Abstract
Objectives
Assess trends in hospitalizations and outcomes for Takotsubo cardiomyopathy (TTC).
Background
There is a paucity of nationally representative data on trends in short- and long-term outcomes for TTC.
Methods
We reported hospitalization rates, in-hospital, 30-day, 1-year mortality, and all-cause 30-day readmission for Medicare fee-for-service beneficiaries with a principal and secondary diagnosis of TTC from 2007 to 2012.
Results
Hospitalizations for principal or secondary diagnosis of TTC increased from 5.7 per 100,000 person-years in 2007 to 17.4 in 2012 (p for trend <0.001). Patients were predominantly female and of white race. For principal TTC, in-hospital, 30-day, and 1-year mortality was 1.3% (95% Confidence interval [CI] 1.1–1.6), 2.5% (95% CI 2.2–2.8), and 6.9% (95% CI 6.4–7.5), and 30-day readmission rate was 11.6% (95% CI 10.9–12.3). For secondary TTC, in-hospital, 30-day, and 1-year mortality was 3% (95% CI 2.7–3.3), 4.7% (95% CI 4.4–5.1), 11.4% (95% CI 10.8–11.9), and 30-day readmission was 15.8% (15.1–16.4). Over time, there was no change in mortality or readmission for both cohorts. Patients ≥85 years had higher in-hospital, 30-day, and 1-year mortality, and 30-day readmission. Among principal TTC patients, male and non-white patients had higher 1-year mortality than their counterparts, while in secondary TTC, the mortality was worse at all 3 time points. Non-white patients had higher 30-day readmission for both cohorts.
Conclusions
Hospitalization rates for TTC are increasing, but short- and long-term outcomes have not changed. At 1 year, 14 in 15 patients with principal TTC and 8 in 9 with secondary TTC are alive. Older, male, and non-white patients have worse outcomes.
Keywords: stress cardiomyopathy, apical ballooning syndrome, mortality, readmission
UNSTRUCTURED ABSTRACT
We assessed hospitalization rates and outcomes for Medicare fee-for-service beneficiaries with a principal and secondary diagnosis of TTC from 2007 to 2012. Hospitalizations for principal or secondary diagnosis of TTC increased from 5.7 per 100,000 person-years in 2007 to 17.4 in 2012 (p for trend <0.001). For principal TTC, in-hospital, 30-day, and 1-year mortality was 1.3% (95% Confidence interval [CI] 1.1–1.6), 2.5% (95% CI 2.2–2.8), and 6.9% (95% CI 6.4–7.5). For secondary TTC, in-hospital, 30-day, and 1-year mortality was 3% (95% CI 2.7–3.3), 4.7% (95% CI 4.4–5.1), and 11.4% (95% CI 10.8–11.9). Older, male, and non-white patients had worse outcomes.
INTRODUCTION
Takotsubo cardiomyopathy (TTC), also known as stress cardiomyopathy or apical ballooning syndrome, is a rare, but increasingly recognized cardiac syndrome that mimics acute myocardial infarction (AMI).(1) It is frequently triggered by an acute medical illness or intense emotional or physical stress, predominantly affecting elderly women. TTC is usually characterized by transient systolic dysfunction of segments of the left ventricle in the absence of angiographic evidence of obstructive coronary artery disease (CAD) or acute plaque rupture.(2)
Our knowledge regarding outcomes of patients with TTC is largely limited to case series due to the rarity of the disease.(3–5) These studies suggest that the short-term prognosis for this enigmatic condition is favorable, with most patients surviving the acute episode and experiencing recovery of ventricular function. However, wide variation (0–8%) in in-hospital mortality rates have been reported(6) and there is a paucity of nationally representative data. Further, little is known about longer term clinical outcomes, including mortality and readmission, following TTC, or trends in hospitalizations and outcomes.
Accordingly, we assessed trends in hospitalization rates and outcomes for TTC in the United States among Medicare fee-for-service beneficiaries between 2007 and 2012. We evaluated in-hospital, 30-day, and 1-year mortality, 30-day readmission, and risk-adjusted trends in these outcomes. We also evaluated trends in length of stay (LOS) and discharge disposition. Finally, we assessed differences in outcomes by sub groups of age, sex, and race.
As TTC can present both as an acute coronary syndrome or occur in conjunction with an acute medical illness, we reported outcomes separately for principal and secondary diagnosis of TTC. We reasoned that hospitalizations with a principal diagnosis of TTC more likely represent primary coronary presentations of TTC, while hospitalizations with a secondary diagnosis of TTC more likely represent cases where there was a significant acute medical illness that was the primary reason for admission, and TTC was precipitated by the acute medical illness. This distinction is important, as outcomes for secondary diagnosis of TTC are likely to be driven by the primary reason for hospitalization.
METHODS
Study population
We used Medicare inpatient claims data and Medicare enrollment data from the Centers for Medicare & Medicaid Services (CMS) to identify all Medicare fee-for-service (FFS) beneficiaries aged 65 years or older hospitalized with a principal or secondary diagnosis of TTC in an acute-care hospital in the United States from January 1, 2007 to December 31, 2012 using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 429.83. As the specific ICD-9-CM code for TTC was introduced in October 2006, we used only data from 2007 onward. Although there is no worldwide consensus on the diagnostic criteria for TTC, most criteria for diagnosing TTC require the absence of obstructive CAD or angiographic evidence of acute plaque rupture.(2,7) Thus, we included only those patients in our study sample who underwent coronary angiography (ICD-9-CM codes 37.22, 37.23, 88.55, 88.56, and 88.57) and did not receive revascularization therapy (i.e., percutaneous coronary intervention [ICD-9-CM codes 36.01, 36.02, 36.05, 36.07, 36.09, or 00.66] or coronary artery bypass grafting [ICD-9-M codes 36.1x]). This method has been used previously.(8) For the hospitalization analysis, the unit of analysis was at the Medicare fee-for-service beneficiary level; for reporting patient characteristics and the outcome analysis, the unit of analysis was at the patient level. Thus, if a patient had >1 admission for TTC during the year, we randomly selected 1 hospitalization. Institutional review board approval was obtained from the Yale University Human Investigation Committee.
