Abstract
Objective
To determine whether a social cognitive theory (SCT)-based intervention improves resistance training (RT) maintenance and strength, and reduces prediabetes prevalence.
Research design and methods
Sedentary, overweight/obese (BMI: 25–39.9 kg/m2) adults aged 50–69 (N = 170) with prediabetes participated in the 15-month trial. Participants completed a supervised 3-month RT (2×/wk) phase and were randomly assigned (N = 159) to one of two 6-month maintenance conditions: SCT or standard care. Participants continued RT at a self-selected facility. The final 6-month period involved no contact. Assessments occurred at baseline and months 3, 9, and 15. The SCT faded-contact intervention consisted of nine tailored transition (i.e., supervised training to training alone) and nine follow-up sessions. Standard care involved six generic follow-up sessions. Primary outcomes were prevalence of normoglycemia and muscular strength.
Results
The retention rate was 76%. Four serious adverse events were reported. After 3 months of RT, 34% of participants were no longer prediabetic. This prevalence of normoglycemia was maintained through month 15 (30%), with no group difference. There was an 18% increase in the odds of being normoglycemic for each % increase in fat-free mass. Increases in muscular strength were evident at month 3 and maintained through month 15 (P<0.001), which represented improvements of 21% and 14% for chest and leg press, respectively. Results did not demonstrate a greater reduction in prediabetes prevalence in the SCT condition.
Conclusions
Resistance training is an effective, maintainable strategy for reducing prediabetes prevalence and increasing muscular strength. Future research which promotes RT initiation and maintenance in clinical and community settings is warranted.
Trial Registration
ClinicalTrials.gov NCT01112709.
Introduction
The prevalence of diabetes among adults in the United States (US) is estimated to be 12.3%, and 25.9% among those aged 65 years or older [1]. Prediabetes, defined as impaired fasting glucose (IFG) or impaired glucose tolerance (IGT), affects more than one-third of US adults, and 51% of individuals aged 65 years or older [1]. Up to 70% of individuals with prediabetes may advance to type 2 diabetes [2]; within one year, the rate of progression is 5–10% [3].
The Community Preventive Task Force recommends intensive combined diet and physical activity promotion programs to reduce type 2 diabetes, with reversion to normoglycemia ranging from 20% to 52% depending upon program duration and intensity [4]. However, limited evidence is available to determine the optimal maintenance phase structure and the effectiveness of web-based programs targeting lifestyle change [4]. Clinical practice recommendations for diabetes prevention include lifestyle modification, specifically 5–10% weight loss and 30 minutes of moderate intensity physical activity per day [2, 5]. Yet weight reduction remains a challenge for most individuals, and a “portfolio of approaches” to prevent diabetes may be needed to maximize intervention reach and effectiveness [6].
Resistance training (RT) is increasingly recognized as an important treatment component for type 2 diabetes [5, 7, 8]. This mode of exercise is particularly beneficial for older, prediabetic adults given the loss of lean body mass and worsening of glucose tolerance with advancing age [9, 10]. Regular RT engagement (1–2 sessions per week) is associated with lower odds of impaired glucose metabolism [11] and all-cause mortality [12], and with improved physical functioning [13]. Despite these benefits, less than 10% of adults aged 65 years and older report engaging in muscle strengthening exercise two or more times per week [12].
Continuing the beneficial lifestyle outcomes evident in a supervised clinical setting to largely unsupervised community settings has been a challenge for diabetes prevention programs [14–16]. Furthermore, exercise adherence is rarely reported following supervised exercise intervention phases [17] in typical diabetes prevention programs. These issues also have been a focus of studies including individuals with type 2 diabetes, and were initially resistance training under supervision and then either trained at community facilities or at home [18, 19]. Some evidence of effectiveness for glycemic control was found, enhanced by theory-based behavior change procedures, though adherence to the established protocol varied [18, 19]. However, the standard protocol used in these studies involved training three times per week with between 24 to 32 sets per training session.
The Resist Diabetes trial was designed to assess if an RT protocol entailing training twice per week and involving 12 sets per session could reduce prediabetes prevalence and improve strength in a supervised clinical setting, and then be successfully translated and maintained without direct supervision in community settings by implementing a Social Cognitive Theory (SCT)-based maintenance intervention. Using results from this trial, we previously reported that the initiation of RT was associated with short-term changes in dietary intake (e.g., reduced intake of carbohydrates and total sugars [20], that short-term improvements in glucose tolerance with RT initiation may be limited to individuals with prediabetes who have IGT (vs isolated IFG) [21], RT adherence and cost estimates of the Standard and SCT-based intervention conditions [22], The current article presents the main trial outcomes. The primary objective of this trial was to determine whether an SCT-based intervention improves RT maintenance and muscular strength, and reduces prediabetes prevalence among older adults with prediabetes. It was hypothesized that SCT-based intervention will produce better outcomes than the Standard Care follow-up at 9-month and 15-month assessments.
Materials and methods
Study design
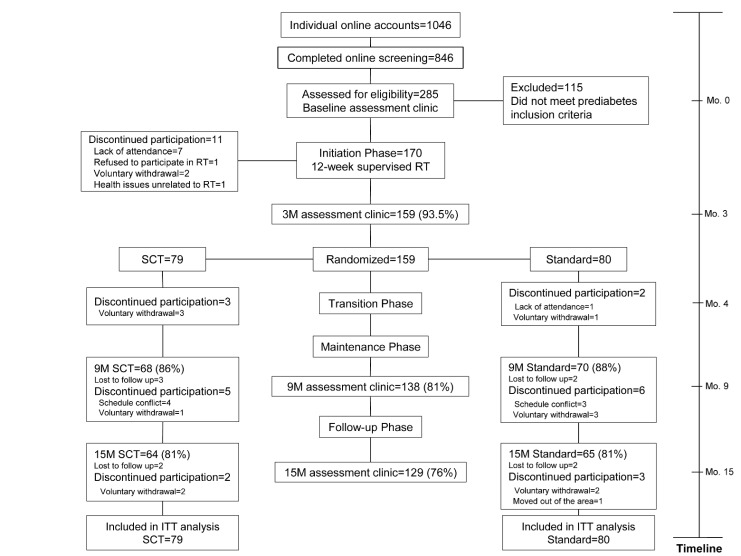
Resist Diabetes was a 15-month randomized controlled trial including 170 men and women aged 50–69 years (N = 170) with prediabetes, defined as exhibiting either IFG (fasting glucose = 95–125 mg/dl) and/or IGT (2-hour glucose = 140–199 mg/dl) [23], and who met all other inclusion criteria (described below). Following screening and baseline testing (Fig 1), participants first completed a 3-month initiation phase. Resistance training sessions were completed two times per week on nonconsecutive days, and were supervised by an American College of Sports Medicine-certified Personal Trainer in a laboratory/gym. The protocol conformed to recommended guidelines [24] and included the following exercises on Nautilus equipment: leg press, leg extension, seated leg curl, calf raise, chest press, lat pulldown, row, shoulder press, seated dip, lower back, abdominal crunch and rotary torso. Participants performed one set of all 12 exercises at moderate resistance for 8–12 repetitions (3-second concentric, 3-second eccentric contractions) with good form and a high degree of effort to concentric failure. To progress to the next phase of the study, participants were required to attend at least 17 of the 24 scheduled RT sessions (70% minimum adherence).
Fig 1. Resist Diabetes study consort diagram.
Abbreviations: RT = resistance training; 3M = 3-month; SCT = social cognitive theory group; 9M = 9-month; 15M = 15-month; ITT = intent-to-treat.
