Abstract
Background
Young women (<65 years) experience a 2–3-fold greater mortality risk than younger men after acute myocardial infarction (AMI). However, it is unknown whether they are at higher risk for 30-day readmission, and if this association varies by age. We examined sex differences in the rate, timing and principal diagnoses of 30-day readmissions, including the independent effect of sex following adjustment for confounders.
Methods and Results
We included patients aged 18–64 years with a principal diagnosis of AMI. Data was utilized from the Healthcare Cost and Utilization Project-State Inpatient Database for California (07–09). Readmission diagnoses were categorized using an aggregated version of the Centers for Medicare and Medicaid Services’ Condition Categories, and readmission timing was determined from the day after discharge. Of 42,518 younger patients with AMI (26.4% female), 4,775 (11.2%) had at least one readmission. The 30-day all-cause readmission rate was higher for women (15.5% vs. 9.7%, P<0.0001). For both sexes, readmission risk was highest on days 2–4 after discharge and declined thereafter, and women were more likely to present with non-cardiac diagnoses (44.4% vs. 40.6%, P=0.01). Female sex was associated with a higher rate of 30-day readmission, which persisted after adjustment (HR=1.22, 95% CI 1.15, 1.30). There was no significant interaction between age and sex on readmission.
Conclusions
Compared with men, younger women have a higher risk for readmission, even after adjustment for confounders. The timing of 30-day readmission was similar in women and men, and both sexes were susceptible to a wide range of causes for readmission.
Keywords: Acute myocardial infarction, readmission, gender differences, women, Post-hospital syndrome
INTRODUCTION
Younger women with ischemic heart disease represent a distinct phenotype. They have pathophysiologic and clinical features that contrast with men and older patients.1, 2 Moreover, women hospitalized with acute myocardial infarction (AMI) are at higher risk for a broad range of in-hospital adverse outcomes.2–7 Younger women experience a two- to three-fold greater risk of in-hospital mortality following AMI than similarly aged men, and this association persists following adjustment for a range of factors.3, 4
Readmission, which commonly does not track with mortality and has different predictors,8 is also an important outcome as it imposes significant physical and psychological burden on patients;9,10, 11 however it is unknown whether younger women are at higher risk for readmission after AMI. Furthermore, it is not known if the transient period of generalized risk for readmission following hospitalization for many conditions - a phenomenon called ‘post hospital syndrome’-12, 13 differs by sex in young patients with AMI. That is, whether the post-hospital period is characterized by a period of vulnerability to a wide range of acute events requiring hospitalization and whether it varies by sex. Identifying sex differences in the incidence, timing and patterns of readmission has yet to be studied and could inform initiatives to reduce readmissions among younger women after AMI and improve outcomes.
Accordingly, we utilized data from the state of California to (a) evaluate sex differences in the rate, timing and principal diagnosis of 30-day readmissions following AMI, (b) examine the association of sex with 30-day readmissions, and assessing whether or not there is an age-sex interaction. We hypothesized that younger women (<65 years) have a higher risk of readmission than younger men, even following extensive adjustment for covariates, as well as similar timing of readmission, and a broad range of readmission diagnoses.
METHODS
Study Sample
The study population was derived from the Healthcare Cost and Utilization Project (HCUP) - State Inpatient Dataset of California from January 2007 to November 2009. Inclusion criteria consisted of patients 18–65 years old with a principal discharge diagnosis of AMI, as defined by the International Classification of Diseases, Ninth Revision Clinical Modification (ICD-9-CM) codes of 410.xx, except the fifth digit of 2 which indicates an old AMI, used for the Center for Medicare & Medicaid Services (CMS) publicly reported readmission measures.14–16 We excluded hospitalizations where a patient (a) left against medical advice (b) was transferred to another facility or (c) died in-hospital. We also excluded hospitalizations for non-California residents, as subsequent readmissions may not have been captured in the state inpatient dataset.
We considered only the first readmission within 30 days for our analysis, similar to the federal measures and previous research.13, 15 Additional re-hospitalizations within this 30-day period were not counted as index hospitalizations. Subsequent hospitalizations occurring after 30-days from discharge were counted as index admissions if they met inclusion criteria. For each index admission, baseline comorbidities were derived using the diagnosis codes in the index admission, as well as admissions in the preceding one-year. The Yale University Human Investigation Committee approved this study, including waiver of the requirement for participant informed consent.
Readmission Rate and Timing
The first unplanned readmission due to any cause, within 30-days of the index admission, was identified as readmission for each index admission as used by the CMS criteria for reporting hospital readmission performance. Planned hospitalizations, as identified by the CMS planned readmission algorithm, were excluded.14–17 To assess the timing of readmissions, the percentage of readmissions occurring on each day over the 30-days following discharge were calculated among all the readmissions.
Risk Factors at Presentation and Principal Diagnoses among Readmissions
The risk factors at presentation (i.e. cardiovascular risk factors and co-morbidities) included in this study were derived from the diagnosis codes in the previous hospitalization within one-year prior to the current hospitalization or the secondary diagnosis codes in the current hospitalization, and were grouped into condition categories using the condition category system.18 Potential complications in the current hospitalization were excluded14–17. The principal diagnoses of readmissions were also matched to the corresponding CMS condition categories,18 which assemble presenting diagnoses into clinically coherent conditions.
