Abstract
This prospective study assessed whether gender differences in health insurance help explain gender differences in delay in seeking care for US patients with acute myocardial infarction (AMI). We also assessed gender differences in such prehospital delay for AMI in Spain, a country with universal insurance. We used data from 2,951 US and 496 Spanish patients aged 18–55 years with AMI. US patients were grouped by insurance status: adequately insured, underinsured, or uninsured. For each country, we assessed the association between gender and prehospital delay (symptom onset to hospital arrival). For the US cohort, we modeled the relationship between insurance groups and delay of >12 hours. US women were less likely than men to be uninsured, but more likely to be underinsured and a larger proportion of women than men experienced delays of >12 hours (38% versus 29%). We found no association between insurance status and delays of >12 hours in men or women. Only 17.3% of Spanish patients had delays of >12 hours and there were no significant gender differences. In conclusion, women were more likely than men to delay, though it was not explained by differences in insurance status. The lack of gender differences in prehospital delays in Spain suggests that these differences may vary by health care system and culture.
Keywords: Prehospital delay, acute myocardial infarction, health insurance, multinational study
Introduction
Prehospital delays in seeking medical care for acute myocardial infarction (AMI) are vastly longer among women compared with men.1,2 Such delays are harmful and increase the risk of mortality.3,4 However, the causes of the gender difference in delays are unknown. Inadequate health insurance is a known barrier to timely care seeking.2,5 Adults with lower income, those covered by Medicaid, and the uninsured all delay seeking care for emergencies compared with those with private insurance.1,2 This relationship has been established in mostly elderly cohorts.2 However, unlike the elderly who are nearly universally covered (i.e., Medicare), a large portion of younger adults are uninsured or underinsured,6 especially women.7,8 While the Affordable Care Act aims to increase access,7 it is unknown if adequate insurance affects care seeking for AMI, and whether similar levels of delay exist in countries with national insurance. Accordingly, we sought to assess whether gender differences in insurance contribute to gender differences in prehospital delay among young patients with AMI. We used data from VIRGO (Variation in Recovery: Role of Gender on Outcomes in Young AMI Patients), a prospective study of adults aged 18–55 with AMI in the US and Spain.9 We aimed to (1) compare the extent of prehospital delay among young US women and men; (2) compare health insurance adequacy among young US women and men with AMI; and (3) assess whether gender differences in prehospital delay are mediated by gender disparities in insurance in the US. Since VIRGO included patients from Spain, a country with a national insurance system that does not require payment from the patient, we secondarily analyzed data from the Spanish cohort to examine gender differences in prehospital delay there.
Methods
We used data from patients, age 18–55 years, in the US and Spain who were enrolled in VIRGO.9 US patients were enrolled between August 2008 and January 2012 from 108 hospitals at geographically diverse sites; Spanish patients were enrolled between April 2009 and December 2011 from 24 hospitals. Designed to focus on women, VIRGO enrolled consecutive women and every other man to achieve a 2:1 gender ratio (3,572 in total, and 516 in Spain). Detailed eligibility and exclusion criteria for VIRGO were previously published.9 We further excluded those with unknown prehospital delay times (32 in the US and 19 in Spain) or insurance status (2 in the US and 1 in Spain) to create a final study cohort of 2,951 patients in the US and 496 in Spain. Institutional Review Board approval was obtained at each participating institution and patients provided informed consent for their study participation including interviews during initial hospitalization.
The dependent variable was prehospital delay, defined as the time between symptom onset and presentation to the first hospital. The time of symptom onset was obtained as part of the structured interview; the time of arrival at the emergency department of the first hospital was obtained via abstraction of medical records. Prehospital delay >6 hours was confirmed by 2 VIRGO investigators at Yale for patients lacking exact symptom onset information. Consistent with previous research, we combined the continuous prehospital delay time (symptom onset to arrival at the first hospital) and dichotomized prehospital delay (<6 hours, >6 hours) to clinically relevant categories: ≤2, >2 to 6, >6 to 12, and >12 hours.2,10 Patients who had continuous prehospital delay times available were categorized based on the calculated time. For patients who only had dichotomized prehospital delay time (<6 hours, >6 hours), those with a prehospital delay within 6 hours were categorized as >2 to 6 hours. Patients with a prehospital delay >6 hours were categorized as >6 to 12 hours. To examine prehospital delays <12 hours and >12 hours, the <2, >2 to 6, and >6 to 12 were combined to create the <12 hours category.
