Abstract
Background
Recent studies show an association between neighborhood-level measures of socioeconomic status (SES) and outcomes for patients with heart failure. We do not know if neighborhood SES has a primary effect or is a marker for individual SES.
Methods and Results
We used the data from participants of the Tele-HF trial, recruited from 33 US internal medicine and cardiology practices, and examined the association between neighborhood SES and outcomes of patients with heart failure. We used census tracts as proxies for neighborhoods and constructed summary SES scores that included information about wealth and income, education, and occupation. The primary endpoints were readmission and all-cause mortality at 6 month. We conducted patient interviews and medical chart reviews to obtain demographic information, clinical factors, therapies, and individual SES. We included 1557 patients: 524, 516, and 517 from low, medium, and high SES neighborhoods, respectively (mean age: 61.1 ± 15.2 years, 42.2% female). Overall, 745 patients (47.8%) had at least one readmission and 179 patients (11.5%) died. Compared with patients in high SES neighborhoods, those living in low SES neighborhoods were more likely to be readmitted (odds ratio: 1.35, 95% confidence interval: 1.01–1.82) but the mortality rates were not significantly different (odds ratio: 0.78, 95% confidence interval: 0.50–1.18). The results were consistent after multivariable adjustments for individual demographics, clinical factors, and individual SES.
Conclusions
Among patients with heart failure, neighborhood SES was significantly associated with 6-month all-cause readmission even after adjusting for other patient-level factors, including individual SES. Greater number of events and longer follow-up is required to ascertain the potential impact of neighborhood SES on mortality.
Clinical Trial Registration Information
NIH Clinical Trials #NCT00303212, accessible at: http://clinicaltrials.gov/show/NCT00303212
Keywords: heart failure, socioeconomic status, residence, readmission, mortality
Introduction
Physical and social attributes of neighborhoods –that constitute a spatially-defined collection of people, infrastructures, and institutions influenced by common environmental, cultural, and economic forces1– can contribute to the development or aggravation of cardiovascular risk factors. Neighborhood characteristics have been shown to be associated with the incidence and outcomes of cardiovascular disease, as well as all-cause death.2–9 Neighborhood characteristics may be particularly important in patients with chronic conditions such as heart failure. The availability of healthcare resources, nutritious food options, and outlets for physical activity in a neighborhood may influence cardiovascular risk factors and self-management of chronic disease. Community-level stressors (e.g. pollution, crime) and social norms may also play a role in worsening of heart failure.10 Neighborhoods may also be associated with the quality of care.
The distinct contribution of neighborhoods to outcomes of patients with heart failure is not known. Several studies have linked neighborhood characteristics such as low neighborhood socioeconomic status (SES) with lower adherence to therapy, worse quality of care, and worse outcomes among patients with heart failure11–24, but these studies used neighborhood level information as a proxy for individuals’ SES. None of these studies controlled extensively for individual SES factors such as income, education, occupation, insurance, and the burden of healthcare costs, and only few controlled for other important clinical factors, such as disease severity or therapies received.11–24 Therefore, we do not know whether the association between neighborhood SES and heart failure outcomes exists because neighborhood is a proxy for individuals’ SES or it has an effect that is independent of an individual’s SES.25 Such distinction is critical in determining what factors influence heart failure outcomes and whether interventions specifically designed to address neighborhood and contextual factors are needed in addition to interventions that address individual level risk factors.
The Telemonitoring to Improve Heart Failure Outcomes (Tele-HF) trial was a trial designed to evaluate the potential benefits of telemonitoring to improve the outcomes of patients with recent hospitalization for heart failure. The trial enrolled patients from multiple neighborhoods throughout the US and included detailed individual-level clinical and SES factors.26, 27 We used data from Tele-HF to measure the effect of neighborhood SES on heart failure outcomes and to see if the association, if it exists, persists after adjustment for an array of patient-level clinical and SES factors.
Methods
Patients
The methodology and design of the Tele-HF trial (NIH Clinical Trials #NCT00303212) have been previously described.26, 27 In summary, we enrolled 1653patients with heart failure hospitalization within the past 30 days from 2006 through 2009 at 33 internal medicine and cardiology practices across the United States. We excluded patients residing in long-term nursing homes, those with expected survival of less than 6 months for reasons other than heart failure, patients unable to stand on a scale, those with planned hospitalization for a procedure, those unable to speak either English or Spanish, and patients with severe cognitive impairment.
Patient Characteristics
In addition to review of medical records, research staff interviewed and examined the patients at the time of randomization. These data included baseline information about medical history, use of medications, physical findings, left ventricular function, laboratory test results, quality of life, satisfaction with care, and individual SES.