Due to prior data indicating that 85% of the 189 condition categories groups each accounted for less than 1% of all readmissions after AMI,13 the condition categories were further consolidated into 30 diagnostic categories, as done previously,13 to make data presentation and interpretation more meaningful. These categories were designed to be clinically relevant, internally consistent, and delineate the most common readmission diagnoses after discharge from AMI hospitalizations (see Supplemental Tables 1–2).13
For readmission diagnoses, the percentage of readmissions occurring due to each of the 30 modified condition categories during the 30-days post discharge were calculated. We also determined the proportion of readmission diagnoses occurring due to cardiovascular versus non-cardiovascular conditions.13
Statistical Analysis
Baseline characteristics were examined for the total sample and compared between men and women using Chi-squared tests for categorical variables and t-tests for continuous variables. We measured timing of the first readmission within 30-days post discharge by days elapsed since discharge, and characterized readmissions by principal diagnoses among all readmissions within 30-days post discharge. Patients were censored at 30-days if they did not have a readmission within 30-days of discharge. Cox proportional hazards models, using sequential adjustment for potential confounders, were used to determine the relationship between sex and 30-day readmission, which were represented by risk-adjusted hazard ratios (HR’s) and 95% confidence intervals (CI). Proportional-hazards assumption was tested using (a) the graph of the log (-log [survival]) versus the log of survival time (to observe if the curves of men and women were parallel), and (b) Schoenfeld residuals on the functions of time (to observe if there was a zero slope), whereby no parallel curve or a non-zero slope indicates a violation of the proportion-hazards assumption. For all models, we sequentially adjusted for potential confounders and, at each step, assessed the association of sex with outcomes. The unadjusted model included sex only. The first model included socio-demographics (age, race, and insurance status) in addition to sex (Model 1). The second model included socio-demographics and cardiovascular risk factors/conditions/procedures (acute coronary syndrome, heart failure, diabetes, cerebrovascular disease/stroke, AMI, other location of AMI, angina pectoris, atherosclerosis, valvular/rheumatic heart disease, arrhythmias, percutaneous coronary angioplasty, coronary artery bypass surgery) (Model 2). The third model included socio-demographics, cardiovascular risk factors/conditions/procedures, and other co-morbidities (chronic obstructive pulmonary disease (COPD), pneumonia, asthma, renal failure, end-stage renal disease or dialysis, vascular or circulatory disease, other urinary tract disorders, disorders of fluid/electrolyte/acid-base, history of infection, metastatic cancer and acute leukemia, cancer, iron deficiency and/or anemia, decubitus ulcer or chronic skin ulcer, protein-calorie malnutrition, hemiplegia, paralysis, functional disability, dementia and senility, major psychiatric disorders (includes schizophrenia, major depressive, bipolar and paranoid disorders and reactive and unspecified psychosis), drug and alcohol abuse) (Model 3). The fourth model included socio-demographics, cardiovascular risk factors/conditions/procedures, other co-morbidities, and length of stay (Model 4). The fifth model included socio-demographics, cardiovascular risk factors/conditions/procedures, other co-morbidities, length of stay, and discharge disposition (Model 5). In the final model we tested an interaction between age and sex on 30-day readmission, with age modeled as a continuous variable. For all statistical analyses, the significance level was 2-sided with a P-value <0.05. All analyses were conducted using SAS 9.2 (SAS Institute Inc., Cary, NC) and STATA/SE 12.0 (Stata Corp, College Station, TX).
RESULTS
Risk Factors at Presentation
The 42,518 index admissions included in the study cohort, were from 40,851 patients; of whom 39,422 (96.5%) had only one admission and 1,429 (3.5%) had more than one admission. Of the index admissions 11,215 (26.4%) were among women (Table 1). Women, as compared with men, were older (55±8 vs. 54±8 years) and more likely to be African American or Hispanic and to have Medicare or Medicaid as their primary health insurance. Women also had a substantively higher frequency of unfavorable cardiovascular risk factors and co-morbidities as compared with men, such as heart failure, diabetes, stroke, pneumonia, asthma, cancer, COPD, renal failure, vascular/circulatory disease, arrhythmia, acute coronary syndrome, hemiplegia/paralysis/functional disability, infection, dementia, valvular/rheumatic heart disease, iron deficiency, angina pectoris and major psychiatric disorders (p <0.0001 for all). Women also had a longer length of stay in hospital than men, and were more likely to be transferred to a skilled nursing/immediate care facility and/or receive home health care.
