.984 | 3.791 | 9.444 | <.0001 |
| 2 | Diagnosis | 1.346 | 0.888 | 2.042 | 0.1618 |
| 3 | Site type | 1.110 | 0.743 | 1.660 | 0.6096 |
Multivariate logistic regression was used to examine the predictors of post-operative bleeding. The predictors examined are age (< 12 vs ≥ 12), diagnosis (infectious vs. non-infectious) and site type (academic vs community). Age is the only significant predictor with those greater than 12 having 6 times the odds of having post-operative bleeding.
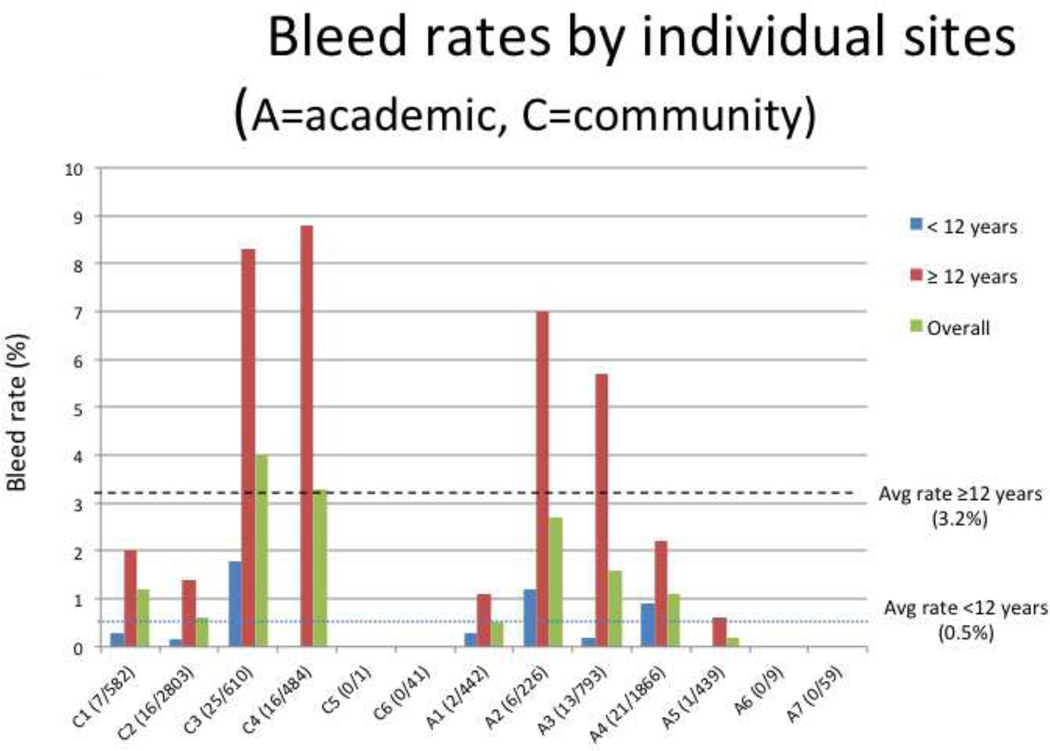
Individual sites were graphed together along with the average bleed rates for patients <12 years and ≥12 years. There are four community type practices (C1–4) and five academic practices (A1–5) that had more than 100 patients having tonsillectomy. All included sites demonstrated a higher bleed rate for the older group (range 1.1–8.8%) compared with the younger group (0–1.2%) (p=<0.0001, odds ratio 5.98 95%CI [3.79, 9.44]). The remaining four sites each had no bleeding cases from a total of 9 (A6), 59 (A7), 1 (C5) and 41 (C6) tonsillectomy cases. This specific site comparison of bleed rates is shown in Figure 2.
Figure 2.
Bleed rates by individual sites. There are six community sites (C1–6) and seven academic sites (A1–7). Individual bleeding rates for < 12 years, ≥ 12 years and overall are shown for each site. Average bleeding rate for < 12 years (0.5%), and ≥ 12 years (3.2%) is shown for comparison. Numbers in parenthesis are the total post-operative bleed cases over the total number of cases at the specific site.