Patient characteristics
We examined patients’ age, sex, race (white, black, other) as well as common comorbidities and trends in the demographic and clinical profiles separately for patients with a principal and secondary diagnosis of TTC. Comorbidities included those used in risk-adjustment models of 30-day mortality measures for AMI and heart failure.(9,10) They were identified from secondary discharge diagnosis codes in the index hospitalization for TTC as well as principal or secondary diagnosis codes of all inpatient hospitalizations up to 1 year prior. For patients hospitalized in 2007, comorbidities were assessed using in-patient claims data from 2006.
Hospitalization rates and outcomes
We reported hospitalization rates separately for principal diagnosis, secondary diagnosis, and any diagnosis (principal or secondary) of TTC. We calculated the annual rate of hospitalization for TTC by dividing the number of hospitalizations with a discharge diagnosis of TTC by the corresponding person-years for all fee-for-service Medicare beneficiaries in that year, in order to account for new enrollment, disenrollment, or death during an index year.
We reported outcomes separately for principal and secondary diagnosis of TTC. We evaluated the following outcomes associated with these hospitalizations: all-cause in-hospital and 30-day mortality; LOS; proportion discharged to home; all-cause 30-day readmission rates; and 1-year mortality and reported trends in these outcomes. To permit complete follow-up, we restricted the 1-year mortality analysis to 2011 discharges and the 30-day all-cause readmission analysis to November 30, 2012 discharges. Among strata of age, sex, and race (white vs. non-white), we only reported outcomes for the entire time period combined. For patients admitted with a secondary diagnosis of TTC we listed the top 10 principal diagnoses.
Statistical analysis
Annual hospitalization rates were expressed as per 100,000 person-years. We calculated hospitalization rates for TTC overall and for the first (2007) and last (2012) year of the cohort. To simplify presentation, we assessed patient demographics, clinical characteristics, and outcomes of unique patients hospitalized for TTC in 2-year intervals. Rates of mortality, readmission, and proportion discharged to home were expressed as percentages. LOS was represented in days. We used the Mantel-Haenszel chi-square test to determine the significance of temporal changes in hospitalization rates, patient characteristics, and outcomes. In addition, we fitted a linear mixed-effects model with a logit link function and hospital-specific random intercepts, adjusting for patient demographics and comorbidities, as in the CMS mortality measures,(9–11) to estimate temporal changes in rates of 30-day and 1-year mortality. For 30-day readmission, we conducted a survival analysis to calculate the proportion of patients who were readmitted for any cause to an acute care hospital, censoring those who died before readmission. We constructed a Cox proportional hazards model to assess the change in the readmission rate over time. We fitted separate models for each outcome. All models included an ordinal time variable, ranging from 0 to 5, corresponding to each year of the study period, after the visual inspection of crude rates revealed a linear pattern. All statistical tests were 2-sided at a significance level of p<0.05. All analyses were performed with SAS version 9.3 64-bit (SAS Institute, Cary, North Carolina).
RESULTS
Hospitalizations
Overall, there were 9,442 hospitalizations with a principal diagnosis of TTC from 2007–2012. Of those, there were 8,090 (85.7%) hospitalizations contributed by 8,068 unique Medicare beneficiaries in which the patient underwent an angiogram but did not receive revascularization therapy (from here on called the principal TTC cohort). The annual number of principal TTC hospitalizations increased from 634 in 2007 to 2008 in 2012 and the corresponding incidence of TTC increased from 2.3 hospitalizations per 100,000 person-years in 2007 to 7.1 in 2012 (p for trend <0.001).
From 2007–2012, 26,048 hospitalizations were associated with a secondary diagnosis of TTC. Of those, there were 11,971 (46%) hospitalizations, contributed by 11,898 unique Medicare beneficiaries, in which the patient with a secondary diagnosis of TTC underwent an angiogram but did not receive revascularization therapy (from here on we call this the secondary TTC cohort). The annual number of secondary TTC hospitalizations increased from 944 in 2007 to 2921 in 2012, and the corresponding incidence of TTC increased from 3.4 hospitalizations per 100,000 person-years in 2007 to 10.3 in 2012 (p for trend <0.001).
Combined, the incidence of TTC hospitalizations with principal or secondary diagnosis of TTC where the patient underwent an angiogram but did not receive revascularization therapy increased from 5.7 hospitalizations per 100,000 person-years in 2007 to 17.4 in 2012 (p for trend <0.001).
Patient characteristics
Patients were predominantly female (94.3% for principal TTC and 90.3% for secondary TTC) and of white race (92.6% for principal TTC and 90.3% for secondary TTC) in both principal and secondary TTC, but patients with secondary TTC were more likely male and non-white (P<0.001 for both). Cardiovascular risk factors were common and increased over time. A large proportion had a prior diagnosis of atherosclerotic disease (46.1% among principal TTC and 47.5% among secondary TTC) (Table 1).
Table 1.
Patient characteristics, by 2-year intervals and combined years for principal and secondary TTC cohort.