Table 1.
Risk Factors at Presentation Stratified by Sex in Younger Patients with AMI.*
| Total Sample (N=42518) |
Men (N=31303, 74%) |
Women (N=11215, 26%) |
P-value | |
|---|---|---|---|---|
| Socio-demographics (%) | ||||
| Age: Mean±SD | 53.9±7.6 | 53.6±7.6 | 54.6±7.5 | <.001 |
| Race (%) | ||||
| White | 23848 (56.1) | 17902 (57.2) | 5946 (53.0) | |
| Black | 3475 (8.2) | 2025 (6.5) | 1450 (12.9) | <.001 |
| Hispanic | 8536 (20.1) | 6206 (19.8) | 2330 (20.8) | |
| Other | 6659 (15.7) | 5170 (16.5) | 1489 (13.3) | |
| Insurance Status (%) | ||||
| Medicare | 5247 (12.3) | 3413 (10.9) | 1834 (16.4) | |
| Medicaid | 6009 (14.1) | 3678 (11.8) | 2331 (20.8) | <.001 |
| Private insurance | 23550 (55.4) | 18173 (58.1) | 5377 (47.9) | |
| Other | 7712 (18.1) | 6039 (19.3) | 1673 (14.9) | |
|
| ||||
| CV Risk Factors (%) | ||||
| Acute coronary syndrome | 3196 (7.5) | 2036 (6.5) | 1160 (10.3) | <.001 |
| Congestive Heart failure | 3214 (7.6) | 1855 (5.9) | 1359 (12.1) | <.001 |
| Diabetes and Complications | 15092 (35.5) | 10117 (32.3) | 4975 (44.4) | <.001 |
| Cerebrovascular Disease | 847 (1.9) | 479 (1.5) | 368 (3.3) | <.001 |
| Stroke | 338 (0.8) | 193 (0.6) | 145 (1.3) | <.001 |
| Anterior Myocardial Infarction | 7024 16.5) | 5652 (18.1) | 1372 (12.2) | <.001 |
| Other Location of AMI | 10126 23.8) | 8081 (25.8) | 2045 (18.2) | <.001 |
| Angina pectoris/old AMI | 6488 (15.3) | 4635 (14.8) | 1853 (16.5) | <.001 |
| Coronary atherosclerosis | 34970 (82.3) | 26427 (84.4) | 8543(76.2) | <.001 |
| Valvular/Rheumatic Heart Disease | 2841 (6.7) | 1754 (5.6) | 1087 (9.7) | <.001 |
| Arrhythmias | 2015 (4.7) | 1303 (4.2) | 712 (6.4) | <.001 |
|
| ||||
| Procedures (%) | ||||
| Percutaneous Coronary Angioplasty | 6242 (14.7) | 4714 (15.1) | 1528 (13.6) | <.001 |
| Coronary Artery Bypass Graft Surgery | 1963 (4.6) | 1427 (4.6) | 536 (4.8) | .34 |
|
| ||||
| Co-morbidities (%) | ||||
| Chronic Obstructive Pulmonary Disease | 5172 (12.2) | 3306 (10.6) | 1866 (16.6) | <.001 |
| Pneumonia | 2781 (6.5) | 1741(5.6) | 1040 (9.3) | <.001 |
| Asthma | 2088 (4.9) | 1111(3.6) | 977 (8.7) | <.001 |
| Renal Failure | 2998 (7.1) | 1739 (5.6) | 1259 (11.2) | <.001 |
| End-stage renal disease or dialysis | 1068 (2.5) | 581 (1.9) | 487 (4.3) | <.001 |
| Vascular or Circulatory Disease | 2373 (5.6) | 1387 (4.4) | 986 (8.8) | <.001 |
| Other urinary tract disorders | 2120 (4.9) | 1554 (4.9) | 566 (5.1) | .73 |
| Disorders of fluid/electrolyte/acid-base | 3887 (9.1) | 2263 (7.2) | 1624 (14.5) | <.001 |
| History of infection | 1607(3.8) | 913 (2.9) | 694 (6.2) | <.001 |
| Metastatic Cancer and Acute Leukemia | 253 (0.6) | 132 (0.4) | 121 (1.1) | <.001 |
| Cancer | 964 (2.3) | 599 (1.9) | 365 (3.3) | <.001 |
| Iron deficiency and/or Anemia | 8603 (20.2) | 5240 (16.7) | 3363 (29.9) | <.001 |
| Decubitus ulcer or chronic skin ulcer | 921 (2.2) | 526 (1.67) | 395 (3.5) | <.001 |
| Protein-Calorie Malnutrition | 745 (1.8) | 446 (1.4) | 299 (2.7) | <.001 |
| Hemiplegia, Paralysis, Disability | 1098 (2.6) | 700 (2.2) | 398 (3.6) | <.001 |
| Dementia and Senility | 343 (0.8) | 197 (0.6) | 146 (1.3) | <.001 |
| Major psychiatric disorders | 1583 (3.7) | 913 (2.9) | 670 (5.9) | <.001 |
| Drug and alcohol abuse | 1663 (3.9) | 1274 (4.1) | 389 (3.5) | .01 |
|
| ||||
| LOS/Primary Discharge Disposition | ||||
| LOS, Mean ± SD | 4.53±5.8 | 4.4±6.0 | 4.9±6.4 | <.001 |
| LOS, Median (Q1, Q3) | 2 (5) | 2 (5) | 2 (5) | <.001 |
| Routine (home) | 38088 (89.6) | 28293 (90.3) | 9795 (87.3) | |
| Transfer other including SNF/ICF | 1642 (3.8) | 1074 (3.4) | 568 (5.0) | <.001 |
| HHC | 2694 (6.3) | 1870 (5.9) | 824 (7.3) | |
| Alive but place unknown | 93 (0.2) | 65 (0.2) | 28 (0.3) | |
CV= cardiovascular, AMI= acute myocardial infarction, SNF= skilled nursing facility, ICF= intermediate care facility, HHC= home health care, LOS= length of stay
The information about the patient’s cardiovascular risk factors and comorbidities were captured from the diagnosis codes in the hospitalization within one-year prior to the secondary diagnosis codes in the current hospitalization. Potential complications in the current hospitalization were excluded.
30-Day Readmission Rate
There were a total of 4,775 30-day all-cause readmissions, of which 1,736 were women. The crude readmission rate for women was 15.5%, compared with 9.7% for men (P<0.001) (Figure 1A). Among all sub-groups of age, women had higher rates of 30-day readmissions compared with similarly aged men: women aged 18–49 (14.9% vs. 8.7%), aged 50–54 (14.2% vs. 9.6%), aged 55–59 (15.7% vs. 10.0%), and aged 60–64 (16.5% vs. 10.5%) (P<0.0001 for all) (Figure 1B). When examining subgroups by race and payer status, younger women also had higher rates of 30-day readmission compared with younger men (P<0.0001 for all) (Figures 1C–D).
Figure 1.
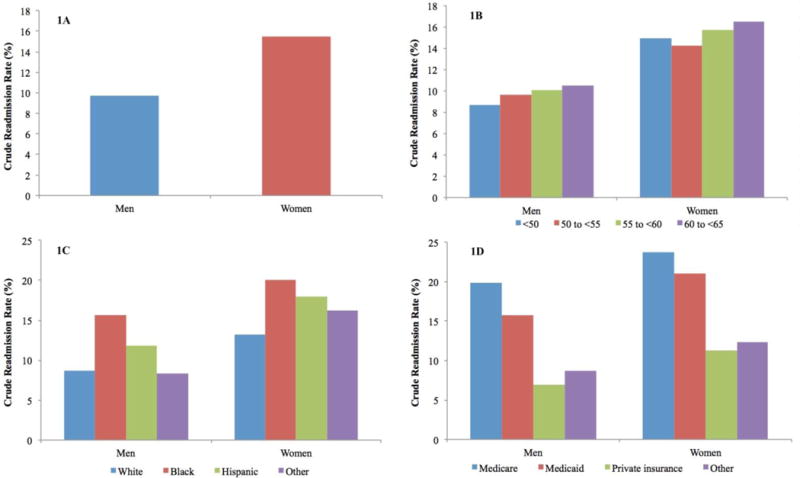
Readmission rates stratified by sex and specified groups in younger patients with AMI (1A: overall readmission rate, 1B: age groups, 1C: race groups and 1D: payer status groups). P-values for all <0.001.