After the initiation phase, participants (N = 159; 94% retention) were randomly assigned (by ELM) to one of two RT transition and maintenance conditions for 6 months: 1) a Social Cognitive Theory (SCT)-based intervention delivered over nine transition sessions and nine brief maintenance sessions using interactive, self-regulation procedures (e.g., goal setting, monitoring, reporting, feedback, planning, problem solving) with tailored in-person and web-based feedback, 2) a standard, usual care condition consisting of four transition and two brief maintenance sessions with SCT content (e.g., didactic instruction in problem solving) and generic web-based tracking of RT sessions [22]. The study principal investigators (BMD and RAW), statistician co-investigator (JSS), and participants were blinded to group assignment. Participants transitioned from supervised training to training alone at a self-selected community facility during the maintenance phase and paid associated membership fees. In both conditions, contact ended after 6 months, but participants were expected to continue RT at their respective facilities and all participants continued to have access to the web-based RT tracking system. Assessments occurred at baseline and months 3 (post-initiation), 9 (post-maintenance intervention), and 15 (after 6 months of no contact). A detailed description of study procedures has been published [25].
Participants
Men and women aged 50–69 years were recruited from Roanoke, Virginia and its surrounding area using newspaper, workplace, and church advertisements and direct mailings between January 2011 and September 2012, and all follow-up assessments were completed by January 14 (trial ended as sample size was attained). Individuals were directed to a study information website, and if interested, they completed an online screening questionnaire (Fig 1). Internet access was required for participation as some intervention components were delivered online. Eligible individuals were apparently healthy (no known presence of heart disease), with no cardiovascular symptoms (e.g., chest discomfort, dizziness, shortness of breath). Inclusion criteria included a sedentary lifestyle (defined as moderate PA <120 min/week or vigorous PA <60 minutes/week), overweight or obese weight status (BMI 25–39.9 kg/m2), and not having engaged in RT in the past 12 months. Individuals who appeared eligible following the online screening were required to obtain medical clearance from their personal physician and were scheduled for baseline testing to determine prediabetes status. Only those meeting prediabetes criteria were eligible to participate.
Exclusion criteria were as follows: current smokers, cardiovascular disease diagnosis, pulmonary, liver or kidney disease, uncontrolled hypertension (BP>160/100 mmHg), diabetes or use of diabetes medications, conditions precluding RT such as major orthopedic injuries or musculoskeletal disabilities, and short-term use of any medications known to influence metabolism (e.g., beta blockers) or body weight (e.g., thyroid replacement, antidepressants). Individuals taking commonly prescribed medications (e.g., hormone replacement therapy) were eligible for participation if they had been on a stable dose of the medication for greater than one year. Individuals with hypertension whose blood pressure (BP) was adequately controlled (i.e., <140/<90 mm Hg) with antihypertensive medications were permitted to participate. The protocol was approved by the institutional review board (IRB) of Virginia Tech, and all participants gave written informed consent prior to enrollment.
Assessments
At each assessment period, participants completed online surveys to determine physical activity level [26] and health beliefs related to RT [27] prior to each scheduled laboratory assessment. Laboratory testing took place over two days. The first day of testing included a detailed health and medical history, assessment of height, weight, body mass index (BMI), and BP. Height was measured using a wall-mounted stadiometer and body mass was measured using a digital scale (Healthometer ProPlus™). Body mass index (BMI) was calculated as weight (kg)/height (m)2. Blood pressure was measured according to recommended guidelines [28] using an automated device (Dinamap Procare Model 9300, GE HealthCare, Milwaukee, WI). The mean of two consecutive readings was used.
Fasting glucose and glucose tolerance were assessed using a 2-hr oral glucose tolerance test (OGTT). After a baseline fasting glucose sample was collected, participants consumed an 8-ounce 75 g glucose beverage (Fisherbrand, Fisher Scientific, Hanover Park, IL) within the first 5 min of the test. Additional samples were obtained at minutes 10, 20, 30, 60, 90 and 120. Glucose concentrations (mg/dl) were determined using a YSI 2700 Select glucose analyzer (YSI Life Sciences, Yellow Springs, OH). Insulin and C-peptide concentrations were analyzed using commercially-available assay kits (ELISA, ALPCO; IMMULITE, Siemens). HOMA was calculated to assess insulin resistance [29]. Glucose, insulin and C-peptide area-under-the-curve (AUC) were determined using the trapezoidal method [30].
Adherence was determined using a time-line follow-back approach at the 9- and 15-month assessment time points. On a printed calendar, participants noted each day of RT within the past 30 days [25]. Dietary intake was assessed using three 24-hour dietary recalls. The first recall was obtained in-person by a trained research dietitian, and the second and third recalls were completed via phone by the same dietitian in the two-week period following the testing session. Printed food diagrams were used to assist in portion size estimation. Recalls were analyzed using the Nutrition Data System for Research software (NDS-R 2010, University of Minnesota, Minneapolis, MN).
The second day of testing, included assessments of waist circumference, body composition (dual-energy x-ray absorptiometry), and strength tests (3-repetition maximum [RM]), at the laboratory/gym. Waist circumference was measured using a Gulick tape measure at the level of the umbilicus and recorded as the mean of two measurements. Body fat percent, absolute fat mass and fat-free mass was assessed using dual-energy X-ray absorptiometry (DXA; GE Lunar Prodigy, Madison, WI). Strength change on the chest press and leg press resistance machines was assessed during a three-repetition maximum (3RM) test following ACSM guidelines [24].
Adverse events
Participants were instructed to immediately contact a member of the study staff by phone or email if a serious adverse event occurred; these were documented and reviewed by the study Medical Director to determine the appropriate course of action (e.g., discontinue training, medical follow-up).
Sample size and power calculations
With a minimum sample size of 110, our study was powered to detect significant group differences (80%) in change over the four assessment points for achievement of normal FPG, 2-hr plasma glucose concentration and increases in strength, assuming a maximum difference between the control and treatment group to be 15–20%, comparable to Cohen’s d of 0.6 [31]. To allow for a 35% attrition rate, we recruited a sample of 170 participants to ensure that we had complete data on 110 participants at all four assessment points of the study [25].
Statistical analysis
At month 3, a stratified random assignment procedure (generated by JSS) was used with sex and responsiveness (i.e., initial mean strength gains on chest press and leg press of <15%, 15% to <35%, or ≥35%) as randomization variables. No significant group or sex differences were found in participant characteristics at the time of randomization [25]. All analyses were conducted in STATA (version 14; StataCorp) using intention-to-treat and with 2-sided tests of α = .05. Linear mixed effects models were estimated to compare the outcomes between the two groups at baseline, month 3, 9, and 15. Random class effects were used to control for repeated measurements. The fixed effects parameters were group (SCT vs. Standard), month of assessment, and the interaction of group × time. Contrasts were used to estimate and test the Bonferroni-adjusted within-group differences. Secondary outcomes were analyzed using the same approach. Results are presented as the difference in regression coefficients, along with an overall test of interaction effect. For the proportion of participants who reverted to normoglycemia [5], we used a repeated measures generalized estimation model with xtgee procedure in STATA. Similar to the linear mixed models, this model included a random intercept to account for repeated measurements within participants, as well as fixed effects for group, time, and group × time interaction. The xtgee model controlled for sex, prediabetes phenotype at baseline and change in lean body mass percent over the three study phases. The results are presented as population-averaged odds ratios.
Results
Baseline and month 3 (i.e., at randomization) participant characteristics are provided in Table 1. Participants were predominantly non-Hispanic, white, college-educated, and female. Mean BMI was in the obese range, and mean waist circumference was indicative of visceral obesity [32]. Almost half of participants were taking antihypertensive medications, and one-third were using statins (Table 1). One participant in the Standard group was prescribed metformin at month 3 by her personal physician. Of the antihypertensive medications used by participants, one has been reported to increase type 2 diabetes risk (i.e., hydrochlorothiazide[HCTZ]) [33]. Six individuals in each group were taking HCTZ. With regard to prediabetes phenotype, most participants were categorized as either isolated IFG or combined IFG/IGT. Upon randomization at month 3, there were no group differences in participant characteristics [25].