| Principal | Secondary | |||||||
|---|---|---|---|---|---|---|---|---|
| Patient characteristics |
2007–2008 | 2009–2010 | 2011–2012 | Total | 2007–2008 | 2009–2010 | 2011–2012 | Total |
| No. of patients | 1540 | 2733 | 3795 | 8068 | 2561 | 4009 | 5328 | 11898 |
| Demographics | ||||||||
| Mean age, years (SD) |
75.7(6.5) | 76.1(6.7) | 76.0(6.8) | 76.0 (6.7) | 76.3(6.5) | 76.4(6.9) | 76.5(7.0) | |
| Female | 1471(95.5) | 2577(94.3) | 3560(93.8)* | 7701(94.3) | 2381(93) | 3682(91.8) | 4830(90.7)* | 10800(90.8) |
| Race | ||||||||
| White | 1441(93.6) | 2515(92.0) | 3517(92.7) | 7564(92.6) | 2358(92.1) | 3626(90.4) | 4851(91) | 10744(90.3) |
| Black | 57(3.7) | 117(4.3) | 149(3.9) | 329(4) | 120(4.7) | 227(5.7) | 279(5.2) | 620(5.2) |
| Other race@ | 42(2.7) | 101(3.7) | 129(3.4) | 274(3.4) | 83(3.2) | 156(3.9) | 198(3.7) | 435(3.7) |
| Risk factors and cardiovascular conditions | ||||||||
| Hypertension | 1009(65.5) | 1837(67.2) | 2592(68.3)* | 5507(67.4) | 1615(63.1) | 2490(62.1) | 3466(65.1)* | 7502(63.1) |
| Diabetes | 225(14.6) | 529(19.4) | 742(19.6)* | 1510(18.5) | 466(18.2) | 781(19.5) | 1155(21.7) * |
2388(20.1) |
| Atherosclerotic disease |
658(42.7) | 1276(46.7) | 1787(47.1)* | 3763(46.1) | 1220(47.6) | 1877(46.8) | 2591(48.6) | 5646(47.5) |
| Unstable angina | 16(1.0) | 25(0.9) | 26(0.7) | 68(0.8) | 29(1.1) | 45(1.1) | 51(1) | 124(1) |
| Prior myocardial infarction |
20(1.3) | 50(1.8) | 69(1.8) | 140(1.7) | 51(2) | 93(2.3) | 129(2.4) | 272(2.3) |
| Prior heart failure | 74(4.8) | 166(6.1) | 182(4.8) | 427(5.2) | 191(7.5) | 281(7) | 451(8.5) * | 918(7.7) |
| Stroke | 15(1.0) | 29(1.1) | 37(1.0) | 81(1) | 31(1.2) | 55(1.4) | 81(1.5) | 167(1.4) |
| Cerebrovascular disease other than stroke |
35(2.3) | 61(2.2) | 85(2.2) | 185(2.3) | 75(2.9) | 109(2.7) | 187(3.5) | 367(3.1) |
| Peripheral vascular disease |
62(4.0) | 86(3.1) | 121(3.2) | 274(3.4) | 114(4.5) | 194(4.8) | 265(5) | 568(4.8) |
| Other conditions | ||||||||
| Malnutrition | 45(2.9) | 99(3.6) | 158(4.2)* | 305(3.7) | 120(4.7) | 248(6.2) | 377(7.1) * | 742(6.2) |
| Dementia | 53(3.4) | 156(5.7) | 113(3.0)* | 325(4) | 111(4.3) | 199(5) | 251(4.7) | 558(4.7) |
| Functional disability |
21(1.4) | 37(1.4) | 66(1.7) | 125(1.5) | 33(1.3) | 63(1.6) | 94(1.8) | 189(1.6) |
| Renal failure | 52(3.4) | 125(4.6) | 187(4.9)* | 367(4.5) | 136(5.3) | 250(6.2) | 411(7.7) * | 794(6.7) |
| Respiratory failure |
50(3.2) | 90(3.3) | 128(3.4) | 271(3.3) | 109(4.3) | 196(4.9) | 341(6.4) * | 643(5.4) |
| Chronic obstructive pulmonary disease |
310(20.1) | 598(21.9) | 776(20.4) | 1704(20.9) | 646(25.2) | 909(22.7) | 1396(26.2) | 2931(24.6) |
| Pneumonia | 156(10.1) | 256(9.4) | 327(8.6) | 753(9.2) | 310(12.1) | 484(12.1) | 801(15) * | 1581(13.3) |
| Trauma in past year |
92(6.0) | 149(5.5) | 210(5.5) | 461(5.6) | 173(6.8) | 252(6.3) | 355(6.7) | 770(6.5) |
| Major psychiatric disorders |
42(2.7) | 77(2.8) | 106(2.8) | 227(2.8) | 80(3.1) | 91(2.3) | 168(3.2) | 337(2.8) |
| Depression | 161(10.5) | 249(9.1) | 462(12.2)* | 880(10.8) | 237(9.3) | 321(8) | 564(10.6) * | 1114(9.4) |
TTC: Takotsubo cardiomyopathy
Other race includes Asian, Hispanic, North American Native, or other not specified.
P for trend <0.05
Outcomes
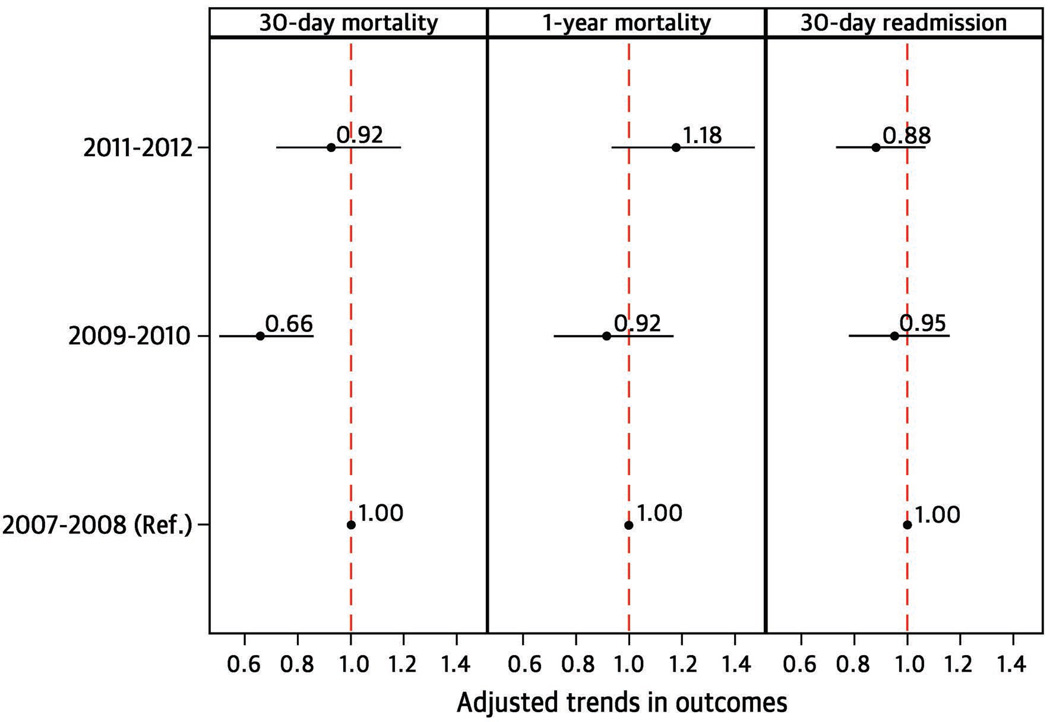
Overall, the in-hospital mortality rate for the principal TTC cohort was 1.3% (95% Confidence interval [CI] 1.1–1.6) and the 30-day mortality rate was 2.5% (95% CI 2.2–2.8). The average LOS was 4±3.3 days. The majority of patients were discharged to home [73.6% (95% CI 72.7–74.6)]. Within 30 days of discharge, 11.6% (10.9–12.3) of patients were rehospitalized. The 1-year mortality was 6.9% (95% CI 6.4–7.5). Outcomes by study year are shown in Table 2. There was a significant decrease over time in the LOS (p<0.001) and the proportion of patients discharged directly to home (p=0.045). In the risk-adjusted model, there was no significant difference in 30-day and 1-year mortality, or in 30-day readmission between 2007–2008 and 2011–2012 (Figure 2).