Timing and Readmission Diagnosis
The daily percentages of all readmissions were highest between days 2–4 after discharge, with a peak at day 2 and a gradual decline thereafter for both sexes. In both women and men, the first week following AMI accounted for 42% of all hospital readmissions (Figure 2).
Figure 2.
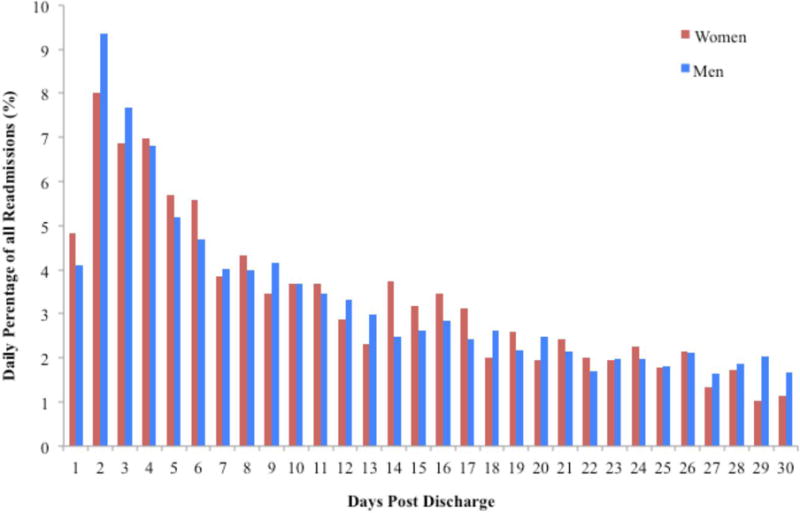
Timing of readmissions per day (0–30) post AMI for younger women (red) and men (blue). Non-significant for women vs. men.
The most frequent readmission diagnoses, by modified condition categories, for women and men are presented in Table 2. Overall, in comparison to men, women were more likely to present with non-cardiac causes (44.4% vs. 40.6%, P=0.01). Largely, the percentages of all readmissions were similarly distributed across diagnostic categories with a few exceptions. Specifically, women were more likely to present with COPD (2.4% vs. 0.9%, P<0.0001) and urinary tract disorders (1.7% vs. 0.5%, P<0.0001), whereas men were more likely to present with syncope (1.3% vs. 0.3%, P=0.001), chronic angina/coronary artery disease (8.5% vs. 6.9%, P<0.05) and chest pain (13.9% vs. 11.9%, P<0.05). On readmission, younger women were also less likely to receive cardiac catheterization (8.9% vs. 12.2%; P<0.0001) and percutaneous coronary intervention than men (5.0% vs. 7.7%; P<0.0001). However, rates of receiving coronary artery bypass grafting were similar between sexes (0.6% vs. 1.1%; P=0.06).
Table 2.
Principal Diagnosis at Readmission within 30 Days Post AMI Stratified by Sex and by Cardiac vs. Non-cardiac Causes.
| Characteristics | Total (N=4,775) |
Men (N=3,039) |
Women (N=1,736) |
P-value |
|---|---|---|---|---|
| Readmission for cardiac diagnosis*(%) | 2770 (58.0) | 1805 (59.4) | 965 (55.6) | .01 |
| Heart Failure | 614 (12.9) | 372 (12.2) | 242 (13.9) | .09 |
| Acute Myocardial Infarction | 457 (9.6) | 303 (9.9) | 154 (8.9) | .21 |
| UA and Other Acute Ischemic HD | 174 (3.6) | 105 (3.5) | 69 (3.9) | .36 |
| Chronic Angina and CAD | 376 (7.9) | 257 (8.5) | 119 (6.6) | .05 |
| Valvular/rheumatic Heart Disease | 8 (0.2) | 6 (0.2) | 2 (0.1) | .50 |
| Other Congenital Heart/Hypertensive Disease | 86 (1.8) | 52 (1.7) | 34 (1.9) | .54 |
| Arrhythmias and Conduction Disorders | 120 (2.5) | 82 (2.7) | 38 (2.2) | .28 |
| Chest Pain | 628 (13.2) | 422 (13.9) | 206 (11.9) | .04 |
| Syncope | 45 (0.9) | 39 (1.3) | 6 (0.4) | .01 |
| Acute stroke/TIA | 101 (2.1) | 64 (2.1) | 37 (2.1) | .95 |
| Pulmonary Embolism/DVT | 61 (1.3) | 37 (1.2) | 24 (1.4) | .63 |
| Other Peripheral Vascular Disease | 100 (2.1) | 66 (2.2) | 34 (1.9) | .62 |
|
| ||||
| Readmission for non-cardiac diagnosis*(%) | 2005 (42.0) | 1234 (40.6) | 771 (44.4) | .01 |
| Pleural Effusion/Pneumothorax | 46 (0.9) | 35 (1.2) | 11 (0.6) | .08 |
| Cardio-Respiratory Failure | 86 (1.8) | 54 (1.8) | 32 (1.8) | .87 |
| COPD | 69 (1.5) | 27 (0.9) | 42 (2.4) | <.001 |
| Pneumonia | 125 (2.6) | 77 (2.5) | 48 (2.8) | .63 |
| Septicemia/Shock | 130 (2.7) | 80 (2.6) | 50 (2.9) | .61 |
| UTI and Urinary System | 43 (0.9) | 14 (0.5) | 29 (1.7) | <.001 |
| Cellulitis | 33 (0.7) | 22 (0.7) | 11 (0.6) | .72 |
| Clostridium Difficile Infection | 14 (0.2) | 9 (0.3) | 5 (0.3) | .96 |
| Renal Disorders (Renal Failure) | 174 (3.6) | 104 (3.4) | 70 (4.0) | .28 |
| Anemia | 27 (0.6) | 15 (0.5) | 12 (0.7) | .38 |
| Gastrointestinal Hemorrhage | 75 (1.6) | 51 (1.7) | 24 (1.4) | .43 |
| Diabetes and its Complications | 84 (1.8) | 49 (1.6) | 35 (2.0) | .31 |
| Fibrosis of Lung & Other Disorders | 8 (0.2) | 5 (0.2) | 3 (0.2) | .95 |
| Hip Fracture | 4 (0.1) | 2 (0.1) | 2 (0.1) | .57 |
| Complications of Care | 391 (8.2) | 259 (8.5) | 132 (7.6) | .26 |
| Other Lung Disorders* | 22 (0.5) | 13 (0.4) | 9 (0.5) | .66 |
| Primary Cancer† | 11 (0.2) | 6 (0.2) | 5 (0.3) | .53 |
| Other | 663 (13.9) | 412 (13.6) | 251 (14.5) | .39 |
UA=unstable angina, HD=heart disease, CAD=coronary artery disease, TIA=transient ischemic attack, DVT=deep vein thrombosis, COPD=chronic obstructive pulmonary disease, UTI=urinary tract infection.