Table 1. Resist Diabetes: Participant characteristics at Baseline and at Randomization (Month 3).
| At Baseline (n = 170) | At Randomization | ||
|---|---|---|---|
| Standard (N = 80) | SCT (N = 79) | ||
| Age (years) | 59.5 ±5.4 | 59.7 ±5.1 | 59.6 ±5.6 |
| Sex | |||
| Female | 124 (73%) | 57 (71%) | 58 (73%) |
| Male | 46 (27%) | 23 (29%) | 21 (27%) |
| Weight (kg) | 93.31 ±13.82 | 93.74 ±14.62 | 92.85 ±13.47 |
| BMI (kg/m2) | 32.95 ±3.77 | 33.02 ±3.87 | 32.99 ±3.93 |
| Blood Pressure (BP) | |||
| Systolic BP (mmHg) | 131 ±15 | 130 ±13 | 127 ±13 |
| Diastolic BP (mmHg) | 76 ±9 | 74 ±9 | 73 ±8 |
| Body composition | |||
| Fat percent (%) | 43.83 ±6.95 | 43.24 ±6.71 | 43.07 ±6.91 |
| Fat mass (kg) | 40.61 ±8.36 | 40.10 ±8.57 | 39.62 ±8.07 |
| Fat-free percent (%) | 56.16 ±6.96 | 56.76 ±6.71 | 56.93 ±6.91 |
| Fat-free mass (kg) | 52.09 ±10.37 | 52.72 ±10.77 | 52.72 ±10.69 |
| Waist Circumference (cm) | 109.08 ±10.31 | 108.90 ±10.63 | 107.56 ±10.67 |
| Strength | |||
| Chest press 3RM (kg) | 33.64 ±11.56 | 43.49 ±15.10 | 42.14 ±14.63 |
| Leg press 3RM (kg) | 140.99 ±35.90 | 167.23 ±37.63 | 165.44 ±41.20 |
| Blood measures | |||
| Fasting glucose (mg/dL) | 102 ± 8 | 100 ±10 | 102 ±10 |
| 2hr glucose (mg/dL) | 142 ± 36 | 136 ±37 | 133 ±35 |
| Fasting insulin (uIU/mL) | 15.2 ± 12.5 | 16.6 ±12.4 | 16.9 ±10.7 |
| 2hr insulin (uIU/mL) | 139.2 ±122.8 | 140.6 ±122.9 | 136.6 ±116.0 |
| HOMA-IR | 3.83 ±3.28 | 4.17 ±3.29 | 4.34 ±2.83 |
| Fasting C-peptide (ng/mL) | 3.99 ±2.11 | 3.89 ±1.87 | 3.89 ±1.55 |
| 2hr C-peptide (ng/mL) | 16.14 ±8.42 | 17.16 ±7.65 | 16.56 ±7.16 |
| Prediabetes criteria | |||
| Normal | 0 (0%) | 28 (35%) | 27 (34%) |
| IFG | 81 (48%) | 21 (26%) | 23 (29%) |
| IGT | 21 (12%) | 9 (11%) | 9 (11%) |
| Both IFG & IGT | 68 (40%) | 22 (28%) | 20 (25%) |
| Race | |||
| White | 160 (94%) | 75 (94%) | 74 (94%) |
| Black | 9 (5%) | 5 (6%) | 4 (5%) |
| Other | 1 (1%) | 0 (0%) | 1 (1%) |
| Ethnicity | |||
| Hispanic | 2 (1%) | 0 (0%) | 2 (3%) |
| Non-Hispanic | 168 (99%) | 80 (100%) | 77 (97%) |
| Education level | |||
| High school | 6 (4%) | 3 (4%) | 1 (1%) |
| College (partial or completed) | 111 (65%) | 52 (65%) | 52 (66%) |
| Grad/professional degree | 53 (31%) | 25 (31%) | 26 (33%) |
| Medications | |||
| Antihypertensives | 82 (48%) | 43 (54%) | 37 (47%) |
| Statins | 52 (31%) | 19 (24%) | 30 (38%) |
| Antidepressants | 41 (24%) | 19 (24%) | 17 (22%) |
| Thyroid medications | 35 (21%) | 10 (13%) | 22 (28%) |
| HRT | 14 (8%) | 8 (10%) | 6 (8%) |
| Blood thinners | 6 (4%) | 4 (5%) | 2 (3%) |
| Inhalers | 5 (3%) | 4 (5%) | 0 (0%) |
| Eye disease medications | 1 (1%) | 1 (1%) | 0 (0%) |
| Glucocorticoids | 1 (1%) | 0 (0%) | 1 (1%) |
| Insulin-sensitizing medication | 0 (0%) | 1 (1%) | 0 (0%) |
Variables expressed as means±SD or frequency (%).
Abbreviations used: BMI, body mass index; RM, repetition maximum; HOMA-IR, Homeostatic model assessment of insulin resistance; IFG = impaired fasting glucose; IGT = impaired glucose tolerance; HRT = hormone replacement therapy.
SI conversion: To convert glucose to mmol/L, multiply by 0.0555; insulin to pmol/L, multiply by 6.945; C-peptide to nmol/L, multiply by 0.331.
The overall retention rate was 76% (Fig 1). Adherence to the twice weekly RT sessions during the 3-month Initiation Phase was 91% (i.e., 22 of 24 sessions completed) [34]. Self-reported adherence among those present at assessment sessions, using the time-line follow-back calendars completed at month 9, was 78% and 72% in the SCT and Standard groups, respectively. At month 15, adherence was 53% in both groups. There were no significant group differences in adherence. Including non-completers, and assuming no RT adherence among those individuals, adherence at 15 months was 42% (SCT) and 44% (Standard) [22].
Changes in primary and secondary outcomes over the study period are presented in Tables 2and 3. No changes were noted in fasting glucose concentrations. However, glucose tolerance improved in the Standard group in the first 3 months of the trial, which was maintained at 15 months (11 mg/dl reduction) (p<0.05). No group differences over time were detected in fasting or 2-hour insulin concentrations, insulin and glucose AUC, HOMA-IR, or fasting C-peptide. A group difference over time was noted in 2-hr C-peptide concentrations (p = 0.05), with significant increases occurring in the SCT group from baseline to month 15. Eleven of 129 participants (Standard, 4; SCT, 7) were classified as diabetic according to fasting or 2-hour glucose concentrations at month 15.
Table 2. Changes in diabetes-related outcomes, strength, body weight and composition, blood pressure, physical activity and dietary intake during the 15-month Resist Diabetes trial.A.