Table 2.
Outcomes, by 2-year intervals and combined years, for principal and secondary TTC cohort.
| 2007–2008 | 2009–2010 | 2011–2012 | Total | |
|---|---|---|---|---|
| Principal | ||||
| No. of patients | 1540 | 2733 | 3795 | 8068 |
| In-hospital mortality |
1.8(1.2–2.6) | 1.2(0.9–1.7) | 1.1(0.8–1.5) | 1.3(1.1–1.6) |
| 30-day mortality | 3.1(2.3–4.1) | 2.1(1.6–2.7) | 2.6(2.1–3.1) | 2.5(2.2–2.8) |
| 1-year mortality | 6.8(5.6–8.1) | 6.3(5.4–7.3) | 7.4(6.6–8.3) | 6.9(6.4–7.5) |
| Length of stay, days (SD)* |
4.3(3.7) | 4.0(3.2) | 3.8(3.2) | 4(3.3) |
| Discharged home* | 75.3 (73.1–77.5) | 73.9 (72.3–75.6) | 72.7 (71.3–74.1) | 73.6(72.7–74.6) |
| 30-day readmission | 12.2(10.5–13.8) | 11.9(10.7–13.8) | 11.2(10.2–12.2) | 11.6(10.9–12.3) |
| Secondary | ||||
| No. of patients | 2561 | 4009 | 5328 | 11898 |
| In-hospital mortality |
2.5(1.9–3.2) | 3.6(3.1–4.3) | 2.7(2.3–3.2) | 3(2.7–3.3) |
| 30-day mortality | 4.3(3.5–5.2) | 5.2(4.5–5.9) | 4.6(4.1–5.2) | 4.7(4.4–5.1) |
| 1-year mortality | 10.5(9.3–11.7) | 11.3(10.4–12.4) | 11.8(11–12.7) | 11.4(10.8–11.9) |
| Length of stay, days (SD) |
5.9(5.3) | 5.9(5.2) | 5.7(4.8) | 5.8 |
| Discharged home* | 62(60.1–63.9) | 58.7(57.2–60.2) | 57.8(56.5–59.2) | 59(58.1–59.9) |
| 30-day readmission | 16.4(15–18) | 15.8(14.7–17) | 15.3(14.4–16.4) | 15.8(15.1–16.4) |
SD: Standard deviation
TTC: Takotsubo cardiomyopathy
P for trend <0.05
Figure 2.
Risk-adjusted trend in 30-day mortality, 1-year mortality, and 30-day readmission for principal TTC cohort.
The figure is divided vertically into 3 panels (1-year mortality, 30-day mortality, and 30-day readmission). On the vertical axis are the 3 time periods (2007–2008, 2009–2010, 2011–2012, with 2007–2008 serving as reference). Within each panel, the strength of effect is shown along the horizontal axis with the vertical dotted line demarcating an odds ratio (OR) of 1 (i.e., no difference in the risk adjusted outcome compared with 2007–2008); estimates to the right (i.e., >1) are associated with a greater likelihood of the outcome, while those to the left (i.e., <1) indicate a reduced likelihood of the outcome. Each dot represents the point estimate of the effect of that time period in the model, while the line shows the 95% confidence interval (CI).
For the secondary TTC cohort, in-hospital mortality, 30-day mortality, and 1-year mortality were 3% (95% Confidence interval [CI]: 2.7–3.3), 4.7% (95% CI: 4.4–5.1), and 11.4% (95% CI: 10.8–11.9). Within 30 days of discharge, 15.8% (15.1–16.4) of patients were re-hospitalized. There was no significant difference in 30-day and 1-year mortality or 30-day readmission between 2007–2008 and 2011–2012. There was a significant decrease over time in the proportion of patients discharged directly to home (p=0.001) (Table 2).
Outcomes by strata of age, sex, and race are shown in Table 3. In both principal and secondary TTC cohorts, older patients (≥85 years) had higher rates of mortality (in-hospital, 30-day, and 1-year) and readmission, longer LOS, and were more likely to require post-acute care services compared with their counterparts. In the principal TTC cohort, both male and non-white patients had no appreciable difference in short-term mortality compared with their counterparts, but had higher 1-year mortality. In the secondary TTC cohort, male and non-white patients had higher mortality at all 3 time points compared with their counterparts.
Table 3.
