Abstract
The etiology of premenstrual syndrome (PMS) is unknown; it may be due to the normal effect of hormones during the menstrual cycle as it occurs in the late luteal phase of the menstrual cycle.PMS affects women of childbearing age and remits with the onset of menstruation. The menstrual phase is known to influence stage 2 and REM sleep in women, irrespective of premenstrual dysphoric disorder (PMDD). Women with PMDD showed a decreased response to melatonin in their luteal phase as compared to the follicular phase of the menstrual cycle. However, melatonin duration or timing of offset in the morning has not been reported to correlate with the mood. Rather, improvement in mood-related symptoms of PMDD has been found to be influenced by sleep deprivation, be it sleep restrictions in early or late night. Sleep disturbance and decreased melatonin secretions due to hormonal fluctuations during the luteal phase of the menstrual cycle could explain the sleep complaints of PMDD.
Keywords: Follicular, Hormone, Insomnia, Luteal, Menstrual cycle, Ovulation, PMDD, PMS, Sleep, Women
INTRODUCTION
Normal sleep is essential for an individual’s physical and mental wellbeing. Although there is a variation in sleep requirements amongst individuals, most adults require approximately seven hours on a regular basis for the promotion of optimal health [1].Women have more disturbed sleep than men. Menstrual-related hormonal fluctuations may be responsible for this sleep disturbance, which is a part of the premenstrual dysphoric disorder (PMDD) [2].Women with PMDD experience anger, irritability and other mood symptoms six days prior to menses, with a peak in severity two days prior to menses. While symptoms can carry over into the next menstrual cycle, a diagnosis of PMDD requires freedom from symptoms during the pre-ovulatory period. In addition, the constellation of symptoms tends to be consistent from month to month [3]. The common sleep problems associated with PMDD are sleep onset insomnia, frequent night time awakenings, and non-restoration of sleep. These sleep related problems also have daytime consequences in the form of poor concentration, daytime sleepiness, decreased alertness and poor performance at work [4].
Menstrual Cycle and Premenstrual Syndrome
There are monthly cyclical changes in the uterus and ovary, which are essential for sexual reproduction. These changes are under the influence of hormones, which include estrogen, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). The menstrual cycle is responsible for the production of eggs and it prepares the uterus for pregnancy [5]. The average length of the cycle is 28 days (ranges 21–35 days), and the cycle itself starts between the ages of menarche (12 years’ average) until menopause (51 years’ average). Its timing is governed by endogenous (internal) biological cycles. Premenstrual syndrome is related with menstrual cycle, especially with the luteal phase of the menstrual cycle and subsides with menstruation [6].
Phases of Menstrual Cycle and Premenstrual Syndrome
The menstrual cycle is divided into four phases, starting with the first day of menstruation when the menstrual phase begins (day 1–5). This followed the follicular phase that extends from day 1 to day 13. Ovulation occurs on day 14. After ovulation, there is a luteal phase that lasts from day 15 to day 28. Premenstrual syndrome starts at the luteal phase, and the severity of symptoms peak in the late luteal phase and subsides with the end of menstruation [7].
Definition and Diagnosis of Premenstrual Syndrome
The etiology of PMDD is unknown; it may be due to the normal effect of hormones (estrogen, progesterone) during the menstrual cycle as it occurs in the late luteal phase. It effects women of childbearing age and remits with the onset of menstruation. It affects the physical and psychological health of women. The DSM-5 says that PMDD is characterized primarily by mood changes, and the symptoms may appear in the form of depressed mood, anxiety/tension, mood swings or noticeable irritability. In addition, it may be associated with other symptoms related to cognitive, psychomotor and biological functions and bodily domains. These symptoms include poor concentration, feelings that one is not in control of herself; lethargy or easy fatigability, appetite changes (e.g. decrement or increment), and physical symptoms (e.g., tenderness and bloating of breasts, body aches and pains). There are no laboratory tests that confirm PMDD. The diagnosis is made by looking at the patient’s medical history and noticing the symptoms for two prospective menstrual cycles [7] (Table 1).
Table 1.
Menstrual cycle associated premenstrual syndrome.
| Menstrual Phase |
Follicular Phase |
Ovulation Phase |
Luteal Phase |
|---|---|---|---|
| Day (1–6) | Day (1–13) | Day (14) | Day (15–28) |
| Remission of Symptoms |
No Symptoms |
No Symptoms |
Premenstrual Syndrome DSM-5 Criteria: Symptoms Physiological: Depressed mood, Anxiety/ Tension, Mood swings, Appetite changes, Food cravings, Concentration difficulties, Feeling out of control. Physical: Tenderness and bloating of breast, Premenstrual migraine. |
Menstrual Cycle and Functional Ovarian Diseases in Young Women
Functional ovarian lesions mainly include follicular cysts and corpus luteum cysts. These cysts represent 45% of adnexal masses in both children and in young women, and commonly occur in post-men archeal girls due to ovulatory cycles. Hemorrhagic corpus luteum cysts are medical emergencies for post-menarche women. Patients can present with persistent, acute, and severe abdominal pain, signs of peritoneal irritation, and adnexal mass, just after the menarche. The diagnostic intervention is ultrasound, and the treatment option is surgery, either laparoscopy or laparotomy depending on the severity of the symptoms. No recurrence of the disease is reported and normal menstruation is restored within two years [8–10].