| Study Group | Study Period Mean (SD) Score | Within-Group Difference Point Estimate (Bonferroni 95% CI) | p-value Overall Group x Time Interaction | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 3m | 9m | 15m | Baseline to 15 M | Baseline to 3 M | 3M to 15M | ||
| Fasting glucose (mg/dL) (n = 159, Obs = 585) | ||||||||
| SCT | 102 | 102 | 104 | 103 | 0.13 | 0.05 | 0.08 | 0.75 |
| (8) | (10) | (13) | (14) | (-2.77 to 3.03) | (-2.64 to 2.75) | (-2.82 to 2.98) | ||
| Standard | 101 | 100 | 101 | 101 | -0.25 | -1.61 | 1.36 | |
| (9) | (10) | (11) | (10) | (-3.13 to 2.63) | (-4.29 to 1.07) | (-1.52 to 4.24) | ||
| 2hr glucose (mg/dL) (n = 159, Obs = 580) | ||||||||
| SCT | 140 | 133 | 143 | 142 | 1.49 | -6.86 | 8.35 | 0.004 |
| (38) | (35) | (45) | (45) | (-8.61 to 11.59) | (-16.18 to 2.45) | (-1.76 to 18.47) | ||
| Standard | 149 | 136 | 138 | 140 | -11.09* | -12.97** | 1.88 | |
| (33) | (37) | (36) | (37) | (-20.99 to -1.18) | (-22.18 to -3.75) | (-8.02 to 11.79) | ||
| Glucose AUC (n = 109, Obs = 375) | ||||||||
| SCT | 18911 | 19077 | 20033 | 18963 | 136.75 | 53.09 | 83.65 | 0.11 |
| (3132) | (3084) | (4343) | (3487) | (-901.13 to 1174.63) | (-884.46 to 990.64) | (-963.58 to 1130.89) | ||
| Standard | 19070 | 17950 | 18561 | 18488 | -501.63 | -1112.29** | 610.66 | |
| (2865) | (3173) | (2969) | (3168) | (-1487.63 to 484.36) | (-2000.56 to -224.02) | (-337.44 to 1598.76) | ||
| Fasting insulin (uIU/mL) (n = 157, Obs = 532) | ||||||||
| SCT | 14.2 | 16.9 | 19.7 | 17.3 | 4.22** | 3.05 | 1.17 | 0.09 |
| (11.3) | (10.7) | (13.2) | (8.2) | (0.78 to 7.66) | (-0.21 to 6.32) | (-2.05 to 4.39) | ||
| Standard | 16.4 | 16.6 | 17.0 | 17.4 | 1.68 | 0.89 | 0.79 | |
| (14.1) | (12.4) | (9.2) | (9.8) | (-1.62 to 4.97) | (-2.24 to 4.03) | (-2.36 to 3.93) | ||
| 2hr insulin (uIU/mL) (n = 157, Obs = 528) | ||||||||
| SCT | 126.6 | 136.6 | 131.3 | 124.8 | -13.13 | 2.37 | -15.50 | 0.99 |
| (109.5) | (116.0) | (94.1) | (84.9) | (-41.48 to 15.22) | (-24.74 to 29.49) | (-41.69 to 10.69) | ||
| Standard | 158.6 | 140.6 | 127.4 | 133.3 | -14.23 | -12.80 | -1.43 | |
| (138.5) | (122.9) | (89.7) | (107.6) | (-41.25 to 12.78) | (-38.46 to 12.86) | (-27.06 to 24.19) | ||
| Insulin AUC (n = 106, Obs = 327) | ||||||||
| SCT | 9848 | 10530 | 10030 | 10135 | -247.60 | 264.38 | -511.98 | 0.76 |
| (6343) | (6831) | (6641) | (7292) | (-2073.18 to 1577.98) | (-1444.05 to 1972.82) | (-2098.56 to 1074.59) | ||
| Standard | 10809 | 9931 | 10186 | 10125 | -834.14 | -1040.43 | 206.29 | |
| (7380) | (7719) | (6869) | (6701) | (-2434.36 to 766.07) | (-2548.18 to 467.32) | (-1288.87 to 1701.44) | ||
| HOMA-IR (mg/dL) (n = 157, Obs = 532) | ||||||||
| SCT | 3.6 | 4.3 | 5.1 | 4.5 | 1.20** | 0.84† | 0.36 | 0.06 |
| (2.9) | (2.8) | (3.6) | (2.3) | (0.26 to 2.13) | (-0.04 to 1.72) | (-0.52 to 1.23) | ||
| Standard | 4.2 | 4.2 | 4.3 | 4.4 | 0.39 | 0.16 | 0.23 | |
| (3.8) | (3.3) | (2.5) | (2.6) | (-0.50 to 1.28) | (-0.69 to 1.01) | (-0.62 to 1.08) | ||
| Fasting C-peptide (ng/mL) (n = 159, Obs = 584) | ||||||||
| SCT | 4.1 | 3.9 | 3.9 | 3.8 | -0.22 | -0.22 | 0.01 | 0.34 |
| (2.2) | (1.5) | (1.8) | (1.6) | (-0.67 to 0.24) | (-0.64 to 0.19) | (-0.45 to 0.46) | ||
| Standard | 3.9 | 3.9 | 3.8 | 3.9 | 0.01 | 0.01 | 0.00 | |
| (2.0) | (1.9) | (1.5) | (1.5) | (-0.44 to 0.45) | (-0.40 to 0.42) | (-0.45 to 0.44) | ||
| 2hr C-peptide (ng/mL) (n = 159, Obs = 581) | ||||||||
| SCT | 15.0 | 16.6 | 18.1 | 17.8 | 2.60** | 1.69† | 0.90 | 0.05 |
| (7.1) | (7.2) | (6.8) | (7.5) | (0.74 to 4.45) | (-0.03 to 3.42) | (-0.94 to 2.75) | ||
| Standard | 17.5 | 17.2 | 18.1 | 18.4 | 0.81 | -0.36 | 1.17 | |
| (9.6) | (7.7) | (6.4) | (6.7) | (-1.02 to 2.64) | (-2.06 to 1.33) | (-0.65 to 3.00) | ||
| C-peptide AUC (n = 109, Obs = 375) | ||||||||
| SCT | 966 | 1068 | 1195 | 1243 | 260.36** | 100.02 | 160.34* | 0.08 |
| (513) | (504) | (458) | (497) | (113.70 to 407.01) | (-33.65 to 233.69) | (13.33 to 307.34) | ||
| Standard | 1124 | 1156 | 1274 | 1274 | 132.63 | 25.70 | 106.94 | |
| (537) | (428) | (369) | (424) | (-5.90 to 271.16) | (-100.96 to 152.36) | (-32.82 to 246.69) | ||
| Chest press 3RM (kg) (n = 159, Obs = 569) | ||||||||
| SCT | 33.50 | 42.14 | 42.47 | 43.44 | 10.65** | 8.90** | 1.75 | 0.23 |
| (11.75) | (14.63) | (17.00) | (17.74) | (8.41 to 12.90) | (6.90 to 10.90) | (-0.48 to 3.99) | ||
| Standard | 34.02 | 43.49 | 43.43 | 42.43 | 9.23** | 9.39** | -0.15 | |
| (11.66) | (15.10) | (15.29) | (14.72) | (7.06 to 11.41) | (7.39 to 11.38) | (-2.33 to 2.02) | ||
| Leg press 3RM (n = 159, Obs = 560) | ||||||||
| SCT | 139.29 | 165.44 | 163.54 | 164.22 | 26.83** | 26.89** | -0.05 | 0.21 |
| (38.27) | (41.20) | (40.44) | (38.52) | (19.92 to 33.75) | (20.73 to 33.05) | (-6.98 to 6.87) | ||
| Standard | 142.94 | 167.23 | 167.04 | 164.93 | 21.74** | 24.30** | -2.56 | |
| (34.13) | (37.63) | (38.38) | (40.93) | (15.06 to 28.41) | (18.25 to 30.34) | (-9.23 to 4.11) | ||
| Weight (kg) (n = 159, Obs = 585) | ||||||||
| SCT | 92.82 | 92.85 | 92.14 | 91.65 | -0.58 | 0.03 | -0.61 | 0.77 |
| (13.30) | (13.47) | (13.97) | (13.99) | (-1.61 to 0.46) | (-0.92 to 0.99) | (-1.64 to 0.42) | ||
| Standard | 93.89 | 93.74 | 92.77 | 92.74 | -0.82 | -0.15 | -0.68 | |
| (14.21) | (14.62) | (13.47) | (13.51) | (-1.84 to 0.20) | (-1.09 to 0.80) | (-1.70 to 0.34) | ||
| BMI (kg/m2) (n = 159, Obs = 585) | ||||||||
| SCT | 32.98 | 32.99 | 32.75 | 32.62 | -0.22 | 0.01 | -0.23 | 0.90 |
| (3.85) | (3.93) | (4.00) | (3.94) | (-0.58 to 0.15) | (-0.33 to 0.35) | (-0.60 to 0.14) | ||
| Standard | 33.07 | 33.02 | 32.79 | 32.63 | -0.27 | -0.06 | -0.22 | |