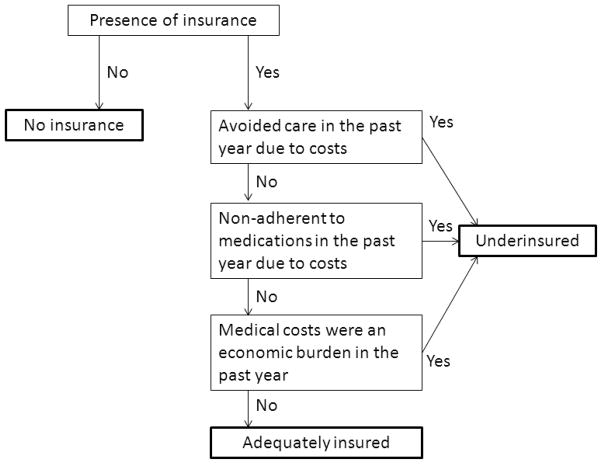
The main independent variables were health insurance status and gender. Participants were divided into 3 groups according to health insurance information obtained during the interview during the initial hospitalization: (1) adequately insured, (2) underinsured, and (3) not insured. We stratified patients with insurance into those who were underinsured and adequately insured based on questions assessing financial barriers to care. Patients were underinsured if in the past year they reported any of the following: avoidance of care or non-adherence to medications due to costs, or perceived medical costs to be an economic burden (Appendix). Additional variables known to be associated with prehospital delay11 were gathered through structured interviews and medical record review during the initial hospitalization. These included socio-demographic characteristics (age, gender, race, marital, education and employment status) and social support, as assessed by the 7-item Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Social Support Inventory (ESSI-7).12 Perceived stress level was assessed by the 14-item Perceived Stress Scale (PSS-14).13,14 Pertinent medical history collected included depression, diabetes, renal dysfunction, obesity; and cardiac risk factors such as family history, smoking, alcohol abuse, and recreational drug use. Clinical characteristics of AMI admission included Killip class on arrival (classified as class I versus class II–IV), absence of chest pain, and arrival to the hospital within regular work hours (weekday, non-night-time admission).
We examined the associations between gender and insurance groups (not insured, underinsured and adequately insured); between gender and patient characteristics/prehospital delay; and between insurance groups and patient characteristics/prehospital delay in the US separately using the Chi-squared test for categorical variables and F-test or the median score test for continuous variables. Heterogeneity of the effects of gender on prehospital delay across insurance groups was tested using the Cochran–Mantel–Haenszel test.
We used hierarchical logistic models to account for the clustering effects at the site level and made sequential adjustments for patient characteristics. Separate hierarchical logistic models were used to evaluate the independent effect of the 3 insurance groups on prehospital delay of >12 hours and the independent effect of gender on pre-hospital delay of >12 hours, sequentially adjusting for site clustering, socio-demographics, medical history, and clinical characteristics on admission (Killip class, absence of chest pain, and arrival to the hospital within regular work hours). We also assessed interaction between gender and insurance groups using these models. Missing data were <1% except for Killip class (1.3%), ejection fraction (2.9%), number of dependents (4.0%), PSS-14 (6.2%) and ESSI (2.1%). For the multivariable model analyses, we imputed the missing values to the most common category for categorical variables and median value for the continuous variables, and to 4 dummy indicators representing the missing values of the 5 variables mentioned above. Identical categories of delay were used for the Spanish cohort. Whether gender differences existed in the Spanish cohort in prehospital delay of >12 hours was examined using the Chi-squared test.
For all comparisons, we considered a p-value <0.05 to be statistically significant. All analyses were performed using SAS 9.3 (SAS institute Inc., Cary, NC).
Results
The study population in the US included 2,951 patients with AMI (67% women) with a median age of 48 years (IQR=44, 52). Table 1 lists the differences in demographics and socioeconomic characteristics and medical comorbidities among women and men in our cohort.