Prevalence of PMMD Worldwide
Studies show the prevalence of PMDD varies in different populations of the world (Table 2).
Table 2.
Prevalence and severity of premenstrual symptoms [11].
| PMDD Preva- lence (DSM-4 criteria) |
Population (n) |
Study design |
Population based study title |
References |
|---|---|---|---|---|
| 16 % | 300 | Cross- sectional study |
Prevalence and sever- ity of premenstrual symptoms among Ira- nian female university students |
(Bakhshani, Mousavi et al. 2009) [11] |
| 60.3 % | 1395 | Cross- sectional study |
Population study of premenstrual syn- drome |
(Silva, Gi- gante et al. 2006) [12] |
| 3–8 % | 1488 | Prospec- tive lon- gitudinal study |
Prevalence, incidence and stability of PMDD in the community |
(Wittchen, Becker et al. 2002) [13] |
| 3–8 % | 299 | Prospec- tive lon- gitudinal study |
The epidemiology of perimenstrual psycho- logical symptoms |
(Angst, Sellaro et al. 2001) [14] |
| 19% | 153 | Cross- sectional study |
Relationship b/w pre- menstrual tension syn- drome and anxiety in Chinese adolescents |
(Chau, Chang et al. 1998) [15] |
Prevalence and Severity of Premenstrual Symptoms
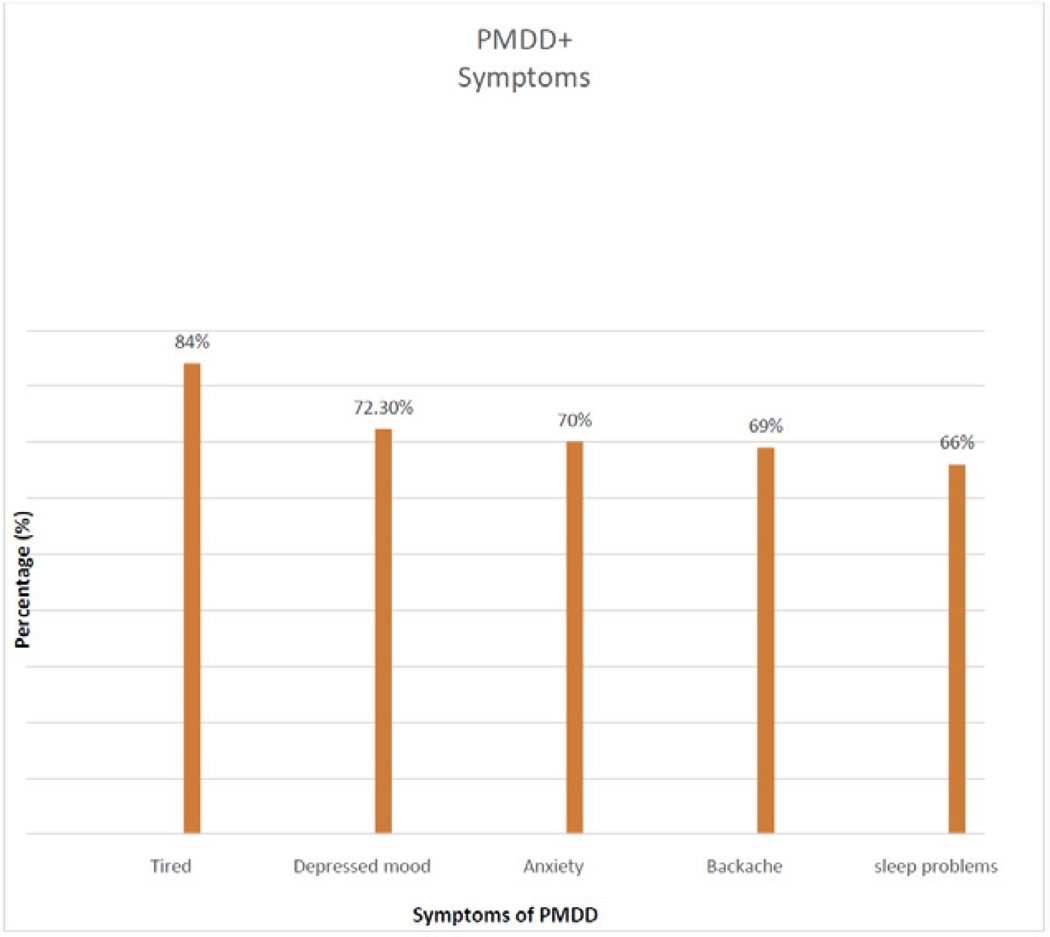
Studies show that the most common symptoms of PMDD are feeling tired (84%), depressed mood (72.3%), tearfulness (70.3%), anxiety (70%), and backache (69%), and sleep problems (66%) [11] (Figure 1).
Figure 1.
Prevalence and severity of premenstrual symptoms [11].
More severe symptoms such as anger attacks, severe depression and suicidal thoughts require special attention including psychiatric consultation [16]. A Korean study has reported the one-year prevalence of PMDD was 24 in the women of 18–64 years’ age group [17]. Women with PMDD have higher prevalence of psychiatric disorders, such as insomnia, suicidality, depression, and anxiety [17].