Readmission diagnosis grouped into cardiac vs. non-cardiac diagnoses based on criteria indicated in Supplemental Table 2.
Includes Acute, Congenital, and Unspecified Lung Abnormalities.
Includes cancer of the Trachea, Bronchus, Lung, and Pleura.
Independent Association of Sex on Readmission
No violation on the proportional-hazards assumption was found, the proportional-hazard survival models are appropriate for the evaluation on the sex differences on readmission. Figure 3 shows the association of sex with readmission, sequentially adjusting for important confounders. In the unadjusted model, women were more likely to have a higher rate of readmission than men (HR=1.65, 95% CI 1.55, 1.75). After sequentially adjusting for socio-demographics (HR=1.40, 95% CI 1.32, 1.49), both socio-demographics and cardiovascular risk factors (HR=1.28, 95% CI 1.20, 1.36), socio-demographics, cardiovascular risk factors and other co-morbidities (HR=1.21, 95% CI 1.14, 1.29), socio-demographics, cardiovascular risk factors, other co-morbidities, and length of stay (HR=1.22, 95% CI 1.15, 1.30), as well as socio-demographics, cardiovascular risk factors, other co-morbidities, length of stay, and discharge disposition (HR=1.22, 95% CI 1.15, 1.30), women still had a 22% higher risk of readmission compared with similarly aged men. When assessing the interaction between age and sex on readmission in the final model (age as a continuous variable), this was not statistically significant, suggesting that this association with readmission is not modified by age (P=0.53). To directly assess whether a secondary diagnosis of heart failure explained the higher readmission rate in women (23% women vs. 17% men, P<0.001), we further adjusted for this in the final step of our Cox regression model. Despite this adjustment we found that women still had a 22% higher risk of 30-day readmission compared with men (HR=1.22, 95% CI 1.15, 1.30). In addition, to test whether participants with multiple admissions produced bias by underestimating the standard errors, we repeated the Cox regression model by adding the index admissions clustering with the patients and found a similar result. This is likely due to the fact that few patients appeared more than once (N=1,429 total).
Figure 3.
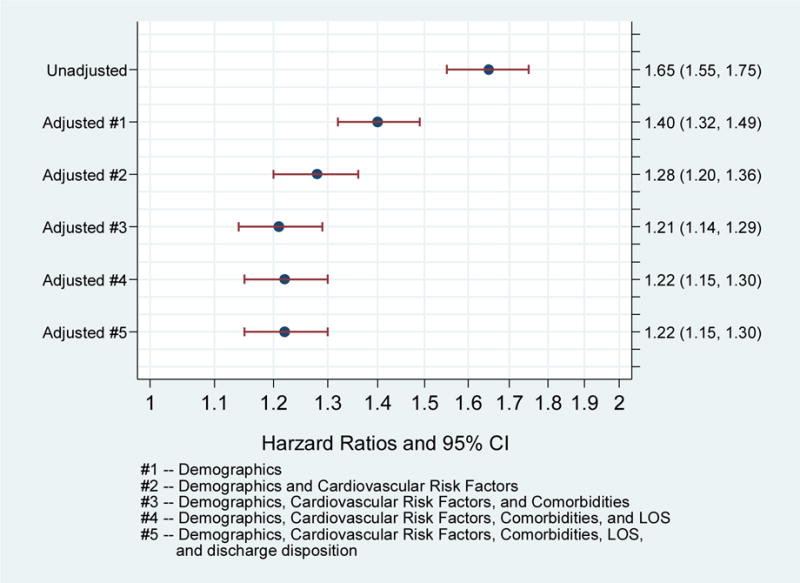
Forest Plot showing the independent association of sex on readmission (unadjusted and adjusted) (Hazard ratios & 95% Confidence intervals). P-values for each model <0.001.
DISCUSSION
We found that younger women (<65 years) have nearly a two-fold higher crude 30-day readmission rate following AMI compared with younger men, an association that persists following extensive adjustment for confounders, and is consistent across all strata of age. We also observed a higher crude rate of readmission in younger women across race and insurance status sub-groups. Despite the higher magnitude, the timing of readmission within 30-days was similar in women compared with men. In both sexes, more than two-fifths of readmissions were due to causes unrelated to their initial AMI, with women having a higher proportion of non-cardiac admissions.
This is the first comprehensive assessment of sex differences in 30-day readmissions after AMI in younger women, systematically characterizing the timing and causes of these readmissions. Younger women with AMI are at greater risk of adverse outcomes,2–4 and represent a population who have not been specifically investigated.19–21 Previous studies examining sex differences in readmissions after AMI have focused solely on older populations. They suggest that older women (aged ≥65 years) have a 20–60% greater risk for readmission compared with men.22–25 However, these studies looked only at longer time periods (6 months to 1-year), which include risk that may not be related to the initial hospitalization.23–25 The 30-day period following hospitalization is a crucial interval, as it accounts for over a third of the annual hospitalizations after medical conditions and is the focus of national improvement efforts.10 Therefore, identifying patients at a higher risk for re-hospitalization during this period provides opportunities to develop interventions to reduce readmissions that are appropriate for an individual’s risk of readmission.