Information about individual SES included annual household income (<$10,000, $10,000–29,999, $30,000–69,999, and >$70,000), level of education (high school or less, some college or vocational school, graduated from college, or a post graduate degree), health literacy, self-reported burden of healthcare costs, and health insurance status. During the interviews, a validated tool was used to determine the patients’ quality of life.28–32
Geo-coding and assigning the neighborhood attributes
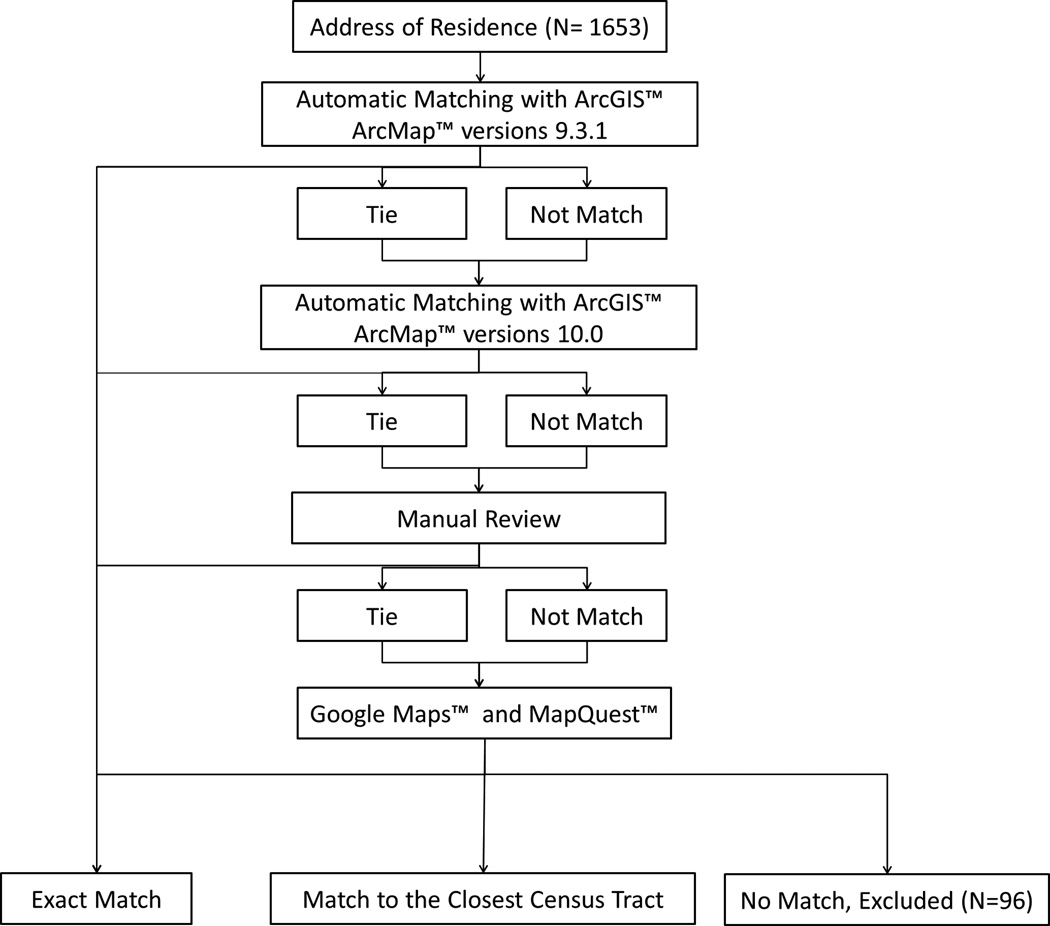
In order to determine the neighborhood SES for patients, we used the patients’ address of residence and determined the census tracts where patients lived through geocoding with ArcGIS™ ArcMap™ versions 9.3.1 and 10.0 (ESRI®, Redlands, CA; See Figure 1 and Appendix 1 for further details). Census tracts represent economically and socially homogenous groups of approximately 4,000 to 7,000 people.33 We excluded 96 patients who could not be reliably assigned to a census tract.
Figure 1. Flow Diagram for Geocoding.
See text for further details.
To derive neighborhood-level indicators for patients (i.e. neighborhood SES and primary care shortage area designation), we linked the set of geocoded patient addresses of the census tracts with data from spatially-defined datasets, including the 2000 Decennial United States Census, American Community Survey 5-year (2005–2009), and Health Professional Service Area at the census-tract level.
Neighborhood SES
We used a summary score as the indicator of neighborhood SES, following the methodology by Diez Roux and colleagues.2 In brief, we derived the summary indicator from six variables representing dimensions of wealth and income (log of the median household income, log of the median value of housing units, the percentage of households receiving interest, dividend, or net rental income), education (the percentage of adults≥ 25 years who completed high school and the percentage of adults ≥ 25 years who had completed college), and occupation (the percentage of employed persons≥ 16 years in executive, managerial, or professional specialty occupations). For each variable, we calculated a z-score for each census tract by subtracting the overall mean (across all census tracts in the sample) and dividing by the standard deviation. We calculated the neighborhood summary score by summing the z-scores for each of the six variables. Neighborhood scores for the census tracts in our study ranged from −12.6 to 15.3, with an increasing neighborhood z-score signifying an increasing neighborhood SES. As stated above, we reported the neighborhood SES at the census tract level for enrolled patients, rather than at the level of enrolling sites. We grouped the patients according to the distribution of the neighborhood summary score into tertiles of high, medium, and low SES.2
Outcomes
The primary endpoints were all-cause readmission and mortality at 6 months. We chose to observe the outcomes at 6-month follow-up because this was the chosen time interval to determine the primary event rates in the Tele-HF trial. At 6 months, research staff contacted the patients and reviewed the office and hospital medical records to ascertain any hospital readmissions. An independent committee adjudicated all readmissions to differentiate them from other clinical encounters such as emergency department visits. Since hospital readmissions and mortality may have complex correlations (e.g. less readmissions in case of more deaths), we decided to consider a composite of death or readmission at 6 month as a secondary endpoint. This analysis was primarily intended to see if these endpoints potentially nullified each other, if they moved on different directions.
Statistical Analysis
We described continuous variables as means (standard deviation) and compared them using one-way analysis of variance (ANOVA). We described categorical variables as frequencies and compared them using Chi squared tests. We compared the all-cause hospital readmission, all-cause mortality, and the composite of all-cause hospital readmission and all-cause mortality at 6-month follow-up across the neighborhood SES groups.