Sleep and Premenstrual Syndrome
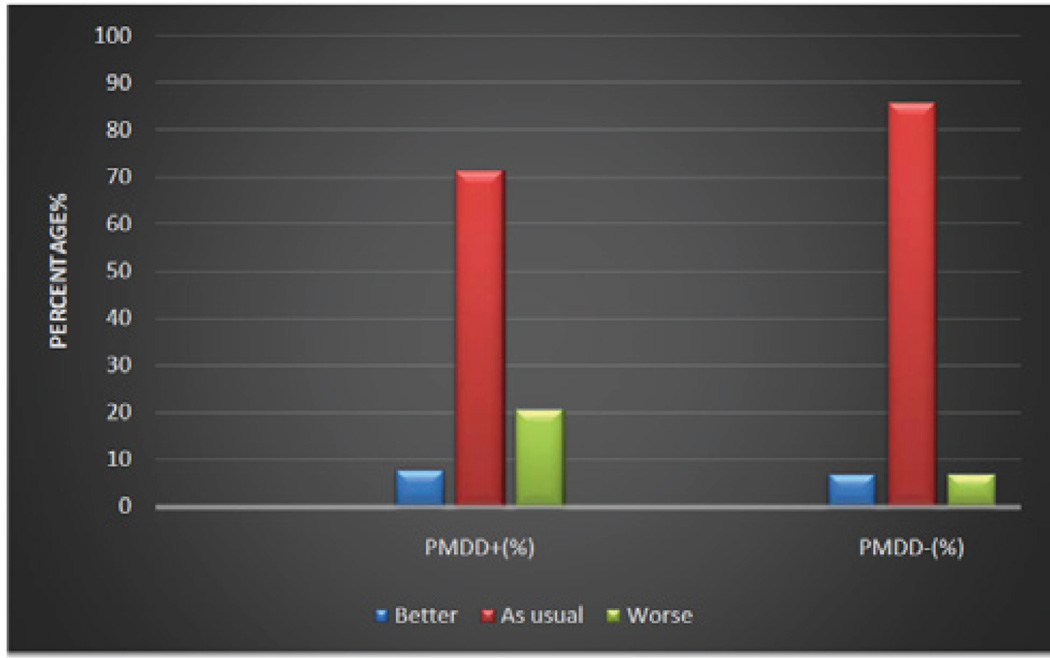
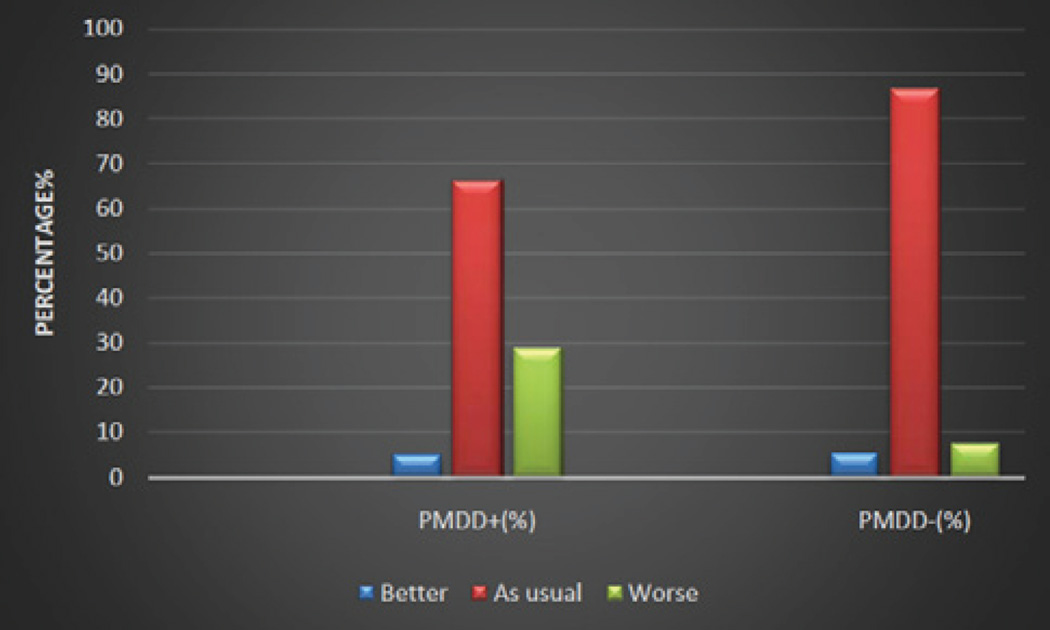
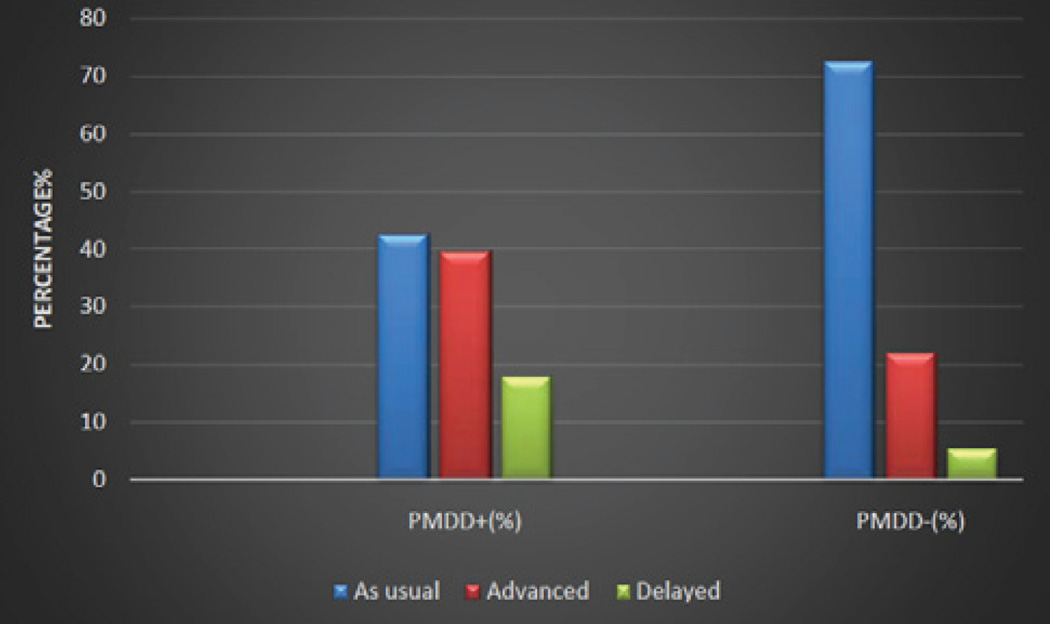
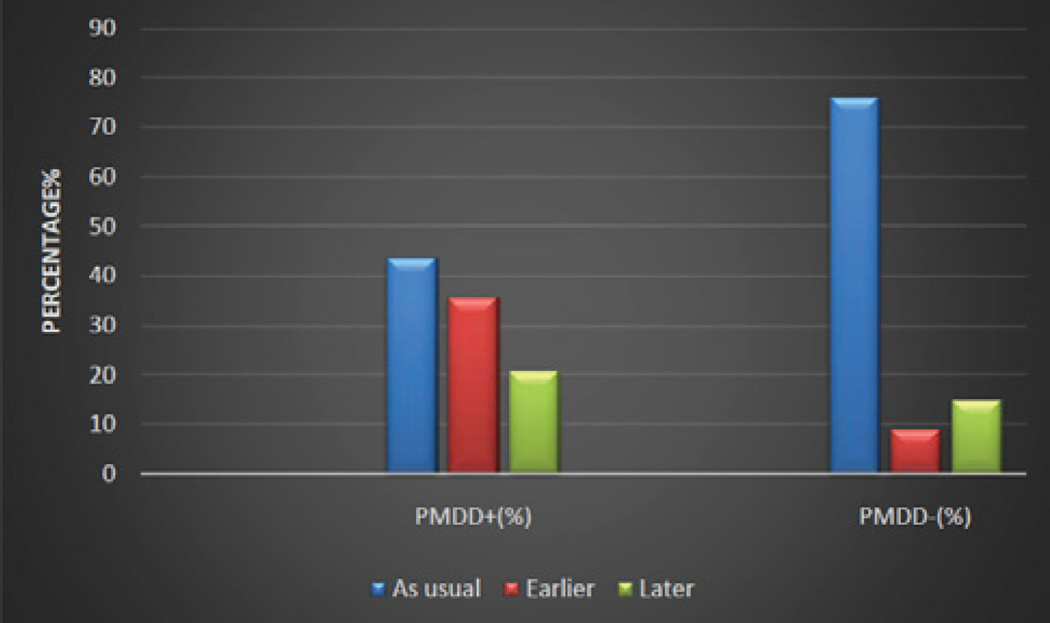
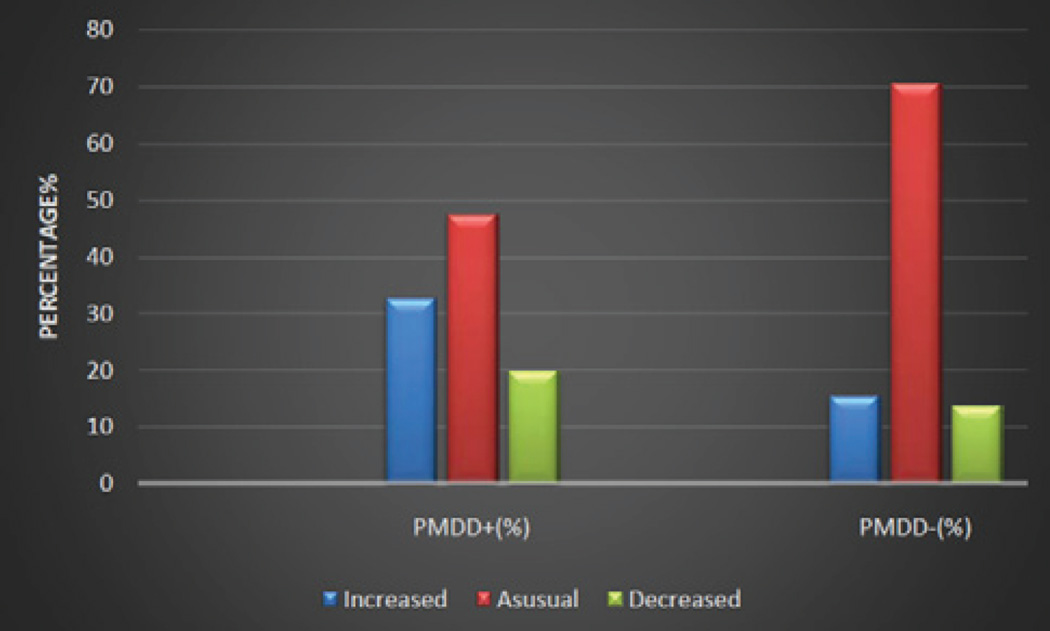
Studies show women with PMDD have poorer sleep than those without PMDD. Variables related to sleep included bed time, sleep quality, sleep onset latency, sleep maintenance and wake time [18, 19] (Figures 2–5).