Table 1.
Patient Characteristics by Gender
| Women n = 1987 |
Men n = 964 |
P | |
|---|---|---|---|
| Demographics/Socioeconomic Characteristics | |||
| Age, median (IQR) (Years) | 48 (44, 52) | 48 (44, 52) | |
| Race | <0.001 | ||
| Black | 21% | 11% | |
| White | 73 | 82% | |
| Other | 6% | 7% | |
| Has health insurance | 78% | 75% | <0.05 |
| Insurance payer | <0.001 | ||
| Private health insurance (commercial/PPO, HMO) | 50% | 58% | |
| Medicare | 8% | 6% | |
| Medicaid | 11% | 4% | |
| Veterans Affairs | <1 % | 1% | |
| Other | 9% | 6% | |
| Insurance status | <0.001 | ||
| Adequately insured | 37% | 42% | |
| Underinsured | 41% | 33% | |
| Not insured | 22% | 25% | |
| Number of dependents, median | 2 | 3 | <0.001 |
| Marital status | <0.001 | ||
| With partner | 52% | 62% | |
| Without partner | 47% | 37% | |
| Other | 1% | <1% | |
| Education status | 0.75 | ||
| Unknown | <1% | <1% | |
| < high school | 2% | 2% | |
| Some high school | 41% | 41% | |
| > high school | 56% | 56% | |
| Employment status | <0.001 | ||
| Working full-time | 43% | 65% | |
| Working part-time | 13% | 7% | |
| Not working | 44% | 28% | |
| Depression diagnosis prior to AMI | 49% | 24% | <0.001 |
| Major psychiatric disorder | 6% | 2% | <0.001 |
| Perceived stress level by PSS-14, median | 27 | 24 | <0.001 |
| Low social support by ESSI-7, median | 27 | 28 | 0.05 |
|
| |||
| Chronic obstructive pulmonary disease | 14% | 6% | <0.001 |
| Diabetes mellitus | 40% | 27% | <0.001 |
| Renal dysfunction | 13% | 9% | <0.01 |
| Dyslipidemia | 66% | 72% | <0.01 |
| Hypertension | 67% | 65% | 0.18 |
| Prior peripheral artery disease | 3% | 2% | 0.57 |
| Prior angina/stable CAD | 28% | 26% | 0.36 |
| Family history of CAD | 74% | 73% | 0.75 |
| Prior cardiac catheterization | 23% | 22% | 0.53 |
| Congestive heart failure | 6% | 3% | <0.001 |
| Sleep apnea | 5% | 6% | 0.44 |
| Alcohol abuse | 5% | 11% | <0.001 |
| Smoked within last 30 days | 58% | 56% | 0.46 |
| Cocaine use | 5% | 5% | 0.94 |
| Illicit drug use | 8% | 9% | 0.81 |
| Body mass index, median | 31 | 30 | <0.001 |
|
| |||
| Clinical characteristics at AMI admission | |||
| ST-segment elevation | 46% | 58% | <0.001 |
| Ejection fraction <40% | 11% | 11% | 0.49 |
| Killip class at arrival | <0.01 | ||
| I | 90% | 92% | |
| II or III or IV | 5% | 2% | |
| Unknown | 5% | 5% | |
| No chest pain, | 5% | 6% | 0.31 |
| Arrival to hospital within regular work hours | 36% | 33% | 0.20 |
IQR = interquartile range
PPO = preferred provider organization
HMO = health maintenance organization
PSS-14 = 14-item Perceived Stress Scale
ESSI-7 = 7-item Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD)
Social Support Inventory
CAD = coronary artery disease
AMI = acute myocardial infraction
Insurance status among the US patient cohort was highly variable: 1,141 (39%) were adequately insured; 1,132 (38%) were underinsured; and 678 (23%) were uninsured. Among the underinsured, 46% qualified as underinsurance because of avoidance of medical care in the past year due to costs; 49% from medication non-adherence in the past year due to costs; and 84% from feeling that medical costs were an economic burden in the past year. While men had higher rates of being uninsured (25% vs. 22%), more women were underinsured (41% vs. 33%, p<0.001) or covered by Medicaid (11% vs. 4%, p<0.001).
