Abstract
Objective
The value of antiangiogenic inhibitors for patients with recurrent ovarian cancer has not been completely affirmed. Therefore, we aimed to assess the effectiveness and toxicities of various antiangiogenic drugs for the treatment of recurrent ovarian cancer.
Methods
In this meta-analysis, we searched PubMed, EMBASE, and the Cochrane Central Register of Controlled Trials databases for complete randomized controlled trials. The searches were extended to May 15, 2016. The risk of bias of the included studies was evaluated via a Cochrane systematic evaluation, and the statistical analyses were performed using RevMan 5.2 software.
Results
In total, we included 8 randomized controlled trials involving 3,211 patients and divided them into 3 groups, vascular endothelial growth factor receptor inhibitors (VEGFRIs), vascular endothelial growth factor (VEGF) inhibitors (bevacizumab), and angiopoietin inhibitors (trebananib). The progression-free survival improved significantly in all the groups being given antiangiogenic drugs (hazard ratio [HR]: 0.55, 95% confidence interval [CI]: 0.45–0.67, I2=0%, P<0.00001 for the VEGFRI group; HR: 0.53, 95% CI: 0.45–0.63, I2=51%, P<0.00001 for the VEGF inhibitor group; HR: 0.67, 95% CI: 0.58–0.77, I2=0%, P<0.00001 for the trebananib group). Overall survival was obviously prolonged in the VEGFRI (HR: 0.76, 95% CI: 0.59–0.97, I2=0%, P=0.03), the VEGF inhibitor (HR: 0.87, 95% CI: 0.77–0.99, I2=0%, P=0.03), and trebananib groups (HR: 0.81, 95% CI: 0.67–0.99, I2=0%, P=0.04). The incidence of grade 3/4 side effects was different among the 3 groups, for example, proteinuria, hypertension, gastrointestinal perforation, and arterial thromboembolism were presented in the VEGF inhibitor group. Increased incidences of fatigue, diarrhea, and hypertension were seen in the VEGFRI group, and the trebananib group had a higher incidence of hypokalemia.
Conclusion
This meta-analysis showed that antiangiogenic drugs improved the progression-free survival. The VEGFRI, bevacizumab, and trebananib groups showed increased overall survival. Adding antiangiogenic drugs to chemotherapy treatment resulted in a higher incidence of grade 3/4 side effects, but these were manageable.
Keywords: antiangiogenesis, recurrent ovarian cancer, progression-free survival, overall survival, toxicity
Introduction
Currently, ovarian cancer is the leading cause of cancer-related death in middle-aged and elderly females.1 Despite the significantly improved prognosis of advanced ovarian cancer, it will recur in >50% of women within 18–24 months.2 The treatment of relapsing ovarian cancer mainly consists of a single or a combination of intravenous chemotherapy. The addition of antiangiogenic drugs in the treatment of relapsed ovarian cancer has not yet been fully defined.3
According to our search results, 8 randomized controlled trials (RCTs) have been conducted on this topic.4–11 To the best of our knowledge, there are 2 pathways for neovascularization, including the vascular endothelial growth factor (VEGF) and angiopoietin pathways. VEGF signaling through VEGF receptors (VEGFRs) activated downstream signal transduction molecules phospholipase C-γ(PLC-γ), PI3K, Akt, Ras, Src, and MAPK and regulated cell proliferation, migration, survival, and vascular permeability.10,12–15 Therefore, we divided these RCTs into 3 groups, including a VEGF receptor inhibitor (VEGFRI) group, VEGF inhibitor group, and angiopoietin group.
Several meta-analyses have been conducted on a single antiangiogenic drug or advanced ovarian cancer. However, this meta-analysis aimed to estimate the efficacy and toxicity of various antiangiogenic drugs for the treatment of patients with recurrent ovarian cancer.
Methods
The PubMed, EMBASE, and Cochrane Central Register of Controlled Trials databases were comprehensively searched from January 2000 to May 2016, without language restrictions. The search was limited to RCTs with or without antiangiogenic therapy for recurrent ovarian cancer. The search terms included “ovarian cancer”, “ovarian carcinoma”, “ovarian neoplasm”, “ovarian tumor”, “angiogenesis”, “angiogenic”, and “randomized controlled trial”. Abstracts from the annual meetings of the American Society of Clinical Oncology, the European Society of Medical Oncology, and the Society of Gynecologic Oncology from within the past five years were also searched.
Study selection and inclusion criteria
The inclusion criteria were as follows: 1) the research subjects were patients with recurrent ovarian cancer, including platinum-sensitive and platinum-resistant patients; 2) chemotherapy interventions with or without antiangiogenic drugs; and 3) RCTs. The articles were obtained for an independent assessment of eligibility by 2 of the authors (SY Yi and LJ Zeng). A difference of opinion was resolved via consultation with a third author (Y Kuang), if necessary.