Outcomes by sub groups of age, sex, race for principal and secondary TTC cohort, combined years.
| 65–74 | 75–84 | ≥85 | Non-white | White | Female | Male | |
|---|---|---|---|---|---|---|---|
| Principal | |||||||
| No. of patients | 3661 | 3415 | 992 | 595 | 7473 | 7608 | 460 |
| In-hospital mortality |
0.74(0.5–1.1) | 1.5(1.1–2.0) | 2.6(1.7– 3.8)* |
1.7(0.8–3.1) | 1.2(1.0–1.5) | 1.3(1.0–1.6) | 1.7(0.8–3.4) |
| 30-day mortality |
1.7(1.3–2.2) | 2.7(2.2–3.3) | 4.9(3.7– 6.5)* |
2.9(1.7–4.5) | 2.5(2.2–2.9) | 2.5(2.1–2.9) | 3.3(1.8–5.3) |
| 1-year mortality |
5.3(4.6–6.1) | 7(6.2–7.9) | 12.5(10.5– 14.7)* |
8.9(6.7– 11.5) |
6.7(6.2– 7.3)* |
6.6(6.1–7.2) | 12.0(9.1–15.3)* |
| Length of stay, days (SD) |
3.7(3.2) | 4.2(3.4) | 4.5(3.2)* | 4.5(3.8) | 4(3.3)* | 4(3.3) | 4.1(3.5) |
| Discharged home |
83.2(81.9– 84.4) |
69.5(68.0– 71.0) |
52.6(49.5– 55.7)* |
70.6(66.8– 74.1) |
73.9(72.9– 74.9) |
73.7(72.7– 74.6) |
73.3(69.0– 77.1) |
| 30-day readmission |
10.0(9.0–11.0) | 12.5(11.4– 13.6) |
14.4(12.3– 16.8)* |
15.1(12.3– 18.3) |
11.3(10.6– 12.1)* |
11.5(10.8– 12.2) |
13.9(10.8– 17.4) |
| Secondary | |||||||
| No. of patients | 5069 | 5156 | 1673 | 1063 | 10835 | 10893 | 1005 |
| In-hospital mortality |
2.2(1.8–2.7) | 3.3(2.8–3.8) | 4.5(3.5– 5.6)* |
4.6(3.4–6) | 2.8(2.5– 3.2)* |
2.9(2.6–3.2) | 4.4(3.2– 5.8)* |
| 30-day mortality |
3.6(3.1–4.1) | 5.1(4.5–5.7) | 7.7(6.4–9)* | 6.8(5.3–8.5) | 4.6(4.2–5)* | 4.6(4.2–5) | 7.2(5.6– 8.9)* |
| 1-year mortality |
9.6(8.8–10.4) | 11.6(10.7– 12.5) |
16(14.3– 17.9)* |
14.1(12.1– 16.4) |
11.1(10.5– 11.7)* |
10.7(10.1– 11.3) |
18.2(15.9– 20.7)* |
| Length of stay, days (SD) |
5.7(5.6) | 5.9(5.2) | 6(4.7)* | 6.6(6.7) | 5.7(5.1)* | 5.7(5.3) | 6.3(5.9)* |
| Discharged home |
68.3(67–69.5) | 55.6(54.2–57) | 41.7(39.3– 44.1)* |
55.1(52.1– 58.1) |
59.4(58.4– 60.3)* |
59.2(58.3– 60.1) |
57.1(54– 60.2) |
| 30-day readmission |
14.4(13.4– 15.4) |
16.8(15.7– 17.8) |
17.3(15.5– 19.3)* |
18.6(16.2– 21.1) |
15.6(14.9– 16.3)* |
15.9(15.2– 16.6) |
16(13.4– 18.5) |
TTC: Takotsubo cardiomyopathy
SD: Standard deviation
P <0.05
Among the secondary TTC cohort, the top-10 principal diagnoses by 3-digit ICD-9-CM codes were AMI (58.2%), heart failure (4.3%), other disease of the lung (which includes respiratory failure) (4.2%), other forms of chronic ischemic heart disease (3.1%), septicemia (3.0%), cardiac dysrhythmias (2.5%), chronic bronchitis (2.0%), symptoms involving respiratory system and other chest symptoms (1.5%), pneumonia (1.0%), and conduction disorders (0.9%).
In the secondary TTC cohort, a substantial proportion of patients were coded with a principal diagnosis of AMI and it is likely that these patients are similar to those in the principal TTC cohort. Thus, as a sub-analysis of the secondary TTC cohort, we reported outcomes separately for those with a principal diagnosis of AMI and all other principal diagnoses. Patients with principal diagnoses other than AMI had much higher mortality at all 3 time points and higher readmission rates, while those coded as AMI in the principal diagnosis had mortality rates comparable to those in the principal TTC cohort (Table 4).
Table 4.
Outcomes for patients with a secondary diagnosis of TTC with a principal diagnosis of AMI versus all other principal diagnoses, combined years
| AMI | All other principal diagnoses |
|
|---|---|---|
| N | 6925 | 4977 |
| In-hospital mortality* | 1.9(1.6–2.3) | 4.5(3.9–5.0) |
| 30-day mortality* | 3.3(2.9–3.7) | 6.8(6.1–7.5) |
| 1-year mortality* | 8.0(7.4–8.7) | 16.0(15.0–17.0) |
| 30-day readmission* | 13.7(12.8–14.5) | 18.7(17.6–19.8) |
TTC: Takotsubo cardiomyopathy
AMI: Acute myocardial infarction
P <0.05
During the cohort construction, a notable observation was that a substantial proportion of hospitalizations coded for a secondary diagnosis of TTC did not have obstructive CAD excluded by angiography (54%), and over time there was an increasing trend of such coding (from 42.5% in 2007 to 57.7% in 2012, P for trend <0.001). The outcomes for these patients (in-hospital mortality of 7.0% [6.5–7.5], 30-day mortality of 11.9% [11.2–12.5], and 1-year mortality of 24.5% [23.6–25.3]) were much worse than for those in the secondary TTC cohort.
Among hospitalizations coded with a principal diagnosis of TTC, 14.3% did not have obstructive CAD excluded by angiography. The outcomes for these patients were in-hospital mortality of 3.0% [2.7–3.3], 30-day mortality of 4.7% [4.4–5.2], and 1-year mortality of 11.4% [10.8–11.9].