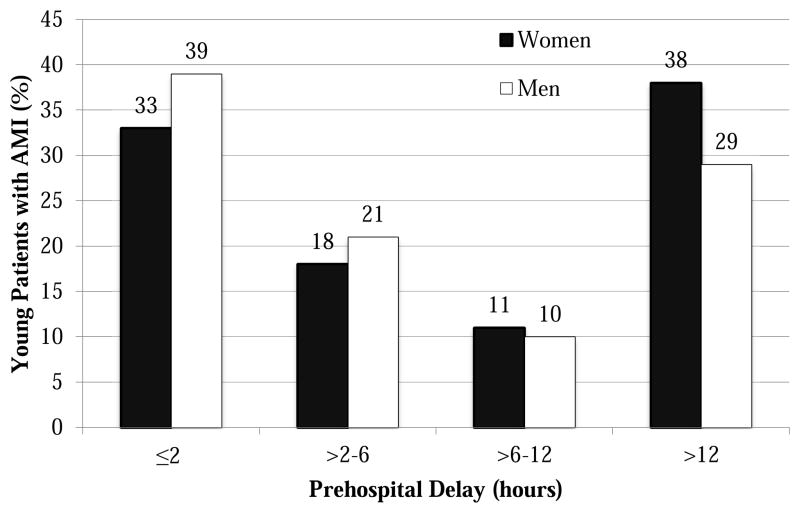
A substantial portion of the US cohort experienced clinically significant prehospital delays: 35% presented within 2 hours of symptom onset; 20%, between 2 to 6 hours; 10%, between 6 to 12 hours; and 35% presented >12 hours after symptom onset. US women were more likely than men to experience delays of >12 hours (Figure 1, p<0.001). This gender disparity persisted after sequential adjustment for socio-demographic factors, medical history and clinical characteristics on admission (OR=1.3; 95% CI: 1.1, 1.6).
Figure 1. Prehospital Delay among Women and Men in the US Cohort.
Test for difference between women and men on prehospital delay: P < 0.0001
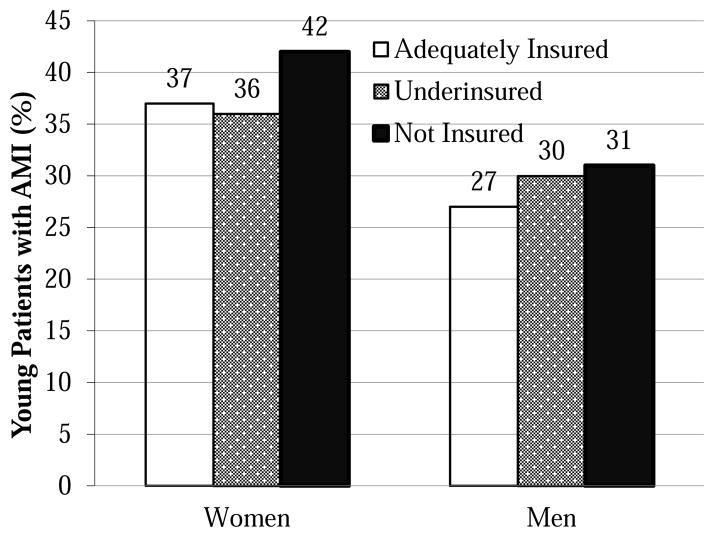
We found no significant association between prehospital delays >12 hours and insurance status (34% of the adequately insured, 34% underinsured and 38% uninsured had >12 hours of delays; p=0.17) or between delays of any length and insurance status (p=0.30). Women in all insurance categories had higher rates of >12 hour prehospital delay compared with men (Figure 2, p=0.12). We also did not find any significant interaction between gender and insurance status on prehospital delay (p=0.30).
Figure 2. Prehospital Delay of >12 Hours in Women and Men of Different Insurance Status among US Cohort.