Data extraction and quality assessment
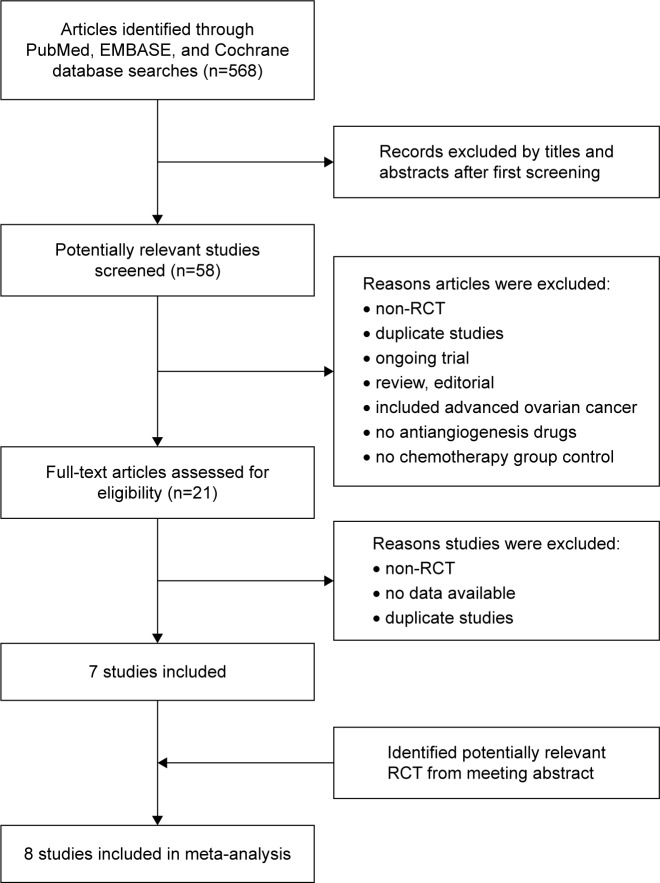
Two of the authors (SY Yi and LJ Zeng) independently extracted the data on the basis of the following: first author, year of publication, age, pathology, sample size, intervention, and outcome data. As shown in Figure 1, we assessed the quality of the eligible studies according to the Cochrane Collaboration’s risk of bias tool in the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0. We resolved any disagreements by discussing them with a third review author (Y Kuang).
Figure 1.
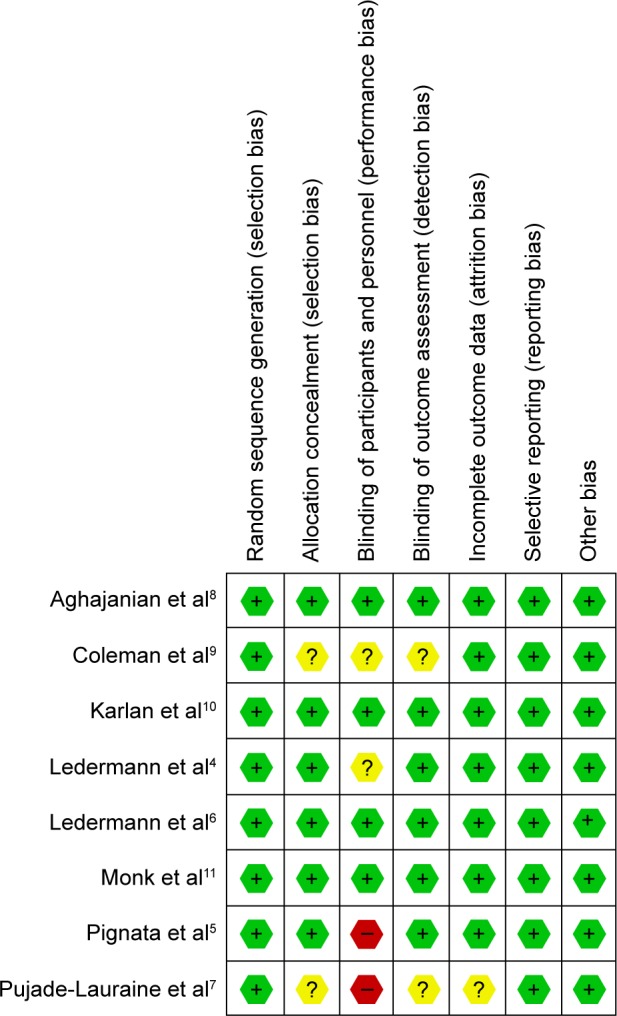
Assessment of the quality of the included randomized controlled trials: low risk of bias (green hexagons), unclear risk of bias (yellow hexagons), and high risk of bias (red hexagons).
Statistical analysis
The pooled hazard ratios (HRs) and 95% confidence interval (95% CI) for the progression-free survival (PFS) or overall survival (OS) and the relative risks (RRs) for adverse events from all the articles were calculated using RevMan 5.2. The heterogeneity among the studies was estimated using the I2 index. We use the fixed-effects model if I2≤50%, otherwise the random-effects model was applied. The statistical analyses were performed using the RevMan 5.2 software.
Results
Search and study characteristics
The search process of this study is presented in Figure 2, and the characteristics of the RCTs used are presented in Table 1. After searching the literature, only 8 RCTs containing 3,211 patients with recurrent ovarian cancer were included in this analysis. We divided them into the following 3 groups according to the different active targets of the antiangiogenic drugs: 3 RCTs with VEGFRIs,4–6 3 RCTs with VEGF inhibitors,7–9 and 2 RCTs with angiopoietin inhibitors.10,11 One RCT applied antiangiogenic drugs during the maintenance phase,4 but the other drugs were fully employed from the beginning of therapy to disease progression in the other 7 RCTs. The evaluation of the quality of the RCTs included in this study is shown in Figure 1. We were not concerned about publication bias due to the fact that only 8 articles were included.16
Figure 2.
Flowchart showing study selection procedure.
Abbreviation: RCT, randomized controlled trial.
Table 1.