Figure 2.
Sleep Quality. Comparison of sleep related variables between possible PMDD and no PMDD groups [19].
Figure 5.
Sleep maintenance. Comparison of sleep related variables between possible PMDD and no PMDD groups [19].
The menstrual phase is known to influence stage 2 sleep and REM sleep. In women, irrespective of PMDD, it has been found that stage N2 (non-rapid eye movement) (NREM 2) increases and REM (rapid eye movement) decreases during the mid-luteal phase, as compared to the early follicular phase [20]. However, slow wave sleep has been found to increase with the reduction in melatonin in PMDD women, as compared to those without PMDD [20]. Research has attempted to correlate sleep in PMS with polysomnographic findings. Only subtle EEG changes have been reported, that included increment of theta with reduction of delta proportion in the late luteal phase [21]. Despite comparable nocturnal awakenings and other EEG parameters, however, women with PMS have poorer sleep [21].
Role of Melatonin
Women with PMDD showed a decreased response to melatonin in their luteal phase as compared to the follicular phase. As a result, this deregulated circadian rhythm change could be the cause of the development of the mood disturbances in the late luteal phase of the menstrual cycle [22]. However, melatonin duration or timing, of its offset in the morning, has not been reported to correlate with the mood; rather, improvement in mood symptoms of PMDD has been found to be influenced by sleep deprivation, be it the sleep restriction in early or late night [23].
Role of Allopregnenalone in PMDD and Sleep Disturbances
Increased levels of progesterone and decreased levels of its metabolite (allopregnenalone) increase sleep disturbances in the luteal phase [21]. In women with PMDD, in the luteal phase the concentration of allopregnenalone diminishes even further, which causes increased levels of gamma-Amino butyric acid (GABA) due to an inability to increase GABA mediated inhibition. Increased levels of GABA are responsible for mood disturbance, anxiety, depression, and sleep disturbances in the luteal phase in women with PMDD [21, 24].
Daytime Sleepiness and Psychosocial Health in Women with PMDD
Women with PMDD show increased daytime sleepiness and fatigue when symptomatic as compared to when they are not, especially during the luteal phase. There is also a decline in performance at various routine activities [21].
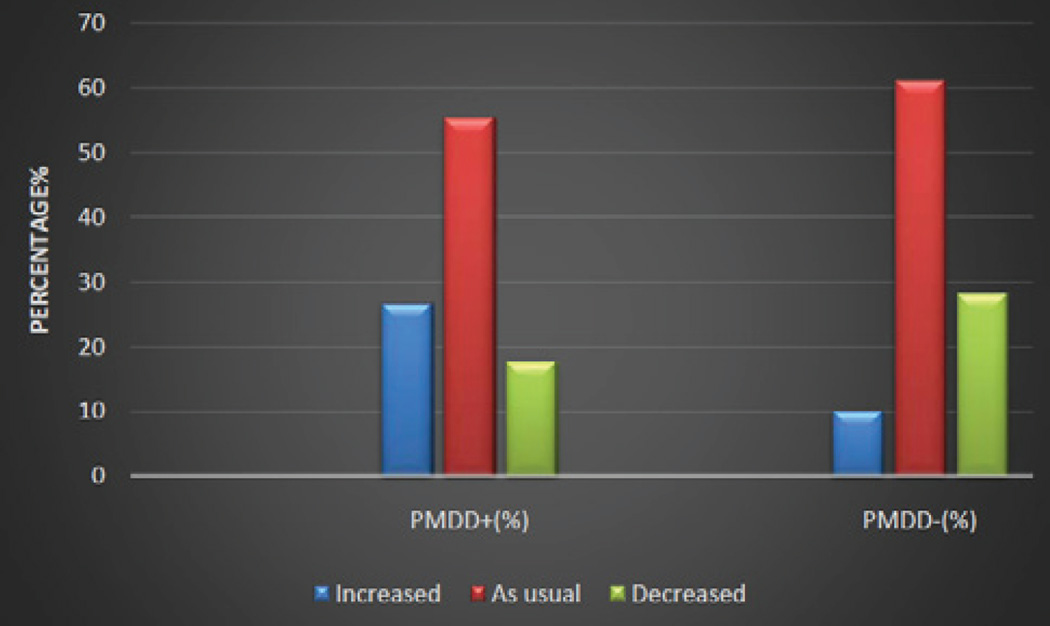
Treatment of PMDD
Patients with severe PMDD require treatment in the luteal phase of the menstrual cycle. Treatment options listed below are in addition to lifestyle modifications and stress management (Figures 6,7).