Test for difference among insurance groups on prehospital delay >12 hours: P = 0.17. Test for interaction between gender and insurance groups on prehospital delay of >12 hours: P = 0.12
We also found no independent association between inadequate insurance and prehospital delay: the odds of having >12 hours of delay among underinsured and uninsured patients compared with those adequately insured showed no significant difference even after adjusting for socio-demographics, medical history and clinical characteristics on admission (Table 2).
Table 2. Independent Effect of Insurance Status on Prehospital Delay > 12 hours.
(Reference: adequately insured)
| Underinsured OR (95% CI) |
Not Insured OR (95% CI) |
|
|---|---|---|
| Unadjusted | 1.01 (0.85, 1.21) | 1.12 (0.92, 1.38) |
| Adjusted for Demographics | 0.98 (0.82, 1.18) | 1.11 (0.90, 1.38) |
| Adjusted for Demographics and Medical History | 0.98 (0.81, 1.18) | 1.10 (0.88, 1.38) |
| Adjusted for Demographics, Medical History, and Clinical Characteristics on Admission | 0.99 (0.81, 1.19) | 1.11 (0.88, 1.39) |
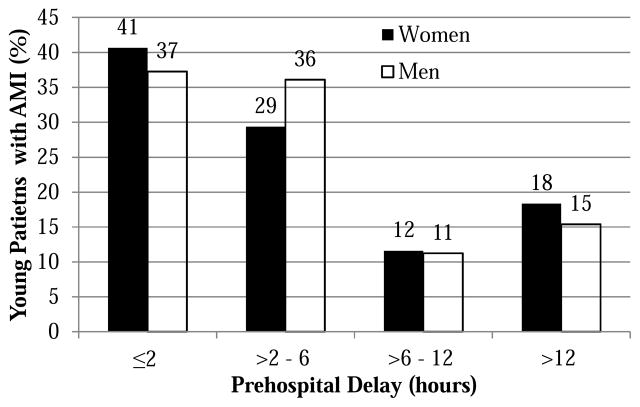
The Spanish cohort (n= 496, 66% female) did not have significant gender differences in prehospital delays of >12 hours (Figure 3, p=0.4;). Both men and women had lower rates of >12 hours of prehospital delay compared with to US patients (Figures 1 and 3).
Figure 3. Prehospital Delay among Young Women and Men among the Spanish Cohort.
Test for difference between male and female on prehospital delay: P = 0.47
Discussion
Among young US patients with AMI, we found that a large portion arrived at hospitals >12 hours after symptom onset. Young women had a higher risk for experiencing such delays. But while women had a higher rate of underinsurance compared with men, differences in insurance did not explain the gender differences in prehospital delay. In contrast, our secondary analysis of prehospital delay in Spain showed a lower rate of >12 hours of delay in both women and men compared with the US, and showed no gender differences in delays.
This study extends prior literature in AMI presentation delays in several ways. First, while a previous study showed that being uninsured or underinsured were each associated with delays in seeking emergency care for AMI,2 it and other studies were based on cohorts that were exclusively or predominantly elderly.1,15–17 The young population in the US, however, is unique because of its diversity in insurance types and perceptions about financial barriers to care, especially before the enactment of the Affordable Care Act, which our study has captured. Our findings did not support the hypothesis that insurance is chiefly responsible for why young women delay more when seeking care.
Second, there is also added value in examining patients’ perception of insurance adequacy. Although the provision of emergency care in the US is guaranteed, the financing of such care for individual patients is not.18 This gap between service and payment could cause those not insured or underinsured to delay seeking care for AMI.2 To assess whether feelings of underinsurance may be a barrier to seek emergency care requires patient interview data. We were able to take advantage of the diverse range of data in VIRGO, which includes interviews that captured patients’ feeling of underinsurance with questions that were well established in assessing financial barriers in care-seeking.19 And while prior studies have noted gender to be a risk factor in patient delays,4 our results show that achieving gender equity in delays would be insufficient, because long delays for both genders were extremely common in the US. Lastly, previous studies of prehospital delay have mostly focused on a single nation.20,21 Our study in 2 countries using the same methodology takes advantage of the multinational nature of VIRGO to demonstrate that not all countries share the same degree of public health challenge in care-seeking delays. Whether the shorter and more gender-equal patient delay in Spain is at all due to universal health insurance or other influences is outside the scope of this study.