We used logistic regression with generalized estimating equations (GEE) method to determine the association between neighborhood SES and outcomes while accounting for clustering of patients within hospitals or practices that recruited them. We examined whether the associations persisted with adjustment for important individual-level covariates. For this analysis, we grouped the individual-level covariates into categories of demographics, clinical variables related to disease severity and co-morbidities, therapies received, and individual SES2 (Table 1). Accordingly, we built several GEE models, adding the aforementioned sets of covariates in a sequential order. In all models, we considered patients in high SES neighborhoods as the referent group.
Table1.
Demographics, Clinical Condition, Laboratory Results, and Baselines Treatments Stratified Based on Neighborhood Socioeconomic Groups
| Total (N=1557) |
Low SES (N=524) |
Middle SES (N=516) |
High SES (N=517) |
P-value | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age (years, SD) | 61.1 (15.2) | 57.6 (13.9) | 59.1 (14.9) | 66.6 (15.2) | <0.0001 |
| Female (%) | 42.2 | 46.0 | 39.3 | 41.2 | 0.0808 |
| Race | <0.0001 | ||||
| White (%) | 49.2 | 33.4 | 49.4 | 65.0 | |
| Black (%) | 39.6 | 62.2 | 39.5 | 16.6 | |
| Other (%) | 11.2 | 4.4 | 11.0 | 18.4 | |
| Individual SES | |||||
| Insurance | <0.0001 | ||||
| Commercial, PPO, HMO (%) | 34.9 | 23.9 | 34.7 | 46.2 | |
| Medicare (%) | 34.8 | 34.7 | 33.7 | 36.0 | |
| Medicaid (%) | 13.0 | 17.0 | 14.7 | 7.4 | |
| None/self-pay (%) | 11.9 | 18.1 | 10.7 | 6.8 | |
| Other (%) | 5.4 | 6.3 | 6.2 | 3.7 | |
| Reported annual household income | <0.0001 | ||||
| <$10,000 (%) | 28.2 | 39.8 | 28.5 | 15.1 | |
| $10,000–29,999 (%) | 35.2 | 41.4 | 36.3 | 27.5 | |
| $30,000–69,999 (%) | 27.6 | 17.2 | 29.6 | 37.0 | |
| >$70,000 (%) | 9.0 | 1.5 | 5.6 | 20.4 | |
| Education | <0.0001 | ||||
| High school or less (%) | 61.0 | 75.0 | 61.0 | 47.0 | |
| Some college or vocational school (%) | 24.5 | 18.8 | 28.0 | 26.9 | |
| Graduated from college (%) | 9.3 | 4.9 | 7.8 | 15.2 | |
| Post graduate degree (%) | 5.2 | 1.3 | 3.2 | 10.8 | |
| Clinical condition and co-morbidities at baseline | |||||
| Body mass index (kg/m2; mean, SD) | 26.6 (11.4) | 28.0 (11.5) | 27.1 (11.3) | 24.7 (11.0) | <.0001 |
| Hypertension (%) | 77.4 | 84.2 | 74.8 | 73.1 | <.0001 |
| Diabetes mellitus (%) | 46.6 | 48.1 | 48.1 | 43.5 | 0.2367 |
| Hyperlipidemia (%) | 52.0 | 50.2 | 53.3 | 52.6 | 0.5739 |
| Smoking Status | 0.0002 | ||||
| Current smoker (%) | 35.2 | 31.1 | 34.6 | 39.8 | |
| Never smoked cigarettes, not even a puff (%) | 3.9 | 4.7 | 4.4 | 2.6 | |
| Smoked in the past, but less than 100\n cigarettes total (%) | 39.8 | 38.5 | 37.4 | 43.3 | |
| Stopped smoking more than 1 year ago (%) | 10.6 | 12.3 | 10.5 | 9.0 | |
| Stopped smoking between 1 month ago and 1 year ago (%) | 10.5 | 13.4 | 13.1 | 5.3 | |
| Smoked (even a puff) in the past 30 days (%) | 35.2 | 31.1 | 34.6 | 39.8 | |
| Coronary artery disease | 40.7 | 36.3 | 39.0 | 47.0 | 0.0012 |
| Chronic kidney disease | 42.5 | 45.7 | 41.6 | 40.0 | 0.1842 |
| Chronic lung disease | 21.2 | 21.6 | 22.7 | 19.3 | 0.4103 |
| NYHA class | 0.0003 | ||||
| I | 6.0 | 8.0 | 5.2 | 4.6 | |
| II | 37.0 | 35.7 | 31.4 | 43.9 | |
| III | 50.5 | 49.4 | 55.4 | 46.8 | |
| IV | 6.5 | 6.9 | 7.9 | 4.6 | |
| Left Ventricular ejection fraction <40% | 70.4 | 75.0 | 72.5 | 63.3 | 0.0001 |
| Laboratory | |||||
| Hemoglobin (gr/dl; mean, SD) | 12.4 (2.1) | 12.3 (2.0) | 12.4 (2.1) | 12.4 (2.1) | 0.6255 |
| Plasma creatinine (mg/dl; mean, SD) | 1.5 (0.7) | 1.5 (0.7) | 1.5 (0.8) | 1.4 (0.7) | 0.2512 |
| Serum potassium (meq/lit, mean, SD) | 4.1 (0.6) | 4.0 (0.5) | 4.1 (0.6) | 4.1 (0.6) | 0.1031 |
| Baseline treatments | 49.1 | 50.5 | 47.1 | 49.7 | 0.5572 |
| ACEIs or ARBs | 58.0 | 60.0 | 56.1 | 57.8 | 0.4925 |
| Beta blocks | 23.4 | 22.5 | 25.1 | 22.5 | 0.5663 |
| Aldosterone antagonists | 19.5 | 16.8 | 22.2 | 19.5 | 0.1278 |
| Digoxin | 5.3 | 3.8 | 4.5 | 7.7 | 0.0106 |
| CRT | 24.5 | 24.2 | 27.1 | 22.2 | 0.1854 |
| ICD | 49.7 | 46.0 | 52.1 | 51.1 | 0.1061 |
| Telemonitoring | 49.1 | 50.5 | 47.1 | 49.7 | 0.5572 |
ACEI: angiotensin converting enzyme inhibitor, ARB: angiotensin receptor blocker, HMO: Health Maintenance Organization, PPO: Preferred Provider Organization, SD: standard deviation, SES: Socioeconomic Status.