Figure 6.
Nocturnal awakening. Comparison of sleep related variables between possible PMDD and no PMDD groups [19].
Figure 7.
Wake time. Comparison of sleep related variables between possible PMDD and no PMDD groups [19].
Non Pharmacological Treatment
Bright light therapy is an effective treatment during the late luteal phase of the menstrual cycle; studies showed it reduces depression, premenstrual tension and stress in women with PMDD [25, 26].Total or partial sleep deprivation is also one of the effective treatments of PMDD; early and late sleep deprivation is effective in improving sleep quality [25].
Pharmacological Treatment
Severe mood instability requires pharmacological treatment. The most effective treatment for severe mood symptoms is selective serotonin reuptake inhibitors (SSRIs). These antidepressants are the first line of treatment in PMDD and have shown efficacy in the treatment of this disorder [17]. There is a close relationship between gonadal hormones and the serotonergic system, so treatment with SSRIs is the most effective approach. SSRIs are being used as a first line therapy for PMDD [27]. Tricyclicantidepressants (TCAs) can also be used to treat PMDD. When anxiety and insomnia are predominant symptoms, a benzodiazepine can also be prescribed in addition to an SSRI [28].Combined oral contraceptive pills (20 µg of ethinyl estradiol and 3 mg of the progestin drospirenone), have also shown effectiveness in PMDD treatment. Ethinylestradiole 20microgram/drospirenone 3mg have also been shown to help alleviate the symptoms of PMDD.
DISCUSSION
There are several etiological factors that can cause sleep disturbances in women of childbearing age; one major cause is PMDD. Women who have this disorder could experience insomnia, depression, fatigue, headache, abdominal bloating, breast tenderness and severe dysmenorrhea. These symptoms occur during the late luteal phase of a woman’s menstrual cycle and subside with the onset of menstruation [29]. The lowered levels of progesterone metabolite and higher levels of progesterone could contribute to the symptoms of PMDD, including mood symptoms such as anxiety, depression and tension [30].
Recent studies have shown that women experience various sleep disturbances during the late luteal phase of the menstrual cycle. Women with PMDD showed a decrease in melatonin secretion as compared to non-PMDD women. Sleep disturbance and decreased melatonin secretions due to hormonal fluctuations during the luteal phase of the menstrual cycle could explain the sleep complaints of PMDD [31]. Studies have also shown altered sleep and wake cycles in women with PMDD.
There is a decrease in rapid eye movement (REM) sleep and slow wave sleep (SWS) or stage N3 sleep in PMDD as compared to healthy individuals during the luteal phase as compared to the follicular phase. Altered REM sleep is a hallmark of PMDD sleep disturbances [32]. The estrogen level rises during the follicular phase of the menstrual cycle (especially day 14), and it has a vasodilation effect on the endothelium. As a result, women of reproductive age are less prone to cardiovascular diseases compared to postmenopausal women. In the late luteal phase, the estrogen level declines significantly and the progesterone level rises. The nasal administration of 17-β estradiol significantly causes vasodilation and is a protective factor against cardiovascular diseases. This hormonal fluctuation also plays an important role in menstruating women, and they can develop PMDD symptomatology [33, 34].
CONCLUSIONS
PMDD is a cluster of symptoms which usually occurs one week before the menstrual cycle. Symptoms include depressed mood, anxiety, sudden tearfulness, irritability, sleep disturbances, breast tenderness and bloating. All these symptoms occur in the late luteal phase of the menstrual cycle. According to DSM IVcriteria, there should be at least five symptoms present to diagnose PMDD.
The etiology of PMDD is complicated by the fluctuations of hormonal levels during the normal menstrual cycle. In the luteal phase, there is an increased level of progesterone and decreased level of its metabolite, allopregnenalone, which can cause increased sleep disturbances. Allopregnenalone increases dopamine levels thus leading to an increased anxiety state, which could cause sleep disturbances. Patients also experience daytime sleepiness, tiredness and fatigue.
There is no clinical laboratory test available to diagnose PMDD. It is a clinical diagnosis, and so patients are directed to keep a daily diary of symptoms in the days leading up to the onset of menses. These symptoms should be noted for two consecutive menstrual cycles in order to make a diagnosis of PMDD. The clinician should be aware of other disorders that can mimic PMDD. Treatment for severe symptoms of PMDD includes lifestyle modifications, stress management, light therapy, SSRIs, TCAs, oral contraceptives. Benzodiazepines can be administered, especially when anxiety symptoms are predominant.
There are only a few studies available that focus on treatment options for sleep complaints in women with PMDD. More studies are needed to evaluate this menstrual-related problem, which could be the major factor of women’s disturbed sleep in the reproductive period. We also emphasize diagnosing this sleep disorder early to get proper treatment in a primary care setting.