Consistent with previous studies,5,22 our results show that young women have an increased risk of inadequate health insurance and coverage by Medicaid. Young women are traditionally more prone to underinsurance because of greater health care use and lower income.23 However, we found no evidence that gender differences in health insurance coverage accounted for the observed gender disparity in prehospital delay.
There are several potential reasons why insurance status was not independently associated with presentation delays in women or men. It may simply be that health insurance is not a factor in the decision-making of young AMI patients seeking emergency care or that only a sub-group of patients consider their insurance status when making such a decision. For example, one study suggested that black women, compared with white women, may be more sensitive to insurance status in the decision to present promptly.24 Another possibility is that the economic costs associated with care-seeking include not only payment for treatment, but also transportation expenses and opportunity costs with forgone competing responsibilities e.g., childcare, work, which may not be adequately offset by having health insurance or the financial means to pay for treatment. Finally, because our study was limited to patients who presented to the hospital, we cannot assess the role of perceived insurance adequacy on delays for patients who did not seek hospital care for their symptoms.
The reasons that women have a 30% higher odds of having substantial delays remain unclear. Other studies have suggested that differences in symptoms or lower risk awareness cause women to delay seeking care.25 Our results from Spain, however, cast some doubt on the extent to which awareness or risk perception could account for the increased delays observed among women in the US, since there is no evidence to suggest that women in Spain experience a different set of symptoms or are much better informed. Furthermore, since Spain has a lower prevalence of AMI than the US,26 one would have expected young women in Spain to be less concerned about having an AMI thus potentially presenting later. Yet not only was the gender difference in prehospital delay not present, both women and men delayed less in Spain. The overall shorter delays may be due to higher population density, an increased culture of seeking care, or a variety of other factors, but they do show the possibility of having gender equity in prehospital delay and prompt presentation. Thus, while we have yet to identify the key components in patient presentation decision-making, our findings from Spain support the downplaying of patient awareness, towards which educational interventions have yet to yield encouraging results.10,27
Our study has several important policy implications. Among US patients, even those adequately insured have high rates of >12 hours of prehospital delay. Thus, adequate health insurance appears to be insufficient in preventing severe prehospital delay for young patients with AMI. Our results underscore the importance of recognizing the limitations of health insurance on affecting patient outcomes. However, it is also important to note that patients may have different responses to health insurance when affected by different acute illnesses; for example, the provision of insurance has been shown to be associated with shorter presentation delays for appendicitis.28 Furthermore, while care-seeking behavior for AMI does not appear to be affected by insurance status, the provision of insurance may nonetheless impact long-term outcomes via other mediators such as the decision to seek routine and follow-up care.29
This study has several limitations. First, VIRGO was designed as an interview-based study focused on patient perspectives, requiring that patients to consent to participate. Consequently, the VIRGO cohort did not capture those who choose not or could not consent, those who died before 48 hours of hospitalization, or those who failed to present. Second, our definition of prehospital delay included transportation time, thus our results would have been affected by population density, the mode of transportation available, and the local emergency medical response systems. However, transportation time alone cannot account for severe delays of >12 hours and past studies based on patients of all age groups with AMI have documented that treatment is most often delayed due to patients not seeking care promptly,27,30 instead of transport. Third, by using patient interviews to determine the time of symptom onset, our study may have been subject to recall bias. However, such bias is unlikely to be specific to a gender or insurance group, and patient interviews nonetheless represent a more precise data source relative to other sources such as medical records.17 Fourth, we were unable to assess insurance sufficiency by objective standards (e.g., healthcare expenditures as a proportion of household income). However, patients’ self-perceived insurance adequacy and financial barriers may exert more influence than objective measures of insurance insufficiency on their care-seeking decision.
Supplementary Material
Acknowledgments
The VIRGO study was supported by grant 5 R01 HL081153 from the National Heart, Lung, and Blood Institute. IMJOVEN was supported in Spain by a grant from the Fondo de Investigaciones Sanitarias del Instituto Carlos III (PI 081614), Ministry of Science and Technology, and additional funds from the Centro Nacional de Investigaciones Cardiovasculares (CNIC). Dr. Krumholz is supported by grant U01 HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute.