DISCUSSION
To our knowledge, this is the largest nationally representative study of post-discharge outcomes up to 1 year among patients hospitalized with TTC as well as the first to provide information on trends in hospitalizations and outcomes nationwide. We found that among Medicare fee-for-service beneficiaries, hospitalizations for both principal and secondary diagnosis of TTC increased 3-fold from 2007–2012. For the principal TTC cohort, the outcomes were excellent. In-hospital mortality was low, with almost all patients surviving the acute episode. These patients continued to do well after discharge: 1-year mortality rates were low, and only 1 in 10 patients were re-hospitalized within 30-days of discharge. There was no change in outcomes over time. The secondary TTC cohort had worse outcomes compared with the principal cohort. Excluding those who were coded with a principal diagnosis of AMI, the mortality of the remainder of the secondary cohort was nearly 3 times worse than that of the principal cohort. In both the principal and secondary cohorts older, male, and non-white patients had worse outcomes. We also found that a large proportion of patients were being coded with a secondary diagnosis of TTC who did not undergo angiography.
The prevalence of TTC reported in prior studies is approximately 1–2% of all patients presenting with an initial diagnosis of either an acute coronary syndrome or AMI.(2,12) In our study, in 2012, the incidence of principal TTC among Medicare fee-for-service beneficiaries was 7.1 per 100,000 person-years which, when compared with the hospitalization rate for AMI in the same population in 2010–2011 of 816 per 100,000 person-years,(13) is about 0.9%. Adding the patients in the secondary TTC cohort who were coded as AMI for the principal diagnosis field, this proportion rises to 1.6%, which is similar to that observed in the prior case series of TTC.(2,14,15) We found that over the study period, the incidence of TTC steadily increased. This is likely due to both increased recognition of the syndrome and increased recognition of the specific ICD code for TTC, which was introduced in October 2006.(16)
TTC affects postmenopausal women disproportionately,(8,17) for reasons that remain unclear, and 94% of our principal TTC cohort was female. A lower proportion of patients with TTC (46.1%) had a history of atherosclerotic disease compared with that reported for patients hospitalized with AMI (73.4%).(13) In fact, studies of angiographic findings in TTC patients have reported a 40–80% prevalence of CAD.(18,19) Although a lower incidence than in AMI, this is still a substantial burden of CAD and one that would be expected, given that TTC occurs commonly in the elderly. This has important implications for the diagnosis of TTC, emphasizing the frequent co-existence of CAD with TTC and the need for careful assessment of the characteristics and distribution of echocardiographic and angiographic findings for a diagnosis of TTC.
Our method of isolating a cohort with a principal diagnosis of TTC who underwent angiography but did not undergo revascularization therapy provides a high degree of specificity to identify true TTC hospitalizations. Further, this cohort likely represents the classic coronary presentations of TTC in which the outcome is driven largely by TTC instead of a primary acute illness. The other important advantage of this approach is that the secondary diagnosis field in administrative data often represents a prior history of the condition rather that the condition occurring in the same hospitalization. Consequently, it is possible that some hospitalizations with a secondary diagnosis of TTC may in fact represent a prior history of the illness. However, our requirement of angiography without revascularization therapy should help minimize this bias in the secondary TTC cohort.
There is one prior national-level study, using data from the Healthcare Cost and Utilization Project,(20) which examined in-hospital outcomes for TTC. However, this study did not use the additional criteria, such as receipt of cardiac catheterization and the absence of revascularization, used in our study to reliably identify TTC, and thus the outcomes may not be robust. Exclusion of obstructive CAD or acute plaque rupture by angiography is a prerequisite for diagnosing TTC.(2,7) Further, it did not provide long-term outcomes.
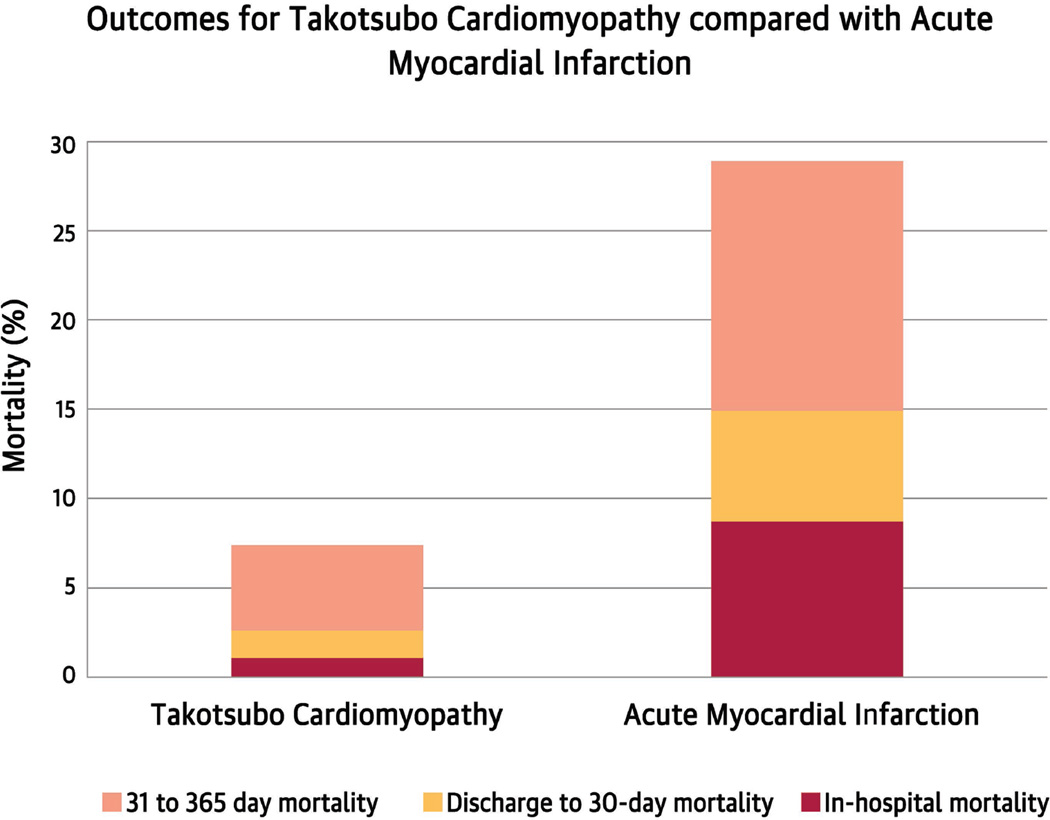
We found outcomes for our principal TTC cohort to be excellent, with almost all patients surviving to discharge. Our observed in-hospital mortality rate of 1.3% in the principal TTC cohort is on the lower end of the entire spectrum of reported rates (0–8%) in case series on TTC.(6,21) In contrast to outcomes for principal TTC in 2011–2012, the in-hospital mortality for AMI in 2010–2011 for the white-female subgroup, which is the demographic for TTC and thus more comparable, was 6 times higher (Figure 1).(13) Further, 3 in 4 patients were discharged directly to home without the need for post-acute care services. These patients continued to do well after discharge, with only 1 in 9 needing to be re-hospitalized within 30 days compared with 1 in 5 who were post-AMI. The long-term outcomes of TTC were excellent; in 2012, only 1 in 15 patients with TTC did not survive to 1 year, compared with 1 in 4 patients with AMI.(13) In summary, although TTC closely mimics AMI, the outcomes are vastly better. Studies show that patients who survive an acute episode of TTC typically recover ventricular function within weeks to months.(5)
Figure 1.