| (3.71) | (3.87) | (3.92) | (4.03) | (-0.64 to 0.09) | (-0.39 to 0.28) | (-0.58 to 0.15) | ||
| Body fat percent (%) (n = 159, Obs = 581) | ||||||||
| SCT | 43.73 | 43.07 | 42.98 | 42.75 | -0.47 | -0.66** | 0.19 | 0.73 |
| (6.89) | (6.91) | (6.64) | (6.57) | (-0.99 to 0.06) | (-1.14 to -0.18) | (-0.34 to 0.72) | ||
| Standard | 43.82 | 43.24 | 42.99 | 42.85 | -0.54* | -0.58** | 0.04 | |
| (6.79) | (6.71) | (6.98) | (7.08) | (-1.06 to -0.02) | (-1.06 to -0.10) | (-0.48 to 0.56) | ||
| Fat mass (kg) (n = 159, Obs = 581) | ||||||||
| SCT | 40.35 | 39.62 | 39.21 | 39.07 | -0.75 | -0.73† | -0.02 | 0.85 |
| (7.81) | (8.07) | (8.10) | (8.22) | (-1.57 to 0.07) | (-1.47 to -0.01) | (-0.84 to 0.80) | ||
| Standard | 40.79 | 40.10 | 39.55 | 39.25 | -0.86* | -0.69 | -0.17 | |
| (8.43) | (8.57) | (8.76) | (8.87) | (-1.66 to -0.06) | (-1.43 to 0.05) | (-0.97 to 0.63) | ||
| Fat-free mass percent (n = 159, Obs = 581) | ||||||||
| SCT | 56.27 | 56.93 | 57.02 | 57.21 | 0.43 | 0.66** | -0.23 | 0.66 |
| (6.89) | (6.91) | (6.64) | (6.58) | (-0.10 to 0.95) | (0.18 to 1.13) | (-0.75 to 0.30) | ||
| Standard | 56.17 | 56.76 | 56.98 | 57.13 | 0.53* | 0.59** | -0.06 | |
| (6.80) | (6.71) | (6.98) | (7.09) | (0.01 to 1.04) | (0.11 to 1.06) | (-0.58 to 0.45) | ||
| Fat-free mass (kg) (n = 159, Obs = 581) | ||||||||
| SCT | 52.01 | 52.72 | 52.12 | 51.92 | -0.33 | 0.71** | -1.04** | 0.27 |
| (10.29) | (10.69) | (10.12) | (10.27) | (-0.99 to 0.32) | (0.11 to 1.30) | (-1.69 to -0.38) | ||
| Standard | 52.43 | 52.72 | 52.41 | 52.27 | -0.05 | 0.29 | -0.34 | |
| (10.57) | (10.77) | (9.98) | (9.87) | (-0.69 to 0.59) | (-0.30 to 0.88) | (-0.98 to 0.30) | ||
| Waist Circumference (cm) (n = 159, Obs = 580) | ||||||||
| SCT | 108.83 | 107.56 | 106.47 | 106.49 | -2.86** | -1.27* | -1.59** | 0.17 |
| (10.36) | (10.67) | (10.33) | (10.77) | (-4.22 to -1.49) | (-2.50 to -0.03) | (-2.96 to -0.22) | ||
| Standard | 109.75 | 108.90 | 107.66 | 107.50 | -1.97** | -0.86 | -1.12 | |
| (10.19) | (10.63) | (10.77) | (10.79) | (-3.30 to -0.64) | (-2.08 to 0.37) | (-2.45 to 0.22) | ||
| Systolic Blood Pressure (mmHg) (n = 159, Obs = 580) | ||||||||
| SCT | 131 | 127 | 130 | 131 | 0.49 | -3.82† | 4.31† | 0.32 |
| (17) | (13) | (15) | (15) | (-3.80 to 4.78) | (-7.81 to 0.16) | (-0.002 to 8.62) | ||
| Standard | 132 | 130 | 131 | 132 | -1.08 | -1.59 | 0.51 | |
| (13) | (13) | (15) | (14) | (-5.34 to 3.17) | (-5.54 to 2.35) | (-3.74 to 4.77) | ||
| Diastolic Blood Pressure (mmHg) (n = 159, Obs = 580) | ||||||||
| SCT | 75 | 73 | 73 | 73 | -1.70 | -2.71** | 1.01 | 0.80 |
| (8) | (8) | (8) | (9) | (-3.80 to 0.40) | (-4.65 to -0.76) | (-1.10 to 3.11) | ||
| Standard | 76 | 74 | 75 | 75 | -1.32 | -1.79† | 0.47 | |
| (9) | (9) | (10) | (9) | (-3.39 to 0.76) | (-3.71 to -0.13) | (-1.61 to 2.55) | ||
| MET/hr/wk (other than RT) (n = 157, Obs = 507) | ||||||||
| SCT | 11.78 | 13.07 | 15.11 | 15.97 | 4.80** | 1.02 | 3.78† | 0.59 |
| (10.87) | (8.50) | (13.35) | (10.99) | (0.64 to 8.97) | (-2.60 to 4.64) | (-0.36 to 7.93) | ||
| Standard | 11.70 | 13.15 | 15.86 | 14.28 | 3.40 | 1.78 | 1.62 | |
| (9.20) | (11.03) | (14.28) | (17.07) | (-0.61 to 7.41) | (-1.72 to 5.28) | (-2.36 to 5.60) | ||
| Total MET/hr/wk (including RT) (n = 159, Obs = 526) | ||||||||
| SCT | 11.96 | 21.34 | 23.73 | 20.89 | 10.13*** | 9.54*** | 0.59 | 0.66 |
| (10.89) | (9.38) | (14.89) | (11.71) | (5.62 to 14.63) | (5.64 to 13.44) | (-3.81 to 4.99) | ||
| Standard | 11.89 | 21.25 | 23.52 | 19.43 | 8.99*** | 10.04*** | -1.05 | |
| (9.17) | (12.32) | (16.00) | (18.61) | (4.70 to 13.28) | (6.24 to 13.84) | (-5.27 to 3.16) | ||
| Energy (kcals) (n = 159, Obs = 583) | ||||||||
| SCT | 1762.31 | 1735.56 | 1690.11 | 1739.74 | -16.23 | -21.71 | 5.47 | 0.10 |
| (494.43) | (474.28) | (456.68) | (527.35) | (-155.60 to 123.13) | (-150.56 to 107.15) | (-133.33 to 144.27) | ||
| Standard | 1850.42 | 1751.23 | 1762.99 | 1720.87 | -160.31** | -99.19 | -61.12 | |
| (517.33) | (451.89) | (452.07) | (471.45) | (-297.31 to -23.31) | (-226.72 to 28.34) | (-198.12 to 75.88) | ||
| Carbohydrate (%) (n = 159, Obs = 583) | ||||||||
| SCT | 44.19 | 43.06 | 42.23 | 43.25 | -1.00 | -1.10 | 0.10 | 0.37 |
| (7.44) | (8.13) | (9.15) | (9.65) | (-3.83 to 1.83) | (-3.72 to 1.52) | (-2.72 to 2.92) | ||
| Standard | 42.76 | 42.61 | 41.74 | 42.85 | 0.37 | -0.15 | 0.52 | |
| (8.38) | (8.75) | (9.62) | (10.68) | (-2.42 to 3.15) | (-2.75 to 2.44) | (-2.26 to 3.30) | ||
| Fat (%) (n = 159, Obs = 583) | ||||||||
| SCT | 36.00 | 36.05 | 36.88 | 36.44 | 0.74 | 0.08 | 0.66 | 0.08 |
| (6.99) | (6.60) | (7.19) | (7.50) | (-1.72 to 3.21) | (-2.21 to 2.38) | (-1.80 to 3.12) | ||
| Standard | 37.39 | 37.13 | 38.02 | 35.63 | -1.75 | -0.27 | -1.48 | |
| (6.92) | (6.38) | (7.02) | (7.17) | (-4.17 to 0.68) | (-2.54 to 2.00) | (-3.90 to 0.95) | ||
| Protein (%) (n = 159, Obs = 583) | ||||||||
| SCT | 18.17 | 18.95 | 18.55 | 17.96 | -0.36 | 0.71 | -1.07 | 0.05 |
| (4.45) | (4.30) | (4.86) | (4.44) | (-1.99 to 1.27) | (-0.80 to 2.23) | (-2.69 to 0.55) | ||
| Standard | 17.88 | 18.21 | 18.37 | 19.28 | 1.35 | 0.33 | 1.02 | |
| (4.14) | (4.28) | (4.43) | (5.98) | (-0.26 to 2.95) | (-1.17 to 1.83) | (-0.58 to 2.62) | ||
| Fiber (g) (n = 159, Obs = 583) | ||||||||
| SCT | 18.60 | 17.87 | 18.52 | 17.69 | -1.22 | -0.72 | -0.49 | 0.73 |
| (7.59) | (6.97) | (6.93) | (6.68) | (-3.19 to 0.75) | (-2.55 to 1.10) | (-2.46 to 1.47) | ||
| Standard | 18.66 | 17.65 | 18.03 | 18.33 | -0.73 | -1.01 | 0.28 | |
| (6.75) | (5.93) | (6.68) | (6.29) | (-2.67 to 1.21) | (-2.81 to 0.79) | (-1.66 to 2.21) | ||