Appendix. Classification of insurance groups
Figure 4.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ting HH, Bradley EH, Wang Y, Lichtman JH, Nallamothu BK, Sullivan MD, Gersh BJ, Roger VL, Curtis JP, Krumholz HM. Factors associated with longer time from symptom onset to hospital presentation for patients with ST-elevation myocardial infarction. Arch Intern Med. 2008;168:959–968. doi: 10.1001/archinte.168.9.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smolderen KG, Spertus JA, Nallamothu BK, Krumholz HM, Tang F, Ross JS, Ting HH, Alexander KP, Rathore SS, Chan PS. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA. 2010;303:1392–1400. doi: 10.1001/jama.2010.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, Peterson ED, Blaney M, Frederick PD, Krumholz HM. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47:2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 4.Ting HH, Bradley EH, Wang Y, Nallamothu BK, Gersh BJ, Roger VL, Lichtman JH, Curtis JP, Krumholz HM. Delay in presentation and reperfusion therapy in ST-elevation myocardial infarction. Am J Med. 2008;121:316–323. doi: 10.1016/j.amjmed.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. Health insurance and mortality in US adults. Am J Public Health. 2009;99:2289–2295. doi: 10.2105/AJPH.2008.157685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schoen C, Hayes SL, Collins SR, Lippa JA, Radley DC. [Accessed May, 2014];America’s underinsured: a state-by-state look at health insurance affordability prior to the new coverage expansions. http://www.commonwealthfund.org/~/media/Files/Publications/FundReport/2014/Mar/1736_Schoen_americas_underinsured.pdf Published March, 2014.
- 7.Kaiser Family Foundation. [Accessed May, 2014];Health reform: implications for women’s access to coverage and care. https://kaiserfamilyfoundation.files.wordpress.com/2012/03/7987-03-health-reform-implications-for-women_s-access-to-coverage-and-care.pdf Published August, 2013.
- 8.Rustgi SD, Doty MM, Collins SR. [Accessed August, 2014];Women at risk: why many women are forgoing needed health care. http://www.commonwealthfund.org/publications/issue-briefs/2011/may/women-at-risk. Published May, 2009. [PubMed]
- 9.Lichtman JH, Lorenze NP, D’Onofrio G, Spertus JA, Lindau ST, Morgan TM, Herrin J, Bueno H, Mattera JA, Ridker PM, Krumholz HM. Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients (VIRGO) study design. Circ Cardiovasc Qual Outcomes. 2010;3:684–693. doi: 10.1161/CIRCOUTCOMES.109.928713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. Decade-long trends and factors associated with time to hospital presentation in patients with acute myocardial infarction: the Worcester Heart Attack study. Arch Intern Med. 2000;160:3217–3223. doi: 10.1001/archinte.160.21.3217. [DOI] [PubMed] [Google Scholar]
- 11.Moser DK, Kimble LP, Alberts MJ, Alonozo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Korthari RU, Mensah GA, Morris DL, Pancioli AM, Riegel B, Zerwic JJ. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on cardiovascular nursing and stroke council. Circulation. 2006;114:168–182. doi: 10.1161/CIRCULATIONAHA.106.176040. [DOI] [PubMed] [Google Scholar]
- 12.The ENRICHD investigators. Enhancing recovery in coronary heart disease patients (ENRICHD): study design and methods. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 13.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 14.Otte C, McCaffery J, Ali S, Whooley MA. Association of a serotonin transporter polymorphism (5-HTTLPR) with depression, perceived stress, and norepinephrine in patients with coronary disease: the Heart and Soul Study. Am J Psychiatry. 2007;164:1379–1384. doi: 10.1176/appi.ajp.2007.06101617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ting HH, Chen AY, Roe MT, Chan PS, Spertus JA, Nallamothu BK, Sullivan MD, DeLong ER, Bradley EH, Krumholz HM, Peterson Ed. Delay from symptom onset to hospital presentation for patients with non- ST-segment elevation myocardial infarction. Arch Intern Med. 2010;170:1834–1841. doi: 10.1001/archinternmed.2010.385. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen HL, Gore JM, Saczynski JS, Yarzebski J, Reed G, Spencer FDA, Goldberg RJ. Age and sex differences and 20-year trends (1986 to 2005) in prehospital delay in patients hospitalized with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2010;3:590–598. doi: 10.1161/CIRCOUTCOMES.110.957878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen HL, Saczynski JS, Gore JM, Goldberg RJ. Age and sex differences in duration of prehospital delay in patients with acute myocardial infarction a systematic review. Circ Cardiovasc Qual Outcomes. 2001;3:82–92. doi: 10.1161/CIRCOUTCOMES.109.884361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emergency Medical Treatment and Labor Act, 42 U.S.C. §1395dd(1986).