Discussion
This research demonstrates the feasibility of using a practice based network database to examine performance as recommended by national guidelines regarding post-tonsillectomy bleed rates. Overall, this work demonstrates that the CHEER RDC is a useful construct for comparing post-operative bleeding rates between practices. Although primary and secondary bleed rates could not be assessed due to the lack of time information in the RDC database, we feel the rates we are able to report meet the overall intent of Guideline 10. Furthermore, we provide individual site bleeding rates for patients <12 as well as ≥12 years of age over a one year period.
Within the CHEER network, our results demonstrate a significant difference in post-tonsillectomy bleed rates: 0.5% for patients <12 years and 3.2% for those ≥12 years of age (p= <0.0001). This rate is similar to other reports in the literature examining post-tonsillectomy bleeding in these age groups.8,9 This work also revealed that in patients ≥12 years that there is 6 times the odds of having a post-operative bleed. We speculate that the reason for the increased bleed rate may be due to higher systolic pressures in older patients. Furthermore, there is a larger area exposed after tonsillectomy as well as larger caliber vessels in older patients compared to younger patients.
There was a significant difference in the distribution of diagnoses types (infectious vs. non-infectious) between the two age groups (p=<0.0001). Those in the older group had a more evenly distributed pattern of infectious and non-infectious diagnoses (43% and 57% respectively). The younger group had 75% of patients having a non-infectious diagnoses. In 2012, Perkins et al. reported that a non-infectious diagnosis (ie, obstructive sleep apnea) resulted in a significantly lower bleeding rate than an infectious diagnosis (ie, chronic tonsillitis).10 Further work pinpointing diagnoses with higher bleed rates may prove useful in future studies and in care processes. Among the CHEER sites, there were no significant difference of bleed rates between tonsillectomy procedures performed at academic vs. community sites (p=0.59).
These important research findings were produced using the existing RDC database and exemplifies the power of even a limited data registry as the foundation for ongoing quality improvement and data registry initiatives. This data was easily generated, available to sites, and can be used to track quality improvement over time. Future steps allow for the participating sites to know where they compare with other CHEER sites within Figure 2. This work allows for opportunities to examine practice patterns at sites that are outliers provide further research questions. For example, do the sites with higher bleed rates practice a different technique for tonsillectomy compared to the sites that have a lower rate of bleeding?11 Furthermore, do post-operative bleed instructions or protocols differ at sites which would impact how rates are measured? Having data at a site specific level allows for further considerations on how to improve practice patterns. This will not only benefit patient care, but also allow for a decrease in health care expenditures. Indeed, it has been estimated that the cost for control of post-tonsillectomy bleeding in a child to be $150212 and $6388 for adults.13
Limitations of the study are centered on the limited data elements of the CHEER database. As mentioned, not having the exact date of the visit limited our ability to look at the timing of the bleed. Additionally, when CHEER was first conceived, the network focused on otology and neurotology (and was later expanded to all of otolaryngology at the approval of NIDCD) and therefore data for some conditions is only available from certain sites. Some CHEER sites may only focus on a certain area of the specialty (e.g. otology) and did not contribute patients for this study. There is also another potential limitation in that there is an inability to track patients who present for post-operative bleeding at sites outside of the CHEER network. This may underestimate the overall rates at sites and could be highly variable based on geographical location, access to care, and insurance policies. As with all data sets, the data is only as accurate as the codes that are collected and entered. For example, a physician may have coded chronic tonsillitis (474.00) for a patient. However, based clinical information, it may have been more accurate to have coded the patient as tonsillar hypertrophy (474.11)
Another limitation of this study is that is does not account for differences among individual surgeon practices. If there are a number of surgeons performing tonsillectomy at a specific practice site, there may be variances among individual surgeon bleed that may unduly impact the bleed rate from the site as a whole. It is hoped that despite this limitation, the information provided at the site level would be an impetus to examine ways for all the members of the group to share best practices and to improve their practice if indicated. Having this type of data allows for a conversation to begin on improving practice outcomes on an individual level.
Obtaining and importing current information on a real-time basis to the RDC database could provide a solution to some of the aforementioned limitations. This emphasizes the need for automated approaches that can accurately query existing electronic medical records such that data can be extracted in an efficient manner. The CHEER Task Force and executive leadership are currently examining opportunities that could accomplish this goal.