Data about demographics, neighborhood SES, clinical co-morbidities and outcomes were available for 100% of participants. There were missing values for some patients for some of the covariates related to laboratory tests, baseline therapies and individual SES. None of such covariates had a missing rate higher than 30%, with total household income (29.3%), baseline B-type natriuretic peptide values (22.9%), baseline Personal Health Questionnaire Depression Scale (PHQ-9) values (19.4%), and self-reported avoidance of healthcare due to costs (14.9%) being the 4 variables with highest missing rates. We used the multiple imputation technique for the covariates with missing values in the GEE models.34 All predictors were used to impute missing values with fully conditional specification (FCS) approach. Linear regression method was used for continuous variables and logistic regression method was used for categorical variables in FCS. The coefficients of 20 rounds of imputation were combined to obtain the final estimates for the GEE model.
In the final GEE model, we also introduced census tract level primary care shortage area designation as an indicator for access to care and quality of care. The purpose is to determine whether the neighborhood effect, if it exists, persists after accounting for such differences. We performed all analyses on SAS Version 9.2 (SAS Inc., Cary, NC). P values less than 0.05 were considered statistically significant. The institutional review boards at Yale University School of Medicine and each participating site approved the study protocol of the Tele-HF trial and the subjects provided informed consent for the study. The National Heart, Lung and Blood Institute funded the Tele-HF trial.
Results
From the total of 1653 participants, we excluded 96 who could not be matched to a census tract address. Accordingly, we considered 1557 patients for this analysis: 524 (33.7%) patients from low SES neighborhoods, 516 (33.1%) patients from middle SES neighborhoods, and 517 (33.2%) patients from high SES neighborhoods. Compared with those in high-SES neighborhoods, patients living in low-SES neighborhoods were younger, were less frequently white, had lower levels of education and income, and were less often medically insured (P<0.001 for all comparisons). Almost 40% of patients living in low-SES neighborhoods and 15.2% of patients in high-SES neighborhoods reported annual income <$10,000 a year. In contrast, 1.5% of those in low-SES neighborhoods and 20.4% of those in high-SES neighborhoods reported annual income>$70,000. Those living in high-SES neighborhoods had a higher frequency of cigarette smoking (P<0.001) and coronary artery disease (P=0.001) but had slightly lower body mass indices, lower frequency of hypertension, less severe New York Heart Association (NYHA) Functional Classification, and slightly lower frequency of having left ventricular ejection fraction of less than 40%(P<0.001 for all comparisons). Other baseline characteristics were comparable in the three groups (Table 1).
Readmission, Mortality, and the Composite of Readmission or Mortality at 6 Months
Over the follow-up period, 745 (47.8%) patients had at least one readmission: 272 patients from low-SES neighborhoods, 242 patients from medium-SES neighborhoods, and 231 patients from high-SES neighborhoods. Unadjusted results showed that compared with patients in high SES neighborhoods, those living in low SES neighborhoods were more likely to have hospital readmission within 6 months (51.9% versus 44.7%, odds ratio: 1.35, 95% confidence interval: 1.01–1.82, P=0.042). The results were consistent after multivariable adjustment for demographics, NYHA functional class, co-morbidities and laboratory test results, individual SES factors, and baseline therapies (odds ratio: 1.49, 95% confidence interval: 1.04–2.13). The results remained fundamentally unchanged after further adjustment for primary care shortage area designation (odds ratio: 1.57, 95% confidence interval: 1.10–2.23) (Table 2). The results were also consistent if we excluded patients that died prior to having a non-fatal readmission (N=57, odds ratio from the final model: 1.54 [95% confidence interval: 1.08–2.18]).
Table 2.