The basic characteristics of the included randomized controlled trials
| Reference | Agent type | Median age (years)
|
Sample size (n)
|
Platinum (sensitive/resistant) (n)
|
Histologic type (n)
|
Intervention group | Control group | |
|---|---|---|---|---|---|---|---|---|
| Exp/Con | Exp/Con | Exp | Con | Exp/Con | ||||
| Ledermann et al4 | VEGFRIs | 60/63 | 43/40 | 26/17 | 23/17 | Serous (34/35) Mucinous (1/0) Endometrioid (0/1) Clear cell (0/2) Others (8/1) Missing (0/1) |
Chemotherapy followed by nintedanib maintenance | Chemotherapy followed by placebo |
| Pignata et al5 | VEGFRIs | 56/58 | 37/36 | 0/37 | 1/35 | Serous (26/24) Mucinous (1/0) Endometrioid (4/2) Undifferentiated (3/1) Clear cell (1/3) Mixed (0/3) Transitional (1/2) Mixed Mullerian (1/1) |
Paclitaxel + pazopanib until disease progressed | Paclitaxel until disease progressed |
| Ledermann et al6 | VEGFRIs | 62/62 | 338/118 | 338/0 | 118/0 | Serous (245/87) Mucinous (4/0) Endometrioid (16/3) Undifferentiated (2/3) Clear cell (13/3) Others (56/21) Not available (2/1) |
Platinum-based chemotherapy + cediranib for 6 cycles followed by cediranib or placebo maintenance | Platinum-based chemotherapy + placebo for 6 cycles followed by placebo maintenance |
| Pujade-Lauraine et al7 | VEGF inhibitor | 62/61 | 179/182 | 0/179 | 0/182 | Serous (156/152) Endometrioid (8/9) Clear cell (4/12) |
Single-agent chemotherapy + bevacizumab until disease progressed | Single-agent chemotherapy until disease progressed |
| Aghajanian et al8 | VEGF inhibitor | 60.5/61.5 | 242/242 | 242/0 | 242/0 | Serous (189/202) Mucinous (3/1) Endometrioid (13/16) Transitional cell (2/2) Clear cell (9/6) Mixed (6/5) Others (20/10) |
Carboplatin + gemcitabine + bevacizumab for 6–10 cycles followed by bevacizumab maintenance | Carboplatin + gemcitabine for 6–10 cycles |
| Coleman et al9 | VEGF inhibitor | 60/60 | 335/339 | 335/0 | 339/0 | Unclear | Carboplatin + paclitaxel + bevacizumab followed by bevacizumab maintenance | Paclitaxel + carboplatin |
| Karlan et al10 | Angiopoietin inhibitor | 60/62 | 106/55 | 54/51 | 30/24 | Serous (53/34) Endometrioid (13/3) Clear cell (1/2) Mucinous (1/1) Unclassified (33/13) Unavailable (5/2) |
Paclitaxel + trebananib until disease progressed | Paclitaxel until disease progressed |
| Monk et al11 | Angiopoietin inhibitor | 60/59 | 461/458 | 223/238 | 212/246 | Serous (385/388) Endometrioid (29/26) Undifferentiated (15/10) Transitional (4/2) Others (28/32) |
Paclitaxel + trebananib until disease progressed | Paclitaxel until disease progressed |
Abbreviations: Exp, experiment group; Con, control group; VEGFRIs, vascular endothelial growth factor receptor inhibitors; VEGF, vascular endothelial growth factor.
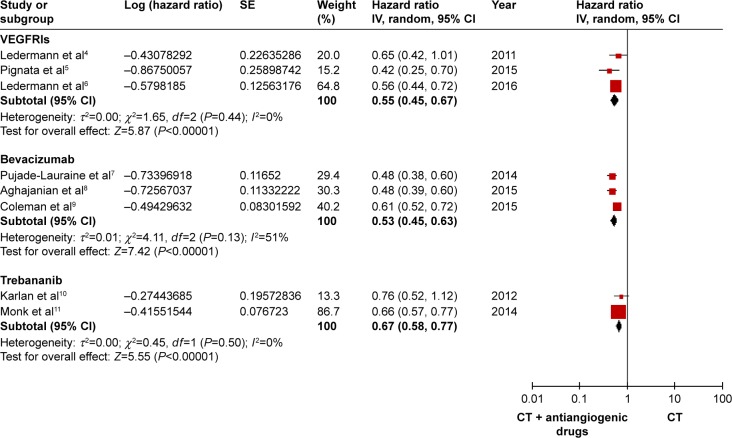
PFS
A random-effects model was applied with high heterogeneity, and all the RCTs included reported the HRs and 95% CIs of the PFS. As illustrated in Figure 3, compared with chemotherapy alone, the PFS improved significantly in all the groups, as follows: HR: 0.55, 95% CI: 0.45–0.67, I2=0%, P<0.00001 for the VEGFRI group; HR: 0.53, 95% CI: 0.45–0.63, I2=51%, P<0.00001 for the VEGF inhibitor group; and HR: 0.67, 95% CI: 0.58–0.77, I2=0%, P<0.00001 for the trebananib group.
Figure 3.
Forest plot of progression-free survival data for different antiangiogenic drugs.
Abbreviations: SE, standard error; CI, confidence interval; IV, instrumental variable; VEGFRIs, vascular endothelial growth factor receptor inhibitors; CT, chemotherapy.
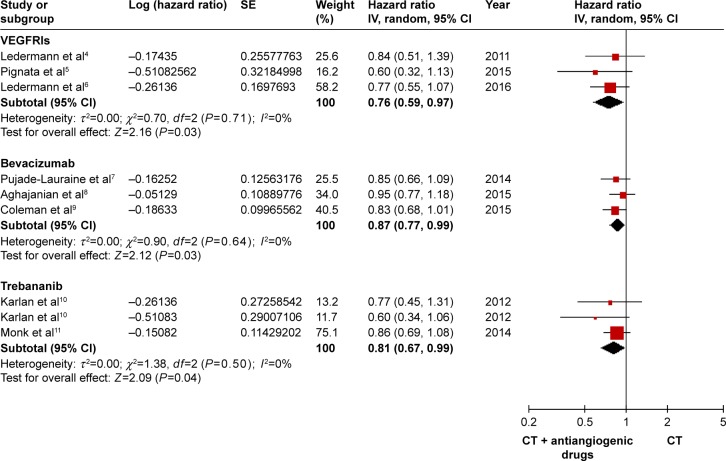
OS
The OS was determined by using a fixed-effects model attributed to low heterogeneity among the studies. Only 1 study did not report the OS.5 The OS was obviously prolonged in the VEGFRI (HR: 0.76, 95% CI: 0.59–0.97, I2=0%, P=0.03), the VEGF inhibitor group (HR: 0.87, 95% CI: 0.77–0.99, I2=0%, P=0.03), and the trebananib group (HR: 0.81, 95% CI: 0.67–0.99, I2=0%, P=0.04). The outcomes are shown in Figure 4.