We found nearly twice as many readmissions in younger women as compared with younger men, and this was observed among all age sub-groups. In the sequential model, a large proportion of the association of sex on readmission was explained by socio-demographic differences. Younger women with AMI were more likely African-American and dependent on federal insurance. Further, we noted that women had a much higher comorbidity burden, which added to their vulnerability for readmission. However, even in the final model after adjusting for all covariates, women remained at a 22% higher risk for readmission. These findings suggest that there are other factors at play that predispose younger women to readmission. Mechanistic features underlying this risk may include differences in co-morbidities and/or consequences of the AMI, as well as social and/or psychosocial factors. Nevertheless, after an AMI, younger women bear a much greater burden of risk of an acute event requiring a hospitalization than younger men. There are several possible reasons why readmission rates are higher for younger women than younger men. Firstly, younger women are prone to more complications after a hospitalization for AMI, such as longer lengths of stay and bleeding events.2–4 In addition, we hypothesize that women may be more susceptible to the disruption of the hospitalization itself and have more stressful and difficult experiences than men, and this excess allostatic load may lead to a greater vulnerability after discharge.
Moreover, readmission has multifaceted elements, and previous studies examining sex differences have indicated that psychosocial factors such as depression may also have negative consequences for readmission.25 Indeed, our analyses did not account for potential important psychosocial influences such as health status (symptoms, functioning, quality of life),26, 27 social support and the role of stress.28, 29 Further, it has previously been shown that work/home roles, including providing care to their children and family, play an important prognostic role in women post AMI;30, 31 since they have additional caregiving responsibilities,32 we hypothesize that women may be less likely to focus on their own recovery following AMI, and this may act as a potential social explanation for the sex based differences in readmission. Providing care for family members may be a burden, but also raises the possibility that women may be less likely to have caregivers themselves after an AMI.33, 34 In fact, having a caregiver following a cardiac hospitalization has been shown to be a predictor of re-hospitalization and/or adverse outcomes.32, 35–37 The influence of these factors on readmission should be further investigated in regards to sex differences.
Although younger women had a higher rate of readmission compared with similarly aged men, the pattern of readmission timing was generally similar. Specifically, the risk for readmission was greatest between days two and four (peaking at day two) with a large proportion of readmissions occurring in the first week, and this pattern did not vary by sex. Similar to previous research,13 the timing of 30-day readmissions in our study highlights that the immediate few days following discharge represent an extremely high-risk period, particularly after AMI. This is an intense period of recovery and adjustment for the patient and they are not likely to be seeing a physician or other health care professional during this period,38, 39 especially for this young population, as a large majority are discharged home. Reducing readmissions during this period may necessitate in-hospital interventions and better discharge planning practices, including incorporating early ambulatory interventions.
There were a variety of causes for readmission, and a large proportion of readmission diagnoses in both sexes were due to reasons unrelated to the primary reason for hospitalization10, 13 and women were shown to have a higher proportion of non-cardiac admissions compared with men, although this was only a modest difference. Further, it is important to point out that in absolute rates, the rate of both cardiac (8.6%) and non-cardiac hospitalizations were higher in women than in men (5.8% and 3.9%), and thus this should not be interpreted as a lower likelihood that a readmission be cardiac instead of non-cardiac among women, to be confused with lower rates of cardiac hospitalizations. This period of acquired vulnerability to readmission for a broad range of diagnoses following hospitalization- a phenomenon called the post-hospital syndrome12, 13- has been shown across a variety of conditions, and we found that both sexes were similarly susceptible. Even in the first week following hospital discharge, a sizeable proportion of readmissions were for non-cardiovascular causes. Although the mechanism for the post-hospital syndrome is currently unclear, it may be a result of allostatic stress during the hospital stay (i.e. loss of strength and mobility40 difficulty performing daily activities,41–43 nutritional/sleep deprivation,44, 45 and delirium,46 and/or a complex interplay between community level and patient related factors). Overall, women were more likely to have non-cardiac diagnoses compared with men, but the difference was small. The reasons why women are more vulnerable for unrelated causes for readmission is unclear and warrants further study.
Study Implications
This study highlights, that younger women of all age groups <65 years, are at higher risk for readmission than similarly aged men. Moving forward, healthcare providers should be made aware of this disparity, and research efforts be directed toward identifying risk factors or opportunities in care that differ between groups and that may mediate the observed disparities in the risk of readmission, which may inform effective interventions. Given the high risk for early readmission after AMI, there may need to be continued focus on safe discharge planning and early ambulatory interventions following hospital discharge. More specifically, there is an opportunity to focus on young women, a high-risk group, who are inherently more unaware of the prevalence of coronary artery disease.
Limitations
Our study has several limitations. First, our analysis is based on administrative claims data, which lack information on potential explanatory factors, for example health status and the severity of the initial AMI, which may explain the sex disparities observed. Second, our data may not be nationally representative, as we analyzed only the state of California. However, California is the most populous state, representing 12% of the US population. Third, as there is no denominator file for California we have only reported the rates of re-hospitalization within California, and thus there is a possibility that some patients would be hospitalized outside of California, however we expect that to be rare and to not have biased our results. Fourth, we lacked information regarding treatment, including the use of fibrinolytic therapy, guideline medications (i.e. aspirin, statins, beta blockers), as well as rates of filling these medications post discharge. Fifth, the readmission causes included in this study were by primary discharge diagnosis and not via presentation/admission reason for re-hospitalization. Lastly, due to unavailability of mortality data we were unable to account for the competing risk of mortality on the risk of readmission. However, as we know from prior studies that younger women have a higher mortality than younger men, accounting for the competing risk of mortality may only make the differences in risk for readmission more pronounced.
CONCLUSION
We observed nearly a 2-fold greater risk of readmission in younger women with AMI as compared with younger men. Importantly, the association of sex persists even following extensive adjustment for covariates, and does not vary by age. The timing of readmission was broadly similar between sexes, and both sexes were vulnerable for a wide range of unrelated causes for readmission, a pattern consistent with a ‘post-hospital syndrome.’ The key finding is that the pattern was similar in women and men, but the rate was substantially higher in women.