Outcomes of Patients in High, Middle, and Low SES Neighborhoods: Number of Events (A), and Adjusted Models (B)
| All-cause Readmissions At 6 Months, N (%) |
All-cause Death At 6 Months, N (%) |
All-cause Death or Readmission At 6 Months, N (%) |
||||||
|---|---|---|---|---|---|---|---|---|
| Low-SES | Middle SES | High-SES | Low-SES | Middle-SES | High SES | Low-SES | Middle-SES | High-SES |
| 272 (51.9) | 242 (46.9) | 231 (44.7) | 50 (9.5) | 66 (12.8) | 63 (12.2) | 286 (54.6) | 265 (51.4) | 251 (48.5) |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
|---|---|---|---|---|---|---|---|---|
| Unadjusted results |
Adjusted for* Individual demographics |
NYHA | Clinical comorbidities and laboratory test |
General individual SES |
Health- related individual SES |
Baseline therapies |
Neighborhood- level PCSA designation |
|
| ALL CAUSE READMISSION AT 6 MONTHS | ||||||||
| High SES | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Middle SES OR (95% CI) | 1.09 (0.88–1.36) | 1.16 (0.91–1.48) | 1.11 (0.88–1.41) | 1.09 (0.86–1.38) | 1.09 (0.86–1.38) | 1.08 (0.86–1.37) | 1.07 (0.85–1.35) | 1.09 (0.87–1.38) |
| Low SES OR (95% CI) | 1.35 (1.01–1.82) | 1.50 (1.06–2.14) | 1.48 (1.03–2.12) | 1.46 (1.03–2.06) | 1.47 (1.04–2.07) | 1.49 (1.05–2.12) | 1.49 (1.04–2.13) | 1.57 (1.10–2.23) |
| ALL-CAUSE DEATH AT 6 MONTHS | ||||||||
| High SES | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Middle SES OR (95% CI) | 1.07 (0.78–1.48) | 1.39 (0.93–2.09) | 1.27 (0.84–1.92) | 1.27 (0.83–1.93) | 1.22 (0.78–1.93) | 1.14 (0.71–1.83) | 1.15 (0.71–1.86) | 1.06 (0.66–1.72) |
| Low SES OR (95% CI) | 0.78 (0.50–1.18) | 1.11 (0.67–1.86) | 1.074 (0.69–1.68) | 1.126 (0.73–1.74) | 1.05 (0.67–1.64) | 0.93 (0.58–1.47) | 0.93 (0.59–1.48) | 0.75 (0.48–1.17) |
| DEATH OR READMISSION AT 6 MONTHS | ||||||||
| High SES | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Middle SES OR (95% CI) | 1.12 (0.92–1.36) | 1.21 (0.96–1.53) | 1.15 (0.92–1.45) | 1.14 (0.89–1.44) | 1.14 (0.89–1.45) | 1.12 (0.89–1.42) | 1.12 (0.88–1.41) | 1.13 (0.89–1.44) |
| Low SES OR (95% CI) | 1.29 (0.98–1.70) | 1.46 (1.04–2.07) | 1.43 (1.01–2.04) | 1.43 (1.02–2.01) | 1.44 (1.04–2.00) | 1.45 (1.04–2.02) | 1.45 (1.04–2.02) | 1.50 (1.09 – 2.07) |
Odds ratios were calculated with reference to patients who had high neighborhood socioeconomic status.
Each model also includes all variables in the model above it.
CI: confidence interval, OR: odds ratio, PCSA: primary care shortage area, SES: socioeconomic status.
There were 179 (11.5%) deaths over the 6-month follow-up. Unadjusted and multivariable adjusted models did not show a statistically significant association between neighborhood SES and mortality (odds ratio for mortality in low-SES versus high-SES neighborhoods after multivariable adjustment for demographics, NYHA functional class, co-morbidities and laboratory test results, general individual SES, health-related SES, and baseline therapies: 0.93 [95% confidence interval: 0.59–1.48], see Table 2).
Overall, 802 (51.5%) patients died or had at least one episode of hospital readmission. Unadjusted results showed a trend toward worse results for the composite endpoint among patients living in low SES neighborhoods (odds ratio: 1.29, 95% confidence interval: 0.98–1.70, P=0.073). Once adjusted for demographics, the trend for worse outcomes in low SES neighborhoods reached statistical significance (odds ratio: 1.46; 95% confidence interval: 1.04–2.07, P=0.03). The results were consistent after further multivariable adjustments for NYHA functional class, co-morbidities and laboratory test results, general individual SES, health-related SES, baseline therapies, and primary care shortage area designation (odds ratio: 1.50, 95% confidence interval: 1.09–2.07)(Table 2).
Discussion
Our study demonstrated higher rates of all-cause readmission and a composite of death or readmission at 6 months for patients with heart failure who lived in low SES neighborhoods, a finding which is consistent with previous studies.11, 12, 16, 21 More importantly, we showed that the neighborhood effect persisted after multivariable adjustment for demographics, clinical factors, and also an extensive set of individual SES variables. Lack of attenuation of the neighborhood effect after adjustment for individual’s SES factors implies that a large proportion of the association between neighborhood SES and outcomes is not mediated by the individual-level SES.
Our study is the first to show an effect of neighborhood SES on outcomes of patients with heart failure which persists after adjustment for a wide array of individual-level clinical and SES variables. Previous research has shown that neighborhood SES is associated with the incidence and outcomes of other cardiovascular diseases, as well as all-cause mortality, even after adjustment for individual-level risk factors and individual SES.2, 5–9 The causal role of neighborhood is supported by a randomized housing mobility experiment which showed that moving from a low SES to a high SES neighborhood leads to improvements in objective and subjective physical and mental health indices.35
We must clarify that the intent of our study was to determine the association between neighborhood characteristics and outcomes of patients with heart failure and to see if such associations are, at least in part, independent of individual SES. Our findings confirmed such associations. Identifying the exact mediators of the neighborhood effect is a crucial next step which should be followed in subsequent studies. While we cannot specifically comment on such mediators, several potential explanations exist. It can be speculated that various neighborhood characteristics may have immediate or long-term effects. Tobacco advertising, availability and costs of healthier foods, liquor stores, and availability and quality of exercise facilities vary widely across neighborhoods, as do institutional resources and social ties and interactions of residents, and easily accessible healthcare.2–4 Such factors may lead into short-term changes in disease outcomes such as hospital readmissions. For example, patients living in “food deserts” may be more likely to use processed, high-salt food that can lead into fluid retention and decompensation of heart failure. Likewise, lack of easy access to healthcare can lead into suboptimal tailoring of medications leading into readmissions. Pharmacological and non-pharmacological treatment adherence is also contingent upon social support and community norms regarding health care, which may be deficient in low SES areas. Moreover, living in certain neighborhoods can be associated with sources of chronic stress such as noise, air pollution, violence, and poverty.2, 4 These, as well as other components of built environment such as availability of parks and walkability may impact long-term outcomes after prolonged exposure.