Figure 4.
Forest plot of overall survival data for different antiangiogenic drugs.
Abbreviations: SE, standard error; CI, confidence interval; IV, instrumental variable; VEGFRIs, vascular endothelial growth factor receptor inhibitors; CT, chemotherapy.
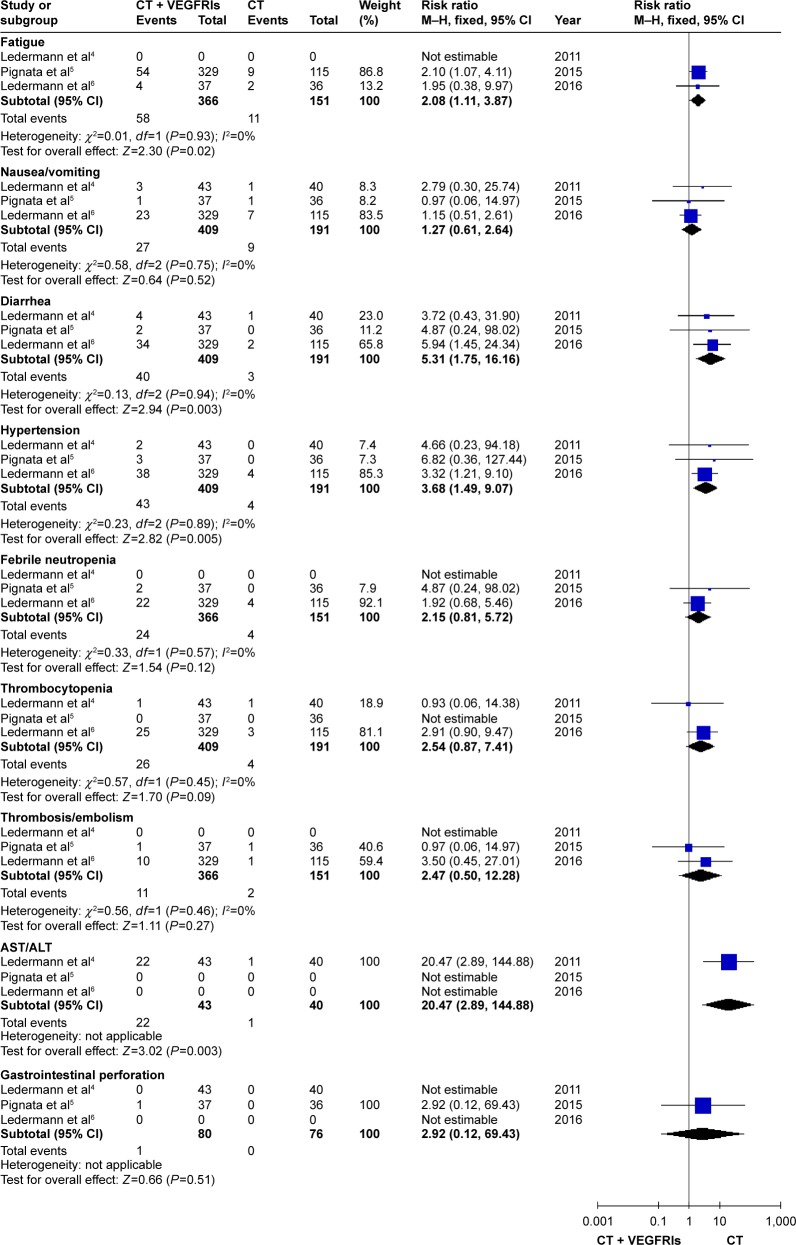
Toxicity (adverse effect grade ≥3, except gastrointestinal perforation [GIP] grade ≥1)
As presented in Figure 5, the rates of hypertension (RR: 3.68, 95% CI: 1.49–9.07, I2=0%, P=0.005), fatigue (RR: 2.08, 95% CI: 1.11–3.87, I2=0%, P=0.02), and diarrhea (RR: 5.31, 95% CI: 1.75–16.16, I2=0%, P=0.003) were numerically higher in the VEGFRI treatment group. In addition, the nintedanib as a VEGFRI was associated with higher incidences of hepatotoxicity (RR: 20.47, 95% CI: 2.89–144.88, P=0.003).
Figure 5.
The forest plot for evaluating the toxicity (the VEGFRI group).
Abbreviations: CT, chemotherapy; VEGFRI, vascular endothelial growth factor receptor inhibitor; CI, confidence interval; AST, aspartate transaminase; ALT, alanine transaminase; M–H, Mantel–Haenszel.