- 19.Spertus J, Decker C, Woodman C, House J, Jones P, O’Keefe J, Borkon AM. Effect of difficulty affording health care on health status after coronary revascularization. Circulation. 2005;111:2572–2578. doi: 10.1161/CIRCULATIONAHA.104.474775. [DOI] [PubMed] [Google Scholar]
- 20.Løvlien M, Schei B, Gjengedal E. Are there gender differences related to symptoms of acute myocardial infarction? A Norwegian perspective. Prog Cardiovasc Nurs. 2006;2:14–19. doi: 10.1111/j.0197-3118.2006.04656.x. [DOI] [PubMed] [Google Scholar]
- 21.Isaksson R-M, Holmgren L, Lundblad D, Brulin C, Eliasson M. Time trends in symptoms and prehospital delay time in women vs. men with myocardial infarction over a 15-year period. The Northern Sweden MONICA Study. Eur J Cardiovasc Nurs. 2008;7:152–158. doi: 10.1016/j.ejcnurse.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 22.McWilliams MJ. Health consequences of uninsurance among adults in the United States: recent evidence and implications. Milbank Q. 2009;87:443–494. doi: 10.1111/j.1468-0009.2009.00564.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Patchias EM, Waxman J. [Accessed August, 2014];Women and Health Coverage: The Affordability Gap. http://www.commonwealthfund.org/usr_doc/1020_Patchias_women_hlt_coverage_affordability_gap.pdf. Published April, 2007. [PubMed]
- 24.McSweeney JC, Lefler LL, Fischer EP, Naylor AJ, Jr, Evans LK. Women’s prehospital delay associated with myocardial infarction: does race really matter? J Cardiovasc Nurs. 2007;22:279–285. doi: 10.1097/01.JCN.0000278958.98124.6e. [DOI] [PubMed] [Google Scholar]
- 25.Herning M, Hansen PR, Bygbjerg B, Lindhardt T. Women’s experiences and behaviour at onset of symptoms of ST segment elevation acute myocardial infarction. Eur J Cardiovasc Nurs. 2011;10:241–247. doi: 10.1016/j.ejcnurse.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Sans S, Puigdefabregas A, Paluzie G, Monterde D, Balaguer-Vintro I. Increasing trends of acute myocardial infarction in Spain: the MONICA-Catalonia Study. Eur Heart J. 2005;26:505–515. doi: 10.1093/eurheartj/ehi068. [DOI] [PubMed] [Google Scholar]
- 27.Dracup K, Moser DK, Eisenberg M, Meischke H, Alonzo AA, Braslow A. Causes of delay in seeking treatment for heart attack symptoms. Soc Sci Med. 1995;40:379–392. doi: 10.1016/0277-9536(94)00278-2. [DOI] [PubMed] [Google Scholar]
- 28.Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994;331:444–449. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- 29.Shah SJ, Krumholz HM, Reid KJ, Rathore SS, Mandawat A, Spertus JA, Ross JS. Financial stress and outcomes after acute myocardial infarction. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0047420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rasmussen CH, Munck A, Kragstrup J, Haghfelt T. Patient delay from onset of chest pain suggesting acute coronary syndrome to hospital admission. Scand Cardiovasc J. 2003;37:183–186. doi: 10.1080/14017430310014920. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.