| Added sugar (g) (n = 159, Obs = 583) | ||||||||
| SCT | 53.67 | 50.52 | 44.41 | 49.98 | -2.12 | -2.88 | 0.76 | 0.73 |
| (30.74) | (31.09) | (21.15) | (27.67) | (-11.15 to 6.92) | (-11.24 to 5.48) | (-8.24 to 9.76) | ||
| Standard | 51.63 | 46.90 | 48.93 | 49.34 | -2.55 | -4.73 | 2.18 | |
| (30.27) | (30.84) | (27.05) | (33.64) | (-11.44 to 6.33) | (-13.01 to 3.54) | (-6.70 to 11.06) | ||
Abbreviations used: AUC, area under the curve; BMI, body mass index; MET, metabolic equivalents; M, month; RM, repetition maximum; SCT, Social Cognitive Theory.
A Data are presented for 159 participants, except for the AUC data which included a subset of 109 participants.
† p < 0.10
* p < 0.05
** p < 0.01
*** p < 0.001.
Table 3. Odds of achieving normoglycemia among Resist Diabetes trial participants.a.
| Parameter | Coefficient (SE) | OR | 95% CI | Interpretation |
|---|---|---|---|---|
| Phase | ||||
| SCT Group | ||||
| Initiation | Ref | 1.00 | ||
| Maintenance (M 9) | 0.11 (0.31) | 1.12 | (0.61, 2.04) | |
| No-Contact (M 15) | -0.11 (0.33) | 0.90 | (0.47, 1.70) | |
| STD Group | ||||
| Initiation | -0.03 (0.35) | 0.97 | (0.49, 1.94) | |
| Maintenance (M 9) | -0.31 (0.37) | 0.74 | (0.35, 1.53) | |
| No Contact (M 15) | -0.26 (0.38) | 0.77 | (0.36, 1.63) | |
| Δ in Lean Mass Percentb | 0.18 (0.08) * | 1.19 | (1.02, 1.39) | The odds of reverting to normoglycemia are higher for participants with an increase in lean body mass percentage. |
| Gender | ||||
| Male | Ref | 1.00 | ||
| Female | -0.37 (0.30) | 0.69 | (0.38, 1.24) | |
| Prediabetes Phenotype | ||||
| IFG and IGT | Ref | 1.00 | ||
| IFG | 1.27 (0.32) ** | 3.58 | (1.93, 6.63) | Participants with isolated IFG and isolated IGT have higher odds of reverting to normoglycemia compared to those with both IFG & IGT. |
| IGT | 1.59 (0.43) ** | 4.92 | (2.13, 11.34) | |
| Intercept | -1.34 (0.39) ** | 0.26 | (0.12, 0.56) |
NInitiation = 159; NMaintenance = 138; NNo Contact = 129; Number of observations used in analyses = 422.
Abbreviations: CI, confidence interval; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; M, month; OR, odds ratio; SCT, Social Cognitive Theory; STD, standard.
a Population-averaged Generalized Estimation Model.
b Within-Person change from Baseline to 15 Months.
* p<0.05
** p<0.01.
After three months of RT, approximately 34% of the study sample achieved normoglycemia. This prevalence of normoglycemia was maintained through the Maintenance (32%) and No-Contact phases (30%). Although, the SCT group had slightly higher odds of achieving normoglycemia, there were no significant differences between groups (Table 3). Participants with isolated IFG or IGT had greater likelihood of achieving normoglycemia than those with combined IFG and IGT.
Both groups demonstrated significant improvements in muscular strength (p<0.001), but there were no group differences in strength change (Table 2). Strength increases were evident month 3, and maintained through month 15. These absolute increases represent improvements of 21% and 14% for chest and leg press, respectively. There were no significant group differences in body weight change over time. Body fat (%) decreased, and fat-free mass (%) increased, in both groups from baseline to month 3, which was maintained in the Standard group though month 15. Waist circumference decreased in both groups baseline to month 15. However, there were no group differences in these outcomes. Among trial participants, there was an 18% increase in the odds of reverting to normoglycemic for each 1% increase in fat-free mass (Table 3).
No group differences were noted in blood pressure, self-reported physical activity level or dietary intake, other than in percentage of energy from protein (p = 0.05). However, increases in reported physical activity (including RT) were noted in both groups from baseline to month 3, and from baseline to month 15.
Four serious adverse events were reported during the 15-month trial, which did not differ by group (Table 4). Three of these involved musculoskeletal and/or joint pain persisting for more than 3–4 days.
Table 4. Adverse Events.
| SCT group (n = 79) | Standard group (n = 80) | No group (n = 11) | |
|---|---|---|---|
| Serious adverse events* | 2(1) | 2(1) | 0(0) |
| Heart attack-related symptoms–Chest pain, difficulty breathing, fatigue | 0 | 1 | 0 |
| Musculoskeletal pain & difficulty breathing | 0 | 1 | 0 |
| Prolonged musculoskeletal pain | 1 | 0 | 0 |
| Prolonged joint pain | 1 | 0 | 0 |
| Injury or musculoskeletal discomfort | 26(15) | 26(15) | 2(1) |
| Side effects and complaints | |||
| Shoulder pain | 3(2) | 3(2) | 0(0) |
| Aggravation of preexisting arthritis | 2(1) | 2(1) | 0(0) |
| Tendonitis | 1(1) | 0(0) | 0(0) |
| Back pain | 6(4) | 4(2) | 1(1) |
| Ligament or tendon tear/pain | 0(0) | 3(2) | 0(0) |
| Pinched nerve (sciatic, femoral, or cervical) | 2(1) | 1(1) | 0(0) |
| Musculoskeletal injury due to accident while exercising | 0(0) | 2(1) | 0(0) |
| Musculoskeletal injury due to accident outside of RT program | 0(0) | 2(1) | 1(1) |
| Inflammation/swelling | 2(1) | 2(1) | 0(0) |
| Other musculoskeletal discomfort | 10(6) | 7(4) | 0(0) |
| Other medical events | 3(2) | 3(2) | 0(0) |
| Surgery (heart stent, foot, hand, melanoma) | 2(1) | 2(1) | 0(0) |
| Heart attack-related symptoms | 0(0) | 1(0.6)† | 0(0) |
| Other | 1(0.6) | 0(0) | 0(0) |
Notes: Data are number (percentage) of participants. The “No group” category indicates participants who withdrew from study during the Initiation phase, before randomization occurred. RT = resistance training.