Quality of care may also vary by neighborhood with health system interventions in lower income neighborhoods being less comprehensive and of lower quality than in higher income neighborhoods, or less well-tailored to needs of the particular community. It could be argued that since patients living in low SES neighborhoods may have worse access to care, the higher readmission rates among such patients reflects higher use of hospital emergency department, simply as an alternative to outpatient visits.19 However, readmissions in the Tele-HF trial were adjudicated by an independent committee and hence, emergency department visits were not counted as readmissions in the Tele-HF dataset. We believe the higher rate of readmission among patients from socioeconomically deprived neighborhoods does not reflect greater use of hospital emergency department as a substitute to outpatient clinics. Another mediating mechanism could be that practicing physicians had a lower threshold to hospitalize patients from low SES neighborhoods, in part due to issues related to care coordination for such patients. Even if this assumption accounts for some of the increased readmissions in patients from low SES neighborhoods, it represents neighborhood level disparities that need to be addressed for improving care and outcomes. Although we looked at primary care shortage area designation as a potential mediator of such quality of care differences, our results suggest that primary care shortages do not mediate the neighborhood effect. Additional work is needed to identify the key elements of neighborhoods that mediate neighborhood-level disparities in disease incidence and outcomes. Among the neighborhood-level mediators, some may be more readily modifiable. Policy and interventions aimed at removing the modifiable geographic disparities in such elements could be tested to determine their role. For example, future studies can assess whether establishment of healthy food stores in “food deserts” or improving factors such as air pollution and neighborhood walkability can impact short-term and long-term outcomes of patients with heart failure. Likewise, it could be tested to determine whether using neighborhood characteristics to identify particularly vulnerable patients leads into better outcomes.
Previous studies have shown that neighborhood characteristics can impact both short-term and long-term health outcomes.11, 21, 35 In our study, adjusted 6-month mortality rates were not significantly different across the neighborhood SES groups. However, a previous study showed that compared with those living in high SES neighborhoods, patients with heart failure who lived in socioeconomically deprived neighborhoods had similar rates of 30-day mortality but higher death at 1-year.21 As stated earlier, investigating the impact of several of the neighborhood chronic stressors may require long-term follow-up. Because of the short follow-up period of the Tele-HF trial, we are unable to determine the impact of the neighborhood effect beyond 6 months. Future studies with longer term follow-up will provide additional insights. We should also clarify that the association between the neighborhood SES and the composite endpoint of all-cause death or readmission at 6 months was primarily driven by readmissions, rather than deaths.
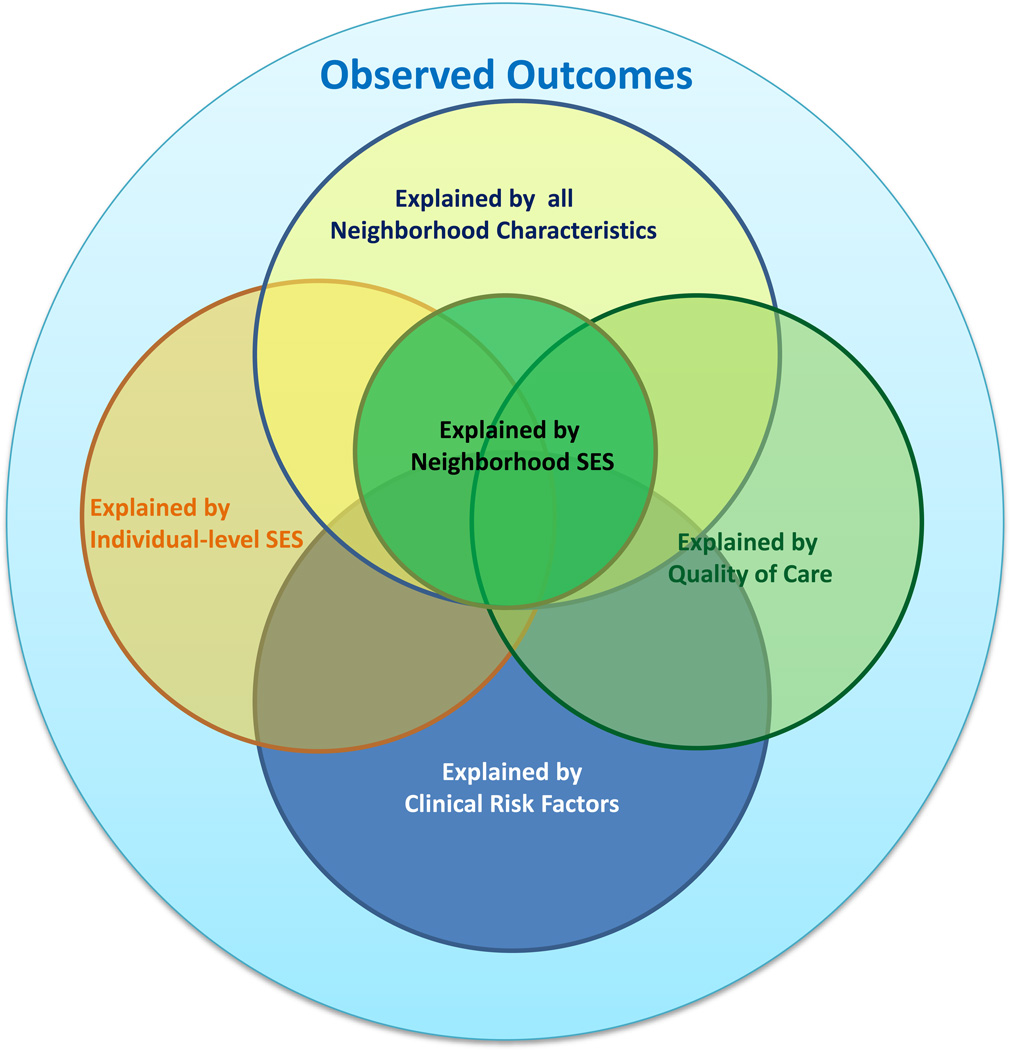
There are some limitations to our study. First, although demographics, clinical variables, and the studied endpoints were abstracted rigorously and had minimal to no missing values, there were missing values for some patients for individual SES variables. Particularly, suboptimal reporting of individual income has been almost invariably seen in previous studies.36 We used multiple imputation techniques to calculate estimates for those missing values using several other variables with low missing rates. The consistent trends we observed in unadjusted, as well as several multivariable adjusted models (including models with variables that had very low to no missing values) suggest the robustness of the neighborhood effect. Second, there was also inevitably some overlap between neighborhood SES and individual-level SES. However, formal statistical tests between neighborhood SES and components of individual SES did not show evidence of multicolinearity (Spearman’s coefficient: 0.36 between individual income and neighborhood SES, and 0.28 between level of education and neighborhood SES), further confirming that the neighborhood SES is related to but not merely a proxy for individual SES (see Figure 2). Finally, Tele-HF participants were slightly younger than patients in heart failure registries, such as ADHERE.37 However, enrolled patients in Tele-HF had substantial racial and SES diversity. Such diversity makes our cohort well-suited for understanding the neighborhood effects on heart failure outcomes and for isolating neighborhood effect from that of race or individual SES.