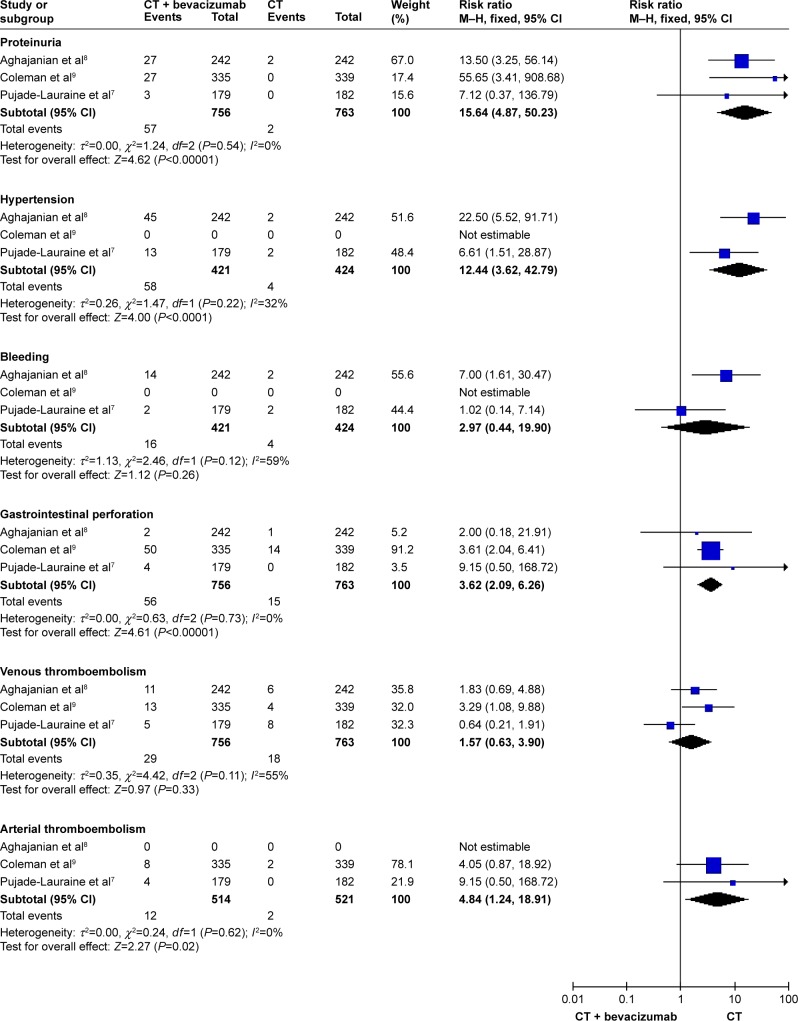
With regard to the VEGF inhibitor group, the proteinuria (RR: 15.64, 95% CI: 4.87–50.23, I2=0%, P<0.00001), hypertension (RR: 12.44, 95% CI: 3.62–42.79, I2=32%, P<0.0001), arterial thromboemboli (RR: 4.84, 95% CI: 1.24–18.91, I2=0%, P=0.02), and GIP (RR: 3.62, 95% CI: 2.09–6.26, I2=0%, P<0.00001) were significantly different (Figure 6).
Figure 6.
The forest plot for evaluating the toxicity (the bevacizumab group).
Abbreviations: CT, chemotherapy; CI, confidence interval; M–H, Mantel–Haenszel.
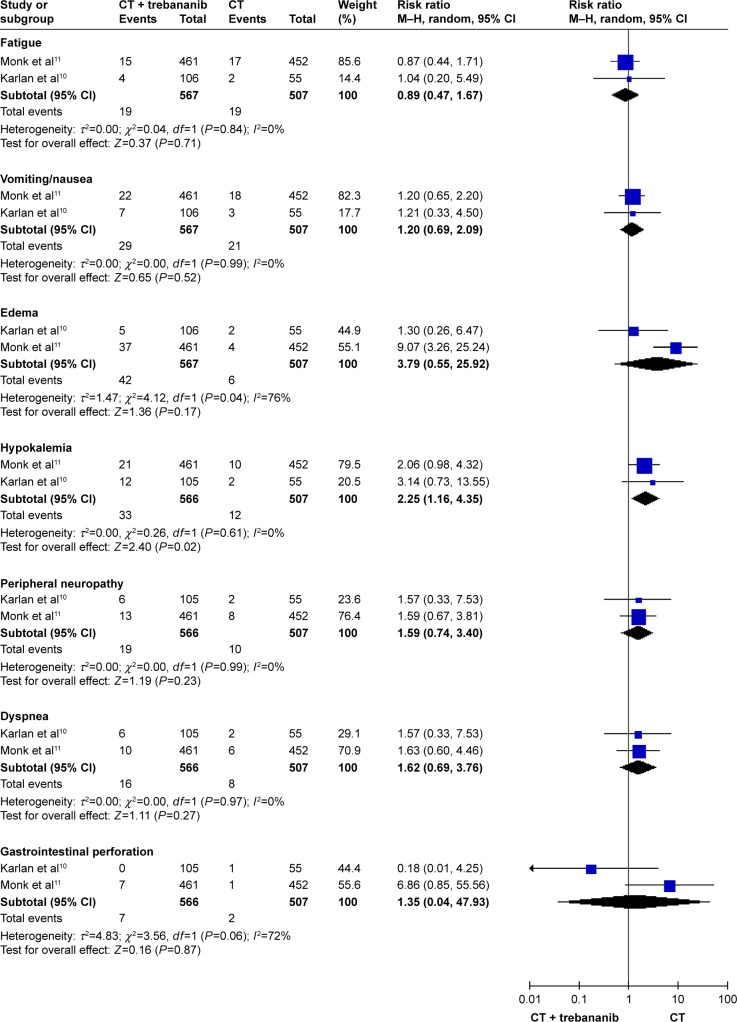
As shown in Figure 7, the trebananib treatment may cause a higher risk of hypokalemia (RR: 2.25, 95% CI: 1.16–4.35, I2=0%, P=0.02).
Figure 7.
The forest plot for evaluating the toxicity (the trebananib group).
Abbreviations: CT, chemotherapy; CI, confidence interval; M–H, Mantel–Haenszel.