In summary, we present data examining the post-tonsillectomy bleed rate from the CHEER practice based research network. The findings not only are consistent with published rates, but provide individual sites information based on published guidelines. Furthermore, the data presents opportunities to research practice patterns that can further decreased post-operative bleeding rates for patients undergoing tonsillectomy. Research performed in practice networks (ie, CHEER) such as this current work will be vital in a healthcare environment that focus on quality outcomes and improvement rather than fee-for-service.14
Acknowledgments
We would like to thank Ross McKinney, MD, for his thoughtful input and comments and Maragatha Kuchibhatla, PhD. for her comments and statistical support. The views expressed in this article are those of the author and do not necessarily represent the views of the Department of Veterans Affairs or the United States government.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
References
- 1.Mora R, Jankowska B, Mora F, Crippa B, Dellepiane M, Salami A. Effects of tonsillectomy on speech and voice. J Voice. 2009;23:614–618. doi: 10.1016/j.jvoice.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Witsell DL, Orvidas LJ, Stewart MG, et al. Quality of life after tonsillectomy in adults with recurrent or chronic tonsillitis. Otolaryngol Head Neck Surg. 2008;138(1 Suppl):S1–S8. doi: 10.1016/j.otohns.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Baugh RF, Archer SM, Mitchell RB, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;144(1 Suppl):S1–S30. doi: 10.1177/0194599810389949. [DOI] [PubMed] [Google Scholar]
- 4.Windfuhr JP. Serious complications following tonsillectomy: how frequent are they really? ORL J Otorhinolaryngol Relat Spec. 2013;75:166–173. doi: 10.1159/000342317. [DOI] [PubMed] [Google Scholar]
- 5.Goldman JL, Baugh RF, Davies L, et al. Mortality and major morbidity after tonsillectomy: etiologic factors and strategies for prevention. Laryngoscope. 2013;123:2544–2553. doi: 10.1002/lary.23926. [DOI] [PubMed] [Google Scholar]
- 6.Witsell DL, Rauch SD, Tucci DL, et al. The Otology Data Collection project: report from the CHEER network. Otolaryngol Head Neck Surg. 2011;145:572–580. doi: 10.1177/0194599811416063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soderman AC, Odhagen E, Ericsson E, et al. Post-tonsillectomy haemorrhage rates are related to technique for dissection and for haemostasis. An analysis of 15734 patients in the National Tonsil Surgery Register in Sweden. Clin Otolaryngol. 2015;40:248–254. doi: 10.1111/coa.12361. [DOI] [PubMed] [Google Scholar]
- 8.Kim DW, Koo J-W, Ahn S-H, Lee CH, Kim J-W. Difference of delayed post-tonsillectomy bleeding between children and adults. Auris Nasus Larynx. 2010;37:456–460. doi: 10.1016/j.anl.2009.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Bhattacharyya N, Kepnes LJ. Revisits and postoperative hemorrhage after adult tonsillectomy. Laryngoscope. 2014;124:1554–1556. doi: 10.1002/lary.24541. [DOI] [PubMed] [Google Scholar]
- 10.Perkins JN, Liang C, Gao D, Shultz L, Friedman NR. Risk of post-tonsillectomy hemorrhage by clinical diagnosis. Laryngoscope. 2012;122:2311–2315. doi: 10.1002/lary.23421. [DOI] [PubMed] [Google Scholar]
- 11.Gysin C, Dulguerov P. Hemorrhage after tonsillectomy: does the surgical technique really matter? ORL J Otorhinolaryngol Relat Spec. 2013;75:123–132. doi: 10.1159/000342314. [DOI] [PubMed] [Google Scholar]
- 12.Curtis JL, Harvey DB, Willie S, et al. Causes and costs for ED visits after pediatric adenotonsillectomy. Otolaryngol Head Neck Surg. 2015;152:691–696. doi: 10.1177/0194599815572123. [DOI] [PubMed] [Google Scholar]
- 13.Seshamani M, Vogtmann E, Gatwood J, Gibson TB, Scanlon D. Prevalence of complications from adult tonsillectomy and impact on health care expenditures. Otolaryngol Head Neck Surg. 2014;150:574–581. doi: 10.1177/0194599813519972. [DOI] [PubMed] [Google Scholar]
- 14.Mahant S, Keren R, Localio R, et al. Variation in quality of tonsillectomy perioperative care and revisit rates in children's hospitals. Pediatrics. 2014;133:280–288. doi: 10.1542/peds.2013-1884. [DOI] [PubMed] [Google Scholar]