Figure 2. Proposed Model for Contribution of Individual-level and Neighborhood Factors in Disease Outcomes.
SES: socioeconomic status.
In conclusion our study showed the effect of neighborhood SES on all-cause hospital readmissions among patients with heart failure, which persisted after adjustment for individual-level risk factors and therapies, and individual SES. To prevent readmission we may need to focus on neighborhood factors as well as individual patient factors.
Supplementary Material
Acknowledgements
The authors would like to thank Beth Hodshon for her administrative support.
Funding Sources
The Telemonitoring to Improve Heart Failure Outcomes trial was supported by a grant (5 R01 HL080228) from the National Heart, Lung, and Blood Institute. The current manuscript was also supported by grant number U01HL105270-03 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the sponsor.
Dr. Krumholz reports that he is the recipient of a research grant from Medtronic through Yale University and chairs a cardiac scientific advisory board for United Healthcare.
Footnotes
Conflict of Interest Disclosures
The other authors report no potential conflicts of interest.
References
- 1.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing "neighborhood effects": Social processes and new directions in research. Annual Rev Sociol. 2002;28:443–478. [Google Scholar]
- 2.Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 3.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 4.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 5.Subramanian SV. The relevance of multilevel statistical methods for identifying causal neighborhood effects. Soc Sci Med. 2004;58:1961–1967. doi: 10.1016/S0277-9536(03)00415-5. [DOI] [PubMed] [Google Scholar]
- 6.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6:712–722. doi: 10.1038/nrcardio.2009.163. [DOI] [PubMed] [Google Scholar]
- 7.Gerber Y, Benyamini Y, Goldbourt U, Drory Y. Neighborhood socioeconomic context and long-term survival after myocardial infarction. Circulation. 2010;121:375–383. doi: 10.1161/CIRCULATIONAHA.109.882555. [DOI] [PubMed] [Google Scholar]
- 8.Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. Am J Epidemiol. 1999;149:898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- 9.Stjarne MK, Fritzell J, De Leon AP, Hallqvist J. Neighborhood socioeconomic context, individual income and myocardial infarction. Epidemiology. 2006;17:14–23. doi: 10.1097/01.ede.0000187178.51024.a7. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg MS, Giannetti N, Burnett RT, Mayo NE, Valois MF, Brophy JM. Shortness of breath at night and health status in congestive heart failure: effects of environmental conditions and health-related and dietary factors. Environ Res. 2009;109:166–174. doi: 10.1016/j.envres.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Hawkins NM, Jhund PS, McMurray JJ, Capewell S. Heart failure and socioeconomic status: accumulating evidence of inequality. Eur J Heart Fail. 2012;14:138–146. doi: 10.1093/eurjhf/hfr168. [DOI] [PubMed] [Google Scholar]
- 12.Philbin EF, Dec GW, Jenkins PL, DiSalvo TG. Socioeconomic status as an independent risk factor for hospital readmission for heart failure. Am J Cardiol. 2001;87:1367–1371. doi: 10.1016/s0002-9149(01)01554-5. [DOI] [PubMed] [Google Scholar]
- 13.Gamble JM, Eurich DT, Ezekowitz JA, Kaul P, Quan H, McAlister FA. Patterns of care and outcomes differ for urban versus rural patients with newly diagnosed heart failure, even in a universal healthcare system. Circ Heart Fail. 2011;4:317–323. doi: 10.1161/CIRCHEARTFAILURE.110.959262. [DOI] [PubMed] [Google Scholar]
- 14.Havranek EP, Wolfe P, Masoudi FA, Rathore SS, Krumholz HM, Ordin DL. Provider and hospital characteristics associated with geographic variation in the evaluation and management of elderly patients with heart failure. Arch Intern Med. 2004;164:1186–1191. doi: 10.1001/archinte.164.11.1186. [DOI] [PubMed] [Google Scholar]
- 15.McAlister FA, Murphy NF, Simpson CR, Stewart S, MacIntyre K, Kirkpatrick M, Chalmers J, Redpath A, Capewell S, McMurray JJ. Influence of socioeconomic deprivation on the primary care burden and treatment of patients with a diagnosis of heart failure in general practice in Scotland: population based study. BMJ. 2004;328:1110. doi: 10.1136/bmj.38043.414074.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Foraker RE, Rose KM, Suchindran CM, Chang PP, McNeill AM, Rosamond WD. Socioeconomic status, Medicaid coverage, clinical comorbidity, and rehospitalization or death after an incident heart failure hospitalization: Atherosclerosis Risk in Communities cohort (1987 to 2004) Circ Heart Fail. 2011;4:308–316. doi: 10.1161/CIRCHEARTFAILURE.110.959031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jhund PS, Macintyre K, Simpson CR, Lewsey JD, Stewart S, Redpath A, Chalmers JW, Capewell S, McMurray JJ. Long-term trends in first hospitalization for heart failure and subsequent survival between 1986 and 2003: a population study of 5.1 million people. Circulation. 2009;119:515–523. doi: 10.1161/CIRCULATIONAHA.108.812172. [DOI] [PubMed] [Google Scholar]