The figure contrasts the outcomes for the principal TTC (Takotsubo cardiomyopathy) cohort with a comparable group of white, female Medicare fee-for-service beneficiaries with acute myocardial infarction. On the x-axis is percentage mortality. On the y-axis are 2 stacked bars, 1 for each condition, showing in-hospital, discharge to 30-day and 31–365 day mortality. Data for Takotsubo cardiomyopathy are for 2011–2012 and data for acute myocardial infarction are for 2010–2011.
The outcomes for the secondary TTC cohort were, expectedly(6), worse compared with those of the principal TTC cohort. An important and surprising finding was that nearly 3 in 5 patients with a secondary diagnosis of TTC were coded as AMI for the principal diagnosis. These patients are either being coded as AMI in the principal diagnosis field incorrectly, or possibly intentionally for billing purposes. These patients are likely clinically similar to the principal TTC cohort, and we found their outcomes to be similar to those of the principal TTC cohort. Future studies of TTC using administrative data may want to account for this observation when defining principal versus secondary TTC. Excluding patients with a principal diagnosis of AMI, 1 in 15 patients of the remainder of the secondary TTC cohort did not survive the hospitalization and 1 in 6 did not survive to 1 year. However, this is lower than the in-hospital mortality reported in prior studies for TTC secondary to acute medical conditions (10%).(6) Respiratory conditions such as respiratory failure, bronchitis, and pneumonia, and sepsis were the most common acute conditions among secondary TTC patients.
Older patients were at higher risk for adverse outcomes in both principal and secondary TTC cohorts, as were non-white and male patients, which warrants further study and increased attention to these sub-groups of TTC. There is some evidence that males presenting with TTC tend to have higher disease acuity,(22,23) and a previous meta-analysis has shown that they may be at higher risk of mortality. Our study using nationally representative data corroborates this observation. Further, we observed that over the study period, there was no change in outcomes for TTC. The optimal medical regimen for TTC is not defined and there are no controlled data available. The management is largely supportive and patients are usually treated with standard medications for left ventricular systolic dysfunction.
Limitations
Our study has several limitations. First, we studied Medicare fee-for-service beneficiaries, which limits the generalizability of the findings to younger populations. Nevertheless, TTC usually affects the elderly, a population captured in our cohort. Second, we relied on ICD-9-CM codes to identify TTC. To our knowledge, there are no validation studies for this ICD code (429.83). However, the code has good face validity as the code description reads ‘takotsubo syndrome’ and is unlikely to be coded incorrectly. To improve the specificity of TTC, we limited the study cohort to those who underwent cardiac catheterization only. This method has been used previously.(8) Third, it is possible that cases of TTC may have been coded incorrectly as only AMI and we may underestimate the incidence of TTC. On the other hand, cases with true acute coronary syndromes but minimal angiographic findings, which were unrecognized by the physicians, may lead to over-coding of TTC. Fourth, there may be patients in the secondary TTC cohort in whom the secondary diagnosis of TTC may represent a prior history of the condition rather that the condition occurring in the same hospitalization.
CONCLUSIONS
Among Medicare fee-for-service beneficiaries, hospitalization rates for TTC are increasing over time. Although the syndrome mimics AMI at presentation, we found short- and long-term outcomes of principal TTC to be excellent compared with those for AMI, with nearly all TTC patients surviving to discharge and 14 in 15 surviving to 1 year. Patients with secondary TTC had worse outcomes, likely driven by their primary acute medical condition. Older, male, and non-white subgroups were more vulnerable for adverse outcomes after TTC.
PERSPECTIVES.
Competency in Medical Knowledge
Hospitalization rates for Takotsubo cardiomyopathy (TTC) are increasing in the United States. This condition predominantly affects women, of white race. Short- and long-term outcomes of primary TTC are excellent, with 14 in 15 patients surviving to 1 year. Outcomes for TTC secondary to other medical conditions are worse and 8 in 9 survive to 1 year. Older, male, and non-white patients have worse outcomes.
Competency in Patient Care
Although frequently precipitated by an episode of stress, short- and long-term outcomes for principal TTC are excellent. Making patients aware of their good prognosis is important to avoid further stress from the illness. Outcomes for secondary TTC are worse and largely driven by the primary acute medical condition.
Translational Outlook
Further study is required to elucidate why male and non-white patients have comparatively poorer outcomes than their counterparts.
Acknowledgments
FUNDING: This project was supported by grant 1U01 HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute.
Abbreviations and Acronyms
- AMI
Acute myocardial infarction
- CAD
Coronary artery disease
- CI
Confidence interval
- CMS
Centers for Medicare & Medicaid Services
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- LOS
Length of stay
- SD
Standard deviation
- TTC
Takotsubo cardiomyopathy
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES: Dr. Krumholz is the recipient of research agreements from Medtronic and from Johnson & Johnson (Janssen), through Yale University, to develop methods of clinical trial data sharing and is chair of a cardiac scientific advisory board for UnitedHealth. The other authors report no conflicts of interest.