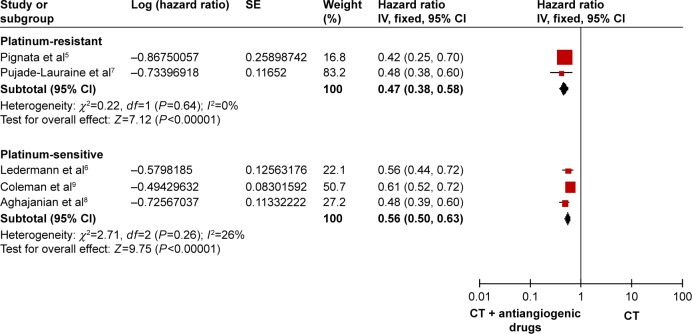
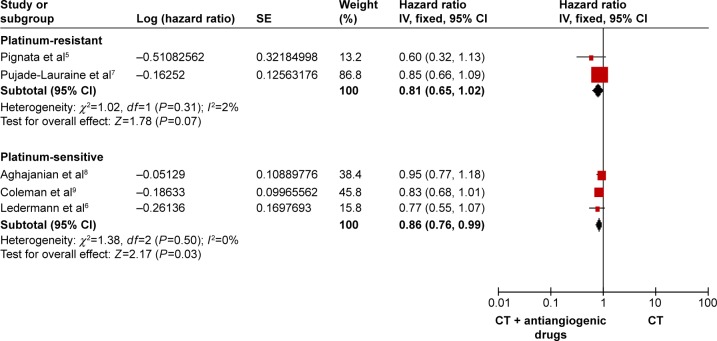
Subgroup analysis
We divided the RCTs into 2 subgroups, 2 RCTs with platinum-resistant5,7 and 3 RCTs with platinum-sensitive.6,8,9 As shown in Figure 8, the PFS improved significantly both the platinum-resistant and the platinum-sensitive recurrent ovarian cancer (HR: 0.47, 95% CI: 0.38–0.58, I2=0%, P<0.00001 for the platinum-resistant group; HR: 0.56, 95% CI: 0.50–0.63, I2=26%, P<0.00001 for the platinum-sensitive group). As presented in Figure 9, the OS was clearly better in the platinum-sensitive group (HR: 0.86, 95% CI: 0.76–0.99, P=0.03), with no obvious statistical significance for OS in the platinum-resistant group (HR: 0.81, 95% CI: 0.65–1.02, I2=2%, P=0.07).
Figure 8.
Forest plot for progression-free survival based on whether patients were platinum-resistant or -sensitive.
Abbreviations: SE, standard error; CI, confidence interval; IV, instrumental variable; CT, chemotherapy.
Figure 9.
Forest plot for overall survival based on whether patients were platinum-resistant or -sensitive.
Abbreviations: SE, standard error; CI, confidence interval; CT, chemotherapy.
Discussion
Ovarian cancer is the leading cause of cancer deaths in women,1 and many patients with advanced ovarian cancer will undergo recurrences with chemotherapy resistance. Ovarian carcinoma is a complicated disease, controlled by multiple mutating genes, and there are no clear molecular therapeutic targets. Therefore, a new promising therapy targeting the tumor microenvironment has been proposed. Neovascularization is crucial for tumor growth and metastasis, and various antiangiogenic drugs have subsequently emerged.17–19
To the best of our knowledge, VEGF plays an important role in neovascularization. VEGF signals through VEGFRs and upregulates downstream signaling pathways. Another pathway uses angiopoietin, which is a regulator of tumor angiogenesis. Based on the mechanism of vascularization, we divided the RCTs into 3 groups to perform our analysis.10,12–14 In this meta-analysis, the PFS showed significant improvement with antiangiogenic therapy in those patients with relapsed ovarian cancer. The OS was clearly better in the VEGFR inhibitor, the bevacizumab and trebananib groups. In addition, both the platinum-resistant and the platinum-sensitive subgroups had a benefit in the PFS. The OS was obviously improved in the platinum-sensitive group; however, it was not statistically significant in the platinum-resistant group.
In our study, the incidences of grade 3/4 toxicity were higher when compared with chemotherapy alone but were manageable; however, the type and incidence of side effects (≥ grade 3) varied with the different anti-angiogenic drugs. Furthermore, the incidence of GIP in the bevacizumab group was higher than the VEGFRIs and trebananib groups. Oncologists gradually realized the significant risk of GIP. They reported that the rate of GIP in recurrent ovarian cancer varies from 0% to 11.4%. However, in large Phase III clinical trials, the rate of perforation is 0%–2.6%. GIPs carry a high rate of mortality, especially in the setting of recurrent, platinum-resistant ovarian cancer.20 Overall, the application of antiangiogenic drugs remains controversial. Bevacizumab is the most successful antiangiogenic drug, but it is not currently the upfront chemotherapy, because it has shown no statistical significance in improving the OS in recurrent ovarian cancer according to original studies.3,7–9
Antiangiogenic therapy could be applied for recurring ovarian cancer, if the patient has previously received antiangiogenic therapy; however, the impact on the efficacy is not known. Both Huijbers’s and Bergers’s studies have shown the role of tumor stromal cells in the resistance to antiangiogenic drugs, and the mechanisms for use are diverse, including endothelial (progenitor) cells, smooth muscle cells, pericytes, fibroblasts, immune cells, and platelets. Multiple mechanisms develop evasive or intrinsic resistance and finally become resistant to antiangiogenic therapy. Although the incidence of resistance to antiangiogenic therapy after previous antiangiogenic therapy is not clear, it is closely related to the prognosis of the patient with recurrent ovarian cancer. Currently, there are no relevant trials in the literature.3,21,22
Which recurrent patients benefit most from antiangiogenic therapy remains unclear. Abu-Jawdeh et al discovered that VEGF and its receptors were not expressed in benign ovarian tumors, with intermediate levels of expression shown in borderline ovarian tumors and strong expression shown in malignant cancer, via detection in the serum, ovarian tumor tissue, and ascites. Recently, Pasquet et al reported that ascites-derived stromal cells play a role in promoting tumor growth by inducing angiogenesis. Antiangiogenic therapy alone delays tumor tissue growth, narrows metastatic lesions, and reduces malignant peritoneal effusion. The research by Ferriss et al showed that patients with ascites treated with bevacizumab had significantly better PFS and OS, but the issue has not reached consistency.23–26
In addition to bevacizumab, there were several antiangiogenic drugs described in our meta-analysis. Therefore, the decision about selecting an appropriate antiangiogenic drug to obtain the most benefit for recurrent patients will be complicated. Both the characteristics of the patients and the toxicity of the drugs must be taken into account. Currently, only bevacizumab and pazopanib have been recommended for application in ovarian cancer by the National Comprehensive Cancer Network.3
In addition, the optimal doses and therapeutic time period have not yet been determined. In our meta-analysis, the doses and durations differed among the 8 RCTs we included in this study. The survival outcomes were improved with the use of antiangiogenic therapy as a maintenance therapy for patients with recurrent ovarian cancer. A previous meta-analysis, conducted by Qian et al, also confirmed that both the PFS and OS were improved in the antiangiogenic maintenance therapy group, when compared with the chemotherapeutic group alone.27,28 According to preclinical researches, tumor vessels were known to be leaky and dysfunctional, which disturb delivery of chemotherapy to tumor. Vascular normalization by crossover application of antiangiogenic therapy was proposed to increase the density of chemotherapeutic agents in tumor. Currently, clinical studies were not enough to prove the vascular normalization theory. Therefore, the effect of difference was still unknown between crossover and subsequent antiangiogenic therapy.29,30 In a word, a standard antiangiogenic regime has not yet been established.