Figure 3.
Time to bed Comparison of sleep related variables between possible PMDD and no PMDD groups [19].
Figure 4.
Sleep onset latency. Comparison of sleep related variables between possible PMDD and no PMDD groups [19].
Acknowledgments
ACKNOWLEDGEMENT AND FUNDING
This work is supported by the following funding agencies: R25-HL105444 and R25-HL116378 (NHLBI); R01-MD007716 (NIMHD) to GJL. However, the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
DISCLOSURE STATEMENT
The authors have read the journal’s policy and have the following potential conflicts: This study was not an industry-supported study. S.R. Pandi-Perumal is a stockholder and the President and Chief Executive Officer of Somnogen Canada Inc., a Canadian Corporation. This does not alter his adherence to all the journal policies. He declares that he has no competing interests that might be perceived to influence the content of this article. All remaining authors declare that they have no proprietary, financial, professional, nor any other personal interest of any nature or kind in any product or services and/or company that could be construed or considered to be a potential conflict of interest that might have influenced the views expressed in this manuscript.
REFERENCES
- 1.Consensus Conference Panel. Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. J Clin Sleep Med. 2015;11:931–952. doi: 10.5664/jcsm.4950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manber R, Bootzin RR. Sleep and the menstrual cycle. Health Psychol. 1997;16:209–214. doi: 10.1037//0278-6133.16.3.209. [DOI] [PubMed] [Google Scholar]
- 3.Pearlstein T, Yonkers KA, Fayyad R, Gillespie JA. Pretreatment pattern of symptom expression in premenstrual dysphoric disorder. J Affect Disord. 2005;85:275–282. doi: 10.1016/j.jad.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Halbreich U, Backstrom T, Eriksson E, O’brien S, Calil H, Ceskova E, et al. Clinical diagnostic criteria for premenstrual syndrome and guidelines for their quantification for research studies. Gynecol Endocrinol. 2007;23:123–130. doi: 10.1080/09513590601167969. [DOI] [PubMed] [Google Scholar]
- 5.Farage MA, Neill S, MacLean AB. Physiological changes associated with the menstrual cycle: a review. Obstet Gynecol Surv. 2009;64:58–72. doi: 10.1097/OGX.0b013e3181932a37. [DOI] [PubMed] [Google Scholar]
- 6.Ryu A, Kim TH. Premenstrual syndrome: A mini review. Maturitas. 2015;82:436–440. doi: 10.1016/j.maturitas.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Freeman EW. Treatment of depression associated with the menstrual cycle: premenstrual dysphoria, postpartum depression, and the perimenopause. Dialogues in Clinical Neuroscience. 2002;4:177. doi: 10.31887/DCNS.2002.4.2/efreeman. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bottomley C, Bourne T. Diagnosis and management of ovarian cyst accidents. Best Pract Res Clin Obstet Gynaecol. 2009;23:711–724. doi: 10.1016/j.bpobgyn.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Spinelli C, Di Giacomo M, Cei M, Mucci N. Functional ovarian lesions in children and adolescents: when to remove them. Gynecol Endocrinol. 2009;25:294–298. doi: 10.1080/09513590802530932. [DOI] [PubMed] [Google Scholar]
- 10.Spinelli C, Di Giacomo M, Mucci N, Massart F. Hemorrhagic corpus luteum cysts: an unusual problem for pediatric surgeons. J Pediatr Adolesc Gynecol. 2009;22:163–167. doi: 10.1016/j.jpag.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 11.Bakhshani NM, Mousavi MN, Khodabandeh G. Prevalence and severity of premenstrual symptoms among Iranian female university students. J Pak Med Assoc. 2009;59:205–208. [PubMed] [Google Scholar]
- 12.Silva CM, Gigante DP, Carret ML, Fassa AG. Population study of premenstrual syndrome. Rev Saude Publica. 2006;40:47–56. doi: 10.1590/s0034-89102006000100009. [DOI] [PubMed] [Google Scholar]
- 13.Wittchen HU, Becker E, Lieb R, Krause P. Prevalence, incidence and stability of premenstrual dysphoric disorder in the community. Psychol Med. 2002;32:119–132. doi: 10.1017/s0033291701004925. [DOI] [PubMed] [Google Scholar]
- 14.Angst J, Sellaro R, Merikangas KR, Endicott J. The epidemiology of perimenstrual psychological symptoms. Acta Psychiatr Scand. 2001;104:110–116. doi: 10.1034/j.1600-0447.2001.00412.x. [DOI] [PubMed] [Google Scholar]
- 15.Chau JP, Chang AM, Chang AM. Relationship between premenstrual tension syndrome and anxiety in Chinese adolescents. J Adolesc Health. 1998;22:247–249. doi: 10.1016/S1054-139X(97)00206-1. [DOI] [PubMed] [Google Scholar]
- 16.Dean BB, Borenstein JE, Knight K, Yonkers K. Evaluating the criteria used for identification of PMS. J Womens Health (Larchmt) 2006;15:546–555. doi: 10.1089/jwh.2006.15.546. [DOI] [PubMed] [Google Scholar]