The difference in adverse events between Standard vs. SCT was not significant
[χ2 (df = 2, N = 159) = 0.44 (p = 0.80)].
* Serious unanticipated or anticipated problems, including study-related prolonged (>3–4 days) muscle pain.
† Reported after check-up with primary care physician; all tests were normal.
Discussion
The findings of this randomized, controlled trial suggest that after adopting RT, twice per week using a 12-set, whole body protocol, the SCT-based approach was not more effective for maintenance in community-based settings. Overall, a significant reduction in prediabetes prevalence was demonstrated among previously sedentary overweight and obese older adults with prediabetes. Significant improvements in muscular strength were demonstrated, and maintained throughout the 15-month trial period. Importantly, about one-third of participants were normoglycemic at month 15. Improvements in other health outcomes, such as body composition and physical activity level, were also noted.
Contrary to our hypothesis, the SCT-based approach did not demonstrate greater effectiveness than the lower-dose standard care maintenance intervention. Although a formal cost effectiveness analysis was not performed, program delivery costs were estimated to be $1200 per participant for the initial 3-month supervised RT initiation period, $595 per participant for the SCT transition and maintenance condition, and $160 per participant for the Standard transition and maintenance condition [22]. The lower cost suggests this approach could be extended in future applications with long-term maintenance of unsupervised training noted as a critical research and translation area for prevention and treatment of chronic diseases and disorders [35].
Intensive combined diet and physical activity promotion programs are recommended to reduce type 2 diabetes [4]. Our findings suggest that RT alone may represent an effective single-component strategy to reduce prediabetes prevalence and thus, type 2 diabetes risk. The Diabetes Prevention Program (DPP) lifestyle intervention resulted in a prevalence of normoglycemia of about 40% in years 1 and 2 [36]. In contrast to our findings, the DPP lifestyle and metformin interventions reduced fasting glucose concentrations [36], which may suggest that a variety of diabetes prevention strategies are needed depending upon prediabetes phenotype [21], program accessibility, resources, and individual preferences.
Strength declines markedly with advancing age; the clinical implications of poor muscular strength include impaired mobility and limitations in activities of daily living, such as rising from a chair [37], and increased risk of type 2 diabetes [35]. Only 24% of US adults over age 45 report engaging in muscle strengthening activity two or more times per week [38], and less than 5% of adults over age 45 report meeting muscle strengthening recommendations of twice per week which includes all seven major muscle groups [39]. Yet, older adults who meet twice/week RT guidelines have a 46% lower odds of all-cause mortality than those who do not [12], and improved physical functioning [13].
Strengths of this trial include the high retention rate, a low rate of serious adverse events across about 12,500 training sessions, a theoretically-based approach, and the efficacy/effectiveness design, which may facilitate translation into clinic- and community-based interventions. Limitations of this investigation include a predominantly white, female, well-educated sample. The trial also did not include a control group, who received no intervention over the 15-month trial period. Findings cannot be generalized to younger, less-educated populations or to minorities, who may be at greater risk for developing type 2 diabetes. It is also unknown if the reduced prevalence of prediabetes was maintained beyond the 15-month trial period, however, findings from the Diabetes Outcomes Prevention Program indicate that even transient improvements in blood glucose homeostasis are associated with reduced risk of future diabetes [40].
Conclusions
It has been estimated that 70% of individuals with prediabetes will progress to type 2 diabetes [1]. Prediabetes affects more than half of adults over 65 years of age [2], thus effective strategies to reduce type 2 diabetes risk among older adults with prediabetes are needed. The results of several 10-year cost effectiveness analyses from the DPP concluded that lifestyle interventions to reduce diabetes risk among high-risk adults are cost effective [41, 42]. Potential challenges in implementing multi-component interventions, such as the DPP, include program costs, resource limitations, and accessibility. Lower costs are possible with group-based programs and with clinic- and community-based programs [43]. Our findings suggest that the adoption and maintenance of RT, using a higher-contact SCT-based maintenance approach, is not more effective in reducing prediabetes prevalence than a lower-contact approach, with overall results comparable to that noted in the lifestyle intervention group of the DPP [36], as well as for improving muscular strength and body composition among older, overweight, prediabetic adults.
Supporting information
(DOC)
(DOCX)
(DOC)
(PDF)
Acknowledgments
We extend our gratitude to the Resist Diabetes participants for their time and commitment to our research study. We thank all of the RD staff members for their efforts during data collection and study interventions (research nurse: John Pownall, RN, MPH; personal trainers: Daniel Gochenour, MS, Nabil Boutagy, PhD; dietitians and research assistants: Adrienne Ginter Clark, MS, RD, Rachel Cornett Hart, MS, RD, Valisa Hedrick, PhD, RD, Leanne Shelley, BS, Joshua Eikenberg, MPH, MD; software developer: Chad Blake). Thank you to our data and safety monitoring board consisting of Janet Rankin, PhD, and Robert Stephens, PhD, of Virginia Tech and Soheir Boshra, MD, of Carilion Clinic for yearly study review and approval of enrollment, retention, and adverse events data. We appreciate the valuable comments provided by Eugene Barrett MD, PhD, for the development and implementation of this investigation.
Data Availability
Data are contained within the paper
Funding Statement
The authors received funding from the National Institutes of Health (BMD, RAW: R01DK082383).
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services, 2014.