Directly predicting the clinical efficacy of antiangiogenic drugs using biomarkers is currently under study, but the results do not look good. The measurement of serum-free VEGF was proposed first based on its easy accessibility and reasonable price. However, there is little predictive value as a serum biomarker due to its dynamic change between the total and free VEGF levels. Recently, 2 studies have recognized several biomarkers (mesothelin, FLT4, AGP, CA-125, and miR-378) that seem predictive of the benefits from the antiangiogenic treatment of ovarian cancer, but further larger population studies are required.31–33
Despite the fact that we only included RCTs to minimize bias in our meta-analysis, several potential limitations remain. Due to the disparate design of the research studies, characteristics of the recurrent patients, various ovarian tumor types, unclear International Federation of Gynecology and Obstetrics staging, and different doses and durations of the drugs, there was heterogeneity among all 8 studies.
Conclusion
The antiangiogenic therapy showed a clear improvement in the PFS in the treatment of relapsed ovarian cancer patients. In addition, the bevacizumab and trebananib groups showed prolonged OS. Antiangiogenesis as a targeted therapy seems to be promising, despite the many uncertainties put forth in our study.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Luvero D, Milani A, Ledermann JA. Treatment options in recurrent ovarian cancer: latest evidence and clinical potential. Ther Adv Med Oncol. 2014;6(5):229–239. doi: 10.1177/1758834014544121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Cancer Society Cancer facts and figures 2008. [Accessed December 31, 2008]. Available from: http://www.cancer.org/research/cancerfactsstatistics/cancerfacts-figures2008/index.
- 3.National Comprehensive Cancer Network NCCN Clinical practice Guidelines in Oncology: Ovarian Cancer Including Fallopian Tube Cancer and Primary Peritoneal Cancer. 2015. [Accessed 2, 2015]. Version 2. Available from: http://www.nccn.org.
- 4.Ledermann JA, Hackshaw A, Kaye S, et al. Randomized phase II placebo-controlled trial of maintenance therapy using the oral triple angiokinase inhibitor BIBF 1120 after chemotherapy for relapsed ovarian cancer. J Clin Oncol. 2011;29(28):3798–3804. doi: 10.1200/JCO.2010.33.5208. [DOI] [PubMed] [Google Scholar]
- 5.Pignata S, Lorusso D, Scambia G, et al. Pazopanib plus weekly paclitaxel versus weekly paclitaxel alone for platinum-resistant or platinum-refractory advanced ovarian cancer (MITO 11): a randomized, open-label, phase 2 trial. Lancet Oncol. 2015;16(5):561–568. doi: 10.1016/S1470-2045(15)70115-4. [DOI] [PubMed] [Google Scholar]
- 6.Ledermann JA, Embleton AC, Raja F, et al. Cediranib in patients with relapsed platinum-sensitive ovarian cancer (ICON6): a randomized, double-blind, placebo-controlled phase 3 trial. Lancet. 2016;387(10023):1066–1074. doi: 10.1016/S0140-6736(15)01167-8. [DOI] [PubMed] [Google Scholar]
- 7.Pujade-Lauraine E, Hilpert F, Weber B, et al. Bevacizumab combined with chemotherapy for platinum-resistant recurrent ovarian cancer: the AURELIA open-label randomized phase III trial. J Clin Oncol. 2014;32(13):1302–1308. doi: 10.1200/JCO.2013.51.4489. [DOI] [PubMed] [Google Scholar]
- 8.Aghajanian C, Goff B, Nycum LR, Wang YV, Husain A, Blank SV. Final overall survival and safety analysis of OCEANS, a phase 3 trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent ovarian cancer. Gynecol Oncol. 2015;139(1):10–16. doi: 10.1016/j.ygyno.2015.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coleman RL, Brady MF, Herzog TJ, et al. Gynecologic oncology; Presented at: Society of Gynecologic Oncology 2015 Annual Meeting on Women’s Cancer; March 28–31, 2015; Chicago, IL, USA. Abstract 3. [Google Scholar]
- 10.Karlan BY, Amit MO, Gary ER, et al. Randomized, double-blind, placebo-controlled phase II study of AMG 386 combined with weekly paclitaxel in patients with recurrent ovarian cancer. J Clin Oncol. 2012;30(4):362–371. doi: 10.1200/JCO.2010.34.3178. [DOI] [PubMed] [Google Scholar]
- 11.Monk BJ, Andrés P, Ignace V, et al. Anti-angiopoietin therapy with trebananib for recurrent ovarian cancer (TRINOVA-1): a randomized, multicenter, double-blind, placebo-controlled phase 3 trial. Lancet Oncol. 2014;15(8):799–808. doi: 10.1016/S1470-2045(14)70244-X. [DOI] [PubMed] [Google Scholar]