- 17.Hong JP, Park S, Wang HR, Chang SM, Sohn JH, Jeon HJ, et al. Prevalence, correlates, comorbidities, and suicidal tendencies of premenstrual dysphoric disorder in a nationwide sample of Korean women. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1937–1945. doi: 10.1007/s00127-012-0509-6. [DOI] [PubMed] [Google Scholar]
- 18.Mauri M, Reid RL, MacLean AW. Sleep in the premenstrual phase: a self-report study of PMS patients and normal controls. Acta Psychiatr Scand. 1988;78:82–86. doi: 10.1111/j.1600-0447.1988.tb06304.x. [DOI] [PubMed] [Google Scholar]
- 19.Gupta R, Lahan V, Bansal S. Subjective sleep problems in young women suffering from premenstrual dysphoric disorder. N Am J Med Sci. 2012;4:593–595. doi: 10.4103/1947-2714.103326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shechter A, Lespérance P, Ng Ying Kin NM, Boivin DB. Nocturnal polysomnographic sleep across the menstrual cycle in premenstrual dysphoric disorder. Sleep Med. 2012;13:1071–1078. doi: 10.1016/j.sleep.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 21.Baker FC, Driver HS. Circadian rhythms, sleep, and the menstrual cycle. Sleep Med. 2007;8:613–622. doi: 10.1016/j.sleep.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 22.Parry BL, Hauger R, LeVeau B, Mostofi N, Cover H, Clopton P, et al. Circadian rhythms of prolactin and thyroid-stimulating hormone during the menstrual cycle and early versus late sleep deprivation in premenstrual dysphoric disorder. Psychiatry Res. 1996;62:147–160. doi: 10.1016/0165-1781(96)02905-8. [DOI] [PubMed] [Google Scholar]
- 23.Parry BL, Meliska CJ, Martínez LF, López AM, Sorenson DL, Hauger R, et al. Late, but not early, wake therapy reduces morning plasma melatonin: relationship to mood in Premenstrual Dysphoric Disorder. Psychiatry Res. 2008;161:76–86. doi: 10.1016/j.psychres.2007.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rapkin AJ, Morgan M, Goldman L, Brann DW, Simone D, Mahesh VB. Progesterone metabolite allopregnanolone in women with premenstrual syndrome. Obstet Gynecol. 1997;90:709–714. doi: 10.1016/S0029-7844(97)00417-1. [DOI] [PubMed] [Google Scholar]
- 25.Parry BL, Berga SL, Mostofi N, Sependa PA, Kripke DF, Gillin JC. Morning versus evening bright light treatment of late luteal phase dysphoric disorder. Am J Psychiatry. 1989;146:1215–1217. doi: 10.1176/ajp.146.9.1215. [DOI] [PubMed] [Google Scholar]
- 26.Lam RW, Carter D, Misri S, Kuan AJ, Yatham LN, Zis AP. A controlled study of light therapy in women with late luteal phase dysphoric disorder. Psychiatry Res. 1999;86:185–192. doi: 10.1016/s0165-1781(99)00043-8. [DOI] [PubMed] [Google Scholar]
- 27.Yonkers KA. Antidepressants in the treatment of premenstrual dysphoric disorder. J Clin Psychiatry. 1997;58:4–10. [PubMed] [Google Scholar]
- 28.Krejza J, Mariak Z, Nowacka A, Melhem ER, Babikian VL. Influence of 17-beta-estradiol on cerebrovascular impedance during menstrual cycle in women. J Neurol Sci. 2004;221:61–67. doi: 10.1016/j.jns.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 29.Chung SH, Kim TH, Lee HH, Lee A, Jeon DS, Park J, et al. Premenstrual syndrome and premenstrual dysphoric disorder in perimenopausal women. J Menopausal Med. 2014;20:69–74. doi: 10.6118/jmm.2014.20.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rapkin AJ, Morgan M, Goldman L, Brann DW, Simone D, Mahesh VB. Progesterone metabolite allopregnanolone in women with premenstrual syndrome. Obstet Gynecol. 1997;90:709–714. doi: 10.1016/S0029-7844(97)00417-1. [DOI] [PubMed] [Google Scholar]
- 31.de Zambotti M, Nicholas CL, Colrain IM, Trinder JA, Baker FC. Autonomic regulation across phases of the menstrual cycle and sleep stages in women with premenstrual syndrome and healthy controls. Psychoneuroendocrinology. 2013;38:2618–2627. doi: 10.1016/j.psyneuen.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shechter A, Boivin DB. Sleep, Hormones, and Circadian Rhythms throughout the Menstrual Cycle in Healthy Women and Women with Premenstrual Dysphoric Disorder. Int J Endocrinol. 2010;2010:259–345. doi: 10.1155/2010/259345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adams Hillard PJ. Menstruation in adolescents: what do we know? And what do we do with the information? J Pediatr Adolesc Gynecol. 2014;27:309–319. doi: 10.1016/j.jpag.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 34.Ciccone MM, Scicchitano P, Gesualdo M, Fornarelli F, Pinto V, Farinola g, et al. Systemic vascular hemodynamic changes due to 17-β-estradiol intranasal administration. J Cardiovasc Pharmacol Ther. 2013;18:354–358. doi: 10.1177/1074248413484385. [DOI] [PubMed] [Google Scholar]