REFERENCES
- 1.Akashi YJ, Nef HM, Lyon AR. Epidemiology and pathophysiology of Takotsubo syndrome. Nat Rev Cardiol. 2015;12:387–397. doi: 10.1038/nrcardio.2015.39. [DOI] [PubMed] [Google Scholar]
- 2.Prasad A, Lerman A, Rihal CS. Apical ballooning syndrome (Tako-Tsubo or stress cardiomyopathy): A mimic of acute myocardial infarction. Am Heart J. 2008;155:408–417. doi: 10.1016/j.ahj.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Eitel I, von Knobelsdorff-Brenkenhoff F, Bernhardt P, et al. Clinical characteristics and cardiovascular magnetic resonance findings in stress (takotsubo) cardiomyopathy. JAMA. 2011;306:277–286. doi: 10.1001/jama.2011.992. [DOI] [PubMed] [Google Scholar]
- 4.Singh NK, Rumman S, Mikell FL, Nallamothu N, Rangaswamy C. Stress cardiomyopathy: Clinical and ventriculographic characteristics in 107 North American subjects. Int J Cardiol. 2010;141:297–303. doi: 10.1016/j.ijcard.2008.12.043. [DOI] [PubMed] [Google Scholar]
- 5.Sharkey SW, Windenburg DC, Lesser JR, et al. Natural history and expansive clinical profile of stress (tako-tsubo) cardiomyopathy. J Am Coll Cardiol. 2010;55:333–341. doi: 10.1016/j.jacc.2009.08.057. [DOI] [PubMed] [Google Scholar]
- 6.Singh K, Carson K, Shah R, et al. Meta-analysis of clinical correlates of acute mortality in takotsubo cardiomyopathy. Am J Cardiol. 2014;113:1420–1428. doi: 10.1016/j.amjcard.2014.01.419. [DOI] [PubMed] [Google Scholar]
- 7.Parodi G, Citro R, Bellandi B, Provenza G, Marrani M, Bossone E. Revised clinical diagnostic criteria for Tako-tsubo syndrome: the Tako-tsubo Italian Network proposal. Int J Cardiol. 2014;172:282–283. doi: 10.1016/j.ijcard.2013.12.239. [DOI] [PubMed] [Google Scholar]
- 8.Deshmukh A, Kumar G, Pant S, Rihal C, Murugiah K, Mehta JL. Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J. 2012;164:66–71. doi: 10.1016/j.ahj.2012.03.020. e1. [DOI] [PubMed] [Google Scholar]
- 9.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113:1693–1701. doi: 10.1161/CIRCULATIONAHA.105.611194. [DOI] [PubMed] [Google Scholar]
- 10.Krumholz HM, Wang Y, Mattera JA, et al. An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113:1683–1692. doi: 10.1161/CIRCULATIONAHA.105.611186. [DOI] [PubMed] [Google Scholar]
- 11.Bratzler DW, Normand SL, Wang Y, et al. An administrative claims model for profiling hospital 30-day mortality rates for pneumonia patients. PLoS One. 2011;6:e17401. doi: 10.1371/journal.pone.0017401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gianni M, Dentali F, Grandi AM, Sumner G, Hiralal R, Lonn E. Apical ballooning syndrome or takotsubo cardiomyopathy: a systematic review. Eur Heart J. 2006;27:1523–1529. doi: 10.1093/eurheartj/ehl032. [DOI] [PubMed] [Google Scholar]
- 13.Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999–2011. Circulation. 2014;130:966–975. doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akashi YJ, Goldstein DS, Barbaro G, Ueyama T. Takotsubo cardiomyopathy: a new form of acute, reversible heart failure. Circulation. 2008;118:2754–2762. doi: 10.1161/CIRCULATIONAHA.108.767012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kurowski V, Kaiser A, von Hof K, et al. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132:809–816. doi: 10.1378/chest.07-0608. [DOI] [PubMed] [Google Scholar]
- 16. [Accessed September 11, 2015];ICD-9-CM Coordination and Maintenance Committee Meeting. http://www.cdc.gov/nchs/data/icd/agendasept05.pdf. September 30, 2005.
- 17.Singh K, Carson K, Usmani Z, Sawhney G, Shah R, Horowitz J. Systematic review and meta-analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int J Cardiol. 2014;174:696–701. doi: 10.1016/j.ijcard.2014.04.221. [DOI] [PubMed] [Google Scholar]
- 18.Prasad A, Dangas G, Srinivasan M, et al. Incidence and angiographic characteristics of patients with apical ballooning syndrome (takotsubo/stress cardiomyopathy) in the HORIZONS-AMI trial: an analysis from a multicenter, international study of ST-elevation myocardial infarction. Catheter Cardiovasc Interv. 2014;83:343–348. doi: 10.1002/ccd.23441. [DOI] [PubMed] [Google Scholar]
- 19.Hoyt J, Lerman A, Lennon RJ, Rihal CS, Prasad A. Left anterior descending artery length and coronary atherosclerosis in apical ballooning syndrome (Takotsubo/stress induced cardiomyopathy) Int J Cardiol. 2010;145:112–115. doi: 10.1016/j.ijcard.2009.06.018. [DOI] [PubMed] [Google Scholar]
- 20.Brinjikji W, El-Sayed AM, Salka S. In-hospital mortality among patients with takotsubo cardiomyopathy: a study of the National Inpatient Sample 2008 to 2009. Am Heart J. 2012;164:215–221. doi: 10.1016/j.ahj.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 21.Redfors B, Vedad R, Angeras O, et al. Mortality in takotsubo syndrome is similar to mortality in myocardial infarction - A report from the SWEDEHEART registry. Int J Cardiol. 2015;185:282–289. doi: 10.1016/j.ijcard.2015.03.162. [DOI] [PubMed] [Google Scholar]
- 22.Patel SM, Chokka RG, Prasad K, Prasad A. Distinctive clinical characteristics according to age and gender in apical ballooning syndrome (takotsubo/stress cardiomyopathy): an analysis focusing on men and young women. J Card Fail. 2013;19:306–310. doi: 10.1016/j.cardfail.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 23.Schneider B, Athanasiadis A, Stollberger C, et al. Gender differences in the manifestation of tako-tsubo cardiomyopathy. Int J Cardiol. 2013;166:584–588. doi: 10.1016/j.ijcard.2011.11.027. [DOI] [PubMed] [Google Scholar]