Supplementary Material
Acknowledgments
Funding Sources: Dr Krumholz is supported by grant U01 HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. Dr. Isuru Ranasinghe is supported by an early career fellowship co-funded by the National Health and Medical Research Council of Australia and the National Heart Foundation of Australia. Dr. Dharmarajan is supported by grant K23AG048331-01 from the National Institute on Aging and the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Health and Medical Research Council of Australia, the National Heart Foundation of Australia, the American Federation for Aging Research or the National Institutes of Health.
Disclosures: Mr. Wang, Dr. Dharmarajan, and Dr. Krumholz work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. Dr. Krumholz is chair of a cardiac scientific advisory board for UnitedHealth and is the recipient of research agreements from Medtronic, Inc. and Johnson and Johnson through Yale University. In addition, Dr. Spertus is supported by grants from Gilead, Genentech, Lilly, Amorcyte, and EvaHeart, and has a patent Seattle Angina Questionnaire with royalties paid.
Footnotes
Journal Subject Codes: [100] Health policy and outcome research, [4] Acute myocardial infarction, [8] Epidemiology
The other authors report no conflicts.
References
- 1.Levit RD, Reynolds HR, Hochman JS. Cardiovascular disease in young women: A population at risk. Cardiol Rev. 2011;19:60–65. doi: 10.1097/CRD.0b013e31820987b5. [DOI] [PubMed] [Google Scholar]
- 2.Beckie T. Biopsychosocial determinants of health and quality of life among young women with coronary heart disease. Curr Cardiovasc Risk Rep. 2014;8:1–10. [Google Scholar]
- 3.Vaccarino V, Horwitz RI, Meehan TP, Petrillo MK, Radford MJ, Krumholz HM. Sex differences in mortality after myocardial infarction: Evidence for a sex-age interaction. Arch Intern Med. 1998;158:2054–2062. doi: 10.1001/archinte.158.18.2054. [DOI] [PubMed] [Google Scholar]
- 4.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National registry of myocardial infarction 2 participants. N Engl J Med. 1999;341:217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 5.Vaccarino V, Krumholz HM, Yarzebski J, Gore JM, Goldberg RJ. Sex differences in 2-year mortality after hospital discharge for myocardial infarction. Ann Intern Med. 2001;134:173–181. doi: 10.7326/0003-4819-134-3-200102060-00007. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Z, Fang J, Gillespie C, Wang G, Hong Y, Yoon PW. Age-specific gender differences in in-hospital mortality by type of acute myocardial infarction. Am J Cardiol. 2012;109:1097–1103. doi: 10.1016/j.amjcard.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde-Price C, D’Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol. 2014;64:337–345. doi: 10.1016/j.jacc.2014.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drye EE, Normand SL, Wang Y, Ross JS, Schreiner GC, Han L, Rapp M, Krumholz HM. Comparison of hospital risk-standardized mortality rates calculated by using in-hospital and 30-day models: An observational study with implications for hospital profiling. Ann Intern Med. 2012;156:19–26. doi: 10.1059/0003-4819-156-1-201201030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruiz B, Garcia M, Aguirre U, Aguirre C. Factors predicting hospital readmissions related to adverse drug reactions. Eur J Clin Pharmacol. 2008;64:715–722. doi: 10.1007/s00228-008-0473-y. [DOI] [PubMed] [Google Scholar]
- 10.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 11.Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and readmission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170:1664–1670. doi: 10.1001/archinternmed.2010.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krumholz HM. Post-hospital syndrome–an acquired, transient condition of generalized risk. N Engl J Med. 2013;368:100–102. doi: 10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Bernheim SM, Suter LG, Drye EE, Krumholz HM. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindenauer PK, Normand SL, Drye EE, Lin Z, Goodrich K, Desai MM, Bratzler DW, O’Donnell WJ, Metersky ML, Krumholz HM. Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. J Hosp Med. 2011;6:142–150. doi: 10.1002/jhm.890. [DOI] [PubMed] [Google Scholar]
- 15.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp MT, Mattera JA, Normand SL. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–252. doi: 10.1161/CIRCOUTCOMES.110.957498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keenan PS, Normand SL, Lin Z, Drye EE, Bhat KR, Ross JS, Schuur JD, Stauffer BD, Bernheim SM, Epstein AJ, Wang Y, Herrin J, Chen J, Federer JJ, Mattera JA, Krumholz HM. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29–37. doi: 10.1161/CIRCOUTCOMES.108.802686. [DOI] [PubMed] [Google Scholar]
- 17.Center for Medicare & Medicaide Services. Planned Readmission Algorithm. 2013 Available: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed 1 July 2013.