- 12.Papadopoulos N, Martin J, Ruan Q, et al. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF trap, ranibizumab, and bevacizumab. Angiogenesis. 2012;15(2):171–185. doi: 10.1007/s10456-011-9249-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holash J, Maisonpierre PC, Compton D, et al. Vessel cooption, regression, and growth in tumors mediated by angiopoietins and VEGF. Science. 1999;284(5422):1994–1998. doi: 10.1126/science.284.5422.1994. [DOI] [PubMed] [Google Scholar]
- 14.Lokadasan R, James FV, Narayanan G, Prabhakaran PK. Targeted agents in epithelial ovarian cancer: review on emerging therapies and future developments. Ecancer medical science. 2016;10:626. doi: 10.3332/ecancer.2016.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nilsson M, Heymach JV. Vascular endothelial growth factor (VEGF) pathway. J Thorac Oncol. 2006;1:768–770. [PubMed] [Google Scholar]
- 16.Song F, Eustwood AJ, Gilbody S, Duley L, Sutton AJ. Publication and related biases. Health Technol Assess. 2000;4(10):1–115. [PubMed] [Google Scholar]
- 17.Coleman RL, Monk BJ, Sood AK, Herzog TJ. Latest research and treatment of advanced-stage epithelial ovarian cancer. Nat Rev Clin Oncol. 2013;10(4):211–224. doi: 10.1038/nrclinonc.2013.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cancer Genome Atlas Research Network Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474(7353):609–615. doi: 10.1038/nature10166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hansen JM, Coleman RL, Sood AK. Targeting the tumor microenvironment in ovarian cancer. Eur J Cancer. 2016;56:131–143. doi: 10.1016/j.ejca.2015.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McClung EC, Wenham RM. Profile of bevacizumab in the treatment of platinum-resistant ovarian cancer: current perspectives. Int J Womens Health. 2016;8:59–75. doi: 10.2147/IJWH.S78101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huijbers EJ, van Beijnum JR, Thijssen VL, Sabrkhany S, Nowak-Sliwinska P, Griffioen AW. Role of the tumor stroma in resistance to anti-angiogenic therapy. Drug Resist Updat. 2016;25:26–37. doi: 10.1016/j.drup.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 22.Bergers G, Hanahan D. Modes of resistance to anti-angiogenic therapy. Nat Rev Cancer. 2008;8(8):592–603. doi: 10.1038/nrc2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abu-Jawdeh GM, Faix JD, Niloff J, et al. Strong expression of vascular permeability factor (vascular endothelial growth factor) and its receptors in ovarian borderline and malignant neoplasms. Lab Invest. 1996;74(6):1105–1115. [PubMed] [Google Scholar]
- 24.Yamamoto S, Konishi I, Mandai M, et al. Expression of vascular endothelial growth factor (VEGF) in epithelial ovarian neoplasms: correlation with clinicopathology and patient survival, and analysis of serum VEGF levels. Br J Cancer. 1997;76(9):1221–1227. doi: 10.1038/bjc.1997.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pasquet M, Golzio M, Mery E, et al. Hospicells (ascites-derived stromal cells) promote tumorigenicity and angiogenesis. Int J Cancer. 2010;126(9):2090–2101. doi: 10.1002/ijc.24886. [DOI] [PubMed] [Google Scholar]
- 26.Ferriss JS, Java JJ, Bookman MA, et al. Ascites predicts treatment benefit of bevacizumab in front-line therapy of advanced epithelial ovarian, fallopian tube, and peritoneal cancers: an NRG oncology/GOG study. Gynecol Oncol. 2015;139(1):17–22. doi: 10.1016/j.ygyno.2015.07.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khalique S, Hook JM, Ledermann JA. Maintenance therapy in ovarian cancer. Curr Opin Oncol. 2014;26(5):521–528. doi: 10.1097/CCO.0000000000000110. [DOI] [PubMed] [Google Scholar]
- 28.Qian X, Qin J, Pan S, Li X, Pan Y, Ma S. Maintenance therapy in ovarian cancer with targeted agents improves PFS and OS: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0139026. doi: 10.1371/journal.pone.0139026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 30.Jain RK. Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat Med. 2001;7:987–989. doi: 10.1038/nm0901-987. [DOI] [PubMed] [Google Scholar]
- 31.Jubb AM, Harris AL. Biomarkers to predict the clinical efficacy of bevacizumab in cancer. Lancet Oncol. 2010;11(12):1172–1183. doi: 10.1016/S1470-2045(10)70232-1. [DOI] [PubMed] [Google Scholar]
- 32.Chan JK, Kiet TK, Blansit K, et al. MiR-378 as a biomarker for response to anti-angiogenic treatment in ovarian cancer. Gynecol Oncol. 2014;133(3):568–574. doi: 10.1016/j.ygyno.2014.03.564. [DOI] [PubMed] [Google Scholar]
- 33.Collinson F, Hutchinson M, Craven RA, et al. Predicting response to bevacizumab in ovarian cancer: a panel of potential biomarkers informing treatment selection. Clin Cancer Res. 2013;19(18):5227–5239. doi: 10.1158/1078-0432.CCR-13-0489. [DOI] [PMC free article] [PubMed] [Google Scholar]