- 18.Menec VH, Shooshtari S, Nowicki S, Fournier S. Does the relationship between neighborhood socioeconomic status and health outcomes persist into very old age? A population-based study. J Aging Health. 2010;22:27–47. doi: 10.1177/0898264309349029. [DOI] [PubMed] [Google Scholar]
- 19.Struthers AD, Anderson G, Donnan PT, MacDonald T. Social deprivation increases cardiac hospitalisations in chronic heart failure independent of disease severity and diuretic non-adherence. Heart. 2000;83:12–16. doi: 10.1136/heart.83.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stewart S, Murphy NF, McMurray JJ, Jhund P, Hart CL, Hole D. Effect of socioeconomic deprivation on the population risk of incident heart failure hospitalisation: an analysis of the Renfrew/Paisley Study. Eur J Heart Fail. 2006;8:856–863. doi: 10.1016/j.ejheart.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 21.Rathore SS, Masoudi FA, Wang Y, Curtis JP, Foody JM, Havranek EP, Krumholz HM. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2006;152:371–378. doi: 10.1016/j.ahj.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blackledge HM, Tomlinson J, Squire IB. Prognosis for patients newly admitted to hospital with heart failure: survival trends in 12 220 index admissions in Leicestershire 1993–2001. Heart. 2003;89:615–620. doi: 10.1136/heart.89.6.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Antonelli-Incalzi R, Ancona C, Forastiere F, Belleudi V, Corsonello A, Perucci CA. Socioeconomic status and hospitalization in the very old: a retrospective study. BMC Public Health. 2007;7:227. doi: 10.1186/1471-2458-7-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shah SM, Carey IM, DeWilde S, Richards N, Cook DG. Trends and inequities in beta-blocker prescribing for heart failure. Br J Gen Pract. 2008;58:862–869. doi: 10.3399/bjgp08X376195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cook NL, Lauer MS. The socio-geography of heart failure: why it matters. Circ Heart Fail. 2011;4:244–245. doi: 10.1161/CIRCHEARTFAILURE.111.962191. [DOI] [PubMed] [Google Scholar]
- 26.Chaudhry SI, Barton B, Mattera J, Spertus J, Krumholz HM. Randomized trial of Telemonitoring to Improve Heart Failure Outcomes (Tele-HF): study design. J Card Fail. 2007;13:709–714. doi: 10.1016/j.cardfail.2007.06.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chaudhry SI, Mattera JA, Curtis JP, Spertus JA, Herrin J, Lin Z, Phillips CO, Hodshon BV, Cooper LS, Krumholz HM. Telemonitoring in patients with heart failure. N Engl J Med. 2010;363:2301–2309. doi: 10.1056/NEJMoa1010029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riegel B, Carlson B, Glaser D. Development and testing of a clinical tool measuring self-management of heart failure. Heart Lung. 2000;29:4–15. doi: 10.1016/s0147-9563(00)90033-5. [DOI] [PubMed] [Google Scholar]
- 29.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Seeman TE, Berkman LF. Structural characteristics of social networks and their relationship with social support in the elderly: who provides support. Soc Sci Med. 1988;26:737–749. doi: 10.1016/0277-9536(88)90065-2. [DOI] [PubMed] [Google Scholar]
- 31.Green CP, Porter CB, Bresnahan DR, Spertus JA. Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure. J Am Coll Cardiol. 2000;35:1245–1255. doi: 10.1016/s0735-1097(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 32.Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, Crouch MA. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–395. [PubMed] [Google Scholar]
- 33.Sasson C, Magid DJ, Chan P, Root ED, McNally BF, Kellermann AL, Haukoos JS, Group CS. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–1615. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, Sanbonmatsu L. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337:1505–1510. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lillard L, Smith JP, Welch F. What do we really know about wages? The importance of nonreporting and census information. J Polit Econ. 1986;94:489–506. [Google Scholar]
- 37.Adams KF, Jr, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Berkowitz RL, Galvao M, Horton DP Committee ASA, Investigators. Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2005;149:209–216. doi: 10.1016/j.ahj.2004.08.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.