- 2.Nathan DM, Davidson MB, DeFronzo RA, Heine RJ, Henry RR, Pratley R, et al. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007;30(3):753–9. 10.2337/dc07-9920 [DOI] [PubMed] [Google Scholar]
- 3.Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimaki M. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379(9833):2279–90. 10.1016/S0140-6736(12)60283-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the Community Preventive Services Task Force. Ann Intern Med. 2015;163(6):437–51. 10.7326/M15-0452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37 Suppl 1:S14–80. [DOI] [PubMed] [Google Scholar]
- 6.Ackermann RT. Diabetes prevention at the tipping point: aligning clinical and public health recommendations. Ann Intern Med. 2015;163(6):475–6. 10.7326/M15-1563 [DOI] [PubMed] [Google Scholar]
- 7.Umpierre D, Ribeiro PA, Kramer CK, Leitao CB, Zucatti AT, Azevedo MJ, et al. Physical activity advice only or structured exercise training and association with HbA1c levels in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2011;305(17):1790–9. 10.1001/jama.2011.576 [DOI] [PubMed] [Google Scholar]
- 8.Dunstan DW, Vulikh E, Owen N, Jolley D, Shaw J, Zimmet P. Community center-based resistance training for the maintenance of glycemic control in adults with type 2 diabetes. Diabetes Care. 2006;29(12):2586–91. 10.2337/dc06-1310 [DOI] [PubMed] [Google Scholar]
- 9.Shimokata H, Muller DC, Fleg JL, Sorkin J, Ziemba AW, Andres R. Age as independent determinant of glucose tolerance. Diabetes. 1991;40(1):44–51. [DOI] [PubMed] [Google Scholar]
- 10.Short KR, Nair KS. Muscle protein metabolism and the sarcopenia of aging. Int J Sport Nutr Exerc Metab. 2001;11 Suppl:S119–27. [DOI] [PubMed] [Google Scholar]
- 11.Minges KE, Magliano DJ, Owen N, Daly RM, Salmon J, Shaw JE, et al. Associations of strength training with impaired glucose metabolism: the AusDiab Study. Med Sci Sports Exerc. 2013;45(2):299–303. 10.1249/MSS.0b013e31826e6cd1 [DOI] [PubMed] [Google Scholar]
- 12.Kraschnewski JL, Sciamanna CN, Poger JM, Rovniak LS, Lehman EB, Cooper AB, et al. Is strength training associated with mortality benefits? A 15year cohort study of US older adults. Prev Med. 2016;87:121–7. 10.1016/j.ypmed.2016.02.038 [DOI] [PubMed] [Google Scholar]
- 13.Liu CJ, Latham NK. Progressive resistance strength training for improving physical function in older adults. Cochrane Database Syst Rev. 2009(3):CD002759 10.1002/14651858.CD002759.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ackermann RT, Finch EA, Brizendine E, Zhou H, Marrero DG. Translating the Diabetes Prevention Program into the community. The DEPLOY Pilot Study. Am J Prev Med. 2008;35(4):357–63. 10.1016/j.amepre.2008.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Estabrooks PA, Smith-Ray RL. Piloting a behavioral intervention delivered through interactive voice response telephone messages to promote weight loss in a pre-diabetic population. Patient Educ Couns. 2008;72(1):34–41. 10.1016/j.pec.2008.01.007 [DOI] [PubMed] [Google Scholar]
- 16.Amundson HA, Butcher MK, Gohdes D, Hall TO, Harwell TS, Helgerson SD, et al. Translating the diabetes prevention program into practice in the general community: findings from the Montana Cardiovascular Disease and Diabetes Prevention Program. Diabetes Educ. 2009;35(2):209–10, 13–4, 16–20 passim. 10.1177/0145721709333269 [DOI] [PubMed] [Google Scholar]
- 17.Johannsen NM, Swift DL, Lavie CJ, Earnest CP, Blair SN, Church TS. Combined aerobic and resistance training effects on glucose homeostasis, fitness, and other major health indices: a review of current guidelines. Sports Med. 2016. [DOI] [PubMed] [Google Scholar]
- 18.Payne WR, Walsh KJ, Harvey JT, Livy MF, McKenzie KJ, Donaldson A, et al. Effect of a low-resource-intensive lifestyle modification program incorporating gymnasium-based and home-based resistance training on type 2 diabetes risk in Australian adults. Diabetes Care. 2008;31(12):2244–50. 10.2337/dc08-0152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Teychenne M, Ball K, Salmon J, Daly RM, Crawford DA, Sethi P, et al. Adoption and maintenance of gym-based strength training in the community setting in adults with excess weight or type 2 diabetes: a randomized controlled trial. Int J Behav Nutr Phys Act. 2015;12(1):105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halliday TM, Davy BM, Clark AG, Baugh ME, Hedrick VE, Marinik EL, et al. Dietary intake modification in response to a participation in a resistance training program for sedentary older adults with prediabetes: findings from the Resist Diabetes study. Eat Behav. 2014;15(3):379–82. 10.1016/j.eatbeh.2014.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eikenberg JD, Savla J, Marinik EL, Davy KP, Pownall J, Baugh ME, et al. Prediabetes phenotype influences improvements in glucose homeostasis with resistance training. PLoS One. 2016;11(2):e0148009 10.1371/journal.pone.0148009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Winett RA, Davy BM, Savla J, Marinik EL, Kelleher SA, Winett SG, et al. Theory-based approach for maintaining resistance training in older adults with prediabetes: adherence, barriers, self-regulation strategies, treatment fidelity, costs. Transl Behav Med. 2015;5(2):149–59. 10.1007/s13142-015-0304-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22(4):623–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription, 7th edition Philadelphia: Lippincott, Williams & Williams; 2005. [Google Scholar]
- 25.Marinik EL, Kelleher S, Savla J, Winett RA, Davy BM. The resist diabetes trial: rationale, design, and methods of a hybrid efficacy/effectiveness intervention trial for resistance training maintenance to improve glucose homeostasis in older prediabetic adults. Contemp Clin Trials. 2014;37(1):19–32. 10.1016/j.cct.2013.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kohl HW, Blair SN, Paffenbarger RS Jr., Macera CA, Kronenfeld JJ. A mail survey of physical activity habits as related to measured physical fitness. Am J Epidemiol. 1988;127(6):1228–39. [DOI] [PubMed] [Google Scholar]
- 27.Williams DM, Savla J, Davy BM, Kelleher SA, Marinik EL, Winett RA. Questionnaires for outcome expectancy, self-regulation, and behavioral expectation for resistance training among young-old adults: development and preliminary validity. J Aging Phys Act. 2015;23(2):279–85. 10.1123/japa.2013-0184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves JW, Hill MN, et al. Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens. 2005;7(2):102–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9. [DOI] [PubMed] [Google Scholar]
- 30.Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28(7):916–31. [DOI] [PubMed] [Google Scholar]
- 31.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91. [DOI] [PubMed] [Google Scholar]
- 32.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–52. 10.1161/CIRCULATIONAHA.105.169404 [DOI] [PubMed] [Google Scholar]
- 33.Standards of Medical Care in Diabetes-2016: Summary of Revisions. Diabetes Care. 2016;39 Suppl 1:S4–5. [DOI] [PubMed] [Google Scholar]
- 34.Winett RA, Davy BM, Savla J, Marinik EL, Winett SG, Baugh ME, et al. Using response variation to develop more effective, personalized behavioral medicine?: evidence from the Resist Diabetes study. Transl Behav Med. 2014;4(3):333–8. 10.1007/s13142-014-0263-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peterson MD, Zhang P, Choksi P, Markides KS, Al Snih S. Muscle weakness thresholds for prediction of diabetes in adults. Sports Med. 2016;46(5):619–28. 10.1007/s40279-015-0463-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. 10.1056/NEJMoa012512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Looker AC, Wang CY. Prevalence of reduced muscle strength in older U.S. adults: United States, 2011–2012. NCHS data brief, no 179 Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 38.Vezina JW, Der Ananian CA, Greenberg E, Kurka J. Sociodemographic correlates of meeting US Department of Health and Human Services muscle strengthening recommendations in middle-aged and older adults. Prev Chronic Dis. 2014;11:E162 10.5888/pcd11.140007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Loustalot F, Carlson SA, Kruger J, Buchner DM, Fulton JE. Muscle-strengthening activities and participation among adults in the United States. Res Q Exerc Sport. 2013;84(1):30–8. 10.1080/02701367.2013.762289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Perreault L, Pan Q, Mather KJ, Watson KE, Hamman RF, Kahn SE, et al. Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the Diabetes Prevention Program Outcomes Study. Lancet. 2012;379(9833):2243–51. 10.1016/S0140-6736(12)60525-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Diabetes Prevention Program Research Group. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes Care. 2012;35(4):723–30. 10.2337/dc11-1468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Herman WH, Edelstein SL, Ratner RE, Montez MG, Ackermann RT, Orchard TJ, et al. Effectiveness and cost-effectiveness of diabetes prevention among adherent participants. Am J Manag Care. 2013;19(3):194–202. [PMC free article] [PubMed] [Google Scholar]
- 43.Li R, Qu S, Zhang P, Chattopadhyay S, Gregg EW, Albright A, et al. Economic evaluation of combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the Community Preventive Services Task Force. Ann Intern Med. 2015;163(6):452–60. 10.7326/M15-0469 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(DOC)
(PDF)
Data Availability Statement
Data are contained within the paper