- 18.Pope GCER, Ash AS, Ayanian JZ, Bates DW, Burstin H, Iezzoni LI, Marcantonio E, Wu B. Report prepared for the health care financing administration. Waltham, MA: Health Economics Research, Inc; 2000. Diagnostic cost group hierarchical condition category models for medicare risk adjustment. [Google Scholar]
- 19.Kim AM, Tingen CM, Woodruff TK. Sex bias in trials and treatment must end. Nature. 2010;465:688–689. doi: 10.1038/465688a. [DOI] [PubMed] [Google Scholar]
- 20.Kim ES, Carrigan TP, Menon V. Enrollment of women in national heart, lung, and blood institute-funded cardiovascular randomized controlled trials fails to meet current federal mandates for inclusion. J Am Coll Cardiol. 2008;52:672–673. doi: 10.1016/j.jacc.2008.05.025. [DOI] [PubMed] [Google Scholar]
- 21.Kim ES, Menon V. Status of women in cardiovascular clinical trials. Arterioscler Thromb Vasc Biol. 2009;29:279–283. doi: 10.1161/ATVBAHA.108.179796. [DOI] [PubMed] [Google Scholar]
- 22.Anand SS, Xie CC, Mehta S, Franzosi MG, Joyner C, Chrolavicius S, Fox KA, Yusuf S. Differences in the management and prognosis of women and men who suffer from acute coronary syndromes. J Am Coll Cardiol. 2005;46:1845–1851. doi: 10.1016/j.jacc.2005.05.091. [DOI] [PubMed] [Google Scholar]
- 23.Dey S, Flather MD, Devlin G, Brieger D, Gurfinkel EP, Steg PG, Fitzgerald G, Jackson EA, Eagle KA. Sex-related differences in the presentation, treatment and outcomes among patients with acute coronary syndromes: The global registry of acute coronary events. Heart. 2009;95:20–26. doi: 10.1136/hrt.2007.138537. [DOI] [PubMed] [Google Scholar]
- 24.Humphries KH, Pu A, Gao M, Carere RG, Pilote L. Angina with “normal” coronary arteries: Sex differences in outcomes. Am Heart J. 2008;155:375–381. doi: 10.1016/j.ahj.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 25.Parashar S, Rumsfeld JS, Reid KJ, Buchanan D, Dawood N, Khizer S, Lichtman J, Vaccarino V. Impact of depression on sex differences in outcome after myocardial infarction. Circ Cardiovasc Qual Outcomes. 2009;2:33–40. doi: 10.1161/CIRCOUTCOMES.108.818500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spertus JA. Evolving applications for patient-centered health status measures. Circulation. 2008;118:2103–2110. doi: 10.1161/CIRCULATIONAHA.107.747568. [DOI] [PubMed] [Google Scholar]
- 27.Garavalia LS, Decker C, Reid KJ, Lichtman JH, Parashar S, Vaccarino V, Krumholz HM, Spertus JA. Does health status differ between men and women in early recovery after myocardial infarction? J Womens Health (Larchmt) 2007;16:93–101. doi: 10.1089/jwh.2006.M073. [DOI] [PubMed] [Google Scholar]
- 28.Bucholz EM, Strait KM, Dreyer RP, Geda M, Spatz ES, Bueno H, Lichtman JH, D’Onofrio G, Spertus JA, Krumholz HM. Effect of low perceived social support on health outcomes in young patients with acute myocardial infarction: Results from the virgo (variation in recovery: Role of gender on outcomes of young ami patients) study. J Am Heart Assoc. 2014;3:e001252. doi: 10.1161/JAHA.114.001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xu X, Bao H, Strait K, Spertus JA, Lichtman JH, D’Onofrio G, Spatz E, Bucholz EM, Geda M, Lorenze NP, Bueno H, Beltrame JF, Krumholz HM. Sex differences in perceived stress and early recovery in young and middle-aged patients with acute myocardial infarction. Circulation. 2015;131:614–23. doi: 10.1161/CIRCULATIONAHA.114.012826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kristofferzon ML, Lofmark R, Carlsson M. Myocardial infarction: Gender differences in coping and social support. J Adv Nurs. 2003;44:360–374. doi: 10.1046/j.0309-2402.2003.02815.x. [DOI] [PubMed] [Google Scholar]
- 31.Brezinka V, Kittel F. Psychosocial factors of coronary heart disease in women: A review. Soc Sci Med. 1996;42:1351–1365. doi: 10.1016/0277-9536(95)00284-7. [DOI] [PubMed] [Google Scholar]
- 32.Aggarwal B, Liao M, Christian A, Mosca L. Influence of caregiving on lifestyle and psychosocial risk factors among family members of patients hospitalized with cardiovascular disease. J Gen Intern Med. 2009;24:93–98. doi: 10.1007/s11606-008-0852-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamilton GA, Seidman RN. A comparison of the recovery period for women and men after an acute myocardial infarction. Heart Lung. 1993;22:308–315. [PubMed] [Google Scholar]
- 34.Rose GL, Suls J, Green PJ, Lounsbury P, Gordon E. Comparison of adjustment, activity, and tangible social support in men and women patients and their spouses during the six months post-myocardial infarction. Ann Behav Med. 1996;18:264–272. doi: 10.1007/BF02895288. [DOI] [PubMed] [Google Scholar]
- 35.Mosca L, Mochari-Greenberger H, Aggarwal B, Liao M, Suero-Tejeda N, Comellas M, Rehm L, Umann TM, Mehran R. Patterns of caregiving among patients hospitalized with cardiovascular disease. J Cardiovasc Nurs. 2011;26:305–311. doi: 10.1097/JCN.0b013e3181f34bb3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in u.S. Women: A prospective study. Am J Prev Med. 2003;24:113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 37.Samuel-Hodge CD, Headen SW, Skelly AH, Ingram AF, Keyserling TC, Jackson EJ, Ammerman AS, Elasy TA. Influences on day-to-day self-management of type 2 diabetes among african-american women: Spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23:928–933. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- 38.Sommers A, Cunningham PJ. Physican visits after hospital discharge: Implications for reducing readmissions. National Instiute for Health Care Reform; 2011. (Report no. 6). [Google Scholar]
- 39.Balady GJ, Ades PA, Bittner VA, Franklin BA, Gordon NF, Thomas RJ, Tomaselli GF, Yancy CW, American Heart Association Science A, Coordinating C Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: A presidential advisory from the american heart association. Circulation. 2011;124:2951–2960. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 40.Kortebein P, Ferrando A, Lombeida J, Wolfe R, Evans WJ. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA. 2007;297:1772–1774. doi: 10.1001/jama.297.16.1772-b. [DOI] [PubMed] [Google Scholar]
- 41.Gill TM, Allore HG, Gahbauer EA, Murphy TE. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304:1919–1928. doi: 10.1001/jama.2010.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gill TM, Allore HG, Holford TR, Guo Z. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 43.Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, Burant CJ, Landefeld CS. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 44.Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients: A prospective study. JAMA. 1999;281:2013–2019. doi: 10.1001/jama.281.21.2013. [DOI] [PubMed] [Google Scholar]
- 45.Yoder JC, Staisiunas PG, Meltzer DO, Knutson KL, Arora VM. Noise and sleep among adult medical inpatients: Far from a quiet night. Arch Intern Med. 2012;172:68–70. doi: 10.1001/archinternmed.2011.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kiely DK, Bergmann MA, Murphy KM, Jones RN, Orav EJ, Marcantonio ER. Delirium among newly admitted postacute facility patients: Prevalence, symptoms, and severity. J Gerontol A Biol Sci Med Sci. 2003;58:M441–445. doi: 10.1093/gerona/58.5.m441. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


